
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 30 June 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.904792
 Azmeraw Ambachew Kebede1
Azmeraw Ambachew Kebede1 Mastewal Belayneh Aklil1*
Mastewal Belayneh Aklil1* Dereje Nibret Gessesse1
Dereje Nibret Gessesse1 Nuhamin Tesfa Tsega2
Nuhamin Tesfa Tsega2 Wubedle Zelalem Temesgan1
Wubedle Zelalem Temesgan1 Marta Yimam Abegaz1
Marta Yimam Abegaz1 Tazeb Alemu Anteneh1
Tazeb Alemu Anteneh1 Nebiyu Solomon Tibebu1
Nebiyu Solomon Tibebu1 Haymanot Nigatu Alemu1
Haymanot Nigatu Alemu1 Tsion Tadesse Haile1
Tsion Tadesse Haile1 Asmra Tesfahun Seyoum1
Asmra Tesfahun Seyoum1 Agumas Eskezia Tiguh1
Agumas Eskezia Tiguh1 Ayenew Engida Yismaw1
Ayenew Engida Yismaw1 Goshu Nenko3
Goshu Nenko3 Kindu Yinges Wondie1
Kindu Yinges Wondie1 Birhan Tsegaw Taye4
Birhan Tsegaw Taye4 Muhabaw Shumye Mihret1
Muhabaw Shumye Mihret1Background: In developing countries, intimate partner violence is increasing alarmingly, though attention to this issue is rarely given. It has devastating effects on the general wellbeing of women, pregnancy outcomes, and the long-term health of children, and this needs to be addressed. Hence, this study was designed to assess intimate partner violence and associated factors in northwest Ethiopia.
Methods: A community-based cross-sectional study was conducted from July 1st to August 30th, 2021, among 858 postpartum women in Gondar city. A cluster sampling technique was employed to select the study participants. EPI DATA version 4.6 and SPSS 25 were used for data entry, cleaning and analysis, respectively. A bivariable and multivariable logistic regression model was fitted to identify factors associated with intimate partner violence. The level of significant association was declared using the adjusted odds ratio (AOR) with 95 % confidence interval (CI) and a p-value of ≤ 0.05.
Results: In this study, 48.6% of women indicated having experienced intimate partner violence during pregnancy (95% CI: 45.3, 51.7). The odds of intimate partner violence during pregnancy were significantly higher among women who were not able to read and write (AOR = 4.96; 95% CI: 2.15, 11.41), were private workers (AOR = 1.78; 95% CI: 1.05, 3.02), and had low decision-making power (AOR = 1.43; 95% CI: 1.06, 1.95), a poor social support (AOR = 1.99; 95% CI: 1.32, 3.02), and unsupported pregnancy by family (AOR = 2.32; 95% CI: 1.26, 4.24). Whereas a family size of ≥ 5 (AOR = 0.73; 95% CI: 0.54, 0.98) appeared to be a protective factor for intimate partner violence.
Conclusion: The magnitude of intimate partner violence was unacceptably high in the study area and connected to poor women's empowerment and social determinants of health. Thus, it is important to focus on interventions that improve women's access to social support and allow them to participate in all aspects of household decision-making through community-based structures and networks. It is also important to encourage women to improve their educational status and arrange risk-free employment opportunities.
Intimate partner violence (IPV) is a form of violence against a woman by her current or former spouse, leading to pain, psychological threat, and even death (1). It is one of the most common forms of violence against women (1, 2). Violence against women is increasing in Ethiopia, though little attention is paid to violence committed by intimate partners, especially against pregnant women (3). Pregnant women are more vulnerable psychologically and physically because of their pregnancy and IPV also to pose a risks to the unborn child (4, 5).
Existing evidence shows that three-quarters of women worldwide have experienced physical violence by their intimate partner; one-third of these women have been physically and/or sexually abused by their intimate partners (6). About 53.7% of women experienced either physical or sexual violence annually, and 70.9% of all women experience IPV during their lifetime (7). The magnitude of IPV ranged from 4–54% worldwide (8). Other studies conducted in Uganda and Gambia revealed IPV during pregnancy was 40.6 and 67%, respectively (9, 10). In Ethiopia, the pooled prevalence of IPV was 26.1% in 2018 (11).
Intimate partner violence (IPV) during pregnancy is associated with long-term effects on the physical and mental disorders of women and children (2, 3, 12). Some of the negative effects of IPV on women include pain, sexually transmitted infections (STI), traumatic fistula, inflammatory diseases of the pelvis (PID), and poor general health (13, 14). IPV is also has been associated with mental health disorders including anxiety, depression, suicidal ideation, and reduced health-seeking practices, poor motherhood, and addiction to different risky behaviors (i.e. drinking alcohol, cigarette smoking) (15–18). At its worst, IPV during pregnancy could result in unpleasant birth outcomes, such as fetal loss, low birth weight, premature birth, abortion, and infant death (19, 20).
