- 1Department of Clinical Sciences, Institute of Tropical Medicine, Antwerp, Belgium
- 2Faculty of Psychology, Open University, Heerlen, Netherlands
- 3Department of Interdisciplinary Social Science, Utrecht University, Utrecht, Netherlands
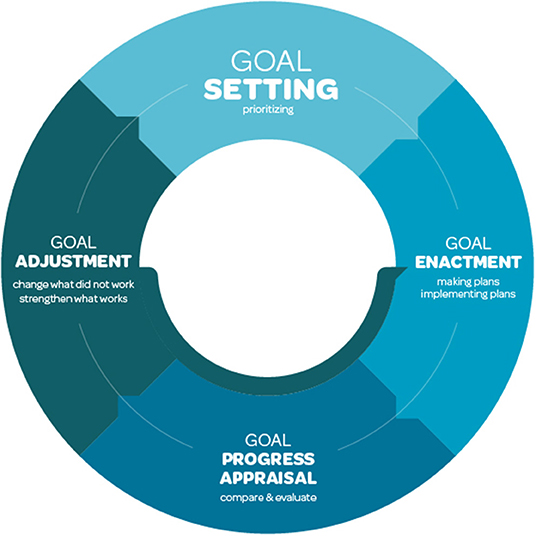
Few theory-informed interventions to support people who use drugs during sex have been conceptualized and developed. We conceptualize sexualized drug use, also referred to as chemsex or pharmacosex, as a self-control challenge, and draw on extant theory and research to propose intervention approaches that can be tailored to meet the differing needs of people who engage in sexualized drug use. We draw on a continuum perspective of sexualized drug use, in particular chemsex, and discuss the role of reasoned and automatic processes in behavioral decisions, as well as critical components of effective self-control of behavior. A self-control approach can empower people to tackle their sexualized drug use, and classify their experienced sex-related drug use as problematic. Self-control encompasses clarifying one's goals and identifying strategies to mitigate behaviors to achieve these goals, despite competing pharmacosex desires. Our approach to self-control sexualized drug use contains three critical components: goal setting, goal enactment, and goal progress appraisal and goal adjustment. Goals should be formulated specific, ambitious yet realistic, and tailored to the individual's needs and wishes. Goals may target aspects of drug use, protecting sexual health and mitigating negative impacts. Implementing goal enactment implies translating goals into concrete (short-term) actions to move toward the higher-order goal via goal intentions and action/coping plans. During the goal progress appraisal and adjustment stage, people compare their actual with their planned behavior. This reflection may result in goal adjustment through feedback loops to adjust their goals and action/coping plans. We propose that our self-control approach can guide the development of interventions to effectively support people to prevent or limit pharmacosex, and helps to effectively mitigate or reduce negative impacts via self-help, peer support or professional support, offered via personal counseling or digital tools.
Sexualized Drug Use and Potential Harms
Chemsex, “the use of drugs before or during planned sexual activity to sustain, enhance, disinhibit or facilitate the experience” (1), has become a public health concern, especially among gay, bisexual and other men who have sex with men (GBMSM) (2, 3). Chemsex is a specific form of sexualized drug use characterized by the use of potent substances [i.e., methamphetamine (“crystal meth”), mephedrone and gamma-hydroxybutyrate (GHB)/gamma-butyrolactone (GBL)] (4), albeit that differences in the specific drugs that are used have been observed between regions (5, 6) and user samples (7). Chemsex is also characterized by the contexts in which it used, notably during events that may last for several days, and its association with previously unseen harm among a specific group of GBMSM using (digital) technologies (8). People in other population groups are also found to engage in sexualized drug use, in particular swingers, heterosexual men and women who as a couple have sex with others (9). As chemsex has come to refer to specific types of sexualized drug use among GBMSM, the more inclusive term pharmacosex has been proposed to cover the range of substances that are used in conjunction with sex by diverse population groups (10). We will interchangeably use the terms sexualized drug use, and pharmacosex, unless we draw on work specifically referring to chemsex.
People initiate sexualized drug use for diverse reasons. Some people use drugs in combination with sex for hedonistic reasons, as drug use can enhance the qualities valued in sex and may increase the capability for the sex that is wanted. Others initiate sexualized drug use to increase a sense of belonging or to cope with everyday problems (11, 12). Taking drugs when having sex has in particular been found to be a coping strategy to deal with negative emotions and experiences, such as loneliness, anxiety (traumatic), stress, or low self-esteem (13). Feelings of loneliness may stem from an accumulation of intersecting adverse experiences (14).
Research has found associations between sexualized drug use, in particular chemsex, and a variety of sex and drug-specific health and social harms. Possible drug related health harms include dehydration, hyperthermia, drug-induced violence and injuries, psychosis, overdose and drug dependence (15). Furthermore, the majority of chemsex users combine different substances during a chemsex event (16–19). This polydrug use exposes the individual to even higher risks due to the combined effects (15, 20) and is associated with a higher risk of drug overdose (20). In addition to these drug related harms, chemsex is also associated with sexual risk behaviors, such as a large number of sexual partners, transactional sex, sharing sex toys, prolonged sexual sessions, condomless anal intercourse and other higher risk sexual practices, for example fisting (21–25). These behaviors increase the risk of sexually transmitted infections (STI), including HIV (21, 24, 26–28), and/or infections with (other) blood-borne viruses (e.g., hepatitis B or hepatitis C) (22). Chemsex is also associated with non-consensual or unwanted sex (6, 29). Furthermore, adverse mental health outcomes, such as anxiety and depression, have also been reported to be associated with chemsex (30, 31), especially when users inject drugs (“slamming”) (32).
Sexualized Drug Use Prevention and Support
In the context of these potential adverse impacts, recent research finds that some GBMSM who engage in sexualized drug use experience a need for support. An online survey among 511 GBMSM attending an STI-clinic in the Netherlands showed that 23% of men who engaged in chemsex expressed a need for professional counseling (6). These chemsex users primarily sought more information about existing healthcare services and peer support. However, where such services exist, GBMSM are found to encounter barriers related to both access to services and individual service providers' attitudes (33). Research has documented a need for dedicated, non-judgmental, and possibly anonymous support among GBMSM engaging in chemsex, as they may experience shame, fear of being recognized (26, 34), and stigmatization by their healthcare provider (35).
