- 1School of Medical Sciences, University of Hyderabad, Hyderabad, India
- 2Health Systems and Population Studies Division, International Centre for Diarrhoeal Disease Research, Dhaka, Bangladesh
Over the past two decades, there has been an increased demand for Public Health Education (PHE) in South Asia. While this region has a large number of Public Health (PH) institutions, the quality of PHE has not been aligned with the core PH competencies. In this article, we present an overview of Master of Public Health (MPH) programs across South Asian countries. An extensive systematic search on various web search engines regarding PH course offerings was conducted, including specific institute and educational websites. By 2021, more than 180 institutions in South Asia provided an MPH degree. Most of these institutions/universities were found in India, Pakistan, and Bangladesh, and a few among these institutions were established as independent Schools of Public Health (SPH), separate from medical colleges, and had a multidisciplinary faculty. But, dedicated training facilities in the specialized field of public health were not found in most of these institutions. Generally, a well-defined MPH curriculum is not currently available except in India where the University Grants Commission (UGC) guideline for a model MPH curriculum has been proposed by the Ministry of Health and Family Welfare. The entry criteria for an MPH degree in India is accepting students in multidisciplinary fields, while in other South Asian countries this is primarily restricted to medical/paramedical students with a basic understanding of preventive medicine. The aim of this review was to document the current and future PHE opportunities and challenges in South Asia.
Introduction
Public health (PH), an interdisciplinary field takes into account not only physical ailments but also incorporates psychological and social well-being. PH encompasses the science and art of preventing diseases, prolonging life, and improving quality of life through organized efforts and informed choices of society, organizations, communities, and individuals (1). In 1978, the Alma Ata Conference restated the critical role of PH in accomplishing health for all by addressing the importance of equity, community participation, and inter-sectoral collaboration (2). The determinants of health in the population and analysis of the threats are grounded in the PH approach (3).
For the growth and prosperity of a nation, health is a key aspect to be considered (4). The field of PH encompasses various courses including epidemiology, bio-statistics, management of health services, environmental health, community health, behavioral health, health economics, public health policy, health politics, occupational safety including sub-fields such as disability, gender issues in health, mental health, and maternal and child health (5). On an international level, conflicting viewpoints on the approach to public health issues may arise, for instance, the goal of preventive vs. curative services, selective vs. comprehensive primary health care, or integrated (horizontal) vs. top down (vertical) programs (6). Intervention strategies that incorporate the PH sector's collaboration must contain the establishment of appropriate graduate and post-graduate study opportunities in PH.
Significance of the review
The South Asian countries form the South Asian Association for Regional Cooperation (SAARC) including Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka. The SAARC nations are home to nearly one-fifth of the world's population and have been suffering from a vast number of health-related challenges such as a double burden of infectious and non-communicable diseases (NCDs), malnutrition, unsafe pregnancies, and a rapidly escalating plethora of NCD epidemics (7). Even though PH existed for over a century, it is still an evolving field in SAARC nations. PH knowledge is necessary to help students develop community health by organizing, evaluating, and implementing effective and equity-based PH programs (8). However, the multidisciplinary field of PH needs coordinated efforts with teams of PH workforce, specialists, and professionals from diverse sectors who contribute to the broader field of PH (9). The SPH is better placed to offer comprehensive health professional education, conduct multidisciplinary research, population studies, and adopt collaborative partnerships to achieve the sustainable development goals (SDGs) (9). With an aim to examine the challenges and opportunities in professional PHE in South Asia, a brief review was undertaken.
Review of the literature
MPH programs in South Asia were explored by Google scholar, CINAHL, Pub Med, Web of Science, ELDIS using keywords-PHE, South Asia, SAARC nations, higher education, study programs, MPH/M.Sc., career opportunities for PH graduates, challenges of PHE in SAARC nations. The Masters of Public Health (MPH) program is of 2 years duration as per the University Grants Commission standards (10). Post Graduate Diploma in Health Science, which is comparable to a 1-year MPH, was not included. The University websites, and education-based websites including Collegedunia.com (11), career360 (12), Eduvision (13), Collegedekho (14) were searched. Further, information on the SAARC nation's PHE, current situation, and challenges was obtained from the World Health Organization (WHO) and the Centre for Disease Control and Prevention (CDC) country pages. Articles in other regional languages apart from English, Bachelor's degree in Public Health, and doctoral programs were excluded.
