
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 13 May 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.872220
 Chin-Wei Kuo1,2†
Chin-Wei Kuo1,2† Chung-Fu Lin1†
Chung-Fu Lin1† Chuan-Yu Chen3,4†
Chuan-Yu Chen3,4† Ru-Hsueh Wang3
Ru-Hsueh Wang3 Chieh-Ying Chou3
Chieh-Ying Chou3 Hsiang-Ju Cheng3
Hsiang-Ju Cheng3 Jin-Shang Wu3
Jin-Shang Wu3 Chang-Wen Chen1
Chang-Wen Chen1 Chi-Chang Shieh2
Chi-Chang Shieh2 Tsung Yu5*
Tsung Yu5*Background: Smoking behavior differs between the sexes. Weight control is one of the main reasons leading to tobacco abuse in women but not in men. Studies on the predictive factors of cessation failure between sexes are scarce. This study is aim to investigate whether there are sex differences in the effect of weight gain on smoking cessation rate.
Methods: Participants in the smoking-cessation program at a Medical Center in Taiwan between 2018 and 2019 were included. Details of age, sex, comorbidities, depression screening, nicotine dependence, body weight, and cessation medications of the participants were collected. The participants were classified based on their sex, and multivariable logistic regression analyses were conducted. Multivariable logistic regression analyses were performed for sensitivity analysis after stratifying the participants according to their weight loss (weight loss ≥ 1.5 kg and weight loss ≥ 3.0 kg).
Results: A total of 1,475 participants were included. The body-weight gain in women was associated with failed abstinence (adjusted odds ratio (OR): 3.10, 95% CI: 1.10–9.04). In contrast, body-weight gain in men was associated with successful 6-month prolonged abstinence (adjusted OR: 0.77, 95% CI: 0.61–0.98). The adjusted ORs for any body-weight loss, body-weight loss ≥1.5 kg, and body-weight loss ≥3.0 kg were 0.28 (95% CI: 0.09–0.88), 0.14 (95% CI: 0.03–0.55), and 0.03 (95% CI: 0.01–0.42), respectively.
Conclusion: Body-weight gain in women during a hospital-based smoking-cessation program is associated with abstinence failure. Further multicenter studies, including participants of different races and cultural backgrounds, are warranted.
Cigarette smoking is a widespread unhealthy behavior that leads to several diseases and premature death (1). Although the tobacco control policy reduced the worldwide prevalence of smoking, 9.5% of women were found to be active smokers in 2015 (2) indicating that women's smoking is an important public issue. Men and women smokers vary significantly in their physiological, cultural, and behavioral factors (3). For example, most men smoke for the pleasure and enjoyment of smoking, while women smoke to relieve stress and control their body weight (BW) (4, 5). Smoking activates dopamine in the ventral striatum of men, and the discrete subregion of the dorsal putamen of women (6). Plasma and saliva cortisol levels have predicted smoking relapse in men but not in women (7). Although the prevalence of women smokers is much lesser than that of men smokers (2), the former are more likely to get smoking attributable diseases, even under controlled tobacco exposure (8, 9) In addition, smoking during pregnancy is associated with poor birth outcomes (10) and early onset of smoking in children (11).
Abstinence is the most important way to reduce the harm caused by smoking. Studies have shown that women face greater difficulty in quitting smoking as compared with men (12). One plausible reason is that women are more likely to continue smoking for controlling their BW. Body-image challenges motivate young women to smoke (13), and smoking cessation is often associated with an increase in BW. A previous meta-analysis inferred that after 12 months of abstinence from smoking, 84% of individuals gained 4 to 5 kg mean BW (14). However, during the cessation program smoking abstinence-related negative mood and greater motivation to relieve distress from withdrawal symptoms were reported more in women than in men (15), suggesting that the barriers to smoking cessation differ between the sexes.
To the best of our knowledge, studies on the predictive factors of cessation failure between different sexes are scarce. In this study, we hypothesized that the predicted factor of failed smoking-cessation differs between the sexes and that the BW gained by women during the cessation program is associated with failed abstinence. Therefore, we performed a retrospective cohort study by using a well-registered, real-world in-hospital cessation program data from a Medical Center in the southern Taiwan to verify the hypothesis.
