- 1School of Public Health, Southeast University, Nanjing, China
- 2Department of Humanities, Institute of Technology Carlow, Carlow, Ireland
- 3Faculty of Science and Engineering, University of Nottingham Ningbo China, Ningbo, China
- 4Network for Education and Research on Peace and Sustainability, Hiroshima University, Hiroshima, Japan
- 5Rufaidah Nursing College, Peshawar, Pakistan
- 6Faculty of Health Studies, University of Sarajevo, Sarajevo, Bosnia and Herzegovina
- 7Marketing, Fundação Dom Cabral—FDC, Nova Lima, MG, Brazil
Tobacco is both toxic and addictive. Mounting evidence shows that tobacco use has a detrimental impact on almost every aspect of human health, causing or worsening deadly public health crises from the cancer epidemic to the COVID-19 pandemic. However, while tobacco use is a threat to both personal and public health, it continues to surge across the world, especially in China and other low- and middle-income countries. To this end, this article argues in favor of using a ban on the sale of all tobacco products as a practical solution to the global tobacco use epidemic. It is our hope that insights provided by our work will inspire swift policy actions in countries such as China and beyond to curb the tide of rising tobacco consumption, so that populations around the world could be better shielded from the pervasive and long-lasting damage that tobacco products cause or compound.
Introduction
Tobacco is toxic. A preponderance of evidence shows that tobacco smoking has a detrimental impact on almost every aspect of human health, causing or worsening deadly epidemics from cancer to coronavirus disease 2019 (COVID-19) (1). Yet, despite the growing body of evidence that reinforces and restates its damaging impacts on personal and public health (2–7), tobacco use remains prevalent across the globe. Analyses, for instance, showed that, in 2019, there were 1.14 billion people who were current smokers; throughout a period of nearly three decades, they consumed more than 7.4 trillion cigarette equivalents of tobacco products (8). This cumulative consumption has exerted a sobering toll on society. Approximately 8 million lives have been lost to tobacco-related diseases each year (9), making the global death toll from tobacco use greater than the mortality of AIDS, malaria, and tuberculosis combined. Tobacco use is also highly addictive. In a 2018–2019 analysis of 87,709 participants aged 20–69 in China, researchers found that against the backdrop of an already high prevalence of 25.1% of current smoking, men in China had an even higher rate−47.6% (10). These sobering statistics help explain why once people initiate and become accustomed to tobacco use, the addiction becomes entrenched and exceedingly difficult to manage, even when there is access to evidence-based interventions that are easy to adopt, such as technology-based programs (11).
Taken together, these revelations explain why tobacco use exerts such a heavy burden on society—it costs the global economy $1.4 trillion each year, ranging from expenses incurred from healthcare utilization, lost productivity, fire damage, to cigarette litter-induced environmental harm (12). Unfortunately, these alarming data and trends are not subsiding, underscoring the growing need for more effective interventions to curb tobacco use around the world, especially in low- and middle-income countries—where over 80% of tobacco users live, individuals who often lack access to health care infrastructure that is essential to effectively treat and manage their addiction (1).
Although global tobacco control efforts have been ongoing for quite some time (13–21), they are often too fragmented to comprehensively address the tobacco use epidemic in a fundamental fashion—people's exposure and easy access to tobacco products. This means that, rather than incentivizing the tobacco industry to transform its businesses into those that focus on health-promoting goods or services, existing tobacco control policies often contain too many loopholes that allow these companies to circumvent accountability for their products' negative health impacts. Ranging from surreptitious marketing practices to the wide dissemination of addictive e-cigarettes (22–24), the industry has continued to perpetuate the global tobacco epidemic rather than to temper it. Even the recent tobacco control policy developed by the United States (U.S.), which aims to ban menthol-flavored cigarettes and related products (25), may lead to mixed results or unintended consequences. Announced in April 2022 and considered a public health win, the U.S. Food and Drug Administration's draft rule may be too narrow to limit or discourage people's access to tobacco products (26). A 2022 study that gauges current American smokers' responses to the forthcoming ban shows that 51% of the participants, who were recruited online anonymously, said they would use non-flavored cigarettes as alternatives (27).
Policies that can be bypassed by alternative tobacco products (e.g., e-cigarettes) could also inadvertently promote tobacco use and pose unnecessary barriers to people who are trying to quit. Analyzing findings of three randomized controlled trials that involve 1,607 smokers, for instance, researchers found that, compared to gradual cessation, abrupt smoking cessation is more likely to yield positive outcomes (28). This research suggests that a number of ongoing factors continue to counter the years of interventions implemented to reduce tobacco use. The fact that tobacco consumption remains a global epidemic around the world, underscores the urgent need for further tobacco control actions especially policies that are more comprehensive and could more directly reduce the tobacco industry's ability to expand public access and exposure to tobacco products. To this end, this article explores the advantages and potential trade-offs of a ban on the sale of all tobacco products as a practical policy intervention for combatting the global tobacco epidemic. Using China as an example, we argue that such a ban in a country with the world's largest population is (1) reasonable, (2) feasible, and (3) can benefit the broader global community. Any change, however small, in China (given the size of its population—around 1.5 billion people—and the scope of its economy—second-largest globally in terms of its gross domestic product) can profoundly help move the needle forward to stem the tide of tobacco use worldwide.
Secondhand smoke: An unintended consequence of using tobacco products
A tobacco product could be understood as “a product that can be consumed and consists, even partly, of tobacco” (29). In the context of this article, tobacco products refer to both conventional (e.g., cigarettes) and newer iterations (e.g., e-cigarettes). Unlike nutritious foods and effective medicines, which are essential for maintaining and sustaining personal and public health, tobacco products are deleterious and dispensable. Different from substances that are beneficial to human health and productivity, such as tea and coffee (30–32), almost all aspects of tobacco consumption are detrimental to personal and public health (33). Tobacco's damaging impacts on global health centers on its unique mode of consumption. Different from other addictive substances like cocaine, the smoke generated by tobacco products not only harms the health of the direct users (i.e., smokers), but also that of people who happen to be in the vicinity of the secondhand smoke.