Current status of public health education in SAARC nations
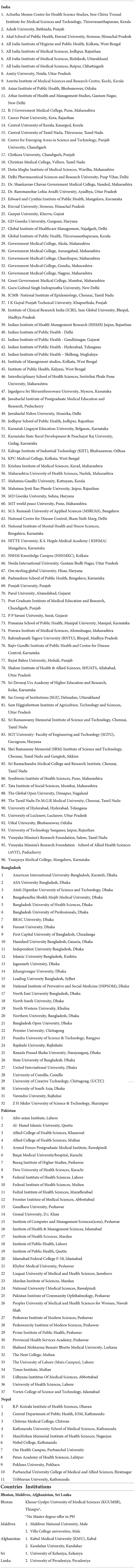
India
In India, 95 institutions were identified that provide MPH programs of 2 years duration with English as the medium of instruction. The number of MPH programs has increased dramatically during the last two decades and specifically over the last couple of years with the onset of the COVID-19 pandemic (15). However, it is necessary to recognize that the curricula and criteria for admissions in these programs are diverse (16). The universities follow the Model Curriculum floated by the Ministry of Health and Family Welfare (17). A new National Education Policy (NEP 2020), replacing the National Policy on Education from 1986, addressing the importance of research and a multi-disciplinary approach has been approved by the Union Cabinet of India (18). Under the NEP 2020, Higher Education Institutes (HEIs) in India have a choice of providing a 1 year Master's degree for those who have done their Bachelors degree of 4 years that includes research component in the programme (19). A 2-year Master's program with research activities in the second year is offered for those who obtained a bachelor's degree in 3 years (18). The NEP 2020 allows students to experience research-based learning on par with the academic structure of HEIs in developed countries (18, 19).
The MPH program includes five traditional core areas proposed by the Association of Schools and Program of Public Health (ASPPH). These disciplines are Epidemiology, Bio-statistics, Environmental Health Sciences, Health Policy and Management, Social and Behavioral Sciences. Some universities offer unique non-core subjects such as global health technology in PH by Kalinga Institute of Industrial Technology, food and nutrition courses and field posting at Career Point University. Medical colleges have traditionally been the primary source of PH specialty training in India (20). Outside of medical institutions, there has been an intentional shift in the past decade toward the establishment of SPH that allow non-medical personnel to obtain academic competencies in PH (21). Incidentally, India is the largest educational hub among the SAARC nations and accepts students from neighboring and other foreign nations to enroll in HEIs offering an MPH course. The Government of India through the Indian Council for Cultural Relations (ICCR) offers scholarships for students from SAARC nations and the MPH course has gained increased demand over the past 2 years. The private-public partnership (PPP) model too has boosted MPH programs that provide PHE to students in the region. The Public Health Foundation of India (PHFI) remains a one-of-a-kind private–public collaboration that aims to reinvigorate PH by pooling resources from the government and private philanthropy to address the most pressing public health issues (22).
Bangladesh
In Bangladesh, 32 institutions offer MPH programs as of mid-year 2022. At Jahangirnagar University, there has been a M.Sc. in PH degree program for which only B.Sc. in PH students of this department can enroll. Most of the courses are of 1-year duration and the medium of instruction is English, while some courses are 16/18 months in duration. There is only one University (First capital) that provides an MPH degree with 2-year duration for students from a non-medical background. The most reputable University for an MPH degree is the James P. Grant School of Public Health established in 2005 at BRAC University. This program offers an innovative 12-month MPH curriculum that begins with 6 months of training in basic PH skills in the context of rural health action on the Savar rural campus, followed by training on the BRAC University campus (23).
Pakistan
In Pakistan, PH programs are available in 44 institutions including the MPH and MSPH degrees. Most of the courses were regular (2 year duration) and full time. The Provincial Health Services Academy provides a 4-year program and the Institute of PH and Gandhar University offer a 1-year MPH program. The entry criteria include medical/non-medical background and few universities require work experience to enroll in the MPH program (e.g., Jinnah Sindh Medical University). Very few universities provide training to graduates in primary health care and research including Jinnah Sindh Medical University.
Nepal
Ten universities provide MPH programs of 2 years duration, except Manmohan Technical University and Tribhuvan University, which offer programs with a duration of one and half years and 1 year, respectively. Some universities ask for the TOEFL/IELTS test as a pre-requisite for admission (notably Purbanchal University in Biratnagar).
