- 1The Architectural Design and Research Institute of Zhejiang University Co., Ltd., Hangzhou, China
- 2Center for Balance Architecture, Zhejiang University, Hangzhou, China
- 32nd Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China
The outbreak of COVID-19 has had a huge global impact, and it continues to test the resilience of medical services to emergencies worldwide. In the current post-epidemic era, vaccination has become a highly effective strategy to prevent the spread of COVID-19. However, using conventional mathematical models to evaluate the spatial distribution of medical resources, including vaccination, ignore people's behaviors and choices and make simplifications to the real world. In this study, we use an enhanced model based on the Theory of People Behavior (TPB) to perform a macro analysis of the satisfaction ability of medical resources for vaccination in Hangzhou, China, and attribute the city to a three-level structure. According to the allocation, the supply capacity of vaccination sites is calculated and divided into four categories (good, normal, not bad, and bad). Meanwhile, we raise an assumption based on the result and the general development law of the city and analyze the reasons for the impact of personal behavior on the spatial distribution of medical resources, as well as the relationship between the demand distribution and spatial distribution of medical resources and future development strategies. It is considered that the overall medical resources, especially vaccination in Hangzhou, feature the situation of central supply overflow, and are found to hardly meet the needs of population points in surrounding areas, requiring a more flexible strategy to allocate facilities in these areas.
Introduction
“Healthy city” is a concept that was proposed by the World Health Organization (WHO) in 1984. In the past 40 years, researchers have derived various healthy city planning goals and built corresponding evaluation systems. In China, the relevant research increased rapidly between 2009 and 2019 (1). Since 2019, COVID-19 has severely threatened all citizens' health systems, even those in the most developed countries. Governments all over the world have been urged to introduce political decisions aimed at containing the pandemic. Large-scale non-pharmaceutical interventions were put in place, such as social distancing, school closures, the isolation of symptomatic people and their contacts, and generalized lockdowns in some severely affected areas (2–4) . The long-term statistical results show that the higher the population density (mainly in urban areas), the higher the probability of a COVID-19 outbreak (5, 6). Currently, under the influence of the COVID-19 pandemic, both the Chinese government and academics consider that building a more stable healthy city and the corresponding medical system requires urban planning to intersect with other disciplines, such as medicine or public health management (7–9). Judged from the current epidemic prevention achievements, the defense capability of China and even major cities of the world against COVID-19 is still incomplete (10, 11).
In the post-COVID-19 pandemic era, it is an important guarantee for people's normal life that comprehensive epidemic prevention work is performed (12, 13). Above all, the government updates the epidemic data in real time by establishing an information system, laying a strong foundation for a “dynamic clearing case” in China; meanwhile, for individuals, getting vaccinated is the most important part of epidemic prevention work. Thus far, China has implemented three rounds of vaccination (the first dose, the second dose, and the booster dose). During the execution of the vaccination program, it was found that vaccination is likely to be offered at existing community healthcare centers, and if these centers cannot meet the actual needs, a temporary vaccination site in different forms will be constructed nearby.
Since 1997, China has launched the community healthcare center service (14). By 2016, more than 98% of cities were able to provide such services. During the COVID-19 vaccination work, community healthcare centers were selected as key vaccination sites. However, in the process of mass vaccination in Hangzhou, we also found that there were many cases of temporary suspension of vaccination sites, the addition of new vaccination sites, or the resumption of suspension of vaccination sites. The continuous change of vaccination site information also reflects the lack of coordinated vaccination arrangements. Therefore, it is necessary to evaluate the overall medical service capacity of Hangzhou in terms of medical function, especially regarding vaccination services.
Previous research results provide some data on the links between travel time, patient type, patient choice, and hospital visits. Huff proposed using the gravity analysis method to judge the relationship between the supply and demand of urban facilities (15, 16). During the following 30 years, represented by Radke, the corresponding mathematical system was improved according to the resource allocation of medical facilities, and this was gradually developed into the two-step floating catchment area (2SFCA) method (17, 18).
The TPB theory originates from the choice model, which is one of the important theoretical foundations of social psychology. It can be traced back to Fishbein's theory of multi-attribute attitude, which later evolved into the theory of reasoned action (19, 20). In 1991, Ajzen further deepened the theory of rational behavior, and formally proposed the TPB (21). This theory explains the general decision-making process of individual behavior from the perspectives of information processing and expected value theory (22, 23).
The TPB has been used effectively in research in many behavioral fields, as it can significantly improve the interpretation and prediction of behavior. In 2006, the British National Institute of Health and Clinical Optimization conducted a detailed investigation on which several behavioral selection models should be used in certain environments, and TPB was considered to be a relatively effective strategy. At present, there are few research on medical facilities based on TPB (24), especially in China. Studies on TPB theory in the analysis of medical resource allocation are mainly based on questionnaire surveys and the analytic hierarchy process. Nie Jinghong used the TPB model to identify the most important factor affecting patients' choice of hospital and concluded that it was the distance to the hospital, with the second factor being the scale of the hospital (25). Furthermore, Shen Yue et al.'s research on the survey of patients in a small number of hospitals in Shanghai reached the following conclusions: (1) Health-seeking behavior is principally affected by the availability of cars or other motorized vehicles; and (2) when the disease tends to be serious, the patient will be less sensitive to distance. Last year, our team carried out the overall evaluation of medical supplementary services by combining 2SFCA and TPB to build a mathematical model based on Hangzhou general hospital and population data and reported the phenomenon of medical resource run (26).
