- 1Department of Stomatology, Clinical Traditional Chinese Medicine College of Yangzhou University, Yangzhou, China
- 2Department of Gastroenterology, Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou, China
- 3Health Management Center, Affiliated Hospital of Yangzhou University, Yangzhou, China
Background: Emotion and quality of life may have been impacted by the coronavirus disease 2019 (COVID-19) crisis, especially in the lockdown. The impact of temporomandibular disorders (TMD) symptoms and tooth loss on mental status and Oral Health-Related Quality of Life (OHRQoL) are not fully understood in a stressful situation.
Objectives: We aimed to investigate whether TMD and tooth loss were the impaired risks of psychological states and OHRQoL in COVID-19 lockdown, and attempt to explore other potential risk factors.
Methods: This cross-sectional study surveyed residents via an online self-reported questionnaire, when Yangzhou was in lockdown. Demographic data, clinical information, the level of anxiety, depression and OHRQoL were collected and analyzed.
Results: Painful TMD symptoms and tooth loss are the risks of more severe anxiety and depression. TMD symptoms and tooth loss worsened OHRQoL. Lower education degree (OR: 6.31, P = 0.019), TMD-related pain symptoms (OR: 10.62, P = 0.005), tooth loss (OR: 3.12, P = 0.035), sleep disorders (OR: 2.92, P = 0.049) and relatively close contacts (OR: 3.95, P = 0.020) were verified as risk factors for increased level of anxiety. With respect to depression, low socio-economic status (OR: 6.22, P = 0.021), TMD-related pain (OR: 7.35, P = 0.012), tooth loss (OR: 4.48, P = 0.009), sleep disorders (OR: 5.13, P = 0.007) and relatively close contacts (OR: 12.94, P = 0.001) were identified as independent factors for developing depression. Additionally, drinking (B: −2.584, P = 0.013) and never going to the dental clinic (B: −3.675, P = 0.024) were relevant to better OHRQoL, while TMD without pain (B: 2.797, P = 0.008), TMD-related pain (B: 12.079, P < 0.001), tooth loss (B: 2.546, P = 0.006), sleep disorders (B: 2.598, P = 0.003) were independent factors for impaired OHRQoL.
Conclusion: Painful TMD symptoms, tooth loss and sleep disorders were the impaired risks of psychological states. TMD symptoms and tooth loss damaged OHRQoL when the city was in lockdown. Therefore, individualized psychological counseling is supposed to maintain control of mental health and OHRQoL under the stressful event.
Introduction
Temporomandibular disorders (TMD) are a group of conditions that cause pain and dysfunction of the masticatory muscles, temporomandibular joint (TMJ), and the surrounding musculoskeletal structures (1). Being the third most prevalent social dental disease, TMD affects about 10–15% population across the world and the incidence is still rising (2, 3). Typical symptoms of TMD include local pain, limited mandibular movement, and TMJ sounds during movement (4). The etiology of TMD still remains elusive, accumulating evidence suggests that factors from biologic, environmental, social, emotional, and cognitive aspects all play an indispensable role in the occurrence and development of TMD (5). Among these triggers, the contribution of psychological issues involved in emergency or threatening situations like the ones faced with the coronavirus disease 2019 (COVID-19) pandemic, to the onset and duration of TMD has been acknowledged by more and more researchers (6, 7). Psychological and socio-demographic factors, including somatization, depression, stress, anxiety, daytime sleepiness, optimism, gender and age, aggravated pain intensity and pain-related disability in patients with TMD (8). In turn, previous studies showed that TMD patients exhibited higher level of psychological disorders such as anxiety and depression compared with healthy controls (9–11). Patients with self-reported TMD-pain reported higher scores for anxiety, depression, and somatic symptoms compared to patients with no TMD-Pain complaint (12). In addition, ample evidence demonstrates that tooth loss is negatively associated with depression, anxiety and Oral Health-Related Quality of Life (OHRQoL) (13, 14), which is in line with the observation that effective treatment of tooth loss have positive effects on quality of life and mental status (15). Collectively, the influence of the bidirectional relationship between psychosocial and physical factors deserves further clinical attention.
Since the end of 2019, a novel, threatening pandemic, the COVID-19 caused by severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) infection, caused a health crisis worldwide (16–18). Many countries adopted a policy of lockdown aiming to decelerate the contagion, which subsequently made dramatical changes of the daily lifestyle of the residents, and negatively influenced the mental health of individuals (19, 20). Recent studies implicated that outbreak of COVID-19 was supposed to cause emotional disorders, cognition dysfunction, behavioral disturbance and impaired quality of life, especially in population with psychosomatic diseases such as coronary heart disease, irritable bowel disease and psoriasis, in whom psychological distress and somatic diseases could mutually influence one another (21–24). Regarding dentistry, most of the studies indicated adverse effects of COVID-19 on psycho-emotional status (stress, anxiety, depression), which lead to the intensification of TMD symptoms and increased orofacial pain (OFP) (25). However, few studies have examined whether some dental problems may be the risk factors of the mental health and OHRQoL during COVID-19 lockdown.
Dental clinic is confronted with potential risk of transmitting COVID-19. On one hand, multiple dental procedures using ultrasound instruments tend to produce aerosol fog of saliva or blood droplets in the workplace, which has been proven to be a potent carrier of the virus (26); on the other hand, the execution of dental treatment involves close contact between dentist and patients, which further exacerbates the possibility of human-to-human transmission (27, 28). Thus, according to the American Dental Association (ADA) recommendation, all dental treatments, in addition to the emergency treatment, should be delayed.
There was a COVID-19 outbreak in Yangzhou, a tourist city in Eastern China. It was a resurgence of the coronavirus since Wuhan lockdown. Before this resurgence, the pandemic of COVID-19 in China had been at stable status. To cope with it, the government took strict lockdown measures. This cross-sectional study was performed using an online questionnaire to explore potential risk factors of the altered psychological status and OHRQoL during Yangzhou lockdown, thereby modifying the variables for which intervention is feasible, and optimizing the management of susceptible people. We assume that TMD or tooth loss are the risk factors of higher levels of anxiety and depression as well as poorer OHRQoL.
Methods
Participants
Due to the impossibility of clinical evaluation because of the social isolation, the evaluation of TMD symptoms, OHRQoL, anxiety, and depression was carried out through online questionnaires. The questionnaires were edited through the Wen-Juan-Xing online platform. Then, an electronic two-dimensional code of the questionnaire was created. When Yangzhou was in the lockdown, every residential district has its own WeChat group. A lot of information about epidemic lockdown was sent through the WeChat group, and the questionnaires were randomly distributed to those groups by the group advocates. All the subjects were residents in these enclosed districts, and the sample size collected during the opening hour had reached the expectation. A total of 300 online questionnaires were randomly distributed, but 23 individuals were excluded from the analysis, including 9 were diagnosed with psychological diseases at the time of our study; 10 had other physical disorders closely related to their psychological state, and the remaining 4 cases did not provide sufficient information. The inclusion criteria were as follows: (1) those who were residents in these enclosed districts during Yangzhou lockdown. (2) volunteered to participate in research. The exclusion criteria included (1) those who did not answer the questionnaire in the opening hours; (2) those who were diagnosed with psychological diseases at the time of our study; (3) those who had other physical disorders closely related to their psychological state. According to Peduzzi et al. (29) and Concato et al. (30), the sample size satisfied the following analysis. This survey was conducted 1 month after the implement of the lockdown. All protocols in the study were carried out in accordance with the principles of the Declaration of Helsinki. This study was approved by the Institutional Review Board and Ethics Committee of Clinical Traditional Chinese Medicine College of Yangzhou University (REC ref 2021-29). We obtained their authorization by signing the informed consent.