Bhutan, Maldives, Afghanistan, and Sri Lanka
In Bhutan, Bachelor's of Public Health is offered by Khesar Gyalpo University of Medical Sciences (KGUMSB). There is no MPH program offered.
The Maldives higher education system consists of four universities with a total of 40 study programs. Two universities, the Maldives National University and the Villa College University, provide MPH program with English as the medium of instruction. However, there is no core course offered in Statistics.
In Afghanistan, a total of nine provinces have 87 universities. The website of universities was not updated and meager information was available. Only two universities appeared to offer an MPH credential with the medium of instruction as English. The Minister of Higher Education in partnership with WHO formally created the MPH program at Kabul Medical University (KMU) in the year 2013. Another MPH program was developed at Kandahar University with funding from the United States of America Agency for International Development (USAID), University Support and Workforce Development Program (USWDP), and technical help from Johns Hopkins University in the United States of America (23).
In Sri Lanka, the University Grants Commission provides oversight of 17 Sri Lankan universities and other educational institutions, all of which are classified as HEIs. A joint MPH program is provided by two institutions: the University of Kelaniya and the University of Peradeniya. Thus, by 2022 nearly 183 institutions in SAARC nations provided an MPH degree (Table 1).
Core competencies of public health education
The essential minimum set of attributes, such as applied knowledge, skills, and attitudes, that enable an individual to perform a set of tasks to an appropriate standard efficiently and effectively is defined as core competencies (24). Core competencies provide a common shared language for all PH professions to define what all are expected to be able to do to work optimally (25).
The COVID-19 pandemic has underlined the necessity of core competencies in performing PH functions such as disease outbreak prevention, detection, and response (26). However, most resource-poor countries struggle to impart the necessary PH competencies to the public health personnel to conduct these and other PH duties successfully (22, 27). In order to effectively deliver the critical PH functions such as epidemiological surveillance, situation assessments, and health promotion required that the PH professional should have fundamental competencies (28, 29). The functions are multidisciplinary in nature and not limited to a single program or topic, and every staff at all levels in the PH system should have these core skills established (26). Toward this goal, the core competencies of the Association of Schools and Program of Public Health (ASPPH) in the United States established by a national consensus in 2006 remain a useful resource and reference for PH educators, administrators, and students (30). The ASPPH proposed Core Competence in Public Health model includes competencies in five traditional PH core areas as well as seven interdisciplinary/cross-cutting areas (Figure 1). The MPH students graduated from a Council on Education for Public Health (CEPH)-accredited school or program of PH in the United States are equipped with these core competencies. The discipline specific competencies are Bio-statistics, Environmental Health Sciences, Epidemiology, Health Policy and Management, Social and Behavioral Sciences. The Interdisciplinary/Cross-cutting competencies include Communication and Informatics, Diversity and Culture, Leadership, Public Health Biology, Professionalism, Program Planning, Systems Thinking. The core competency assessment for MPH graduates in low and middle-income countries (LMICs) is uncommon and there exists a need for a Accreditation Council on PHE in the region (26, 30).

Figure 1. Core competency model for the MPH degrees proposed by Association of Schools and Program of Public Health (ASPPH) 30.
The WHO-ASPHER (Association of Schools of Public Health in the European Region) Competency Framework can be used as a starting point for more context-specific competencies to be developed (31). It contains three core categories: Content and context, Relations and interactions, and Performance and achievement.
Among South Asian countries, we found few studies regarding core competencies and one study emphasized the cross-cutting domain that included health communication and informatics, health management and leadership, professionalism, systems thinking, and PH biology along with the five core areas (32, 33). A study from Uttar Pradesh in India has identified core competencies for practicing PH professionals using a Delphi exercise (26). This study proposed 48 competency statements across eight domains: PH sciences, assessment and analysis, policy and program management, financial management and budgeting, partnerships and collaboration, social and cultural determinants, communication, and leadership.