Methods and data
Enhanced model based on TPB
TPB is a theory mainly focused on how people behave (21). According to the principle of TPB, people's behavior is decided by three aspects: attitude toward behavior (A), degree of perceived behavioral control (B), and subjective norm (C). We summarize this theory in a simple formula to evaluate the degree of how people would conduct their behavior (D).
Specifically, attitude toward behavior (A) refers to the degree to which a person has a favorable or unfavorable evaluation or appraisal of certain behavior. Degree of perceived behavioral control (B) refers to the perceived ease or difficulty of performing that behavior and is assumed to reflect experience as well as anticipated impediments and obstacles. Subjective norm (C) means the perceived social pressure on one to perform or not to perform a certain behavior. In this research, as shown in Formula (2), we use S to represent A, which denotes the scale of the facility, and d to represent B, which denotes the distance between every two facilities.
As TPB is an appropriate theory to explain people's behaviors, we build an enhanced model to predict how people will act in a city and how allocation satisfies the needs of individuals according to Formulas (3)–(5).
where:
i denotes the different population points;
j denotes the different medical facility (hospital);
Ki−min denotes the prerequisite attitude of a certain kind of people;
Dij denotes the willingness to travel to a hospital in the region;
denotes the scale of the facility at j and β is the influence coefficient of the facility scale;
denotes the distance between i and j, and λ denotes the influence coefficient of distance;
Eij denotes the intention probability of a certain kind of people at i going to j to use the supplementary service.
In addition, prerequisite attitudes are preconditions that determine whether an action occurs. For an individual, when P=1, the behavior is possible; meanwhile, when P=0, the behavior is impossible. For the same kind of people, the P-values of different individuals in a crowd are not the same, but their preferences are relatively similar. Therefore, in a large-scale study, the weighted average of the P-values of different populations can be regarded as Ki−min, and their value should be between 0 and 1, which shows the preference of this kind of people for this type of behavior. For example, if only people over 18 years of age can be vaccinated in a specific region, the Ki−min of people under this age limit in this region will be 0. Therefore, the Ki−min in that region can be replaced by the actual action proportion of the group in a certain period; in this article, we consider that Ki−min = 1, because everyone is assumed to be vaccinated in China.
The scale difference between general hospitals is obvious for patients, and the subjective willingness of patients to use a medical service is positively correlated with the scale of the general hospital. Thus, we consider that β = 1, as described previously. At the same time, the scale difference between vaccination sites is not obvious for patients; therefore, the impact of the scale of vaccination sites on the patient's willingness is considered to be the same, that is, β = 0.
In this study, we consider that the distance patients are willing to travel to seek medical treatment at the hospital is negatively correlated with perceived behavioral control. Through the trial and fitting of different values, we found that using λ = −2 based on our previous study is reasonable because patients have a stronger willingness to go to a large-scale hospital when they have a serious disease. However, patients are more sensitive to distance when they need daily medical services, so λ = −3 is more reasonable under this condition. Here, the distance is calculated by using the road network.
Once we have evaluated the intention probability of a person's behavior, assuming that there are i residential points and j supplementary service points in total, by calculating the preference of each residential point for different supplementary service points, the demand for medical resources of each residential point for a certain supplementary service point under the preference of choice can be obtained and is expressed as:
In this formula, represents the number of medical needs demanded by the hospital, Pi represents the total population of the region, and Eij is the preference for the supplementary service in the region. After summation, we can obtain all of the demanded medical needs for supplementary services favored by the residents. Using Formula (4), the number of needs required by each supplementary service to satisfy the residents' wishes based on their choice can be obtained and then compared with the existing supplementary services.
Through comparison, we generated a difference between the supply sizes that are demanded and the supply sizes that can be supplied. This difference leads to a mismatch between the actual supply of available medical resources and the true demand of residents, which in turn leads to the inability of residents to access the desired amount of medical resources. Thus, we calculated the number of true resources that can be allocated to a certain point by taking the true demand of residents as the benchmark. The relevant expression is as follows:
where AiQ represents the accessibility of population points calculated by behavioral analysis from the perspective of demand to supply.
Next, we used this method to infer the total amount of medical resources available to individuals in different areas of Hangzhou under the TPB-generated results caused by individual willingness selection.
