- 1Department of Epidemiology, Center for Global Health, School of Public Health, Nanjing Medical University, Nanjing, China
- 2College of Public Health, Zhengzhou University, Zhengzhou, China
- 3Key Laboratory of Infectious Diseases, School of Public Health, Nanjing Medical University, Nanjing, China
Background: Tuberculosis (TB) infection interferes with the health-related quality of life (HRQOL), including physical, social, mental, emotional and financial domains of individuals. The goal of this scoping review is to outline the most frequent mental issues encountered by TB patients and evaluate the effects of mental health on TB treatment outcomes. Our findings identify research gaps that could help bridge the overall treatment outcomes in the near future.
Method: A systematic stepwise approach was adopted to search online resource databases like PubMed, Web of science, and gray literature to retrieve published scientific articles for the review. Titles and abstracts of selected studies were examined for their possible eligibility. The studies matching our eligibility criteria were taken into account for this scoping review.
Results: One hundred and ninety three articles were retrieved out of which 26 met the final inclusion criteria. We found that studies adopting interventional approaches reported good mental wellbeing outcomes and better medical compliance as compared with studies that just investigated the subjects. The data represented 15 countries including three low-income countries (LICs), four low-middle-income-countries (LMICs), seven upper-middle-income countries (UMICs), and one high-income country (HIC).
Conclusion: Depression, anxiety, and poor social support, and stigma affect the wellbeing of individuals across the globe irrespective of age, race, demographic characteristics, geographical location, and social status.
Introduction
Ever since its discovery and first global outbreak in the year 1882 (1), tuberculosis (TB) has been the leading infectious disease cause of death worldwide and remains a public health concern (2). A report released by the World Health Organization (WHO) estimated the TB-related death toll at 1.3 million as of 2017 with a projection of millions more getting infected in subsequent years (3). Despite the global implementation of Directly Observed Therapy, Short Course (DOTS), TB incidence is decreasing by only 1–2% per year (4). This is substantially lower than the estimated speed through mathematical modeling. The World Health Organization (WHO) clearly defines health as an overall state of complete physical, mental and social wellbeing and not merely the absence of any infirmity or disease (5). TB infection interferes with the health-related quality of life (HRQOL), including physical, social, mental, emotional and financial domains of individuals (6). Adherence and HRQOL are both important indicators of the overall TB treatment spectrum. Evaluating psychiatric comorbidities in HRQOL is needed alongside the diagnosis of TB and likewise assessment with the continuity of anti-TB treatment (7).
Major mental health problems associated with TB are anxiety and depression (8). Anxiety disorders are characterized extensively by excessive worrying, apprehensiveness, the fear of future events, and uneasiness (9). Anxiety disorders make up one of the most common complications of psychiatric disorders. In 2013 alone, it was estimated that 8.2 million cases were reported in the general population of the UK with women being twice the number of people becoming anxious than men (10). Depression on the other hand is a common mental disorder that allows people to experience low mood, loss of self-interest or pleasure, the feeling of guilt or low self-worth, disturbed sleep or appetite, low energy, and poor concentration (11). According to the estimation by WHO, 300 million people are currently living with depression (12) and with no doubt, most people falling in this category are likely to be a patient suffering from TB or other chronic diseases (12). This has been reported in many studies that there is a three to six times increase in the tendency of becoming depressed due to TB and associated co-morbidities (13). These co-conditions pose a greater public health threat because it may lead to medication default.