Challenges and opportunities of PHE for SAARC nations
The South Asian countries have similar health profiles to their neighboring countries. India, as the biggest among the SAARC nations in the region, has encountered challenges such as a scarce PH workforce; a lack of skilled workers in accordance with the health system needs of the population, and an unequal range of types and levels of ability of health workforce (34). There are gaps in PHE requiring in-depth understanding and addressing including the quantity and quality of PH education (35). The shortages in the health workforce are not the only issues, the limited availability of jobs, and lack of opportunities to absorb the recent MPH graduates within the health system, NGOs, and the industry seems a huge concern and this scenario was affecting the enrolment in higher studies in PH (36). In the wake of the pandemic, “Health” has become a central issue in our lives; thus, to attain it, the SAARC nations need to act in an organized manner. The curricula require to evolve in such a way that all levels of students can find the opportunities to enter the PH program and acquire training on health and human ecology (37). As PH deals with the health of the population as a whole, the term “Health literacy” can be a goal of our learning system in a true sense (38). Explicitly, the spread of health challenges and duties in society creates a demand for health training in a variety of vocations that do not include the word “health” in the title (37). A small percentage of students join MPH program by choice after undergraduate studies, prompted by the desire to work in the health-care field (22). However, research capabilities, financial accessibility, and innovation are strengths of SPH in India. But there is a need to improve collaborations and synchronize training with well-defined career routes (39).
Public health allied practitioners have always been viewed as being at the bottom of the health-care hierarchy (40). When there will be appropriate course curricula with evidence-based research opportunities and training in epidemiological studies, a better workforce in health care will be added. While there has always been a mismatch between supply and demand for healthcare workers in Bangladesh's healthcare sector, the situation has been different for allied PH practitioners and medical professionals (40).
Competence is critical in determining a health worker's capacity and preparedness for offering high-quality care (41). According to the findings of a study, academic institutions are creating PH graduates that lack the necessary abilities to operate in a variety of PH disciplines, and also the present MPH curriculum varies greatly between institutes with different emphasis (42, 43). A recent scoping analysis sheds light on the state of the MPH program across South Asian countries. Due to the lack of a comprehensive and consistent curriculum, the competencies acquired by these graduates may vary (44). WHO South-East Asia region (45) showed vast variation in institutes and courses offered regardless of the existence of numerous postgraduate courses and undergraduate courses in these countries. It demonstrates that there is a significant gap in our understanding of how effectively research outputs affect PH decision-making as a result of this gap between PHE and real-world PH policies and practices (46).
MPH is largely a professional practice degree in Nepal, as it is in most other SAARC nations. Despite this, MPH graduates are likely to work in research and academic settings due to the scarcity of possibilities for further education in PH (47). “Community Medicine” is an integral part of Nepalese medical school curricula. It was observed that a synergistic relationship between departments of PH and clinical sciences was not well integrated in actual practice (47). The notion that research has to be “community-based” has further discouraged interdisciplinary research within these institutions. The SPH in Nepal is located in educational institutions affiliated with specialized health centers, hospitals, and peripheral health facilities, all of which are engaged in the treatment and prevention of disease. Some of these diseases/conditions include infectious and chronic diseases, trauma, maternal and child health problems, and mental illness (47).
The literature available regarding PHE and training programs in Pakistan is scant. One study involving In-depth interviews with stakeholders revealed PH practitioners preferred to recruit someone with a medical degree (48). They further seek practical experience, skills in program coordination, resource mobilization, management, analytical skills, grant-writing abilities, strategic thinking, monitoring, and program evaluation as well as specific knowledge of Pakistan's health system. Investing in a PH training program is difficult as the government of Pakistan funds only 5% of the Health Service Academy's budget and the rest is to be raised through grants for capacity building and research (48). The literature on medical education has continued evidence of dispute on whether or not to include PH in a basic medical curriculum. Woodward, argues that the “clinical imperative of diagnosis and treatment is so firmly entrenched in the minds of students and in the cultures of medical schools that PH will always be diminished and elbowed to one side in medical curricula” (49). Usually, the dissimilarity is in the fundamental, philosophical, and practical differences between these two fields (50). The emphasis of PH is on the health of populations and stress prevention and health promotion, whereas clinical medicine focuses on the individual's health by concentrating on curative measures e.g., diagnosis and treatment (50). However, the COVID-19 pandemic highlighted the need for interdisciplinary collaboration to address the worsening pre-existing disparities and inequity that exacerbated the lack of access to health care around the world (51). The epidemic has raised awareness of the urgency for more funding for SPH and PH programs to create and execute new courses and techniques for acquiring key competencies (51, 52).