Study area and data
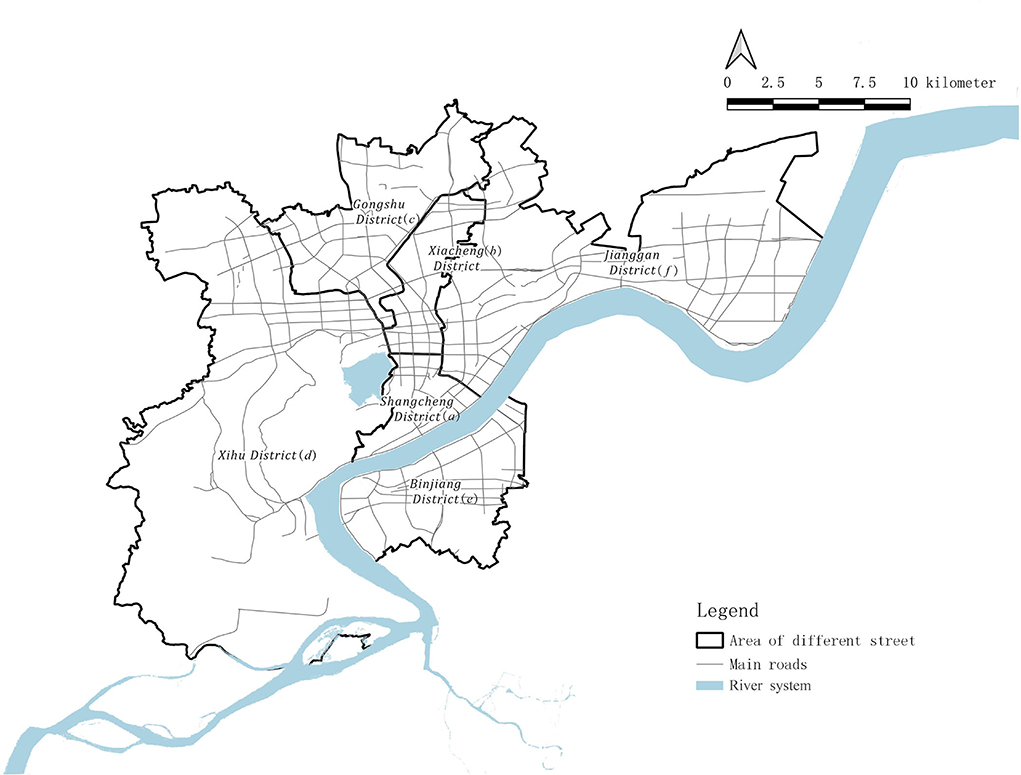
Hangzhou, as one of the central cities of the Yangtze River Delta, is the capital of Zhejiang Province and also its economic, political, and cultural center. The city has three famous World Heritage Sites, including West Lake, The Great Canal, and Liangzhu District, and its history has greatly shaped the present state of the city. This study considers the “main city area,” including six districts based on the “Hangzhou Urban Medical and Health Facilities Layout Plan (2016–2035, approved by the Hangzhou Government)” as the research area, including Shangcheng District (District a), Xiacheng District (District b), Gongshu District (District c), Xihu District (District d), Binjiang District (District e), and Jianggan District (District f). The subjects of this study include all residents in this area and vaccination sites at different levels (Figure 1).
It is important to note that not only do we focus on the traditional treatment that heals the disease but also on the comprehensive treatment needs, such as physical examination, medical care, pre-treatment, and emergency response to public health events. Therefore, this article considers that, in the COVID-19 pandemic era, the vaccination sites that provide vaccination and COVID testing for the entire society should well-represent the public vaccination sites in the area.
Before discussing the results, the following assumptions are made for both of the above aspects: This study takes the public medical resource provider as the service provider, including 68 vaccination sites with public information; the population in relation to the population demand point is that of the six districts of the main city of Hangzhou. We divide this population according to a 300 m × 300 m grid to obtain a total of 7,152 population grids, with a total population of 5.57 million (Figure 2) as the research object. The sensitivity of patients from population sites to the factor of distance to different levels of medical facilities is inconsistent. However, although the degree of people's intention to choose vaccination sites at various distances is generally different, it should not be assumed that vaccination sites that are farther than their medical address will not be chosen. Therefore, demand can be summarized as: “as long as the disease can be treated, people will go to any vaccination site in the six districts of the main city of Hangzhou.”
With respect to the different levels of vaccination sites, patients' needs are not the same. In general, since the service capacity of comprehensive vaccination sites is easy to perceive, the scale of such vaccination sites has an obvious impact on the patient's willingness to seek medical treatment. For comprehensive vaccination sites, the level of medical resources is often characterized by the number of beds. Therefore, we use this parameter to characterize the level of medical resources. At the same time, according to the requirements set forth by the “National Medical and Health Service System Planning Outline (2015–2020)” issued by the State Council in 2015, the number of beds in health institutions in China should reach 6 per 1,000 permanent residents by 2020. We use this item as an important indicator to evaluate whether Hangzhou's healthcare resources meet the basic needs of residents. This study is based on the data from vaccination sites in Hangzhou as of November 2020 (i.e., until the second dose is administered).
Results
Current situation and policy requirements for medical resources in Hangzhou
Herein, we consider six districts as the main city region based on the “Hangzhou Urban Medical and Health Facilities Layout Plan (2016–2035, approved by the government in July 2019)” as the research region, which includes Districts a, b, c, d, e, and f. All residents of the main city region are included in this work. Thus, we take general hospitals and vaccination points in Hangzhou as the two typical types of medical resources.
