
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 12 May 2022
Sec. Public Health and Nutrition
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.861627
This article is part of the Research TopicDiabetes in Africa in the 21st Century: The Unique and Important Challenge of Diabetes in Africa, Volume IIView all 5 articles
Background: Diabetes mellitus (DM) is a metabolic disorder marked by a persistently high blood glucose level over a prolonged period of time linked to either defects in insulin secretion, insulin action, or both. It is responsible for 537 million adult cases and 6.7 million deaths in 2021. However, about half of the people with diabetes go undiagnosed. Low-income and socially disadvantaged communities are the most vulnerable to the disease. Despite this fact, nothing has been done among these communities, so this study aimed to assess the extent of undiagnosed diabetes and its predictors among the socially marginalized Menja communities of Southwest Ethiopia, 2021.
Methods: A community-based cross-sectional study was done in the Menja communities from April 21/2021 to June 30/2021. The required sample size was calculated using the single population proportion formula and systematic sampling techniques were employed to select the households. Data were collected through face-to-face interviews utilizing an interviewer-administered questionnaire to collect socio-demographic and behavioral characteristics, and anthropometric measurements were taken from each participant. Diabetes was defined as participants who had an FBG ≥ 126 mg/dL or RBG > 200 mg/dL. The multivariate logistic regression model was used to identify the predictors of diabetes; adjusted OR with a 95% CI was computed to assess the strength of associations.
Results: The prevalence of undiagnosed DM among the socially marginalized Menja communities was 14.7% [95% CI: (11.1–18.3)], and sex-specific prevalence was 16.8%, and 11.1% for men and women respectively. Factors like alcohol consumption (AOR = 3.0, 95% CI 1.49 to 6.05), family history of DM 4.4 (AOR = 4.37, 95% CI 2.04 to 9.35), lower vegetable consumption 3.5 (1.19–10.31) (AOR = 3.5, 95% CI 1.19 to 10.31), and less physical exercise 3.3 (AOR = 3.34, 95% CI 1.61 to 6.90) were the independent predictors that increase the risk of diabetes among Menja communities.
Conclusion and Recommendations: Undiagnosed diabetes was high as compared to other settings. Alcohol use, family history of diabetes, vegetable consumption, and physical exercise were predictors of diabetes. Hence, the study suggests frequent screening and treatment for high-risk groups. Minimizing alcohol drinking, frequent vegetable consumption, and physical exercises were recommended measures for the prevention and control of DM among the population of Ethiopia.
Diabetes mellitus (DM) is a metabolic disorder marked by a persistently high blood glucose level over a prolonged period of time linked to either defects in insulin secretion, insulin action, or both (1, 2). Type 2 diabetes affects the majority of people, and nearly entirely occurs among adults (2). Around 537 million adults (20–79 years) worldwide have DM; 541 million have impaired glucose tolerance, putting them at high risk of developing the disease; this figure is expected to rise to 643 million by 2,030 and 784 million by 2,045, and more than four out of five (81%) adults live in low- and middle-income countries (3).
The disease prevalence has been rising more rapidly in low- and middle-income countries than in high-income countries, and the socially disadvantaged in any country are the most vulnerable to the disease (4, 5). In 2019, the International Diabetic Federation (IDF) Africa Region has approximately 19 million and 47 million persons (20–79) living with diabetes and impaired glucose tolerance, respectively. By 2,045, this number is expected to rise to 47 million people with diabetes and 110 million people with impaired glucose tolerance, putting them at a high risk of developing type 2 diabetes (6). According to the IDF, the prevalence of diabetes among Ethiopian adults is 3.2% (7).
Diabetes will be the seventh leading cause of death by 2,030, accounting for 6.7 million fatalities (1 every 5 s) (3, 8). It is expected to cost at least USD 966 billion in health expenditure in 2021, and this is a 316% increase over the last 15 years (3), In Africa about USD 9.5 billion was spent on healthcare for people with diabetes in 2019 (7). Furthermore, diabetes affected more than 21 million live births in the IDF Africa Region in 2013, accounting for 1 in every 9 live births (5, 7). Regular physical activity, a healthy body weight, a balanced diet, and avoiding tobacco use are among the most popular lifestyle changes that can help prevent this (8).
Poorly managed diabetes increases the risk of heart attacks and strokes by two to three times, as well as neuropathy (nerve damage), renal failure, foot ulcers, lower limb amputation, and 2.6 presence of global blindness in 2021 (9), Early identification and treatment are critical interventions for preventing diabetes complications and mortality, as well as for better treatment outcome (2), however, about half of diabetics go undiagnosed (3). Furthermore, consequences from undiagnosed diabetes have a significant impact on patients' quality of life, which may typically be avoided by early identifying risk factors (10).