Data Collection
The first part of the questionnaire collects basic information of the participants, including gender, age, occupation, education, economic level, marital status, etc. The second part is some issues related to the epidemic, for example: Were you close contacts of any confirmed cases or familiar with someone who is confirmed case? Have you been vaccinated? Did you join in the voluntary service against the epidemic in the local community?
The third part mainly assesses the presence of symptoms related to TMD. On the basis of the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD), which was translated and validated into Chinese with objective questions about TMD symptoms. The answered questionnaires were analyzed by a specialist in the field and the participants were classed into three groups according to their symptoms: without TMD symptoms, with non-painful TMD symptoms, or painful TMD symptoms (31). In this part, there are also some issues about sleep disorder, tinnitus, tooth loss and so on.
The fourth part focuses on the psychological status and OHRQoL of the responders. The Generalized Anxiety Disorder Scale 7 (GAD-7), which assesses the patient's anxiety over the past month, consists of seven questions, each with four choices, with scores ranging from 0 to 3, for a total of 21 points. The higher the score is, the worse the anxiety is. A score of 0–4 is classified as normal, 5–9 as mild anxiety, 10–14 as moderate anxiety and 15–21 as severe anxiety (32). Depression was assessed with Patient Health Questionnaire-9 (PHQ-9). There are nine questions, each score is 0–3 points, with a total score of 27 points. Zero to four is minimal depression, 5–9 mild, 10–14 moderate, 15–19 moderately severe and 20~27 severe (33). To evaluate the OHRQoL of the participants, the Oral Health Impact Profile-14 (OHIP-14) scale was applied. It covers 14 items in seven areas with five choices in each item. The score is 0 to 4 for each item with a total score of 56, which is inversely proportional to the level of OHRQoL (34).
Statistical Analysis
Statistical analysis was performed using SPSS version 22.0 (IBM SPSS Statistics, USA). Continuous variables were presented as mean ± standard deviation (SD) and categorical variables were presented as proportions. Univariate logistic regression was performed to identify potential modifiers of psychological stress.
In univariate analysis, the screening criteria for candidate predictors was P < 0.05. Then, multivariate analysis was further used to eliminate the variables with no statistical significance. P < 0.05 in multivariate analysis was considered statistically significant. Odds ratios (OR) were applied to measure the correlation between variables and outcomes of psychological stress.
Using the added scores of OHIP-14 as a continuous outcome, multiple linear regression analyses were performed adjusted for all variables. The coefficients 95% confidence intervals (CI) for Beta and P-values were calculated.
Result
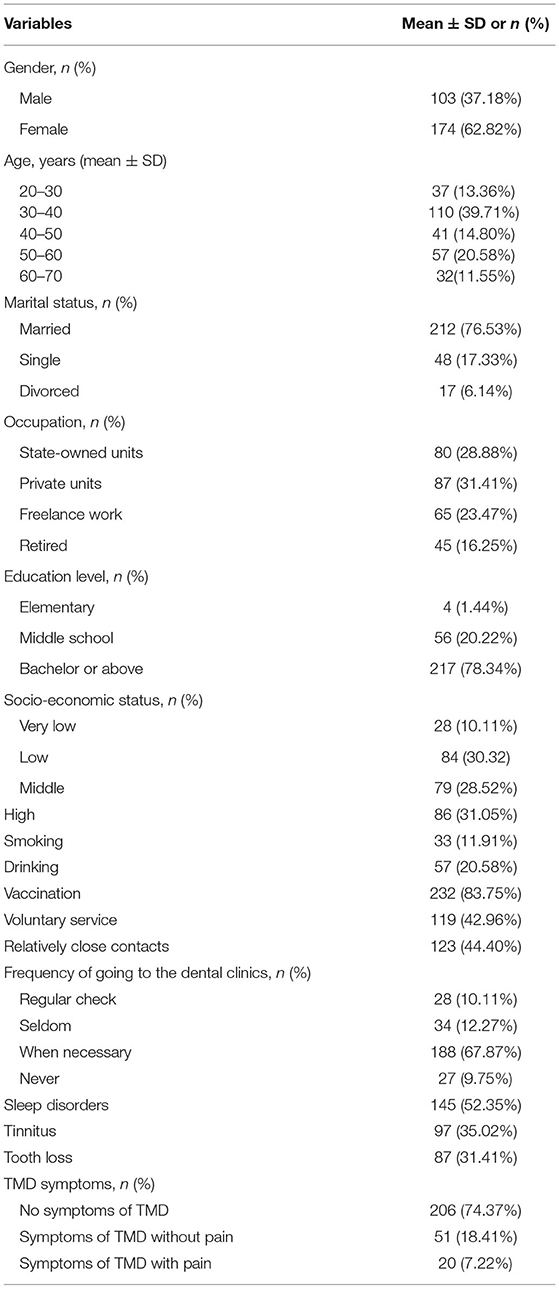
A total of 300 online questionnaires were randomly distributed among the lockdown population, 23 individuals were excluded as described above. Basic information is shown in Table 1. The age is mainly distributed in the 30–40 stage, and the male: female ratio was 103:174. Seventy- seven percent were married, 17.33% single, and 6.14% divorced. In regard to the occupation, 28.88% worked in state -owned units; 31.41% in private units; 23.47% worked freelance; and the remaining 16.25% had retired. In terms of education level, 78.34% got a bachelor's degree or higher. Smokers and drinkers accounted for 11.91% and 20.58%, respectively.
Concerning the TMD symptoms, most participates (74.37%) did not report any symptoms of TMD, 51 patients suffered from TMD without pain, while the rest complained of TMD with pain. A total of 145 patients (52.35%) reported sleep disorders. Tinnitus and tooth loss were present in 35.02% and 31.41% patients, respectively. When talking about the frequency of going to the dental clinics, 10.11% of the participates had a regular check, while the majority turned to a dental clinic when necessary. After the outbreak of the epidemic, 119 patients in our study joined in the voluntary service against the epidemic in the local community, and most of the population (83.75%) accepted vaccine injection. In addition, 123 (44.40%) were considered as relatively close contacts.
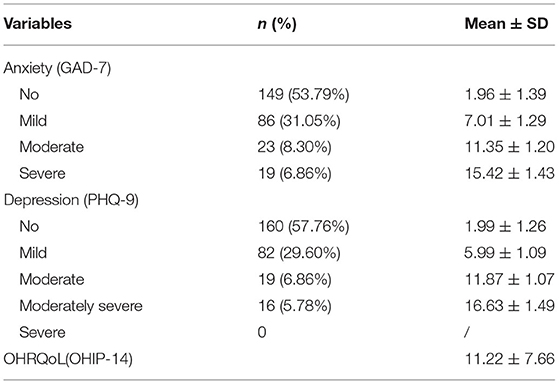
When using 5 as the cut-off value for the GAD-7 scale, the incidence of anxiety was 46.21% (128/277), with 86 in the mild group, 23 in the moderate group and 19 in the severe group (Table 2). In terms of depression, 117 (42.24%) scored ≥5 for the PHQ-9 scale, regarded as the existence of depression, and among these, 82 (29.60%) presented mild depression, 19 (6.86%) moderate, and 16 (5.78%) moderately severe. During the closure, the mean score of the OHRQoL assessed by OHIP-14 is 11.22 ± 7.66.