In an analysis of data from 1990 to 2016, researchers found that even though progress has been made, the consequences of tobacco use on non-smokers remain high—i.e., in 2016, for every group of 52.3 individuals who smoked a mean of 24 years, there was an associated death of 1 individual attributable to secondhand smoke exposure (34). Though most, if not all, governments across the world agree on the end goal when it comes to tobacco control—elimination or eradication of tobacco use across society, especially among the young and vulnerable, they differ drastically in terms of the measures they implement to regulate tobacco use (33). One important example is China—the country is struggling with the damage that tobacco use has already caused but yet has the opportunity to make meaningful impacts by adopting and implementing a more coordinated tobacco control effort via a ban on tobacco products.
Case example: Impact of tobacco use in China
When it comes to tobacco products, China is simultaneously the world's largest producer, the biggest consumer, and its most traumatized victim (35). In a study of 71 countries—accounting for over 95% of the world's total cigarette use and 85% of the global population—between 1970 and 2015, researchers found that not only has China's tobacco use been skyrocketing, but its total consumption of cigarettes, in 2013 alone, was 2.5 million metric tons (MMT); this was greater than the combined consumption of the next 39 highest countries during the same period, including Russia (0.36 MMT), the U.S. (0.28 MMT), and Japan (0.20MMT) (36). Comparatively, China bears arguably the most alarming toll of tobacco use worldwide. It is estimated that approximately 4,100 people per day in China died from tobacco-related diseases (estimate from 2022) (37). This sobering statistic is projected to jump to 6,000 deaths per day−3 million per year—by 2050, if effective interventions are not taken or remain a low priority in the country (37). The high prevalence of tobacco use in China is even more chilling if the negative impacts of secondhand smoke exposure are considered. The World Health Organization reports that over 700 million non-smokers in China are exposed to secondhand smoke, among which, 180 million are children (35). Yet despite the sobering toll of tobacco use, the evidence of which has been accumulating for decades (38–41), China has been lagging behind in developing and adopting impactful policies and other effective tobacco control interventions to fight the growing health and socioeconomic repercussions caused by this adverse behavior (42).
More stringent tobacco control policies and related interventions are needed
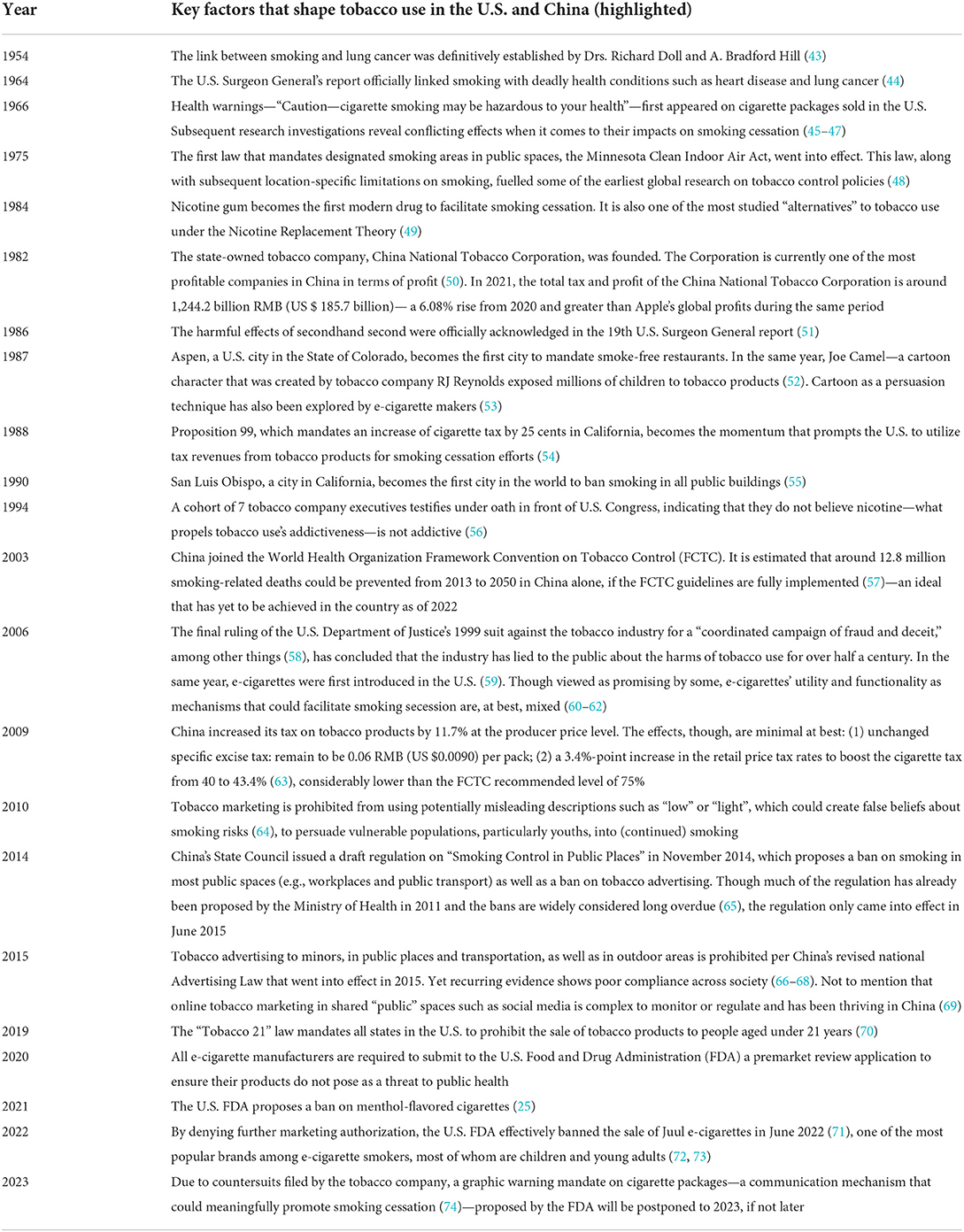
As illustrated in Table 1, meaningful tobacco control policies, especially those that can promote material changes in tobacco-related morbidity and mortality rates in the population have historically been negligible in countries like China. By contrast, tobacco control efforts have been more robust in developed nations such as the U.S. In spite of highly visible home to household tobacco brands such as Marlboro and powerful tobacco industry advertising, which normalized and socialized smoking with the zeitgeist at the time—from personal liberty to women's rights (75–77), the U.S. has been able to gradually and substantively reduce tobacco use among its diverse populations during the past several decades (78). Between 2000 and 2020, adult smoking rates in the U.S. dropped from 33.8 to 23.0% (78). Similar achievements have been observed in other countries such as India, the United Kingdom and Brazil. China, as one of the largest countries in the world, did not share in these improvements (see Figure 1) (78), though the scale, scope, and severity of its tobacco epidemic are simply too glaring to ignore, especially when they are coupled with known shortcomings of moderate control policies. These insights, collectively, suggest that stronger and more straightforward legislative actions, such as a ban on the sale of all tobacco products across the entire country (79–82), are urgently needed to avoid the catastrophic health and socioeconomic consequences that will likely mushroom as a result of the country's ever-growing tobacco use epidemic.