We conducted a retrospective cohort study by collecting data from smokers who participated in smoking-cessation programs at the National Cheng Kung University Hospital (NCKUH) from 1 January 2018 to 30 November 2019. Participants aged ≥ 20 years and who received one or more cessation counseling in the program were included. The exclusion criteria were: (1) missing information on their demographics, smoking history, and follow-up smoking status, and (2) lost to follow-up when assessing the 6-month prolonged smoking abstinence. We checked every missing data and tried to fill them by crosslinking the electronic medical record and smoking cessation databank of NCKUH before excluding the participants. The first program was selected to analyze if the subjects participated in two or more cessation programs during the study period. Before commencing, the study was approved by the Institutional Review Board of NCKUH (ID number: B-ER-110-126).
We collected the participants' clinical information, including age, sex, marital status, underlying comorbidities (cardiovascular disease, cancer, cerebral vascular disease, diabetes mellitus, hypertension, liver disease, respiratory system disease, and renal disease), BW on each return to the clinic, site of cessation program initiation, smoking cessation history, Patient Health Questionnaire-2 (PHQ-2) depression screening test score (16, 17), Fagerstrom Test for Nicotine Dependence (FTND) score (18), type and duration of received cessation medication, and 6-month prolonged smoking abstinence of the participant from the electronic medical record and databank of tobacco-cessation of NCKUH. PHQ-2 is a 4-level, 2-item screening tool for major depressive disorder (MDD). The screening accuracy of the Chinese version of PHQ-2 had been validated. With a PHQ-2 score ≥ 2, the sensitivity and specificity of MDD are 0.88 and 0.82, respectively (17). The Fagerström Test for Nicotine Dependence (FTND) is a self-reported instrument that measures dependence through physiological and behavioral symptoms (19). FTND score ≥ 6 is defined as high-nicotine dependence (19). The outcome of this study was a 6-month prolonged abstinence rate, which is referred to as the rate of participants' sustained abstinence after the initial grace period until the 6-month follow-up (20). The grace period is 12 weeks in this study.
In 2002, the Taiwan Bureau of Health Promotion launched a nationwide smoking-cessation program. The participating institutions received grant support to implement the program and record normative individual-level registration data (21). Active smokers who visited our hospital would be referred to the tobacco-cessation team, which consisted of government-certified health education nurses, a chest physician, and a family physician. A 12-week tobacco-cessation program would be initiated under the agreement of participants. The cessation program could be initiated from in-hospital or out-patient services. The hospital-initiated cessation program followed the Ottawa model (22) and the clinical smoking cessation services guidelines of Taiwan (23), which were adapted from the published guidelines from the Department of Health and Human Services of the United States with updates (24) providing health education, behavioral intervention, and cessation medications. The out-patient cessation services were performed by health education nurses and medical doctors, giving the individual cessation counseling and medication. On the first visit of each participant, health education nurses recorded the participants' smoking history, PHQ-2 score, and FTND score (18). All the participants were recommended to receive pharmacotherapy for smoking cessation. Pharmacotherapy included nicotine replacement therapy (NRT; nicotine patch, nicotine gum, and nicotine inhaler) and non-NRT (varenicline and bupropion). The choice of medication was based on the preferences and contraindications of the participant. The dose of medication determined the participants' daily cigarette consumption (25–27). Participants were asked to return to the smoking cessation clinic every 1 or 2 weeks for the first 4 weeks, and every 3 to 4 weeks in the following 8 weeks. Upon the return, the smoking status, BW, and compliance with cessation medications would be recorded. The BW of the participants was measured using the same electric weighing scale on every visit. The status of the 6-month prolonged smoking abstinence was assessed via telephonic interviews. Participants who refused for telephone interviews or cannot be contacted were recorded as lost to follow-ups.