However, psychological issues complicate treatment outcomes in people with infectious diseases like TB and chronic diseases such as diabetes, multiple sclerosis, Alzheimer's, HIV, and cancer (14). Maneuvering the gaps between the physical, mental and social aspects of health will affect the overall outcome of diseases. Therefore, assessing the association of TB on the mental wellbeing of its victims is usually underestimated in most institutions. Moreover, social support and stigma could be an important factor in the treatment outcomes of TB patients, leading to a decrement in mental wellbeing (15). The socioeconomic burden on households and individuals could pose a devastating effect if a strong social network within one's outreach is lost. Social support is defined as various means by which individuals help others or social interactions making the subject or individual believe he/she is being valued and cared for (16). Social support helps individuals to seek the appropriate and timely help when conditions and network interactions are strong and reliable for psychological support through stressful events especially when it's solely demonstrated through health-seeking behaviors (17). Stigma on the other hand is defined as a mark of disgrace or a form of disgrace associated with a particular circumstance. It's a process that usually begins when a trait of an individual is identified as disvalued or undesirable (15). This is a complex setting involving the community, institutions, and intrapersonal relationships leading to decrement of self-worth and self-value for one self (18).
The goal of this scoping review is to outline the most frequent mental issues encountered by TB patients and evaluate the effects of mental health on TB treatment outcomes. Our findings identify research gaps that could help bridge the overall treatment outcomes in the near future.
Materials and Methods
Search Strategy and Study Selection
We systematically searched for studies in PubMed, Web of Science, and the gray literature. A systematic stepwise approach based on the methodological framework proposed by Arksey and O'Malley in 2005 (19) was adopted. An incorporated recommendation by Levac was also used to make the search more comprehensive (20) and up to date. Additionally, the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) (21) was employed to guide this review. The search approach was updated to February 2018 and publications in English were included. Keywords for database searching included “mental health status”, “mental health”, “treatment outcomes”, “social support”, “depression”, “anxiety”, “stigma”, “tuberculosis”, and “Mycobacterium tuberculosis” amongst others (full search strategies are detailed in Supplementary File 1). Titles and abstracts of selected studies were examined for their possible eligibility. The studies matching our eligibility criteria were taken into account for this scoping review. Studies were required to have all of the following characteristics: Papers included in our research included both qualitative and quantitative if they fit the mental health status. Articles were also included if they conformed with the search terms of TB and mental health co-morbidity with HIV/AIDS since the majority of studies showed that most people in Africa living with HIV are co-infected with TB. The paper selection flow chart is shown in Figure 1.
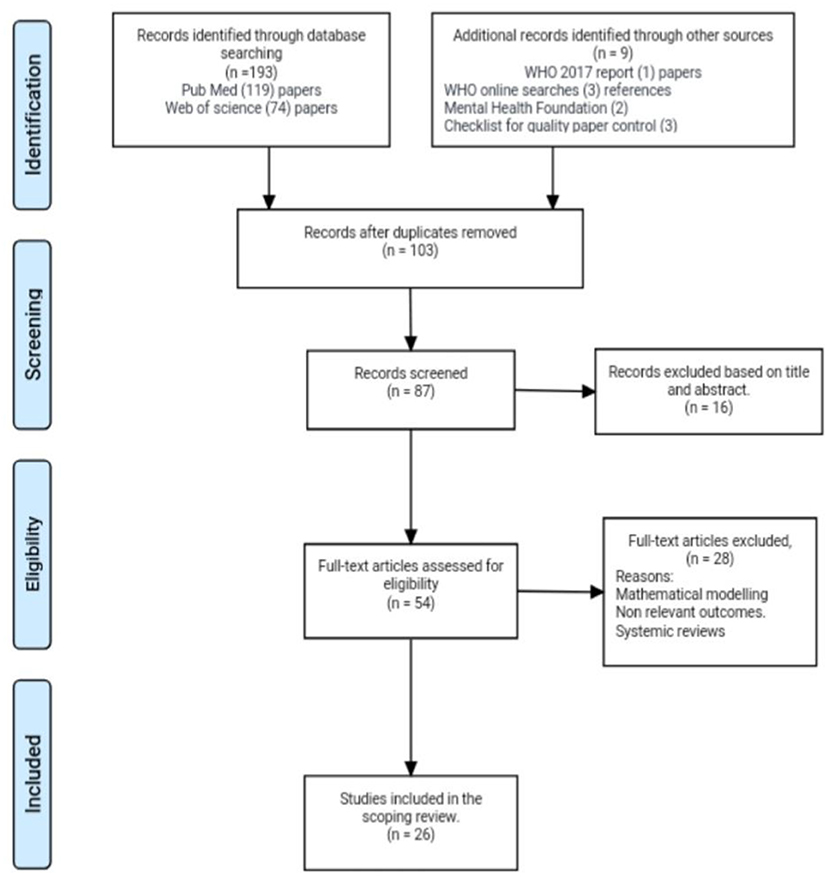
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) flow diagram for scoping review.