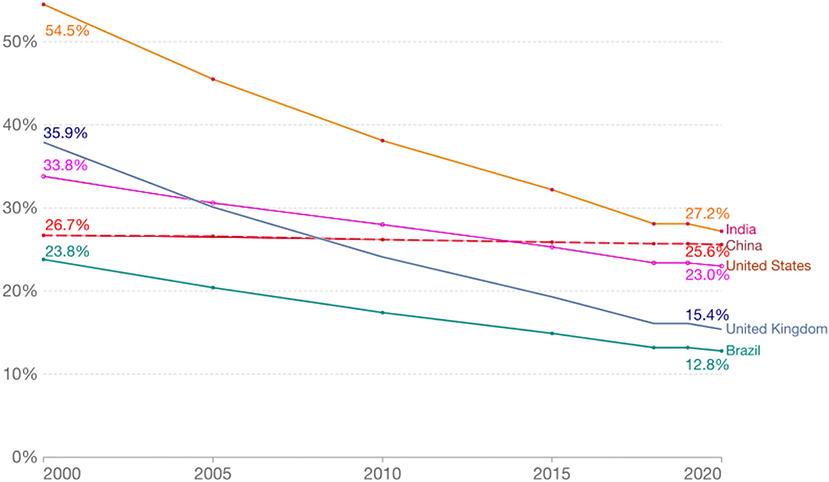
Figure 1. Percent of adult smokers from each of the selected countries, 2000 and 2020. Data source: The World Health Organization; Adults: people aged 15 years and older.
A ban on the sale of tobacco products
A ban on the sale of tobacco products is the prohibition of the sale or purchase of tobacco products, including e-cigarettes, across sectors of society within its borders. Again, using China as an example, this means that all business-to-business or person-to-person exchanges of tobacco products will be prohibited in the country, including international e-commerce. Different from a comprehensive ban on all tobacco-related activities, like the one adopted in Bhutan (83), a ban on the sale of tobacco products would only prohibit the exchange of tobacco products—both legally or in the back market within the borders of China, as opposed to controlling people's rights to access or use of tobacco products, not the least of which because the latter raised legal issues and could be extremely difficult to monitor or control. Under a sales ban, residents in China could still make international trips to obtain tobacco products, or for those who are truly determined, grow their own tobacco leaves, but they are not allowed to exchange these products. Similarly, tobacco farmers and corporations could still grow or manufacture tobacco products, but these products would not be allowed to be sold to people living in China. Compared to existing strategies, this policy intervention bears a multitude of advantages, most of which are its feasibility and practicality, not to mention a strong first step forward in addressing China's tobacco use epidemic.
Feasibility of establishing the ban
There are a number of reasons to call for action on a ban on the sale of all tobacco products. First, such a ban is simple and straightforward to understand and to implement. A common pitfall of many existing tobacco regulations is that they are often too complicated for the general public to understand or appreciate (84). A ban on the sale of all tobacco products means that tobacco products will no longer be available in the marketplace, or exchanged between people or businesses—a relatively straightforward policy that can be understood by tobacco users across age, education, or other socio-demographic spectra, as well as by other stakeholders such as sellers, marketers, and law enforcement agencies. A ban on the sale of all tobacco products is less complex than nuanced bans that are often seen in developed countries. A straightforward ban would also be more in line with many developing countries' public health realities. Different from high-income nations like the U.S., which have been changing the public's attitudes toward tobacco consumption for decades, countries like China, which have a more pronounced prevalence of smoking and less available public health resources, may need more rigorous and less reserved interventions to prevent their tobacco use epidemic from further expanding in a timely manner. A ban on the sale of all tobacco products, regardless of their flavors or modes of consumption, would be much easier to follow and carry out under these countries' circumstances.
Second, the people-first focus of the proposed ban could help facilitate public adherence. As opposed to prioritizing politics or profits, a ban on the sale of all tobacco products validates the government's determination and devotion to protecting public health, above and beyond short-term considerations such as political gains or losses. Considering the Chinese government's recent response to the COVID-19 pandemic, using a whole-of-society zero-COVID strategy approach, a direct and people-first policy from the government is not unattainable and could help the public better understand and appreciate the severity of the global tobacco use epidemic and adjust their mindset accordingly to comply with the policy. Third, similar to other countries that are burdened with the tobacco use epidemic, China has the urgency and the capacity to carry out a ban on the sale of all tobacco products successfully. Presently, approximately one in every three global tobacco users lives in China (9)—populations that are likely to both personify and perpetuate the country's raging double-whammy epidemics—the tobacco use epidemic and the cancer epidemic (85).
Fourth, in addition to tobacco-related morbidity and mortality, China's economic health is considerably compromised by the tobacco use epidemic. It is estimated that, in 2017 alone, the economic tolls of lung cancer on the country have reached over $25 billion (86), a considerable amount of financial burden that a ban on the sale of tobacco products could help in lowering. As such, China has the administrative motivation to carry out whole-of-society policies like a ban on the sale of all tobacco products across society. Fifth, and perhaps most importantly, China has the agency to ban the sale of tobacco products. For starters, the world's largest producer of cigarettes, China National Tobacco Corporation, is state-owned. On one hand, the nature of the company reveals how entrenched the tobacco industry is in the administrative fabric of China (87). But on the other hand, this also means that as long as officials in China are willing and committed, they could effectively implement a ban on the sale of all tobacco products without the need of back-and-forth negotiations with private sectors, as seen in other countries (88).