According to the 2014 estimate, 179.2 million people worldwide have undiagnosed diabetes (2), the IDF Africa Region has the greatest rate of undiagnosed people of any of the IDF regions, with 60% of adults living with diabetes unaware of their condition (7). A systematic analysis from African countries revealed that the pooled prevalence of undiagnosed DM among adults was 3.85%, thus 4.43% in Eastern Africa; 4.72% in Western Africa; 4.27% in Northern Africa, and 1.46% in southern Africa respectively (11). In Ethiopia, various studies have revealed varying rates of undiagnosed diabetes. For example, research conducted in Bahr Dar, Dire Dawa, Gonder, and Dembia found that the prevalence of undiagnosed diabetes was 10.2, 6.2, 6.34, and 11.5% respectively (12–15).
Age, marital status, educational level, family history, overweight, lack of awareness of diabetes symptoms, alcohol consumption, waist circumference, history of hypertension, cigarette smoking, exercise, and low health-seeking behavior, such as lack of regular health check-ups, were all found to be independently associated with undiagnosed diabetes mellitus (12, 13, 15, 16). Even though these studies have been conducted in various parts of Ethiopia, nothing has been done among the socially marginalized communities. So, this study aimed to assess the prevalence of undiagnosed diabetes and its contributors among culturally marginalized communities of Menja in Southwest, Ethiopia, this helps to carry out evidence-based intervention for policymakers, governmental and non-governmental organizations.
A community-based cross-sectional study was done in the Menja communities from April 21/2021 to June 30/2021. The Menja community is located 534 km from Addis Abeba, the capital of Ethiopia in the southwest direction. The Menja is a minority group living in pockets of the Kafa, and Bench Maji zone of the southwest region of Ethiopia. There is no census data on the Menja population because they live within the majority culture and are considered members of the majority ethnic group. Nevertheless, the Menja do have a separate identity. Menja community administration has 13 dispersed kebeles.
The Menja are hunters; most of their subsistence is derived from hunting wild animals such as colobus monkeys, porcupines, and wild boar, and from gathering and selling forest products such as firewood, charcoal, and honey. Farmers, who represent the majority of the society, consider themselves 'dirty' because of their different dietary habits, i.e., eating wild animals and those not ritually slaughtered. Indeed, the Menjo are disdained and discriminated against by the majority groups. The Menja population is physically different from farmers and other minorities as they are darker and shorter in stature and have curly hair, flat noses, and smaller foreheads. Until recently, the Menja population has not been the main focus of studies and listed substantive ethnographic data have been compiled about them.
The source population was all adults over the age of 18 who resided in the Menja community for more than 6 months, and the study population was adults over the age of 18 residing in eligible homes in randomly selected kebeles in the community. The single population proportion formula was used to compute the minimal sample size required for this research, with the following assumptions: Due use a lack of previous research in the study context, there was a 50% proportion of undiagnosed diabetes, a 95% confidence level, a 5% margin of error, and a 10% non-response rate, resulting in a total of 422 participants (17).
Based on the number of homes, the total sample size was proportionally allocated to each of the randomly selected kebeles. A systematic sampling approach was utilized to choose the households at every “K” interval (2,525/422 = 6) with a random starting point determined from inside the first 6 houses using the household record. For households with more than one eligible individual, the lottery technique was used to select only one person, but in the event of a household with no eligible individuals, the immediate next household (HH) was used.
After reviewing different kinds of literature, the English version data collection tool was prepared. The questionnaire was translated into the local language (Amharic and Benchgna) and back-translated into English to maintain consistency. The questionnaire was divided into four sections: socio-demographic, behavioral, or lifestyle, and clinical or anthropometric characteristics. The primary investigator recruited and trained four laboratory personnel (three data collectors and a supervisor) on the study's goal and how to collect blood samples. Face-to-face interviews utilizing an interviewer-administered questionnaire were used to collect socio-demographic and behavioral data.
It was measured on the right arm, the average was taken for two evaluations 5 min apart, and then Hypertension was defined as a systolic BP of ≥140 mmHg and diastolic BP of ≥ 90 mmHg (18).