The characteristics of both the sexes were compared using a chi-square test or Fisher's exact test and are presented as numbers and percentages. The characteristics affecting the failure of smoking abstinence during the 6-months were analyzed by performing univariable and multivariable logistic regression analyses. Firth logistic regression was conducted for the analysis of binary outcomes with small samples. Characteristics include age (≥ 65 vs. < 65 years), sex (men vs. women), number of comorbidities (≥ 2 vs. < 2), PHQ-2 (≥ 2 vs. < 2), FTND score (≥ 6 vs. < 6), ever quit smoking for 6 months (yes vs. no), BW gain (yes vs. no), and cessation medications (only varenicline, only bupropion, only NRT, both NRT, and non-NRT vs. no use or use < 4 weeks) were considered covariables for the regression model. Because the cessation medications yield better outcomes when used for 4 weeks or longer (28), participants using these medications for < 4 weeks and those not using them were placed under the same category. For participants who received cessation medication for ≥ 4 weeks, they would be categorized into “only varenicline”, “only bupropion”, and “only NRT”. Whether participants received NRT and non-NRT concurrently or separately, they were classified into “both NRT and non-NRT groups. The association between covariable and failure of smoking abstinence for 6 months was presented using odds ratios (ORs) and 95% CIs. Two-sided P-values of < 0.05 were considered statistically significant. All the statistical analyses were conducted using the SAS software (version 9.4, SAS Institute, Cary, NC, USA).
To test the robustness of the effect of BW changes on smoking abstinence in different sexes, a multivariable logistic regression analysis was performed by changing the covariable from BW gain to BW loss. We used 1.5 and 3.0 kg as cutoff values based on the median and upper quartile of participant BW loss. We did not analyze the dose-response effect of BW gain because it might have been affected by the participants who withdrew from the cessation program on gaining slight BW.
Among the 2,635 individuals who participated in the smoking-cessation program during the study period, 303 participants were excluded as they were lost to follow-up when assessing the 6-month prolonged smoking abstinence, 804 participants were excluded because of their missing information, and 53 participants were excluded because of duplicated data. The remaining 1,475 participants were included in the analysis (Figure 1). Table 1 shows the demographic and clinical characteristics of 1,339 (90.8%) men and 136 (9.2%) women among a total of 1,475 participants. Compared with men, a larger proportion of the women were younger than 65 years, unmarried, had fewer comorbidities, PHQ-2 ≥ 2, and were initiated through outpatient service. The FTND score, BW gain during the program, and usage of types of cessation medication were similar for both the sexes. The 6-month prolonged abstinence rate of women was lower than that of men (21.3 vs. 36.7%, P < 0.001).
The results of the univariate and multivariable logistic regression analyses for all the included participants are shown in Table 2. The univariable analysis inferred a positive association with a failed 6-month prolonged smoking abstinence in participants who scored FTND ≥ 6 or used both NRT and non-NRT. On the contrary, covariates including those aged ≥ 65 years, men, married, comorbidities ≥ 2, ever cessation for 6 months, BW gain, in-patient initiated were negatively associated with failed abstinence. The multivariable analysis associated FTND ≥ 6 (OR: 1.99, 95% CI: 1.56 to 2.53) with a failed 6-month prolonged smoking abstinence, and negatively associated age ≥ 65 (OR: 0.59, 95% CI: 0.44 to 0.79), male (OR: 0.55, 95% CI: 0.35 to 0.86), married (OR: 0.59, 95% CI: 0.45 to 0.77), ever cessation for 6 months (OR: 0.54, 95% CI: 0.40 to 0.74), in-patient initiated (OR: 0.32, 95% CI: 0.23 to 0.43), with only varenicline usage (adjusted OR: 0.54, 95% CI: 0.32 to 0.92), and only NRT usage (adjusted OR: 0.59, 95% CI: 0.36 to 0.95) with a failed 6-month prolonged smoking abstinence. BW gain and PHQ-2 ≥ 2 unaffected 6-months prolonged smoking abstinence (P > 0.05).

Table 2. Univariable and multivariable logistic regression for predictors of failed 6-month smoking abstinence for all the participants (n = 1475).