The largely state-owned nature of China's tobacco industry means that, when political will is well-established, government officials can instruct and transform its existing tobacco industry workforce into other industries that do not produce products that are debilitating to national and global health. Amid the COVID-19 pandemic, to protect children and adolescents from becoming too addicted to online gaming, China successfully regulated the duration of which youths could be exposed to these entertainment venues (89). In a similar vein, to alleviate the burden on school students and their parents, in 2021, China also banned for-profit private tutoring across the country (90). Taken together, these recent events and actions by China suggest that the world's largest country (by population size) has the capability to ban the sale of all tobacco products within its borders. It would be impactful if this can be accomplished by China in a timely manner, since, substance use, which is highly associated with tobacco use, has been prevalent and is on the rise across the globe (91). By designing, developing, and delivering bans that could eradicate the public's vulnerability toward addictive substances like tobacco, China could serve as a harbinger in the protection of the health and quality of life of the global community, above and beyond those living within its borders.
The broader implications and potential effects of banning tobacco products
The impacts of a ban on the sale of tobacco products could be largely categorized into two types: desirable outcomes and unintended consequences. A wide range of positive changes could be expected from the said ban. First, in addition to the welcoming impacts on society discussed earlier, a ban on the sale of tobacco products could also help countries across the globe better cope with the negative consequences of COVID-19 on personal and public health. Recurring evidence shows that COVID-19 could cause greater adverse health consequences to people with damaged lungs, such as tobacco users (3, 92, 93). A review of evidence on 32,849 COVID-19 patients across the globe shows that people with any smoking history experienced significantly more severe COVID-19 symptoms and worse hospitalization outcomes compared to non-users (92). In a study of 6,003 Italian adults amid the pandemic, researchers found that the total tobacco consumption has further increased by 9.1% (94). These findings suggest that there may be a vicious cycle between tobacco use and heightened COVID-19 risks. As COVID-19 continues evolving (95–99), and, paired with the rising presence of infectious diseases and geopolitical conflicts that could be equally damaging to our health systems (100–103), a ban on the sale of tobacco products should also be seen as an even more necessary step, since the vicious cycle between tobacco use and COVID-19 infections has been shown to worsen health conditions and lead to severe COVID-19 disease and death.
Second, a reduction in tobacco use could also persuade tobacco growers and producers to switch to other products or industries that do not harm planetary health. If history is a sagacious guide, the ultimate market force—synergistic dynamics between supply and demand—could be the best shadow policymaker for phasing out the tobacco industry. A ban on tobacco sale (demand drops) could lead to a material reduction in the marketability of tobacco products (short-term loss of profitability), which in turn, has the potential to incentivize tobacco farmers and producers to grow and market health-promoting crops instead of tobacco (long-term supply chain transformation). This would, effectively leverage the market forces and strategically use them to promote positive societal changes. Considering Chinese consumers' growing purchasing power and subsequent sway in the global economy (China has the largest population in the world and a growing economy), and the fact that China's largely state-owned tobacco industry is closely connected with the global tobacco scene (50, 104), the said ban, when optimally executed, has the potential to reduce the global presence of tobacco products right away in terms of sales and usage—the ultimate goal we hope tobacco control policies could achieve.
Third, it is also important to note that a ban on the sale of all tobacco products has the potential to introduce unintended consequences, such as enabling or deepening illicit markets for tobacco products. However, the potential for inadvertent outcomes neither means that they could not be predicted nor prevented. Policymakers in China and elsewhere, for example, could collaborate with researchers in academia, practitioners in the tobacco industry, public relations professionals and other experts and stakeholders to ensure that these unintended consequences are properly mitigated. Essentially, all policy interventions can yield both wanted and unwanted outcomes. A ban that could have unintended results should hardly surprise policymakers. Rather than pouring valuable public resources into developing less effective tobacco control policies, we believe it is more sensible and practical to invest in decisive intervention mechanisms, like the proposed ban, as its strength of impact and benefits should likely outweigh its unintended consequences (if any).
Conclusion
Tobacco is toxic and addictive. The preponderance of evidence on tobacco use's harm substantiates the call for a stronger, more straightforward policy intervention that bans the sale of all tobacco products, especially for developed countries that are lagging behind in tobacco control wins and for developing countries that have limited public health infrastructure or resources to launch multi-modal campaigns to counter the tobacco industry's aggressive sales and advertising of tobacco products. Using China as an example, this article presented key rationales for advocating the adoption and implementation of such a ban, suggesting that it is a practical policy intervention for the world stage. It is our hope that the insights provided in this perspective will inspire swift policy actions in curbing tobacco use across the globe. In places like China where the population is enormous and the health infrastructure is tenuous, even an incremental change in the prevalence of tobacco use could lead to significant improvements in tobacco-related healthcare utilization and costs, as well as salutary decreases in human suffering from predictable and preventable tobacco-related diseases and deaths. Time is ripe for society to control the tobacco epidemic with a bang.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
ZS, DM, AC, JA, SŠ, and CV conceptualized this work, reviewed the literature, as well as drafted and edited the manuscript for intellectual content.
Acknowledgments
The authors wish to express their gratitude to the editor and reviewers for their constructive input and kind feedback.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
COVID-19, coronavirus disease 2019; MMT, million metric tons; U.S., United States; FDA, U.S. Food and Drug Administration.
References
1. World Health Organization. Tobacco. (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/tobacco (accessed June 25, 2022).
