
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 16 August 2022
Sec. Public Health Policy
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.906602
This article is part of the Research TopicSystems thinking: strengthening health systems in practiceView all 11 articles
 Caitlin B. Biddell1,2*
Caitlin B. Biddell1,2* Karl T. Johnson1
Karl T. Johnson1 Mehul D. Patel3
Mehul D. Patel3 Raymond L. Smith4
Raymond L. Smith4 Hillary K. Hecht1
Hillary K. Hecht1 Julie L. Swann5
Julie L. Swann5 Maria E. Mayorga5
Maria E. Mayorga5 Kristen Hassmiller Lich1
Kristen Hassmiller Lich1Introduction: The COVID-19 pandemic response has demonstrated the interconnectedness of individuals, organizations, and other entities jointly contributing to the production of community health. This response has involved stakeholders from numerous sectors who have been faced with new decisions, objectives, and constraints. We examined the cross-sector organizational decision landscape that formed in response to the COVID-19 pandemic in North Carolina.
Methods: We conducted virtual semi-structured interviews with 44 organizational decision-makers representing nine sectors in North Carolina between October 2020 and January 2021 to understand the decision-making landscape within the first year of the COVID-19 pandemic. In line with a complexity/systems thinking lens, we defined the decision landscape as including decision-maker roles, key decisions, and interrelationships involved in producing community health. We used network mapping and conventional content analysis to analyze transcribed interviews, identifying relationships between stakeholders and synthesizing key themes.
Results: Decision-maker roles were characterized by underlying tensions between balancing organizational mission with employee/community health and navigating organizational vs. individual responsibility for reducing transmission. Decision-makers' roles informed their perspectives and goals, which influenced decision outcomes. Key decisions fell into several broad categories, including how to translate public health guidance into practice; when to institute, and subsequently loosen, public health restrictions; and how to address downstream social and economic impacts of public health restrictions. Lastly, given limited and changing information, as well as limited resources and expertise, the COVID-19 response required cross-sector collaboration, which was commonly coordinated by local health departments who had the most connections of all organization types in the resulting network map.
Conclusions: By documenting the local, cross-sector decision landscape that formed in response to COVID-19, we illuminate the impacts different organizations may have on information/misinformation, prevention behaviors, and, ultimately, health. Public health researchers and practitioners must understand, and work within, this complex decision landscape when responding to COVID-19 and future community health challenges.
Declared a pandemic by the World Health Organization on March 11, 2020 (1, 2), the coronavirus disease 2019 (COVID-19) continues to rapidly spread, resulting in over 6 million deaths worldwide as of March 2022 (3). COVID-19 has posed the most challenging and complex global health crisis in at least 100 years. Specifically, the complexity of COVID-19 has been characterized by: uncertain and rapidly changing information; interdependencies and feedback loops between decisions made by many individuals/organizations with different perspectives and their outcomes across organizational and sector boundaries; and time lags between policy changes and their ripple effects (4, 5).
In the United States, though federal guidance has been issued, the COVID-19 pandemic response has largely been implemented at the state and local level, involving ongoing decision-making by stakeholders across numerous sectors at these levels. Even before COVID-19, with the increasing recognition of the social and economic influences on health and health inequities, promoting local community health has demanded the involvement of numerous sectors operating at multiple levels of influence (e.g., individuals, organizations, policy-making).6 Health outcomes are thus collectively produced by a broad spectrum of stakeholders—defined as individuals and organizations with an interest in a given problem and its resolution (7, 8)—acting in accordance with their own goals, incentives, knowledge, and mental models of the problem at hand (9).
As a result, local community health promotion can be conceptualized as a complex system in and of itself, with interactions between different sectors resulting in feedback loops producing emergent properties across the entire system (6). In complex systems theory, emergent properties develop when systems evolve over time and develop effects that are different, or greater than, the sum of their parts (10, 11). In the context of community health, such properties could be understood as different dimensions of the community's health and safety (e.g., access to healthcare, safe environmental conditions, a positive culture of healthy behavior, etc.,). For this reason, studying the independent parts of a system, including decision-making within different sectors, is not sufficient to understand the emergent system properties influencing system outcomes. It is the collective decision-making of all stakeholders within the community that produces the overall level of community health.
Given the complexity of the COVID-19 pandemic, layered on top of the already complex landscape of local community health promotion, studying the local pandemic response demands a complex systems approach that recognizes the distinct yet interconnected stakeholder roles shaping decisions within and across organizational boundaries (12). In the context of a local pandemic response, stakeholders range from individuals deciding whether to wear a mask to local public health officials developing and communicating guidance around mask usage (13, 14). Given the influence that organizational policies had on individual-decision making during the pandemic, we bounded our study of the local pandemic response by focusing on organizational decision-makers, defined as individuals whose job responsibilities included making decisions with a substantial impact on the organization as a whole or individuals the organization serves.
Specifically, we sought to study the local cross-sector decision landscape emerging in response to the early-stages (first year) of the COVID-19 pandemic in North Carolina, a large, diverse state in the US with several metropolitan centers. North Carolina's local public health system is comprised of 85 local health departments, most commonly organized at the county-level (there are 100 counties in North Carolina). Historically, public health agencies have collaborated with county emergency management divisions for emergency preparedness and response—especially in response to hurricanes in the eastern region of the state—with several counties merging the role of public health preparedness coordinator with emergency management (15, 16).
We define the local cross-sector decision landscape in terms of who is involved in making decisions that affect community health, the relationship between decision-makers' roles and the types of decisions made, and the methods of influence between different stakeholders within the same community. Viewed through a complex systems lens, we considered decision-makers' organizations as nodes and the connections between them, formed through the decision-making process, as interrelationships. We conducted a network mapping-based qualitative analysis of organizational decision-makers in North Carolina.
