- 1Department of Pharmacy Practice, College of Pharmacy, AlMaarefa University, Riyadh, Saudi Arabia
- 2Pharm.D Student, College of Pharmacy, AlMaarefa University, Riyadh, Saudi Arabia
- 3Consultant Family Medicine, Armed Forces Hospitals, Khamis Mushayt, Saudi Arabia
- 4Clinical and Hospital Pharmacy Department, College of Pharmacy, Taibah University, Al-Madinah Al-Munawwarah, Saudi Arabia
- 5Department of Clinical Pharmacy, School of Pharmacy, Management and Science University, University Drive, Shah Alam, Malaysia
- 6General Practitioner Physician at Almansk PHCC, Directorate of Health Affairs in Asir Region, Ministry of Health, Abha, Saudi Arabia
- 7Department of Family and Community Medicine, College of Medicine, Najran University, Najran, Saudi Arabia
- 8Department of Pharmacology, College of Pharmacy, Najran University, Najran, Saudi Arabia
- 9Medical Department, College of Medicine, Najran University, Najran, Saudi Arabia
Irrational Self-Medication (SM) practice leads to incorrect diagnosis and is a risk factor for disease exacerbation and serious health consequences. Hence Responsible SM is vital for better health outcomes. In the present community-based study we explored the SM practice during the last 3 months, frequency, outcome, medications used, reasons influencing SM, source of the drug, and information. Data were analyzed using SPSS; chi-square test was performed to indicate significance, Odds ratio, Pearson correlation, univariant and multivariant regression analysis were performed to find out factors and predictors of SM. A total of 611 residents completed the survey. SM was practiced by 52.9% of participants during the last 3 months, with a frequency of one to two times. Headache (64.8%), pain (35.4%), fever/flu (31.4%), cold & cough (21.9%) and dysmenorrhea (20.9%) were illnesses managed using pain killers (75.9%), multivitamins (25.5%), anti-pyretic (24.7%) and herbal medicines (18.5%). Minor illness (67.9%), earlier experience (33.9%) and shortness of time to attend healthcare facilities (18.8%) were the reasons for practicing SM. Distance to healthcare and routine physical activity have significantly influenced the SM practice. Residents stated that inappropriate SM would lead to negative outcomes, including drug side effects (70%), Interaction (34.2%), poor treatment outcome (32.6%) and return of symptoms (26.5%). Interestingly, two-thirds of participants (68.9%) have recommended SM in case of minor illnesses only, 85.3% of respondents have expressed their desire to learn more about appropriate SM, and 76.6% are willing to return their leftover or unused medications to drug take-back centers.
Introduction
“An attribute which differentiates man from animals is the wish to take medicine,” as stated by William Osler (1). Everyone practices Self-care (SC), and it's not new. The world health organization (WHO) defines self-care as “The ability of individuals, families and communities to promote health, prevent disease, maintain health, and cope with illness and disability with or without the support of a healthcare provider” (2). SC is a key element for better health outcomes and existed well ahead of formal health systems. SC remains a key factor for maintaining health, although healthcare systems do exist (3). Every individual exercise Self-medication (SM) as a part of SC of their health (4). The activity pratctised individually or directed by someone to handle the minor health illnesses is regarded as SM. This definition spells out that all medications cannot be taken on one's own initiative, doctor's prescription is necessary for some medications and medical supervision is essential and clarifies that there is a rational position for SM in developed societies (5). Using leftover medications or medications received from family and friends, including over the counter (OTC) drugs, is considered SM practice (6).
Although SC and SM are essential components of healthcare provision, SM poses benefits and risks. The United States Food and Drug Authority (FDA) defines OTC medicines as “drugs that are safe and effective for use by the general public without seeking treatment by a health professional” (5). Worldwide, it is an acceptable practice to use OTC medications without a prescription (4). As per the WHO's statement, rational SM has numerous benefits in managing several minor health conditions which doesn't require prior medical consultation. Furthermore, SM is an inexpensive replacement that provide several benefits to the patients including increased accesses to treatment, reduce treatment cost and visit to doctors hence decreases the load on health care facilities (5).
Despite all this, irrational and irresponsible SM comes with countless adverse health consequences including low drug efficacy, resistance and tolerance to certain medicines, extreme side effects, drug intolerance, mask the actual diagnosis, numerous drug and food interactions, dependence, under or overdose of drugs, toxicity of drugs and withdrawal symptoms (7). Moreover, inappropriate practice of SM possess numerous potential risks for the individual consumer including incorrect self-diagnosis, failure to seek appropriate medical advice promptly, incorrect choice of therapy, inability to identify certain pharmacological risks, some rare but sever adverse effects, failure to detect contraindications, warnings, precautions and interactions, failure to identify that same medication is consumed under different brand name, failure to report present SM to the prescribing physician, wrong rout or frequency of administration, unnecessary prolonged use, incorrect or prolonged storage of medication than specified by the manufacturer or dispenser, drug induced disease or hospitalization and wasting of public health expenditure. Therefore, the SM should be practiced with the aim of maximizing the benefits and minimizing the above-mentioned risk and adverse consequences (5).
Such preventable adverse consequences of irrational SM practices should be highlighted to the community and acquiring an educational approach toward health education to curb it. The inappropriate practice of SM is increasing steadily in developing countries, approximately as developed countries, prevailing it as a public health concern (8). Apart from harming the patient's health, inappropriate SM also increases treatment cost and frequency of hospital admission.
WHO estimates a projected shortfall of 18 million health workers by 2030, mostly in low- and lower-middle-income countries (9). Hence some countries encourage their residents to adopt SC behavior to manage trivial illnesses including SM. The Responsible SM helps reduce the cost of treatment, traveling time, and consultation time (4, 10). While SM practice's commonness varies from one country to another, the familiar factor that influences SM includes age, gender, income, educational level, medical knowledge, and trivial illnesses (11, 12). Numerous studies have reported the following factors as common reasons to indulge in SM practice; minor illness, previous experience with similar health problems, financial limitations, unavailability of healthcare, waiting time in healthcare facilities, and easy access to OTC drugs (13, 14). Nevertheless, the growing trend of advertisements by pharmaceutical companies, media, and the Internet has largely promoted SM behavior (12, 15). In Saudi Arabia, SM is practiced by all ages, including students, teenagers, adults, and parents (14, 16, 17).