Figure 2 demonstrates the results of the multivariable analysis after gender stratification of the participants. The BW gain was positively associated with a failed 6-month prolonged smoking abstinence in the women (adjusted OR: 3.10, 95% CI: 1.06 to 9.04) and negatively associated in the men (adjusted OR: 0.77, 95% CI: 0.61 to 0.98). The PHQ-2 ≥ 2 (adjusted OR: 0.09, 95% CI: 0.02 to 0.55) and only varenicline use (adjusted OR: 0.09, 95% CI: 0.01 to 0.59) were negatively associated with a failed 6-month prolonged smoking abstinence in the women, and unassociated with smoking abstinence in the men. FTND ≥ 6 was associated with a failed smoking abstinence in men (adjusted OR: 1.95, 95% CI: 1.52 to 2.51). For men, age ≥ 65 years (adjusted OR:0.59, 95% CI:0.44 to 0.80), with only NRT usage (adjusted OR: 0.59, 95% CI: 0.36 to 0.95), and ever quit smoking for 6 months (adjusted OR: 0.57, 95% CI: 0.41 to 0.78) were associated with successful abstinence. In both the sexes, participants associated with a successful 6-month prolonged smoking abstinence were married and had participated through in-patient initiated programs.
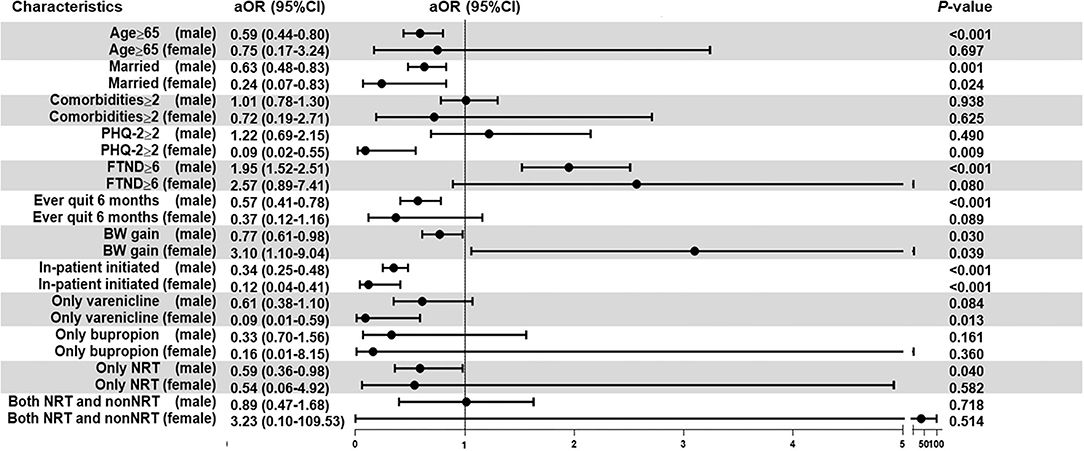
Figure 2. Multivariable logistic regression following sex stratification. The analyses were adjusted for age, sex, comorbidities, PHQ-2, FTND, cessation history, BW gain, site of program initiation, and cessation medication. Firth regression analyses were used for the women subgroup. Bold values indicate a statistically significant difference with a p-value of < 0.05. aOR, adjusted odds ratio; BW, body weight; CI, confidence interval; FTND, Fagerstrom test for nicotine dependence; NRT, nicotine replacement therapy; PHQ-2, Patient Health Questionnaire-2.
The results of the sensitivity analysis are listed in Table 3. In the multivariable analysis, the BW loss during the cessation program was associated with a successful 6-month prolonged smoking abstinence for women by replacing the covariable of BW gain by BW loss (adjusted OR: 0.28, 95% CI: 0.09 to 0.88), BW loss ≥ 1.5 kg (adjusted OR: 0.14, 95% CI: 0.03 to 0.55), and BW loss ≥ 3.0 kg (adjusted OR: 0.03, 95% CI: 0.01 to 0.42). However, no statistically significant association was observed between BW loss and successful abstinence in men.
