
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health, 17 October 2022
Sec. Aging and Public Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.902599
This article is part of the Research TopicConsequences of Population Aging for Public Health in Different Areas of LifeView all 11 articles
Aim: This study aims to clarify the risk factors for falls to prevent severe consequences in older adults.
Methods: We searched the PubMed, Web of Science, Embase, and Google Scholar databases using the terms “risk factors” OR “predicting factors” OR “predictor” AND “fall” OR “drop” to identify all relevant studies and compare their results. The study participants were divided into two groups, the “fall group” and the “control group”, and differences in demographic characteristics, lifestyles, and comorbidities were compared.
Results: We included 34 articles in the analysis and analyzed 22 factors. Older age, lower education level, polypharmacy, malnutrition, living alone, living in an urban area, smoking, and alcohol consumption increased the risk of falls in the aging population. Additionally, comorbidities such as cardiac disease, hypertension, diabetes, stroke, frailty, previous history of falls, depression, Parkinson's disease, and pain increased the risk of falls.
Conclusion: Demographic characteristics, comorbidities, and lifestyle factors can influence the risk of falls and should be taken into consideration.
By 2050, people older than 65 years are estimated to account for 16% of the population (1). Falls are a major public health problem, as approximately 28–35% of individuals aged ≥ 65 years experience falls each year. As the aging population increases, more individuals will be at risk of falling (2).Among older people, physical falls are events that adversely affect health and lead to disability and mortality (3, 4). Moreover, fall-associated economic burdens are substantial and continue to increase worldwide (4, 5). Even non-injury falls are associated with negative impacts, such as anxiety, depression, and decreased mobility, which greatly affect the quality of life (QOL) and aging trajectory. The most harmful consequences of injurious falls are hip fracture and brain damage (4). Research on the risk of falling has become increasingly important to maintain the health of older individuals (2).Early screening for the risk of fall that takes risk factors into account is needed. Many retrospective, cross-sectional, and longitudinal studies have examined fall prevalence, fall-related consequences, and risk factors for falls in older individuals. However, even though some reviews have addressed these topics (6, 7), a high-quality systematic review has yet to be conducted. Therefore, in this study, we aimed to investigate the association between lifestyle factors and fall risk in aging adults to promote the development of effective fall prevention strategies.
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines in this systematic review. As this study was a review, no ethical approval was necessary.
We hypothesized that demographic characteristics, lifestyle factors, and comorbidities would influence the risk of falls in the aging population. We chose these risk factors on the basis of records in the literature. After searching and carefully reading the literature, we found that the above factors had the most related studies and received the most attention. Therefore, we compared these factors between fall and non-fall groups. We searched for potentially relevant articles published in English before January 2022 during the initial search process. The terms searched in the PubMed, Web of Science, Embase, and Google Scholar databases were as follows: “risk factors” OR “predicting factors” OR “predictor” AND “fall” OR “drop”. Since Boolean operators do not work on Google Scholar, we used search terms like “risk factors for fall” and “predicting factors for fall” on Google Scholar. Two authors independently screened all the abstracts and citations of all studies identified with the search strategy to determine eligible studies. Data were independently extracted by two of the authors using a standardized Excel file. Studies were considered eligible if they included two groups and aging individuals (≥65 years old) with or without falls, and presented data on the baseline lifestyle characteristics and comorbidities of the participants. The exclusion criteria were as follows: duplicate publications, reviews, studies on unrelated topics, studies with different variables, and studies with different group criteria. The search process consisted of 2 steps, the initial search with short keywords and then detailed search with detailed search strategy (present in Supplementary File 1). The description of the detailed search strategy for each part of the PICO research question is provided in Supplementary File 1, which is amended for other databases using database-specific subject headings, where available, and keywords in both titles and abstracts. The extracted data included baseline characteristics, lifestyle habits, comorbidities, and occurrence of falls. All the included data were subsequently entered in RevMan 5.1.4.
In our meta-analysis, we compared 22 factors between the two groups (the fall group and the control [no falls] group). The factors included age, body mass index (BMI), education level, polypharmacy, sex, relationship status (living alone), residential location (rural), (mal)nutrition, smoking status, alcohol consumption, and comorbidities including cardiac disease, hypertension, diabetes, stroke, depression, Parkinson's disease, pain, vision impairment, frailty, previous history of falls, and cognitive impairment.