2. Adashi EY, Vine MF, Margolin BH, Morrison HI, Hulka BS, et al. Cigarette smoking and sperm density: a meta-analysis. Fertil Steril. (1994) 61:35–43. doi: 10.1016/S0015-0282(16)56450-4
3. van Zyl-Smit RN, Richards G, Leone FT. Tobacco smoking and COVID-19 infection. Lancet Respir Med. (2020) 8:664–5. doi: 10.1016/S2213-2600(20)30239-3
4. Wen H, Xie C, Wang F, Wu Y, Yu C. Trends in disease burden attributable to tobacco in China, 1990-2017: findings from the Global Burden of Disease Study 2017. Front Public Health. (2020) 8:237. doi: 10.3389/fpubh.2020.00237
5. Aune D, Schlesinger S, Norat T, Riboli E. Tobacco smoking and the risk of sudden cardiac death: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. (2018) 33:509–21. doi: 10.1007/s10654-017-0351-y
6. Asthana S, Labani S, Kailash U, Sinha DN, Mehrotra R. Association of smokeless tobacco use and oral cancer: a systematic global review and meta-analysis. Nicotine Tobacco Res. (2019) 21:1162–71. doi: 10.1093/ntr/nty074
7. Yang JJ Yu D, Wen W, Shu XO, Saito E, Rahman S, et al. Tobacco smoking and mortality in Asia: a pooled meta-analysis. JAMA Network Open. (2019) 2:e191474–e191474. doi: 10.1001/jamanetworkopen.2019.1474
8. Reitsma MB, Kendrick PJ, Ababneh E, Abbafati C, Abbasi-Kangevari M, Abdoli A, et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet. (2021) 397:2337–60. doi: 10.1016/S0140-6736(21)01169-7
9. World Health Organization. WHO Global Report on Trends in Prevalence of Tobacco Use 2000-2025, fourth edition. World Health Organization: Geneva, Switzerland (2021).
10. Liu Z, Li YH, Cui ZY, Li L, Nie XQ, Yu CD, et al. Prevalence of tobacco dependence and associated factors in China: Findings from nationwide China Health Literacy Survey during 2018–2013. Lancet Reg Health Western Pac. (2022). 24:e100464. doi: 10.1016/j.lanwpc.2022.100464
11. Grabovac I, Oberndorfer M, Fischer J, Wiesinger W, Haider S, Dorner TE. Effectiveness of electronic cigarettes in smoking cessation: a systematic review and meta-analysis. Nicotine Tobacco Res. (2021) 23:625–34. doi: 10.1093/ntr/ntaa181
12. World Health Organization. The Economics of Tobacco. (2021). Available online at: https://www.euro.who.int/en/health-topics/disease-prevention/tobacco/publications/the-economics-of-tobacco (accessed December 8, 2021).
13. Beaglehole R, Bates C, Youdan B, Bonita R. Nicotine without smoke: fighting the tobacco epidemic with harm reduction. Lancet. (2019) 394:718–20. doi: 10.1016/S0140-6736(19)31884-7
14. Flor LS, Reitsma MB, Gupta V, Ng M, Gakidou E. The effects of tobacco control policies on global smoking prevalence. Nat Med. (2021) 27:239–43. doi: 10.1038/s41591-020-01210-8
15. Allen LN, Wigley S, Holmer H. Implementation of non-communicable disease policies from 2015 to 2020: a geopolitical analysis of 194 countries. Lancet Global Health. (2021) 9:e1528–38. doi: 10.1016/S2214-109X(21)00359-4
16. Erinoso O, Smith KC, Iacobelli M, Saraf S, Welding K, Cohen JE, et al. Global review of tobacco product flavour policies. Tob Control. (2021) 30:373. doi: 10.1136/tobaccocontrol-2019-055454
17. Koval R, Dorrler N, Schillo B. Tobacco industry advertising: efforts to shift public perception of big tobacco with paid media in the USA. Tobacco Control. (2022) 2022:tobaccocontrol-2021-057189. doi: 10.1136/tobaccocontrol-2021-057189
18. Gupta R, Pednekar MS, Kumar R, Goel S. Tobacco cessation in India—current status, challenges, barriers and solutions. Indian J Tuberc. (2021) 68s:S80–5. doi: 10.1016/j.ijtb.2021.08.027
19. Kumar A, Gupta A, Goel S, Gauba K, Goyal A. Adherence to the tobacco-free educational institution guidelines at schools of Raipur Rani, Haryana. Indian J Public Health. (2021) 65:67–70. doi: 10.4103/ijph.IJPH_38_20
20. Goel S, Siddiqi K, Singh RJ, Lal P, Aghi MB, Gupta P, et al. Fuelling the tuberculosis epidemic: The role of tobacco control in ending the TB emergency. Indian J Tuberc. (2019) 66:555–60. doi: 10.1016/j.ijtb.2019.11.009
21. Lal P, Srinath S, Goel S, Singh RJ, Sharma D, Kumar R, et al. Unravelling India's tobacco epidemic–priorities and recommendations for the second round of Global Adult Tobacco Survey (GATS). Glob Health Promot. (2015) 22:7–19. doi: 10.1177/1757975914536914
22. Watts C, Burton S, Freeman B. 'The last line of marketing': Covert tobacco marketing tactics as revealed by former tobacco industry employees. Glob Public Health. (2021) 16:1000–13. doi: 10.1080/17441692.2020.1824005
23. Russell AM, Yang M, Barry AE, Merianos AL, Lin HC. Stealth vaping among college students on four geographically distinct tobacco-free college campuses: prevalence and practices. Nicotine Tobacco Res. (2022) 24:342–8. doi: 10.1093/ntr/ntab153
24. Ramamurthi D, Chau C, Jackler RK. JUUL and other stealth vaporisers: hiding the habit from parents and teachers. Tob Control. (2019) 28:610. doi: 10.1136/tobaccocontrol-2018-054455
25. The United States Food and Drug Administration. FDA Proposes Rules Prohibiting Menthol Cigarettes and Flavored Cigars to Prevent Youth Initiation, Significantly Reduce Tobacco-Related Disease and Death (2022). Available online at: https://www.fda.gov/news-events/press-announcements/fda-proposes-rules-prohibiting-menthol-cigarettes-and-flavored-cigars-prevent-youth-initiation (accessed June 25, 2022).
26. Denlinger-Apte RL, Lockhart DE, Strahley AE, Cassidy RN, Donny EC, O'Connor RJ, et al. “I think it's a good idea for the people that's young, the kids, but for someone like me it's a bad idea”—Interviews about a US menthol cigarette ban with people who smoke menthol cigarettes. Drug Alcohol Depend. (2022) 232:109293. doi: 10.1016/j.drugalcdep.2022.109293
27. Yang Y, Lindblom EN, Ward KD, Salloum RG. How smokers of menthol cigarettes and flavored cigars might respond to FDA's proposed bans. Nicotine Tobacco Res. (2022) 2022:ntac078. doi: 10.1093/ntr/ntac078
28. Tan J, Zhao L, Chen H. A meta-analysis of the effectiveness of gradual versus abrupt smoking cessation. Tob Induc Dis. (2019) 17:09–09. doi: 10.18332/tid/100557
29. The U.K. Government. The Tobacco and Related Products Regulations 2016 (2016). Available online at: https://www.legislation.gov.uk/uksi/2016/507/part/1/made (accessed June 25, 2022).