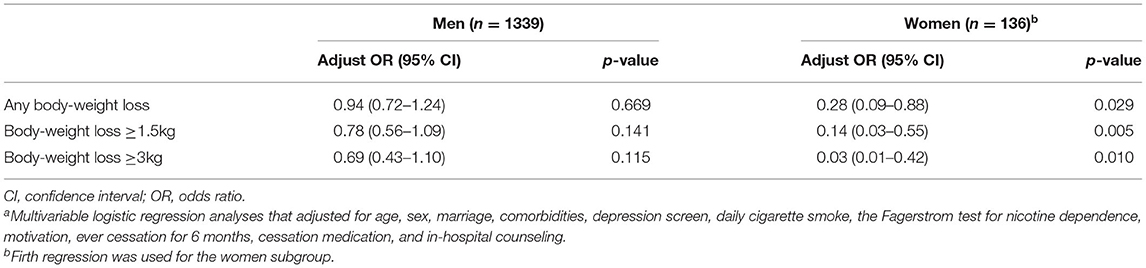
Table 3. Multivariable logistic regression for predictors of failed 6-month smoking abstinence after replacing covariable of body weight gain by body weight lossa.
Previous studies have found that smoking behavior differed between the sexes (3), and women smokers have more difficulty in quitting smoking than men smokers (13). To lower the prevalence of smoking among women, it is important to understand the factors associated with the failure of cessation in women smokers. However, studies investigating the predictors of failed smoking abstinence in hospital-based cessation programs are paucity. In this retrospective cohort study, data from 1,475 individuals were analyzed who had participated in a hospital-based smoking-cessation program. The collected data were considered credible because the factors, including age, sex, comorbidities, FTND scores, and cessation medications were monitored by the Taiwan Bureau of Health Promotion. In the multivariable logistic regression model adjusted for age, FTND score, PHQ-2, a cessation medication, other factors, and the BW gain was found to be associated with a failed 6-month prolonged smoking abstinence in women (OR: 3.10, 95% CI: 1.10 to 9.04) and with a successful 6-month prolonged smoking abstinence in men (OR: 0.77, 95% CI: 0.61 to 0.98). The sensitivity analyses showed that BW loss during the cessation program was associated with a successful 6-month prolonged smoking abstinence in women, but not in men. Thus, it was concluded that BW gain might be a sex-specific predictor of failed smoking abstinence in smoking-cessation programs.
Body-image dissatisfaction differs between the sexes. Women choose a smaller size whereas men choose a similar or larger size than their ideal body sizes (29, 30). In comparison with men, women have a higher risk of dissatisfaction with their body weight, report more disordered eating, and are less likely to recover their ideal BW from eating disorders (31, 32). Weight control is one of the main reasons leading to tobacco abuse in women (4, 5). On the other hand, weight gain might be one of the barriers in quitting smoking for women (33, 34). Cropsey et al. reported that women prisoners, who arguably have a stable energy intake and output, had average 10 pounds weight gain on the 6th month of smoking cessation, although the gain of body weight was decreased on the 12th month of cessation (35). The effect of smoking cessation on body mass index was higher for older women than for younger (36). In a previous smoking cessation study for postmenopausal women, the average weight gained was 6.5 kg (14 pounds) after 16 months of quitting smoking (37). To avoid failure of smoking abstinence, multidisciplinary weight control strategies (including education, calorie restriction, increasing physical activity, and cessation medication) should be introduced to the participants (38), especially women. Metanalysis concluded that pharmacological interventions limited the short-term weight gain during smoking cessation. However, there are no clinically effective interventions to restrict long-term weight gain currently (39).
Our study results showed that women participants with a PHQ-2 score ≥ 2 were associated with successful abstinence from smoking. However, previous research showed that depressive symptoms predicted a lower smoking abstinence rate, and there was no evidence of sex-specific effects of depression on smoking cessation (40, 41). PHQ-2 is a depression screening questionnaire rather than a diagnostic tool (17). Further investigation regarding PHQ-2 and smoking cessation in women is warranted.
Several limitations required to be acknowledged in this study. First, this study was conducted in Taiwan and body dissatisfaction differs based on cultural background, race, and economic status, (42) thus, the result of this study should be generalized with caution. Second, as this study was conducted retrospectively and the smoking history was dependent on the report of the participants, recall bias could not be excluded. However, other data including comorbidities, FTND, and cessation medication were regulated by the Taiwan Bureau of Health Promotion, so the robustness and accuracy of these data are supposed to be reliable. Third, apart from the information regarding the marital status of participants, information regarding active pregnancy, or child-bearing was unavailable. Although several pregnant women try to quit smoking due to the health concerns surrounding them and the fetus (3). A previous study had reported that among the few Taiwanese women who quit smoking during pregnancy, most relapsed in the 1st year after childbirth (43). Thus, the absence of pregnancy and child-bearing data should not affect the results of this study. Fourth, the women comprise only 9.2% of the participants. Given the large size of our study cohort, the sample size of women participants were sufficient. At last, the doses of NRT are different among the participants. However, the dose of NRT was determined by the participants' daily cigarette consumption in our study. This dosing strategy is widely used in the clinical trials and real-world conditions, and this limitation should not affect the results of our study.