During the eighteenth and nineteenth centuries, the focus shifted to the development of personal preventive services and also the establishment of maternal and child health services including mass vaccination (53). To ensure “Health for all”, preventive practice in PH in parallel with the clinical practice was emphasized. By the early twentieth century, it was clear that PH was required to combat chronic diseases. Over the recent decades, it has become obvious that PH is needed to address the social, political, and commercial determinants of health, including through actions outside of the health system, such as in the agriculture sector, rural development, urban planning, and Health in all policies (53). Some studies document the surge in enrolment of MPH education following the onset of the COVID-19 pandemic. The applications to Masters in PH programs in the USA had seen a sharp increase (20%) for the academic year 2020-21 and were nearly 40,000, according to the Association of Schools and Programs of PH (54). Likewise, the number of institutions and universities offering MPH courses has gone up in South Asia specifically in India. But, there are no studies available in current literature that estimated the number of students successfully graduating with MPH degrees annually.
For obvious reasons, the COVID-19 pandemic has had a particularly important influence on the need for online education in PH. The MOHFW, Government of India has recognized these training programs as an innovative model of education in their National innovation summits (55). The holistic education envisaged under the NEP 2020 offers students at HEIs an internship with local industries/craftspeople as well as research internships at their own/other institutions. This enables them to actively engage with practical learning and, as a result, improve their skills and employability. The credits earned at foreign universities will be allowed to be counted toward the award of a degree if suitable and in accordance with the rules of each HEI (18). In Bangladesh, the government has big plans for digital and e-learning with the goal of making it a permanent part of the educational system (56). In Pakistan, The Prime Institute of Public Health offers competency-based PH courses that are practice-oriented to individuals with at least 14 years of education and interest in PH (57).
Evaluation method of MPH program in South Asia
As discussed earlier, the content and structure of the WHO-ASPHER competency have proposed the development of a new approach to evaluating the MPH level programs, which highlighted that there is a wide range of competencies required to perform professional duties in PH (58). The choice-based credit system (CBCS) gives students the option of three different course types: Core, Elective, and Foundation. The CBCS is followed by most South Asian universities. But few universities lack the option of fundamental courses. Regarding the evaluation, we found that the method is mostly formative (Internally by the concerned faculty member through quizzes, tutorials, lab works, home assignments, class tests, class participation, term papers, and internal exams) and summative (Externally by the Office of the Controller of Examinations of concern University through year/semester-end examinations). In Bangladesh, private universities mostly follow the semester system, while public universities offer annual system courses; especially, while for other countries, majority of the universities offered semester system courses. The total credits varied across South Asian universities for MPH programs with most universities requiring more than 50 credits except Afghanistan (46 credit). The universities offered internship opportunities and facilitated the process, but a program-based research opportunities were generally lacking. Despite the vast scope, there is a strong necessity to improve cooperation and align training and employment paths as well as effective community engagement techniques in the region. An MPH program evaluation survey revealed that MPH graduates should be able to monitor health problems and epidemics in their communities, develop indicators and instruments to monitor and evaluate community health programs, develop proposals, apply biostatistics principles in public health, conduct operations/action research, understand social and community influences on public health, and involve the community in planning, delegating, and evaluating community health programs (33). In this review, the scarcity of literature on the evaluation of MPH programs in South Asia presents a challenge. A study on the transdisciplinarity of India's master's level public health programs revealed the lack of inclusivity of non-medical disciplines (59).
Strengths and limitations of the review
This review provides an up-to-date perspective on the availability of rapidly emerging professional public health training and education programs in South Asia. The introduction of the National Education Policy, 2020 in India has large positive implications for Public Health Education nationally, regionally, and globally. This review updates the public health educational institutions that emerged in response to the pandemic in the region and generate greater awareness among the general public and PH professionals. Further, it emphasizes the need for a robust public health curriculum and core competencies for aspiring professionals who would constitute the future public health workforce in the region. However, there are some limitations, such as a lack of information pertaining to country-wise number of students' enrollment, professional accreditation, and regulatory bodies in South Asia to evaluate public health education.
Conclusion
The professional PHE is evolving rapidly in the South Asia region. Among the eight SAARC nations, India has structured and well-defined PH course curricula. Indian universities and HEIs welcome foreign nationals for higher studies in PH. The literature and information on PHE are more readily available for India than for other SAARC nations. Till now Bhutan, Maldives, Afghanistan, and Sri Lanka have not expanded the scope of PHE in independent schools or separated it from medical schools. Some countries are strict in the eligibility criteria in Master's programs to only medical students (Sri Lanka, Afghanistan). Therefore, as PH is a multidisciplinary field, students from varied backgrounds should find the chance to enroll in the program. Since PH literacy is required for the recognition and fundamental grasp of how the social and physical environment influences health, it is a legitimate and worthwhile societal aim.