Several studies conducted across the world, including Bangladesh (18), India (19), Ethiopia (20) and Egypt (21), have highlighted the factors contributing to the promotion of SM practice and identified the key factors responsible for irrational SM. Various national studies targeting people and patients who visited community pharmacies, primary healthcare centers and hospitals have been conducted to explore the prevalence of SM (22–25). A few studies were conducted to determine SM with antibiotics (26). The previous two SM studies conducted in Riyadh city almost a decade ago (24, 25) mainly targeted people who attended primary health care centers and community pharmacies. In both studies, male participation was dominant. We conducted this study to determine the prevalence of SM and its pattern among all residents above 18 years of age residing in Riyadh city. Additionally, efforts were made to gather information about frequency of SM during last 3 months, source of drug information, place of obtaining medications, outcomes of SM and reason influencing such practice along with their opinions, recommendations, and impact of covid-19 on SM practice.
Materials and Methods
Study Design and Population
The present community-based cross-sectional study was carried out to explore the prevalence of self-medication, factors, and suggestions to limit irrational SM practice. The study was conducted between September and October 2021 among residents aged 18 and above of Riyadh, Saudi Arabia. The institutional review board of AlMaarefa University (UM) approved the study with the registration number (02-20102021). The study population was divided into 5 geographical areas in Riyadh city: North, South, East, West, and Central. The residents under 18 years of age, residing outside of Riyadh, staying in Saudi Arabia on visit visas and students of UM (in recent past, SM study has been conducted on UM students) were excluded from the participation. The informed consent was displayed at the beginning of the online survey and the study purpose. Participation was voluntary; they had participation option to choose either agree or disagree. Those who selected disagree option were directed to decline the participation section and finish participation.
Approach to Convey the Study Purpose and Its Criteria to Participants Effectively
We tried to convey our study's purpose, significance, and criteria through a short video clip [https://youtu.be/KC-E8WiGxjY]. The video clip was uploaded at the beginning of the study and the consent form. Considering that in-person interaction and briefing about the work was not possible with all participants, residents may be reluctant to have any face-to-face interaction due to ongoing Covid-19 pandemic. Lastly, it may be convenient for low educated and elderly participants to refer to video rather than reading. Watching the video was not mandatory; participants could skip the video and attempt the survey if they wish to do so. This approach describes the study purpose and encourages the residents to participate.
Sample Size and Sampling Method
We calculated the sample size by estimating the total population of Riyadh in 2021 to be 7,387,817 as reported by World Population Review [https://worldpopulationreview.com/world-cities/riyadh-population]. Sample size was calculated using Raosoft sample size calculator by presuming a 95% confidence level, 5% margin of error, and precision level of 5%, yielding a sample size of 385. We adopted convenience and snowball sampling techniques to collect the data.
Questionnaire Construction
The questionnaire was developed based on a review of relevant literature. We referred three local (Riyadh, Hail and Abha) and four international (India, Bangladesh, Egypt and Ethiopia) studies addressing our topic of interest among community and educational institutes to draft the study tool (14, 17–22). The study tool was subjected to extensive revision to fit the characteristics of the study population. A self-administered questionnaire was categorized into sections. The first section addressed sociodemographic information about participants such as gender, age, education, occupation, marital status, number of children at home, distance to nearest hospital and pharmacy, health insurance, family member working in the health sector, etc. The second segment measured the SM pattern including SM practice during the last 3 months, frequency and outcome of SM, common medical illnesses for which SM was practiced, type of drug used, source of drug information, place of obtaining the drug. The third sections measured reasons influencing SM practice, the negative impact of inappropriate SM and adverse outcome of SM and steps taken to overcome such events. The fourth part was developed to record the participants' opinions toward SM, including their recommendation, willingness to return unused medications, spreading awareness, and the impact of Covid-19 on SM practice.
Validity, Reliability of Study Tool and Data Collection
The experts from the college of pharmacy, community Pharmacist and Epidemiologist completed the review and evaluation of the questionnaire draft to ensure content validity. The questionnaire was translated into Arabic language by independent professional translator and then back translated to English version through another professional translator to ensure the similarity. The final questionnaire was displayed online bilingually. The face validity was tested by conducting a pilot study on 25 residents (5 participants were randomly selected from each region of Riyadh city), aged between 20 and 50 years. The comments from pilot respondents were, to reduce the number of questions, to simplify the English terminologies for drug class such as mentioning Fever lowering drugs instead of antipyretics and number of children part in the socio-demographic section was changed to a number of children under 18 years of age staying with you, because some respondents mentioned they have children but not staying with them in the city, so that may not have any influence on their SM practice. The data of pilot participants was not included in the final analysis. Moreover, questionnaire reliability was measured by calculating the Cronbach's alpha factor for the questions addressing prevalence, frequency, health outcome, adverse consequences and their management and viewpoint toward self-medication (0.82). The social media platforms and personal contacts were used to distribute the online questionnaire.
Statistical Analysis
The collected responses were evaluated for their completeness and consistency. Disagreed and incomplete responses were excluded from the analysis. The SPSS (version 27.0, IBM, New York, NY, USA) was used to analyze the data. Cross-tabulation was performed by applying the chi-square test. The odds ratio was calculated to estimate the risk of SM practice; Pearson's correlation was done to establish the link between opinions with SM practice during the last 3 months. Multivariant logistic regression was performed to find the relationship between independent predictors and SM practice. A p-value of <0.05 was considered significant.
