
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 06 October 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.867456
This article is part of the Research TopicWomen in Psychiatry 2022: AutismView all 6 articles
 TaeEung Kim1
TaeEung Kim1 Eun Hye Kwon2*
Eun Hye Kwon2*Obesity-related information in children with Autism Spectrum Disorder (ASD) is limited, and research findings are contradictory. Thus, this study aimed to use a nationwide non-clinical sample to examine the association of sociological factors with overweight status in children with ASD and reveal the degree of differences in the risk factors for overweight in children with and without ASD. The data for this cross-sectional study, based on the modified ecological system theory model, were obtained from the 2019 National Survey of Children's Health. The weighted logistic regressions were performed to determine the factors associated with overweight status in children with ASD, controlling for demographics, physical activity-related behaviors, and family and environmental conditions. A total of 529 children were identified (mean age 13.78 years, 83.21% boys). Two-parent households, less healthy parents and households, households with smokers, poor sleep quality, and greater participation in organized activities were associated with a higher likelihood of overweight in children with ASD (all P < 0.05). The determinants of obesity among children with ASD go beyond the individual level; family and community support are important. Therefore, greater attention should be directed toward the families of children with ASD and community-level administrative policies to improve quality of life by preventing or reducing obesity in children with ASD.
The prevalence of childhood obesity has been well investigated. In the United States of America (US), more than one in three children and adolescents (“children” hereafter) are overweight or obese (“overweight” hereafter) (1). In childhood, considering age and sex, overweight is defined as a body mass index (BMI) above the 85th percentile but below the 95th percentile, whereas obesity is defined as a BMI above the 95th percentile (2). During the past three decades, childhood obesity in the US has quadrupled (3).
Childhood obesity negatively impacts overall health and wellbeing. Studies show that overweight children are at a higher risk of cardiovascular diseases, including high blood pressure and/or high cholesterol, (4) pre-diabetes resulting in diabetes later in life, (5) and bone and joint problems, as well as sleep problems (6). Additionally, they are at an increased risk of psychosocial problems, such as low self-esteem and stigmatization (7). Moreover, childhood obesity increases the likelihood of health problems later in life; these include obesity, (8) heart disease, type 2 diabetes, stroke, and osteoarthritis (6). There is also a high association with different types of cancer, such as breast, colon, kidney, pancreatic, thyroid, ovarian, cervical, and prostate, as well as multiple myeloma and Hodgkin's lymphoma (9).
In general, childhood obesity is strongly associated with lifestyle habits, such as a high calorie intake and inadequate physical activity (6). Such lifestyle patterns are substantially attributed to families, (10) schools, (11) communities, (12), and environments (13). Since family, school, and the community play an important role in preventing and minimizing obesity in children, it is critical to establish healthy and positive environments through appropriate policies and initiatives. In this manner, children can learn ‘about and practice healthy eating and become more physically active (14).
Several studies have sought to identify the determinants of childhood obesity. However, such research is limited in the context of Autism Spectrum Disorder (ASD), perhaps owing to the relatively few cases compared to the general population. Since children with ASD often face substantial social and behavioral challenges at both the familial and societal levels, (15) they may be more vulnerable to obesity and its associated complex behavioral, psychosocial, and physical difficulties (16). Therefore, children with ASD face extreme hardships related to learning, thinking, and problem solving (17).
Obesity in children with ASD is a complex phenomenon. The features and possible outcomes of some of the symptoms of ASD, such as lack of autonomy, self-motivation, and social inspiration, can be considered major risk factors for obesity to obesity. Additionally, children with ASD are less likely than their typically developing counterparts to participate in structured physical activity (18) or family meals, resulting in unhealthy weight (19). They are also likely to experience poor sleep quality, which can contribute to obesity (20). Limited community resources play an important role in maintaining a healthy weight in children with ASD, including parents' health, neighborhood and school safety, proper physical activity programs, and accessibility to facilities.
Studies on physical activity and sedentary behavior associated with obesity in typically developing children or at the medical level have suggested directions for the prevention and improvement of obesity in children with ASD (21–23). However, while these studies may provide insight into obesity prevention among children with ASD on a broad level, there is a limitation to understanding the related socioecological factors and prevention strategies for obesity in this population. Therefore, it is imperative to measure the level of physical inactivity, sedentary lifestyles, and community resources and to understand the correlates of overweight in children with ASD. Unfortunately, a lack of understanding of the factors associated with childhood obesity in this population diminishes the quality of public health and results in societal financial burdens (24, 25). To gain a holistic understanding of obesity and its related factors, it is crucial to draw insights from a large sample of children with ASD in a non-clinical setting.
In this context, this study aimed to examine overweight and its associated factors in a large non-clinical sample of children with ASD. It is hypothesized that in children with ASD: (1) social interactions (e.g., social involvement, voluntary activities, and family meals) are negatively associated with overweight status; (2) parents' physical and mental health status is associated with overweight status; (3) insufficient sleep is positively associated with overweight status; and (4) neighborhood conditions (e.g., accessibility of and number of parks and recreational facilities) are associated with overweight status.