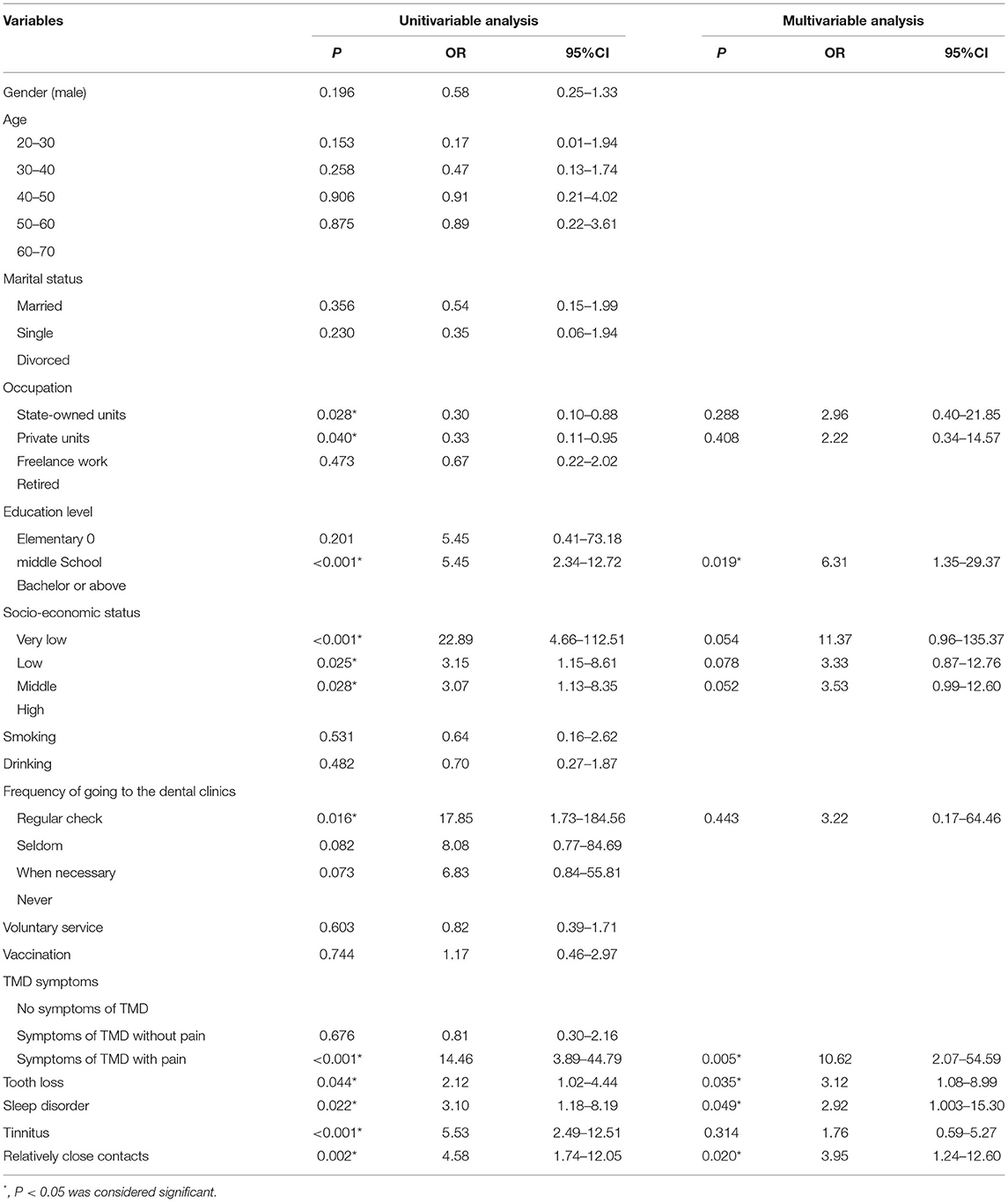
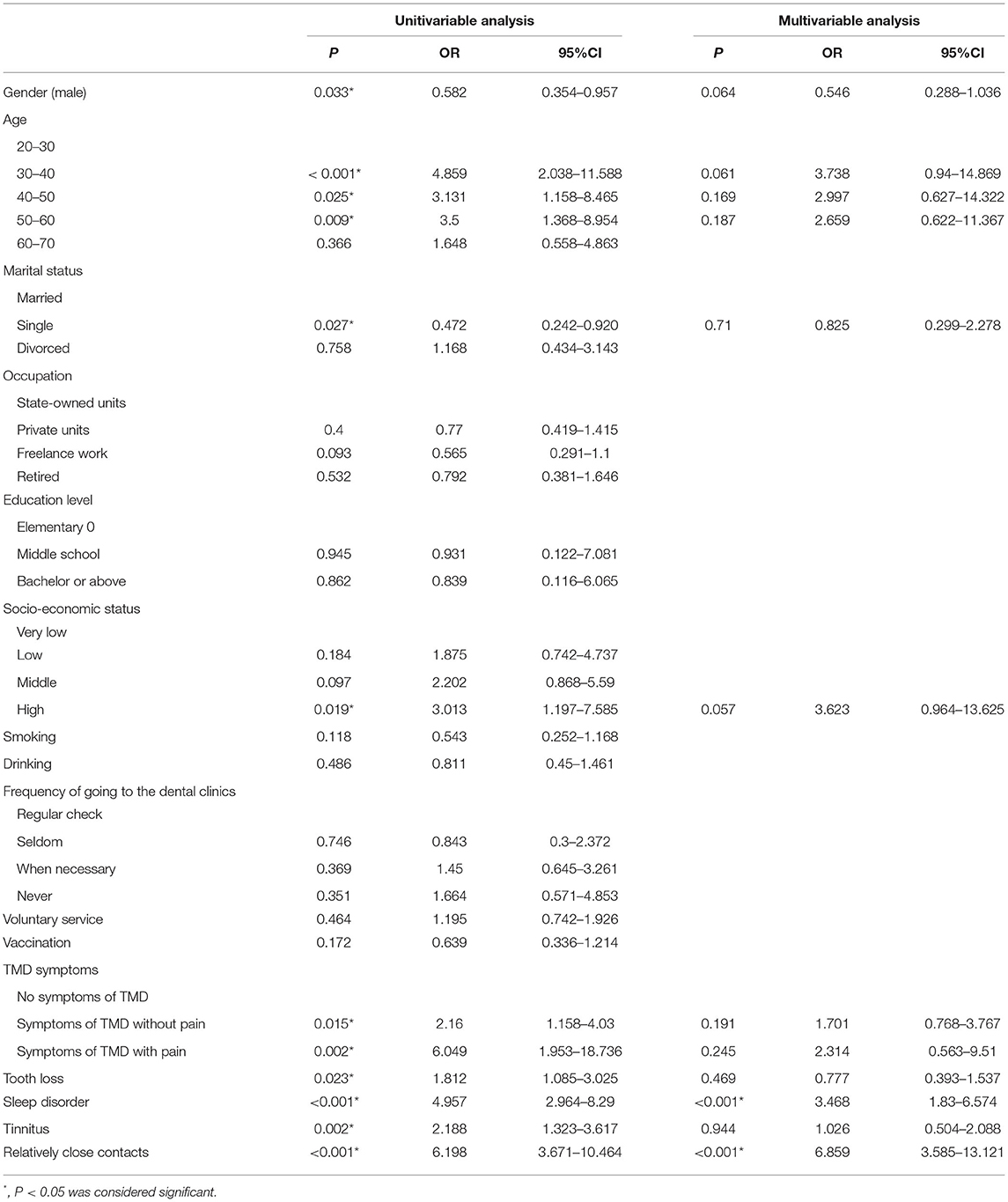
To explore the influencing factors of anxiety in the situation of COVID-19 lockdown, we first applied univariate logistics regression to screen potential variables. As shown in Table 3, compared with retired, working in state-owned [OR: 0.30 (95% CI: 0.10–0.88), P = 0.028) or private units [OR: 0.33 (95% CI: 0.11–0.95), P = 0.040] tended to have lower anxiety. Lower education degree [OR: 5.45 (95% CI: 2.34–12.72), P < 0.001], poorer socio-economic status, regular check at the dental clinics, [OR: 17.85 (95% CI: 1.73–184.56), P = 0.016], TMD-related pain [OR: 14.46 (95% CI: 3.89–44.79), P < 0.001], tooth loss [OR: 2.12 (95% CI: 1.02–4.44), P = 0.044], sleep disorders [OR: 3.10 (95% CI: 1.18–8.19), P = 0.022], tinnitus [OR: 5.53 (95% CI: 2.49–12.51), P < 0.001] and relatively close contacts [OR: 4.58 (95% CI: 1.74–12.05), P = 0.002] were significantly related to higher anxiety. After adjustment by multivariant analysis, lower education degree [OR: 6.31 (95% CI: 1.35–29.37), P = 0.019], TMD-related pain [OR: 10.62 (95% CI: 2.07–54.59), P = 0.005), tooth loss [OR: 3.12 (95% CI: 1.08–8.99), P = 0.035], sleep disorders [OR: 2.92 (95% CI: 1.003–15.30), P = 0.049) and relatively close contacts [OR: 3.95 (95% CI: 1.24–12.60), P = 0.020] were verified as risk factors for more severe anxiety.
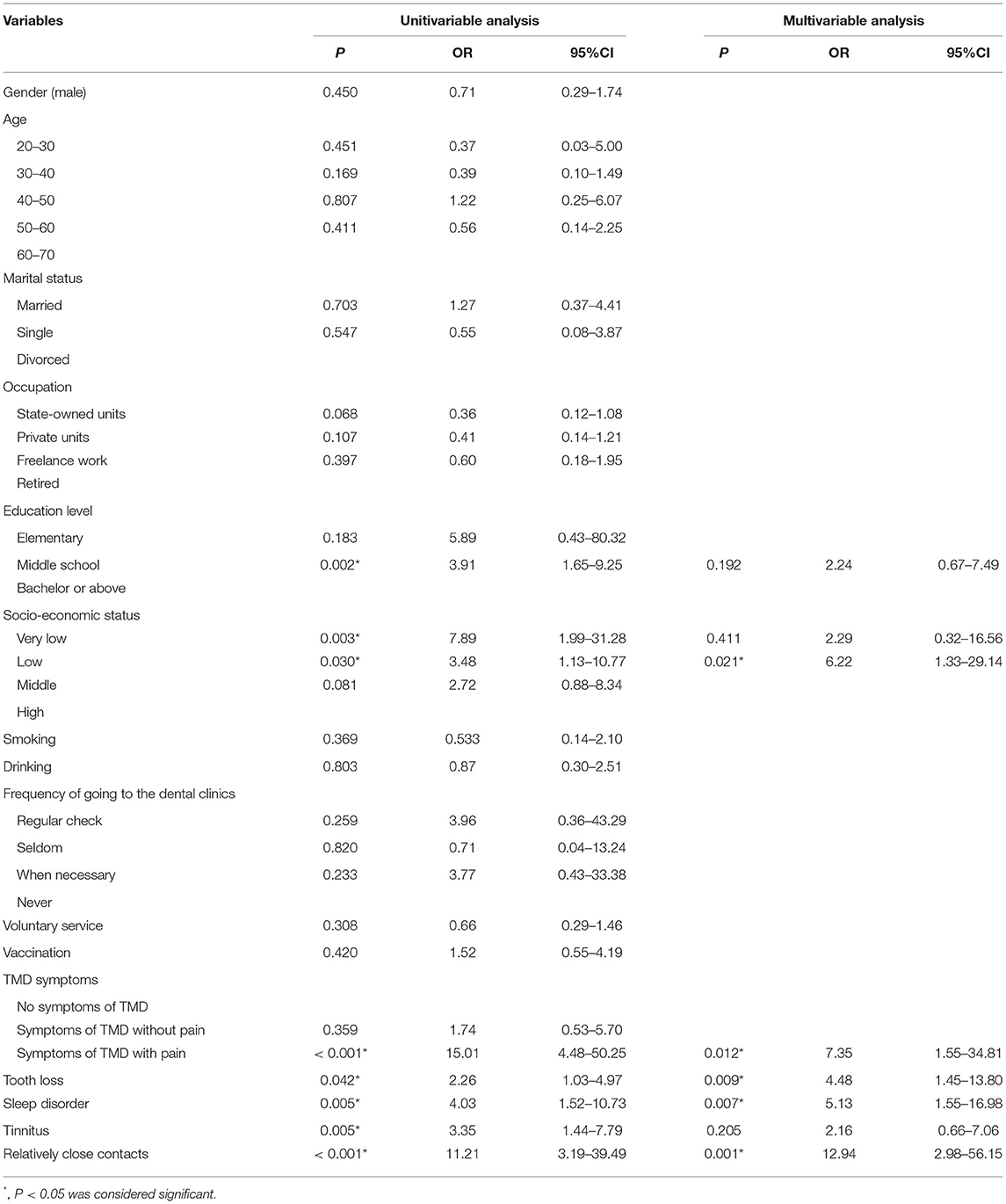
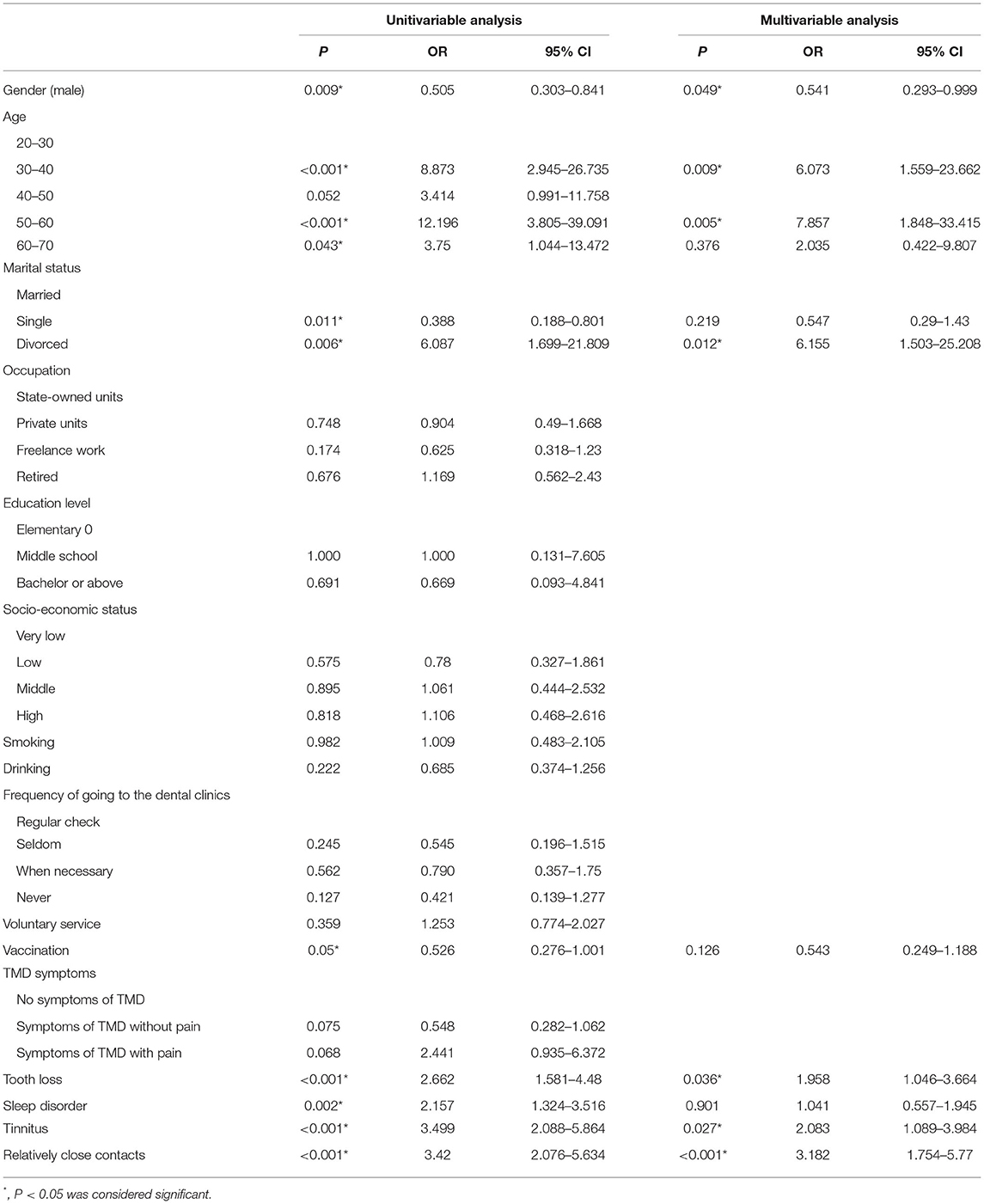
With respect to depression, after using univariate logistics regression to screen potential variables, we performed multivariant analysis. Low socio-economic