Improving health, particularly amidst crises such as COVID-19, requires coordinating complex decision landscapes. This analysis illustrates a replicable approach to mapping and characterizing a complex organizational decision landscape. Within the context of the various organizational perspectives, priorities, and incentives involved in community health, the results of this analysis serve to inform decision-making by public health practitioners and researchers when responding to this and future infectious disease outbreaks, as well as other complex public health challenges that require system-level coordination.
Defining sectors as subdivisions of society that include similar types of agencies or organizations serving distinct functions (7, 17), we interviewed state and local decision-makers from nine sectors: business (n = 4; small business owners, real estate agent, technology company director; B1-B4), non-profit organizations (n = 3; senior director, vice presidents (VP) of operations and risk management; NP1-NP3), county government (n = 4; county managers, director of social services; G1-G4), healthcare (n = 5; directors/VPs of healthcare associations, systems engineer, director of student health; H1-H5), local public health (n = 5; local health directors; PH1-PH5), public safety (n = 7; emergency managers, county sheriffs; PS1-PS7), religion (n = 6; church pastors, member of church COVID taskforce; R1-R6), education (n = 7; principal, school board member, community college president, university vice president; E1-E7), transportation (n = 3; transportation planner and pedestrian coordinator, traffic safety engineer; T1-T3) (Table 1).
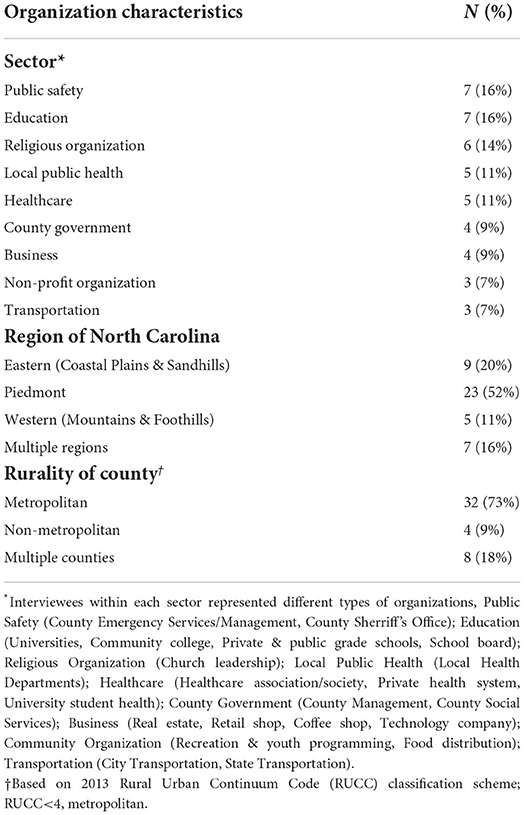
Table 1. Characteristics of organizations represented in interviews with local decision-makers (N = 44).
Given the challenge of asking organizational leaders to meet during the early stages of the pandemic, we used a snowball sampling approach, starting with intentionally diverse decision-makers recommended by our research team and their cross-sector contacts. We then asked interviewees for referrals to decision-makers in related organizations who may provide a meaningful and diverse perspective from their own. We interviewed 44 of the 120 potential interviewees contacted (37% response); four interviewees were previously known to one or more coauthors. Of those contacted who did not complete an interview, most did not respond to our email request. As such, we are not able to know the exact reasons for non-response. However, we suspect that this was due to the substantial competing demands of organizational leaders during the first year of the pandemic. No candidates explicitly refused to participate due to hesitation surrounding the study objectives. We determined sample size by reaching thematic saturation across sectors and ensuring at least three interviews within each sector. While the interviewees do not represent an exhaustive list of organizations responding to the pandemic, the objective of our sampling approach was to recruit decision-makers from diverse organizations and ensure representation across sectors and the state of North Carolina.
Three members of the study team (KTJ, MDP, KHL) developed the semi-structured interview guide following a review of decision theory literature and iteratively revised it during the first three interviews (Supplemental Appendix 1). One member of the study team (KTJ), a graduate research assistant with qualitative interview experience and visible racial and gender privilege, conducted semi-structured interviews using a secure web-based video-conferencing platform. All 45–60-min interviews were recorded and transcribed by an external audio to text automatic transcription service. Transcripts were cleaned and de-identified by members of the study team prior to analysis. Interviews were conducted between October 2020 and January 2021, during which North Carolina experienced a surge in cases, with daily COVID-19 hospitalization counts increasing from ~900 in early October to almost 4,000 in January. North Carolina began administering vaccines in mid-December 2020, however widespread distribution did not begin until late-January (18).
We asked interviewees about their perceived individual and organizational roles in the COVID-19 pandemic response. Interviewees were then prompted to reflect on the key decisions that their organizations made in response to the COVID-19 pandemic in the first two months (February and March 2020) and at the time of the interviews (October 2020 through January 2021), including decisions they anticipated having to make in the near future. In discussing each key decision, we probed interviewees on the other stakeholders (within and across sectors) influencing or contributing to their decision-making process. Interviewees were also asked about the decision-making context (e.g., community beliefs), inputs (e.g., data and scientific guidelines), and processes (e.g., decision-making systems) used by their organizations. Responses to these questions were analyzed and reported separately (manuscript under review). This study was determined to be exempt from review by the UNC Institutional Review Board (#20-2087).
We employed conventional content analysis to derive themes from the qualitative data (19). Using an inductive, iterative coding approach, we outlined a general codebook structure stemming from the semi-structured interview guide (Supplemental Appendix 1). We allowed interview codes and themes to emerge as two independent researchers (CBB, KTJ) coded each transcript using MAXQDA software (see Supplemental Appendix 2 for final codebook) (20). We analyzed excerpts within each code relating to the decision landscape (decision-making process codes analyzed separately), identifying major and minor themes. Decision-maker roles were coded to describe the individual's role in the organization, broadly speaking, as well as their role in the organization's pandemic response. Decisions identified by stakeholders were coded as belonging to one or more emergent categories: continuing/suspending in-person services, safety protocols, population served, testing/tracing, vaccination, physical resource allocation, human resource allocation. Within each decision category we analyzed excerpts by sector, identifying key decisions and documenting the interrelationships between decision topics across sectors. To explicitly analyze the interrelationships across sectors resulting from collaborative decision-making processes, we coded for examples of collaboration between organizations, defined as either mutual (both organizations benefitting) or dependent (one organization relying on another for either resources or information). We defined collaboration broadly as two or more entities involved in a joint venture or decision-making process (21, 22). Further, we coded for instances in which interviewees described perceiving the behavior of other local organizations and institutions as indirectly influencing these decisions, another form of interrelationships between stakeholders. The Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist was used to guide our reporting of the qualitative analysis and results (23).