The quality of the included studies was assessed by two authors according to the Cochrane Collaboration Reviewer's Handbook and the Quality of Reporting of Meta-analysis guidelines (40, 41).
The data were analyzed using RevMan 5.1.4. Continuous outcomes are presented as weighted mean differences (MDs) with 95% confidence intervals (CIs). Dichotomous data are presented as relative risks (RRs) with 95% CIs. A meta-analysis was performed using fixed-effect or random-effects models as appropriate. Specifically, the fixed-effects models were used when no significant heterogeneity was present, and the random-effects models were used when heterogeneity was present. Statistical heterogeneity among the trials was evaluated by the I2 test, with significance set at P < 0.05.
A total of 14,144 reports were initially identified from the databases. After screening for duplicate publications, reviews, and irrelevant records based on the titles and abstracts, 13,139 reports were excluded from the study. After screening the full texts, 422 articles with different baseline data, 432 articles with different results criteria, and 117 articles with different group classifications were excluded. Thus, we eventually included 34 articles in the final analysis (8–32, 34–39, 42–44). The conditions of these studies and the clinical details of the participants are presented in Table 1. A flow chart of the literature search is shown in Figure 1.
First, we compared aging adults in terms of age, BMI, education level, polypharmacy, malnutrition, sex (female), living alone, living in a rural area, smoking status, and alcohol consumption (Figures 2A–L). Older age (MD 1.87; 95% CI 1.14–2.6; p < 0.00001, Figure 2A), number of drugs used (MD.36; 95% CI.19–0.52; p < 0.0001, Figure 2E), and polypharmacy (RR 1.06; 95% CI 1.03–1.09; p = 0.0002, Figure 2F) were associated with increased incidence of falls. Malnutrition (RR 1.4; 95% CI 1.19–1.64; p < 0.0001, Figure 2G), living alone (RR 1.39; 95% CI 1.29–1.5; p < 0.00001, Figure 2I), living in a rural area (RR 