Supply capacity of medical resources in Hangzhou
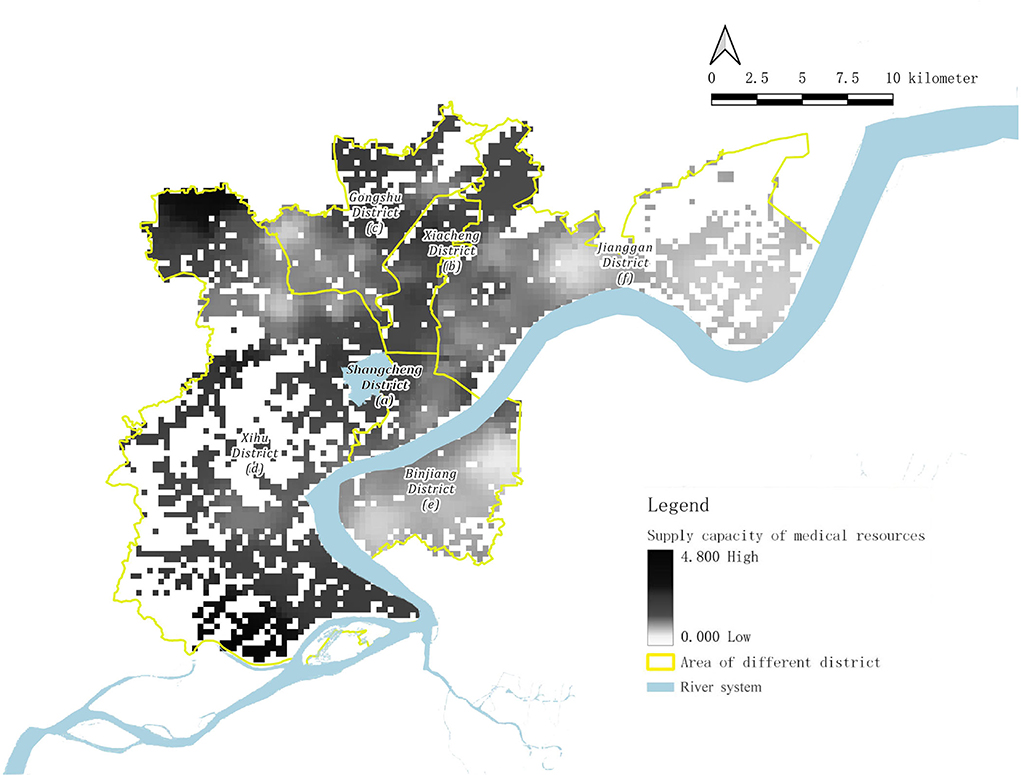
With regard to the integral distribution of vaccination points, the supply capacity of medical resources in terms of vaccination is approximately high in the west and low in the east of Hangzhou. The medical resource supply capacity of Districts a, b, c, and d (except Sandun Street) can easily meet or even exceed the medical needs of residents in these regions when compared with the local medical demand capacity. However, in Districts e, f, and Sandun Street in District d, the supply capacity of medical resources cannot satisfactorily meet the medical demands of residents.
As for the spatial distribution of vaccination sites, it can be divided into three types: overmet regions, unmet regions, and balanced regions (Figure 3).
The overmet regions include the Sandun Town area in the northwest corner, the Zhuantang area on the south side, the Kangqiao Street area on the north side, and the surrounding area of Zhejiang University City College, in which there is a higher basic medical service capacity.
The unmet regions include the whole area of District e, Wenxin Street, Zhaohui Street, Hemu Street, Xiangfu Street, Shiqiao Street, Ziyang Street, Jiubao Street in the west of the city, and the entire Xiasha area.
The balanced regions mainly include the areas that do not belong to the former two types, such as Xiaoying Street in District a, Changqing Street, Wenhui Street in District b, Shangtang Street in District c, Jianqiao Street, and Caihe Street in District f.
The detailed distribution of vaccination points in Hangzhou exhibits centripetal concentration and centrifugal dispersion. The vaccination points are concentrated in the north of District d, and Districts a, b, and c, which have experienced relatively long-time construction and development. Opposite to these areas, the distribution of vaccination points in Districts e and f are relatively scattered because of the comparatively short-term development in these areas.
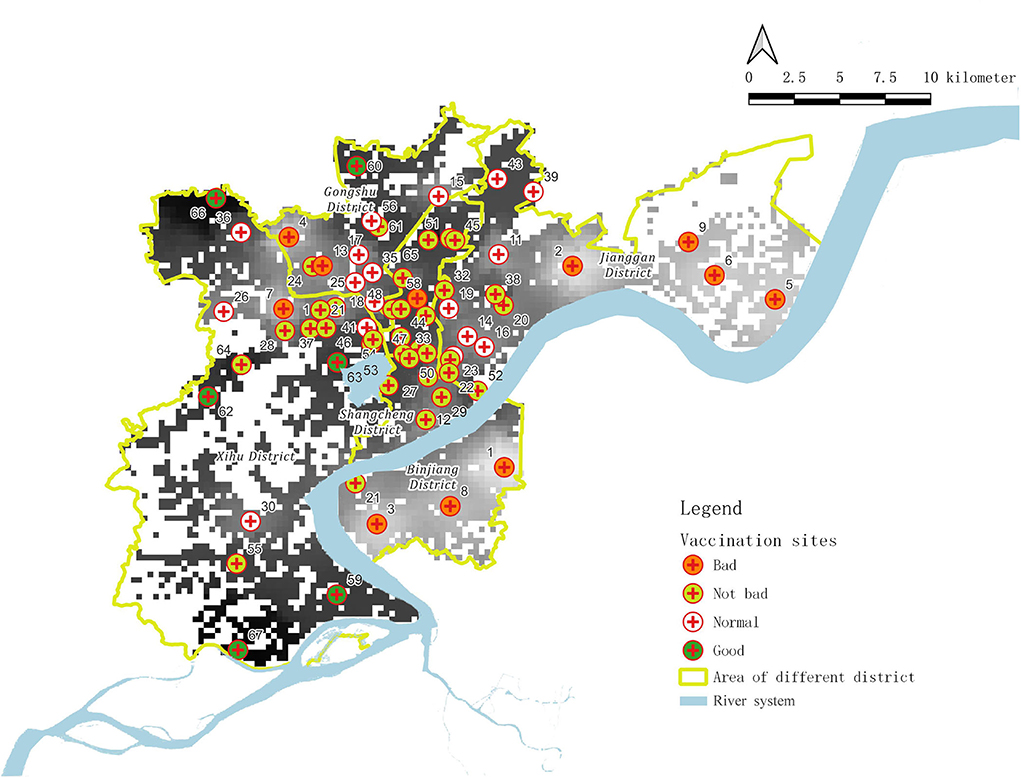