Care and support programs for GBMSM who engage in sexualized drug use remain limited. Some peer-based initiatives have been initiated to support GBMSM through harm-reduction services, peer support, health promotion, strengthening communities, training professionals and investing in advocacy and policy (8, 34–38), as well as mindfulness and yoga (personal communication). Behavioral interventions have been implemented, making use of text-messages communication (39), expressive writing (40), safer sex counseling (41), behavioral activation (42), personalized cognitive counseling (43) and motivational interviewing and cognitive behavioral therapy (44). Pharmatherapeutical approaches have also been implemented in healthcare settings (45, 46). In addition, some interventions using digital technology are in the pipeline, including for GBMSM who use chemsex in Hong Kong (47), the United States (48) and Belgium (49). The latter is conceived as an intervention to make chemsex users more conscious about their use, with the aim of reducing and tackling negative impacts of chemsex (49).
Despite these initiatives, the absence of evidence-based interventions to support people who engage in chemsex is concerning (6, 26, 49, 50). As is well-established in health promotion planning [e.g., (51)], we propose that appropriate and effective support programs for sexualized drug use should be adapted to the needs of beneficiaries, and grounded in theory and evidence. People who engage in sexualized drug use may have a variety of support needs, including drug related issues (e.g., dependence), as well as issues related to sexual health and the relational, professional and social implications of their sexualized drug use. Support should hence be tailored to these specific needs and provide different treatment options, including to tackle various interconnecting issues. In this paper, we first provide an outline of a conceptual perspective to guide support for people who engage in sexualized drug use. Subsequently, we propose intervention approaches aligned with the conceptual framework to address pharmacosex users' diverse needs. The suggested intervention components can be integrated in dedicated and comprehensive approaches in community and healthcare settings.
Theories to Understand Sexualized Drug Use
An important question to understand and prevent potential adverse impacts among people who engage in sexualized drug use is why people initiate and continue to engage in pharmacosex. To answer this question, we draw on a continuum perspective of chemsex use, a social cognition perspective on the interplay between reasoned and automatic processes in behavioral decisions, and critical components of effective self-control of behavior.
Continuum Perspective of Chemsex
Most definitions, views and understandings of substance use, including chemsex, reflect a binary perspective of problematic vs. non-problematic use (52). This binary perspective has major implications for support approaches, as it suggests that only problematic use requires support, and abstinence generally is the main focus of such support [cf. (53)]. This, however, obscures the importance of preventing chemsex behavior from becoming problematic, and the need for appropriate and tailored support for people who do not (yet) experience (major) adverse impacts of sexualized drug use. Support should thus be available for all chemsex users who require it, not solely for those whose use is considered “problematic” according to some sort of standard. Rather, it is important to effectively respond to self-perceived support needs of chemsex users (35).
To tailor support to the varying needs of chemsex users, a continuum-model of chemsex use has been proposed (14). This model describes chemsex use as a journey, with problematic chemsex as a possible but not inevitable outcome (14). A critical assumption of the journey model is that even though chemsex need not be problematic, it nevertheless carries the potential for harm. The journey model describes a spiraling process of chemsex use across six “stages,” from its onset toward severe health impact caused by chemsex use. In the earlier stages, some people who engage in sexualized drug use may not experience any harm as they can accommodate drug use in their life, while other users in those same stages may experience negative impacts. It is the self-perception of adverse impacts that is critical to whether chemsex is problematic or not, and this self-perceived impact underlies demand for support. The individual's evaluation of the impact of sexualized drug use on their everyday life (e.g., relational, professional, psychological and health aspects) is thus key in the understanding of the problematic character of sexualized drug use.
Reasoned and Automatic Processes in Sexualized Drug Use
Using drugs while understanding its risks, and possibly even experiencing adverse impacts, seems paradoxical, and in the past decades (problematic) substance use has been explained as a chronic brain disease (54, 55). From the perspective of this brain disease model of addiction (BDMA) (56, 57), a vulnerable brain gets taken over by addictive substances (58), making behavior progressively less voluntary and more compulsive. How these involuntary processes affect people's actions can be understood from the perspective of dual systems models of behavior.
Dual-systems models of decision-making and behavior distinguish between an automatic and a reasoned pathway to behavior [e.g., (59)]. The automatic pathway represents a fast, impulsive system, while the reasoned pathway reflects a slower, reasoned system. In the case of sexualized drug use, the automatic, impulsive system can be thought of as a representation of the influences stemming from a strong, compulsive, desire for the immediate experience that is enabled by sexualized drug use. The slower, reasoned system involved in sexualized drug use encompasses a person's deliberate consideration of its various positive and negative outcomes. Dual systems models suggest that behavior can result either from automatic processes or reasoned decisions, with the BDMA positing that continued substance use mostly reflects automatic processes. An alternative multi-systems model, however, proposes that substance use is not fully cue-driven and rigid, reflecting a loss of choice as the BDMA suggests, but results from a biased choice as drug use becomes more attractive (53). We propose that as people progress through their chemsex journey, automatic, cue-driven processes come to dominate substance use, through biases related to triggers in situations that people may frequently encounter (e.g., pharmacosex events), the formation of habits, and dependence or addiction to substances.
Self-Control Processes in Sexualized Drug Use
People may experience their sexualized drug use as problematic if automatic processes conflict with and override the reasoned decisions they want to make. For instance, when sexualized drug use comes to be experienced as dependence and interfering with other important life goals, and as exceeding self-control. Self-control is a cognitive process that refers to one's ability to forego immediate or momentary pleasures, which may have negative consequences, in favor of longer-term, more abstract benefits or the prevention of adverse impacts that may never occur (60). In the case of sexualized drug use, self-control refers to, for instance, foregoing the immediate excitation of combining sex and drugs to avoid potential negative impacts, including physical harm, legal sanctions, social disapproval or self-disappointment. Self-control encompasses the idea that how people react to and deal with temptations in the here and now is affected by their consideration of potential outcomes (61), which is enabled and limited by the human capacity for foresight and simulation (62).