Results
Sociodemographic Details
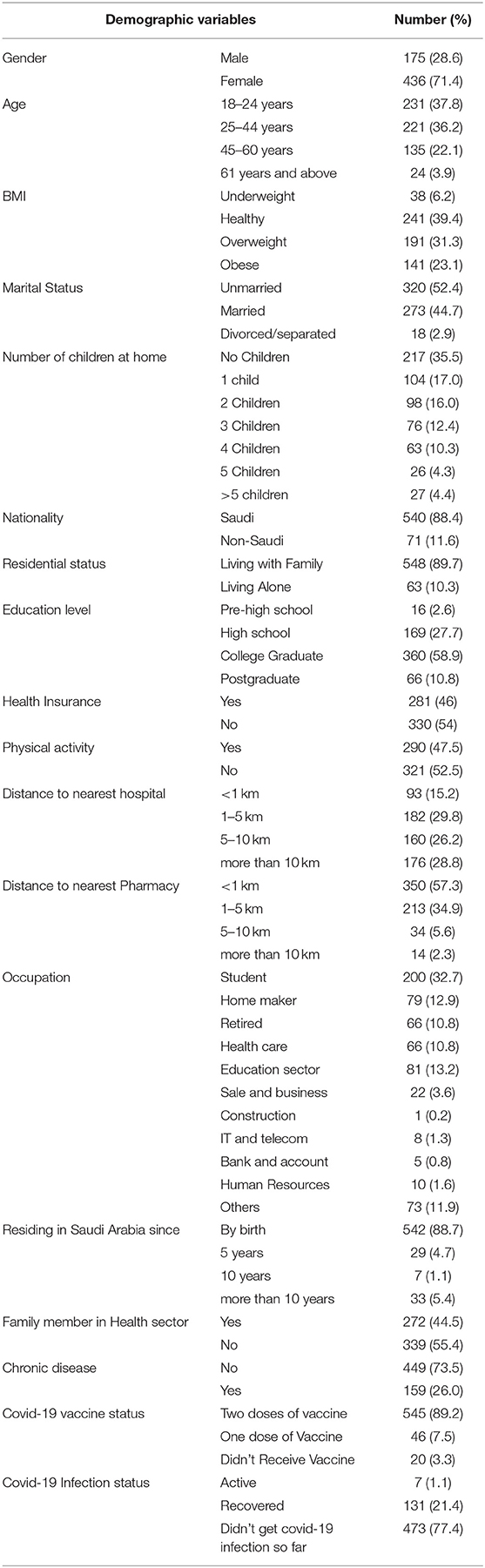
Thankfully, 91 participants viewed the video clip uploaded at the beginning of questionnaire, indicating it's usefulness. Overall, 625 residents attempted the survey link, out of which 14 disagreed to participate. Hence a total of 611 responses were subjected for data analysis. Major participants were from North of Riyadh (200), followed by Central (110), East (108), West (101) and South parts of the city. Highest participants were females (71.4%); unmarried (52.4%); Saudi citizens (88.4%) and staying with family (89.7%). Regarding Covid-19 vaccination, 545 (89.2%) took two vaccine doses (Table 1).
Prevalence of Self-Medication During Last 3 Months
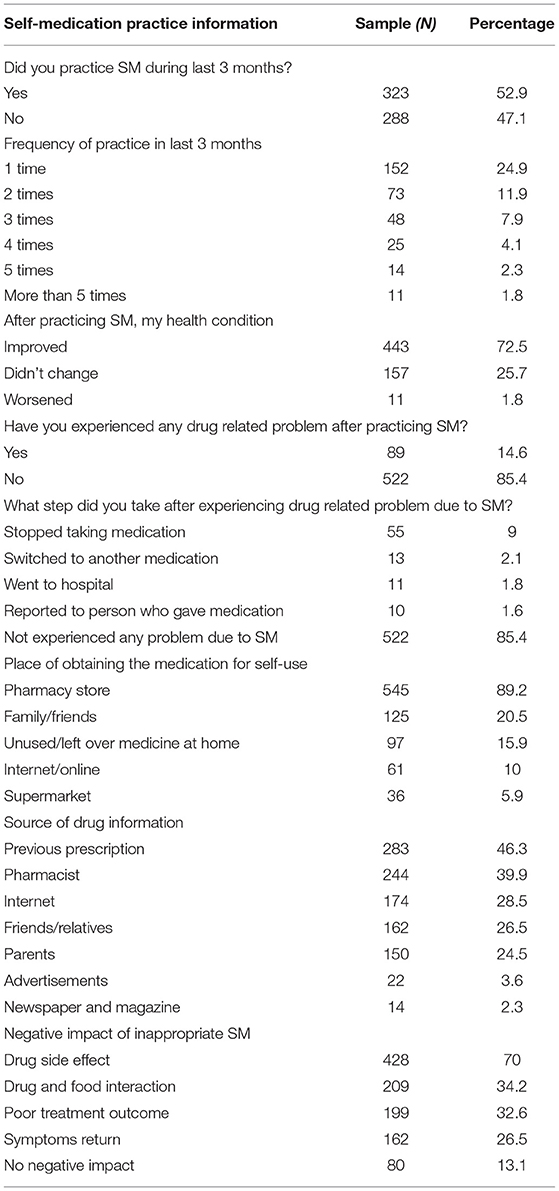
The prevalence of SM is increasing globally, and its rational practice warrant the benefits. Overall, 52.9% have practiced SM during the last 3 months. About one-fourth of participants (24.9%) have practiced SM just one time during the last 3 months. More than two-thirds of participants (72.5%) stated that their health condition improved after practicing SM. About eighty-nine (14.6%) residents mentioned that they experienced some drug-related problems after practicing SM. Out of these, fifty-five (9%) stated they stopped taking medications, and 2% switched to another drug to overcome the drug-related problems (Table 2).
Source of Information and Place of Obtaining the Drugs for SM
Sources utilized to obtain drug information and to collect the medications influence the appropriateness of SM practice. Overall, half of the participants mentioned previous prescriptions (46.3%) and pharmacists (39.9%) as a main source to obtain drug information. Newspapers, magazines (2.3%) and advertisements (3.6%) were the least referred sources to obtain drug information. Almost 90% of respondents mentioned a Pharmacy store as a prime place to obtain drugs for SM, followed by family & friends (20.5%) and unused/leftover medications (15.9%). Interestingly, respondents reported drug side effects (70%), Interaction (34.2%), poor treatment outcome (32.6%) and return of symptoms (26.5%) as significant adverse consequences of practicing inappropriate SM (Table 2).