1.09; 95% CI 1.02–1.16; p = 0.006, Figure 2J), smoking (RR 1.17; 95% CI 1.05–1.3; p = 0.004, Figure 2K), and alcohol consumption (RR 1.18; 95% CI 1.09–1.28; p < 0.001, Figure 2L) were risk factors for falls. Education level (MD −0.29; 95% CI −0.73–0.16; p = 0.21, Figure 2C) had no impact on risk of falls, but completion of the mandatory level of education (RR 0.93; 95% CI 0.89–0.97; p = 0.006, Figure 2D) decreased the risk of falls. BMI (MD −0.22; 95% CI −0.48–0.05; p = 0.11, Figure 2B) and sex (RR 1.02; 95% CI 1–1.04; p = 0.13, Figure 2H) did not affect risk of falls.
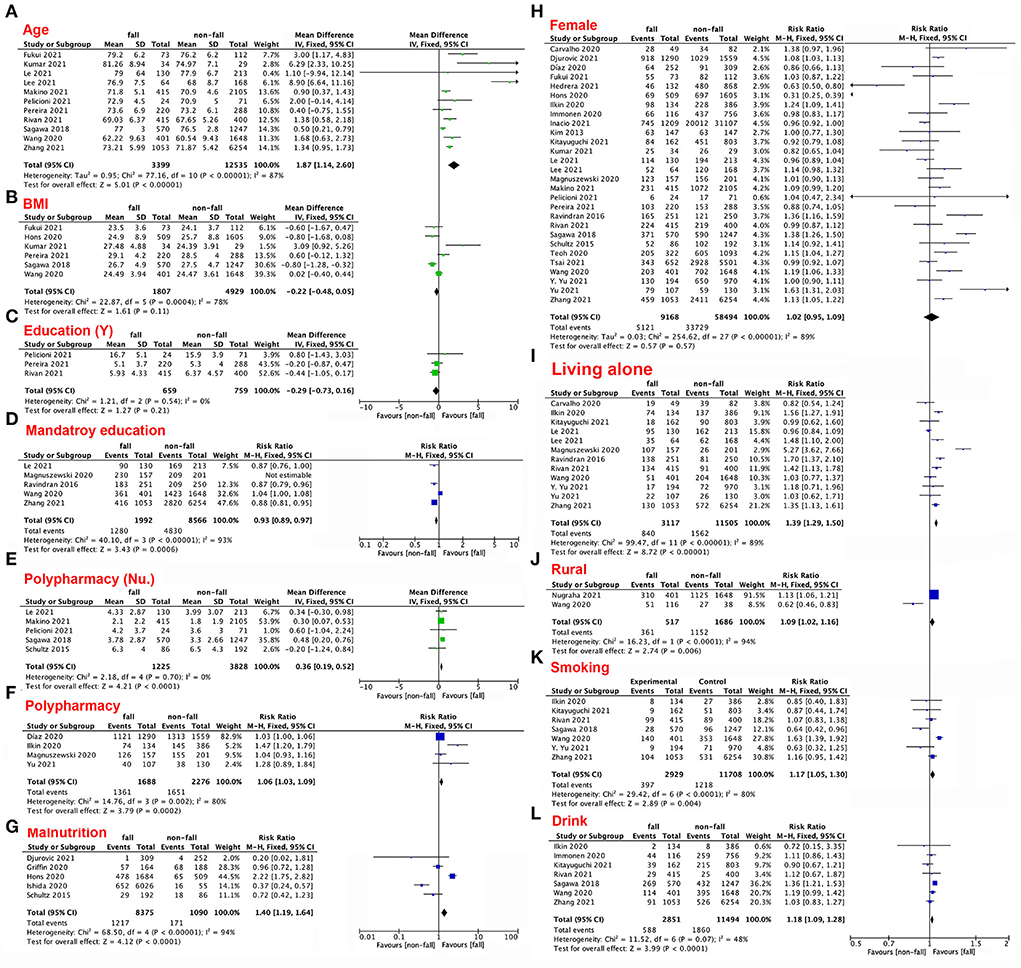
Figure 2. (A–L) Forest plots of the impacts of patient characteristics and lifestyle factors on the risk of falls.
Eleven comorbidities were compared between people with and without falls: cardiac disease, hypertension, diabetes, stroke, vision dysfunction, frailty, fall history, cognitive impairment, depression, Parkinson's disease, and pain (Figures 3A–L). Even though these comorbidities may alter the rate of frailty among elderly individuals (RR 1.1; 95% CI 1.05–1.15; p < 0.0001, Figure 3A), not all of the comorbidities mentioned above necessarily influence falls. For instance, diabetes (RR 1.08; 95% CI 0.87–1.34; p = 0.49, Figure 3D), stroke (RR 1.55; 95% CI 0.72–3.35; p = 0.26, Figure 3E), vision dysfunction (RR 1.24; 95% CI 0.91–1.69; p = 0.17, Figure 3F), and cognitive impairment (RR 1.11; 95% CI 0.88–1.39; p =0.37, Figure 3I) did not significantly differ between the two groups. In contrast, heart disease (RR 1.14; 95% CI 1.09–1.19; p < 0.00001, Figure 3B), hypertension (RR 1.08; 95% CI 1.03–1.12; p = 0.0004, Figure 3C, frailty (RR 1.35; 95% CI 1.25–1.45; p < 0.00001, Figure 3G), fall history (RR 1.53; 95% CI 1.44–1.62; p < 0.00001, Figure 3H), depression (RR 4.34; 95% CI 4.02–4.68; p < 0.00001, Figure 3K), Parkinson's disease (RR 3.05; 95% CI 1.84–5.05; p < 0.0001, Figure 3K), and pain (RR 1.22; 95% CI 1.11–1.34; p < 0.0001, Figure 3L) were associated with increased risk of falls among the aging population.
