- 1Department of Social Sciences, St. Pölten University of Applied Sciences, St. Pölten, Austria
- 2Department of Socioeconomics, Vienna University of Economics and Business, Vienna, Austria
- 3Department of Gerontology and Health Research, Karl Landsteiner University of Health Sciences, Krems an der Donau, Austria
In spite of findings highlighting higher health risk from infection compared to younger people, a certain percentage of older people in Austria still lack a valid vaccination certificate. The current gaps in vaccination coverage in countries such as Austria are likely to be in large part due to vaccination refusal and pose or will pose problems for the health system and consequently for all of society should the initial findings on Omicron coronavirus infectivity prove true. Surprisingly, only a few studies around the globe explicitly address older people's COVID-19 vaccination willingness. The present work therefore intends to contribute to this field by identifying factors associated with the decision for or against a vaccination among the older population in Austria. Data collected between late 2020 and early 2021 via the cross-national panel study Survey of Health, Aging and Retirement in Europe (SHARE) are used to perform multinomial logistic regression to analyse differences between COVID-19 vaccination supporters, undecided persons and rejectors. The results show that persons exhibiting a low risk assessment toward COVID-19, less health protection behaviors, lower education and belonging to households with financial burdens are significantly more likely to refuse vaccination or be ambivalent. Although multimorbidity reduces risk of vaccination refusal, poor subjective health was significantly related to a higher risk of refusing vaccination. The results point to the importance of addressing the factors related to refusal. Only by understanding these factors will it be possible to increase vaccination rates and thus minimize other restrictive measures.
Introduction
Nearly 260 million confirmed infections and five million fatalities from or with COVID-19 (1), as well as estimations from the World Health Organization that another 700,000 people could die from COVID-19 by spring 2022 in the European region alone (2) are the grim results of the SARS-CoV-2 pandemic by the end of 2021. In Austria nearly 1.1 million infections and 12,000 deaths were recorded by November 2021 (3). At completion of this paper, the country has undergone multiple lockdowns, in order to relieve the health care system with the fourth nationwide lockdown starting at the end of November 2021 (4), even though the first COVID-19 vaccinations had already been administered on Dec. 27, 2020 (5) and have been freely available to all people in Austria for several months (6).
Aim
Scientifically, vaccinations are indisputable as an effective means of combating infectious diseases (7) and, in the best case, have a reducing effect on infection, disease and transmission. Based on meta-analyses, COVID-19 vaccines have been shown to be highly effective in reducing infection and preventing severe disease progression (8, 9), additionally recent evidence suggests that transmission probability is reduced in vaccinated individuals (10). However, effective the vaccines may be, the desired consequence of this measures will only be achieved if there is an appropriate vaccination rate (11) and necessary amount of willingness in the population to get vaccinated. To achieve herd immunity, at least theoretically, recent estimates (based on data from Spain) suggest a good upper threshold of 70% for the ancestral variant, while the value for the delta variant is around 90% (12). However, it must be noted that these values vary according to multiple factors (12, 13), and that, even if the thresholds are reached, herd immunity does not constitute a panacea against the virus but requires adaptive and proactive measures.
Studies show that the COVID-19 vaccination acceptance rates at European (14) and at international level (15) varies significantly between countries. A recent review shows that of 114 countries, the acceptance rate is below 60% in 42 countries, whereby the situation is particularly diverse in Europe: At the beginning of 2021, the acceptance rate was 89% in Norway, 55% in Austria, and 47% in Hungary (16). As of December 7, 2021 (last check by the authors) 71.8% of the total population in Austria has had at least one COVID-19 vaccination and 67.6% has an active vaccination certificate (17). Even though the rapid increase of infections as of autumn 2021, followed by restrictions on unvaccinated persons and finally entering the fourth general lockdown as well as the multitude of public debates and subsequent announcement of a nationwide vaccination requirement starting in February 2022 (18) contributed to a slight increase in the coverage rate, which had been largely stagnant from August to November 2021 (17, 19), coverage rates continue to disappoint. It is noteworthy that even a certain percentage of older people in Austria continue to lack a valid vaccination certificate−18% among 55–64 year olds, 14% among 65–74 year olds, 10% among 75–84 year olds, and 13% among those 85 years and older (17)–in spite of findings highlighting higher health risk from infection for older persons as compared to younger people due to age-related physiological changes and multiple age-related comorbid conditions (20, 21). A large number of studies have demonstrated an age-related increase in health risk associated with COVID-19 infection (22, 23), which is reflected in more severe courses of disease and an increased risk of mortality (24, 25). This led many nations to prioritize their older population for vaccination at the advent of COVID-19 vaccines.
The current gaps in vaccination coverage in countries such as Austria are likely to be largely due to vaccination refusal despite availability of the vaccine (26), which poses health, economic, and ultimately social problems for society. The aim of this paper is to identify factors associated with the decision for or against COVID-19 vaccination among the older population using data of Austrian citizens.