Despite the endorsement of appropriate and effective legal policies to promote women's rights, combating violence against women is a major challenge in developing countries, including Ethiopia (21). Previous studies in Ethiopia identified that factors like lower women's educational level, lower decision-making power, poor social support, male dominance, alcohol consumption, and cigarette smoking by partners increase the occurrence of IPV during pregnancy (5, 7, 22, 23). Studies showed that economic dependence of wives on their husbands are at higher risk for IPV due to lack of respection, affordable housing options and poverty (24, 25).
Most of the previous studies evaluated IPV during pregnancy giving a special focus on physical violence. However, sexual and emotional violence are also considered to be determinants of the wellbeing of women and their children. This study stands in accordance with the recently adopted 2016 global agenda, which is aimed at ensuring women's empowerment and gender equality in every country (26). Moreover, research on violence against women, especially IPV during pregnancy, is limited in the study area. Therefore, understanding IPV and its determinant factors are imperative for a country like Ethiopia to design and combat violence against women during pregnancy, which in turn will improve maternal and child health. Hence, this study focused on assessing the prevalence of and factors associated with IPV during pregnancy in Gondar city, northwest Ethiopia. Based on our objectives we hypothesized the following point: Increasing women's education level, having high household decision making power and pregnancy supported by family have significant impact in reduction of IPV during pregnancy.
A community-based cross-sectional study was conducted in Gondar city from July 1st to August 30th, 2021.
This study was conducted in Gondar city. The city is located in Central Gondar Zone, Amhara national regional state, northwest Ethiopia. It is located 750 km from Addis Ababa, the capital city of Ethiopia. There are 1 governmental referral hospital, 8 governmental health centers, 22 health posts, 1 private primary hospital, and 1 general hospital serving the city and other populations outside of the city. The recent estimated total population of the city is 432,191, of whom 224,508 females about 133, 477 (30.88%) of these females are in the reproductive age group (unpublished data by Amhara regional state, 2021).
All women who gave birth in the 6 months prior to data collection were the study population. All women residing for at least 6 months before the data collection period were included in the study.
The single population formula was used to calculate the necessary sample size for the current study by considering the following assumptions: the proportion of IPV-44.5% (27), level of confidence-95%, and margin of error-5%. Therefore, the sample size (n) = 380. Based on a design effect of 2 (since cluster sampling used) and a non-response rate of 10 %, a total sample size of 836 women needed.
In Gondar city, there are 22 kebeles (the smallest administrative unit in the government structure), from which 30% of the total kebeles (seven kebeles) were randomly selected by the lottery method. To reach out to the eligible women, a house-to-house visit was carried out in the selected kebeles (clusters). All women found to be eligible for the study were interviewed. Finally, due to the nature of cluster sampling, 858 women were included in the study.
Intimate partner violence was the outcome variable, whereas women's age, women's occupation, monthly income, religion, women's educational status, marital status, family size, parity, antenatal care (ANC) visit, the number of ANC visits, whether the pregnancy was supported or not by family, pregnancy was planned or not, husband's educational status, husband's occupation, woman's household decision-making power, media exposure, and social support were the independent variables.
Intimate partner is considered as a current spouse, co-habited partner, current boyfriends, or former partner or spouse. If the respondent said “Yes” to any one of the ranges of sexual, psychological, and physical or any combination of the three coercive acts regardless of the legal status of the relationship with current/former intimate partner, it was considered as intimate partner violence (28).
The ability of women to act self-sufficiently about the household activities including their health, children's health, freedom of movement, and control over finance without needing permission from another person (29). Eight questions were prepared to assess the household decision-making power of women. The women's responses were coded 2 (if women decided independently), 1 (if women decided with their husbands), and 0 (if the decision was made by the husband or somebody else). The total score ranged from 0 to16. Thus, based on the summative score of variables designed to assess household decision-making power, women who were answered above the mean value were considered as having higher decision-making power (29, 30).
The Oslo-3 Social Support Scale (OSSS-3) was used to measure social support. The scale consists of 3 items addressing the number of close intimates to the woman, perceived level of concern from others, and perceived easiness of getting support from neighbors. Accordingly, the level of social support was categorized as “poor” with a score of 3–8; “moderate” with a score of 9–11; and “strong” with a score of 12–14 (31).
Study participants were asked how often they watched television, read a newspaper, or listened to the radio. Respondents who responded at least once a week are considered to be regularly exposed to that form of media (21).
After reviewing related literature and WHO multi country study on women's health and domestic violence (5, 8, 27, 28) the data collection instrument was developed to elicit required information on IPV. The English version of the questionnaire was prepared first and translated to the local language (Amharic) and back English to ensure its consistency. Data were collected using a structured and interviewer-administered questionnaire through face-to-face interviews. The questionnaire contains socio-demographic characteristics, obstetric and maternal health services-related characteristics, decision-making power, social support, and intimate partner violence-related questions. A total of 14 BSc and 4 MSc in Midwifery holders were involved in the data collection and supervision process, respectively. The one-day training was provided about the interview technique and information-handling techniques. The pretest was done on 5% (n = 42) of the calculated sample size outside of the study site. The language clarity and validity of the tool were checked and necessary revisions were made after the pretest. The supervisors checked for questionnaire completeness daily.