status [OR: 6.22 (95% CI: 1.33–29.14), P =0.021], TMD-related pain [OR: 7.35 (95% CI: 1.55–34.81), P = 0.012], tooth loss [OR: 4.48 (95% CI: 1.45–13.80), P = 0.009], sleep disorders (OR: 5.13 (95% CI: 1.55–16.98), P = 0.007] and relatively close contacts [OR: 12.94 (95% CI: 2.98–56.15), P = 0.001] were identified to be independent factors for progression of depression (Table 4).
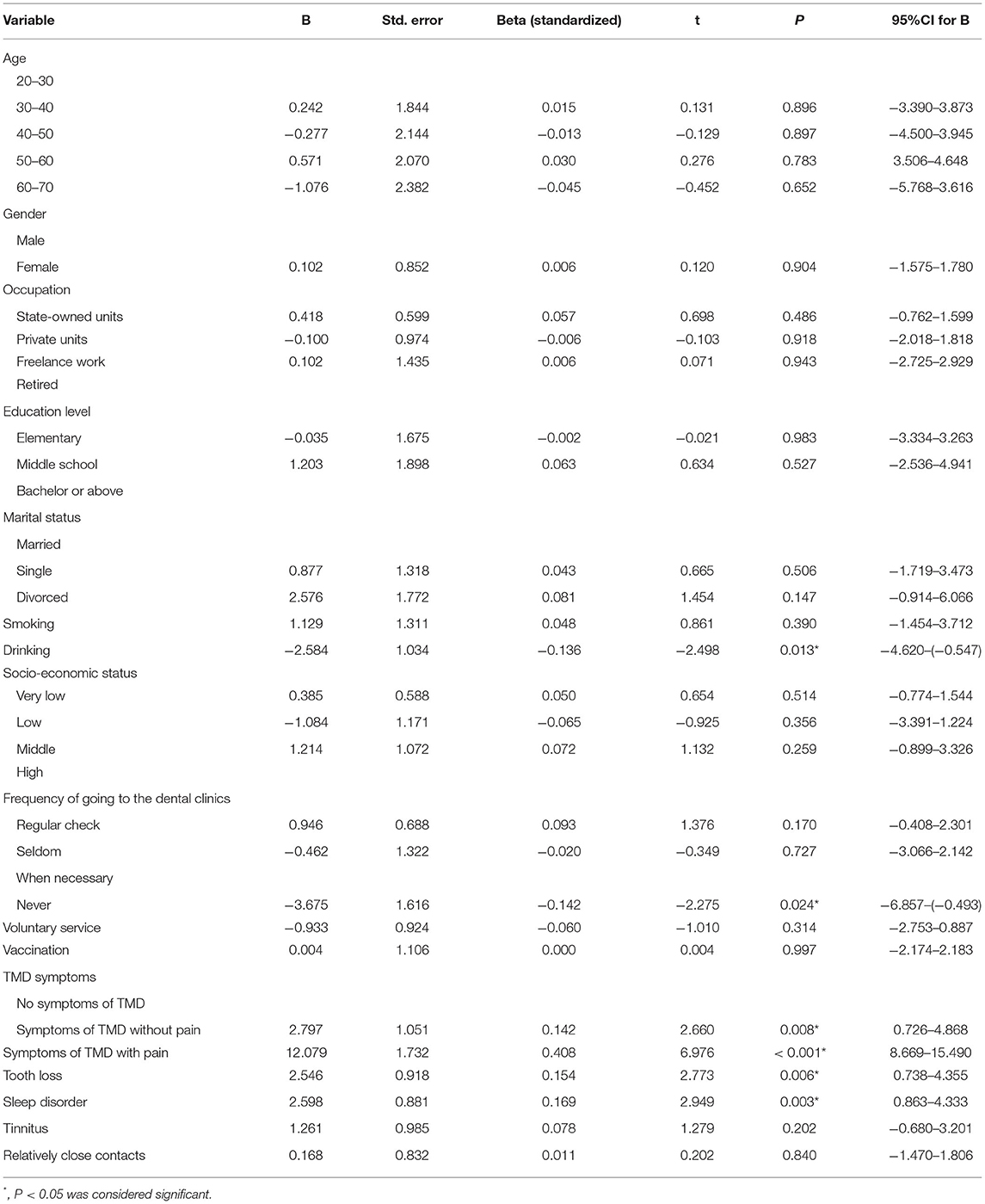
In addition, drinking (B: −2.584, P = 0.013) and never going to the dental clinic (B: −3.675, P = 0.024) were relevant to better oral related quality of life, while TMD without pain (B: 2.797, P = 0.008), TMD-related pain (B: 12.079, P < 0.001), tooth loss (B: 2.546, P = 0.006), sleep disorders (B: 2.598, P = 0.003) were independent risk factors for impaired OHRQoL (Table 5).