State of Research and Hypotheses
A growing body of scientific work on the topic of COVID-19 vaccination willingness can be identified which has already led to several literature reviews (27–31). For Austria, the authors are aware of four internationally published papers (32–35) to date. Surprisingly, only a few studies worldwide explicitly address older people (36–44). Current data availability is likely to play a role here, as the second SHARE Corona Survey data—which includes data on vaccination willingness—for example, are not yet available for scientific analysis, although initial results have already been published (36). Therefore, the present work is intended to expand the knowledge on this important group, which we currently know little about.
Rather than presenting a rundown of the full state of research, the most important results, as per the authors, are highlighted, which are used to formulate hypotheses and will then be empirically tested. Results of studies on COVID-19 vaccination willingness among older adults and literature reviews will be addressed. Studies dealing with the vaccination willingness of specific groups such as parents in relation to their children (45), adolescents (32) or healthcare workers (46) are excluded.
Important factors for the willingness to receive a COVID-19 vaccination were identified as the individual risk assessment of a COVID-19 infection or illness on one hand (28, 29, 37–39) and past health protection behaviors, such as having gotten an influenza vaccination in the past, on the other hand (28, 29, 37, 40). On a theoretical level, this can be explained by Protection Motivation Theory (47). Thus, willingness to be vaccinated becomes less likely when an infection is perceived as unlikely to occur or as posing a negligible threat to health or if the recommended protective action (in this case vaccination), is perceived as ineffective or even harmful in its own right (48). With regard to health status, it has been shown that pre-existing illnesses or a poor subjective health status are associated with a lower rate of vaccination refusal (29, 36, 37, 49). Perceived vulnerability associated with health status (43) and the anticipated risk of infection to health (39) can be used as arguments in this context. Among the socioeconomic factors, financially disadvantaged individuals were shown to be more likely to refuse vaccination (28, 29, 36, 42). Higher education level (28, 29, 31, 37, 40, 42) and older age (27–29, 31, 36, 40–42) have been found to be positively associated with vaccination acceptance. In addition, differences between genders surfaced in multiple studies: men were less likely to refuse vaccination as compared to women (27, 28, 31, 36, 37, 41, 42); however, a recent Italian study came to the opposite conclusion for older people (40). Despite these individual findings, meta-analyses also reveal divergent impacts of socioeconomic factors (27–30) depending, among other things, on the surveyed groups, sociocultural factors and different measurement methods. This emphasizes the importance of further study on the issue, especially among older people. Based on the presented state of research the following hypotheses can be formulated:
• H1: The lower the risk assessment, the higher the risk of refusing vaccination.
• H2: The less health protection behavior is shown, the higher the risk of refusing vaccination.
• H3: The better the health status, the higher the risk of refusing vaccination.
• H4: The lower the level of education and the worse the financial situation, the higher the risk of refusing vaccination.
Furthermore, a relationship between the degree of autonomy and the willingness be vaccinated is suspected, as it had been shown that perceiving vaccination as a social norm in a persons' circle of friends and family positively influenced the acceptance of vaccination (50). Under such conditions, it can be assumed that a high degree of individual autonomy is required (51) to refuse vaccination.
H5: The higher the level of perceived autonomy, the higher the risk of refusing vaccination.
Methods
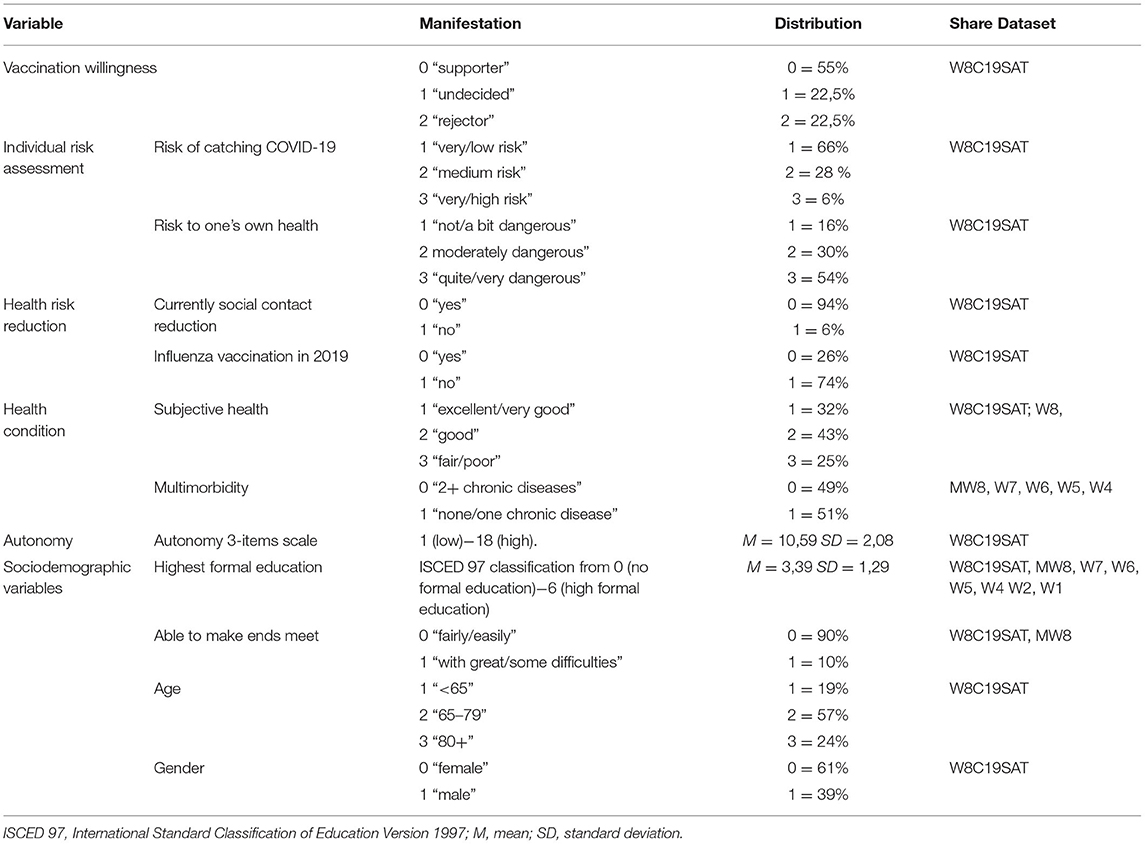