This study is a secondary analysis of the 2019 National Survey of Children's Health, (26) which provides a wealth of data on several intersecting aspects: physical and mental health; access to quality healthcare; and the child's familial, neighborhood, school, and social context. The National Survey of Children's Health is funded and administered by the Health Resources and Services Administration Maternal and Child Health Bureau. In 2019, the Census Bureau conducted a revised version of the survey via post and the internet. The original data pertained to 29,433 children, but as the BMI of children aged 0–9 years could not be determined, in this study, the data of 529 children aged 10–17 years, obtained from their parents, were analyzed.
To make it easier to understand the complex causes of obesity in children with ASD, a modified socioecological approach was employed (27). The five main parts of the framework were as follows: (1) children's age, sex, race/ethnicity, physical activity, and sedentary lifestyle; (2) parenting capacity, which included educational level, income level, and household structure; (3) family health and activities, which included parental health, drinking and smoking status, family eating patterns, and stability of food provision; (4) community and school activities, such as the existence of afterschool programs, community service, and parents' children's activities due to factors in the community and schools; and (5) neighborhood factors, such as the degree of safety and support in the neighborhood, stability of the school and neighborhood, cooperation within the neighborhood, and facilities related to children's activities in the neighborhood (Figure 1).
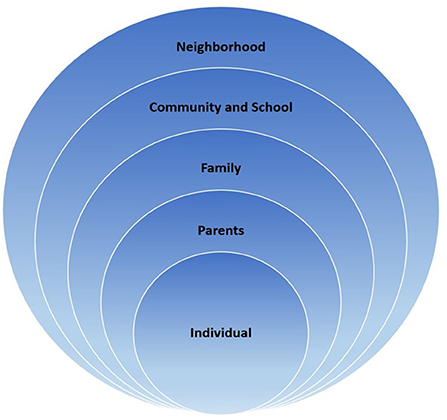
Figure 1. Modified socioecological theory framework from Bronfenbrenner (27).
The main outcome variable was the binary variable of being overweight (≥85th BMI percentile) vs. non-overweight (0th <BMI percentile <85th) for age and sex (2). BMI was obtained by dividing weight in kilograms by the square of height in meters (28). BMI was calculated in percentiles to determine the severity of obesity using a growth chart considering the child's age and sex (29).
Autism Spectrum Disorder was measured as a dichotomous variable, which is whether or not the children currently had Asperger's syndrome, pervasive developmental disorders, or ASD. Obesity-related variables were extracted from five main areas: individual factors, parenting capacity, family activities, and community and school activities, neighborhood support.
First, among the socioecological factors related to obesity in children, individual factors included age, sex, race/ethnicity, physical activity, sedentary lifestyle, and quality of sleep. Owing to the limitations of BMI information, the age of the participants ranged from 10 to 17 years. Participants' race/ethnicity was classified into five groups: Hispanic, non-Hispanic white, non-Hispanic black, non-Hispanic Asian, and others. The level of physical activity was measured on a four-point Likert scale (1 = 0 day to 4 = every day) based on the number of days of physical activity, exercise, or sports that children participated in for at least 60 min during the past week. Sedentary lifestyle was measured on a five-point Likert scale (1 = <1 h to 5 = more than 4 h) over the past week, such as watching television; using computers, cell phones, or other electronic devices; playing online games; surfing the internet; or engaging in non-academic social networks. Sleep quality was measured as the number of hours of sleep on an average day on most weekdays during the past week and converted into a binary variable according to the American Academy of Pediatrics' sleep duration recommendations for 24-h periods (i.e., 9–12 and 8–10 h for children and adolescents aged 6–12 and 13–18 years, respectively) (30).
Childhood obesogenic factors related to parenting capacity were educational level, income level, and family structure. Parents' educational level was measured using a four-point Likert scale (1 = less than high school to 4 = college degree or higher). Parents' income level was measured on a four-point Likert scale (1 = 0–99% of the federal poverty level to 4 = 400% or greater of the federal poverty level). Family structure was initially measured on a five-point Likert scale and then restructured into binary variables (e.g., parents vs. other family structures, such as single parent and guardians).
Factors related to family health and activities contributing to children's obesity included parents' health, drinking, drug use status, stress coping ability, family meals, and food security. Parents' overall health, encompassing physical and mental health, was assessed on a four-point Likert scale. The primary caregiver received a score between 1 and 12 points, with a higher score indicating better overall health. A binary variable was used to determine whether or not a child lived with a person with alcohol or drug-related problems. The smoking status of any person living in a child's home was determined in relation to the use of cigarettes and pipe tobacco. The stress-coping variable, used to determine the frequency of instances of the household demonstrating resilience, was assessed on a three-point Likert scale (0 = 0–1 items of all or most of the time to 2 = all or most of the time to 3= all four items). The aspect of meals assessed how many days over the past week all family members had eaten together; this was done on a four-point Likert scale (1 = 0 day to 4 = every day). Food security was measured on a four-point Likert scale as the child's household's ability to afford food for the past 12 months (1 = always get enough nutritious food to 4 = often not enough).
Three childhood obesity-related community- and school-activity variables were investigated. Organized afterschool activities were assessed in terms of which organized activity or class the child had participated in after school or on weekends over the past 12 months. The child indicated the family's level of engagement in community service or volunteering over the past 12 months based on their participation in such events at school, church, or in the community. Parental event/activity participation was measured on a four-point Likert scale (1 = rarely or never to 4 = always).