In order to assess the impact of these variables to the occurrence of anxiety and depression, logistic regression analyses were performed. The multivariant analysis showed that sleep disorder (OR: 3.468, P < 0.001) and relatively close contacts (OR: 6.859, P < 0.001) were independent risk factors for the occurrence of anxiety, and 30–40 years old (OR: 6.073, P = 0.009), 50–60 years old (OR: 7.857, P = 0.005), tooth loss (OR: 1.958, P = 0.036), divorced status (OR: 6.155, P = 0.012), tinnitus (OR: 2.083, P = 0.027) and relatively close contacts (OR: 3.182, P < 0.001) were verified as risk factors for increasing the occurrence of depression. Male (OR: 0.541, P = 0.049) decreased the occurrence of depression (Tables 6, 7).
Discussion
Our findings showed that during the city-wide lockdown caused by SARS-CoV-2, TMD and tooth loss significantly altered psychological stress and OHRQoL. When confronting the stress of COVID-19, people had to change their daily life and behavior, particularly social relationships, which can affect health in varieties of aspects, including mental and physical risks (35). In the field of dentistry, previous studies showed that the pandemic's influence on psychological factors may increase risks of developing TMD symptoms and certain oral diseases, such as bruxism and OFP (25, 36, 37). For instance, a study conducted during the pandemic in Israeli and Polish indicated that COVID-19-related mental disorders led to the intensification of bruxism and TMD symptoms, and consequently OFP increased (38). Gender differences has been proven to be an influential factor contributed to such processes: the anxiety and stress caused by COVID-19 participate in deteriorating stomatognathic diseases, and women were generally more influential than men (36, 39). The cross-sectional study from Wuhan lockdown showed a significantly higher impact of COVID-related stress in TMD patients in comparison to orthodontic patients and control population (40). A prospective study in Italy revealed that as compare with acute/subacute TMD patients, chronic TMD patients were more likely to suffer from increased facial pain severity and COVID-19-related stress (41). However, whether dental problems such as TMD and tooth loss may aggravate psychological stress and deteriorate OHRQoL during COVID-19 lockdown in China was rarely reported before. We attempted to identify potential risk factors to predict psychological disorders and the impaired sense of wellbeing under the stressful event. The results provide data supports to improve the manner of treatments and optimize management for people with dental problems. Additionally, our findings are complementary and reinforce the influence of the bidirectional relationship between psychosocial and physical factors in dentistry.
According to our questionnaire-based analysis, our findings demonstrated that TMD-related pain was significantly correlated with increased psychological stress. Of the 71 subjects who reported TMD symptoms, 20 (28.19%) suffered from painful TMD symptoms, which was found to be responsible for the development of more severe anxiety and depression. There were previous studies showing that chronic pain increases the severity of anxiety, as well as depression (42, 43). Although we didn't investigate the specific reason behind elevated stress, one important factor that could not be ignored is the intense confinement under the context of lockdown, which may exacerbate feelings of loneliness. Therefore, we can infer that “home isolation” could be considered as a critic trigger, which was previously confirmed in another study (44).
Our study revealed that TMD symptoms significantly decreased OHRQoL of the volunteers, suggesting that perception of happiness was impaired by TMD symptoms. Our findings could partially explain why non-steroidal anti-inflammatory drugs (NSAIDs) and selective serotonin reuptake inhibitors (SSRIs) could effectively improve the OHRQoL of TMD patients (45). Thus, it is reasonable to speculate that NSAIDs and SSRIs may be considered to relieve the decline of OHRQoL during the pandemic, especially in those with prominent TMD symptoms.
We discovered that the score of anxiety, depression and oral quality in the group with tooth loss were remarkably higher than those without tooth loss. This phenomenon was in consistence with other investigations, but might be more serious under that situation, which could be, at least in part, attributed to the closure of the dental clinics (46, 47).
Lower economic status and educational level were also identified as important risk factors for predicting the severity of psychological disorders during the lockdown. This finding was in accordance with previous studies, which have linked long-term stress including financial or educational problems to the increased stress (43, 48). One possible explanation for this phenomenon is the limited understanding of the SARS-CoV-2, which can be considered as a direct trigger for psychological stress.
It was widely acknowledged that sleep problem is a crucial factor in emotional burden. As an important health indicator, sleep quality may help strengthen the immune system against infection and facilitate in the regulation of behavior and emotion (49). Previous studies demonstrated that global stressor events (e.g., global pandemic, wars) were critical factors for sleep and psychological disorders (50). In this study, we also verified the negative impact of sleep disorders on psychological distress and OHRQoL, indicating that sleep quality could be a potent target for the management of dental patients during lockdown. Of note, people who never go dental have lower oral quality scores than other groups. This sounds strange but is actually reasonable, because those who never go dental might be quite satisfied with their oral health, which was reported in previous literatures (51, 52).
In the present study, no individuals were diagnosed with COVID-19, but 123 (44.40%) were considered as relatively close contacts and strongly associated with anxiety and depression. Under that situation, people were under the almost complete lockdown and all non-emergency medical and dental treatments were suspended. Most public places such as shops, restaurants were closes. Personal contact with family members and/or friends who are not cohabiting in the same household is prohibited. For the confirmed cases and their closest contacts, medical isolation was conducted, which means separation in isolation wards, nuresd by medical staff. Importantly, the relatively close contacts who contacted of any confirmed cases relatively closely or was familiar with confirmed case, faced much higher risk and more fear of being contaminated by the virus than the general population. Based on this, it is not surprising that relatively close contacts presented higher levels of anxiety and depression. Our findings suggest the importance of timely psychological counseling for reducing the psychological pressure of the relatively close contacts. It's encouraging that online intervention for TMD or psychological problems can be useful at least at its initial stage in times of isolations when face-to-face consultation is prohibited during COVID-19 (25). Further investigation is obviously needed to confirm the role of online intervention during COVID-19 lockdown in more detail.
Our findings should be considered with caution given some limitations of the study. Firstly, the relatively small sample size may have influenced results. Secondly, this study was conducted in one center in one country, which reduces the external validity and the generalizability of the results. In addition, Since, the questionnaires were self-reported, subjectivity is a factor that cannot be ignored when translating these findings into clinical practice. In some cases, the extent of anxiety/depression may be overstated or underestimated, which lead to the severity of the illness may be inaccurate. Hence, these factors should be taken into consideration when using the results of our study. Despite these limitations, it is worth noting that the current study for the first time to investigate the impacts of TMD symptoms and tooth loss on the COVID-19 lockdown related anxiety, depression and OHRQoL.