To test the hypotheses, data from the cross-national panel study Survey of Health, Aging and Retirement in Europe (SHARE) are used which includes data on persons aged 50 years and older living in the general population: Wave 8—COVID-19 Survey 1—Special Survey Austria (W8C19SAT) Release version: 1.0.0 (52) conducted from November 2020 to January 2021 in Austria via CATI serves were used as the main data source. In addition, data were imported from the main wave 8 survey (MW8) as well as from previous waves to minimize missing values (W7-W1). Table 1 shows the variables, their origin and distribution, whereby the values surveyed at the closest timepoint to the observation period (mainly W8C19SAT) were used for analyses.
Sample Description
A total sample of n = 2,522 respondents in Austria serves as basis for analyses. 61% of the sample are women, the average age of the respondents is M = 72, 67 years (SD = 8, 54 years); 33% live alone, 56% in a two-person, and 11% in a three- or more-person household. 20% of the respondents have low (ISCED 0-2), 51% moderate (ISCED 3-4) and 29% have high formal education (ISCED 5-6). The more highly educated group is overrepresented, overall, the distribution structure can be described as sufficient; see Table 1.
Operationalization
The dependent variable is nominally coded and differentiates between respondents who, during the survey period, (0) could imagine getting vaccinated against COVID-19 should such a vaccine be made available to them (55% hereafter referred to as “supporters”), (1) were undecided (22.5% “undecided”), and (2) were planning to refuse vaccination (22.5% “rejectors”).
Independent variables are divided into five dimensions—individual risk assessment, health protection behaviors, health condition, autonomy, and sociodemographic variables. For individual risk assessment, respondents were asked how threatening an infection with the SARS-CoV-2 virus would be (threat of virus) and how high they would estimate the probability of infection with the virus to their own person (probability of infection). Both items were measured using a 5-point rating scale and were grouped into three levels for analysis (see Table 1). For the dimension of health protection behaviors, a question on whether social contact had been reduced and another assessing whether the respondent had partaken in a vaccination against influenza in 2019 were included, these were answered with 0 “yes” and 1 “no”. Health condition is measured by subjective health assessment and multimorbidity. Multimorbidity is based on a longer list of questions (e.g., diabetes or high blood sugar etc.) and is coded as 0 “2+ chronic diseases” and 1 “none/one chronic disease”. This is due to the consideration that in comparison to persons with multimorbidity (reference group), the chance of belonging to the group of rejectors should increase for persons with no or only one chronic disease. Autonomy is measured using the subscale of the Psychological Well-being Scale of Ryff & Keyes (51) which calculates an additive index from 1 to 18 (low to high autonomy). According to Ryff & Keyes (51) a person with high scores should be independent and resists social pressure.
In addition, sociodemographic variables are included in the analyses. Education is classed into the International Standard Classification of Education (ISCED) for international comparability in SHARE [for more information, see the release guide of wave 8, see (52)]. For analyses, the variable ISCED97−0 = no formal education to 6 = high educational attainment—is used. Since ISCED data were largely unavailable at the time of the analysis in wave 8, this information had to be imported from previous survey waves. Financial situation is depicted using a question on the extent of difficulty for a household to make ends meet in a month; the 4-point scale was summarized in 0 “fairly/easily” and 1 “with great/some difficulties”. Age is coded as 1 “<65”, 2 “65–79” and 3 “80+”, gender as 0 “female” 1 “male”.
Statistical Analysis
Data analysis was conducted using IBM SPSS 27 and unweighted data was used for analysis. To test the hypothesized associations multinomial logistic regression (a method that generalizes logistic regression to multiclass problems) was performed to analyse all three groups (supporters, undecided and rejectors) together. For the statistical model, the category “supporter” was chosen as the reference category in the dependent variable; accordingly, the effects of the independent variables are to be considered in relation to the reference group. In order to check the goodness of fit, independent logical regression models were additionally calculated—among others, the values of the area under the receiver operating characteristic curve (ROC AUC) are shown below.