Four variables of neighborhood safety and support areas were assessed. School safety and safe neighborhoods, evaluated by asking parents about the extent to which they considered their child safe in school or the neighborhood, were measured on a three-point Likert scale (1 = somewhat/definitely disagree to 3 = definitely agree). A binary variable was used to assess whether the neighborhood was supportive. A neighborhood amenities variable, which concerned how many amenities, such as parks, recreation centers, sidewalks, or libraries, that the neighborhood contained, was measured on a five-point Likert scale.
Pearson's χ2 tests and t-tests with weighted counts and column percentages were performed for the descriptive statistics. The weighted logistic regression analyses were performed to investigate the relationship between BMI status and quality of life in children with ASD in terms of socioecological obesity factors, including individual factors, parenting capacity, family health and activities, and community and school activities plus neighborhood safety and support. All statistical and logistic regression analyses were performed for sex, race/ethnicity, socioeconomic status, family, school, community, and other relevant characteristics using STATA version 15.1 (StataCorp LLC, College Station, TX).
The relevant institutional review board exempted this study.
The unweighted (i.e., number of participants and mean) and weighted (i.e., standard deviation and percentage) descriptive statistics of the sample are shown in Table 1. A total of 529 children with ASD (representing 1,291,821 children at the population level) were recruited for this study. The mean age was 13.78 (SD = 2.09) years, and 83.21% of the participants were boys. Table 1 shows that the participants belonged to diverse races and ethnicities, including non-Hispanic whites (52.19%), Hispanics (27.15%), non-Hispanic blacks (14.74%), others (4.33%), and non-Hispanic Asians (1.59%).
One weighted multivariate logistic analysis considering socioecological obesogenic factors was performed (i.e., personal factors, parenting capacity, family health and activities, community and school activities, and neighborhood safety and support). Five independent variables associated with children's overweight status had significantly different odds ratios (ORs) in their binary BMI levels [i.e., overweight (≥85th percentile) vs. non-overweight (0th <BMI percentile <85th percentile)] (see Table 2).
In terms of obesogenic factors, children who slept well had statistically significantly lower odds of being overweight than those who did not receive adequate sleep [OR = 0.38, 95% confidence interval (CI) = 0.19–0.71]. According to parenting capacity, children from two-parent households (OR = 5.70, 95% CI = 1.83–17.79) were more likely to be overweight than children from any other family structure (e.g., one parent, no parents, etc.). Regarding family health and activities, a one-unit increase in parents' health resulted in a lower risk of being overweight (OR = 0.80, 95% CI = 0.68–0.93). Children from households with smokers had 2.62 times higher odds of being overweight than children from households without smokers (OR = 2.62, 95% CI = 1.03–6.65). In terms of community and school activities, children who had participated in more organized activities after school or on weekends over the past 12 months were more likely to be overweight than those who had not (OR = 2.74, 95% CI = 1.35–5.55).
This cross-sectional study examined overweight children with ASD as well as obesogenic factors in this large non-clinical sample. According to the results, the risk factors for obesity in children with ASD were both similar to and different from those reported in a previous study (31). The present study revealed the complexity of the obesity trend in children with ASD in terms of socioecological, multilevel factors.
Physiologically, common comorbidities observed among individuals with ASD include neurological, psychiatric, and physical conditions (32). Neurological comorbidities in ASD, including sleep impairment, sensory abnormalities, and psychiatric conditions, include delays and/or deficits in motor function and attention deficit hyperactivity disorder (32). Some of the medications prescribed to manage the symptoms of these comorbidities have been linked to weight gain, but this aspect has not been explored in previous studies. Egan et al. (33) determined that the psychotropic medication status of children with ASD is not related to the BMI z-score. In summary, individuals with ASD share physiological comorbidities. However, these comorbidities and the prescribed medications cannot be considered as the only factors contributing to overweight in this population. This is the major reason why interdisciplinary analysis is more appropriate for determining obesity factors in ASD.
Previous studies indicate that children with ASD are at a greater risk of being overweight than their typically developing counterparts (33). In the past few decades, many multidisciplinary studies have been conducted to investigate the causes of childhood obesity. These have determined that the major causes of obesity, such as activity level, diet, behavior, and socioeconomic status, interact with each other to increase the obesity rate in children (34–38). We observed the same trend among children with ASD. Several factors such as the level of school activity, ethnic background, community support, and parental status interact and affect the increase in obesity rate among children with ASD. Various obesogenic factors, such as diet, physical activity, and sleep patterns within the context of the family environment have been confirmed (31); thus, family dynamics are the main criteria for any examination of childhood obesity risk factors (31).
In this study, social and community support were also observed to contribute to the development of obesity among children with ASD. Research indicates that social and community support for families of children with ASD improves family adaptation (39). Social support can improve the views of family members concerning their family structure, and optimistic viewpoints are important in the development of helpful coping strategies for eventual family adaptation (40). However, community support is not equally accessible to every family with children with ASD that needs help (41). Since there is a positive relationship between social support, community support, and obesity, systematic support needs to be established for parents of children with ASD after their child's diagnosis.