Illnesses and Class of Drugs Used to Practice SM
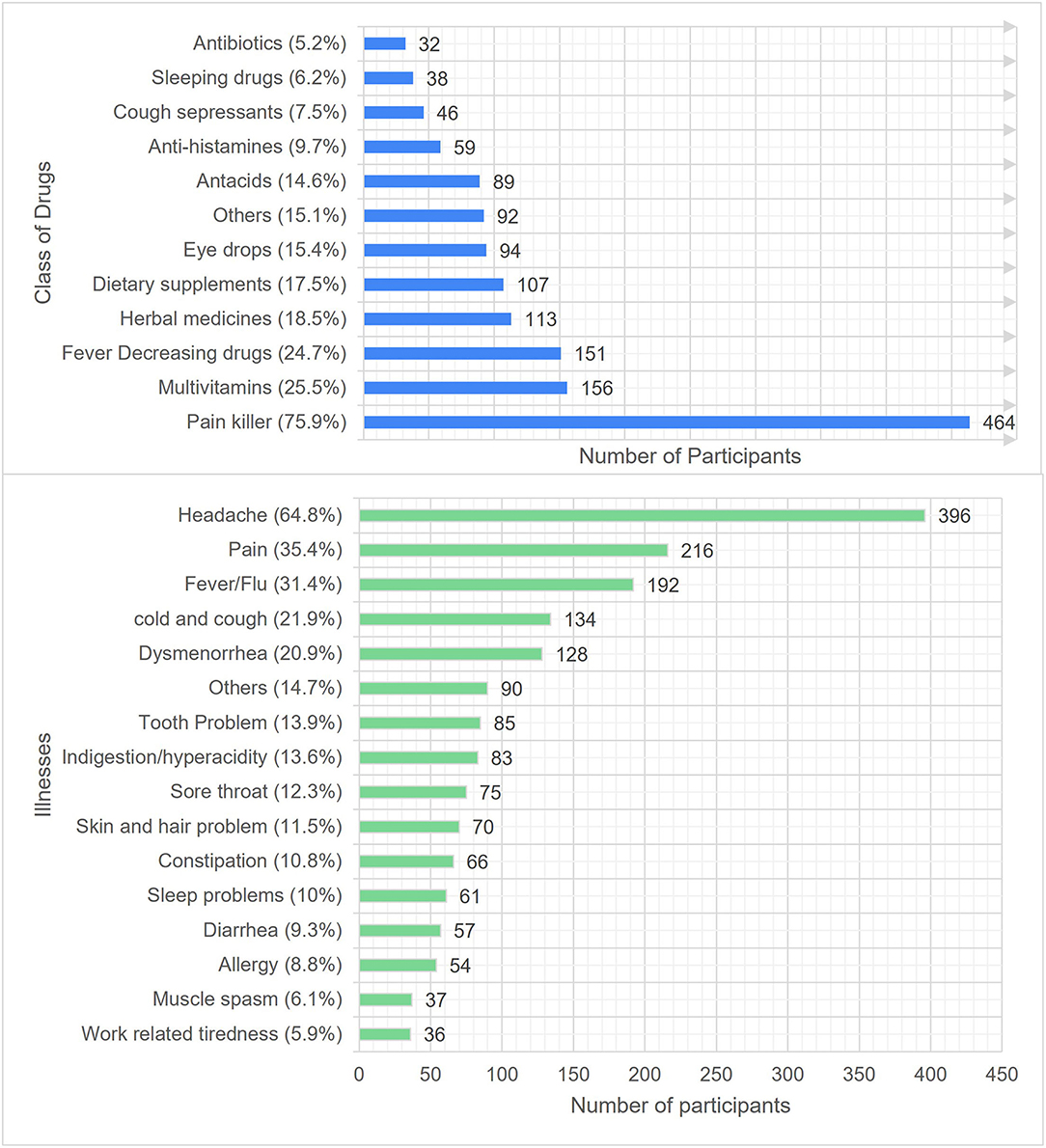
Use of OTC medications to manage the trivial illnesses is an indication of rational SM practice. Furthermore, good level of awareness regarding consequences of inappropriate SM encourages the individual consumer to practice SM consciously and seek essential medical advice. The Figure 1 depicts type of illnesses and classes of drugs used to practice SM. Most respondents have reported using pain killers (75.9%), multivitamins (25.5%), antipyretic (24.7%), herbal medicines (18.5%) and dietary supplements (17.5%) to self-treat the illnesses, including headache (64.8%), pain (35.4%), fever/flu (31.4%), cold & cough (21.9%) and dysmenorrhea (20.9%) during last 3 months. On the other hand, the use of antibiotics (5.2%) and sleeping aids (6.2%) were the least commons. The use of other drugs (15.1%) includes anti-emetics, anti-inflammatory, laxatives and topical medications. Similarly, other illnesses (14.7%) include vomiting, mouth ulcer, stress, eye infections and bodybuilding.
Reasons Impacting SM Practice
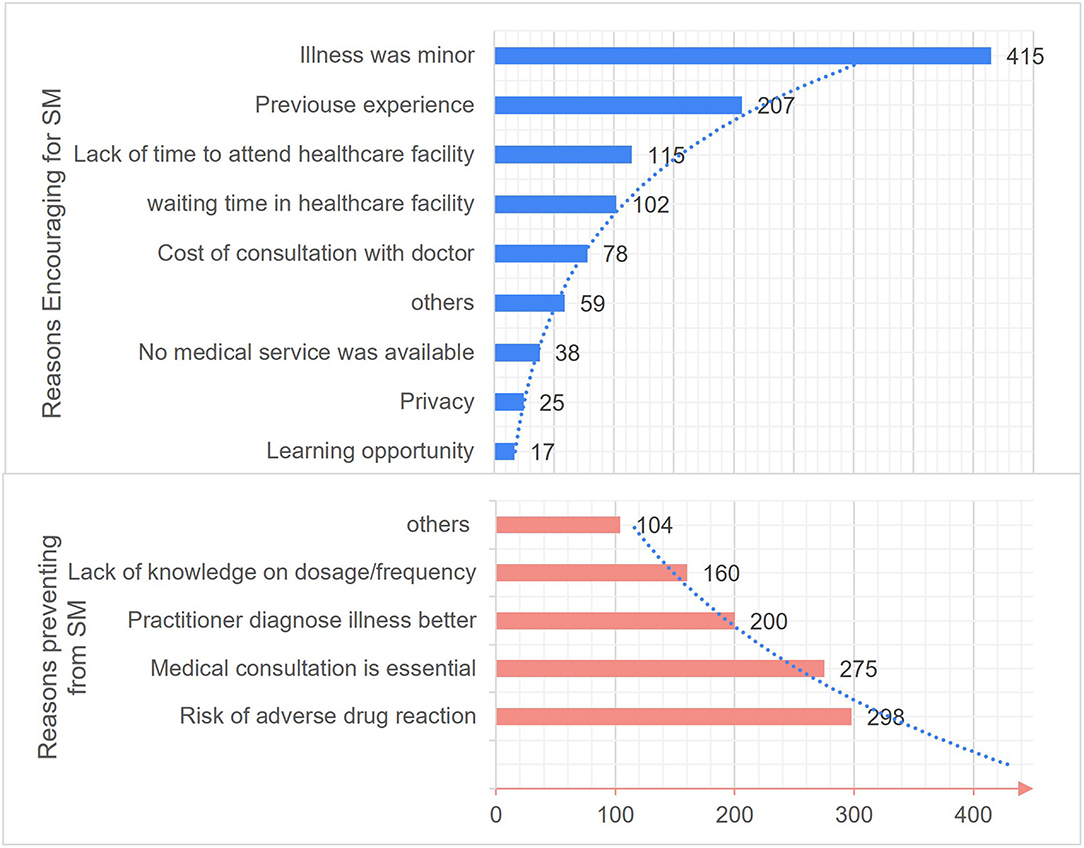
The reasons modulating SM practice are depicted in Figure 2. The most common reasons reported by residents as encouraging factors to practice SM includes minor illness (67.9%), earlier experience (33.9%) and shortness of time to attend healthcare facility (18.8%). Excitingly, only a few (2.8%) respondents mentioned that they practiced SM as a learning opportunity. Contrastingly, the typical reasons preventing from practicing SM were risk of adverse reactions (48.8%), the importance of medical consultation (45%), believing in medical practitioner's ability of illness diagnoses (32.7%) and lack of knowledge on dosage and frequency (26.2%).