Kotabe and Hofmann provide an overview of the challenges and processes involved in effective self-control (63). Their integrative self-control theory posits that behavioral enactment depends on how potential conflict between disparate action tendencies is resolved. Action tendencies can result from a higher order goal, such as to protect one's health, which is associated with reasoned, reflective decisions based on a consideration of long-term benefits (64–66). Alternatively, action tendencies can also result more automatically or impulsively from a current desire, a state of wanting (67), that directs a person toward immediate, rewarding stimuli such as sex or drugs. When this desire is incompatible with the higher-order goal, a desire-goal conflict occurs. This conflict may trigger a self-control effort, if people have the capacity and motivation for self-control (63). According to the integrative self-control theory, one's behavior ultimately depends on the relative strength of the desire and the self-control effort, assuming there are no constraints to enact either the higher-order goal or the desire.
Sexualized drug use can impact self-control in two ways: directly via a strong desire resulting from sexual arousal that can conflict with higher-order goals, as well as indirectly by substance related intoxication. This intoxication impairs an individual's motivation and capacity for self-control to pursue and attain their higher-order goals. When desires related to sexualized drug use conflict with higher order goals, people may actively want and try to control their sexualized substance use. Whether their self-control efforts are successful will depend on their motivation and capacity for self-control, which is likely affected by the use of substances. If people do not succeed in this self-control of sexualized drug use, they might look for help if they experience their behavior as problematic. In our conceptualization, seeking support reflects an individual's evaluation of their situation, including relational, professional, psychological and health aspects, and gaining access to support should not depend on any external definition of problematic pharmacosex.
Promoting Self-Control of Sexualized Drug Use
A critique of dominant perspectives of substance use and addiction, in particular the BDMA, is that this suggest that “there is no road back to controlled use or recovery” [cf. (53) p. 112]. However, it has been noted that many if not most people experiencing addiction recover (53), and the finding that most people relapse may be a misrepresentation based on overrelying on samples in addiction settings (68). We propose that effective self-control is an important leverage point for programs to appropriately support pharmacosex drug users across the sexualized substance use continuum.
Strengthening self-control can play a role in preventing initiation of use, supporting controlled use and harm reduction, as well as enabling discontinuation of use, depending on the individual's situation and wishes. Furthermore, self-control can be bolstered through various approaches, including (digital) self-help tools, peer-based support and professional care throughout the different stages of the chemsex journey. Here, we highlight the importance of approaches to support self-control that focus on enabling people to act on their (higher order) goals. This perspective complements established and controversial views of addiction control that emphasize the importance of continued abstinence to mitigate the overriding influence of substance-related desire [see (53)].
The starting point for our self-control perspective with sexualized substance use should be to assist users in clarifying their higher order goals. Subsequently, users should be encouraged to identify strategies to prevent that behaviors to achieve their higher-order goals are undermined by competing pharmacosex-related desires. Drawing on theories of goal-directed behavior, we propose a self-control approach to support sexualized drug use that distinguishes three critical components: goal setting, goal enactment, goal progress appraisal and goal adjustment (see Figure 1).
Goal Setting—Prioritizing
Goal setting theory (69, 70) is based on the observation that conscious human behavior is purposeful, and goal setting is an effective way of translating abstract wishes into concrete goals. Several goal characteristics have been found to affect the impact of goal setting on goal achievement. The technique of mental contrasting can help people to identify and set effective goals. When employing mental contrasting, people imagine the attainment of a desired future, and reflect on the present situation that obstructs this imagined future (71).
A goal should be specific, realistic and ambitious [e.g., (72)], and defined as a specific learning goal (73) that starts from the individual's personal situation. An ambitious goal generates more effort urging people to be committed to their goal (motivation). This commitment is reflected in the desirability and feasibility of the goal (71), where desirability refers to the importance of the goal (level of pleasantness when achieving it), and feasibility to the individual's self-efficacy and expectations (71, 72).
Applied to pharmacosex support, specific goals that people may want to achieve will differ, and goal setting will need to reflect individuals' priorities. Potential goals that require self-control in the context of sexualized drug use can, among others, be related to aspects of drug use (e.g., which substances and combinations to use/avoid, frequency of use), protecting the (sexual) health and wellbeing of oneself and others (e.g., reducing the risk of STI, ensuring consensual sex) and mitigating adverse social impacts (e.g., relationship conflicts, professional achievements). Once peoples' goals have been clarified, strategies can be put in place to optimize enactment.
Goal Enactment—Making a Plan, and Sticking to It
Goal enactment refers to the planning and execution of specific actions to achieve the higher-order goal that is as reflected in goal intentions (e.g., “I want to limit my sexualized drug use”). A goal intention is “the instruction that people give themselves to perform particular behaviors or to achieve certain desired outcomes” (74). Although considered a critical predictor of health behavior, research shows that people render their “good” intentions into action in only 53% of the time (75). This discrepancy between peoples' intentions and behavior is typically referred to as the intention-behavior gap, reflecting that forming goal intentions is necessary but insufficient for goal attainment (76, 77).
Goal intentions typically reflect peoples' broad aspirations, and it has been suggested that these need to be accompanied by more specific plans that specify concrete actions that need to be undertaken to achieve the goal (71, 76, 78, 79). Such specific plans can take the form of implementation intentions (78, 80), which complement goal intentions and take the form of if-then plans: if a certain situation arises, then I will act like this (e.g., “If I go to the next chemsex event, then I will only use the drugs I brought myself”). The if-then format requires considering two distinct aspects of the process of goal enactment: an effective behavior to achieve one's goal, and a suitable situation to initiate this behavior. A meta-analysis has shown that implementation intentions increase the likelihood that people enact their goal intentions, with effect sizes found to be medium to large (81).