Curtin et al. (31) indicated that the challenges of engaging in physical activity might be uniquely associated with the development of obesity in children with ASD. One of the main reasons for insufficient physical activity is the limited number of school-based extracurricular physical activity programs for children with ASD (42, 43). Additionally, increased time spent engaging in sedentary behavior has been shown to increase the risk of obesity among children with ASD. Since factors that lead to sedentary behavior and lack of engagement in physical activity among children with ASD are interconnected with their social and/or behavioral impairments, they may encounter more difficulties in participating in formal and informal forms of physical activity than typically developing children. The greater risk of overweight among children with ASD was explored in a meta-analysis (44). Based on their results, ethnicity (non-Caucasian race), increasing age, and female sex are potential risk factors for overweight in children with ASD (44).
These studies clarify that it is not possible to identify a single factor as leading to overweight among children with ASD. Therefore, a socioecological approach is crucial. As hypothesized, social interactions (e.g., social involvement, voluntary activities, and family meals) and parents' physical and mental health status played a positive role, whereas insufficient sleep played a negative role. Additionally, neighborhood conditions (e.g., accessibility of and the number of parks and recreational facilities) were associated with overweight status in children with ASD.
Multiple studies have determined the relationship between environmental factors and obesity status in typically developing children, including maternal obesity, (45, 46) lower educational attainment, (47) lower physical activity rates, (48) poor nutrition knowledge, (48) food insecurity, (49) smoking, (45), and rules regarding food consumption and eating at regular times (50). In this study, national-level data from the US were analyzed to determine the relationship between the obesity status of children with ASD and environmental factors. The results indicated a trend between obesity level and sleep patterns, family structure, and household smoking status. Studies on the effect of paternal/household smoking on childhood overweight have reported inconsistent results; some studies have found no association between household smoking and childhood overweight, (51, 52) whereas others have observed positive associations (53–55).
Cross-sectional studies have reported mixed results regarding the association between sleep duration and obesity in children and adolescents. However, sleep deprivation is believed to lead to fatigue, daytime sleepiness, cognitive problems, low activity levels, and changes in the levels of several hormones (56, 57). Hormones that could be affected by sleep deprivation include leptin, ghrelin, insulin, cortisol, and growth hormone (58, 59). Hormonal changes may contribute to energy imbalance, which could lead to overweight or obesity. In this study, a similar trend was observed among children with ASD, indicating a negative correlation between sleep duration and obesity. This indicates that in children with ASD, short sleep duration is positively associated with obesity. However, in this study, the focus was on total sleep duration; sleep quality was not explored. Several issues related to sleep among children with ASD have been reported, such as sleep onset and maintenance by parents (60–62). The quality of sleep in children with ASD should be considered in future studies.
Despite this uncertainty in the literature on obesity in children, there is still some preliminary evidence that family structure matters. Family is the primary source of social learning and influence for children (63). It is known that parents, family structure, and family environment can impact the amount of food a child consumes and the level of physical activity of the child (64). Several studies have indicated that two-parent families may be more effective at nurturing children than single-parent families (48, 49). More recent studies have also found associations between family structure (including parent status and number of siblings) and children's physical health outcomes (51, 64–66). Generally, children from single-parent families are more likely than those from two-parent families to be overweight (64). However, in this study, children with ASD from two-parent families had a higher risk of obesity. Family structure considered as an important factor in the family context linked with child development (67). Thus, family structure affects on family functioning and family dynamics (31). Generally married, biological-parent households are providing less stressful family context than other family structures, due to higher levels of economic resources and social support (68). A growing body of the study pointed out that family function and family dynamics such as, family stress, maternal depression, and family connection play a critical role in developing childhood obesity. Since families with children with ASD may have different family functions or dynamics compared to families with typically developed children in terms of the level of stress and interaction among family members, (69) it is important to focus more on family function than family structure to understand how this element could affect on obesity rates of children with ASD. However, there is lack of research examined how the family structure related to obesity in children with ASD, this line of research warrants future attention.
Parents' perceived stress was examined as several studies have indicated that parents of children with ASD tend to have higher stress levels than parents of typically developing children (70–73). Compared to children with other disabilities, children with ASD characterize disabilities in social interaction, impairment of speech and non-verbal communication, homogeneous behavior, and interest, and are unable to communicate with their parents due to late language development (70–73). These behavior patterns of children with ASD may increase parental stress in child rearing. Studies have also reported a higher prevalence of depressive symptoms and lower quality of life in families with children with ASD than in those with children with other developmental disorders such as physical disabilities or chronic health conditions (72–74). Recent data on stress in families of children with ASD have mainly reported stress as perceived by mothers (70, 75–77). The stress level of family members of children with ASD may affect the time and effort invested in fostering a healthy lifestyle because many unhealthy behaviors are associated with increased stress, such as infrequent exercise, alcohol drinking, smoking, sleep disorders, and eating poorly (78). Studies have also indicated that imbalanced dietary patterns and emotional eating are associated with stress (65, 66, 79). Since the family environment affects the amount of food consumed and level of physical activity, the stressful environment of a family with children with ASD may lead to an unhealthy lifestyle that finally affects the obesity level of children with ASD.