In older adults, falls impose major health, economic, and societal burdens (16). Falls are the leading cause of injury in the elderly population (36). A serious fall could result in decreased independence and reduced QOL (36). Hip fracture, in particular, is a serious and devastating consequence of falling in older individuals (36). Moreover, Makino et al. reported that fall history is the most influential predictor of future falls (25). According to recent research, fall history increases the current risk of falls. Some research has also proposed that fear of falling is significantly associated with falls. Usually, fear of falling arises from a fall history (45). Patil R et al. suggested that fear of falling may increase even after a non-injurious fall. Subsequently, older adults may enter into a negative cycle in which they reduce their activity, leading to reduction in functionality (45). To avoid this negative cycle, we recommend early prevention of falls in elderly adults. Fear of falling was also independently associated with presence of knee pain, with a significant relationship observed between fear of falling and moderate to severe knee pain but not mild knee pain (14). Pain is a frequently mentioned factor, but only a few studies have prospectively collected data on fall occurrence in relation to knee pain or the lack of association between knee pain and fall occurrence during long-term follow-up. Furthermore, fear of falling may exacerbate depression. Our present results demonstrated that depression can also impact the risk of falls. As most falls result from loss of balance while walking and poor balance is the leading risk factor for falls, people tend to focus on the importance of mobility in the risk of falls (46). This explains the lack of sufficient predictive factors in older adults at risk of one or more falls. Additionally, social factors can increase the psychological burden on elderly individuals and reduce self-care capability, a factor with strong influences (47) on the risk of falls as well as the incidence rates of many diseases. Thus, the identification of risk factors for falls will provide important guidance for the care of elderly individuals.
Older age, polypharmacy, malnutrition, frailty, smoking, and alcohol consumption significantly increased the risk of falls; these factors also reflect decline in physical condition. Moreover, chronic illnesses are very common in older adults, and cardiac disease, hypertension, diabetes, stroke, and Parkinson's disease are associated with falls. Older adults residing in urban areas had a higher risk of falling than those residing in rural areas (27). This difference may be explained by traffic, which can impede medical treatment. Residency in suburban areas has certain advantages; for instance, it is easier to engage in physical exercises, such as walking, in suburban and rural areas than in urban areas. Physical exercise helps to reduce the risk of falls in adults and improves lower limb strength in older people (27, 47). Moreover, living in a rural area is associated with less pollution exposure; this factor is particularly important in developing countries because pollution may cause comorbidities. However, only a few articles have focused on this topic. We plan to explore this topic further in the future once a larger number of relevant reports have been published. Sex has been identified as a risk factor for falls among older adults (37), but in our study, women did not have a higher risk of falling than men. While women experience a higher rate of frailty than men (37), men are more likely to exhibit harmful lifestyle habits, such as smoking and consuming alcohol; therefore, sex differences in the risk of falling merit further study. Another risk factor in our study is living alone, which increases the risk of depressive symptoms and the impacts of falls.
A major strength of this study is that we analyzed data from several large-scale, well-characterized cohorts and systematically summarized the risk factors for falls in the elderly population. These findings can inform healthcare in the elderly population. Biswas et al. explored the risk factors for falls among older adults in India (6); however, their study focused on only the Indian population and thus exhibited geographic and ethnic limitations. Xie et al. examined risk factors for the development of fear of falling, but fear of falling was only one of the risk factors for falls; we suggest that it is more meaningful to identify the risk factors for falls. Our meta-analysis also has some limitations. For example, we did not categorize the participants according to whether they lived in the community or in nursing homes, which is a major factor associated with the risk of falls.
We demonstrated that (1) older age, polypharmacy, malnutrition, single status, living in a rural area, smoking, and alcohol consumption significantly increased the risk of falls in elderly adults. In contrast, higher education level was protective against falls. Additionally, we found that (2) individuals with cardiac disease, hypertension, frailty, previous history of falls, depression, Parkinson's disease, and pain had a higher risk of falls than individuals without such comorbidities.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Data acquisition and drafting of the manuscript: QX, XO, and JL. Conception and design of the study: JL. Analysis and/or interpretation of data: QX and XO. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.902599/full#supplementary-material
1. United Nations, Desa, Population Division, World Population Prospects 2019: Highlights. Available online at: http://www.population.un.org/wpp/Publications/Files/wpp2019_highlights.pdf (accessed April 7, 2020).
2. Organization WH. WHO Global Report on Falls Prevention in Older Age. Available online at: https://www.who.int/publications-detail-redirect/9789241563536 (accessed September 26, 2021).