Data were checked, coded, and entered into EPI DATA version 4.6 and further cleaning and analysis were done using SPSS version 25. Binary logistic regression analysis was performed to identify candidate predictors. Predictors with a p-value of < 0.25 were included in the multivariable logistic regression analysis to address the possible effect of confounders. In the last model (multivariable logistic regression analysis,) a p-value of ≤ 0.05 with 95% CI for the AOR was used to decide the level of association. The variance inflation factor (VIF) was used to check the multicollinearity assumption and was acceptable with a value of < 10. The Hosmer Lemeshow goodness-of-fit was performed to check the model fit.
A total of 858 postpartum women were included in the analysis, a response rate of 98.4%. The mean age of the study participants was 29.53 years (±4.79SD) and about 43.2% of them were classified in the age group of 24–29 years old. More than two-fifths (43.2%) of the women had earned a diploma and above education and about 44.4% of women were housewives by occupation (Table 1).
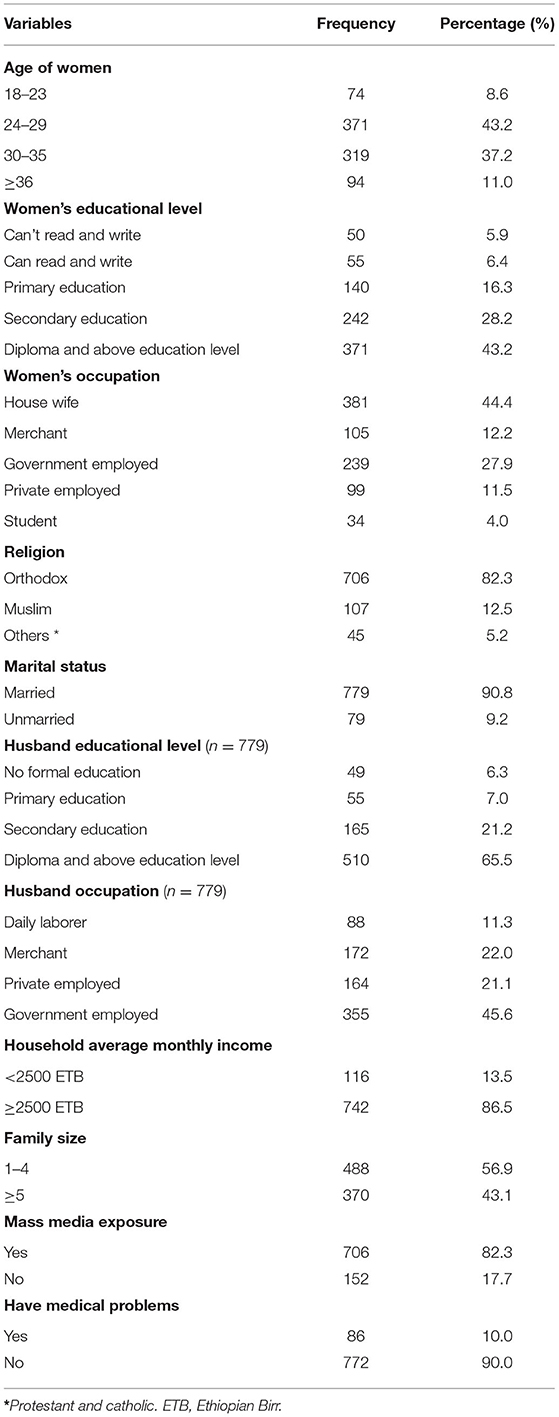
Table 1. Socio-demographic characteristics of the study participants in Gondar city, northwest Ethiopia, 2021 (n = 858).
Most (97.3%) of the study participants had ANC follow-up during their last pregnancy. More than four-fifths (86.8%) of the study participants had planned pregnancies. About 28.8% of the women had poor social support (Table 2).
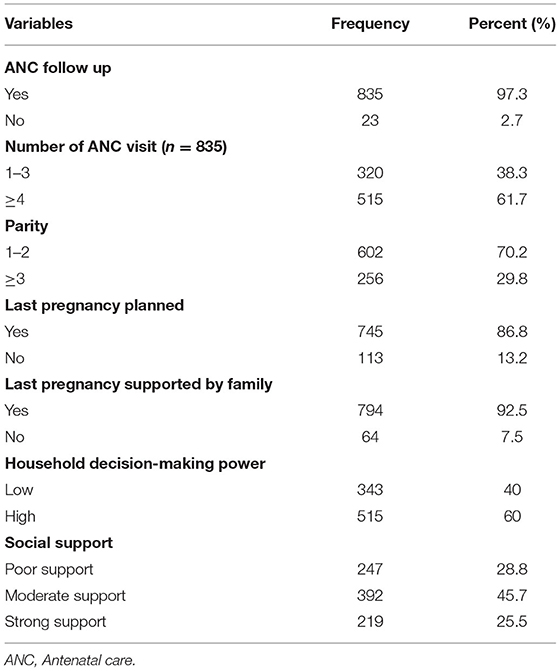
Table 2. Reproductive and maternity health service characteristics of the study participants in Gondar city, (n = 858).