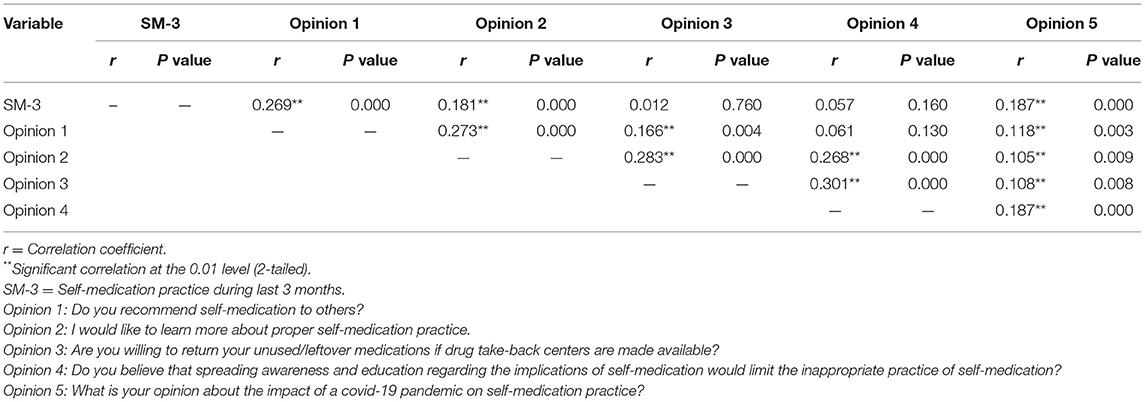
Correlation Between SM Practice With Opinions
Pearson correlation analysis revealed the significant positive correlation between SM during last 3 months and opinions 1, 2 and 5. It indicates that those with SM-3 recommend others to practice SM, would like to learn more about SM and assume that covid-19 has increased the practice of SM. Interestingly, all the opinions were positively correlated with each other (Table 3).
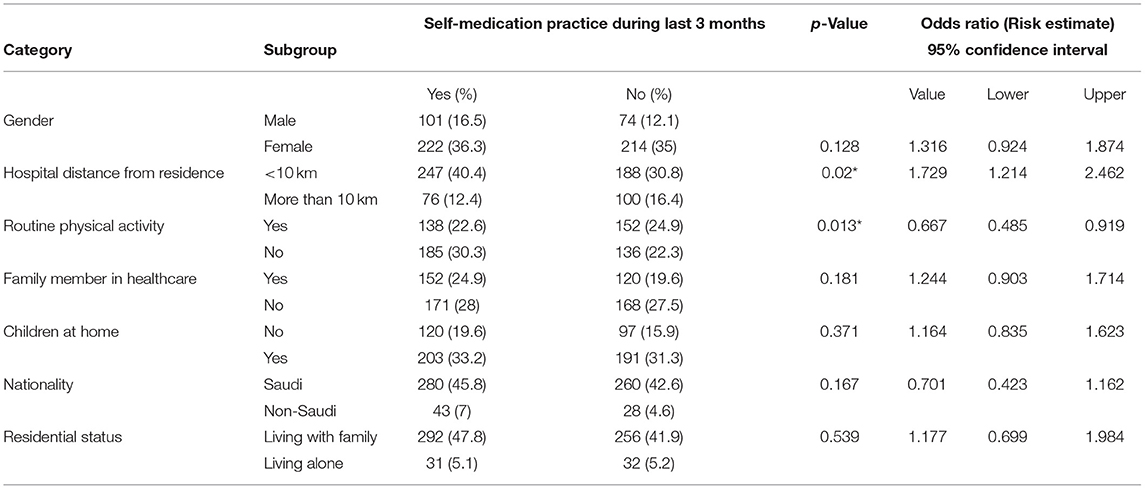
Factors Influencing Self-Medication Practice
Binary logistic analysis was performed to identify the factors influencing SM practice. We didn't observe any significant impact of gender, nationality, residence status, children at home, and family members working in the health sector. Conversely, performing routine physical activity and distance to the nearest hospital from residence showed a significant (p = 0.013 and p = 0.02) impact on SM practice. The residents who were not performing routine physical exercise had 0.6 times high risk of indulging in SM practice than those who performed routine physical activity. Similarly, participants whose residence was more than 10 km away from the healthcare facility have a 1.7 times higher risk of practicing SM than residents staying near the healthcare facility (Table 4).
The variables showing a significant correlation in binary logistic regression were put through multivariant regression analysis to determine individual predictors of SM practice. After fine-tuning potential confounding factors, the distance to healthcare facility from residence, and routine physical activity were significant independent predictors of SM (Table 5). The participants who reside at <10 km to healthcare facility have 0.55 times less likelihood of practicing SM than participants who reside more than 10 km from a health care facility. Surprisingly, residents who perform routine physical activity were predicted to practice SM 1.5 times more than those who don't perform any routine physical activity.
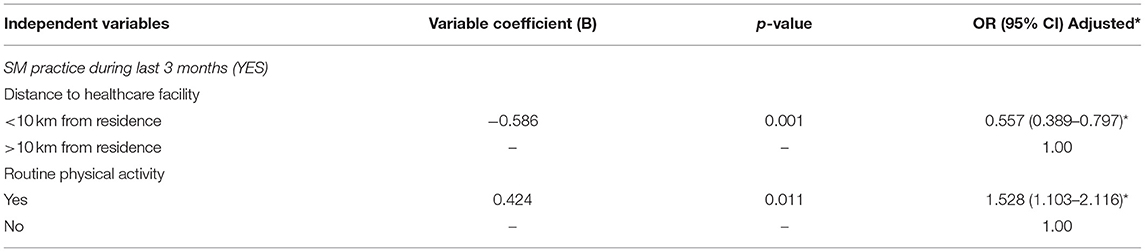
Table 5. Multivariant logistic regression analysis identifying the variables associated with the self-medication during the last 3 months.