Implementation intentions can be concerned with getting started with a particular behavior (e.g., action plans), or with navigating challenges along the path of behavior change (e.g., coping plans). The purpose of an action plan is to translate a goal intention into concrete and feasible actions. In the case of pharmacosex use, an action plan can refer to the behaviors that a person plans to enact at, for instance, the next chemsex event, that contributes to achieving the predefined goal. For instance, a goal could be to have safer sex during pharmacosex, which could be guided by the goal intention “at the next pharmacosex event I will have safer sex.” A related action plan to ensure attainment of the goal intention could be “I will make sure to take PrEP to protect myself during the next pharmacosex event.” Action planning has been used to promote health behavior change in different domains [see (82)] and a recent meta-analysis has also found the forming of plans to be effective in reducing substance use (83).
Coping plans are concerned with overcoming specific barriers to (continued) action that may interfere with goal directed behavior (76), such as distractions and challenges that require effort or persistence. Effective coping planning requires experience and increases over time. In the context of pharmacosex, coping plans could, for instance, be related to preparing oneself to deal with challenging circumstances during a pharmacosex event, such as “I will set an alarm on my phone to remind me to take PrEP during the pharmacosex event” to prevent forgetting to take PrEP, for instance due to a loss of sense of time. Table 1 gives further examples of goal intentions, action plans and coping plans, related directly to the self-control of drug use, as well as the self-control of behaviors to mitigate sexual health risks and potential adverse social impacts of pharmacosex use.
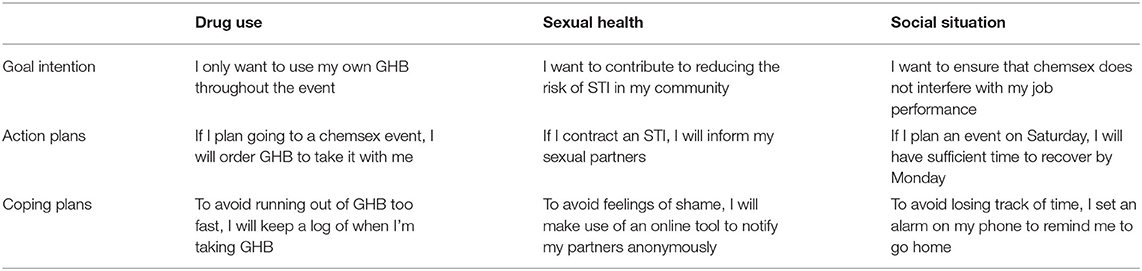
Table 1. Examples of goal intentions, action plans and coping plans for the self-control of sexualized drug use and to mitigate potential health and social impacts.
Goal Progress Appraisal and Adjustment—Comparing, Evaluating, and Adapting
Goal appraisal entails that people compare their behavior to the goal they had set, and evaluate whether they have achieved the goal or not. The outcome of this comparison may result in goal adjustment, reflecting feedback loops that play a critical role in self-control [see (84)]. For instance, some people intend to change their pharmacosex behavior toward a healthier alternative (e.g., not engaging in pharmacosex at all), yet find that they did not behave as planned. This experience of failure to achieve one's goal is a frequent challenge for attempts to change behavior in many health domains, and may contribute to abandoning the goal (e.g., “I am not going to succeed to stop my pharmacosex”) (76). Alternatively, failure to achieve one's goal may also constitute a learning experience for people to adjust their behavior change goal in ways that are more realistic and achievable (e.g., “I am going to engage in pharmacosex less frequently”). Furthermore, action and coping plans may be adjusted to better fit the situational challenges that people encounter (i.e., change what did not work). If, in contrast, the intended behavior has been achieved, more ambitious behavior change goals may be set (e.g., “I want to reduce my pharmacosex engagement from weekly to monthly”), and action and coping plans can be adjusted to enable the achievement of these more ambitious goals (i.e., strengthen what works).
Goal adjustment is not so much the final step in the self-control process, as it is the start of a new goal/action loop (see Figure 1). When goals and action/coping plans have been adjusted, the next loop in the iterative self-control process starts. Goal/action loops enable repeated goal adjustment and may continue until the individual reaches the point where they feel they have achieved their goal or (temporarily) abandon the goal and possibly restart a change process in the future. The process of goal appraisal and adjustment can occur following as well as during engagement in pharmacosex, and draws on processes of action control. Action control entails that a behavior is evaluated against a behavioral standard (85), which can occur during a pharmacosex event (i.e., concurrent action control), and reflecting on the implications of experiences for future events (i.e., prospective action control).
Self-Control of Sexualized Drug Use in Practice
We propose that the successful promotion of self-control in pharmacosex need to encompass approaches to support goal setting, goal enactment, and goal progress appraisal and adjustment. Such approaches can strengthen support for pharmacosex provided by professionals or peers, as well as through self-help. In line with prevailing counseling approaches (i.e., motivational interviewing), in person and online support for individuals or small groups of people who engage in pharmacosex can contribute to setting behavioral goals for the self-control of pharmacosex, and formulating action/coping plans to achieve these goals. Furthermore, counseling also offers opportunities to support goal adjustment strategies. For instance, a person who engaged in pharmacosex may recall experiences during a pharmacosex event, including if they had a particular goal and plan, and whether they behaved accordingly. If the person behaved as planned and achieved their goal, this may result in a positive experience, contribute to a sense of self-efficacy, strengthen self-control, and, consequently, reduce the risk of harm. Moreover, this increased self-control may contribute to a positive feedback loop such that people set more challenging subsequent goals to manage their engagement in pharmacosex, and adjust their action/coping plans to achieve these goals. This process can be repeated until the person achieves their ultimate goal, which may evolve over the course of the change process.
While counseling approaches hold much promise to support the self-control of engagement in pharmacosex, this type of support is disconnected from actual pharmacosex events, and hence limited to prospective action control. Use of smartphone applications may, in addition, enable concurrent action control. Drawing on promising developments in digital health promotion, including in healthcare settings (86, 87), smartphone applications can enable real-time self-control of engagement in pharmacosex events (49).