The Centers for Disease Control and Prevention guidelines also recommended school- and community-based strategies to prevent childhood obesity by altering the environment and developing relevant policies (80). Since children are nested within families and classes, which are nested within schools, which, in turn, are nested within either school districts or communities, a multilevel approach is needed. By using a clear conceptual framework, the complexity of overweight among children with ASD can be understood systematically and deeply. The long-term goal of this study was to improve the understanding of individual and environmental connections with overweight/obesity mechanisms among children with ASD, which can lead to public health prevention and intervention strategies to reduce overweight/obesity in children with disabilities and ASD. Therefore, comprehensive and multi-sectorial approaches are needed to address the many behavioral and environmental risk factors associated with obesity in children with ASD. A multilevel approach analysis would provide more effective intervention programs and/or policies regarding adolescents' obesity in a multilevel setting (e.g., family, school, district, and state) (81).
This study had the following limitations. First was the use of self-reported measures to assess all variables from the respondents' 1-day recollection, which may be inaccurate because of recall bias, respondent bias, or interview bias. Second, owing to the small sample size (e.g., Hispanic and Asian), attempts to generalize the findings to areas with more diversity must be undertaken with caution. A larger and more diverse sample would yield better results. Third, the dataset excluded households without telephones and/or cellphones, which may result in a biased survey population owing to the underrepresentation of certain segments of the population. Therefore, future studies on obesity prevention in children with ASD should consider these limitations. However, these limitations do not outweigh the contributions of this study.
This study revealed various multilevel dimensions of how sociological factors are correlated with overweight status in children with ASD. The overweight status of children with ASD was related not only to individual factors but also family and community support. Parental involvement in physical activities and obtaining family and social support is crucial to the overweight status of children with ASD. More attention should be paid to providing children with ASD with family and social support to help them maintain healthy weight. The significance of this study is that it comprehensively explored the obesity trend of children with ASD-related factors to propose multilevel solutions.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
TK: conceptualization, methodology, data curation and formal analysis, investigation, writing—original draft preparation, and writing—review and editing. Both authors contributed to the article and approved the submitted version.
We would like to express my gratitude to the Texas A&M University-San Antonio and Kyung Hee University Medical School for their support in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. (2014) 311:806–14. doi: 10.1001/jama.2014.732
2. Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. (2007) 120 Suppl(Supplement):S193–228. doi: 10.1542/peds.2007-2329D
3. Ogden CL, Fryar CD, Martin CB, Freedman DS, Carroll MD, Gu Q, et al. Trends in obesity prevalence by race and hispanic origin-−1999–2000 to 2017–2018. JAMA. (2020) 324:1208–10. doi: 10.1001/jama.2020.14590
4. Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the bogalusa heart study. J Pediatr. (2007) 150:12–7.e2. doi: 10.1016/j.jpeds.2006.08.042
5. Li C, Ford ES, Zhao G, Mokdad AH. Prevalence of pre-diabetes and its association with clustering of cardiometabolic risk factors and hyperinsulinemia among U.S. adolescents: national health and nutrition examination survey 2005–2006. Diabetes Care. (2009) 32:342–7. doi: 10.2337/dc08-1128
6. Benjamin RM. The surgeon general's vision for a healthy and fit nation. Public Health Rep. (2010) 125:514–5. doi: 10.1177/003335491012500402
7. Russell-Mayhew S, McVey G, Bardick A, Ireland A. Mental health, wellness, and childhood overweight/obesity. J Obes. (2012) 2012:281801. doi: 10.1155/2012/281801
8. Guo SS, Chumlea WC. Tracking of body mass index in children in relation to overweight in adulthood. Am J Clin Nutr. (1999) 70:145S−8S. doi: 10.1093/ajcn/70.1.145s
9. Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, et al. American cancer society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. (2012) 62:30–67. doi: 10.3322/caac.20140
10. Gibson LY, Allen KL, Byrne SM, Davis L, Zubrick SR. The role of family and maternal factors in the development and maintenance of childhood obesity. Obes Res Clin Pract. (2013) 7:e118–9. doi: 10.1016/j.orcp.2013.12.711
11. Williams AJ, Henley WE, Williams CA, Hurst AJ, Logan S, Wyatt KM. Systematic review and meta-analysis of the association between childhood overweight and obesity and primary school diet and physical activity policies. Int J Behav Nutr Phys Act. (2013) 10:101. doi: 10.1186/1479-5868-10-101
12. Wu Y, Lau BD, Bleich S, Cheskin L, Boult C, Segal JB. Future Research Needs for Childhood Obesity Prevention Programs: Identification of Future Research Needs From Comparative Effectiveness Review No. 115. 2013 Jun AHRQ Comp Eff Rev TypeBookLanguageEnglishJournal InfoPublisher Agency Healthc Res Qual Cited Mediu Internet Impr Name(s)rockv Agency Healthc Res Qual. (2013). Available online at: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?holding=inleurlib_fft&cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=24027795 (accessed September 11, 2021).