In the present study, about 48.6% of the women indicated having experienced IPV during pregnancy (95% CI: 45.3, 51.7) (Figure 1). On bivariable analysis, age of women, women's education, women's occupation, husband education, husband occupation, household decision making power, social support, average monthly income, had ANC follow up, number of family and pregnancy supported family were significantly associated with intimate partner violence during pregnancy at p-value < 0.25. However, woman's education, woman's occupation, woman's decision-making power, woman's social support, family size, and pregnancy supported by families were the factors significantly associated with IPV in multivariable regression.
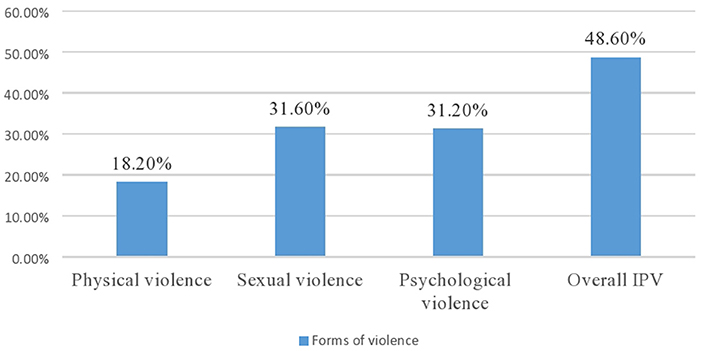
Figure 1. Forms of intimate partner violence during pregnancy in Gondar city, northwest Ethiopia, 2021.
Accordingly, women who were unable to read and write were 4.96 times more likely to report experiencing IPV than women who held a diploma and above education (AOR = 4.96; 95% CI: 2.15, 11.41). Likewise, privately -employed women were 1.78 times more likely to report experiencing IPV compared with government employed women (AOR = 1.78; 95% CI: 1.05, 3.02).
This study revealed that women who had a family size of ≥ 5 were 27% less likely to report experiencing IPV compared with those women who had a family size of 1–4 (AOR = 0.73; 95% CI: 0.54, 0.98). Similarly, women who had low decision-making power had 1.43 times higher odds of experiencing IPV compared with those women having higher decision-making power (AOR = 1.43; 95% CI: 1.06, 1.95). This study also found that the odds of experiencing IPV among women who had poor social support were two times higher (AOR = 1.99; 95% CI: 1.32, 3.02) than women who had strong social support. Moreover, women whose pregnancy was unsupported by their husband or family were 2.32 times more likely to report experiencing IPV during pregnancy as compared to women whose pregnancy was supported by their husband or family (AOR = 2.32; 95% CI: 1.26, 4.24) (Table 3).
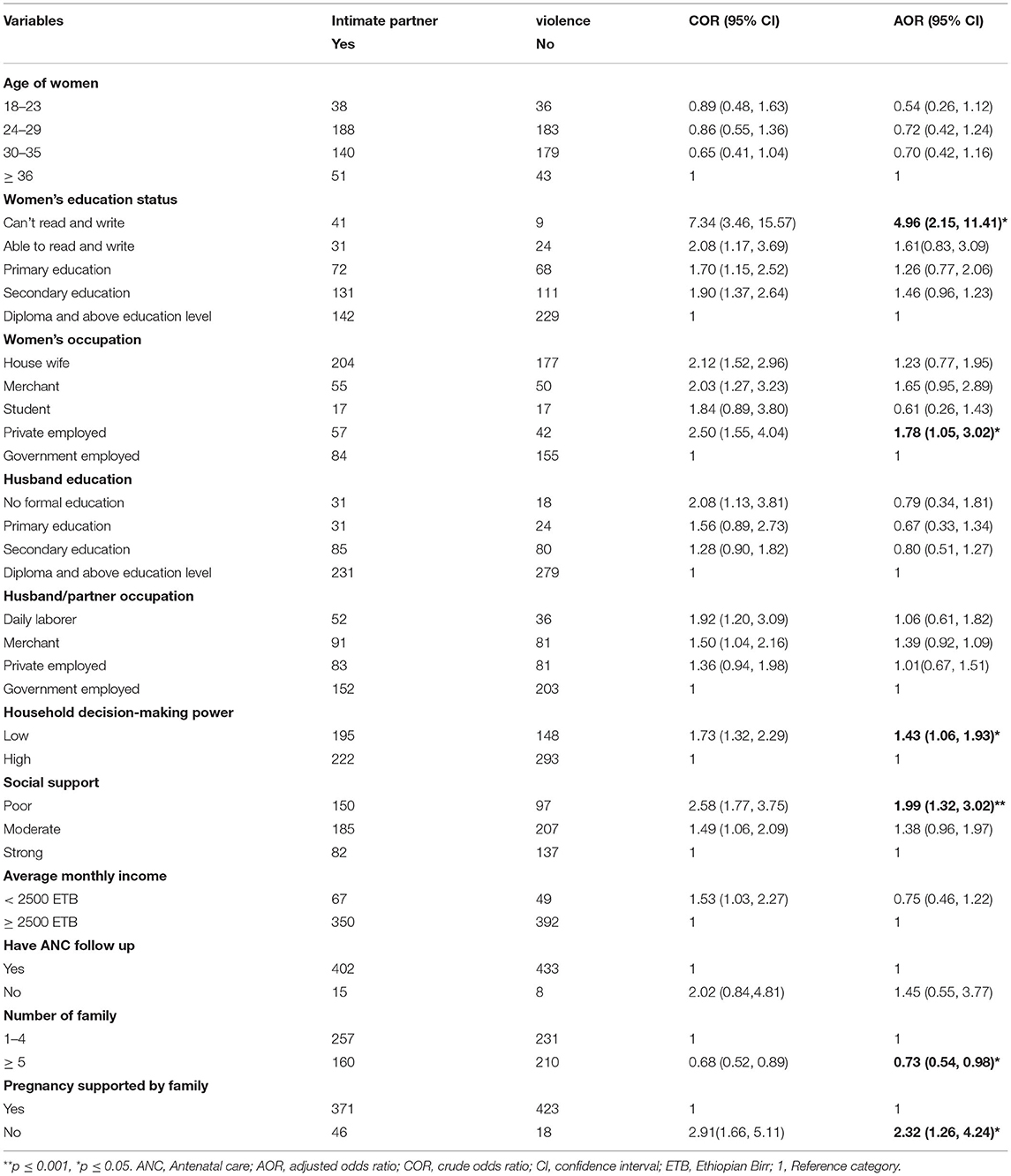
Table 3. Bivariable and multivariable logistic regression analysis of factors associated with intimate partner violence among pregnant women in Gondar city, northwest Ethiopia, 2021.
Intimate partner violence is a major public health concern that needs urgent policy action and multi-sectorial collaboration. Despite an endeavor made to overcome violence against women globally, it is still very much common in developing countries, including Ethiopia. One of the global goals set to be achieved by 2030 is empowering women and ensuring gender equality everywhere (26). Hence, this study focused on assessing the magnitude of IPV during pregnancy and associated factors in Gondar city, northwest Ethiopia.
In this study, about 48.6% of women reported having experienced IPV during pregnancy. This finding is higher than previous studies conducted in Uganda-40.6% (9), Nigeria-33% (32), and Vietnam-35.2% (33). The results of the current study show IPV in Gondar city to be higher than in studies conducted elsewhere in Ethiopia, including Debre markos town-41.1% (28), Shire Enda Selassie town-20.6% (5), and Western Ethiopia-44.5% (27). The possible explanation for the variation might be differences in the study population, time of data collection, and the instrument we used to measure the outcome variable. The study population in the aforementioned studies included women who came for antenatal care (ANC). According