Discussion
In this paper, we set out a conceptual perspective to better understand pharmacosex, and guide intervention to support people who engage in pharmacosex use. Conceptual principles comprise a continuum perspective of chemsex, the altering weight of automatic and reasoned processes in behavioral decision making throughout this continuum, and self-control as a self-regulating strategy to overcome potential negative impacts of sexualized drug use. We acknowledge that this conceptual framework does not fully explain the complexity of factors that may influence people's pharmacosex use, including influential life-events (e.g., adverse childhood events, syndemics, trauma), social factors (e.g., peer norms and pressure, stigma and shame), as well as structural factors (e.g., barriers to accessing care, limited expertise of healthcare professionals) (88). Tackling these broader issues complements our primary focus on self-control capacity, and will require comprehensive programs that also include drug treatment, HIV/STI prevention and mental health care and support.
This conceptual self-control framework, as well as its translation into specific intervention components, may guide people toward improvement and self-control of their sexualized drug use, including the reduction of its negative impacts. This strengthening of one's ability for self-control can be accomplished via personal or digital support, and ideally continues after completion of an empowering support trajectory. This strengthened self-control competency can help the individual to effectively manage their pharmacosex use independently and avoid unwanted progress in their future sexualized drug use journey. This may comprise prevention of the initiation of sexualized drug use, facilitating and maintaining controlled use and harm reduction, and enabling discontinuation of use. Importantly, experiences that increase self-control competency may enable “impulsive” users to become “controlled” users, who can effectively reduce pharmacosex-related harms (31).
We propose that intervention components to support people who engage in pharmacosex can be integrated in dedicated and comprehensive approaches in community and healthcare settings, via personal support or digital self-help. In all these settings and approaches, self-control can help users to clarify their personal behavioral goals and objectives and enable them to achieve these. In order to translate the conceptual self-control perspective into practice, we point out three critical elements of the self-control process that need to be incorporated in effective interventions: goal setting, goal enactment, and goal progress appraisal and adjustment. These three elements reinforce each other via recurrent feedback loops, whereby the successful achievement of a goal can be the starting point of a next change cycle. This process continues until the individual reaches their ultimate goal, which may evolve throughout the self-control process. This self-control approach complements drug support services that tend to focus on abstinence and offers additional tools to focus on harm reduction.
Conclusion
With this self-control framework, we aim to provide guiding principles for the improvement of prevention, and effective support and care programs and interventions. To achieve this overarching objective, specific intervention and intervention components derived from the conceptual framework should be developed and tested for their effectiveness in real-life settings. After all, the ultimate goal of this conceptual self-control framework and inferred intervention is to optimize the support and care for people who experience loss of self-control during their sexualized drug use.
Author Contributions
TP and JW collaborated on the theoretical conceptualization and translation into practical intervention components. EF contributed by reviewing and providing valuable feedback throughout the process of development of the conceptual framework. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Tim Lebacq for the graphic work of the conceptual framework, as presented in Figure 1.
References
2. Kirby T, Thornber-Dunwell M. High-risk drug practices tighten grip on London gay scene. Lancet. UK Government (2013) 381:101–2. doi: 10.1016/S0140-6736(13)60032-X
3. Stuart D. Sexualised drug use by MSM: background, current status and response. HIV Nurs. (2013) 13:6–10. https://www.hivnursing.net/index.php/hiv/issue/view/36/36
4. Bourne A, Reid D, Hickson F, Torres-Rueda S, Steinberg P, Weatherburn P. “Chemsex” and harm reduction need among gay men in South London. Int J Drug Policy. (2015) 26:1171–6. doi: 10.1016/j.drugpo.2015.07.013
5. Schmidt AJ, Bourne A, Weatherburn P, Reid D, Marcus U, Hickson F. Illicit drug use among gay and bisexual men in 44 cities: findings from the European MSM internet survey (EMIS). Int J Drug Policy. (2016) 38:4–12. doi: 10.1016/j.drugpo.2016.09.007
6. Evers YJ, Hoebe CJPA, Dukers-Muijrers NHTM, Kampman CJG, Kuizenga-Wessel S, Shilue D, et al. Sexual, addiction and mental health care needs among men who have sex with men practicing chemsex – a cross-sectional study in the Netherlands. Prev Med Rep. (2020) 18:101074. doi: 10.1016/j.pmedr.2020.101074
7. Edmundson C, Heinsbroek E, Glass R, Hope V, Mohammed H, White M, et al. Sexualised drug use in the United Kingdom (UK): a review of the literature. Int J Drug Policy. (2018) 55:131–48. doi: 10.1016/j.drugpo.2018.02.002
8. Stuart D. A chemsex crucible: the context and the controversy. J Fam Plan Reprod Heal Care. (2016) 42:295–6. doi: 10.1136/jfprhc-2016-101603
9. Evers YJ, Dukers-Muijrers NHTM, Kampman CJG, van Liere GAFS, Hautvast JLA, Koedijk FDH, et al. Prevalence of drug use during sex among swingers and perceived benefits and risks - a cross-sectional internet survey in the Netherlands. Sex Transm Infect. (2020) 96:40–6. doi: 10.1136/sextrans-2019-054113
10. Moyle L, Dymock A, Aldridge A, Mechen B. Reprint of: pharmacosex: reimagining sex, drugs and enhancement. Int J Drug Policy. (2021) 95:103282. doi: 10.1016/j.drugpo.2021.103282
11. Bourne A, Weatherburn P. Substance use among men who have sex with men: patterns, motivations, impacts and intervention development need. Sex Transm Infect. (2017) 93:342–46. doi: 10.1136/sextrans-2016-052674
12. Milhet M, Shah J, Madesclaire T, Gaissad L. Chemsex experiences: narratives of pleasure. Drugs and Alcohol Today. (2019) 19:11–22. doi: 10.1108/DAT-09-2018-0043
13. Arends RM, van den Heuvel TJ, Foeken-Verwoert EGJ, Grintjes KJT, Keizer HJG, Schene AH, et al. Sex, drugs, and impulse regulation: a perspective on reducing transmission risk behavior and improving mental health among MSM Living with HIV. Front Psychol. (2020) 0:1005. doi: 10.3389/fpsyg.2020.01005
14. Platteau T, Pebody R, Dunbar N, Lebacq T, Collins B. The problematic chemsex journey: a resource for prevention and harm reduction. Drugs and Alcohol Today. (2019) 19:49–54. doi: 10.1108/DAT-11-2018-0066
15. Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet. (2007) 369:1047–53. doi: 10.1016/S0140-6736(07)60464-4
16. Boileau-Falardeau M, Contreras G, Gariépy G, Laprise C. Patterns and motivations of polysubstance use: a rapid review of the qualitative evidence. Health Promot Chronic Dis Prev Can. (2022) 42:47–59. doi: 10.24095/hpcdp.42.2.01
17. Bourne A, Reid D, Hickson F, Torres S, Weatherburn RP. The Chemsex Study: Drug Use in Sexual Settings Among Gay and Bisexual Men in Lambeth, Southwark & Lewisham. London: Public Health England (2014).