3. Blain H, Dargent-Molina P, Martin FC, Rosendahl E, van der Velde N, Bousquet J, et al. European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO), Osteoporosis Research and Information Group (GRIO), and International osteoporosis Foundation (IOF), A comprehensive fracture prevention strategy in older adults: The European Union Geriatric Medicine Society (EUGMS) Statement. J Nutr Health Aging. (2016) (6):647–52. doi: 10.1007/s12603-016-0741-y
4. Gill TM, Murphy TE, Gahbauer EA, Allore HG. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol. (2013) 178:418–25. doi: 10.1093/aje/kws554
5. Spaniolas K, Cheng JD, Gestring ML, Sangosanya A, Stassen NA, Bankey PE. Ground level falls are associated with significant mortality in elderly patients. J Trauma. (2010) 69:821–5. doi: 10.1097/TA.0b013e3181efc6c6
6. Biswas I, Adebusoye B, Chattopadhyay K. Risk factors for falls among older adults in India: A systematic review and meta-analysis. Health Sci Rep. (2022) 5:e637. doi: 10.1002/hsr2.637
7. Xie Q, Pei J, Gou L, Zhang Y, Zhong J, Su Y, et al. Risk factors for fear of falling in stroke patients: a systematic review and meta-analysis. BMJ Open. (2022) 12:e056340. doi: 10.1136/bmjopen-2021-056340
8. Díaz LB, Casuso-Holgado MJ, Labajos-Manzanares MT, Barón-López FJ, Pinero-Pinto E, Romero-Galisteo RP, et al. Analysis of fall risk factors in an aging population living in long-term care institutions in SPAIN: A retrospective cohort study. Int J Environ Res Public Health. (2020) 17:7234. doi: 10.3390/ijerph17197234
9. Dixe MDA, Madeira C, Alves S, Henriques MA, Baixinho CL. Gait Ability and Muscle Strength in Institutionalized Older Persons with and without Cognitive Decline and Association with Falls. Int J Environ Res Public Health. (2021) 18:11543. doi: 10.3390/ijerph182111543
10. Djurovic O, Mihaljevic O, Radovanovic S, Kostic S, Vukicevic M, Brkic BG, et al. Risk factors related to falling in patients after stroke. Iran J Public Health. (2021) 50:1832–41. doi: 10.18502/ijph.v50i9.7056
11. Fukui K, Maeda N, Komiya M, Sasadai J, Tashiro T, Yoshimi M, et al. The relationship between modified short physical performance battery and falls: A cross-sectional study of older outpatients. Geriatrics (Basel). (2021) 6:106. doi: 10.3390/geriatrics6040106
12. Griffin A, O'Neill A, O'Connor M, Ryan D, Tierney A, Galvin R. The prevalence of malnutrition and impact on patient outcomes among older adults presenting at an Irish emergency department: a secondary analysis of the OPTI-MEND trial. BMC Geriatr. (2020) 20:455. doi: 10.1186/s12877-020-01852-w
13. Lackoff AS, Hickling D, Collins PF, Stevenson KJ, Nowicki TA, Bell JJ. The association of malnutrition with falls and harm from falls in hospital inpatients: Findings from a 5-year observational study. J Clin Nurs. (2020) 29:429–36. doi: 10.1111/jocn.15098
14. Ilhan B, Bahat G, Erdogan T, Kiliç C, Karan MA. Chronic pain: prevalent and independently associated with frailty and female gender in geriatric outpatients. Eur Geriatr Med. (2019) 10:931–7. doi: 10.1007/s41999-019-00235-8
15. Naharci MI, Tasci I. Frailty status and increased risk for falls: The role of anticholinergic burden. Arch Gerontol Geriatr. (2020) 90:104136. doi: 10.1016/j.archger.2020.104136
16. Immonen M, Haapea M, Similä H, Enwald H, Keränen N, Kangas M, et al. Association between chronic diseases and falls among a sample of older people in Finland. BMC Geriatr. (2020) 20:225. doi: 10.1186/s12877-020-01621-9
17. Inacio MC, Moldovan M, Whitehead C, Sluggett JK, Crotty M, Corlis M, et al. The risk of fall-related hospitalisations at entry into permanent residential aged care. BMC Geriatr. (2021) 21:686. doi: 10.1186/s12877-021-02640-w