to scholars, IPV impacts the utilization of maternal health services, by women who have suffered from IPV. These women might be reluctant to visit the ANC clinic (34). Moreover, the above-mentioned studies included women all trimesters of the pregnancy and some women may experience violence at any time during pregnancy. In contrast, the current study included women after delivery which could be responsible for the higher magnitude of IPV. In addition, the current data were collected during the coronavirus disease 2019 (COVID-19) pandemic. According to empirical evidence, IPV has increased due to the lockdown (35).Another explanation for the high prevalence IPV-rate found in the current study is that IPV was measured using three forms of violence; sexual, physical, and psychological, instead off only physical IPV generally used in other studies (e.g., Shire Enda Selassie town).
There are also studies conducted in other African countries mentioning a higher IPV prevalence rate than found in our study. For instance, in Kenya-66.9% (36) and Gambia-67% (10). This variation could be due to the fact that women's health is getting global attention and violence against women is nowadays considered to be a violation of human rights. The other explanation for the disparity might be related to women's employment status; the majority (75%) of women from Kenya were unemployed suggesting that they could be financially dependent on their sexual partners/husbands. Evidence supports that being unable to secure financial needs and being jobless could increase the likelihood of one form of violence (37, 38). In this regard, concerned stakeholders and human rights commissions need to prepare an assessment instrument that will reach out to all women in the maternal continuum of care and the devastating nature of IPV should be advocated within the community.
This study points out that the odds of falling victim of IPV was 1.43 times higher among women with less decision-making power than among women with more decision-making power. This finding contradicts a study conducted in Sub-Saharan Africa, which reported that women who could make decisions were more likely to experience IPV (37). African culture, particularly Ethiopian culture, is gender stratified, in favor of men, and women are subordinated to men. However, in the present study, less autonomous women were more at risk of falling victims of IPV. This could be since most men in developing countries consider themselves as the main source of household income and they perceive they have every right to violet the women. Besides, less autonomous women are expected to be financially dependent on their partners. According to evidence, being economically dependent increases the odds of experiencing IPV. This finding is supported by a previous study, in which decisions made by the women alone or jointly with their partners had a positive impact on decreasing IPV (39).
The results of the present study also affirmed that social support during pregnancy was significantly associated with IPV. Accordingly, the odds of experiencing IPV were nearly 2 times higher among women who had poor social support as compared to those women who had strong social support. This finding is in agreement with a previous study done in Vietnam (33). According to scholars, social support helps women maintain positive self-esteem and a negative attitude toward IPV, thereby preparing them to solve the conflict of opinions meticulously with their sexual partners (40).