13. Zhao J, Settles BH. Environmental correlates of children's physical activity and obesity. Am J Health Behav. (2014) 38:124–33. doi: 10.5993/AJHB.38.1.13
14. Must A, Curtin C, Hubbard K, Sikich L, Bedford J, Bandini L. Obesity prevention for children with developmental disabilities. Curr Obes Rep. (2014) 3:156–70. doi: 10.1007/s13679-014-0098-7
15. Kuehn BM. CDC: autism spectrum disorders common. JAMA. (2007) 9:940. doi: 10.1001/jama.297.9.940
16. Powell SD, Jordan RR. Being subjective about autistic thinking and learning to learn. Educ Psychol. (1993) 13:359–70. doi: 10.1080/0144341930130312
17. Wojcik DZ, Allen RJ, Brown C, Souchay C. Memory for actions in autism spectrum disorder. Memory. (2011) 19:549–58. doi: 10.1080/09658211.2011.590506
18. Hinckson EA, Dickinson A, Water T, Sands M, Penman L. Physical activity, dietary habits and overall health in overweight and obese children and youth with intellectual disability or autism. Res Dev Disabil. (2013) 34:1170–8. doi: 10.1016/j.ridd.2012.12.006
19. Lee L, Harrington RA, Louie BB, Newschaffer CJ. Quality of life and parental concerns in children with autism. J Autism Dev Disord. (2008) 38:320408. doi: 10.1007/s10803-007-0491-0
20. Dev DA, McBride BA, Fiese BH, Jones BL, Cho H, on behalf of the STRONG Kids R H. Risk factors for overweight/obesity in preschool children: an ecological approach. Child Obes. (2013) 9:399–408. doi: 10.1089/chi.2012.0150
21. Corvey K, Menear KS, Preskitt J, Goldfarb S, Menachemi N. Obesity, physical activity and sedentary behaviors in children with an autism spectrum disorder. Matern Child Health J. (2016) 20:466–76. doi: 10.1007/s10995-015-1844-5
22. Hill AP, Zuckerman KE, Fombonne E. Obesity and autism. Pediatrics. (2015) 136:1051–61. doi: 10.1542/peds.2015-1437
23. Zuckerman KE, Hill AP, Guion K, Voltolina L, Fombonne E. Overweight and obesity: prevalence and correlates in a large clinical sample of children with autism spectrum disorder. J Autism Dev Disord. (2014) 44:1708–19. doi: 10.1007/s10803-014-2050-9
24. Blumberg SJ, Bramlett MD, Kogan MD, Schieve LA, Jones JR, Lu MC. Changes in prevalence of parent-reported autism spectrum disorder in school-aged U. S. children: 2007 to 2011–2012. Natl Health Stat Report. (2013) 65:1–11.
25. Windham GC, Anderson MC, Croen LA, Smith KS, Collins J, Grether JK. Birth prevalence of autism spectrum disorders in the San Francisco Bay area by demographic and ascertainment source characteristics. J Autism Dev Disord. (2011) 41:1362–72. doi: 10.1007/s10803-010-1160-2
26. Data Resource Center for Child & Adolescent Health. National Survey of Children's Health—Data Resource Center for Child and Adolescent Health. (2016). Available online at: http://childhealthdata.org/learn/NSCH (accessed August 30, 2021).
27. Bronfenbrenner U. Environments in development perspective: thoeretical and operational models. Measuring Environment Across the Life Span: Emerging Methods and Concepts. (1999). p. 3–28. doi: 10.1037/10317-001
28. Ogden CL, Caroll MD, Fryar CD, Flegal KM, Kruszon-Moran D. Childhood Obesity Facts. Overweight & Obesity. Centers for Disease Control Prevention (2014). Available online at: https://www.cdc.gov/obesity/data/childhood.html (accessed October 22, 2021).
29. Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. (2013) 128:1689–712. doi: 10.1161/CIR.0b013e3182a5cfb3
30. Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, Lloyd RM, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. (2016) 12:785–6. doi: 10.5664/jcsm.5866
31. Curtin C, Jojic M, Bandini LG. Obesity in children with autism spectrum disorder. Harv Rev Psychiatry. (2014) 22:93–103. doi: 10.1097/HRP.0000000000000031
32. Cheng N, Rho JM, Masino SA. Metabolic dysfunction underlying autism spectrum disorder and potential treatment approaches. Front Mol Neurosci. (2017) 10. doi: 10.3389/fnmol.2017.00034
33. Egan AM, Dreyer ML, Odar CC, Beckwith M, Garrison CB. Obesity in young children with autism spectrum disorders: prevalence and associated factors. Child Obes. (2013) 9:125–31. doi: 10.1089/chi.2012.0028
34. Chung EK, Romney MC. Social determinants of childhood obesity: beyond individual choices. Curr Pediatr Rev. (2012) 8:237–52. doi: 10.2174/157339612802139370
35. Gonzalez-Casanova I, Sarmiento OL, Pratt M, Gazmararian JA, Martorell R, Cunningham SA, et al. Individual, family, and community predictors of overweight and obesity among colombian children and adolescents. Prev Chronic Dis. (2014) 11:140065. doi: 10.5888/pcd11.140065
36. Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff. (2010) 29:503–12. doi: 10.1377/hlthaff.2009.0730
37. Mota J, Ribeiro JC, Carvalho J, Santos MP. The physical activity behaviors outside school and BMI in adolescents. J Phys Act Heal. (2010) 7:754–60. doi: 10.1123/jpah.7.6.754
38. Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. (2004) 5:4–85. doi: 10.1111/j.1467-789X.2004.00133.x