18. Sewell J, Cambiano V, Miltz A, Speakman A, Lampe FC, Phillips A, et al. Changes in recreational drug use, drug use associated with chemsex, and HIV-related behaviours, among HIV-negative men who have sex with men in London and Brighton, 2013–2016. Sex Transm Infect. (2018) 94:494–501. doi: 10.1136/sextrans-2017-053439
19. Pakianathan M, Whittaker W, Lee M, Avery J, Green S, Nathan B, et al. Chemsex and new HIV diagnosis in gay, bisexual and other men who have sex with men attending sexual health clinics. HIV Med. (2018) 19:485–90. doi: 10.1111/hiv.12629
20. Smith GW, Farrell M, Bunting BP, Houston JE, Shevlin M. Patterns of polydrug use in Great Britain: findings from a national household population survey. Drug Alcohol Depend. (2011) 113:222–8. doi: 10.1016/j.drugalcdep.2010.08.010
21. Hegazi A, Lee MJ, Whittaker W, Green S, Simms R, Cutts R, et al. Chemsex and the city: sexualised substance use in gay bisexual and other men who have sex with men attending sexual health clinics. Int J Std Aids. (2017) 28:362–66. doi: 10.1177/0956462416651229
22. Maxwell S, Shahmanesh M, Gafos M. Chemsex behaviours among men who have sex with men: a systematic review of the literature. Int J Drug Policy. (2019) 63:74–89. doi: 10.1016/j.drugpo.2018.11.014
23. Glynn RW, Byrne N, O'Dea S, Shanley A, Codd M, Keenan E, et al. Chemsex, risk behaviours and sexually transmitted infections among men who have sex with men in Dublin, Ireland. Int J Drug Policy. (2018) 52:9–15. doi: 10.1016/j.drugpo.2017.10.008
24. Kenyon C, Wouters K, Platteau T, Buyze J, Florence E. Increases in condomless chemsex associated with HIV acquisition in MSM but not heterosexuals attending a HIV testing center in Antwerp, Belgium. AIDS Res Ther. (2018) 15:14. doi: 10.1186/s12981-018-0201-3
25. Drückler S, van Rooijen MS, de Vries HJC. Chemsex among men who have sex with men: a sexualized drug use survey among clients of the sexually transmitted infection outpatient clinic and users of a gay dating app in Amsterdam, the Netherlands. Sex Transm Dis. (2018) 45:325–31. doi: 10.1097/OLQ.0000000000000753
26. Stevens O, Moncrieff M, Gafos M. Chemsex-related drug use and its association with health outcomes in men who have sex with men: a cross-sectional analysis of Antidote clinic service data. Sex Transm Infect. (2020) 96:124–30. doi: 10.1136/sextrans-2019-054040
27. Pufall EL, Kall M, Shahmanesh M, Nardone A, Gilson R, Delpech V, et al. Sexualized drug use (‘chemsex') and high-risk sexual behaviours in HIV-positive men who have sex with men. HIV Med. (2018) 19:261–70. doi: 10.1111/hiv.12574
28. Kohli M, Hickson F, Free C, Reid D, Weatherburn P. Cross-sectional analysis of chemsex drug use and gonorrhoea diagnosis among men who have sex with men in the UK. Sex Health. (2019) 16:464–72. doi: 10.1071/SH18159
29. Drückler S, Speulman J, van Rooijen M, C De Vries HJ, De Vries HJC. Sexual consent and chemsex: a quantitative study on sexualised drug use and non-consensual sex among men who have sex with men in Amsterdam, the Netherlands. Sex Transm Infect. (2021) 97:268–75. doi: 10.1136/sextrans-2020-054840
30. Prestage G, Hammoud M, Jin F, Degenhardt L, Bourne A, Maher L. Mental health, drug use and sexual risk behavior among gay and bisexual men. Int J Drug Policy. (2018) 55:169–79. doi: 10.1016/j.drugpo.2018.01.020
31. Tomkins A, George R, Kliner M. Sexualised drug taking among men who have sex with men: a systematic review. Perspect Public Health. (2019) 139:23–33. doi: 10.1177/1757913918778872
32. Íncera-Fernández D, Gámez-Guadix M, Moreno-Guillén S. Mental health symptoms associated with sexualized drug use (Chemsex) among men who have sex with men: a systematic review. Int J Environ Res Public Health. (2021) 18:13299. doi: 10.3390/ijerph182413299
33. Hibbert M, Germain J, Brett C, Van Hout M, Hope V, Porcellato L. Service provision and barriers to care for men who have sex with men engaging in chemsex and sexualised drug use in England. Int J Drug Policy. (2021) 92:103090. doi: 10.1016/j.drugpo.2020.103090
34. Tomkins A, Vivancos R, Ward C, Kliner M. How can those engaging in chemsex best be supported? An online survey to gain intelligence in Greater Manchester. Int J Std Aids. (2018) 29:128–34. doi: 10.1177/0956462417719643
35. Herrijgers C, Poels K, Vandebosch H, Platteau T, van Lankveld J, Florence E. Harm reduction practices and needs in a belgian chemsex context: Findings from a qualitative study. Int J Environ Res Public Health. (2020) 17:1–18. doi: 10.3390/ijerph17239081
36. Bakker I, Knoops L. Towards a continuum of care concerning chemsex issues. Sex Health. (2018) 15:173–5. doi: 10.1071/SH17139
37. Moncrieff M. Towards a supportive policy and commissioning environment for chemsex in England. Sex Health. (2018) 15:170–2. doi: 10.1071/SH17188
38. Stardust Z, Kolstee J, Joksic S, Gray J, Hannan S. A community-led, harm-reduction approach to chemsex: Case study from Australia's largest gay city. Sex Health. (2018) 15:179–81. doi: 10.1071/SH17145