The results remind us that as oral health professionals, our work shouldn't be limited to just the oral cavity, but the whole person. When treating patients with TMD or tooth loss, additional attention should be paid to their psychological status, so as to support their oral health as well as the integral ability to perform activities of daily living. Further prospective longitudinal studies are necessary to validate our findings, thus extending the clinical application of the current study.
Conclusion
This study highlights COVD-19 pandemic, especially the lockdown followed have significant adverse impacts on psychological states and OHRQoL in people with TMD symptoms. Those with TMD-related pain, tooth loss and sleep disorders were more prone to experience worse psychological stress. Individualized management such as psychological counseling should be promoted to maintain control of mental health and OHRQoL under the stressful event.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Statement
This study was approved by the Institutional Review Board and Ethics Committee of Clinical Traditional Chinese Medicine College of Yangzhou University (REC ref 2021-29). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
SW, SH, XJ, and YS carried out the studies, participated in the experimental design and statistical analysis, and drafted the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported in part by grant from National Natural Science Foundation of China (No. 31800675 to SH, the Postdoctoral Science Foundation in Jiangsu Province (No. 2018K263C to SH), and 2021 Yangzhou Policy Guidance Plan (Soft Science Research) Project (No.YZ2021231 to XJ).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. (2008) 359:2693–705. doi: 10.1056/NEJMra0802472
2. Małgorzata P, Małgorzata KM, Karolina C, Gala A. Diagnostic of temporomandibular disorders and other facial pain conditions-narrative review and personal experience. Medicina. (2020) 56, 472. doi: 10.3390/medicina56090472
3. Lim PF, Smith S, Bhalang K, Slade GD, Maixner W. Development of temporomandibular disorders is associated with greater bodily pain experience. Clin J Pain. (2010) 26:116–20. doi: 10.1097/AJP.0b013e3181c507ef
4. Xie C, Lin M, Yang H, Ren A. Prevalence of temporomandibular disorders and its clinical signs in Chinese students, 1979-2017: a systematic review and meta-analysis. Oral Dis. (2019) 25:1697–706. doi: 10.1111/odi.13016
5. List T, Jensen RH. Temporomandibular disorders: old ideas and new concepts. Cephalalgia. (2017) 37:692–704. doi: 10.1177/0333102416686302
6. Tay KJ, Yap AU, Wong JCM, Tan KBC, Allen PF. Associations between symptoms of temporomandibular disorders, quality of life and psychological states in Asian Military Personnel. J Oral Rehabil. (2019) 46:330–9. doi: 10.1111/joor.12751
7. Fillingim RB, Ohrbach R, Greenspan JD, Knott C, Diatchenko L, Dubner R, et al. Psychological factors associated with development of TMD: the OPPERA prospective cohort study. J Pain. (2013) 14(12 Suppl):T75–90. doi: 10.1016/j.jpain.2013.06.009
8. Su N, Lobbezoo F, van Wijk A, van der Heijden GJ, Visscher CM. Associations of pain intensity and pain-related disability with psychological and socio-demographic factors in patients with temporomandibular disorders: a cross-sectional study at a specialised dental clinic. J Oral Rehabil. (2017) 44:187–96. doi: 10.1111/joor.12479
9. Boscato N, Almeida RC, Koller CD, Presta AA, Goettems ML. Influence of anxiety on temporomandibular disorders–an epidemiological survey with elders and adults in Southern Brazil. J Oral Rehabil. (2013) 40:643–9. doi: 10.1111/joor.12076
10. De La Torre Canales G, Câmara-Souza MB, Muñoz Lora VRM, Guarda-Nardini L, Conti PCR, Rodrigues Garcia RM, et al. Prevalence of psychosocial impairment in temporomandibular disorder patients: a systematic review. J Oral Rehabil. (2018) 45:881–9. doi: 10.1111/joor.12685
11. Quartana PJ, Buenaver LF, Edwards RR, Klick B, Haythornthwaite JA, Smith MT. Pain catastrophizing and salivary cortisol responses to laboratory pain testing in temporomandibular disorder and healthy participants. J Pain. (2010) 11:186–94. doi: 10.1016/j.jpain.2009.07.008
12. Al-Khotani A, Meisha DE, Al Sayegh S, Hedenberg-Magnusson B, Ernberg M, Christidis N. The association between psychological symptoms and self-reported temporomandibular disorders pain symptoms in children and adolescents. Front Oral Health. (2021) 2:675709. doi: 10.3389/froh.2021.675709
13. Haag DG, Peres KG, Balasubramanian M, Brennan DS. Oral conditions and health-related quality of life: a systematic review. J Dent Res. (2017) 96:864–74. doi: 10.1177/0022034517709737
14. Okoro CA, Strine TW, Eke PI, Dhingra SS, Balluz LS. The association between depression and anxiety and use of oral health services and tooth loss. Community Dent Oral Epidemiol. (2012) 40:134–44. doi: 10.1111/j.1600-0528.2011.00637.x
15. Thomason JM, Heydecke G, Feine JS, Ellis JS. How do patients perceive the benefit of reconstructive dentistry with regard to oral health-related quality of life and patient satisfaction? A systematic review. Clin Oral Implants Res. (2007) 18(Suppl. 3):168–88. doi: 10.1111/j.1600-0501.2007.01461.x
16. Harvey WT, Carabelli AM, Jackson B, Gupta RK, Thomson EC, Harrison EM, et al. SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev Microbiol. (2021) 19:409–24. doi: 10.1038/s41579-021-00573-0
17. Vaidyanathan G. Coronavirus variants are spreading in India - what scientists know so far. Nature. (2021) 593:321–2. doi: 10.1038/d41586-021-01274-7
18. Wang P, Nair MS, Liu L, Iketani S, Luo Y, Guo Y, et al. Antibody resistance of SARS-CoV-2 variants B. 1351 and B117. Nature. (2021) 593:130–5. doi: 10.1038/s41586-021-03398-2
19. Dong L, Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emerg Infect Dis. (2020) 26:1616–8. doi: 10.3201/eid2607.200407
20. Kim HH, Jung JH. Social isolation and psychological distress during the COVID-19 pandemic: a cross-national analysis. Gerontologist. (2021) 61:103–13. doi: 10.1093/geront/gnaa168
21. Wu M, Shen L, Wang Q, Liu L, Lu S, Jin J, et al. Anxiety and depression prevalence and risk factors among patients with cardiovascular diseases in post-COVID-19 China. Front Public Health. (2021) 9:758874. doi: 10.3389/fpubh.2021.758874
22. Kuang Y, Shen M, Wang Q, Xiao Y, Lv C, Luo Y, et al. Association of outdoor activity restriction and income loss with patient-reported outcomes of psoriasis during the COVID-19 pandemic: a web-based survey. J Am Acad Dermatol. (2020) 83:670–2. doi: 10.1016/j.jaad.2020.05.018
23. Quek SXZ, Loo EXL, Demutska A, Chua CE, Kew GS, Wong S, et al. Impact of the coronavirus disease 2019 pandemic on irritable bowel syndrome. J Gastroenterol Hepatol. (2021) 36:2187–97. doi: 10.1111/jgh.15466
24. Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry. (2020) 11:790. doi: 10.3389/fpsyt.2020.00790
25. Emodi-Perlman A, Eli I. One year into the COVID-19 pandemic - temporomandibular disorders and bruxism: what we have learned and what we can do to improve our manner of treatment. Dent Med Probl. (2021) 58:215–8. doi: 10.17219/dmp/132896
26. Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. (2020) 12:9. doi: 10.1038/s41368-020-0075-9
27. Tang S, Mao Y, Jones RM, Tan Q, Ji JS, Li N, et al. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ Int. (2020) 144:106039. doi: 10.1016/j.envint.2020.106039
28. Johansson MA, Quandelacy TM, Kada S, Prasad PV, Steele M, Brooks JT, et al. SARS-CoV-2 Transmission from people without COVID-19 symptoms. JAMA Net Open. (2021) 4:e2035057. doi: 10.1001/jamanetworkopen.2020.35057
29. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. (1996) 49:1373–9. doi: 10.1016/S0895-4356(96)00236-3
30. Concato J, Peduzzi P, Holford TR, Feinstein AR. Importance of events per independent variable in proportional hazards analysis. I Background, goals, and general strategy. J Clin Epidemiol. (1995) 48:1495–501. doi: 10.1016/0895-4356(95)00510-2
31. Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network* and orofacial pain special interest group†. J Oral Facial Pain Headache. (2014) 28:6–27. doi: 10.11607/jop.1151
32. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
33. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
34. El Osta N, Tubert-Jeannin S, Hennequin M, Bou Abboud Naaman N, El Osta L, Geahchan N. Comparison of the OHIP-14 and GOHAI as measures of oral health among elderly in Lebanon. Health Qual Life Outcomes. (2012) 10:131. doi: 10.1186/1477-7525-10-131
35. Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. (2010) 51(Suppl):S54–66. doi: 10.1177/0022146510383501
36. Saki M, Shadmanpour M, Najafi HZ. Are individuals with orofacial pain more prone to psychological distress during the COVID-19 pandemic? Dent Med Probl. (2021) 58:17–25. doi: 10.17219/dmp/131683
37. Colonna A, Guarda-Nardini L, Ferrari M, Manfredini D. COVID-19 pandemic and the psyche, bruxism, temporomandibular disorders triangle. Cranio. (2021). doi: 10.1080/08869634.2021.1989768. [Epub ahead of print].