We used Kumu, an online platform for organizing complex data, to develop a network map of within- and cross-sector organizational collaboration that formed in response to the COVID-19 pandemic in North Carolina, as described by the decision-makers we interviewed (24). Network mapping is a complex systems method intended to describe and visualize the roles, power dynamics, and relationships between stakeholders in a bounded system (25, 26). Using data from the collaboration codes described above, we first developed a matrix (with sectors along each axis) detailing all instances of collaboration described in interviews. We then inputted this information into Kumu, with organization types as nodes (color-coded by sector) and collaboration illustrated through connections (between two or more nodes). After building the full network map, we used functionality within Kumu to calculate two network metrics: degree and closeness. Degree is a measure of the total number of unique connections attached to each node and is used for identifying frequently-connected local organizations, or hubs, in the network. Closeness, quantified on a scale of 0–1, is a measure of how close each node is to other nodes in the network, accounting for the entire network structure, rather than only direct connections (as is the case with degree) (24).
Of the 44 stakeholders interviewed, the majority represented organizations serving constituents within a single county (primarily metropolitan), and constituencies ranged from several hundred to over 1 million (Table 1, Supplemental Table 3). As key informant interviewees provided organizational perspectives, individual characteristics could not be disclosed. Themes (presented below) emerged within each of three domains comprising the COVID-19 pandemic response decision landscape: (1) Perceived organizational roles, (2) Key decisions, and (3) Interrelationships between organizations (Table 2). These themes describe who was involved in making and informing decisions, in what context decisions were made, and the complexity of this decision landscape across sectors.
Interviewees' perceived roles in the COVID-19 pandemic response informed the set of relevant decisions their organizations faced and how they balanced inherent competing priorities (e.g., constituent, staff, and community safety; physical, social, and emotional wellness) in the decision-making process (Table 3). Across all sectors, interviewees described the responsibility of continuing to run their organization's operations within the new legal and safety constraints of stay-at-home orders and mandated safety protocols. Non-profits, religious organizations, and county governments underscored the heightened need for their social services, viewing their role as responding to the social and economic consequences of the pandemic. Education and transportation similarly recognized the necessity of their services and viewed their role as ensuring these services were delivered in an altered form to ensure community safety. Healthcare associations saw their primary role as convening organizations for the purposes of knowledge sharing, personal protective equipment (PPE) allocation, and advocacy to the state. LHDs and emergency management had more central roles in the pandemic response, with communicable disease management and crisis response being core functions of these respective entities. County emergency management and LHDs worked together, with LHDs leading the local public health response and emergency management facilitating communication and logistics. Though the extent to which COVID-19-related roles departed from traditional organizational responsibilities varied by organization, the following themes emerged across sectors.
Interviewees from all sectors prioritized customer, constituent, and community safety, often as a new responsibility in addition to their originally stated missions. For example, an interviewee from a non-profit dedicated to youth and recreational programming emphasized the challenge of carrying out this mission when they could no longer bring the community together in-person. In this case, the organizational mission and the responsibility for community safety were viewed as being in tension with one another; however, other interviewees viewed keeping their constituents safe as consistent with their original organizational mission, which became “more urgent than ever before” (R1, Religion). This responsibility also extended to the health of the broader community. “The safer we are here, the safer folks are in the community” (R2, Religion).
Given that many COVID-19 safety protocols required individual behavior change, interviewees acknowledged the limitations of their organizational roles in enforcing these measures. However, they underscored their role as being to educate and empower the public to uphold their personal responsibilities in mitigating COVID-19 spread. “It's a personal expectation, one, to protect yourself, and two, to comply with it...Our job was really to empower and inform as well as make available resources” (PS7, Public Safety). One pastor disseminated educational videos to combat misinformation—“This is a collaboration and God will help us, but he does not dissolve us of our own responsibilities for ourselves” (R4, Religion). The form of education varied, from ensuring that public health guidance was widely available to tailoring guidance to communities. Interviewees emphasized the importance of ensuring that constituents understood why public health measures were needed. Empowerment included leadership modeling public health behaviors and securing the resources, such as masks, to support community health-minded decisions.
Fulfilling the roles described above involved decisions related to continuing or suspending in-person services, instituting safety protocols, allocating resources (human and physical), testing/screening, contact tracing, and vaccination. Interviewees described a decision ecosystem in which the consequences of one decision (whether related to viral transmission, economic impacts, or organizational realities) prompted the need for subsequent decisions. Further, given how quickly scientific knowledge and public health guidance were changing, interviewees were constantly faced with new decisions across domains. A full matrix of COVID-19-related decisions described is included in Supplemental Appendix 4 and summarized in Table 3. In analyzing the key decisions described by interviewees across sectors, the following thematic decision categories emerged.
All interviewees made decisions to discontinue, or transition remotely, all non-essential in-person services in March 2020, informed by state and local stay-at-home orders. Though this was framed less as a decision, and more as a necessarily cautious response to the uncertainties of the pandemic, it prompted a cascade of decisions related to translating guidance into organizational contexts to maintain services/mission while ensuring employee and community safety. Decisions included distinguishing essential vs. non-essential personnel to inform remote work scheduling, securing PPE for essential personnel, and securing the technology necessary to support remote work. Even LHDs had to make internal staffing and protocol decisions, all while being propelled into a more central role than ever before. “A big part of my workforce have children… How do we work and show up to serve the community while balancing the needs of what you're having to do at home?” (PH4, Public Health).