The formula for calculating body mass index (BMI) is weight in kilograms divided by height in meters squared. A BMI of <18.5 kg/m2, 18.5–24.9 kg/m2, >25–29.9 kg/m2, and ≥ 30 kg/m2 was recognized as underweight, normal, overweight, and obese respectively (19).
Using at least one of a specific substance (alcohol, khat, cigarette, and others) for non-medical purposes within the last 3 months according to the alcohol, smoking, and substance involvement screening tool (ASSIST) (20).
Using at least one of any specific substances (alcohol, khat, cigarette, and others) for non-medical purposes at least once in a lifetime according to ASSIST (20).
Participants with undiagnosed diabetes (type 1 or type 2) with FBG ≥126 mg/dL or RBG ≥200 mg/dL were classified as those who had never had their blood sugar tested before and were not receiving DM medication at the time of the survey (21).
The Global Physical Activity Questionnaire (GPAQ) was used to collect data, and activity levels were estimated using the cut-off points in the analytic guide (22).
It was assessed using the WHO dietary assessment for vegetables and fruit, and then classified into two or fewer servings, one to three servings, and four to seven servings (23).
To safeguard the quality of the data, a pre-test was done on 5% of the sample size at the neighboring Bachuma district having similar socio-cultural characteristics with study subjects, accordingly, the necessary modification was done. The questionnaire was initially prepared in English and then translated into a local language “Amharic and Benchigna”, and then back-translated into English to maintain its consistency. Moreover, the tool was assessed for its clearness, and the items that were problematic to answer were rephrased.
Four laboratory technicians received 4 days of training on questionnaire administration, physical measurement, and biomedical measurement techniques before the survey. The clinical data (family history of DM, hypertension, and ever checked glucose level) of the participants were also collected via interview. Laboratory personnel was organized on proper sample collection before beginning blood collection. Physical measurements were taken twice, and in some cases, three times, to reduce observer error. Data collectors were rotated to compare results in between the data collection. The glucometer apparatus and strips were verified for consistency in reference and test readings regularly.
The collected data completeness was checked manually before being entered into EpiData 3.1 and the necessary correction was made. The entire process of data collection was overseen by supervisors and the principal investigator. Supervisors reviewed the obtained data on a regular basis in the field. Data coding and cleaning were done by cross-checking to print out for possible errors. Missing values and outliers were checked through running descriptive analysis.
The data were cleaned, coded, and entered using Epi-Data version 3.1 and exported to SPSS version 24 for management and statically analysis. Descriptive statistics (means, medians, and percentages) were presented in texts, tables, and graphs. To identify candidate variables for the final model, bivariate logistic regression was used to assess the relationship of undiagnosed diabetes with each variable. Variables with value <0.25 were taken into multiple logistic regression analysis to identify independent predictors of DM.
The model was constructed using the backward likelihood ratio with 0.1 probability elimination. The resulting model's goodness of fit was assessed using the Hosmer-Lemeshow test of goodness of fit, with good fit defined as a value >0.05, and model classification accuracy subsequently assessed. Finally, independent predictors of DM were declared at a p-value < 0.05 cutoff point, and the strength of the association was assessed using AORs with their corresponding 95% confidence level.
This survey had 415 people out of 422 who were chosen, with a response rate of 98.3%. The Mean age of the participants was 36.4 ± (8.7 SD) years. About 63.1% were men, 36.9% self-employed, and 42.7% of the participants had no formal education. More than half 53.5% were married and, a comparable proportion of 53.5% of the participants had an income < 2,500 Ethiopian birr (see Table 1).
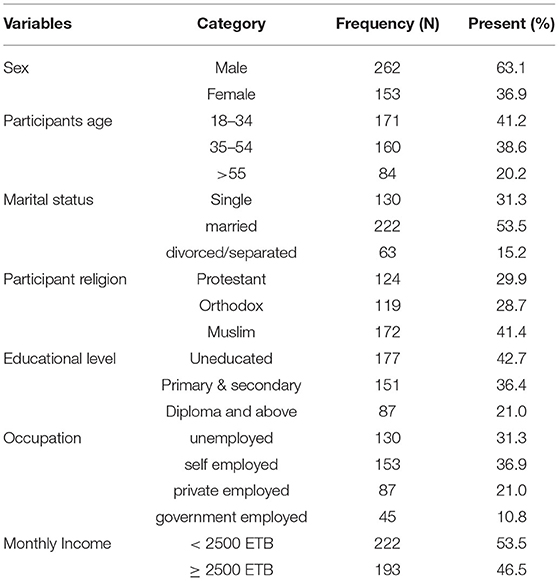
Table 1. The socio-demographic and economic characteristics of the Menja community in Bench-Sheko zone Southwest Ethiopia, 2022, (N = 415).