Results
For statistical requirements linearity was assessed using the Box and Tidwell (53) procedure and all metric variables were found to follow linearity to the logit. Goodness of fit for both independent models—supporters vs. undecided [Nagelkerke's R2 = 0.132 Hosmer–Lemeshow test (8) = 2,703; p = 0.952 and ROC AUC = 0.696] and supporters vs. rejectors [Nagelkerke's R2 = 0.273 Hosmer–Lemeshow test (8) = 2.730; p = 0.950 and ROC AUC = 0.777] are deemed acceptable. Consequently, the multinomial logistic regression with 2116 respondents was calculated [X2(30) = 440.238, p = 0.001]. Pearson's chi-square test [X2(3380) = 3419.328, p = 0.314] and deviance chi-square [X2(3380) = 3062.774, p = 1.00] indicate a good fit and Nagelkerke's R2 = 0.218 is deemed acceptable.
Table 2 shows the results of the multinomial logistic regression. Factors significantly associated with being in the group of undecided persons were found to be classification of risk of catching SARS-CoV-2 virus as moderate (odds ratio or OR 1.765), not having participated in the influenza vaccination in 2019 (OR 3.473), not having any or only one chronic disease(s) (OR 1.362) and reporting financial difficulties (OR 2.308). Being in very good health (OR 0.665), having a higher level of education (OR 0.843) and belonging to the 65–79 age group (OR 0.686) led to a reduction of probability to identify as undecided and a higher likelihood to be classed as a supporter of vaccination.
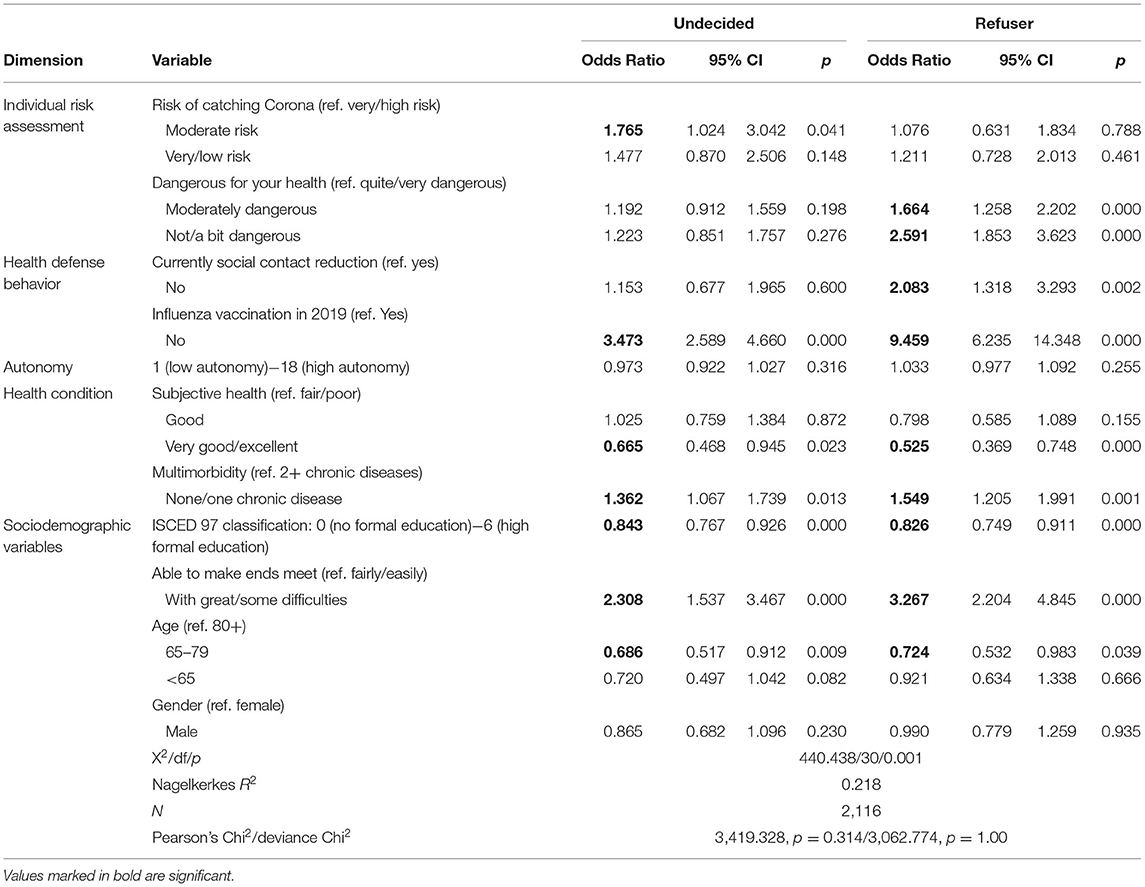
Table 2. Multinomial logistic regression vaccination willingness (supporter vs. undecided and supporter vs. refuser).