In contrast, re-opening decisions were more contentious. While many strove to re-open, some decision-makers remained closed or instituted safety protocols beyond legal mandates. “I needed to be confident that I could keep everyone safe, and that people were on board with protecting one another” (B4, Business). However, pressure from community members to re-open grew over time. “I've watched some of my colleagues at more conservative schools have to make decisions that they weren't 100% comfortable with, in terms of how rooms were organized, in terms of mask use …because of the pressure of their community.” (E3, Education).
While not all sectors were directly involved in testing, tracing, and vaccination, related decisions made by LHDs and emergency management influenced community transmission, and thus decisions about re-opening and safety protocols by organizations in other sectors. LHDs and EMs instituted contact tracing early on. “To date, we believe that we maintained a seven-day rolling average of less than a hundred cases a day because we continue to do contact tracing.” (PS4, Public Safety). LHDs and emergency management also implemented testing, often in partnership with external clinical entities; however, interviewees described challenges in carrying out these services equitably at scale. “Contact tracing in most public health agencies wasn't fit for purpose, for the scale” (B2, Business).
A final category of decisions related to developing new or extending existing services to address social impacts of COVID-19 restrictions, such as homelessness and food insecurity. In some cases, this meant balancing infection risk with health risks of downstream consequences. Interviewees noted a primary tension in that efforts to “dampen down COVID in our community are also the things that are putting some of our most vulnerable population at risk” (PH5, Public Health). For organizations working to meet social needs, the recognition of heightened need motivated organization leaders to ensure services continued, even if processes had to change to keep staff, volunteers, and constituents safe. “There's a whole litany of things that have kept us busier and have really proven the urgency and the significance of community-based and faith-based organizations.” (R1, Religion).
The complexity and novelty of COVID-19 demanded the pooling of resources and expertise in decision-making, exemplifying the interrelationships between individuals, organizations, and resources within and across sectors. Given that organizational decision-makers were thrust into new roles and thus faced new decisions and competing priorities in response to the COVID-19 pandemic, they described turning to existing and new collaborations to navigate these complexities. Collaborative decision-making, as well as the influence of decisions made by other organizations on decision-making, showcase the complex interrelationships between individuals, organizations, and resources within and across sectors.
Figure 1 shows the complexity inherent in the network map developed from the collaboration described by interviewees. Each node in the map represents an organization type, color-coded by sector and sized by closeness metric (larger nodes more connected to other nodes in the network map). Supplemental Appendix 5 presents complete network mapping metrics (i.e., closeness, degree). Additionally, a full, interactive network map can be found online. Hovering over individual connections and labeled loops will provide details about each collaboration represented in the map. Given that interviews were conducted among a small subset of all stakeholders involved in the local pandemic response decision landscape, and that interviews were limited to the most notable decisions interviewees were facing, this network map represents a subset of the connections and complexity involved in the complete decision landscape. Results from the network map, paired with qualitative analysis of excerpts coded as collaboration or the influence of other organizations, led to the synthesis of the following themes.

Figure 1. Network map of cross-sector partnerships formed in North Carolina's local COVID-19 pandemic response. This figure shows the network map developed from the collaboration described by interviewees. Each node in the map represents an organization type, color-coded by sector and sized by closeness metric (larger nodes more connected to other nodes in the network map). A full, interactive network map can be found (24).
Interviewees described creatively responding to COVID-19-imposed challenges by forming new, and leveraging existing, collaborations among diverse stakeholder to prevent blind spots in decision-making. Three main categories of collaboration were identified: (1) Public—Public, particularly within sectors of local government (e.g., public health and emergency management co-leading the local pandemic response), (2) Public—Private, particularly government-initiated collaboration with non-governmental organizations (e.g., county social services partnering with community organizations to distribute COVID federal relief funds), and (3) Private—Private, particularly among businesses, non-profits, and religious organizations (e.g., local businesses partnering to deliver care packages to frontline workers). Interviewees universally described feeling that their collaborative capacity became stronger because of COVID-19, “One of the positives that's going to come out of COVID is that we're going to have a more robust, cohesive, collaborative model of non–profits and organizations working together” (R1, Religion). As measured in both degree and closeness, LHDs, healthcare systems, and county management were the most central actors in the decision landscape, documenting the high frequency with which they collaborated with other organizations in response to COVID-19 and their central role (Supplemental Appendix 5).
LHDs in our network map had a total of 24 unique connections (degree) and the highest closeness metric of 0.867 (Supplemental Appendix 5). As closeness is measured on a scale from 0 to 1, a closeness metric of 0.867 suggests that, of the organizations included in our analysis, LHDs had the most direct and indirect connections to other organizations in the network map. The next highest closeness metric was 0.633 (healthcare systems). On the whole, closeness metrics ranged from 0.356 to 0.867 with a mean of 0.51”.
Central to many of the interrelationships described by interviewees, LHDs served a critical function in the pandemic response, both informing local decision-making and facilitating the implementation of higher-level decisions through collaboration with other sectors impacted by those decisions. LHDs served four primary collaborative roles: (1) Directly responding to the communicable disease outbreak (e.g., testing, tracing, vaccination); (2) Guiding the translation of public health guidance into local organizational contexts; (3) Educating the public; (4) Convening and engaging community stakeholders (Figure 2). Implementing a comprehensive pandemic response required collaborating with other sectors, such as hosting testing and vaccination events in parking lots. As described by an interviewee whose church volunteered as a test site, “…the fourth Saturday of the month, for as long as they want, this will be the test site here. That's one of the ways that we're trying to help folks in the community.” (R2, Religion). LHDs informed decisions at the crossroads between federal- and state-level guidance (e.g., mask mandates, distancing guidelines) and local organizations. They were viewed as “trusted sources” (G3, Government), providing tailored public health advice, visiting local businesses, and reviewing safety protocols. Educating the public required monitoring and reporting local COVID-19 trends through data dashboards and collaborating with leaders from other sectors to host press conferences and conduct educational campaigns. Lastly, LHDs were tasked with convening and connecting stakeholders across sectors to ensure the inclusion of diverse perspectives in addressing the economic and social determinants of health, creating “better health through better partnerships” (PH3, Public Health).