In the present study the odds of experiencing IPV among women who had unsupported pregnancies by families were 2.32 times higher compared with women who were pregnant with support of their families. This finding is consistent with a previous study conducted in Ethiopia (41). Unplanned and therefore unsupported pregnancies could push men to put the responsibility of pregnancy on women and to use violence. Evidence supported that unplanned and undesired pregnancies by partners are common reasons for committing violence against pregnant women (42). It should be noted, that no matter how the pregnancy happened, pregnant women must get respect and appropriate care to have an optimal outcome of the pregnancy and to ensure the wellbeing of the women. To reach this goal, adequate counseling should be offered to male partners on every occasion, with special focus on pregnancies that are unplanned and unsupported.
The present study revealed that the likelihood of experiencing IPV was nearly 5 times higher among women who were unable to read and write than those women attending diploma and above education. This finding is supported by a previous study conducted in Ethiopia where women who had no formal education were victims of IPV (5). This could be due to the reality that less-educated women might have limited access to any information related to their rights and women's empowerment. In addition, less educated women might be more adherent to the local cultures and may accept IPV as normal if it is committed by a formal sexual partner or husband (43).
The odds of experiencing IPV among women having a family size of ≥ 5 were 27% less likely compared with their counterparts. This could be due to the fact that women with a higher family size are expected to be older and therefore get more respect from their husbands and make shared decisions in every aspect of the household. Women with bigger families are expected to have strong social support and social networks, thereby maintaining smooth relationships with their sexual partners/husbands (44).
In the present study, women who were working in the private sector were 1.78 times more likely to experience IPV than those women who were government employees. In the private-sector employees are stimulated to focus on what makes the organization profitable. To do this, the staff can interact with a large number of people in order to attract customers; however, their sexual partners may interpret this in a negative way and this could turn into abusive behaviors.
The present study has limitations. Social desirability and recall biases might have been present. However, the study participants had been informed that their participation was crucial for the study, that the information was anonymous, and kept confidential for the study purpose only. Despite these limitations, the findings from study provide important insights for policy action related to violence against women.
The magnitude of IPV during pregnancy was high. Being unable to read and write, being a private worker, having low-decision-making power, having poor social support, unsupported pregnancy, and having a bigger family were the factors significantly associated with IPV. Concerned stakeholders need to pay special attention to ensuring women's empowerment and gender equality by establishing social support platforms, engaging women in decision-making matters, and capacitating women financially by arranging risk-free employment.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval for the study was obtained from the Institutional Review Board (IRB) of the University of Gondar (Reference No: V/P/RCS/05/2710/2021). The patients/participants provided their written informed consent to participate in this study.
AK conceived and designed the experiments. DG, NTs, MAk, WT, MAb, TA, NTi, HA, TH, AS, AT, AY, MM, GN, KW, and BT investigation, analyzed and interpreted the data, and wrote the article. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We appreciate and thank the University of Gondar for providing ethical clearance to carry out this study. We also would like to acknowledge the data collectors, supervisors, and study participants.
1. World Health Organization (WHO). Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. (2013). p. 1–60. Available online at: www.who.int
2. Devries KM, Mak JYT, García-Moreno C, Petzold M, Child JC, Falder G, et al. The global prevalence of intimate partner violence against women. Science. (2013) 340:1527–8. doi: 10.1126/science.1240937
3. Adhena G, Oljira L, Dessie Y, Hidru HD. Magnitude of intimate partner violence and associated factors among pregnant women in Ethiopia. Adv Public Health. (2020) 2020:1–9. doi: 10.1155/2020/1682847
4. Finnbogadóttir H, Dykes A-K, Wann-Hansson C. Struggling to survive for the sake of the unborn baby: a grounded theory model of exposure to intimate partner violence during pregnancy. BMC Preg Childbirth. (2014) 14:293. doi: 10.1186/1471-2393-14-293
5. Gebrezgi BH, Badi MB, Cherkose EA, Weldehaweria NB. Factors associated with intimate partner physical violence among women attending antenatal care in Shire Endaselassie town, Tigray, northern Ethiopia: a cross-sectional study, July 2015. Reprod Health. (2015) 14:1–10. doi: 10.1186/s12978-017-0337-y
6. WHO. Global status report on violence prevention 2014. (2014). Available online at: https://www.who.int/publications/i/item/9789241564793 (accessed January 9).
7. Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet. (2006) 368:1260–9. doi: 10.1016/S0140-6736(06)69523-8
8. WHO. (2005). WHO multi-country study on women's health and domestic violence against women : initial results on prevalence, health outcomes and women's responses. Available online at: https://apps.who.int/iris/handle/10665/43309 (accessed April 1).