18. Ishida Y, Maeda K, Nonogaki T, Shimizu A, Yamanaka Y, Matsuyama R, et al. Malnutrition at admission predicts in-hospital falls in hospitalized older adults. Nutrients. (2020) 12:541. doi: 10.3390/nu12020541
19. Kim YS, Smi CK. Fall risk factors and fall risk assessment of inpatients. Korean J Adult Nurs. (2013) 25:74–82. doi: 10.7475/kjan.2013.25.1.74
20. Kitayuguchi J, Abe T, Okuyama K, Gomi T, Okada S, Shiwaku K, et al. Association between a hilly neighborhood environment and falls among rural older adults: a crosssectional study. J Rural Med. (2021) 16:214–21. doi: 10.2185/jrm.2021-028
21. Pradeep Kumar D, Wendel C, Mohler J, Laksari K, Toosizadeh N. Between-day repeatability of sensor-based in-home gait assessment among older adults: assessing the effect of frailty. Aging Clin Exp Res. (2021) 33:1529–37. doi: 10.1007/s40520-020-01686-x
22. Ie K, Chou E, Boyce RD, Albert SM. Fall risk-increasing drugs, polypharmacy, and falls among low-income community-dwelling older adults. Innov Aging. (2021) 5:igab001. doi: 10.1093/geroni/igab001
23. Lee YY, Chen CL, Lee IC, Lee IC, Chen NC. History of falls, dementia, lower education levels, mobility limitations, and aging are risk factors for falls among the community-dwelling elderly: a cohort study. Int J Environ Res Public Health. (2021) 18:9356. doi: 10.3390/ijerph18179356
24. Magnuszewski L, Swietek M, Kasiukiewicz A, Kuprjanowicz B, Baczek J, Beata Wojszel Z. Health, functional and nutritional determinants of falls experienced in the previous year-a cross-sectional study in a geriatric ward. Int J Environ Res Public Health. (2020) 17:4768. doi: 10.3390/ijerph17134768
25. Makino K, Lee S, Bae S, Chiba I, Harada K, Katayama O, et al. Simplified decision-tree algorithm to predict falls for community-dwelling older adults. J Clin Med. (2021) 10:5184. doi: 10.3390/jcm10215184
26. Mat S, Kamaruzzaman SB, Chin AV, Tan MP. Impact of knee pain on fear of falling, changes in instrumental activities of daily living, and falls among malaysians age 55 years and above. Front Public Health. (2020) 8:571196. doi: 10.3389/fpubh.2020.571196
27. Nugraha S, Prasetyo S, Susilowati IH, Rahardjo TBW. Urban-rural dimension of falls and associated risk factors among community-dwelling older adults in west java, Indonesia. J Aging Res. (2021) 2021:8638170. doi: 10.21203/rs.3.rs-542482/v1
28. Pelicioni PHS, Lord SR, Sturnieks DL, Halmy B, Menant JC. Cognitive and motor cortical activity during cognitively demanding stepping tasks in older people at low and high risk of falling. Front Med. (2021) 8:554231. doi: 10.3389/fmed.2021.554231
29. Pereira C, Bravo J, Reis G, Mendes F. Aging safely in Alentejo - understanding for action - preventing falls and violence against older people: study rationale, aims, design, and preliminary results. BMC Public Health. (2021) 21:861. doi: 10.1186/s12889-021-10807-8
30. Ravindran RM, Kutty VR. Risk factors for fall-related injuries leading to hospitalization among community-dwelling older persons: a hospital-based case-control study in Thiruvananthapuram, Kerala, India. Asia Pac J Public Health. (2016) 28:70S−6S. doi: 10.1177/1010539515611229
31. Rivan NFM, Singh DKA, Shahar S, Wen GJ, Rajab NF, Din NC, et al. Cognitive frailty is a robust predictor of falls, injuries, and disability among community-dwelling older adults. BMC Geriatr. (2021) 21:593. doi: 10.1186/s12877-021-02525-y
32. Sagawa N, Marcum ZA, Boudreau RM, Hanlon JT, Albert SM, O'Hare C, et al. Low blood pressure levels for fall injuries in older adults: the health, aging and body composition study. Eur J Ageing. (2018) 15:321–30. doi: 10.1007/s10433-017-0449-9
33. Schultz M, Rosted E, Sanders S. Frailty is associated with a history with more falls in elderly hospitalised patients. Dan Med J. (2015) 62:A5058.