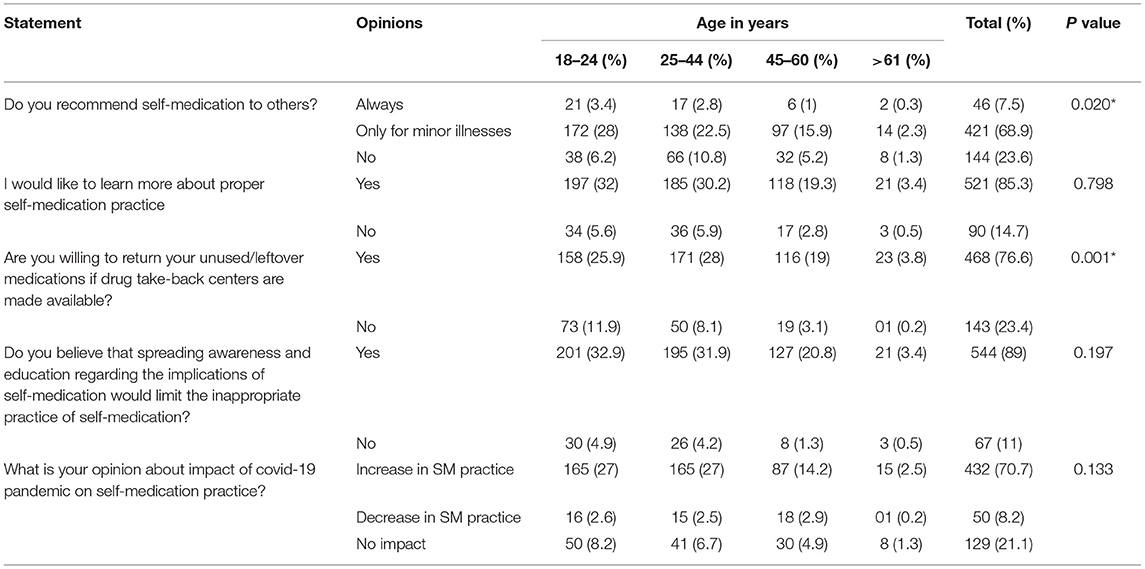
Opinions and Recommendations Toward Self-Medication
We collected a few opinions from our study participants at the end of this questionnaire. Interestingly, two-thirds of participants (68.9%) have recommended SM practice to others in case of minor illnesses only. Likewise, most respondents (85.3%) have expressed their desire to learn more about appropriate SM practices. Similarly, most respondents (76.6%) are willing to return their leftover or unused medications to drug take-back centers. Most residents (89%), believe that spreading awareness about the implications of SM would rationalize and improve the SM practice. Expectedly, about 70% of participants assume that the emergence of covid-19 infection has led to increased SM practice (Table 6). Our study noticed a significant difference in opinions 1 and 3 among different age groups.
Discussion
Although SM is a part of self-care and supported by WHO to manage numerous minor illnesses that don't require medical consultation, its effectiveness is primarily determined by appropriateness and rational use. Hence inappropriate and irrational SM leads to dosage and treatment errors, adverse drug events, and risk of addiction or abuse. Although SM poses numerous advantages, yet it's largely determined by who uses it and how it is practiced.
The earlier two studies conducted in Riyadh to address the SM issue were “Self-medication in central Saudi Arabia: community pharmacy consumers perspective” in 2011 (25) and “Self-medication practice among patients in a public health care system” in 2009 (24). The 2011 study targeted people visiting community pharmacies in Riyadh, whereas a 2009 study was conducted on patients attending primary healthcare centers. However, our study was aimed at all the residents of Riyadh, from age 18 years and above.
Additionally, our study gathered information regarding Covid-19 infection and vaccine's impact on SM, opinion, and recommendations of residents about SM and adverse outcome of SM and their actions to resolve those outcomes. Our study shows that respondents who had practiced SM during the last 3 months were 323 (52.9%), which was lower compared (81.3%) to the regional study of SM for oral health among adults of Riyadh (63.25%) (27), residents of Medina city (28) and international studies from Savar residents (60.2%), in Bangladesh (18), Addis Ababa community (75.5%) Ethiopia (20), people attending oral health program in Tamil Nadu (69.32%) India (19), patients attending El-Mahsama family practice clinic, Ismailia (96%) Egypt (21), a community of Karachi (84.8%) Pakistan (29) and higher (45.4%) compared to the residents of Wuhan, China (30).
Correlating our outcomes with earlier studies (18, 23, 25, 30), where SM was significantly influenced by age, gender, education, occupation and marital status, our study found a significant impact of physical activity and distance to a healthcare facility on the practice of SM. Most respondents (72.5%) stated that their health condition improved after practicing SM, a similar outcome was noted among Addis Ababa Community Ethiopia (20). About half of respondents (55.5%) consider SM as a safe exercise, which is higher compared to the findings from residents of Hail (22), Saudi Arabia (33.5%).
The most common illnesses for which SM was practiced includes headache (64.8%), pain (35.4%), fever/flu (31.4%) and cold and cough (21.9%). Similar findings have been noted in earlier studies (19–23, 28–30). The typical classes of drugs used to practice SM were pain killers (75.9%), multivitamins (25.5%) and antipyretics (24.7%), which are in parallel with the findings of previous studies (19–21, 27, 28) and community pharmacy consumers of Al-Qassim province (31).
Interestingly, antibiotics were the least (5.2%) commonly used medication to practice SM, which are contrary to the finding from Egypt (21) (23.5%), antibiotic use in Saudi Arabia (26) (43.4%), Medina (28) (15.3%), SM for oral health among adults (27) of Riyadh (17.79%) and Qassim (31) (13.8%). Whereas study conducted on a community of Karachi, Pakistan (29) showed much lower (1.2%) use of antibiotics for self-care compared with our findings. Surprisingly, about 18.5% of our participants used herbal products for SM, which are like the findings of Addis Ababa (20) (16%). Likewise, 17.55 of participants used dietary supplements for self-care. The use of such conventional products would be related to the ongoing Covid-19 phase, reluctance to visit healthcare facilities and recommendations from family and friends.
The reinforcing reasons for SM practice mentioned in our study were trivial illness, previous experience, lack of time and waiting time in healthcare facilities like earlier studies conducted in Riyadh. Similar findings were observed in earlier studies (18–20, 28, 30, 31). Whereas studies conducted in Karachi, Pakistan (29) and Ismailia, Egypt (21) indicated convenience, cost-saving and previous experience as major reasons to opt for SM practice. Interestingly, few (2.8%) participants practiced SM as a learning opportunity, which indicates their responsible behavior toward medications and SM. About 47% of residents haven't practiced any SM during the last 3 months. The most common reasons which discouraged them were the risk of adverse drug reaction (48.77%), feeling that medication consultation is necessary (45%), and expertise of medical practitioners in disease diagnosis (32.7%). Parallel to our finding, the study conducted among a community of Addis, Ababa, Ethiopia (20) also found fear of wrong diagnosis, wrong drug and side effects as typical reasons which discouraged SM practice.