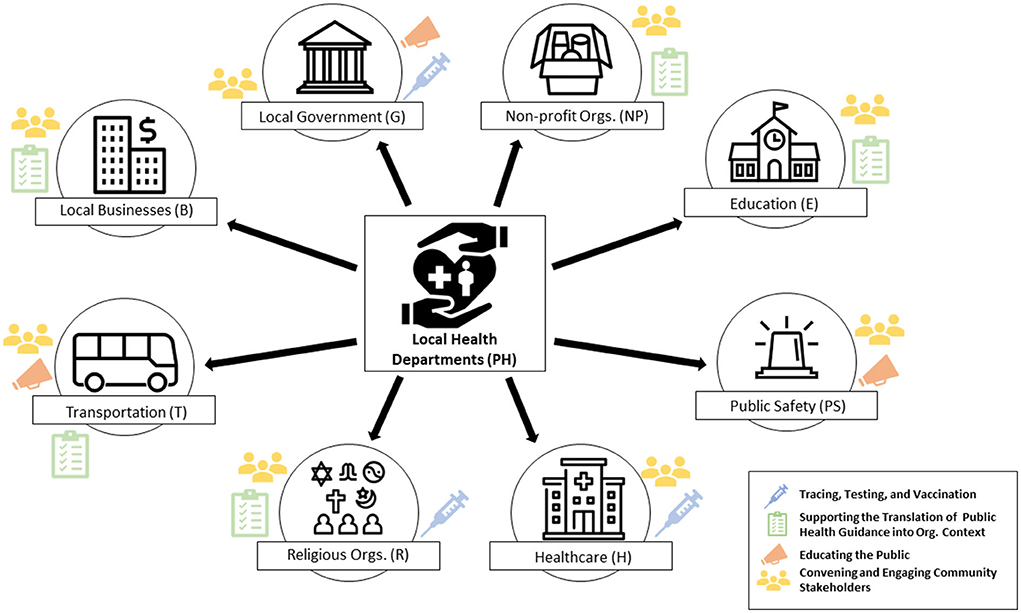
Figure 2. Central roles of local health departments in coordinating local COVID-19 pandemic response across sectors.
Beyond the interrelationships resulting from explicit cross-sector collaboration, interviewees also described the impact of decisions made by the public and other surrounding organizations. As one interviewee noted in reference to the influence of community mask compliance and school district re-openings, “metrics are the result of community action… If we change our behavior, it's going to change the numbers” (E5, Education). In addition to influencing COVID-19 transmission trends, local decisions were described as influencing the feasibility of asking employees, volunteers, or customers to return in-person (e.g., Are schools open to provide childcare? Is public transportation running at full capacity?).
The COVID-19 pandemic has thrust decision-makers across sectors into new roles in a public health crisis response, creating a decision landscape with numerous actors and varying levels of coordination between them. Qualitative inquiry and network mapping and analysis allowed us to examine this cross-sector decision landscape through a complexity/systems thinking lens. The pandemic has forced the development of new decision-maker roles and competing priorities that decision-makers have navigated with limited, uncertain, and changing information. In response to the complexity of COVID-19, decision-makers engaged in both collaborative and semi-autonomous decision-making processes and depended upon new authorities, especially LHDs. In this resulting “polycentric” decision-making system, public and private actors worked across different centers of decision-making and at different scales to collectively produce their community's health during the pandemic (27). This study serves to (1) inform public health researchers, practitioners, and organizational decision-makers in how to navigate this and future complex, cross-sector population health challenges, and (2) illustrate a replicable approach to mapping and characterizing complex decision landscapes.
This study builds off prior work highlighting cross-sector responses to crises such as Hurricane Katrina and H1N1 (28, 29). It also extends prior applications of network mapping to other complex health challenges, such as serious mental illness (26) and community health promotion networks (25). However, this study is the first, to our knowledge, to use network mapping to investigate a cross-sector decision landscape in response to COVID-19. Several prior studies have investigated decision-making in response to COVID-19 within single sectors. These studies support the decision categories that emerged from our analysis, including decisions related to allocating resources (30), translating guidance into real-world organizational context (31), and addressing downstream social impacts (32). Our finding that cross-sector collaborations were critical components of the COVID-19 pandemic response builds upon several prior studies illustrating specific collaborations emerging in response to COVID-19-related needs, ranging from childcare for healthcare workers to local COVID-19 surveillance through school districts (33–36).
In line with our findings, prior work has emphasized the importance of community engagement in comprehensive pandemic responses and the necessity of communicating well (e.g., using accessible yet accurate language) with diverse stakeholders amidst changing, uncertain information (37). Challenges with community-based approaches, however, include balancing the need to respond quickly with the time it takes to meaningfully garner stakeholder perspectives (38). The need to navigate complex tradeoffs and often conflicting priorities within a community further underscores the importance of a cross-system governance or organizing structure with input from many stakeholder groups (32). Given the need to act quickly, communities should agree on such structures in advance of public health crises. Our analysis highlighted the importance of LHDs serving as what “Public Health 3.0” defines as a “chief health strategist” in coordinating the local pandemic response (39), working with other organizations directly and indirectly to govern the local public health system (40).