Slightly < a quarter 21.7% of the participants were current smokers, with 9.2% of them smoking fewer than 5 numbers of sticks per day. About 40.7% had a history of alcohol drinking, and out of them, 19.5% had 1–3/days/month frequency intake. About 17.1% chewed khat, 41.2% had vegetable serving one to three times per week, and a similar proportion of 40.7% and 40.0% had a high (≥ 1,500 MET min) and medium (≥600 MET min) level of total physical activity, respectively (see Table 2).
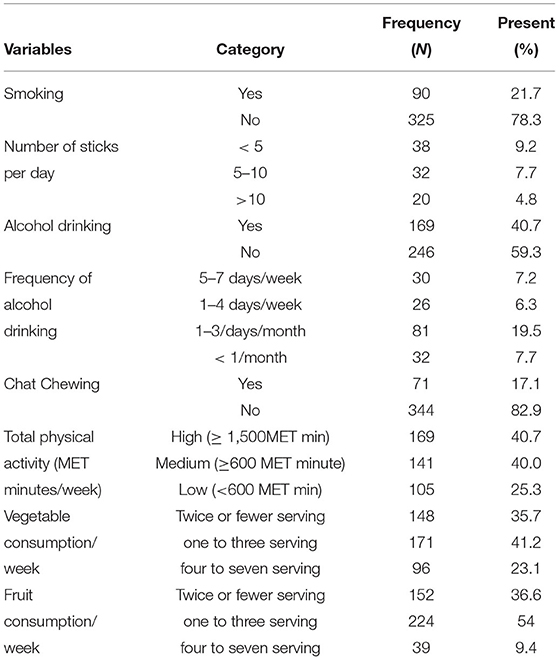
Table 2. Behavioral and lifestyle characteristics of Menja community in South-west, Ethiopia, 2021 (N = 415).
One-quarter of the individuals (24.6%) had a BMI of 25 kg/m2 or higher, 17.1% had a family history of diabetes, and 11.6% had a previous history of hypertension diagnosis. About 14.9% of the participants had previously checked their blood glucose level, and slightly < a quarter (21.9% of the participants) were aware of diabetes symptoms, with polyphagia, polyuria, and polydipsia accounting for 35.2, 27.5, and 20.8% respectively (see Table 3).
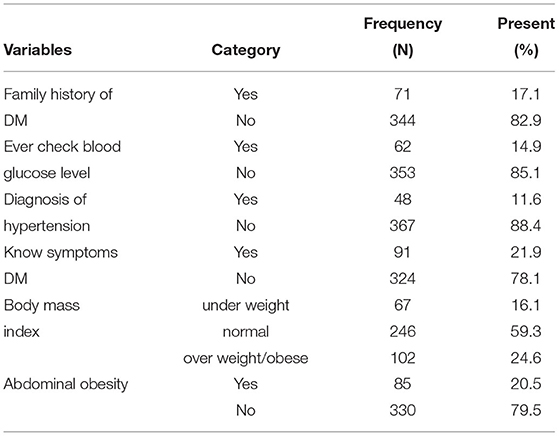
Table 3. Clinical and anthropometric measurements of the participants, Menja community, South-west, Ethiopia, 2021 (N = 415).
The prevalence of undiagnosed DM was 14.7% [95% CI: (11.1–18.3)], with sex-specific prevalence being 16.8, and 11.1% for males and females, respectively (see Figure 1).

Figure 1. Prevalence of Diabetic Mellitus among Menja Community, South-west, Ethiopia, 2021 (N = 415).
During binary logistic regression, the candidate variables with a p-value < 0.25 were age, marital status, educational level, income, alcohol intake, chat use, physical activity, vegetable consumption, family history of diabetes mellitus, and body mass index. Alcohol use, vegetable consumption, and family history of diabetes were found to be independent predictors of undiagnosed DM after multivariate logistic regression with a p-value of < 0,005 cut-off thresholds.
The odds of having undiagnosed diabetes among individuals who drank alcohol were three times (AOR = 3.0, 95% CI 1.49 to 6.05) higher compared to those who did not drink. Similarly, those participants who had a family history of diabetes had 4.4 (AOR = 4.37, 95% CI 2.04 to 9.35) times higher odds of undiagnosed diabetes compared with those who had no such history. Moreover, individuals with two or fewer vegetable consumption/week were a 3.50 (1.19–10.31) (AOR = 3.5, 95% CI 1.19 to 10.31) higher risk of undiagnosed diabetes as compared to the higher frequency of vegetable consumption, and individuals with a low habit of physical exercise were 3.3 times (AOR=3.34, 95% CI 1.61 to 6.90) at higher risk of developing diabetes as compared to the counterparts (see Table 4).