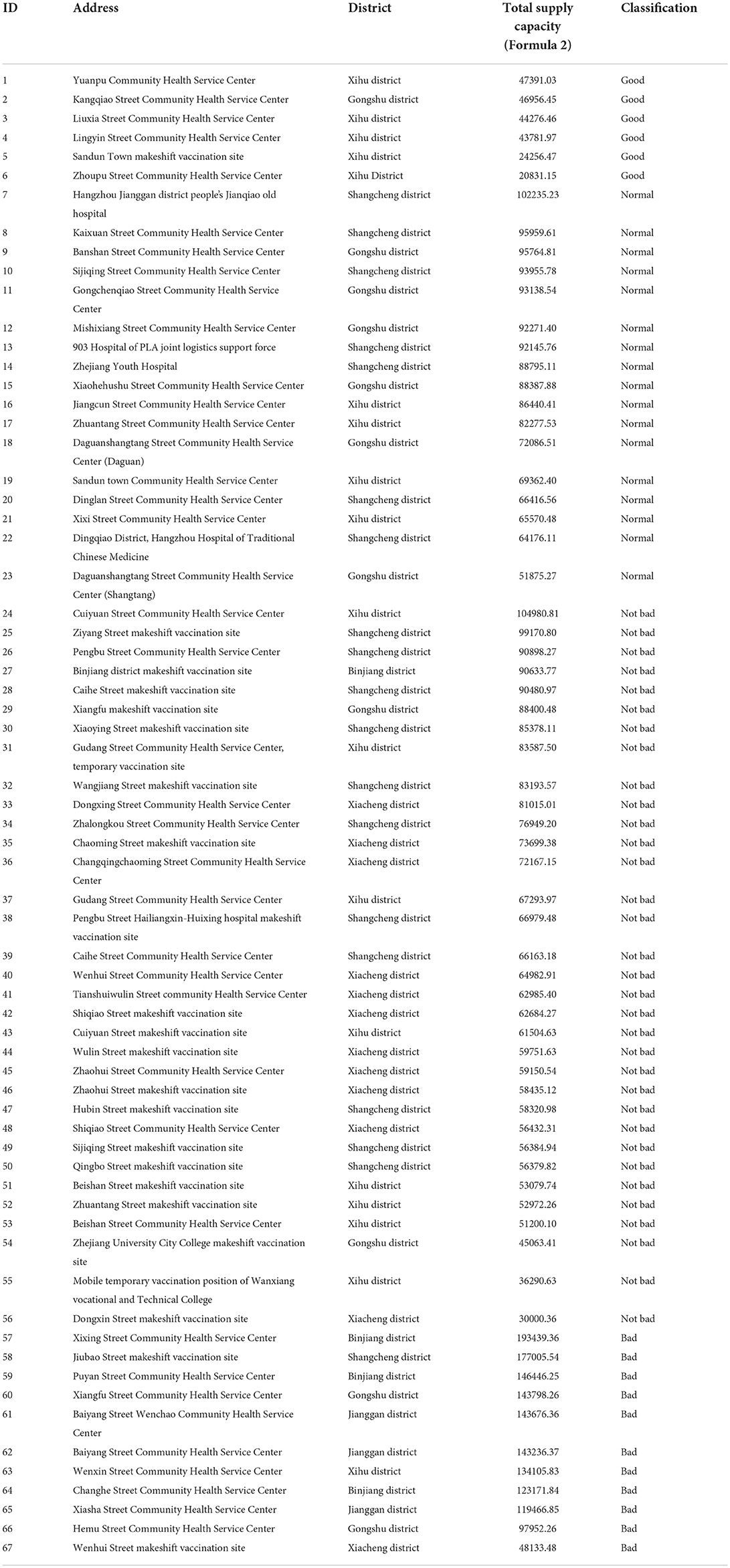
Based on our analysis, the current medical resource points for vaccination in Hangzhou (67 points in total) can be subdivided into the following four categories (Figure 4, Table 1): bad, not bad, normal, and good.
From Table 1, we can find that 11 vaccination points qualify as “bad,” including Xixing Street Community Health Service Center, Jiubao Street Temporary Inoculation Point for Fangcang, and Puyan Street Community Health Service Center, accounting for 16.42%. These points (community health and medical service centers) cannot meet the vaccination needs of the surrounding areas, and no additional emergency vaccination points are provided nearby. At the same time, additional unreasonable emergency vaccination points are included.
Moreover, 33 vaccination points were evaluated as “not bad,” including Cuiyuan Street Community Health Service Center, Ziyang Street Temporary Vaccination Point, and Pengbu Street Community Health Service Center, accounting for 49.25%. These points (community health and medical service centers) cannot meet the vaccination needs of the surrounding areas, but the addition of emergency vaccination points nearby helps to meet the requirements.
The “normal” category includes 17 vaccination points, including Kaixuan Street Community Health Service Center, Banshan Street Community Health Service Center, and Sijiqing Street Community Health Service Center, accounting for 25.37%. These points (community health and medical service centers) can meet the vaccination needs of the surrounding areas, but they cannot meet the vaccination needs of wider areas.
Only six vaccination points are evaluated as “good,” including Yuanpu Community Health Service Center, Kangqiao Street Community Health Service Center, and Liuxia Street Community Health Service Center, accounting for 8.96%. These points (community health and medical service centers) can meet the vaccination needs of surrounding areas, and at the same time, they can take into account the vaccination needs of wider areas.