39. Reback CJ, Fletcher JB, Swendeman DA, Metzner M. Theory-Based text-messaging to reduce methamphetamine use and HIV sexual risk behaviors among men who have sex with men: automated unidirectional delivery outperforms bidirectional peer interactive delivery. AIDS Behav. (2019) 23:37–47. doi: 10.1007/s10461-018-2225-z
40. Carrico AW, Nation A, Gómez W, Dilworth SE, Johnson MO, Moskowitz JT, et al. Pilot trial of an expressive writing intervention with HIV-positive methamphetamine-using men who have sex with men. Psychol Addict Behav. (2015) 29:277–82. doi: 10.1037/adb0000031
41. Mausbach BT, Semple SJ, Strathdee SA, Zians J, Patterson TL. Efficacy of a behavioral intervention for increasing safer sex behaviors in HIV-positive MSM methamphetamine users: results from the EDGE study. Drug Alcohol Depend. (2007) 87:249–57. doi: 10.1016/j.drugalcdep.2006.08.026
42. Mimiaga MJ, Pantalone DW, Biello KB, Hughto JMW, Frank J, O'Cleirigh C, et al. An initial randomized controlled trial of behavioral activation for treatment of concurrent crystal methamphetamine dependence and sexual risk for HIV acquisition among men who have sex with men. AIDS Care. (2019) 31:1083–95. doi: 10.1080/09540121.2019.1595518
43. Santos GM, Coffin PO, Vittinghoff E, DeMicco E, Das M, Matheson T, et al. Substance use and drinking outcomes in personalized cognitive counseling randomized trial for episodic substance-using men who have sex with men. Drug Alcohol Depend. (2014) 138:234–9. doi: 10.1016/j.drugalcdep.2014.02.015
44. Parsons JT, John SA, Millar BM, Starks TJ. Testing the efficacy of combined motivational interviewing and cognitive behavioral skills training to reduce methamphetamine use and improve HIV medication adherence among HIV-positive gay and bisexual men. AIDS Behav. (2018) 22:2674. doi: 10.1007/s10461-018-2086-5
45. Donnadieu-Rigole H, Peyrière H, Benyamina A, Karila L. Complications related to sexualized drug use: what can we learn from literature? Front Neurosci. (2020) 14:1240. doi: 10.3389/fnins.2020.548704
46. Coffin P, Santos G, Hern J, Vittinghoff E, Walker J, Matheson T, et al. Effects of mirtazapine for methamphetamine use disorder among cisgender men and transgender women who have sex with men: a placebo-controlled randomized clinical trial. JAMA Psychiatry. (2020) 77:246–55. doi: 10.1001/jamapsychiatry.2019.3655
47. Choi E, Chau P, Wong W, Kowk J, Choi K, Chow E. Developing and testing of an interactive internet-based intervention to reduce sexual harm of sexualised drug use ('chemsex') among men who have sex with men in Hong Kong: a study protocol for a randomised controlled trial. BMC Public Health. (2021) 21:713. doi: 10.1186/s12889-021-10742-8
48. Reback CJ, Fletcher JB, Mata RP. A theory-based mHealth intervention (Getting Off) for methamphetamine-using men who have sex with men: protocol for a randomized controlled trial. JMIR Res Protoc. (2021) 10:e22572. doi: 10.2196/22572
49. Platteau T, Herrijgers C, De Wit J. Digital chemsex support and care: the potential of just-in-time adaptive interventions. Int J Drug Policy. (2020) 85:102927. doi: 10.1016/j.drugpo.2020.102927
50. Graf N, Dichtl A, Deimel D, Sander D, Stöver H. Chemsex among men who have sex with men in Germany: motives, consequences and the response of the support system. Sex Health. (2018) 15:151–6. doi: 10.1071/SH17142
51. Kok G, Peters LWH, Ruiter RAC. Planning theory- and evidence-based behavior change interventions: a conceptual review of the intervention mapping protocol. Psicol Reflex Crit. (2017) 30:1–13. doi: 10.1186/s41155-017-0072-x
52. Troya J, Martínez de Gándara A, Ryan P, Cuevas G, Pardo V. Mephedrone and chemsex: when it stops being a party and becomes a fatal problem. Int J Std Aids. (2019) 30:1028–30. doi: 10.1177/0956462419857004
53. Wiers RW, Verschure P. Curing the broken brain model of addiction: neurorehabilitation from a systems perspective. Addict Behav. (2021) 112:106602 doi: 10.1016/j.addbeh.2020.106602
54. Leshner AI. Addiction is a brain disease, and it matters. Science (80-). (1997) 278:45–7. doi: 10.1126/science.278.5335.45
55. Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. NEJMra. (2016) 374:363–71. doi: 10.1056/NEJMra1511480
56. Hall W, Carter A, Forlini C. Brain disease model of addiction: misplaced priorities? Lancet Psychiatry. (2015) 2:867. doi: 10.1016/S2215-0366(15)00417-4
57. Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res Theory. (2017) 26:249–55. doi: 10.1080/16066359.2017.1399659
58. Nesse RM, Berridge KC. Psychoactive drug use in evolutionary perspective. Science (80-). (1997) 278:63–6. doi: 10.1126/science.278.5335.63
59. Strack F, Deutsch R, Bühler A, Gawronski B, Kruglanski A, Levy R, et al. Reflective and impulsive determinants of social behavior. Personal Soc Psychol Rev. (2004) 8:220–47. doi: 10.1207/s15327957pspr0803_1
60. de Ridder DTD, de Wit JBF. Self-regulation in health behavior. Self Reg Heal Behav. (2006) 1–247. doi: 10.1002/9780470713150.ch1