The emphasis on core competencies will be meaningful if it culminates with a job or higher education opportunities. To this effect, the engagement and involvement of academia, industry, and government stakeholders are essential. However, currently, there are no clear avenues for absorbing MPH graduates within the existing government health care infrastructure, NGO, or industries. A robust PH culture can be promoted by ensuring training facilities for students from both medical and non-medical backgrounds, a necessity in the twenty-first century. As the new PH graduates enter the government or development sectors, more opportunities to enroll non- medical graduates in the PH workforce become necessary. There is a lack of literature and critical analysis regarding PHE in the South Asia region. There is a compelling need to address the gaps and the consequent scope of PHE and job opportunities in the South Asian region. Given the spread of Institutes and Schools of Public Health in South Asia in recent decades, it would be worthwhile to evaluate the PHE in the region. South Asian countries must examine their human resource needs for health and create the capacity to meet education and health service needs in the future.
Author contributions
CTA contributed to the conceptualization and project administration. CTA and KA contributed to the methodology. KA conducted the investigation and contributed to writing original draft. CTA and KM performed supervision and acquired resources, performed validation, contributed to writing, reviewing, and editing of the manuscript. All authors read and approved the final version of the manuscript for publication and their respective contributions.
Acknowledgments
The University of Hyderabad provided funding for resources like infrastructure, library and logistics under the Institute of Eminence program by the Ministry of Education, Government of India. KA is the recipient of Scholarship from Indian Council for Cultural Relations (ICCR), Government of India.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Winslow C-E. The untilled fields of public health. Science. (1920) 51:23–33. doi: 10.1126/science.51.1306.23
2. Petrakova A, Sadana R. Problems and progress in public health education. Bull World Health Organ. (2007) 85:963–5. doi: 10.2471/BLT.07.046110
3. CDC. What is Public Health. (2022). Available online at: https://www.cdcfoundation.org/what-public-health#:~:text=Public%20health%20is%20the%20science,and%20responding%20to%20infectious%20diseases
4. World Health Organization. South-East Asia public health initiative 2004-2008. New Delhi: WHO Regional Office for South-East Asia (2004).
5. Perdiguero E. Anthropology in public health. Bridging differences in culture and society. J Epidemiol Commun Health. (2001) 55:528. doi: 10.1136/jech.55.7.528b
6. Jamison DT, Mosley WH. Disease control priorities in developing countries: health policy responses to epidemiological change. Am J Public Health. (1991) 81:15–22. doi: 10.2105/AJPH.81.1.15
7. World Health Organization. Regional Office for South-East Asia. A Decade of Public Health Achievements in WHO's South-East Asia Region. WHO Regional Office for South-East Asia (2013).
8. Sadana R, Mushtaque A, Chowdhury R, Petrakova A. Strengthening public health education and training to improve global health. Bull World Health Organ. (2007) 85:163. doi: 10.2471/BLT.06.039321
9. Rabbani F, Shipton L, White F, Nuwayhid I, London L, Ghaffar A, et al. Schools of public health in low and middle-income countries: an imperative investment for improving the health of populations? BMC Public Health. (2016) 16:1–12. doi: 10.1186/s12889-016-3616-6
10. UGC. Minimum Standards of Instruction for the Grant of the Master's Degree through Formal Education Regulations. New Delhi (2003).
11. Collegedunia. Top Colleges, Universities & Institutes in India | Admission, Fees, Rankings of Top Management, Engineering, Medical Colleges. (2021). Available online at: https://collegedunia.com/
12. Careers360. Explore Exams, Colleges, Courses and Latest News about Education. (2021). Available online at: https://www.careers360.com/
13. EduVision. Career Planning and Educational Guidance. (2021). Available online at: https://www.eduvision.edu.pk/
14. Collegedekho.com. Find Top Colleges & Universities in India | Explore Courses, Exams, Admissions & Latest News. (2022). Available online at: https://www.collegedekho.com/
15. Sawleshwarkar S, Zodpey S, Negin J. “Public health is global”: examining Indian stakeholders' perspectives on Global Health education. BMC Public Health. (2020) 20:1–12. doi: 10.1186/s12889-020-09357-2
16. Tiwari R, Negandhi H, Zodpey Z. Current status of master of public health programmes in India: a scoping review. WHO South-East Asia J Public Health. (2018) 7:29–35. doi: 10.4103/2224-3151.228425
17. MOHFW. Model Curriculum Handbook Masters In Public Health. New Delhi: Ministry of Health and Family Welfare 2017-18 (2017).