9. Auma AG, Ayebare E. Intimate partner violence among pregnant teenagers in Lira district, northern Uganda. Afr J. Midwifery Women's Health. (2020) 14:1–11. doi: 10.12968/ajmw.2020.0011
10. Jatta JW, Id AB, Fawole OI, Ojengbede A. Intimate partner violence among pregnant women attending antenatal care services in the rural Gambia. PLoS ONE. (2021) 16:e0255723. doi: 10.1371/journal.pone.0255723
11. Alebel A, Kibret GD, Wagnew F, Tesema C, Ferede A, Petrucka P, et al. Intimate partner violence and associated factors among pregnant women in Ethiopia: a systematic review and meta-analysis. Reprod Health. (2018) 15:1–12. doi: 10.1186/s12978-018-0637-x
12. Bikinesi E. Prevalence of intimate partner violence and associated factors amongst women attending antenatal care at Outapi clinic, Namibia: A descriptive survey. Afr J Prim Health Care Family Med. (2017) 9:e1–6. doi: 10.4102/phcfm.v9i1.1512
13. Kaye DK, Mirembe FM, Bantebya G, Johansson A, Ekstrom AM. Domestic violence during pregnancy and risk of low birthweight and maternal complications: a prospective cohort study at Mulago Hospital, Uganda. Trop Med Int Health. (2006) 11:1576–84. doi: 10.1111/j.1365-3156.2006.01711.x
14. Bailey BA. Partner violence during pregnancy: Prevalence, effects, screening, and management. Int J Women's Health. (2010) 2:183–97. doi: 10.2147/IJWH.S8632
15. Alhusen JL, Ray E, Sharps P, Bullock L. Special feature intimate partner violence during pregnancy: maternal and neonatal outcomes. J Women's Health. (2015) 24:1–7. doi: 10.1089/jwh.2014.4872
16. Laelago T, Belachew T, Tamrat M. Effect of intimate partner violence on birth outcomes. Afr Health Sci. (2017) 17:681–689. doi: 10.4314/ahs.v17i3.10
17. Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS ONE. (2011) 6:e17591. doi: 10.1371/journal.pone.0017591
18. Renner LM. Intimate partner violence victimization and parenting stress: Assessing the mediating role of depressive symptoms. Violence Against Women. (2009) 15:1380–401. doi: 10.1177/1077801209346712
19. Demelash H, Nigatu D, Gashaw K. A case-control study on intimate partner violence during pregnancy and low birth weight, southeast Ethiopia. Obstet Gynecol Int. (2015) 2015:1–6. doi: 10.1155/2015/394875
20. Sigalla GN, Mushi D, Meyrowitsch DW, Manongi R, Rogathi JJ, Gammeltoft T, et al. Intimate partner violence during pregnancy and its association with preterm birth and low birth weight in Tanzania: A prospective cohort study. PLoS ONE. (2017) 12:e0172540. doi: 10.1371/journal.pone.0172540
21. Ethiopia Demographic and Health Survey (EDHS). Ethiopia Demographic and Health Survey. (2016). p. 1–551.
22. Abeya SG, Afework MF, Yalew AW. Intimate partner violence against women in western Ethiopia: prevalence, patterns, and associated factors. BMC Health Serv Res. (2011) 11:913. doi: 10.1186/1471-2458-11-913
23. Makayoto LA, Omolo J, Kamweya AM, Harder VS, Mutai J. Prevalence and associated factors of intimate partner violence among pregnant women attending Kisumu District Hospital, Kenya. Maternal Child Health J. (2013) 17:441–447. doi: 10.1007/s10995-012-1015-x
24. Dhungel S, Dhungel P, Dhital SR, Stock C. Is economic dependence on the husband a risk factor for intimate partner violence against female factory workers in Nepal? BMC Women's Health. (2017) 17:82. doi: 10.1186/s12905-017-0441-8
25. Matjasko JL, Niolon PH, Valle LA. The role of economic factors and economic support in preventing and escaping from intimate partner violence. J Policy Analy Manage. (2013) 32:122. doi: 10.1002/pam.21666
26. UNDP. (2016). United Nations Development Program. The Global Goals and the 2030 Agenda for Sustainable Development - Government.se Available online at: https://www.government.se/government-policy/the-global-goals-and-the-2030-Agenda-for-sustainable-development/ (accessed January 1).
27. Abebe Abate B, Admassu Wossen B, Tilahun Degfie T. Determinants of intimate partner violence during pregnancy among married women in Abay Chomen district, Western Ethiopia: a community based cross sectional study. BMC Women's Health. (2016) 16:1–8. doi: 10.1186/s12905-016-0294-6
28. Azene ZN, Yeshita HY, Mekonnen FA. Intimate partner violence and associated factors among pregnant women attending antenatal care service in Debre Markos town health facilities, Northwest Ethiopia. PLoS ONE. (2019) 14:1–17. doi: 10.1371/journal.pone.0218722
29. Nigatu D, Gebremariam A, Abera M, Setegn T, Deribe K. Factors associated with women ' s autonomy regarding maternal and child health care utilization in Bale Zone : a community based cross-sectional study. BMC Women's Health. (2014) 14:1–9. doi: 10.1186/1472-6874-14-79
30. Kebede AA, Cherkos EA, Taye EB, Eriku GA, Taye BT, Chanie WF. Married women's decision-making autonomy in the household and maternal and neonatal healthcare utilization and associated factors in Debretabor, northwest Ethiopia. PLoS ONE. (2021) 16:e0255021. doi: 10.1371/journal.pone.0255021
31. Abiola T, Udofia O, Psychiatry MZ. Psychometric properties of the 3-item oslo social support scale among clinical students of Bayero University Kano, Nigeria. MjpsychiatryOrg. (2013) 22:1–13.