38. Emodi-Perlman A, Eli I, Smardz J, Uziel N, Wieckiewicz G, Gilon E, et al. Temporomandibular disorders and bruxism outbreak as a possible factor of orofacial pain worsening during the COVID-19 pandemic-concomitant research in two countries. J Clin Med. (2020) 9:3250 doi: 10.3390/jcm9103250
39. DE Caxias FP, Athayde FRF, Januzzi MS, Pinheiro LV, Turcio KHL. Impact event and orofacial pain amid the COVID-19 pandemic in Brazil: a cross-sectional epidemiological study. J Appl Oral Sci. (2021) 29:e20210122. doi: 10.1590/1678-7757-2021-0122
40. Wu Y, Xiong X, Fang X, Sun W, Yi Y, Liu J, et al. Psychological status of TMD patients, orthodontic patients and the general population during the COVID-19 pandemic. Psychol Health Med. (2021) 26:62–74. doi: 10.1080/13548506.2020.1858489
41. Asquini G, Bianchi AE, Borromeo G, Locatelli M, Falla D. The impact of Covid-19-related distress on general health, oral behaviour, psychosocial features, disability and pain intensity in a cohort of Italian patients with temporomandibular disorders. PLoS ONE. (2021) 16:e0245999. doi: 10.1371/journal.pone.0245999
42. De Leeuw R, Bertoli E, Schmidt JE, Carlson CR. Prevalence of traumatic stressors in patients with temporomandibular disorders. J Oral Maxillofac Surg. (2005) 63:42–50. doi: 10.1016/j.joms.2004.04.027
43. Akhter R, Hassan NM Aida J, Kanehira T, Zaman KU, Morita M. Association between experience of stressful life events and muscle-related temporomandibular disorders in patients seeking free treatment in a dental hospital. Eur J Med Res. (2007) 12:535–40.
44. Saccomanno S, Bernabei M, Scoppa F, Pirino A, Mastrapasqua R, Visco MA. Coronavirus lockdown as a major life stressor: does it affect TMD symptoms? Int J Environ Res Public Health. (2020) 17:8907. doi: 10.3390/ijerph17238907
45. Fischoff D, Spivakovsky S. Are pharmacological treatments for oro-facial pain effective? Evid Based Dent. (2018) 19:28–9. doi: 10.1038/sj.ebd.6401294
46. Galindo-Moreno P, Lopez-Chaichio L, Padial-Molina M, Avila-Ortiz G, O'Valle F, Ravida A, et al. The impact of tooth loss on cognitive function. Clin Oral Investig. (2021). doi: 10.1007/s00784-021-04318-4
47. Kisely S, Sawyer E, Siskind D, Lalloo R. The oral health of people with anxiety and depressive disorders - a systematic review and meta-analysis. J Affect Disord. (2016) 200:119–32. doi: 10.1016/j.jad.2016.04.040
48. Pallegama RW, Ranasinghe AW, Weerasinghe VS, Sitheeque MA. Anxiety and personality traits in patients with muscle related temporomandibular disorders. J Oral Rehabil. (2005) 32:701–7. doi: 10.1111/j.1365-2842.2005.01503.x
49. Simon EB, Oren N, Sharon H, Kirschner A, Goldway N, Okon-Singer H, et al. Losing neutrality: the neural basis of impaired emotional control without sleep. J Neurosci. (2015) 35:13194–205. doi: 10.1523/JNEUROSCI.1314-15.2015
50. Uhac I, Tariba P, Kovac Z, Simonić-Kocijan S, Lajnert V, Mesić VF, et al. Masticatory muscle and temporomandibular joint pain in Croatian war veterans with posttraumatic stress disorder. Coll Antropol. (2011) 35:1161–6.
51. Locker D, Gibson B. Discrepancies between self-ratings of and satisfaction with oral health in two older adult populations. Community Dent Oral Epidemiol. (2005) 33:280–8. doi: 10.1111/j.1600-0528.2005.00209.x
Keywords: COVID-19, TMD symptoms, tooth loss, mental health, Oral Health-Related Quality of Life (OHRQoL), lockdown
Citation: Weng S, Hou S, Jiao X and Sun Y (2022) Adverse Impacts of Temporomandibular Disorders Symptoms and Tooth Loss on Psychological States and Oral Health-Related Quality of Life During the COVID-19 Pandemic Lockdown. Front. Public Health 10:899582. doi: 10.3389/fpubh.2022.899582
Received: 18 March 2022; Accepted: 16 June 2022;
Published: 08 July 2022.
Edited by:
Mieszko Wieckiewicz, Wroclaw Medical University, PolandReviewed by:
Antonino Maniaci, University of Catania, ItalyZeinab A. Kasemy, University of Menoufia, Egypt
Copyright © 2022 Weng, Hou, Jiao and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Sun, MDkxOTYyQHl6dS5lZHUuY24=; Xiuping Jiao, MDkwMzczQHl6dS5lZHUuY24=; Sicong Hou, c2hvdUB5enUuZWR1LmNu
 Siwei Weng
Siwei Weng Sicong Hou
Sicong Hou Xiuping Jiao3*
Xiuping Jiao3*