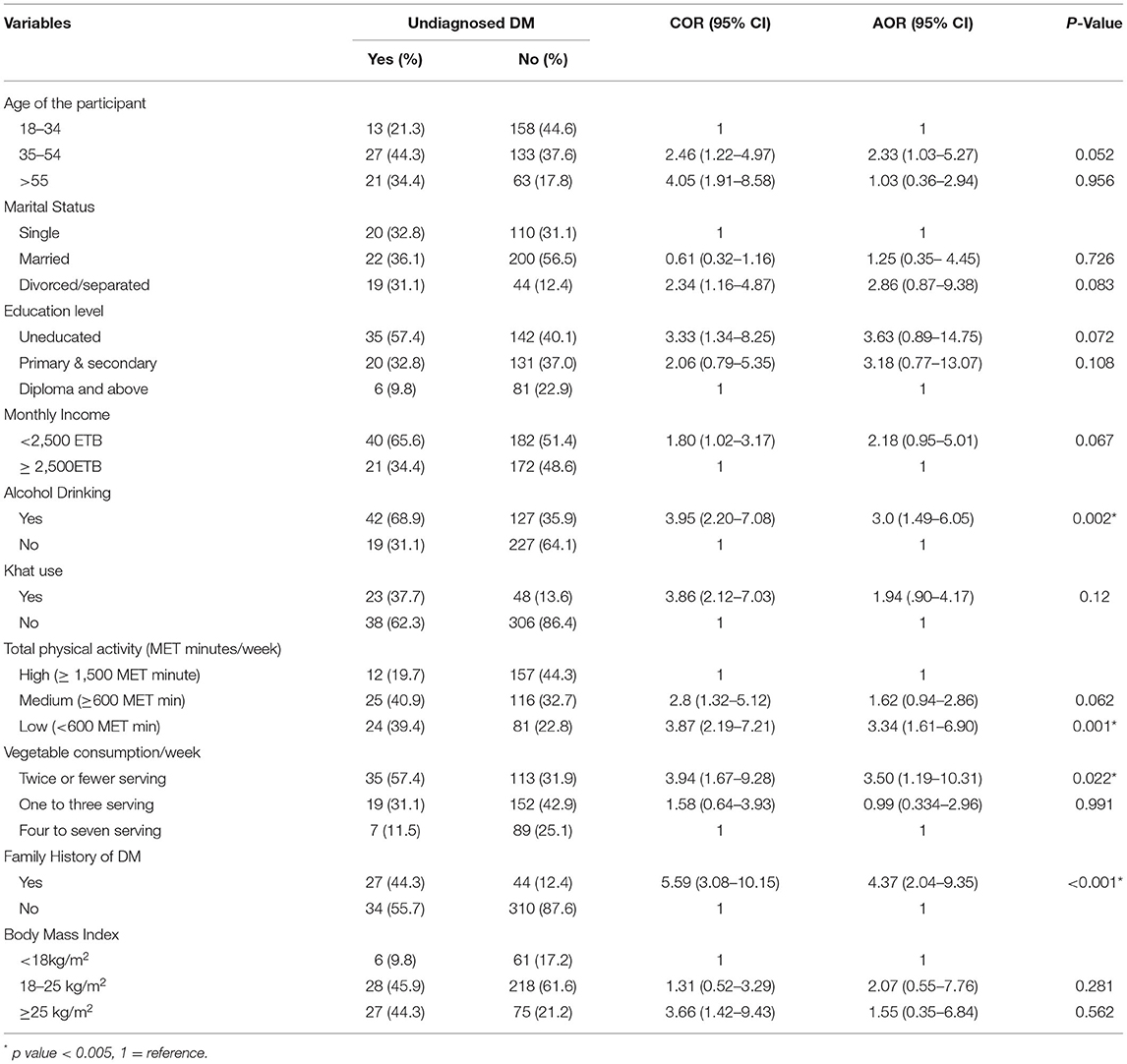
Table 4. Multivariable analysis of different variables with undiagnosed DM in Menja community, Southwest Ethiopia, 2021 (N = 415).