BW gain during a hospital-based smoking-cessation program is a sex-specific predictor of failed abstinence. Furthermore, multicenter studies including participants of different races and cultural backgrounds are warranted.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Institutional Review Board of NCKUH (ID number: B-ER-110-126). The Ethics Committee waived the requirement of written informed consent for participation.
C-WK, C-FL, and TY designed the study. C-WK, C-FL, C-YChe, C-WC, and C-CS searched the literature. C-WK, C-YChe, R-HW, C-YCho, H-JC, and J-SW collected the data. C-WK, C-FL, and TY did the statistical analysis. C-WK, C-FL, and C-YChe wrote the manuscript. All the authors contributed to and approved the final manuscript.
This study was funded by grants from the National Cheng Kung University Hospital (NCKUH-11106011).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We are grateful to Ms. Mei-Chun Shen and Hsiao-Fen Yang for their help in collecting the data.
1. Goodchild M, Nargis N. Tursan d'Espaignet E. Global economic cost of smoking-attributable diseases. Tob Control. (2018) 27:58–64. doi: 10.1136/tobaccocontrol-2016-053305
2. World Health O. WHO Global Report on Trends in Prevalence of Tobacco Smoking 2000-2025. 2nd ed ed. Geneva: World Health Organization (2018). p. 120.
3. Sieminska A, Jassem E. The many faces of tobacco use among women. Med Sci Monit. (2014) 20:153–62. doi: 10.12659/MSM.889796
4. Fidler JA, West R. Self-perceived smoking motives and their correlates in a general population sample. Nicotine Tob Res. (2009) 11:1182–8. doi: 10.1093/ntr/ntp120
5. McEwen A, West R, McRobbie H. Motives for smoking and their correlates in clients attending Stop Smoking treatment services. Nicotine Tob Res. (2008) 10:843–50. doi: 10.1080/14622200802027248
6. Cosgrove KP, Wang S, Kim SJ, McGovern E, Nabulsi N, Gao H, et al. Sex differences in the brain's dopamine signature of cigarette smoking. J Neurosci. (2014) 34:16851–5. doi: 10.1523/JNEUROSCI.3661-14.2014
7. al'Absi M, Nakajima M, Allen S, Lemieux A, Hatsukami D. Sex differences in hormonal responses to stress and smoking relapse: a prospective examination. Nicotine Tob Res. (2015) 17:382–9. doi: 10.1093/ntr/ntu340
8. Ceribelli A, Pino MS, Cecere FL. Gender differences: implications for clinical trials and practice. J Thorac Oncol. (2007) 2(Suppl. 5):S15–8. doi: 10.1097/01.JTO.0000268635.25579.7e
9. Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. (2011) 8:378:1297–305. doi: 10.1016/S0140-6736(11)60781-2
10. Pineles BL, Park E, Samet JM. Systematic review and meta-analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy. Am J Epidemiol. (2014) 179:807–23. doi: 10.1093/aje/kwt334
11. Weber TL, Selya A, Wakschlag LS, Dierker L, Rose JS, Hedeker D, et al. The effect of maternal smoking on offspring smoking is unrelated to heritable personality traits or initial subjective experiences. Nicotine Tob Res. (2021) 23:1754–62. doi: 10.1093/ntr/ntab081
12. Smith PH, Bessette AJ, Weinberger AH, Sheffer CE, McKee SA. Sex/gender differences in smoking cessation: a review. Prev Med. (2016) 92:135–40. doi: 10.1016/j.ypmed.2016.07.013
13. Lopez Khoury EN, Litvin EB, Brandon TH. The effect of body image threat on smoking motivation among college women: mediation by negative affect. Psychol Addict Behav. (2009) 23:279–86. doi: 10.1037/a0014291