39. Gray DE. Ten years on: a longitudinal study of families of children with autism. J Intellect Dev Disabil. (2002) 27:215–22. doi: 10.1080/1366825021000008639
40. Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol. (2000) 55:647–54. doi: 10.1037/0003-066X.55.6.647
41. Shattuck PT, Grosse SD. Issues related to the diagnosis and treatment of autism spectrum disorders. Ment Retard Dev Disabil Res Rev. (2007) 13:129–35. doi: 10.1002/mrdd.20143
42. Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. (2008) 167:875–81. doi: 10.1093/aje/kwm390
43. Dunton GF, Liao Y, Intille SS, Spruijt-Metz D, Pentz M. Investigating children's physical activity and sedentary behavior using ecological momentary assessment with mobile phones. Obesity. (2011) 19:1205–12. doi: 10.1038/oby.2010.302
44. Kahathuduwa CN, West BD, Blume J, Dharavath N, Moustaid-Moussa N, Mastergeorge A. The risk of overweight and obesity in children with autism spectrum disorders: a systematic review and meta-analysis. Obes Rev. (2019) 20:1667–79. doi: 10.1111/obr.12933
45. Janjua NZ, Mahmood B, Islam MA, Goldenberg RL. Maternal and early childhood risk factors for overweight and obesity among low-income predominantly black children at age 5 years: a prospective cohort study. J Obes. (2012) 2012:1–9. doi: 10.1155/2012/457173
46. Melgar-Quiñonez HR, Kaiser LL. Relationship of child-feeding practices to overweight in low-income Mexican-American preschool-aged children. J Am Diet Assoc. (2004) 104:1110–9. doi: 10.1016/j.jada.2004.04.030
47. Brophy S, Cooksey R, Gravenor MB, Mistry R, Thomas N, Lyons RA, et al. Risk factors for childhood obesity at age 5: analysis of the millennium cohort study. BMC Public Health. (2009) 9. doi: 10.1186/1471-2458-9-467
48. Natale RA, Messiah SE, Asfour L, Uhlhorn SB, Delamater A, Arheart KL. Role modeling as an early childhood obesity prevention strategy: effect of parents and teachers on preschool children's healthy lifestyle habits. J Dev Behav Pediatr. (2014) 35:378–87. doi: 10.1097/DBP.0000000000000074
49. Toschke AM, Rückinger S, Böhler E, Von Kries R. Adjusted population attributable fractions and preventable potential of risk factors for childhood obesity. Public Health Nutr. (2007) 10:902–6. doi: 10.1017/S136898000725846X
50. Gable S, Chang Y, Krull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. J Am Diet Assoc. (2007) 107:53–61. doi: 10.1016/j.jada.2006.10.010
51. Durmuş B, Kruithof CJ, Gillman MH, Willemsen SP, Hofman A, Raat H, et al. Parental smoking during pregnancy, early growth, and risk of obesity in preschool children: the generation R study. Am J Clin Nutr. (2011) 94:164–71. doi: 10.3945/ajcn.110.009225
52. Koshy G, Delpisheh A, Brabin BJ. Dose response association of pregnancy cigarette smoke exposure, childhood stature, overweight and obesity. Eur J Public Health. (2011) 21:286–91. doi: 10.1093/eurpub/ckq173
53. Harris HR, Willett WC, Michels KB. Parental smoking during pregnancy and risk of overweight and obesity in the daughter. Int J Obes. (2013) 37:1356–63. doi: 10.1038/ijo.2013.101
54. Chen YC, Chen PC, Hsieh WS, Portnov BA, Chen YA, Lee YL. Environmental factors associated with overweight and obesity in Taiwanese children. Paediatr Perinat Epidemiol. (2012) 26:561–71. doi: 10.1111/ppe.12001
55. Gravel J, Potter B, Dubois L. Parental smoking and childhood obesity: is maternal smoking during pregnancy the critical exposure? Can J Diabetes. (2011) 35:147. doi: 10.1016/S1499-2671(11)52039-8
56. Sekine M, Yamagami T, Handa K, Saito T, Nanri S, Kawaminami K, et al. A dose-response relationship between short sleeping hours and childhood obesity: results of the Toyama birth cohort study. Child Care Health Dev. (2002) 28:163–70. doi: 10.1046/j.1365-2214.2002.00260.x
57. Dinges DF, Pack F, Williams K, Gillen KA, Powell JW, Ott GE, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 h per night. Sleep. (1997) 20:267–77. doi: 10.1093/sleep/20.4.267
58. Jiang F, Zhu S, Yan C, Jin X, Bandla H, Shen X. Sleep and obesity in preschool children. J Pediatr. (2009) 154:814–8. doi: 10.1016/j.jpeds.2008.12.043
59. Miller AL, Lumeng JC, Lebourgeois MK. Sleep patterns and obesity in childhood. Curr Opin Endocrinol Diabetes Obes. (2015) 22:41–7. doi: 10.1097/MED.0000000000000125
60. Diomedi M, Curatolo P, Scalise A, Placidi F, Caretto F, Gigli GL. Sleep abnormalities in mentally retarded autistic subjects: down's syndrome with mental retardation and normal subjects. Brain Dev. (1999) 21:548–53. doi: 10.1016/S0387-7604(99)00077-7
61. Elia M, Ferri R, Musumeci SA, Del Gracco S, Bottitta M, Scuderi C, et al. Sleep in subjects with autistic disorder: a neurophysiological and psychological study. Brain Dev. (2000) 22:88–92. doi: 10.1016/S0387-7604(99)00119-9
62. Godbout R, Bergeron C, Limoges É, Stip E, Mottron L. A laboratory study of sleep in Asperger's syndrome. Neuroreport. (2000) 11:127–30. doi: 10.1097/00001756-200001170-00025