34. Severo IM, Kuchenbecker RS, Vieira DFVB, Lucena AF, Almeida MA. Risk factors for fall occurrence in hospitalized adult patients: a case-control study. Rev Lat Am Enfermagem. (2018) 26:e3016. doi: 10.1590/1518-8345.2460.3016
35. Teoh RJJ, Mat S, Khor HM, Kamaruzzaman SB, Tan MP. Falls, frailty, and metabolic syndrome in urban dwellers aged 55 years and over in the Malaysian elders longitudinal research (MELoR) study - a cross-sectional Study. Postgrad Med. (2021) 133:351–6. doi: 10.1080/00325481.2020.1842026
36. Tsai CY, Lin ES Li YT, Tung TH, Chen WC. The relationship between storey of buildings and fall risk. Front Public Health. (2021) 9:665985. doi: 10.3389/fpubh.2021.665985
37. Wang X, Chen Z, Li Z, Chen B, Qi Y, Li G, et al. Association between frailty and risk of fall among diabetic patients. Endocr Connect. (2020) 9:1057–64. doi: 10.1530/EC-20-0405
38. Yu WY, Hwang HF, Chen CY, Lin MR. Situational risk factors for fall-related vertebral fractures in older men and women. Osteoporos Int. (2021) 32:1061–70. doi: 10.1007/s00198-020-05799-x
39. Zhang XM, Yuan L, Guo N, Bo HX, Jiao J, Wu XJ, et al. Cognitive frailty and falls in a national cohort of older chinese inpatients. J Nutr Health Aging. (2021) 25:993–8. doi: 10.1007/s12603-021-1670-y
40. Julian PT. Higgins and Sally Green, Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.4 The Cochrane Collaboration. Available online at: https://www.cochranehandbook.org/ (2011).
41. Moher D, Liberati A, Tetzlaff J, Altman DG Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. (2010) 8:658. doi: 10.1016/j.ijsu.2010.02.007
42. Carvalho TC, Dini AP. Risk of falls in people with chronic kidney disease and related factors. Rev Lat Am Enfermagem. (2020) 28:e3289. doi: 10.1590/1518-8345.3911.3289
43. Friedman DS, West SK, Gitlin LN, Ramulu PY. Longitudinal changes in daily patterns of objectively measured physical activity after falls in older adults with varying degrees of glaucoma. EClinicalMedicine. (2021) 40:101097. doi: 10.1016/j.eclinm.2021.101097
44. García-Hedrera FJ, Noguera-Quijada C, Sanz-Márquez S, Pérez-Fernández E, Acevedo-García M, Domínguez-Rincón R, et al. Incidence and characteristics of falls in hospitalized patients: A cohort study. Enferm Clin (Engl Ed). (2021) 31:381–9. doi: 10.1016/j.enfcle.2021.04.003
45. Patil R, Uusi-Rasi K, Kannus P, Karinkanta S, Sievänen H. Concern about falling in older women with a history of falls: associations with health, functional ability, physical activity and quality of life. Gerontology. (2014) 60:22–30. doi: 10.1159/000354335
46. Avin KG, Hanke TA, Kirk-Sanchez N, McDonough CM, Shubert TE, Hardage J, et al. Academy of geriatric physical therapy of the American physical therapy association. Management of falls in community-dwelling older adults: clinical guidance statement from the academy of geriatric physical therapy of the American physical therapy association. Phys Ther. (2015) 95:815–34. doi: 10.2522/ptj.20140415
Keywords: age, malnutrition, fall, meta-analysis, rural
Citation: Xu Q, Ou X and Li J (2022) The risk of falls among the aging population: A systematic review and meta-analysis. Front. Public Health 10:902599. doi: 10.3389/fpubh.2022.902599
Received: 23 March 2022; Accepted: 20 September 2022;
Published: 17 October 2022.
Edited by:
Enno Nowossadeck, Robert Koch Institute (RKI), GermanyReviewed by:
Lambert Zixin Li, Stanford University, United StatesCopyright © 2022 Xu, Ou and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinfeng Li, eHVlYmFpXzEzMTRAMTI2LmNvbQ==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.