The overall prevalence of undiagnosed diabetes was 14.7%, with sex-specific prevalence being 16.8, and 11.1% for men and women, respectively. Family history of DM, alcohol intake, vegetable consumption, and physical activity were all found to be independent predictors of undiagnosed diabetes. The prevalence stated above was consistent with studies done in Ethiopia; Addis Ababa (14.8%) (24), Sidama Zuria Woreda 12.4% (25), East Gojam (11.5%) (26), and Kenya 14% (27). However, our findings were higher than the studies in Canada 5.6% (28), Italy (10%) (29), Germany (8%) (30), Bahr Dar town (10.2%) (12), Bisheftu town (5%) (31), Dre Dawa (6.2%) (13), Gonder (6.34%) (14), Koladiba town north-west Ethiopia (2.3%) (15), Kuwait (6.9%) (32), and pooled estimate of the African population (5.37%) (33). This is the fact that the socially disadvantaged or marginalized communities in any country are the most vulnerable to the disease (2). However, the result was lower than that of an Indian study (15%) (34). Differences in socio-demographic characteristics, lifestyle or behavioral patterns, health-seeking behavior, and practice of routine screening for diabetes and other health conditions are expected to be the cause of the gap.
Participants who had a family history of diabetes had a 4.4 times higher risk of having undiagnosed diabetes as compared to those who had not. This statement is supported by a study done in Bahrdar town (12), East Gojam (26), and Koladiba town (15). This is a fact that can be attributed to the hereditary relationship between diabetes and obesity. Moreover, participants who had a history of alcohol drinking had three times higher odds of undiagnosed diabetes as compared to those who did not have such a history. This finding was supported by a study conducted in Ethiopia from Addis Abeba and Bisheftu study settings (24, 31). Alcohol may play a role in insufficient insulin release, diminished insulin binding, and suppression of intracellular signaling, all of which contribute to the development of insulin resistance (35).
This study also revealed that vegetable consumption is associated with undiagnosed diabetes. The odds of undiagnosed diabetes were 3.5 times higher among participants who had vegetables serving two or fewer/week compared to those who had vegetables serving four to seven/week. This report is supported by a study done on Gonder, this could be due to the fiber included in veggies, which helps to lower serum cholesterol while also reducing the release of sugar into the bloodstream, lowering fasting blood glucose levels (36). Moreover, individuals who had a low habit of physical exercise significantly increased the risks of diabetes. Individuals with a low habit of physical exercise were at 3.3 times higher risk of developing diabetes as compared to their counterparts, which is consistent with a study done in East Gojam, and the Southern region of Ethiopia, undiagnosed diabetes was higher risk among those participants with sedentary behavior (26, 37). Regular physical activity is beneficial not only in lowering insulin resistance and increasing insulin production but also in lowering the risk of cardiovascular disease and obesity in diabetic individuals (38).
The prevalence of undiagnosed diabetes was high in the study setting. Alcohol use, family history, vegetable consumption, and physical exercise were the independent predictors of undiagnosed diabetes. As a result, the study recommends frequent screening and treatment for those with a family history of the disease, and raising awareness about the disease is recommended to aid in early detection and treatment. Minimizing alcohol drinking, frequent vegetable consumption, and physical exercise were recommended measures for the prevention and control of DM. Moreover, governmental and non-governmental organizations that are working in the area should give attention to these communities while providing diabetes-related services.
The strengths of this study were that it was community-based and included sufficient samples. The finding could be useful as a starting point for community screening programs for high-risk groups. However, the study has limitations in that it did not show the actual overall magnitude of diabetes, as known patients with diabetes were omitted. Furthermore, the study's cross-sectional design makes it difficult to demonstrate cause-and-effect linkages between the dependent and independent variables.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Mizan Tepi University. The patients/participants provided their written informed consent to participate in this study.
AA and NS had a significant contribution to this research in the conception and design of the study, data acquisition, data analysis, and interpretation, drafting and revising of the article, agreed to submit to the current journal, gave final approval of the version to be published, and agree to be accountable for all aspects of the work. Both authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, adjusted odds ratio; BMI, body mass index; BP, blood pressure; CI, confidence interval; COR, crude odd ratio; DM, diabetes mellitus; FBS, fasting blood sugar; GDM, gestational diabetes mellitus; HH, household; IDF, International Diabetes Federation; SD, standard deviation; WHO, World Health Organization.