Data Extraction
At each stage of review, two reviewers extracted data independently and they subsequently met to resolve discrepancies. In case of continued disagreement, a third reviewer adjudicated study inclusion. The information extracted from the selected papers included Author(s) name, year of publication, country, aim or purpose of the study, the sample size of population, methodology, intervention type (if applicable), implications, concept, and key findings (Table 1). Supplementary File 2 summarizes the data extracted for this scoping review.
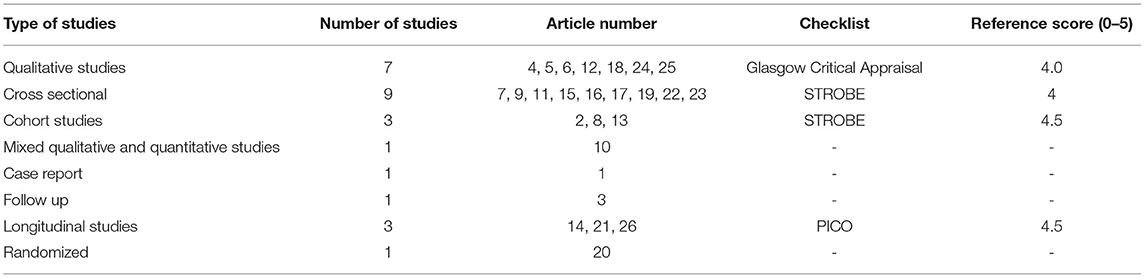
Quality Control
The quality of the articles retrieved was evaluated using different tools. Cross-sectional and observational articles included in this review were cross-checked with the STROBE (strengthening the reporting of observational studies in epidemiology) (22). Longitudinal designs were subjected to a check using the PICO (P stands for population, I stands for intervention, C stands for control and O stands for outcome) (23). Qualitative studies were identified and were also cross-checked by critical appraisal checklist (24). This article was also guided by adopting the PRISMA (21) checklist. The data we retrieved were separated into anxiety, depression and social support, and stigma. The quality check was scored with a reference range of 0–5, where 0 was the least score if articles didn't meet the quality tool checklist and 5 was the highest score if the articles meet the checklist protocol. The three main categorized articles were then combined in one folder using endnote to check for duplications of articles. All studies included in this review met the quality assessment framework of their respective studies. Table 2 shows the quality assessment for eligible studies included in Data extraction.
Results
Study Selection
The results primarily yielded an overall number of 1,972 papers during the initial hit in the search engines. We then applied the combination of the mesh terms to yield 193 papers. Our online search also yielded two links from the mental health foundation, three quality checklist kits, three WHO online searches for statistics on depression, MDGs, and SDGs, and one pdf file from the current WHO report on TB. The first electronic extraction resulted in a total number of 193 papers. In PubMed after extraction hits, using Boolean extractions and screening it yielded a total of 119 articles, and the same was applied to the Web of Science database which consequently also yielded a total result of 74 papers. We screened both databases using abstracts and titles and handpicked 103 articles after duplication. Sixteen articles were further excluded after screening by abstract and titles. Eighty seven articles were eligible. Furthermore, 54 articles were pulled out after accessing their full text. A second reviewer provided recommendations after going through the list and screening. Twenty eight articles were excluded due to non-relevant outcomes and some study designs were mathematical in a model, which didn't fit our criteria, and some were also excluded due to information overlap. We then thoroughly read the full text and were able to get 26 available articles that met our inclusion criteria during our search (Figure 1). After cross-checking carefully, duplication methods were applied and handpicked to prevent a repetition of a particular study. Longitudinal studies were checked using the PICO element, cross-sectional and observational studies was cross-checked using the STROBE checklist and qualitative papers were crossed checked by the critical appraisal checklist. All the articles screened passed for eligibility. Seven qualitative searches were found, one mixed method of qualitative and quantitative, nine cross-sectional articles, and three cohort studies. We also encountered one case report, one follow-up study, three longitudinal studies, and finally one randomized study. Our study also comprised 15 different countries with three different multi-country studies. Articles concluded that decrement in mental health impacts TBs outcome and compliance hence there is an increase tendency to medication adherence and poor prognosis. With prior inclusion and exclusion criteria, our search was narrowed down to a total of 103 papers.