30. Liu D, Li ZH, Shen D, Zhang PD, Song WQ, Zhang WT, et al. Association of sugar-sweetened, artificially sweetened, and unsweetened coffee consumption with all-cause and cause-specific mortality: A large prospective cohort study. Ann Intern Med. (2022) 175:909–17. doi: 10.7326/M21-2977
31. Lin FJ, Wei XL, Liu HY Li H, Xia Y, Wu DT, et al. State-of-the-art review of dark tea: from chemistry to health benefits. Trends Food Sci Technol. (2021) 109:126–38. doi: 10.1016/j.tifs.2021.01.030
32. Sargent A, Watson J, Topoglu Y, Ye H, Suri R, Ayaz H. Impact of tea and coffee consumption on cognitive performance: an fNIRS and EDA study. Appl Sci. (2020) 10:2390. doi: 10.3390/app10072390
33. World Health Organization. WHO Report on the Global Tobacco Epidemic 2021: Addressing New and Emerging Products. Geneva: World Health Organization (2021).
34. Yousuf H, Hofstra M, Tijssen J, Leenen B, Lindemans JW, van Rossum A, et al. Estimated worldwide mortality attributed to secondhand tobacco smoke exposure, 1990–2016. JAMA Netw Open. (2020) 3:e201177. doi: 10.1001/jamanetworkopen.2020.1177
35. World Health Organization. Tobacco in China. (2022). Available online at: https://www.who.int/china/health-topics/tobacco (accessed June 28, 2022).
36. Hoffman SJ, Mammone J, Van Katwyk SR, Sritharan L, Tran M, Al-Khateeb S, et al. Cigarette consumption estimates for 71 countries from 1970 to 2015: systematic collection of comparable data to facilitate quasi-experimental evaluations of national and global tobacco control interventions. BMJ. (2019) 365:l2231. doi: 10.1136/bmj.l2231
37. Chen Z, Peto R, Zhou M, Iona A, Smith M, Yang L, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. (2015) 386:1447–56. doi: 10.1016/S0140-6736(15)00340-2
38. Liu BQ, Peto R, Chen ZM, Boreham J, Wu YP Li JY, et al. Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ. (1998) 317:1411. doi: 10.1136/bmj.317.7170.1411
39. Niu SR, Yang GH, Chen ZM, Wang JL, Wang GH, He XZ, et al. Emerging tobacco hazards in China: 2. Early mortality results from a prospective study. BMJ. (1998) 317:1423. doi: 10.1136/bmj.317.7170.1423
40. Li Q, Hsia J, Yang G. Prevalence of smoking in China in 2010. New Engl J Med. (2011) 364:2469–70. doi: 10.1056/NEJMc1102459
41. Gu D, Kelly TN, Wu X, Chen J, Samet JM, Huang JF, et al. Mortality attributable to smoking in China. New Engl J Med. (2009) 360:150–9. doi: 10.1056/NEJMsa0802902
42. Yang G, Wang Y, Wu Y, Yang J, Wan X. The road to effective tobacco control in China. Lancet. (2015) 385:1019–28. doi: 10.1016/S0140-6736(15)60174-X
43. Doll R, Hill AB. The mortality of doctors in relation to their smoking habits. Br Med J. (1954) 1:1451. doi: 10.1136/bmj.1.4877.1451
44. U.S. Dept. of Health, Education, and Welfare, Public Health Service. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington, DC: U.S. Dept. of Health, Education, and Welfare, Public Health Service (1964).
45. Maynard OM, Attwood A, O'Brien L, Brooks S, Hedge C, Leonards U, et al. Avoidance of cigarette pack health warnings among regular cigarette smokers. Drug Alcohol Depend. (2014) 136:170–4. doi: 10.1016/j.drugalcdep.2014.01.001
46. Drovandi A, Teague PA, Glass B, Malau-Aduli B. Smoker perceptions of health warnings on cigarette packaging and cigarette sticks: a four-country study. Tob Induc Dis. (2019) 17:23. doi: 10.18332/tid/104753
47. Drovandi A, Teague PA, Glass B, Malau-Aduli B. A systematic review of the perceptions of adolescents on graphic health warnings and plain packaging of cigarettes. Syst Rev. (2019) 8:25. doi: 10.1186/s13643-018-0933-0
48. Emont SL, Choi WS, Novotny TE, Giovino GA. Clean indoor air legislation, taxation, and smoking behaviour in the United States: an ecological analysis. Tob Control. (1993) 2:13. doi: 10.1136/tc.2.1.13
49. Lindson N, Chepkin SC, Ye W, Fanshawe TR, Bullen C, Hartmann-Boyce J. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Datab Syst Rev. (2019) 2019:CD013308. doi: 10.1002/14651858.CD013308
50. Fang J, Lee K, Sejpal N. The China National Tobacco Corporation: from domestic to global dragon? Glob Public Health. (2017) 12:315–34. doi: 10.1080/17441692.2016.1241293
51. Centers for Disease Control and Prevention. 1986 Surgeon General's report: the health consequences of involuntary smoking. MMWR Morb Mortal Wkly Rep. (1986) 35:769–70.
52. DiFranza JR, Richards JW, Paulman PM, Wolf-Gillespie N, Fletcher C, Jaffe RD, et al. RJR Nabisco's cartoon camel promotes camel cigarettes to children. JAMA. (1991) 266:3149–53. doi: 10.1001/jama.266.22.3149
53. Allem JP, Cruz TB, Unger JB, Toruno R, Herrera J, Kirkpatrick MG. Return of cartoon to market e-cigarette-related products. Tob Control. (2019) 28:555. doi: 10.1136/tobaccocontrol-2018-054437
54. California Department of Public Health. Legislative Mandate for Tobacco Control—Proposition 99. (2017). Available online at: https://www.cdph.ca.gov/Programs/CCDPHP/DCDIC/CTCB/Pages/LegislativeMandateforTobaccoControlProposition99-.aspx (accessed June 30, 2022).
55. County of San Luis Obispo. Tobacco Control Coalition. (2020). Available online at: https://www.slocounty.ca.gov/https/www-flavorshookkids-org/top.aspx (accessed June 30, 2022).