Discussion
Previously, traditional and common methods like 2SFCA (17, 18), Huff models (15, 16), and others (27–31) were used to analyze the reasonableness of the allocation of facilities and the means to improve it. Meanwhile, few scholars have been concerned about the actual behavior of people in a city, let alone building a model to explain and predict it (32). At the same time, due to the rising demand for both the quality and quantity of medical services in China, it is becoming increasingly important to influence residents' medical behavioral preferences, which phenomenon has led to overcrowded large hospitals. The existing methods lack the mathematical expression of people's subjective demands and behaviors. In addition, traditional methods mainly contain two implicit conditions: All residents have the same demands and preferences; All residents choose a nearby facility, that is, they perform no-choice behavior, which simplifies the actual world. During the past 2 years, some researchers have attempted to analyze the basic medical services in the post-pandemic era, but resorted to using traditional methods (33–35). In contrast, we use the enhanced TPB model to improve the analytical power of predicting how people would choose a facility.
According to the enhanced TPB model, the regions of Hangzhou are categorized into three types (overmet, unmet, and balanced), and their descriptions are given as follows:
Overmet regions: These are mainly characterized by a lower population, which leads to lower demand for and moderate density of medical facilities. Therefore, each medical facility can easily meet the medical demand within a certain geographical range.
Unmet regions: Among them, areas with low medical resources can be further divided into three types as follows:
The whole area of Binjiang District (District e) and Jiubao Street. This is a new construction area of the city with a relatively fast-growing population and sizeable administrative area, which leads to the slow construction of basic medical facilities amid the high speed of urban construction and development. Therefore, the density of basic medical facility service points is relatively low, which causes the inferior medical service capacity of basic public resources in this region.
Wenxin Street, Zhaohui Street, Hemu Street, Xiangfu Street, Shiqiao Street, Ziyang Street, and so on, in the western part of the city. This area is an urban construction area that has already been completed. The population density and the total population are both relatively high, and the demand for the quantity and quality of basic medical facilities is also relatively high. However, in these unmet areas, the number and distribution density of medical facilities cannot keep up with the population's demand, resulting in the poor medical service capacity of basic public resources in these areas. Taking Wenxin Street as an example, the population density is relatively high, and the vaccination capacity is in short supply. Despite this condition, no new temporary vaccination point has yet been established, leading to the low efficiency of the actual vaccination process in this area.
Residents of certain streets are aware of the lack of basic medical facilities in their areas. From the results above, taking Xiangfu Street as an example, when it was realized that the area's vaccine service capacity was in short supply, a temporary vaccination site was set up in the south of this street. However, from a cross-street perspective, this is very close to the health service of Hemu Street, which caused an excess of medical resource supply. Also, this measure is not helping to effectively relieve the shortage of medical service supply for vaccination in Xiangfu Street. Therefore, we suggest that the resource distribution vaccination network needs to be comprehensively arranged on a large scale to avoid similar situations.
Xiasha area. This part of the wider region is extensive, and most of it is occupied by universities. A university always builds its basic medical facilities to serve itself, which increases the basic public resource service capacity of this region. However, it is still insufficient.
Balanced regions, where medical resources can be just satisfied, are mainly those that do not belong to the former two types of regions. Here, the residents' autonomous choice behaviors will form the “invisible hand” of the market for the allocation of medical resources. The medical resources available to residents in these areas are in relatively close proximity.
We found that Hangzhou has an apparent three-level structure of “the old town, the new city and the rural areas.” Old town refers to the old urban area where the construction and development have been completed and possesses the most resources. The new city means that the area is still developing at high speed and keen to have more facilities to meet the needs. And the rural areas refer to the rural parts that have not yet been planned for urban development and construction. Interestingly, the medical resource supply capacity of rural areas is usually not at the worst level; in fact, it is relatively satisfactory in many cases. This is because the rural population is comparatively small, such that these areas can meet the overall medical needs without large-scale or high-density medical facilities.
In addition to comparing the different areas, we also evaluated the facilities. The four main categories listed in Table 1 correspond to four kinds of supply capability of a medical resource (bad, not bad, normal, and good).
Limited by history, “bad” vaccination sites are mainly located in the city areas that have stopped in their development progress. The scale of these facilities is too small to handle public health emergencies, and thus, they cannot be used as strong medical service providers most of the time. Therefore, these facilities must cooperate with general hospitals and even other venues to ensure the satisfaction of medical needs (such as streets in the Shangcheng District (District a), in which the original community service centers fail to meet the needs of vaccination, and it must add temporary facility points instead of using the original community service center). If these areas cooperated with some general hospitals, they could be regarded as “not bad” vaccination sites.
Since “normal” and “good” vaccination sites have more adequate venues, more even distribution, and more sufficient medical resources, these sites can be used as effective providers of basic medical resources and can meet the emergency medical needs in the corresponding part of the city. This category of vaccination sites mainly includes recently constructed street health service centers and vaccination sites converted from some private hospitals, among others.
There are specific situations where several kinds of homogeneous populations are concentrated in specific regions (mainly universities), and a designated vaccination site needs to be set up in these regions to meet the needs of these people. These vaccination sites are not necessarily covered by public healthcare networks because they are special supplements to the city healthcare networks. Another possible situation is that, if an area is difficult-to-enter and there is a medical facility in its area, that facility can easily form an access barrier for public resources at the area boundary to ensure that residents in the area are given priority services.