Persons were more likely to be classed as rejectors as compared to supporters if they assess the threat posed by COVID-19 as moderate (OR 1.664), or low (OR 2.591), did not currently reduce their social contacts (OR 2.083), did not get vaccinated against influenza in 2019 (OR 9.459), reported no or one chronic disease (OR 1.549) and had financial difficulties (OR 3.267). Like the comparison undecided/ supporters, a very good state of health (OR 0.525), higher level of education (OR 0.826) and belonging to the age group 65–79 (OR 0.724) lead to a reduction in likelihood to be part of the rejector group.
It is apparent, that the structure of supporters vs. undecided and supporters vs. rejectors is similar, with autonomy, health status and socioeconomic variables showing particularly striking similarity across both comparisons. Slight differences in individual risk assessment and health protection behavior can be observed: While undecided persons and supporters do not differentiate along the assessment of threat posed by COVID-19, the probability of being undecided increases when the own risk of infection is assessed as low. The reverse is true when comparing supporters and rejectors: while there is no differentiation along the assessment of own risk of infection, the probability of belonging to the group rejecting a vaccination increases when threat of a COVID-19 infection is assessed as lower. Correspondingly, as the threat of the virus is estimated as less severe, social contact reduction is seen less often in this group as compared to supporters. Results of the comparison of supporters vs. rejectors are discussed in more detail below.
Discussion
Focussing on the first two dimensions (health risk assessment and health protection behaviors) it seems clear that a low perception of threat posed by the virus, lack of prior (influenza vaccination) and current (reduction of social contact) health protection behaviors increase the risk of being classed among the persons rejecting a COVID-19 vaccination. All of these factors thus indicate underestimation of risk and, according to the Protection Motivation Theory (47), make willingness to get vaccinated less probable. Therefore, H1 and H2 can be largely confirmed based on the data, with the notable limitation that supporters and rejectors do not differ in respect to the estimated risk of COVID-19 illness (probability of catching COVID-19). Based on Protection Motivation Theory it follows that it is not the perceived risk of getting infected with the virus, but rather the perceived consequences of such an infection for one's own health (severity of expected health problems), which fundamentally differentiates between these two groups. Conclusively, previous results are confirmed (29, 37).
The unexpected result concerning health status, which contradicts expectations set out in H3, must be considered as problematic: assessment of health status as good or fair reduces the risk of rejecting the vaccine by a factor of 0.53, i.e., a negative health assessment lead to a higher probability of refusing vaccination among older respondents. Not only do rejectors show a higher predisposition for infection due to their comparative lack of health protection behaviors but may also have an increased risk for severe courses of illness due to their poorer health status. Results using SHARE data from the summer of 2021 also showed an association between negative assessment of health status and more frequent refusal of vaccination in Bulgaria, Estonia, Latvia and Slovenia whereas no significant correlation has been found in other countries (36). However, as the second variable depicting health status (multimorbidity) followed the hypothesized direction (multimorbidity patients were less likely to reject the vaccination), H3 cannot be fully rejected.
H5 must be rejected based on the empirical analysis: Autonomy does not seem to be related to the decision to be vaccinated. At first glance, this may seem surprising, as the image of the “autonomous rejectors” is often perpetuated by the media. It is likely, that especially in the beginning of vaccination debates, both camps contained a broad cross-section of people with a high and low degree of autonomy. Further studies should examine this aspect, as the group of rejectors is or has become smaller probably due to increasing social pressure.
Hypothesis H4 can be confirmed by the present study and thus supports many of the international findings (28, 29, 36, 42). In short, the higher the level of education and the better the financial means, the lower the risk of refusing Covid-19 vaccination. In addition, gender has no influence, which is also confirmed by another study (36) for Austria, and the age group 65–79 years has a lower risk of refusing vaccination as compared to the oldest old (80+ years). Comparing our used data of the special SHARE survey Austria with the results of the second SHARE Corona Survey (36), a clear reduction of the group of “undecided” persons between the two survey time points—about 8 months apart—can be found, however the block of rejectors remained relatively strong in summer 2021 with 15% (in contrast to 22.5% in the end of 2020/early 2021).
As a limitation, it must be noted that the study presented only a fraction of variables, which is reflected in the level of Nagelkerke's R2. In particular, the exploration of the motivations for and against vaccination of the older population against the socioeconomic background could provide further insights. In view of the different acceptance rates in Europe, caution is required when generalizing the results also because the situation is currently undergoing rapid change. Further analysis is needed to better understand the remaining core of rejectors.
Conclusion
This study points to the importance of understanding reasons for vaccination rejection. Only by understanding these factors it will be possible to increase vaccination rates and thus minimize other restrictive measures put in place to stop the pandemic spread. It seems particularly alarming that people with a poor subjectively health assessment had a higher risk of being among the refusers, and that socioeconomic status plays a considerable role. The question of how these groups can be activated for health measures, which has been raised before and will continue to be asked, will play an important part in the management, and hopefully the end of this health crisis. At least in Austria, the pandemic has proven once again that social inequalities become manifest in health behavior and, arguably, in health inequalities.