18. India. MoHRDGoI. Ministry of Human Resource Development, Government of India. National Education Policy (2020).
19. Kanika Khurana. NEP 2020:4-Year Bacherlors' Degree, M.Phil to be discontinued-how UG/PG Course structure would change. Times now News (2020).
20. Negandhi H, Sharma K, Zodpey SP. How can departments of community medicine shape the future of Public Health Education in India? Indian J Public Health. (2010) 54:184. doi: 10.4103/0019-557X.77257
21. Suresh K. Public Health Schools in India need to go beyond syllabus. J Qual Health Care Econ. (2020) 3:000155. doi: 10.23880/jqhe-16000155
22. Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. (2010) 376:1923–58. doi: 10.1016/S0140-6736(10)61854-5
23. Wadsam. Kandahar University Inaugurates New Online Resource Center. Kandahar: Afghanistan Afghan Business (2018).
24. Moynihan S, Paakkari L, Välimaa R, Jourdan D, Mannix-McNamara P. Teacher competencies in health education: results of a Delphi study. PLoS ONE. (2015) 10:e0143703. doi: 10.1371/journal.pone.0143703
25. Albarqouni L, Hoffmann T, Straus S, Olsen NR, Young T, Ilic D, et al. Core competencies in evidence-based practice for health professionals: consensus statement based on a systematic review and Delphi survey. JAMA Network Open. (2018) 1:e180281–e. doi: 10.1001/jamanetworkopen.2018.0281
26. Bhandari S, Wahl B, Bennett S, Engineer CY, Pandey P, Peters DH. Identifying core competencies for practicing public health professionals: results from a Delphi exercise in Uttar Pradesh, India. BMC Public Health. (2020) 20:1737. doi: 10.1186/s12889-020-09711-4
27. Rao M, Rao KD, Kumar AS, Chatterjee M, Sundararaman T. Human resources for health in India. Lancet. (2011) 377:587–98. doi: 10.1016/S0140-6736(10)61888-0
28. Core Competencies Domains,.aspx. Core Competencies for Public Health Professionals: Domains. (2021). Available online at: http://www.phf.org/programs/corecompetencies/Pages/Core_Competencies_Domains.aspx
29. World Health Organization. Essential Public Health Functions, Health Systems and Health Security: Developing Conceptual Clarity and a WHO Roadmap for Action (2018).
30. ASPH Education Committee. Master's Degree in Public Health Core Competency Development Project. Washington, DC: The Association of Schools of Public Health (ASPH) (2006).
31. World Health Organization. WHO-ASPHER Competency Framework for the Public Health Workforce in the European Region. Copenhegan: World Health Organization; Regional Office for Europe (2021).
32. Raghav PR, Kumar D, Bhardwaj P. Experience of Delphi technique in the process of establishing consensus on core competencies. Int J Appl Basic Med Res. (2016) 6:191. doi: 10.4103/2229-516X.186966
33. Sharma K, Zodpey S, Gaidhane A, Syed ZQ, Kumar R, Morgan A. Designing the framework for competency-based master of public health programs in India. J Public Health Manag Pract. (2013) 19:30–9. doi: 10.1097/PHH.0b013e318241da5d
34. Hazarika I. Health workforce in India: assessment of availability, production and distribution. WHO South-East Asia J Public Health. (2013) 2:106–12. doi: 10.4103/2224-3151.122944
35. Zodpey SP, Negandhi H, Yeravdekar R. Future directions for public health education reforms in India. Front Public Health. (2014) 2:68. doi: 10.3389/fpubh.2014.00068
36. Sharma K, Zodpey S. Public health education in India: Need and demand paradox. Indian J Commun Med. (2011) 36:178. doi: 10.4103/0970-0218.86516
37. Brownson RC, Burke TA, Colditz GA, Samet JM. Reimagining public health in the aftermath of a pandemic. Am J Public Health. (2020) 110:1605–10. doi: 10.2105/AJPH.2020.305861
38. St Leger L. Schools, health literacy and public health: possibilities and challenges. Health Promot Int. (2001) 16:197–205. doi: 10.1093/heapro/16.2.197
39. Miller E, Reddy M, Banerjee P, Brahmbhatt H, Majumdar P, Mangal D, et al. Strengthening institutions for public health education: results of an SWOT analysis from India to inform global best practices. Hum Resour Health. (2022) 20:1–11. doi: 10.1186/s12960-022-00714-3
40. Rahnuma Binte Rashed. The Evolving Trend of Public Health Careers in Pandemic. Dhaka: The Financial Express (2021).
41. Kak N, Burkhalter B, Cooper M-A. Measuring the competence of healthcare providers. Operat Res Issue Paper. (2001) 2:1–28.