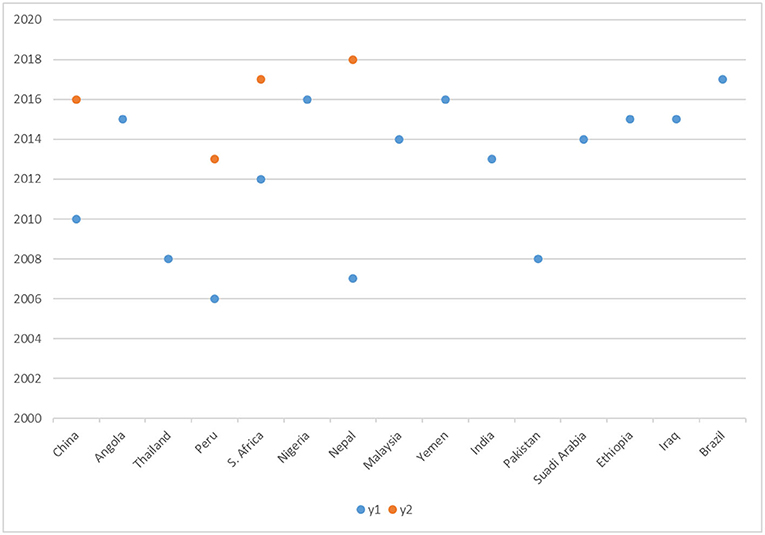
Location of Studies
Of the 26 studies we analyzed, three were multi-country related, three were in South Africa, two were in Peru, two were in Ethiopia, two were in Nepal, two were in China and the other nine studies were conducted across the globe. Based on the World Bank Report (25), we classified the countries into upper-middle-income countries (UMICs), low-middle-income countries (LMICs), low-income countries (LICs), and high-income countries (HIC). Figure 2 illustrates the publications in different regions and different years.
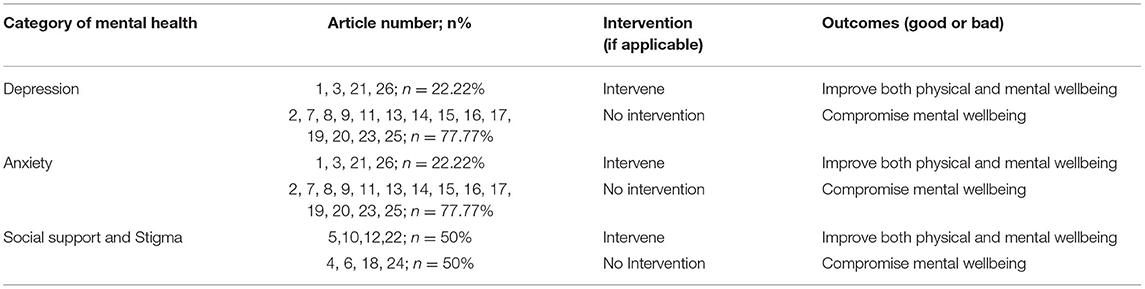
Interventional Outcomes
We divided interventional outcomes into depression, anxiety, and social support, and stigma. There were 18 articles reporting depression but only four articles (#1, 3, 21, and 26) adopted interventions, and the outcome of mental health with medication adherence were improved in patients making up 22.2% of total articles in the depression category. The remaining 14 articles (#2, 7, 8, 9, 11, 13, 14, 15, 16, 17, 19, 20, 23, and 25) did not perform interventions but reported data on depression. There were four articles (#1, 3, 21, and 26) adopted interventions and the other 14 articles (#2, 7,8,9,11,13,14,15,16, 17, 19, 20, 23, 25) reported data on anxiety. Regarding social support and stigma, there were 4 articles (5, 10, 12, and 22) that adopted interventions and six articles (#4, 6, 18, and 24) that had no intervention but reported data on social support and stigma. Table 3 gives the summary of the interventions and non-interventional outcomes.