14. Aubin HJ, Farley A, Lycett D, Lahmek P, Aveyard P. Weight gain in smokers after quitting cigarettes: meta-analysis. BMJ. (2012) 345:e4439. doi: 10.1136/bmj.e4439
15. Pang RD, Bello MS, Liautaud MM, Weinberger AH, Leventhal AM. Gender differences in negative affect during acute tobacco abstinence differ between African American and White Adult cigarette smokers. Nicotine Tob Res. (2019) 21:1072–8. doi: 10.1093/ntr/nty122
16. Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
17. Liu SI, Yeh ZT, Huang HC, Sun FJ, Tjung JJ, Hwang LC, et al. Validation of patient health questionnaire for depression screening among primary care patients in Taiwan. Compr Psychiatry. (2011) 52:96–101. doi: 10.1016/j.comppsych.2010.04.013
18. Fagerström K. Determinants of tobacco use and renaming the FTND to the fagerstrom test for cigarette dependence. Nicotine Tob Res. (2012) 14:75–8. doi: 10.1093/ntr/ntr137
19. Pérez-Ríos M, Santiago-Pérez MI, Alonso B, Malvar A, Hervada X, de Leon J. Fagerstrom test for nicotine dependence vs heavy smoking index in a general population survey. BMC Public Health. (2009) 9:493. doi: 10.1186/1471-2458-9-493
20. Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob Res. (2003) 5:13–25. doi: 10.1080/1462220031000070552
21. Wang SK, Kao CW, Chuang HW, Tseng YK, Chen WC, Yeh CC, et al. Government's subsidisation policy and utilisation of smoking cessation treatments: a population-based cross-sectional study in Taiwan. BMJ Open. (2021) 11:e040424. doi: 10.1136/bmjopen-2020-040424
22. Reid RD, Mullen KA, Slovinec D'Angelo ME, Aitken DA, Papadakis S, Haley PM, McLaughlin CA, Pipe AL. Smoking cessation for hospitalized smokers: an evaluation of the “Ottawa Model”. Nicotine Tob Res. (2010) 12:11–8. doi: 10.1093/ntr/ntp165
23. Guideline for clinical smoking cessation services of Taiwan. Bureau of Health Promotion, Department of Health, Executive Yuan. (2012). Available online at: https://health99.hpa.gov.tw/storage/pdf/materials/21780.pdf (accessed October 05, 2021).
24. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. public health service report. Am J Prev Med. (2008) 35:158–76. doi: 10.1016/j.amepre.2008.04.009
25. Etter JF, Huguelet P, Perneger TV, Cornuz J. Nicotine gum treatment before smoking cessation: a randomized trial. Arch Intern Med. (2009) 169:1028–34. doi: 10.1001/archinternmed.2009.12
26. Aubin HJ, Bobak A, Britton JR, Oncken C, Billing CB Jr, et al Varenicline versus transdermal nicotine patch for smoking cessation: results from a randomised open-label trial. Thorax. (2008) 63:717–24. doi: 10.1136/thx.2007.090647
27. Rennard SI, Glover ED, Leischow S, Daughton DM, Glover PN, Muramoto M, et al. Efficacy of the nicotine inhaler in smoking reduction: a double-blind, randomized trial. Nicotine Tob Res. (2006) 8:555–64. doi: 10.1080/14622200600789916
28. Zhang B, Cohen JE, Bondy SJ, Selby P. Duration of nicotine replacement therapy use and smoking cessation: a population-based longitudinal study. Am J Epidemiol. (2015) 181:513–20. doi: 10.1093/aje/kwu292
29. Hoyt WD, Kogan LR. Satisfaction with body image and peer relationships for males and females in a college environment. Sex Roles. (2001) 45:199–215. doi: 10.1023/A:1013501827550
30. Stanford JN, McCabe MP. Body image ideal among males and females: sociocultural influences and focus on different body parts. J Health Psychol. (2002) 7:675–84. doi: 10.1177/1359105302007006871