32. Oche OM, Adamu H, Abubakar A, Aliyu MS. Intimate partner violence in pregnancy : knowledge and experiences of pregnant women and controlling behavior of male partners in Sokoto, Northwest Nigeria. Int J Reprod Med. (2020) 2020:1–10. doi: 10.1155/2020/7626741
33. Nguyen TH, Ngo TV, Nguyen VD, Nguyen HD, Nguyen HT, Gammeltoft T, et al. Intimate partner violence during pregnancy in Vietnam : prevalence, risk factors and the role of social support. Global Health Action. (2019) 11:1638052. doi: 10.1080/16549716.2019.1638052
34. Musa A, Chojenta C, Geleto A, Loxton D. The associations between intimate partner violence and maternal health care service utilization : a systematic review and meta- analysis. BMC Women's Health. (2019). 19:1–14. doi: 10.1186/s12905-019-0735-0
35. Tadesse AW, Tarekegn SM, Wagaw GB, Muluneh MD, Kassa AM. Prevalence and associated factors of intimate partner violence among married women during covid-19 pandemic restrictions : a community-based study. J Interpers Violence. (2020) 37:NP8632–50. doi: 10.1177/0886260520976222
36. Owaka IO, Nyanchoka MK, Atieli HE. Intimate partner violence in pregnancy among antenatal attendees at health facilities in West Pokot county, Kenya. Pan African Med J. (2017) 28. doi: 10.11604/pamj.2017.28.229.8840
37. Ahinkorah BO, Dickson KS, Seidu AA. Women decision-making capacity and intimate partner violence among women in sub-Saharan Africa. Arch Public Health. (2018) 76:1–10. doi: 10.1186/s13690-018-0253-9
38. Fekadu E, Yigzaw G, Gelaye KA, Ayele TA, Minwuye T. Prevalence of domestic violence and associated factors among pregnant women attending antenatal care service at University of Gondar Referral Hospital, Northwest Ethiopia. BMC Women's Health. (2018) 18:4–11. doi: 10.1186/s12905-018-0632-y
39. Zegenhagen S, Ranganathan M, Maria A. Household decision-making and its association with intimate partner violence : Examining differences in men's and women's perceptions in Uganda. SSM - Population Health. (2019) 8:100442. doi: 10.1016/j.ssmph.2019.100442
40. Trinh OT, Oh J, Choi S, To KG, Do DV. Changes and socioeconomic factors associated with attitudes towards domestic violence among Vietnamese women aged 15–49: findings from the multiple indicator cluster surveys, 2006-2011. Glob Health Action. (2016) 9:29577. doi: 10.3402/gha.v9.29577
41. Tiruye TY, Harris ML, Chojenta C, Holliday E, Loxton D. Determinants of intimate partner violence against women in Ethiopia: A multi-level analysis. PLoS ONE. (2020) 15:1–18. doi: 10.1371/journal.pone.0232217
42. Town H, Zone H, Et S. Prevalence and associated factors of intimate partner violence during pregnancy among recently delivered women in public health facilities of hossana town, hadiya zone, Southern Ethiopia. Open Access Library J Prevalence. (2014) 01:1–9. doi: 10.4236/oalib.1100997
43. Iliyasu Z, Abubakar IS, Galadanci HS, Hayatu Z, Aliyu MH. Prevalence and risk factors for domestic violence among pregnant women in northern Nigeria. J Interpers Violence. (2013) 28:868–83. doi: 10.1177/0886260512455872
Keywords: Ethiopia, intimate partner, violence, social support, pregnancy
Citation: Kebede AA, Aklil MB, Gessesse DN, Tsega NT, Temesgan WZ, Abegaz MY, Anteneh TA, Tibebu NS, Alemu HN, Haile TT, Seyoum AT, Tiguh AE, Yismaw AE, Nenko G, Wondie KY, Taye BT and Mihret MS (2022) Nearly Half of Women Have Experienced Intimate Partner Violence During Pregnancy in Northwest Ethiopia, 2021; The Role of Social Support and Decision-Making Power. Front. Public Health 10:904792. doi: 10.3389/fpubh.2022.904792
Received: 25 March 2022; Accepted: 31 May 2022;
Published: 30 June 2022.
Edited by:
Russell Kabir, Anglia Ruskin University, United KingdomReviewed by:
Joan E. Van Horn, Joan van Horn, NetherlandsCopyright © 2022 Kebede, Aklil, Gessesse, Tsega, Temesgan, Abegaz, Anteneh, Tibebu, Alemu, Haile, Seyoum, Tiguh, Yismaw, Nenko, Wondie, Taye and Mihret. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mastewal Belayneh Aklil, bWFzdGV3YWxiZWxheW5laEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.