Depression
Depression in TB patients leads to the outcome of delay in seeking medical care which eventually leads to negative medication adherence (6). Psychiatric comorbidity being reported as depression was a major decrement to health leading to a default in seeking appropriate health (26). In a research done in South Africa, a significant frequency of psychological distress among tuberculosis patients was found, with most individuals, particularly those from lower socioeconomic classes, becoming depressed throughout treatment, resulting in a lack of negative health-seeking behavior. (27). Furthermore, patients classified as MDR-TB experienced more depression (28). The impact of mental health on TB patients has hindered their wellbeing both emotionally and spiritually which makes it a hindrance to seeking a healthy behavior, hence affecting treatment outcomes in a long round (29, 30). In Peru, a study reported 37% depression in newly identified TB cases (31). A cross-sectional survey from 48 low and middle-income countries concluded that the proportion of depression is relatively high among TB patients with a consequent decrement in health status than in that among the general population (32). Depression peaks in patients on anti TB medications, hence we need strategic outlines and interventions to deal with the side effects of these medications. But fewer studies have been conducted on this subject matter (29).
Anxiety
The impact of anxiety has been demonstrated largely through the feeling of anger and ruminating over past events that led to contracting TB which could prolong treatment duration (31). Psychiatric co-morbidity increases the risk to decrement in health and default (26). Anxiety was found to be a key psychological domain in a Zambian study in which 37.6% of patients were found to be suffering from anxiety (31). A similar study conducted in Huambo Angola had similar findings outlining emotional distress and anxiety to be present among TB patients (33). Anxiety disorder and miliary TB were also reported in a case study of a 67-year-old Saudi man who qualified for anxiety definition under the Diagnostic and Statistical Manual of Mental disorders (DSM-5) with excessive anxiety, but his symptoms elevated due to treatment of TB (34). This report limits the studies only to identifying anxiety symptoms in association with TB but couldn't go on further to outline the mechanism involved in it (34). In Porto Algero, Brazil a study also demonstrated generalized anxiety disorder prevalent in TB patients and quantified the number of psychiatry co-morbidity in 68% of hospitalized TB patients (6). Anxiety and mental health disorder have been demonstrated to be in poor accordance with effective treatment outcomes (6). Poor medical compliance and adherence to treatment were also demonstrative in a study conducted in Pakistan with an anxiety rating of 47% (35). Hence anxiety is also a key mental health problem in TB patients.