42. Sharma K, George S, Zodpey S. Understanding the current status and exploring the potential for distance education in public health in India. Indian J Public Health. (2011) 55:7. doi: 10.4103/0019-557X.82533
43. Sharma K, Zodpey S, Syed Z, Gaidhane A. Career opportunities for master of public health graduates in India. Asia Pacific J Health Manag. (2013) 8:45–50.
44. Ambade P,. Down To Earth. (2021). Available online at: https://www.downtoearth.org.in/blog/health/covid-19-why-indianeeds-a-robust-public-health-infrastructure-77222
45. World Health Organization. South-East Asia Public Health Initiative 2004-2008. New Delhi: WHO (2005).
46. Fee E, Brown TM. The past and future of public health practice. Am J Public Health. (2000) 90:690–1. doi: 10.2105/AJPH.90.5.690
47. Mahat A, Bezruchka SA, Gonzales V, Connell FA. Assessment of graduate public health education in Nepal and perceived needs of faculty and students. Hum Resour Health. (2013) 11:1–12. doi: 10.1186/1478-4491-11-16
48. Mureed S, Hamid S, Hafeez A. Transforming public health education in pakistan: matching competencies to health system needs. Educ Res J. (2017) 7:181–91.
49. Woodward A. For Debate: Public health has no place in undergraduate medical education. J Public Health. (1994) 16:389–92. doi: 10.1093/oxfordjournals.pubmed.a043018
50. Keith KC. Student perspectives on public health education in undergraduate medical education. Diversity Equal Health Care. (2018) 15:181. doi: 10.21767/2049-5471.1000181
51. Ghaffar A, Rashid SF, Wanyenze RK, Hyder AA. Public health education post-COVID-19: a proposal for critical revisions. BMJ Glob Health. (2021) 6:e005669. doi: 10.1136/bmjgh-2021-005669
52. Gummeson H, Goel SR, Elmusharaf K. Public health practicum: a scoping review of current practice in graduate public health education. BMJ Open. (2021) 11:e047512. doi: 10.1136/bmjopen-2020-047512
55. Public Health Foundation of India. Training Division. Available online at: https://phfi.org/thework/research/training-division/
56. Future Learn,. Top 25 Online Courses in Bangladesh - Study for Free with FutureLearn. (2021). Available online at: https://www.futurelearn.com/info/blog/top-25-online-courses-inbangladesh
57. Prime Institute of Public Health. Certificate Courses. Available online at: https://piph.prime.edu.pk/academics/certificate-courses-workshops
58. Gruzieva TS, Hrechyshkina NV, Antonyuk OY, Dufynets VA, Konovalov SE. Self-assessment of the content of the public health master's educational program for compliance with the european public health core competences programme. Wiadomości Lekarskie. (2021) 2021:713. doi: 10.36740/WLek202103227
Keywords: career opportunities, challenges of public health education (PHE), higher education in PH, MPH program, South Asia
Citation: Anitha CT, Akter K and Mahadev K (2022) An overview of public health education in South Asia: Challenges and opportunities. Front. Public Health 10:909474. doi: 10.3389/fpubh.2022.909474
Received: 31 March 2022; Accepted: 03 August 2022;
Published: 26 August 2022.
Edited by:
Melody Goodman, New York University, United StatesReviewed by:
Supriya Patil, Krishna Institute of Medical Sciences, IndiaZahiruddin Quazi Syed, Datta Meghe Institute of Medical Sciences, India
Copyright © 2022 Anitha, Akter and Mahadev. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chandanadur Thippaiah Anitha, YWN0bWRAdW9oeWQuYWMuaW4=; Kalyankar Mahadev, bWttZEB1b2h5ZC5hYy5pbg==
 Chandanadur Thippaiah Anitha
Chandanadur Thippaiah Anitha Konok Akter
Konok Akter Kalyankar Mahadev
Kalyankar Mahadev