Data Availability Statement
This paper uses data from SHARE Waves 1, 2, 4, 5, 6, 7 and 8 (DOIs: 10.6103/SHARE.w1.800, 10.6103/SHARE.w2.800, 10.6103/SHARE.w4.800, 10.6103/SHARE.w5.800, 10.6103/SHARE.w6.800, 10.6103/SHARE.w7.800, 10.6103/SHARE.w8.800, 10.6103/SHARE.w8ca.800), see Börsch-Supan et al. (2013) for methodological details.
Author Contributions
LR was the primary author of this manuscript. Analysis and writing were done in collaboration with SS and TH. All authors contributed to the article and approved the submitted version.
Funding
Under the terms of the Austria Open Access Publishing Framework Agreement, the St. Pölten University of Applied Sciences (Fachhochschule St. Pölten/FH St. Pölten) will cover Article Publishing Fees for eligible authors in any of the Frontiers journals. The SHARE data collection has been funded by the European Commission, DG RTD through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, and SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA No. 211909, SHARE-LEAP: GA No. 227822, SHARE M4: GA No. 261982, and DASISH: GA No. 283646), and Horizon 2020 (SHARE-DEV3: GA No. 676536, SHARE-COHESION: GA No. 870628, SERISS: GA No. 654221, and SSHOC: GA No. 823782) and by the DG Employment, Social Affairs and Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332, and VS 2020/0313. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the United States National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04–064, HHSN271201300071C, and RAG052527A) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. WHO Coronavirus (COVID-19) Dashboard. (2021). Available online at: https://covid19.who.int (accessed November 26, 2021).
2. World Health Organization - Regional Office for Europe. The WHO European Region Could Hit Over 2 Million COVID-19 Deaths by March 2022. We Can Avoid Reaching This Grim Milestone by Taking Action Now. (2021). Available online at: https://www.euro.who.int/en/media-centre/sections/press-releases/2021/the-who-european-region-could-hit-over-2-million-covid-19-deaths-by-march-2022.-we-can-avoid-reaching-this-grim-milestone-by-taking-action-now (accessed November 26, 2021).
3. World Health Organization. Austria: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data. 2021. Available online at: https://covid19.who.int (accessed November 26, 2021).
4. Federal Ministry of Social Affairs, Health, Care and Consumer Protection. 5. COVID-19-Notmaßnahmenverordnung – 5. COVID-19-NotMV [5th COVID-19 Emergency Regulation - 5th COVID-19-NotMV]. BGBl. II Nr. 475/2021. Available online at: https://www.ris.bka.gv.at/eli/bgbl/II/2021/475/20211121 (accessed November 22, 2021).
5. Pollak M, Kowarz N, Partheymüller J. Chronology of the Corona Crisis in Austria - Part 4: Lockdowns, Mass Testing and the Launch of the Vaccination Campaign. Corona-Blog/University of Vienna. 2021. Available online at: https://viecer.univie.ac.at/en/projects-and-cooperations/austrian-corona-panel-project/corona-blog/corona-blog-beitraege/blog100-en/ (accessed December 6, 2021).
6. Pollak M, Kowarz N, Partheymüller J. Chronology of the Corona Crisis in Austria - Part 5: Third Wave, Regional Lockdowns and the Vaccination Campaign. Corona-Blog/University of Vienna. (2021). Available online at: https://viecer.univie.ac.at/en/projects-and-cooperations/austrian-corona-panel-project/corona-blog/corona-blog-beitraege/blog112-en/ (accessed December 6, 2021).
7. Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. (2008) 86:140–6. doi: 10.2471/BLT.07.040089
8. Harder T, Koch J, Vygen-Bonnet S, Külper-Schiek W, Pilic A, Reda S, et al. Efficacy and effectiveness of COVID-19 vaccines against SARS-CoV-2 infection: interim results of a living systematic review, 1 January to 14 May 2021. Eurosurveillance. (2021) 26:2100563. doi: 10.2807/1560-7917.ES.2021.26.28.2100563
9. Harder T, Külper-Schiek W, Reda S, Treskova-Schwarzbach M, Koch J, Vygen-Bonnet S, et al. Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection with the Delta (B.1.617.2) variant: second interim results of a living systematic review and meta-analysis, 1 January to 25 August 2021. Eurosurveillance. (2021) 26:2100920. doi: 10.2807/1560-7917.ES.2021.26.41.2100920
10. Mostaghimi D, Valdez CN, Larson HT, Kalinich CC, Iwasaki A. Prevention of host-to-host transmission by SARS-CoV-2 vaccines. Lancet Infect Dis. (2021) 22:e52–8. doi: 10.1016/S1473-3099(21)00472-2
11. Kemp F, Proverbio D, Aalto A, Mombaerts L. Fouquier d'Hérouël A, Husch A, et al. Modelling COVID-19 dynamics and potential for herd immunity by vaccination in Austria, Luxembourg and Sweden. J Theor Biol. (2021) 530:110874. doi: 10.1016/j.jtbi.2021.110874
12. García-García D, Morales E, Fonfría ES, Vigo I, Bordehore C. Caveats on COVID-19 herd immunity threshold: the Spain case. Sci Rep. (2022) 12:598. doi: 10.1038/s41598-021-04440-z
13. Kadkhoda K. Herd Immunity to COVID-19: Alluring and Elusive. Am J Clin Pathol. (2021) 155:471–2. doi: 10.1093/ajcp/aqaa272
14. Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. (2020) 21:977–82. doi: 10.1007/s10198-020-01208-6
15. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. (2021) 27:225–8. doi: 10.1038/s41591-020-1124-9
16. Sallam M, Al-Sanafi M, Sallam M. A global map of COVID-19 vaccine acceptance rates per country: an updated concise narrative review. J Multidiscip Healthc. (2022) 15:21–45. doi: 10.2147/JMDH.S347669
17. Federal Ministry of Social Affairs, Health, Care and Consumer Protection. Covid-19 in Austria/Vaccination numbers (6.12.2021). (2021). Available online at: https://info.gesundheitsministerium.gv.at/impflage (accessed December 6, 2021).