Social Support and Stigma
Despite the fear of being infected, family support and individual relationships have proven to help most TB patients overcome the fear of public rejection (36). A study conducted in Peru outlined that all patients with TB who disclosed their disease to their families were welcomed and cherished with an abundance of love, encouragement, financial support, and emotional strength as compared to those who hid it away from their loved ones (17). However, a crucial factor leading to high default of TB care is stigma (37). Stigma negatively affects the individuals by breeding depression, self-hate and disappointment, hindering patients from accessing the required healthcare he/she needs (38). With a good support system, family members and loved ones served as advocates who constantly reminded TB clients to seek help (17). External stigma as well as familial stigma both have huge impacts on the mental health wellbeing of people affected by TB. In the family settings, patients suffering from TB were sometimes left alone to fend for themselves, leading to isolation and self-neglect (37). Stigma and discrimination have led to a negative effect on health-seeking behavior in patients who suspects having TB due to long cough duration (39). Being highly portrayed in communities, especially in low and middle-income countries (LMICs), people suffering from TB tend to hide their symptoms and rather spread the infection (40). A research conducted in Peru assessed treatment outcomes when nurses served as emotional supporters to patients with TB and concluded that social support and networking was vital to the recovery as it helped their spiritual wellbeing (41). It is stipulated by other studies that, socio-cultural attributes of most communities due to lack of public education on TB interfere with treatment adherence and may lead to new infections in the future (42, 43). Social support is hence an important determinant for a good outcome in all diseases. A study from Shaanxi province in China showed how lack of TB education among family members affected the outcome of TB and hence an integral program and campaign was needed to improve the outlook on TB (44, 45). The sparse evidence presented is also an indication of mental health neglect.
Interventional Approaches
Quality of Life is a multifaceted notion that spans the physical, social, psychological, economic, spiritual, and other realms. As a result, it's difficult to define and measure, but it may be roughly defined as people's judgments of their place in life in relation to their objectives, aspirations, standards, and worries in the context of the culture and value systems in which they live. As part of mitigations to improve patients' quality of life, some countries implemented interventions to combat clinical depression and anxiety observed among TB patients. One study conducted in Malaysia reported addressing mental wellness on time manner by first accessing it at baseline and during the treatment course. This aided early identification of depression and anxiety onset in TB patients for which psychosocial counseling was offered to improve the mental wellbeing (46). Additionally, two studies found that targeted detection and aggressive treatment of major depressive episodes from baseline would also improve the mental wellbeing of TB throughout treatment (31, 34). In Peru, there was a marked increase in mental health after providing necessary support to patients (41). Counselors were also provided in one setting in Nepal, which saw to counseling TB patients to cope with their disease and treatment side effects (47). An encouragement for a high level of support from family and friends also proved important and effective in the recovery process in India (48). Implementing interventions that measure and mitigate stigma at the local community level also proved an effective way of the intervening potential for depression among TB clients as was observed in Thailand (49). These interventions have a good impact on patients' treatment outcomes and quality of life. Hence, we entreat that such interventions will have in-depth research to help identify suitable measures in treating TB patients worldwide.
The requirement for a multidisciplinary team, such as incorporating the clinical psychologist when sent home or during an inpatient, was highlighted in certain literatures. The core of these disciplines will aid in bridging the gap between depression and home-based long-term care. Another intervention that may be used to reach remote settlers is the use of telemedicine. In its most basic form, telemedicine may be used. In the absence of a smart phone, satellite tiny phones can be used to call clients on a regular basis for a phone checkup. This is an interventional strategy that will be quite beneficial. It will also assist if DOT centers are established in health facilities or primary health care institutions. Health care workers who will staff these clinics should be given extra training in basic psychological assessments to aid in the rapid identification of symptoms for appropriate treatment or referral to a specialist (50). The examples above are only a handful of the interventional strategies that are required.
Discussion
This review ascertained the effects of mental wellbeing on the impact of effective TB treatment around the world. Out of 26 articles retrieved, all articles well documented the observed impacts of mental health on treatment outcomes of TB and consequent decrement in the mental aspects of TB victims. However, limited research existed on the effects of possible interventions to improve the balance between mental wellbeing and improvement of TB outcome (6, 40, 47, 51, 52).