63. Gruber KJ, Haldeman LA. Using the family to combat childhood and adult obesity. Prev Chronic Dis. (2009) 6:A106.
64. Huffman FG, Kanikireddy S, Patel M. Parenthood-a contributing factor to childhood obesity. Int J Environ Res Public Health. (2010) 7:2800–10. doi: 10.3390/ijerph7072800
65. Dallman MF, Pecoraro N, Akana SF, La Fleur SE, Gomez F, Houshyar H, et al. Chronic stress and obesity: a new view of “comfort food.” Proc Natl Acad Sci USA. (2003) 100:11696. doi: 10.1073/pnas.1934666100
66. Macht M. How emotions affect eating: a five-way model. Appetite. (2008) 50:1–11. doi: 10.1016/j.appet.2007.07.002
67. Carr D, Springer KW. Advances in families and health research in the 21st century. J Marriage Fam. (2010) 72:743–61. doi: 10.1111/j.1741-3737.2010.00728.x
68. Amato PR, Cheadle J. The long reach of divorce: divorce and child wellbeing across three generations. J Marriage Fam. (2005) 67:191–206. doi: 10.1111/j.0022-2445.2005.00014.x
69. Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, Davies WH. Controlled study of critical parent and family factors in the obesigenic environment. Obesity. (2007) 15:126. doi: 10.1038/oby.2007.517
70. Baker-Ericzén MJ, Brookman-Frazee L, Stahmer A. Stress levels and adaptability in parents of toddlers with and without autism spectrum disorders. Res Pract Pers with Sev Disabil. (2005) 30:194–204. doi: 10.2511/rpsd.30.4.194
71. Blacher J, McIntyre LL. Syndrome specificity and behavioral disorders in young adults with intellectual disability: cultural differences in family impact. J Intellect Disabil Res. (2006) 50:184–98. doi: 10.1111/j.1365-2788.2005.00768.x
72. Olsson MB, Hwang CP. Depression in mothers and fathers of children with intellectual disability. J Intellect Disabil Res. (2001) 45:535–43. doi: 10.1046/j.1365-2788.2001.00372.x
73. Sanders JL, Morgan SB. Family stress and adjustment as perceived by parents of children with autism or down syndrome: implications for intervention. Child Fam Behav Ther. (1997) 19:15–32. doi: 10.1300/J019v19n04_02
74. Bouma R, Schweitzer R. The impact of chronic childhood illness on family stress: a comparison between autism and cystic fibrosis. J Clin Psychol. (1990) 46:722–30. doi: 10.1002/1097-4679(199011)46:6<722::AID-JCLP2270460605>3.0.CO;2-6
75. Peters-Scheffer N, Didden R, Korzilius H, Matson J. Cost comparison of early intensive behavioral intervention and treatment as usual for children with autism spectrum disorder in the Netherlands. Res Dev Disabil. (2012) 33:1763–72. doi: 10.1016/j.ridd.2012.04.006
76. Phetrasuwan S, Shandor Miles M. Parenting stress in mothers of children with autism spectrum disorders. J Spec Pediatr Nurs. (2009) 14:157–65. doi: 10.1111/j.1744-6155.2009.00188.x
77. Tomanik S, Harris GE, Hawkins J. The relationship between behaviors exhibited by children with autism and maternal stress. J Intellect Dev Disabil. (2004) 29:16–26. doi: 10.1080/13668250410001662892
78. Kandiah J, Yake M, Jones J, Meyer M. Stress influences appetite and comfort food preferences in college women. Nutr Res. (2006) 26:118–23. doi: 10.1016/j.nutres.2005.11.010
79. Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. (2007) 91:449–58. doi: 10.1016/j.physbeh.2007.04.011
80. CDC. Strategies to Prevent Obesity and Other Chronic Diseases: The CDC Guide to Strategies to Support Breastfeeding Mothers and Babies (2013). Available online at: http://www.cdc.gov/breastfeeding (accessed September 26, 2021).
Keywords: Autism Spectrum Disorder, obesity, children, wellbeing, socioecological factors
Citation: Kim T and Kwon EH (2022) Investigating socioecological obesogenic factors in children with Autism Spectrum Disorder. Front. Public Health 10:867456. doi: 10.3389/fpubh.2022.867456
Received: 01 February 2022; Accepted: 21 September 2022;
Published: 06 October 2022.
Edited by:
Rita Barone, University of Catania, ItalyReviewed by:
Poh Ying Lim, Putra Malaysia University, MalaysiaCopyright © 2022 Kim and Kwon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eun Hye Kwon, ZXVuaHllLmt3b25AdGFtdXNhLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.