18. Federal Ministry of Social Affairs, Health, Care and Consumer Protection. Die aktuellen Maßnahmen zum Coronavirus im Überblick [The current measures on coronavirus at a glance]. (2021). Available online at: https://www.sozialministerium.at/Informationen-zum-Coronavirus/Coronavirus—Aktuelle-Maßnahmen.html (accessed December 6, 2021).
19. Desson Z, Kauer L, Otten T, Peters JW, Paolucci F. Finding the way forward: COVID-19 vaccination progress in Germany, Austria and Switzerland. Health Policy Technol. (2021) 100584. doi: 10.1016/j.hlpt.2021.100584
20. Nikolich-Zugich J, Knox KS, Rios CT, Natt B, Bhattacharya D, Fain MJ. SARS-CoV-2 and COVID-19 in older adults: what we may expect regarding pathogenesis, immune responses, and outcomes. GeroScience. (2020) 42:505–14. doi: 10.1007/s11357-020-00186-0
21. Shahid Z, Kalayanamitra R, McClafferty B, Kepko D, Ramgobin D, Patel R, et al. COVID-19 and older adults: what we know. J Am Geriatr Soc. (2020) 68:926–9. doi: 10.1111/jgs.16472
22. Palmer S, Cunniffe N, Donnelly R. COVID-19 hospitalization rates rise exponentially with age, inversely proportional to thymic T-cell production. J R Soc Interface. (2021) 18:20200982. doi: 10.1098/rsif.2020.0982
23. Bartleson JM, Radenkovic D, Covarrubias AJ, Furman D, Winer DA, Verdin E. SARS-CoV-2, COVID-19 and the aging immune system. Nat Aging. (2021) 1:769–82. doi: 10.1038/s43587-021-00114-7
24. Biswas M, Rahaman S, Biswas TK, Haque Z, Ibrahim B. Association of sex, age, and comorbidities with mortality in COVID-19 patients: a systematic review and meta-analysis. Intervirology. (2021) 64:36–47. doi: 10.1159/000512592
25. Flook M, Jackson C, Vasileiou E, Simpson CR, Muckian MD, Agrawal U, et al. Informing the public health response to COVID-19: a systematic review of risk factors for disease, severity, and mortality. BMC Infect Dis. (2021) 21:342. doi: 10.1186/s12879-021-05992-1
26. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
27. Al-Amer R, Maneze D, Everett B, Montayre J, Villarosa AR, Dwekat E, et al. COVID-19 vaccination intention in the first year of the pandemic: a systematic review. J Clin Nurs. (2022) 31:62–86. doi: 10.1111/jocn.15951
28. Aw J, Seng JJB, Seah SSY, Low LL. COVID-19 vaccine hesitancy—a scoping review of literature in high-income countries. Vaccines. (2021) 9:900. doi: 10.3390/vaccines9080900
29. Wake AD. The willingness to receive COVID-19 vaccine and its associated factors: “Vaccination Refusal Could Prolong the War of This Pandemic” – a systematic review. Risk Manag Healthc Policy. (2021) 2021:2609–23. doi: 10.2147/RMHP.S311074
30. Nehal KR, Steendam LM, Campos Ponce M, van der Hoeven M, Smit GSA. Worldwide vaccination willingness for COVID-19: a systematic review and meta-analysis. Vaccines. (2021) 9:1071. doi: 10.3390/vaccines9101071
31. Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. (2021) 194:245–51. doi: 10.1016/j.puhe.2021.02.025
32. Humer E, Jesser A, Plener PL, Probst T, Pieh C. Education level and COVID-19 vaccination willingness in adolescents. Eur Child Adolesc Psychiatry. (2021) 1–3. doi: 10.1007/s00787-021-01878-4 [Epub ahead of print].