Easy availability of medications may encourage SM. The frequent place for obtaining medications for self-care was pharmacy store (89.2%), followed by borrowing medicines from family & friends (20.5%) and use of leftover medications (15.9%). Similar observations were noted among the studies conducted in Bangladesh (18), Addis Ababa (20), rural population in South-western Saudi Arabia (23) and residents of Karachi city, Pakistan (29). Although some OTC medications are available at the supermarket in Saudi Arabia, only a few residents (5.9%) preferred to buy them from Non-pharmacy stores. This behavior indicates the importance of pharmacist and their advice on SM. We noticed that residents of Riyadh city relied on previous prescriptions (46.3%), pharmacists (39.9%), the Internet (28.5%) and family/friends (26.5%) to get the information about medications which they prefer to self-medicate. These findings are in line with earlier study outcomes (20, 21, 25, 28, 30).
Irrational SM not only leads to an incorrect diagnosis but is also a risk factor for exacerbation of disease and severe health consequences. Residents of Riyadh city have depicted consciousness regarding the negative impact of irresponsible SM practice. The most common impact of inappropriate SM stated is a drug side effect (70%) followed by drug interactions (34.2%), poor health outcome (32.6%) and return of symptoms (26.5%). The participants of this study have shared their opinions and recommendations related to SM. About two-thirds (68.9%) of residents have recommended SM practice only for minor illnesses. Likewise, 85.3% have expressed their wish to return unused/leftover medications to drug take bac centers. The majority (85.3%) are willing to learn more about proper SM, whereas 89% recommend spreading awareness about rational SM practice. Eventually, respondents have also mentioned their view on the impact of ongoing Covid-19 on SM practice. About 70.7% of study participants believe that SM practice has increased during this Covid-19 phase.
Strengths and Limitations
Although we needed a sample of 385, we could gather 611 responses from all the regions of Riyadh. We restricted the recall questions (“Did you practice SM during last 3 months?” and “Frequency of practice in last 3 months”) to the last 3 months in the SM practice section to avoid recall bias and get a more realistic return. Because in-personal interaction and briefing about the work are not possible with all participants, residents may be reluctant to have any face-to-face interaction due to the ongoing Covid-19 pandemic. Lastly, it may be convenient for low educated and elderly participants to refer to video rather than reading. We tried to convey our study's purpose, significance, and criteria through a short video clip. The video clip was uploaded at the beginning of the study along with the consent form. We approached the residents through convenient and snowball sampling techniques.
Conclusion
SM has been practiced by about half of the respondents in the recent 3 months. Interestingly, the majority have utilized over-the-counter medications to treat minor and self-diagnosable ailments. Most of them got their medications from a pharmacy and learned about the drugs from the pharmacist. Furthermore, residents have demonstrated a high level of awareness of the detrimental consequences of irrational SM. Only common mild ailments should be treated with SM, according to respondents. They have also stated a desire to return their unneeded and leftover drugs to drug take-back centers, thereby curbing inappropriate SM and decreasing drug storage responsibilities at homes as well as wasteful medication borrowing among friends and relatives. For promoting rational self-medication practices, patient health awareness programs, community pharmacist assistance, continuing medical education programs for health care providers, and planned interventions in the media, such as newspapers, magazines, and television are required.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of AlMaarefa University (UM) approved the study with the registration number (02-20102021). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BM, SAA, and IS devised the project and conceptualized the ideas. JA, MSA, and AA-Q were involved in the literature review. SMBA, NO, and SOA participated in the study design and evaluation of the questionnaire. BM, SMBA, and SAA assisted in data collection and data entry. BM and MYA performed data analysis and drafting of the manuscript. NO, JA, and AA-Q contributed substantially to manuscript revision. All authors have read and agreed to the published version of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The authors are thankful to the Deanship of Scientific Research, Najran University, Najran, Saudi Arabia, for supporting this research through grant research code NU/RC/MRC/11/3.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
BM would like to express his gratitude to AlMaarefa University, Riyadh, Saudi Arabia, for providing funding (TUMA-2021-36) to do this research.
References
1. Phalke VD, Phalke DB, Durgawale PM. Self-medication practices in rural Maharashtra. Indian J Community Med. (2006) 31:34–5. doi: 10.4103/0970-0218.54933
2. World Health Organization (WHO). Human Reproduction Program, Q+A About Self Care. Available online at: https://www.who.int/reproductivehealth/self-care-interventions/questions-answers-self-care.pdf?ua=1 (accessed January 20, 2022).
3. Manjulaa Narasimhan. Self care interventions to advance health and wellbeing: a conceptual framework to inform normative guidance. BMJ. (2019) 365:l688. doi: 10.1136/bmj.l688
4. Vizhi SK, Senapathi R. Evaluation of the perception, attitude and practice of self-medication among business students in 3 select cities, South India. Int J Enterp Innov Manage Stud. (2010)1:40–4.
5. WHO. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication. WHO Drug Information. (2000). Available online at: https://apps.who.int/iris/handle/10665/66154 (accessed January 20, 2022).
6. Ocan M, Obuku EA, Bwanga F, Akena D, Richard S, Ogwal-Okeng J, et al. Household antimicrobial self-medication: a systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health. (2015) 15:742–52. doi: 10.1186/s12889-015-2109-3
7. Bennadi D. Self-medication: a current challenge. J Basic Clin Pharm. (2014) 5:19. doi: 10.4103/0976-0105.128253
8. Kasulkar A, Gupta M. Self medication practices among medical students of a private institute. Indian J Pharm Sci. (2015) 77:178. doi: 10.4103/0250-474X.156569
9. WHO. Health Workforce. Available online at: https://www.who.int/health-topics/health-workforce#tab=tab_1 (accessed January 20, 2022).
10. Porteous T, Bond C, Hannaford P, Sinclair H. How and why are non-prescription analgesics used in Scotland? Fam Pract. (2005) 22:78–85. doi: 10.1093/fampra/cmh719
11. Abay SM, Amelo W. Assessment of self-medication practices among medical, pharmacy, and health science students in Gondar University, Ethiopia. J Young Pharm. (2010) 2:306–310. doi: 10.4103/0975-1483.66798
12. Klemenc-Ketis Z, Hladnik Z, Kersnik J. A cross sectional study of sex differences in self-medication practices among university students in Slovenia. Coll Antropol. (2011) 35:329–34.
13. Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self medication. Drug Saf . (2001) 24:1027–37. doi: 10.2165/00002018-200124140-00002
14. Mannasaheb BA, AlYamani MJ, Alajlan SA, Alqahtani LM, Alsuhimi SE, Almuzaini RI, et al. Knowledge, attitude, practices and viewpoints of undergraduate university students towards self-medication: an institution-based study in Riyadh. Int J Environ Res Public Health. (2021) 18:8545. doi: 10.3390/ijerph18168545
15. Burak LJ, Damico A. College students' use of widely advertised medications. J Am Coll Health. (2000) 49:118–21. doi: 10.1080/07448480009596293
16. Bawazir SA. Prescribing pattern at community pharmacies in Saudi Arabia. Int Pharm J. (1992) 6:5.
17. Alshahrani SM, Alavudeen SS, Alakhali KM, Al-Worafi YM, Bahamdan AK, Vigneshwaran E. Self-medication among king khalid university students, Saudi Arabia. Risk Manag Healthc Policy. (2019) 12:243–249. doi: 10.2147/RMHP.S230257
18. Mst Sabrina Moonajilin, Mohammed A Mamun, Md Estiar Rahman, Md Firoz Mahmud, HM Shamim Al Mamun, Md Sajib Rana, et al. Prevalence and drivers of self-medication practices among Savar Residents in Bangladesh: a cross-sectional study. Risk Manag Healthc Policy. (2020) 13:743–52. doi: 10.2147/RMHP.S256272
19. Subhashini, Bharath Kumar Garla, Muthu Karuppaiah, Taranath. Prevalence of self-medication practice among people attending oral health outreach programs in Madurai East, Tamil Nadu. J Adv Oral Res. (2017) 8:14–20. doi: 10.1177/2229411217729104
20. Shafie M, Eyasu M, Muzeyin K, Worku Y, Martin-Aragon S. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS One. (2018) 13:e0194122. doi: 10.1371/journal.pone.0194122
21. Wael Zeid, Madeha Hamed, Nadia Mansour, Rokaya Diab. Prevalence and associated risk factors of self-medication among patients attending El-Mahsama family practice center, Ismailia, Egypt. Bull Nat Res Cent. (2020) 44:92. doi: 10.1186/s42269-020-00351-7
22. Ansari M, Alanazi A, Moin A. Consumers' awareness, attitude and associated factors towards self-medication in Hail, Saudi Arabia. PLoS One. (2020) 15:e0232322. doi: 10.1371/journal.pone.0232322
23. Makeen HA, Albarraq AA, Banji OJ, Taymour S, Meraya A, Alqhatani S, et al. Knowledge, attitudes, and practices toward self-medication in a rural population in South-Western Saudi Arabia. Saudi J Health Sci. (2019) 8:54–9. doi: 10.4103/sjhs.sjhs_9_19
24. Alghanim SA. Self-medication practice among patients in a public health care system. East Mediterr Health J. (2011) 17:409–16. doi: 10.26719/2011.17.5.409
25. Hisham Aljadhey, Ghada A., Assiri, Mansour A., Mahmoud, Sinaa Al-Aqeel, Michael Murray. Self-medication in Central Saudi Arabia; community pharmacy consumers' perspectives. Saudi Med J. (2015) 36:328–34. doi: 10.15537/smj.2015.3.10523
26. Alghadeer S, Aljuaydi K, Babelghaith S, Alhammad A, Alarifi MN. Self-medication with antibiotics in Saudi Arabia. Saudi Pharm J. (2018) 26:719–24. doi: 10.1016/j.jsps.2018.02.018
27. Aldeeri A, Alzaid H, Alshunaiber R, Meaigel S, Shaheen NA, Adlan A. Patterns of self-medication behavior for oral health problems among adults living in Riyadh, Saudi Arabia. Pharmacy. (2018) 6:15. doi: 10.3390/pharmacy6010015
28. T. Allam A, M. Amer S. Prevalence and factors influencing self-medication in Medina Al-Munawara, Saudi Arabia. Arch Pharma Pract. (2020) 11:43–54.
29. Afridi MI, Rasool G, Tabassum R, Shaheen M, Siddiqullah, Shujauddin M. Prevalence and pattern of self-medication in Karachi: a community survey. Pak J Med Sci. (2015) 31:1241–5. doi: 10.12669/pjms.315.8216
30. Lei X, Jiang H, Liu C, Ferrier A, Mugavin J. Self-medication practice and associated factors among residents in Wuhan, China. Int J Environ Res Public Health. (2018) 15:68. doi: 10.3390/ijerph15010068
Keywords: self-medication, Riyadh (Saudi-Arabia), community, over the counter drugs, opinions
Citation: Mannasaheb BA, Alajlan SA, Alshahrani JA, Othman N, Alolayan SO, Alamrah MS, Asdaq SMB, Al-Qahtani AM, Shaikh IA and Alasmary MY (2022) Prevalence, Predictors and Point of View Toward Self-Medication Among Residents of Riyadh, Saudi Arabia: A Cross-Sectional Study. Front. Public Health 10:862301. doi: 10.3389/fpubh.2022.862301
Received: 25 January 2022; Accepted: 17 February 2022;
Published: 25 March 2022.
Edited by:
Sudip Bhattacharya, Swami Rama Himalayan University, IndiaReviewed by:
Ranjit Kumar Dehury, University of Hyderabad, IndiaDhananjay Kumar Singh, Autonomous State Medical College, India
Manish Goyal, Post Graduate Government College, India
Copyright © 2022 Mannasaheb, Alajlan, Alshahrani, Othman, Alolayan, Alamrah, Asdaq, Al-Qahtani, Shaikh and Alasmary. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed Yahia Alasmary, bXlhbGFzbWFyeUBudS5lZHUuc2E=
 Basheerahmed Abdulaziz Mannasaheb
Basheerahmed Abdulaziz Mannasaheb Sarah Abdulrahman Alajlan2
Sarah Abdulrahman Alajlan2 Syed Mohammed Basheeruddin Asdaq
Syed Mohammed Basheeruddin Asdaq Awad Mohammed Al-Qahtani
Awad Mohammed Al-Qahtani Ibrahim Ahmed Shaikh
Ibrahim Ahmed Shaikh Mohammed Yahia Alasmary
Mohammed Yahia Alasmary