The decision landscape emerging in response to COVID-19 has implications for efforts to promote population health, beyond the immediate context of COVID-19. Though a global pandemic uniquely affects all individuals and organizations, other population health challenges operate within complex systems, influenced by multi-level determinants, ranging from individual action to social policy (41). This can create inconsistent priorities and decisions within communities that block progress. The role of stakeholders across sectors in the pandemic response, and the interrelationships between these sectors, support the growing call for the importance of cross-sector collaboration in promoting population health (7, 42, 43). Our findings further align with the vision of “Public Health 3.0” to expand the reach and scope of public health to “address all factors that promote health and well-being, including those related to economic development, education, transportation, food, environment and housing” (39). Public health leaders advocating for this broadened definition of public health have underscored that carrying out this vision successfully requires sustainable cross-sector collaboration, community engagement, and the application of a systems perspective to problem solving (44).
The “10 Essential Public Health Services”, updated in 2019 to include a focus on health equity, also reflect this reality, which considers the public health system to include not only public health agencies and healthcare providers, but also public safety, human services, and education, among other sectors (45). The decisions described in our analysis broadly fall into the three core domains of the essential services of public health: assessment (e.g., contact tracing, testing), policy development (e.g., implementation of executive orders, mobilizing community partnerships, educating the public to support effective policy change), and assurance (e.g., workforce maintenance, ensuring equitable access to services) (46). However, the COVID-19 pandemic has showcased that the centrality of equity in the revised essential services may still be aspirational. Disparities in COVID-19 morbidity and mortality rates by race and socioeconomic status underscore the need for system-wide decision-making that better prioritizes equitable access to health services, ranging from healthy living conditions to clinical care (47, 48). Additionally, the pandemic has highlighted the importance of the essential service, to “build and maintain a strong organizational infrastructure for public health,” moving forward (46). Bringing together the many sectors involved in the United States' fragmented public health system effectively and sustainably, beyond the immediate aftermath of a crisis, requires local foundational infrastructure supporting timely and comprehensive data collection (49); flexible funding mechanisms that recognize the necessity of cross-sector work in public health (50); and sufficient staffing capacity, particularly in response to the burnout of the current public health workforce (51, 52).
These findings should be viewed in the context of several limitations. While we were intentional in ensuring diverse representation of interviewees across sectors, organization type, and geography (across North Carolina), the sample does not represent an exhaustive list of organization types involved in the COVID-19 response. In all complex systems work, how system boundaries are defined has the potential to influence findings (8). Though we defined the bounds of the system under study based on geography (North Carolina) and organizational decision-makers, this system is too large to have a formal roster of all stakeholders involved. Results may have been different had we focused on a single community (region, city, or county) within the state, which would have allowed us to gain a more complete understanding of all stakeholders and their interactions. The snowball sampling technique employed increases the potential that the opinions uncovered were more homogenous than they would be otherwise. However, we were explicit when asking for recommendations that we were interested in uncovering a more complete and broader perspective on the subject. Thematic saturation was based on generalizable themes that emerged across sectors. Future research should investigate specific instances of cross-sector collaboration in more bounded systems, interviewing a complete roster of stakeholders involved, to gain a more detailed understanding of the role of power dynamics and competing priorities in influencing system dynamics. We hope that this study, which sought a broad boundary, will inform and standardize future efforts to study complex decision landscapes across diverse communities to learn what is similar and distinct.
The timing of interviews with respect to official guidance, transmission rates, and vaccination rollout undoubtedly influenced participant responses. We incorporated timing into interviews and analysis. Additionally, participant responses may be subject to self-report bias, given limitations of recall and the potential for selective reporting. As interviews lasted no more than an hour, it is not feasible to expect interviewees to recount every decision involved in their organization's pandemic response. As such, we asked interviewees to prioritize the key, COVID-related decisions that they perceived to be most important to their organization. Lastly, decision-makers willing to participate in public health research may have differed from those who refused in the extent to which they valued and trusted scientific information. However, participants described a range of perspectives on how they incorporated scientific information into decision-making.
This network mapping qualitative analysis of local decision-makers from nine different sectors in North Carolina documents the complex, cross-sector local decision landscape in response to the COVID-19 pandemic. Most notably, this analysis highlights the expanded roles of decision-makers across sectors in the pandemic response, the key types of decisions faced, and how decision-makers relied on collaboration and the guidance of LHDs to respond to these new challenges. Understanding this decision landscape serves to inform public health researchers and practitioners about who is involved in decision-making related to community health and how. Knowing this can support communities in collaborating to improve organizational decision-making processes with community and population health in mind. It also underscores the need for public health infrastructure to improve information dissemination, priority setting, and alignment in response to future crises and other complex health challenges.
The datasets generated for this study are not publicly available due to data confidentiality. Investigators interested in accessing this dataset for future research may do so under the following conditions: (1) IRB approval has been obtained from the institution covering the investigator, (2) data security procedures ensuring patient privacy have been demonstrated by the investigator, and (3) a data use agreement is completed by UNC and the outside investigator. Final datasets for analysis will not include any identifying information.
The studies involving human participants were reviewed and approved by UNC Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Data curation: CB and KJ. Formal analysis: CB, KJ, and HH. Funding acquisition: MP, MM, JS, and KH. Investigation: KJ and KH. Methodology: CB, KJ, MP, and KH. Project admin: KJ. Supervision: MP and KH. Validation, visualization, and writing–original draft: CB. All authors contributed to the conceptualization of this study, writing–review and editing, and approved the submitted version.
This research was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, Grant No. UL1TR002489, and the Council of State and Territorial Epidemiologists and Centers for Disease Control Cooperative Agreement No. NU38OT000297. CBB is additionally supported by a NIH Cancer Care Quality Training Program grant, UNC-CH, Grant No. T32-CA-116339. Funders did not have any role in the study design; collection, management, analysis, and interpretation of the data; writing of the manuscript; or the decision to submit the report for publication.
The authors are grateful to all of the individuals who participated in the interviews for this analysis. They are also grateful to Paul Mihas, who provided formative qualitative research guidance.
JS reported receiving compensation from Georgia Institute of Technology and Zoetis, Inc. in the prior 12 months.