33. Knobel P, Zhao X, White KM. Do conspiracy theory and mistrust undermine people's intention to receive the COVID-19 vaccine in Austria? J Community Psychol. (2021) 50:1269–81. doi: 10.1002/jcop.22714
34. King I, Heidler P, Marzo RR. The long and winding road: uptake, acceptability, and potential influencing factors of COVID-19 vaccination in Austria. Vaccines. (2021) 9:790. doi: 10.3390/vaccines9070790
35. Schernhammer E, Weitzer J, Laubichler MD, Birmann BM, Bertau M, Zenk L, et al. Correlates of COVID-19 vaccine hesitancy in Austria: trust and the government. J Public Health. (2021) 44:e106–16. doi: 10.1093/pubmed/fdab122
36. Bergmann M, Hannemann T-V, Bethmann A, Schumacher AT. Determinants of SARS-CoV-2 vaccinations in the 50+ Population. SSRN Electron J. (2021). doi: 10.2139/ssrn.3938975
37. Al-Hanawi MK, Alshareef N, El-Sokkary RH. Willingness to receive COVID-19 vaccination among older adults in Saudi Arabia: a community-based survey. Vaccines. (2021) 9:1257. doi: 10.3390/vaccines9111257
38. Chia JL, Hartanto A. Cognitive barriers to COVID-19 vaccine uptake among older adults. Front Med. (2021) 8:756275. doi: 10.3389/fmed.2021.756275
39. Fadda M, Suggs LS, Albanese E. Willingness to vaccinate against Covid-19: A qualitative study involving older adults from Southern Switzerland. Vaccine X. (2021) 8:100108. doi: 10.1016/j.jvacx.2021.100108
40. Gallè F, Sabella EA, Roma P, Da Molin G, Diella G, Montagna MT, et al. Acceptance of COVID-19 vaccination in the elderly: a cross-sectional study in southern Italy. Vaccines. (2021) 9:1222. doi: 10.3390/vaccines9111222
41. Malani PN, Solway E, Kullgren JT. Older adults' perspectives on a COVID-19 vaccine. JAMA Health Forum. (2020) 1:e201539. doi: 10.1001/jamahealthforum.2020.1539
42. Nikolovski J, Koldijk M, Weverling GJ, Spertus J, Turakhia M, Saxon L. et al. Factors indicating intention to vaccinate with a COVID-19 vaccine among older US adults. PLoS ONE. (2021) 16:e0251963. doi: 10.1371/journal.pone.0251963
43. Williams L, Gallant AJ, Rasmussen S, Brown Nicholls LA, Cogan N, Deakin K, et al. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. (2020) 25:1039–54. doi: 10.1111/bjhp.12468
44. Salibi N, Abdulrahim S, El Haddad M, Bassil S, El Khoury Z, Ghattas H, et al. COVID-19 vaccine acceptance in older Syrian refugees: preliminary findings from an ongoing study. Prev Med Rep. (2021) 24:101606. doi: 10.1016/j.pmedr.2021.101606
45. Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents' and guardians' views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. (2020) 38:7789–98. doi: 10.1016/j.vaccine.2020.10.027
46. Szmyd B, Karuga FF, Bartoszek A, Staniecka K, Siwecka N, Bartoszek A, et al. Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: a cross-sectional study from Poland. Vaccines. (2021) 9:218. doi: 10.3390/vaccines9030218
47. Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol. (1975) 91:93–114. doi: 10.1080/00223980.1975.9915803
48. Eberhardt J, Ling J. Predicting COVID-19 vaccination intention using protection motivation theory and conspiracy beliefs. Vaccine. (2021) 39:6269–75. doi: 10.1016/j.vaccine.2021.09.010
49. Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. (2021) 21:804. doi: 10.1186/s12889-021-10816-7
50. Wolff K. COVID-19 vaccination intentions: the theory of planned behavior, optimistic bias, and anticipated regret. Front Psychol. (2021) 12:648289. doi: 10.3389/fpsyg.2021.648289
51. Ryff CD, Keyes CLM. The structure of psychological well-being revisited. J Pers Soc Psychol. (1995) 69:719–27. doi: 10.1037/0022-3514.69.4.719
52. Börsch-Supan A. (2021). Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 8. COVID-19 Survey 1. Release version: 1.0.0. Data set. doi: 10.6103/SHARE.w8ca.100
Keywords: COVID-19, vaccination willingness, Austria, older people, vaccine hesitancy
Citation: Richter L, Schreml S and Heidinger T (2022) Ready for Vaccination? COVID-19 Vaccination Willingness of Older People in Austria. Front. Public Health 10:859024. doi: 10.3389/fpubh.2022.859024
Received: 20 January 2022; Accepted: 02 May 2022;
Published: 03 June 2022.
Edited by:
Marc Jean Struelens, Université Libre de Bruxelles, BelgiumReviewed by:
Malik Sallam, The University of Jordan, JordanShafayat Sultan, University of Dhaka, Bangladesh
Copyright © 2022 Richter, Schreml and Heidinger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lukas Richter, bHVrYXMucmljaHRlckBmaHN0cC5hYy5hdA==
 Lukas Richter
Lukas Richter Stephan Schreml
Stephan Schreml Theresa Heidinger
Theresa Heidinger