56. Marwick C. Tobacco hearings: penetrating the smoke screen. JAMA. (1994) 271:1562–1562. doi: 10.1001/jama.271.20.1562
57. Levy D, Rodríguez-Buño RL, Hu TW, Moran AE. The potential effects of tobacco control in China: projections from the China SimSmoke simulation model. BMJ Br Med J. (2014) 348:g1134. doi: 10.1136/bmj.g1134
58. U.S. Department of Justice. Statement by Attorney General Janet Reno on the Filing Against the Major Tobacco Companies (1999). Available online at: https://www.justice.gov/archive/opa/pr/1999/September/430ag.htm (accessed June 30, 2022).
59. U.S. Department of Justice. The Evolution and Impact of Electronic Cigarettes (2020). Available online at: https://nij.ojp.gov/topics/articles/evolution-and-impact-electronic-cigarettes (accessed June 30, 2022).
60. Chan GC, Stjepanović D, Lim C, Sun T, Anandan AS, Connor JP, et al. A systematic review of randomized controlled trials and network meta-analysis of e-cigarettes for smoking cessation. Addict Behav. (2021) 119:106912. doi: 10.1016/j.addbeh.2021.106912
61. Berry KM, Reynolds LM, Collins JM, Siegel MB, Fetterman JL, Hamburg NM, et al. E-cigarette initiation and associated changes in smoking cessation and reduction: the Population Assessment of Tobacco and Health Study, 2013-2015. Tob Control. (2019) 28:42. doi: 10.1136/tobaccocontrol-2017-054108
62. Wang RJ, Bhadriraju S, Glantz SA. E-cigarette use and adult cigarette smoking cessation: a meta-analysis. Am J Public Health. (2020) 111:230–46. doi: 10.2105/AJPH.2020.305999
63. Hu T-W, Mao Z, Shi J. Recent tobacco tax rate adjustment and its potential impact on tobacco control in China. Tob Control. (2010) 19:80. doi: 10.1136/tc.2009.032631
64. Bansal-Travers M, Hammond D, Smith P, Cummings KM. The impact of cigarette pack design, descriptors, and warning labels on risk perception in the US. Am J Prev Med. (2011) 40:674–82. doi: 10.1016/j.amepre.2011.01.021
65. World Health Organization. Smoke-Free Policies in China: Evidence of Effectiveness and Implications for Action. Geneva: World Health Organization (2015).
66. Nian Q, Cohen JE, Cui Y, Zhang S. Tobacco retailers around schools in 10 cities across China. Tobacco Control. (2022) 2022:tobaccocontrol-2022-057367. doi: 10.1136/tobaccocontrol-2022-057367
67. Zheng P, Xiao L, Wang F, Yang G. Comprehensive ban on tobacco advertising, promotion and sponsorship. In:G. Yang, , editor. Tobacco Control in China. Singapore: Springer Singapore (2018). p. 245–84. doi: 10.1007/978-981-10-8315-0_12
68. Hoe C, Cohen JE, Yang T, Peng S, Zhang W. Association of cigarette production and tobacco retailer density on secondhand smoke exposure in urban China. Tobacco Control. 2021:tobaccocontrol-2021-056655. doi: 10.1136/tobaccocontrol-2021-056655
69. Wang X, Xiong Y, Zhao W. Tobacco control challenges in China: big data analysis of online tobacco marketing information. Int J Nurs Sci. (2020) 7:S52–s60. doi: 10.1016/j.ijnss.2020.07.002
70. U.S. Food and Drug Administration. Tobacco 21. (2021). Available online at: https://www.fda.gov/tobacco-products/retail-sales-tobacco-products/tobacco-21 (accessed June 30, 2022).
71. U.S. Food and Drug Administration. FDA Denies Authorization to Market Juul Products. (2022). Available online at: https://www.fda.gov/news-events/press-announcements/fda-denies-authorization-market-juul-products (accessed June 30, 2022).
72. Gentzke AS, Wang TW, Cornelius M, Park-Lee E, Ren C, Sawdey MD, et al. Tobacco product use and associated factors among middle and high school students - national youth tobacco survey, United States, 2021. MMWR Surveill Summ. (2022) 71:1–29. doi: 10.15585/mmwr.ss7105a1
73. U.S. Food and Drug Administration. Results from the Annual National Youth Tobacco Survey. (2022). Available online at: https://www.fda.gov/tobacco-products/youth-and-tobacco/results-annual-national-youth-tobacco-survey (accessed June 30, 2022).
74. Tam J, Jeon J, Thrasher JF, Hammond D, Holford TR, Levy DT, et al. Estimated prevalence of smoking and smoking-attributable mortality associated with graphic health warnings on cigarette packages in the US From 2022 to 2100. JAMA Health Forum. (2021) 2:e212852–e212852. doi: 10.1001/jamahealthforum.2021.2852
75. Toll BA, Ling PM. The Virginia Slims identity crisis: an inside look at tobacco industry marketing to women. Tob Control. (2005) 14:172. doi: 10.1136/tc.2004.008953
76. Markle GE, Troyer RJ. Smoke gets in your eyes: cigarette smoking as deviant behavior. Soc Probl. (1979) 26:611–25. doi: 10.1525/sp.1979.26.5.03a00110
77. Amos A, Haglund M. From social taboo to “torch of freedom”: the marketing of cigarettes to women. Tob Control. (2000) 9:3. doi: 10.1136/tc.9.1.3
78. Ritchie H, Roser M. Smoking. (2022). Available online at: https://ourworldindata.org/smoking (accessed June 30, 2022).
79. Grill K, Voigt K. The case for banning cigarettes. J Med Ethics. (2016) 42:293. doi: 10.1136/medethics-2015-102682
80. Conly S. The case for banning cigarettes. J Med Ethics. (2016) 42:302. doi: 10.1136/medethics-2016-103520
81. Proctor RN. Why ban the sale of cigarettes? The case for abolition. Tobacco Control. (2013) 22:i27. doi: 10.1136/tobaccocontrol-2012-050811
82. Wilkinson TM. Smokers' regrets and the case for public health paternalism. Public Health Ethics. (2021) 14:90–9. doi: 10.1093/phe/phab002
83. The Royal Government and People of Bhutan. Tobacco Control Act of Bhutan. (2010). Available online at: https://www.tobaccocontrollaws.org/files/live/Bhutan/Bhutan%20-%20Tobacco%20Control%20Act.pdf (accessed January 30, 2022).