The remaining authors declared that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.906602/full#supplementary-material
1. World Health Organization. Director-General's opening remarks at the media briefing on COVID-19-11 March 2020. Geneva: World Health Organization (2020).
2. Cucinotta D, Vanelli M, WHO. Declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
3. WHO. WHO Coronavirus (COVID-19) Dashboard. Availableonline at: https://covid19.who.int/. Published 2022. Updated 1/6/2022 (accessed January 6, 2022).
4. Sturmberg JP, Martin CM. COVID-19 – how a pandemic reveals that everything is connected to everything else. J Eval Clin Pract. (2020) 26:1361–7. doi: 10.1111/jep.13419
5. Wernli D, Tediosi F, Blanchet K, Lee K, Morel C, Pittet D, et al. A complexity lens on the COVID-19 pandemic. Int J Health Policy Manag. (2021). doi: 10.34172/ijhpm.2021.55. [Epub ahead of print].
6. Baugh Littlejohns L, Baum F, Lawless A, Freeman T. The value of a causal loop diagram in exploring the complex interplay of factors that influence health promotion in a multisectoral health system in Australia. Health Res Policy Syst. (2018) 16:126. doi: 10.1186/s12961-018-0394-x
7. Cilenti D, Issel M, Wells R, Link S, Lich KH. System dynamics approaches and collective action for community health: an integrative review. Am J Community Psychol. (2019) 63:527–45. doi: 10.1002/ajcp.12305
8. Hassmiller Lich K, Kuhlberg J. Engaging Stakeholders in Mapping and Modeling Complex System Structure to Inform Population Health Research and Action (Chapter 9). New York, NY: Oxford University Press. (2020). p. 119–33.
9. Koleros A, Mulkerne S, Oldenbeuving M, Stein D. The actor-based change framework: a pragmatic approach to developing program theory for interventions in complex systems. Am J Eval. (2018) 41:34–53. doi: 10.1177/1098214018786462
11. Siegenfeld AF, Bar-Yam Y. An introduction to complex systems science and its applications. Complexity. (2020) 2020:6105872. doi: 10.1155/2020/6105872
12. Emshoff JG, Darnell AJ, Darnell DA, Erickson SW, Schneider S, Hudgins R. Systems change as an outcome and a process in the work of community collaboratives for health. Am J Community Psychol. (2007) 39:255–67. doi: 10.1007/s10464-007-9110-7
13. Czeisler M, Tynan MA, Howard ME, Honeycutt S, Fulmer EB, Kidder DP, et al. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance - United States, New York City, and Los Angeles, May 5-12, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:751–8. doi: 10.15585/mmwr.mm6924e1
14. Vardavas C, Odani S, Nikitara K, Banhawi HE, Kyriakos C, Taylor L, et al. Public perspective on the governmental response, communication and trust in the governmental decisions in mitigating COVID-19 early in the pandemic across the G7 countries. Prev Med Rep. (2021) 21:101252. doi: 10.1016/j.pmedr.2020.101252
15. Vielot NA, Horney JA. Can merging the roles of public health preparedness and emergency management increase the efficiency and effectiveness of emergency planning and response? Int J Environ Res Public Health. (2014) 11:2911–21. doi: 10.3390/ijerph110302911
16. Davis MV, MacDonald PD, Cline JS, Baker EL. Evaluation of public health response to hurricanes finds North Carolina better prepared for public health emergencies. Public Health Rep. (2007) 122:17–26. doi: 10.1177/003335490712200103
17. Kegler MC, Swan DW. An initial attempt at operationalizing and testing the community coalition action theory. Health Educ Behav. (2011) 38:261–70. doi: 10.1177/1090198110372875
19. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
21. Henneman EA, Lee JL, Cohen JI. Collaboration: a concept analysis. J Adv Nurs. (1995) 21:103–9. doi: 10.1046/j.1365-2648.1995.21010103.x
22. Gray B. Collaborating: Finding Common Ground for Multiparty Problems. 1st ed ed San Francisco: Jossey-Bass. (1989).
23. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
24. Kumu Inc. [computer program]. North Carolina Department of Health and Human Services (NCDHHS) (2021).
25. Wijenberg E, Wagemakers A, Herens M, Hartog FD, Koelen M. The value of the participatory network mapping tool to facilitate and evaluate coordinated action in health promotion networks: two Dutch case studies. Glob Health Promot. (2019) 26:32–40. doi: 10.1177/1757975917716923
26. Pinfold V, Sweet D, Porter I, Quinn C, Byng R, Griffiths C, et al. Improving Community Health Networks for People With Severe Mental Illness: A Case Study Investigation. Southampton (UK): NIHR Journals Library. (2015). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK276549/
27. Ostrom E. Beyond markets and states: polycentric governance of complex economic systems. Am Econ Rev. (2010) 100:641–72. doi: 10.1257/aer.100.3.641
28. Gupta R. Enhancing community partnerships during a public health emergency: the school-located vaccination clinics model in Kanawha County, WV during the 2009 influenza A (H1N1) pandemic. W V Med J. (2011) 107:28–34.
29. Simo G, Bies AL. The role of nonprofits in disaster response: an expanded model of cross-sector collaboration. Pub Admin Rev. (2007) 67:125–42. doi: 10.1111/j.1540-6210.2007.00821.x
30. Uppal A, Silvestri DM, Siegler M, Natsui S, Boudourakis L, Salway RJ, et al. Critical care and emergency department response at the epicenter of the COVID-19 pandemic. Health Aff (Project Hope). (2020) 39:1443–9. doi: 10.1377/hlthaff.2020.00901
31. Hoover AG, Heiger-Bernays W, Ojha S, Pennell KG. Balancing incomplete COVID-19 evidence and local priorities: risk communication and stakeholder engagement strategies for school re-opening. Rev Environ Health. (2021) 36:27–37. doi: 10.1515/reveh-2020-0092
32. Ryan B, Coppola D, Canyon D. Incremental community-based exit strategies for initiating and removing COVID-19 lockdowns. In: Daniel K. Inouye Asia-Pacific Center for Security Studies. Honolulu, HI: Daniel K. Inouye Asia-Pacific Center for Security Studies (2020).