31. Santos Silva DA, Nahas MV, de Sousa TF, Del Duca GF, Peres KG. Prevalence and associated factors with body image dissatisfaction among adults in southern Brazil: a population-based study. Body Image. (2011) 8:427–31. doi: 10.1016/j.bodyim.2011.05.009
32. Støving RK, Andries A, Brixen K, Bilenberg N, Hørder K. Gender differences in outcome of eating disorders: a retrospective cohort study. Psychiatry Res. (2011) 186:362–6. doi: 10.1016/j.psychres.2010.08.005
33. Berg CJ, Park ER, Chang Y, Rigotti NA. Is concern about post-cessation weight gain a barrier to smoking cessation among pregnant women? Nicotine Tob Res. (2008) 10:1159–63. doi: 10.1080/14622200802163068
34. Levine MD, Marcus MD, Kalarchian MA, Houck PR, Cheng Y. Weight concerns, mood, and postpartum smoking relapse. Am J Prev Med. (2010) 39:345–51. doi: 10.1016/j.amepre.2010.05.023
35. Cropsey KL, McClure LA, Jackson DO, Villalobos GC, Weaver MF, Stitzer ML. The impact of quitting smoking on weight among women prisoners participating in a smoking cessation intervention. Am J Public Health. (2010) 100:1442–8. doi: 10.2105/AJPH.2009.172783
36. Kasteridis P, Yen ST. Smoking cessation and body weight: evidence from the behavioral risk factor surveillance survey. Health Serv Res. (2012) 47:1580–602. doi: 10.1111/j.1475-6773.2012.01380.x
37. Kleppinger A, Litt MD, Kenny AM, Oncken CA. Effects of smoking cessation on body composition in postmenopausal women. J Womens Health (Larchmt). (2010) 19:1651–7. doi: 10.1089/jwh.2009.1853
38. Bush T, Lovejoy JC, Deprey M, Carpenter KM. The effect of tobacco cessation on weight gain, obesity, and diabetes risk. Obesity (Silver Spring). (2016) 24:1834–41. doi: 10.1002/oby.21582
39. Hartmann-Boyce J, Theodoulou A, Farley A, Hajek P, Lycett D, Jones LL, et al. Interventions for preventing weight gain after smoking cessation. Cochrane Database Syst Rev. (2021) 10:Cd006219. doi: 10.1002/14651858.CD006219.pub4
40. Cinciripini PM, Robinson JD, Karam-Hage M, Minnix JA, Lam C, Versace F, et al. Effects of varenicline and bupropion sustained-release use plus intensive smoking cessation counseling on prolonged abstinence from smoking and on depression, negative affect, and other symptoms of nicotine withdrawal. JAMA Psychiatry. (2013) 70:522–33. doi: 10.1001/jamapsychiatry.2013.678
41. Cooper J, Borland R, McKee SA, Yong HH, Dugué PA. Depression motivates quit attempts but predicts relapse: differential findings for gender from the international tobacco control study. Addiction. (2016) 111:1438–47. doi: 10.1111/add.13290
42. Holmqvist K, Frisén A. Body dissatisfaction across cultures: findings and research problems. Eur Eat Disord Rev. (2010) 18:133–46. doi: 10.1002/erv.965
Keywords: smoking, smoking cessation, failed abstinence, female, body weight
Citation: Kuo C-W, Lin C-F, Chen C-Y, Wang R-H, Chou C-Y, Cheng H-J, Wu J-S, Chen C-W, Shieh C-C and Yu T (2022) Body-Weight Gain in Women During Smoking Cessation Is a Sex-Specific Predictor of 6-Month Abstinence: A Retrospective Cohort Study. Front. Public Health 10:872220. doi: 10.3389/fpubh.2022.872220
Received: 09 February 2022; Accepted: 14 April 2022;
Published: 13 May 2022.
Edited by:
Ozden Gokdemir, Izmir University of Economics, TurkeyReviewed by:
Wei Xia, Sun Yat-sen University, ChinaCopyright © 2022 Kuo, Lin, Chen, Wang, Chou, Cheng, Wu, Chen, Shieh and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tsung Yu, dHN1bmd5dUBtYWlsLm5ja3UuZWR1LnR3
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.