84. Mlinarić M, Hoffmann L, Kunst AE, Schreuders M, Willemsen MC, et al. Explaining mechanisms that influence smoke-free implementation at the local level: a realist review of smoking bans. Nicotine Tobacco Res. (2019) 21:1609–20. doi: 10.1093/ntr/nty206
85. Parascandola M, Xiao L. Tobacco and the lung cancer epidemic in China. Transl Lung Cancer Res. (2019) 8:S21–30. doi: 10.21037/tlcr.2019.03.12
86. Liu C, Shi J, Wang H, Yan X, Wang L, Ren J, et al. Population-level economic burden of lung cancer in China: Provisional prevalence-based estimations, 2017-2030. Chin J Cancer Res. (2021) 33:79–92. doi: 10.21147/j.issn.1000-9604.2021.01.09
87. Li C. The Political Mapping of China's Tobacco Industry and Anti-Smoking Campaign. Washington, D.C.: The Brookings Institution (2012).
88. Peruga A, López MJ, Martinez C, Fernández E. Tobacco control policies in the 21st century: achievements and open challenges. Mol Oncol. (2021) 15:744–52. doi: 10.1002/1878-0261.12918
89. BBC. China Cuts Children's Online Gaming to One Hour. (2021). Available online at: https://www.bbc.com/news/technology-58384457 (accessed June 25, 2022).
90. Reuters. China Bans Private Tutors From Giving Online Classes. (2021). Available online at: https://www.reuters.com/world/china/china-says-private-tutors-will-not-be-able-offer-classes-online-2021-09-08/ (accessed June 25, 2022).
91. Centers for Disease Control and Prevention. Drug Overdose Deaths in the U.S. Top 100,000 Annually. (2021). Available online at: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm (accessed December 8, 2021).
92. Reddy RK, Charles WN, Sklavounos A, Dutt A, Seed PT, Khajuria A. The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. J Med Virol. (2021) 93:1045–56. doi: 10.1002/jmv.26389
93. Hopkinson NS, Rossi N, El-Sayed_Moustafa J, Laverty AA, Quint JK, Freidin M. Current smoking and COVID-19 risk: results from a population symptom app in over 24 million people. Thorax. (2021) 76:714. doi: 10.1136/thoraxjnl-2020-216422
94. Carreras G, Lugo A, Stival C, Amerio A, Odone A, Pacifici R, et al. Impact of COVID-19 lockdown on smoking consumption in a large representative sample of Italian adults. Tobacco Control. (2021) 2021:tobaccocontrol-2020-056440. doi: 10.1136/tobaccocontrol-2020-056440
95. Kofman A, Kantor R, Adashi EY. Potential COVID-19 endgame scenarios: eradication, elimination, cohabitation, or conflagration? JAMA. (2021) 326:303–4. doi: 10.1001/jama.2021.11042
96. Su Z, Wen J, McDonnell D, Goh E, Li X, Šegalo S, et al. Vaccines are not yet a silver bullet: The imperative of continued communication about the importance of COVID-19 safety measures. Brain Behav Immun Health. (2021) 12:100204. doi: 10.1016/j.bbih.2021.100204
97. Nealon J, Cowling BJ. Omicron severity: milder but not mild. Lancet. (2022) 399:412–3. doi: 10.1016/S0140-6736(22)00056-3
98. Su Z, Cheshmehzangi A, McDonnell D, da Veiga CP, Xiang YT, et al. Mind the “vaccine fatigue”. Front Immunol. (2022). 13:839433. doi: 10.3389/fimmu.2022.839433
99. Su Z, McDonnell D, Ahmad J, Cheshmehzangi A, Xiang YT, et al. Mind the “worry fatigue” amid Omicron scares. Brain Behav Immun. (2022) 101:60–1. doi: 10.1016/j.bbi.2021.12.023
100. Carlson CJ, Albery GF, Merow C, Trisos CH, Zipfel CM, Eskew EA, et al. Climate change increases cross-species viral transmission risk. Nature. (2022) 607:555–62. doi: 10.1038/s41586-022-04788-w
101. Adashi EY, Cohen IG. The pandemic preparedness program: reimagining public health. JAMA. (2022) 327:219–20. doi: 10.1001/jama.2021.23656
102. Su Z, McDonnell D, Bentley BL, He J, Shi F, Cheshmehzangi A, et al. Addressing Biodisaster X threats with artificial intelligence and 6G technologies: literature review and critical insights. J Med Internet Res. (2021) 23:e26109. doi: 10.2196/26109
103. Su Z, McDonnell D, Cheshmehzangi A, Ahmad J, Šegalo S, Pereira da Veiga C, et al. Public health crises and Ukrainian refugees. Brain Behav Immun. (2022) 103:243–5. doi: 10.1016/j.bbi.2022.05.004
Keywords: tobacco industry, ban, cancer, public health, health policy, intervention
Citation: Su Z, McDonnell D, Cheshmehzangi A, Ahmad J, Šegalo S and da Veiga CP (2022) A call to ban the sale of tobacco products. Front. Public Health 10:904971. doi: 10.3389/fpubh.2022.904971
Received: 28 March 2022; Accepted: 26 July 2022;
Published: 10 November 2022.
Edited by:
Sonu Goel, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
Tony Kuo, University of California, Los Angeles, United StatesCopyright © 2022 Su, McDonnell, Cheshmehzangi, Ahmad, Šegalo and da Veiga. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhaohui Su, c3V6aGFvaHVpc3poQHllYWgubmV0; Claudimar Pereira da Veiga, Y2xhdWRpbWFyLnZlaWdhQGZkYy5vcmcuYnI=; Y2xhdWRpbWFyLnZlaWdhQGdtYWlsLmNvbQ==
 Zhaohui Su
Zhaohui Su Dean McDonnell
Dean McDonnell Ali Cheshmehzangi
Ali Cheshmehzangi Junaid Ahmad
Junaid Ahmad Sabina Šegalo
Sabina Šegalo Claudimar Pereira da Veiga
Claudimar Pereira da Veiga