To explain the above results, we raise the following assumption. Based on the general law of urban development, a small number of hospitals could meet the healthcare needs well before the city's growth and population explosion. At this stage, only a few small healthcare centers, such as drug stores, rather than healthcare facilities and very few large hospitals are needed, especially in suburban areas. However, during the past 30 years, the city's growth and population explosion made old facilities too small to cover all needs in a growing city area. Moreover, the market rules leading to the lag in the construction of healthcare facilities render basic public healthcare facilities insufficient in the long term, placing this area in the unmet category (such as the west of the city). When an area stops growing (usually the oldest part of the city), which means that market selection and balance have been achieved, the constructed facilities can meet the increased healthcare needs, and the medical resource supply is relatively moderate, making it a balanced area. It is suggested that if some areas (mostly suburban areas, such as Jiubao, Xiasha, and Binjiang area) do not have a significant population that is expected to increase rapidly, new facilities should be built in advance to avoid turning into an unmet area, even though this place would become an overmet area in the short term. In brief, we believe that the result of the current allocation is caused by both historical reasons, like an undeveloped economy, and city planning that is not predictable enough to catch the growth rate of the city.
According to the results and our assumptions, we believe that being flexible in the location, construction, and total volume of medical facilities is the most important factor in dealing with the pandemic of COVID-19. Besides, in this post-pandemic era, the ability to handle a pandemic quickly is the key to preventing it. Although large comprehensive hospitals are more efficient in providing medical care, such facilities cannot be constructed in short periods such as 7 days, which is the critical threshold to prevent the virus from spreading. Under the existing conditions, a large number of facilities are still needed in a flexible way to handle emergencies during the pandemic in Hangzhou, China.
Conclusion
In this work, we investigated COVID-19 vaccine demand satisfaction by evaluating the level of medical services in Hangzhou, China. We used the enhanced TPB model to replace the traditional method that ignores individuals' opinions and behavior. We also put forward the subjective concept of “vaccination attitude P” in the evaluation of medical vaccination services in Hangzhou, China, which needs to be accomplished through sample surveys or other methods in other countries. Based on the results of the enhanced TPB model, the overall situation of medical resources in Hangzhou is that the supply in the city center is overmet, while it is difficult to satisfy the needs of populations in the surrounding areas, requiring the medical resources to be more flexible. The suggested approach to increasing the flexibility includes the construction of new hospitals, setting up branches, building community healthcare centers, and establishing a systematic, multi-level, and moderate-distance distribution medical and health space network. The current study still has the following limitation: certain included vaccination points are community health service centers without vaccination services on several campuses, which cannot be accounted for at present.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Ethics approval and written informed consent were not required for this study in accordance with national guidelines and local legislation.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This work was supported by the construction and scientific research projects in 2021 of Center for Balance Architecture, Zhejiang University (Award number: K-20212791).
Acknowledgments
The author thanks for the generous help from Mr. Xi in Hangzhou.
Conflict of interest
Author MC and YZ were employed by the Architecture Design and Research Institute of Zhejiang University.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang L, Jiang X, Ye D. Research hotspots and progress in China's healthy city planning: a bibliometric analysis based on Citespace. Urban Dev Stud. (2020) 27:8–14.
2. Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, Coupland H. Estimating the effects of nonpharmaceutical interventions on COVID-19 in Europe. Nature. (2020) 584:257–61.
3. Matteo T, Francesca C, Maria BZ. Lifestyle changes and psychological well-being in older adults during COVID-19 pandemic. Clin Geriatr Med. (2022) 38:449–59. doi: 10.1016/j.cger.2022.05.002
4. Howard-Bobiwash HA, Joe JR, Lobo S. Concrete Lessons: policies and practices affecting the impact of COVID-19 for urban indigenous communities in the united states and Canada. Front Sociol. (2021) 23:612029. doi: 10.3389/fsoc.2021.612029
5. Chu Z, Cheng M, Song M. What determines urban resilience against COVID-19: city size or governance capacity?. Sust Cities Soc. (2021) 75:102911. doi: 10.1016/j.scs.2021.103304
6. Mansour S, Al-Kindi A, Al-Said A, Al-Said A, Atkinson P. Sociodemographic determinants of COVID-19 incidence rates in Oman: geospatial modelling using multiscale geographically weighted regression (MGWR). Sust Cities Soc. (2020) 65:102627. doi: 10.1016/j.scs.2020.102627
7. Lin Y, Zhong P, Chen T. Association between socioeconomic factors and the COVID-19 Outbreak in the 39 well-developed cities of China. Front Public Health. (2020) 8:546637. doi: 10.3389/fpubh.2020.546637