1. American Diabetic Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. (2014). 37:81–90. doi: 10.2337/dc14-S081
2. Dr Margaret Chan. Global report on diabetes. Isbn. (2016). 978:6–86. Available online at: http://www.who.int/about/licensing/copyright_form/index.html
3. IDF Diabetes Atlas. Diabetes Around the World. (2021). Available Online at: https://diabetesatlas.org/ (accessed November 10, 2021).
4. WHO. Diabetes. WHO. (2021). Available Online at: https://www.who.int/es/news-room/fact-sheets/detail/diabetes (accessed November 10, 2021).
5. International Diabetes Federation. IDF Diabetes Atlas. (2013). Available Online at: www.idf.org/diabetesatlas (accessed May 27, 2013).
6. International Diabetes Federation Region A. Africa participant characteristics. Int Diabetes Fed. (2019). 60–2. Available online at: https://idf.org/our-network/regions-members/africa/members/9-ethiopia.html
7. International Diabetes Federation Region A. IDF Africa Members. (2021). Available Online at: https://idf.org/our-network/regions-members/africa/members/9-ethiopia.html (accessed March 2).
8. WHO Regional Office for Africa. Diabetes. (2021). Available Online at: https:www.afro.who.int/health-topics/diabetes (accessed November 14, 2021).
9. World health Organization. Diabetes. (2021). Available Online at: http://www.who.int/news-room/fact-sheets/detail/diabetes (accessed November 10, 2021).
10. Risk NCD, Collaboration F. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet (London. England). (2016) 387:1513–30. doi: 10.1016/S0140-6736(16)00618-8
11. Dessie G, Mulugeta H, Amare D, Negesse A, Wagnew F, Getaneh T, et al. A systematic analysis on prevalence and sub-regional distribution of undiagnosed diabetes mellitus among adults in African countries. J Diabetes Metab Disord. (2020) 19:1931–41. doi: 10.1007/s40200-020-00635-9
12. Bantie GM, Wondaye AA, Arike EB, Melaku MT, Ejigu ST, Lule A, et al. Prevalence of undiagnosed diabetes mellitus and associated factors among adult residents of Bahir Dar city, based northwest Ethiopia: a community- cross- sectional study. BMJ Open. (2019) 9:1–7. doi: 10.1136/bmjopen-2019-030158
13. Ayele BH, Roba HS, Beyene AS, Mengesha MM. Prevalent, uncontrolled, and undiagnosed diabetes mellitus among urban adults in Dire Dawa, Eastern Ethiopia: a population- based cross-sectional study. SAGE Open Med. 8:1–11. (2020) doi: 10.1177/2050312120975235
14. Wolde HF, Derso T, Biks GA, Yitayal M, Ayele TA, Gelaye KA, et al. High hidden burden of diabetes mellitus among adults aged 18 years and above in urban Northwest Ethiopia. Hindawi. (2020). 2020:9240398. doi: 10.1155/2020/9240398
15. Worede A, Alemu S, Gelaw YA, Abebe M. The prevalence of impaired fasting glucose and undiagnosed diabetes mellitus and associated risk factors among adults living in a rural Koladiba town, northwest Ethiopia. BMC Res Notes. (2017) 251:1–7. doi: 10.1186/s13104-017-2571-3
16. Bekele ATSGE. Prevalence of Diabetes Mellitus and Associated Factors in Addis Ababa Public Health Facilities. Diabetes, Metab Syndr Obes Targets Ther Dovepress open. (2020). 13:501–8. doi: 10.2147/DMSO.S237995
17. Lwanga SK. Sample Size Determination in Health Studies. world Heal Organ. (1991). Available Online at: https://tbrieder.org/publications/books_english/lemeshow_samplesize.pdf (accessed February 01, 1991).
18. Recommendations NAHA, Measurement BP. New AHA recommendations for blood pressure measurement. Am Fam Physician. (2022) 45:1–9. Available online at: https://www.ahajournals.org/doi/10.1161/CIR.0000000000001063
19. For BMI, Below, BMI, Above, II, Bmi, IIIT. Body Mass Index - BMI. World Health Organization. (2022). Available Online at: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed June 7, 2021).
20. Saitz R. Screening and brief intervention for unhealthy drug use : little or no efficacy screening and brief intervention for unhealthy drug use : little or no efficacy. Front Psychiatry. (2014) 5:121. doi: 10.3389/fpsyt.2014.00121
22. Mumu SJ, Ali L, Barnett A, Merom D. Validity of the global physical activity questionnaire (GPAQ) in Bangladesh. BMC Public Health. (2017) 650:1–10. doi: 10.1186/s12889-017-4666-0
23. Agudo A. Measuring Intake of Fruit Vegetables. World Heal Organ. (2004). Available Online at: https://www.who.int/dietphysicalactivity/publications/f&v_intake_measurement.pdf (accessed September 2004).