61. Fujita K. On conceptualizing self-control as more than the effortful inhibition of impulses. Pers Soc Psychol Rev. (2011) 15:352–66. doi: 10.1177/1088868311411165
62. Baumeister RF, Masicampo EJ, Vohs KD. Do conscious thoughts cause behavior? Annu Rev Psychol. (2011) 62:331–61. doi: 10.1146/annurev.psych.093008.131126
63. Kotabe H, Hofmann W. On integrating the components of self-control. Perspect Psychol Sci. (2015) 10:618–38. doi: 10.1177/1745691615593382
64. Eyal T, Fishbach A. Do global and local systems feel different? Psychol Inq. (2010) 21:213–5. doi: 10.1080/1047840X.2010.503184
65. Hofmann W, Fisher RR. How guilt and pride shape subsequent self-control. Soc Psychol Personal Sci. (2012) 3:682–90. doi: 10.1177/1948550611435136
66. Hofmann W, Kotabe H, Luhmann M. The spoiled pleasure of giving in to temptation. Motiv Emot. (2013) 37:733–42. doi: 10.1007/s11031-013-9355-4
67. Berridge KC, Robinson TE, Aldridge JW. Dissecting components of reward: ‘liking', ‘wanting', and learning. Curr Opin Pharmacol. (2009) 9:65. doi: 10.1016/j.coph.2008.12.014
68. Baumeister RF. Addiction, cigarette smoking, and voluntary control of action: do cigarette smokers lose their free will? Addict Behav Rep. (2017) 5:67–84. doi: 10.1016/j.abrep.2017.01.003
69. Locke EA, Latham GP. Goal Setting: A Motivational Technique That Works!. Hoboken, NJ: Prentice-Hall (1984). 193 p.
70. Locke EA, Latham GP, Smith KJ, Wood RE. A Theory of Goal Setting & Task Performance. Hoboken, NJ: Prentice-Hall. (1990) 413 p.
71. Oettingen G, Gollwitzer P. Strategies of setting and implementing goals : mental contrasting and implementation intentions. In: Maddux JE, Tangney J, editors. Social Psychological Foundations of Clinical Psychology. New York, NY: The Guilford Press. (2010) p. 114–35.
72. Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation: a 35-year odyssey. Am Psychol. (2002) 57:705–17. doi: 10.1037/0003-066X.57.9.705
73. Winters D, Latham GP. The effect of learning versus outcome goals on a simple versus a complex task. Group Organ Manag. (1996) 21:236–50. doi: 10.1177/1059601196212007
75. Sheeran P, Trafimow D, Finlay K, Norman P. Evidence that the type of person affects the strength of the perceived behavioural control-intention relationship. Br J Soc Psychol. (2002) 41:253–70. doi: 10.1348/014466602760060129
76. Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention-behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol Heal. (2005) 20:143–60. doi: 10.1080/08870440512331317670
77. Sheeran P, Webb T. The intention–behavior gap. Soc Personal Psychol Compass. (2016) 10:503–18. doi: 10.1111/spc3.12265
78. Gollwitzer PM, Sheeran P. Implementation intentions: strong effects of simple plans. Am Psychol. (1999) 54:493–503. doi: 10.1037/0003-066X.54.7.493
79. Schwieger Gallo I, Gollwitzer PM. Implementation intentions: a look back at fifteen years of progress. Psicothema. (2007) 19:37–42. https://www.researchgate.net/publication/6509302_Implementation_Intentions_A_Look_Back_at_Fifteen_Years_of_Progress
80. Gollwitzer PM. Goal achievement: the role of intentions. Eur Rev Soc Psychol. (1993) 4:141–85. doi: 10.1080/14792779343000059
81. Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol. (2006) 38:69–119. doi: 10.1016/S0065-2601(06)38002-1
82. de Ridder D, Adriaanse M, Fujita K. Handbook of Self-Control in Health and Wellbeing. Routledge: Abingdon-on-Thames (2018) 542 p.
83. Malaguti A, Ciocanel O, Sania F, Dillond J, Eriksen A, Power K. Effectiveness of the use of implementation intentions on reduction of substance use: a meta-analysis. Drug Alcohol Depend. (2020) 214:108120. doi: 10.1016/j.drugalcdep.2020.108120
84. Carver CS, Scheier MF. On the Self-Regulation of Behavior. Cambridge: Cambridge University Press. (1998) 460 p.
85. Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. (2008) 57:1–29. doi: 10.1111/j.1464-0597.2007.00325.x
86. Fiordelli M, Diviani N, Schulz PJ. Mapping mhealth research: a decade of evolution. J Med Int Res. (2013) 15:e95. doi: 10.2196/jmir.2430
87. Steinhubl SR, Muse ED, Topol EJ. The emerging field of mobile health. Sci Transl Med. (2015) 7:283rv3. doi: 10.1126/scitranslmed.aaa3487
Keywords: pharmacosex, chemsex, conceptual framework, self-control, care and support
Citation: Platteau T, Florence E and de Wit JBF (2022) Self-Control as Conceptual Framework to Understand and Support People Who Use Drugs During Sex. Front. Public Health 10:894415. doi: 10.3389/fpubh.2022.894415
Received: 11 March 2022; Accepted: 24 May 2022;
Published: 15 June 2022.
Edited by:
Abhishek Ghosh, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
Aditya Somani, All India Institute of Medical Sciences Raipur, IndiaSimona Zaami, University of Rome “Sapienza”, Italy
Copyright © 2022 Platteau, Florence and de Wit. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tom Platteau, dHBsYXR0ZWF1QGl0Zy5iZQ==
 Tom Platteau
Tom Platteau Eric Florence
Eric Florence John B. F. de Wit
John B. F. de Wit