33. Hyder A, Trinh A, Padmanabhan P, Marschhausen J. Wu, A, Evans A, et al. COVID-19 surveillance for local decision making: an academic, school district, and public health collaboration. Public Health Rep. (2021) 136:403–12. doi: 10.1177/00333549211018203
34. Storeng KT, de Bengy Puyvallée A. The smartphone pandemic: how big tech and public health authorities partner in the digital response to Covid-19. Glob Public Health. (2021) 16:1482–98. doi: 10.1080/17441692.2021.1882530
35. Lane ECA, Tran AA, Graulty CJ, Bumsted T. Rapid mobilization of medical students to provide health care workers with emergency childcare during the COVID-19 pandemic. Acad Med. (2021) 96:1302–5. doi: 10.1097/ACM.0000000000004115
36. Panneer S, Kantamaneni K, Pushparaj RRB, Shekhar S, Bhat L, Rice L. Multistakeholder participation in disaster management-the case of the COVID-19 pandemic. Healthcare (Basel). (2021) 9:203. doi: 10.3390/healthcare9020203
37. Loewenson R, Colvin CJ, Szabzon F, Das S, Khanna R, Coelho VSP, et al. Beyond command and control: A rapid review of meaningful community-engaged responses to COVID-19. Glob Pub Health. (2021) 16:1–15. doi: 10.1080/17441692.2021.1900316
38. Bruno B, Hurwitz HM, Mercer M, Mabel H, Sankary L, Morley G, et al. Incorporating stakeholder perspectives on scarce resource allocation: lessons learned from policymaking in a time of crisis. Camb Q Healthc Ethics. (2021) 30:390–402. doi: 10.1017/S0963180120000924
39. DeSalvo KB, O'Carroll PW, Koo D, Auerbach JM. Monroe JA. Public health 30: time for an upgrade. Am J Pub Health. (2016) 106:621–2. doi: 10.2105/AJPH.2016.303063
40. Torfing J, Peters GB, Pierre J, Sørensen E. Interactive Governance: Advancing the Paradigm, Chapter 7 - Metagovernance: The art of governing interactive governance. Oxford University Press. (2012). p. 122–44.
41. Apostolopoulos Y. Bridging the Divide: Where Complex Systems Science Meets Population Health Science (Chapter 1). New York, NY: Oxford University Press (2020).
42. Mattessich PW, Rausch EJ. Cross-sector collaboration to improve community health: a view of the current landscape. Health Aff (Project Hope). (2014) 33:1968–74. doi: 10.1377/hlthaff.2014.0645
43. Towe VL, Leviton L, Chandra A, Sloan JC, Tait M, Orleans T. Cross-sector collaborations and partnerships: essential ingredients to help shape health and well-being. Health Aff. (2016) 35:1964–9. doi: 10.1377/hlthaff.2016.0604
44. DeSalvo KB, Wang YC, Harris A, Auerbach J, Koo D. O'Carroll P. Public health 30: a call to action for public health to meet the challenges of the 21st century. Prev Chronic Dis. (2017) 14:E78. doi: 10.5888/pcd14.170017
45. 10 Essential Public Health Services EPHS Toolkit. Public Health National Center for Innovations. (2020).
46. Jarrah S, Khaldun J, Sellers K, Rich N. Bringing the essential public health services to life. J Public Health Manag Pract. (2021) 27:97–8. doi: 10.1097/PHH.0000000000001298
47. Romano SD, Blackstock AJ, Taylor EV, Felix SEB, Adjei S, Singleton CM, et al. Trends in racial and ethnic disparities in COVID-19 hospitalizations, by region — United States, March–December 2020. Morb Mort Wkly Rep. (2021) 70:560–5. doi: 10.15585/mmwr.mm7015e2
48. Dickinson KL, Roberts JD, Banacos N, Neuberger L, Koebele E, Hartigan E, et al. Structural racism and the COVID-19 experience in the United States. Health Secur. (2021) 19:S14–26. doi: 10.1089/hs.2021.0031
49. Galaitsi SE, Cegan JC, Volk K, Joyner M, Trump BD, Linkov I. The challenges of data usage for the United States' COVID-19 response. Int J Inf Manage. (2021) 59:102352. doi: 10.1016/j.ijinfomgt.2021.102352
50. Hester JA, Stange PV, Seeff LC, Davis JB, Craft CA. Towards Sustainable Improvements in Population Health: Overview of Community Integration Structures and Emerging Innovations in Financing. US: Centers for Disease Control and Prevention. (2015). p. 1–16.
51. Stone KW, Kintziger KW, Jagger MA, Horney JA. Public health workforce burnout in the COVID-19 response in the U.S. Int J Environ Res Public Health. (2021) 18:4369. doi: 10.3390/ijerph18084369
Keywords: COVID-19, community health, cross-sector collaboration, decision-making, crisis response
Citation: Biddell CB, Johnson KT, Patel MD, Smith RL, Hecht HK, Swann JL, Mayorga ME and Hassmiller Lich K (2022) Cross-sector decision landscape in response to COVID-19: A qualitative network mapping analysis of North Carolina decision-makers. Front. Public Health 10:906602. doi: 10.3389/fpubh.2022.906602
Received: 28 March 2022; Accepted: 29 July 2022;
Published: 16 August 2022.
Edited by:
Kara Durski, World Health Organization (Switzerland), SwitzerlandReviewed by:
Sharla Annette Smith, University of Kansas Medical Center, United StatesCopyright © 2022 Biddell, Johnson, Patel, Smith, Hecht, Swann, Mayorga and Hassmiller Lich. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caitlin B. Biddell, Y2JpZGRlbGxAbGl2ZS51bmMuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.