24. Ababa A. Prevalence of Diabetes Mellitus and Associated Factors in Addis Ababa Public Health Facilities. Dove Press J Diabetes. (2020) 13:501–8.
25. Woreda Z, Region S. Prevalence and Associated Factors of Diabetes Mellitus Among Adult Population in Hawassa. Dove Press J Diabetes, Metab Syndr Obes. (2020) 13:4571-−9. doi: 10.2147/DMSO.S275230
26. Wondemagegn AT, Bizuayehu HM, Abie DD, Ayalneh GM, Tiruye TY, Tessema MT, et al. Undiagnosed diabetes mellitus and related factors in East Gojjam (NW Ethiopia) in 2016 : a community-based study. J Public Heal Res. (2017) 6:4–9. doi: 10.4081/jphr.2017.834
27. Access O. Prevalence of undiagnosed diabetes and pre-diabetes among hypertensive patients attending Kiambu district hospital, Kenya: a cross-sectional study. Pan Africa Med J. (2015) 8688:1–12. doi: 10.11604/pamj.2015.22.286.7395
28. Asgupta KAD. Estimating the Population Prevalence of Diagnosed and Undiagnosed. Epidemiol Serv Research. (2013) 36:3002–8. doi: 10.2337/dc12-2543
29. Hadaegh F, Bozorgmanesh MR, Ghasemi A, Harati H, Saadat N, Azizi F. High prevalence of undiagnosed diabetes and abnormal glucose tolerance in the Iranian urban population : Tehran Lipid and Glucose study. BMC Public Health. (2008) 2:4–10. doi: 10.1186/1471-2458-8-176
30. Rathmann W, Haastert B, Icks A, Meisinger C, Holle R, Giani G. High prevalence of undiagnosed diabetes mellitus in Southern Germany : target populations for efficient screening. The KORA survey. (2003). 46:1–2. doi: 10.1007/s00125-002-1025-0
31. Institutions S, Shoa E. Prevalence of undiagnosed diabetes mellitus and its risk factors in selected institutions at bishoftu town, East Shoa, Ethiopia. J Diabetes Metab. (2013) 12:1–7. doi: 10.4172/2155-6156.S12-008
32. Mohammad T. Prevalence of prediabetes and undiagnosed diabetes among kuwaiti adults : a cross-sectional study. Dovepress Diabetes, Metab Syndr Obes Targets Ther. (2021). 14:2167–76. doi: 10.2147/DMSO.S296848
33. Asmelash D. Review article the burden of undiagnosed diabetes mellitus in adult African population : a systematic review and meta-analysis. Hindawi. (2019). 2019:4134937. doi: 10.1155/2019/4134937
34. Jawahar Ramasamy UKP. Prevalence of undiagnosed diabetes and prediabetes among voluntary blood donors in a tertiary health care setting. Int J Res Med Sci. (2016) 4:7. doi: 10.18203/2320-6012.ijrms20161850
35. Steiner JL, Crowell KT, Lang CH. Impact of Alcohol on Glycemic Control and Insulin Action. Biomolecules. (2015) 2223–46. doi: 10.3390/biom5042223
36. Asif M. The role of fruits, vegetables, and spices in diabetes. Int J Nutr Pharmacol Neurol Dis. (2011) 1:27. doi: 10.4103/2231-0738.77527
37. Alemayehu Z, Zekewos A, Loha E, Egeno T, Wubshet K, Merga Z. Prevalence of diabetes mellitus and associated factors in Southern Ethiopia: a community based study. Open Access. (2018) 28:451–460. doi: 10.4314/ejhs.v28i4.11
Keywords: diabetes, DM, undiagnosed, Menja, marginalized
Citation: Assefa A and Shifera N (2022) Undiagnosed Diabetes Mellitus and Its Predictors Among Socially Marginalized Menja Communities in Southwest Ethiopia. Front. Public Health 10:861627. doi: 10.3389/fpubh.2022.861627
Received: 08 February 2022; Accepted: 30 March 2022;
Published: 12 May 2022.
Edited by:
Åke Sjöholm, Gävle Hospital, SwedenReviewed by:
Richard Ephraim, University of Cape Coast, GhanaCopyright © 2022 Assefa and Shifera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashenafi Assefa, YXNoZWFzaHUyMUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.