8. Hu M, Roberts J D, Azevedo G P, Milner D. The role of built and social environmental factors in Covid-19 transmission: a look at America's capital city. Sust Cities Soc. (2021) 65:102580. doi: 10.1016/j.scs.2020.102580
9. Wang J, Hu X, Tong C. Urban community sustainable development patterns under the influence of COVID-19: a case study based on the non-contact interaction perspective of Hangzhou City. Sustainability. (2021) 13:1–20. doi: 10.3390/su13063575
10. Acuto M. COVID-19: lessons for an urban(izing) world. One Earth. (2020) 4:317–9. doi: 10.1016/j.oneear.2020.04.004
11. Chen J, Guo X, Pan H, Zhong S. What determines city's resilience against epidemic outbreak: evidence from China's COVID-19 experience. Sust Cities Soc. (2021) 70:102892. doi: 10.1016/j.scs.2021.102892
12. Sannigrahi S, Pilla F, Basu B, Basu AS, Molter A. Examining the association between socio-demographic composition and COVID-19 fatalities in the European region using spatial regression approach. Sust Cities Soc. (2020) 62:102418. doi: 10.1016/j.scs.2020.102418
13. Khavarian-Garmsir AR, Sharifi A, Moradpour N. Are high-density districts more vulnerable to the COVID-19 pandemic? Sust Cities Soc. (2021) 70. doi: 10.1016/j.scs.2021.102911
14. Wang Y, Ma C, Du J. Development of traditional Chinese medicine in community health service in China. J Trad Chin Med Manag. (2012) 20:1151–3. doi: 10.16690/j.cnki.1007-9203.2012.12.017
15. Huff DL. A probabilistic analysis of shopping center trade areas. Land Econ. (1963) 39:81–90. doi: 10.2307/3144521
16. Huff DL. Defining and estimating a trading area. J Mark. (1964) 28:34–8. doi: 10.1177/002224296402800307
17. Matthew RM, John SH. Measuring spatial accessibility to primary care in rural areas: improving the effectiveness of the two-step floating catchment area method. Appl Geograp. (2008) 29:533–41. doi: 10.1016/j.apgeog.2008.12.003
18. Radke J, Mu L. Spatial decompositions, modeling and mapping service regions to predict access to social programs. Geogr Inform Sci. (2000) 6:105–12. doi: 10.1080/10824000009480538
19. Fishbein M. An investigation of the relationships between beliefs about an object and the attitude toward that object. Hum Relat. (1963) 16:233–9. doi: 10.1177/001872676301600302
20. Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an an introduction to theory and research. J Business Ventur. (1977) 10:130–132.
21. Ajzeni. The theory of planned behavior. Organiz Behav Hum Decis Processes. (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
22. John P, Guadalupe XA, Stewart H. Theories and in-tervention approaches to health-behavior change in pri-mary care. Am J Prev Med. (1999) 17:275–84. doi: 10.1016/S0749-3797(99)00094-X
23. Duan W, Jiang G. A review of the theory of planned behavior. Adv Psychol Sci. (2008) 16:315–320.
24. Moscellig G, Siciliani L, Gutacker N, Gravelle H. Location, quality and choice of hospital: evidence evidence from England 2002–2013. Regional Sci Urban Econ. (2016) 60:112–24. doi: 10.1016/j.regsciurbeco.2016.07.001
25. Nie J, Jin H. Analysis of the influencing factors of patient to medical care and health intention: based on planned behavior theory. J Res. (2017) 86–94+150.
26. Shen Y, Shi Y, Wang H, Sun B. The impacts of medical facility accessibility on patients' medical treatment space: a case study in Shanghai. Urban Dev Stud. (2019) 26:46–52+61.
27. Song Z, Chen W, Zhang G, Zhang L. Spatial accessibility to public service facilities and its measurement approaches. Progress Geogr. (2010) 29:1217–1224.
28. Zhang J, Ge Z, Luo Z, Sun S. Research on equalized layout of urban and rural public facilities: a case study of educational facilities in Changzhou. City Plann Rev. (2012) 36:9–15.
29. Tang Z, Gu S. An evaluation of social performance in the distribution of urban parks in the central city of Shanghai: from social equity to social justice. Urban Plann Forum. (2016) 15–21. doi: 10.16361/j.upf.201601002
30. Xing Z, Zhu J. Evaluation on fair performance of urban green space based on coupling model of coordinated development theory. City Plann Rev. (2017) 41:89–96. doi: 10.11819/cpr20171114a
31. Tomnay JE, Coelli L, Davidson A, Hulme-Chambers A, Orr C, Hocking JS. Providing accessible medical abortion services in a Victorian rural community: a description and audit of service delivery and contraception follow up. Sexual Reprod Healthc.(2018) 16:175–180. doi: 10.1016/j.srhc.2018.04.006
32. Cheng M, Zhu Y, Cen P, Huang S. Allocation of urban medical resources based on personal choice preference. J Zhejiang Univ. (2021) 55:2194–206. doi: 10.3785/j.issn.1008-973X.2021.11.021
33. Hajizadeh A, Monaghesh E. Telehealth services support community during the COVID-19 Outbreak in Iran: activities of Ministry of Health and Medical Education. Inform Med Unlocked. (2021) 24:100567. doi: 10.1016/j.imu.2021.100567
Keywords: COVID-19, theory of planned behavior (TPB), population raster, vaccination sites, Hangzhou city
Citation: Cheng M, Zhu Y, Cen P and Huang S (2022) Evaluation of medical services from the perspective of COVID-19 vaccine demand satisfaction in Hangzhou, China. Front. Public Health 10:862283. doi: 10.3389/fpubh.2022.862283
Received: 15 February 2022; Accepted: 18 October 2022;
Published: 09 November 2022.
Edited by:
Salih Djilali, University of Chlef, AlgeriaReviewed by:
Krushna Chandra Sahoo, Regional Medical Research Center (ICMR), IndiaManojit Bhattacharya, Fakir Mohan University, India
Copyright © 2022 Cheng, Zhu, Cen and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingjun Cheng, bWtlbGxlcmNAb3V0bG9vay5jb20=; Shan Huang, MzgxMjE3NzQ5QHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Mingjun Cheng
Mingjun Cheng Yunchen Zhu
Yunchen Zhu Peili Cen
Peili Cen Shan Huang
Shan Huang