One qualitative study from Peru demonstrated how nurses helped hospitalized MDR-TB patients serving as treatment supporters to cope well with their infirmity and there was significant progress in the outcome of treatment (41). We subsequently think this type of intervention should be applied in different regions across the world to help promote the mental health of TB patients in addition to encouraging family members and immediate friends circle to join in the support. One of the interventions was timely actions taken within the treatment period to address mental wellbeing using feasible tools and designing indicators to help alleviate symptoms (46, 49). Another intervention was to extend educational programs to families and caregivers to encourage patient adherence to seeking positive health behavior (48). Educational programs can take place on different platforms such as social media, radio, and TV programs, marketplace campaigns in LMICs, and involving local celebrities to serve as ambassadors for educating the masses on such issues. We think this could help patients establish strong self-worth. A follow-up study in Penang General Hospital using SF-36 questionnaire found that even though other symptoms improved significantly with treatment, 23% of patients were at risk of depression at the end of TB treatment, which may be due to lack of psychological support during the treatment period (46). This implies that assessing psychological status at baseline and working toward improving every domain of HRQOL is significant in the pathway to a free TB world in the near future. We suggest that hospitals should include psychological therapy such as counseling as part of the treatment program. In another study, major depressive and anxiety episodes (MDE) were measured using a 5-item version in 325 patients (31). The presence of major depressive episodes at baseline was associated with negative outcomes (31). Depressive and anxiety are mostly found during an initial stages of diagnosis and may lead to negative outcomes if psychological packages are not strategized to encourage patients to adhere and retain care regimes (14, 48).
HRQOL in TB patients is usually underestimated in many settings, especially in LMICs where major resources are usually directed to improving only microbial symptoms, but neglecting the mental, physical and other domains in relation to HRQOL. A South Africa study adopted the SF-12, EQ-5D and St. George's respiratory scale, and observed a positive relationship between treatment adherence and HRQOL in patients with TB (53). It is therefore obvious that elevating microbial symptoms alone by using drugs will address some domains but others may be left out. LMICs with a high burden of TB may prioritize anti-TB drugs over psychological support. We think this phenomenon may be due to an extra financial burden that will be invested into getting more mental health workers which might not fit into the budget plan of LMICs. Also, a prospective cohort study in Nepal suggested psychological support package is acceptable to patients and hence requires additional investment to counselors in TB clinics (47). This supports the recommendation that there is an urgent need for resource allocation to psychological support training in clinics and DOT centers in LMICs.
There is a need for further studies and improvement on caregivers training in recognizing, identifying, and implementing a social network approach to treating TB patients. National and provincial/district CDCs, primary care facilities, and other public health agencies have to mobilize workforces that will look into all aspects of health during the treatment course. Extra funding and research are needed, especially in the field of mental health. An integral effort by all agencies to increase the capacity of mental health workers in the field and national TB programs and the need to support primary caregivers should also be frontier on the agenda in most countries. Catastrophic cost on the victim's finances and family, socio-economic status considerations in that area of study, and cultural beliefs of the society in question are some of the driving factors we identified that could also lead to a decrement in the mental wellbeing of patients.
We further assessed the quality of reviewed studies and observed some limitations with some articles which may have affected the quality of the findings. For starters, interpreted findings in some articles were not expressed clearly due to data not being solely collected for analyzing the effect of mental wellbeing on medication adherence. Also, some studies used different measurements for assessing the mental wellbeing of patients. Some articles investigated just specific effects of how TB affects them mentally, while others considered measuring other factors leading to a potential decrease of mental wellbeing among TB patients. Other studies also focused on the measurement of physical wellbeing as compared to mental wellbeing but mostly neglected to make it an exclusive inclusion of all factors leading to medication adherence. This review also observed that qualitative studies mostly collected data only at one point in time without follow-up. We deem this an important gap as results may not reflect the true context of mood alterations, which could have led to a bias.
Limitation and Strength
This systemic review was limited in a number of ways. The search was limited to only 13 years from 2005 to 2018. During the search, we might have limited ourselves to only papers which were available in the databases used and their titles as well as abstracts matched our keywords. Moreover, taking data samples representing the whole population is very vital to understanding the variation and complexity of studies. The use of convenient sampling however seemed to be commonly utilized in most research and is a vital limitation to most studies (6, 17, 54). Representation of just a particular group of people, for example, smear-positive TB patients alone, cannot be used as a generalization for the whole population (46). Studies that were cross-sectional in nature did not really identify a clear-cut relation between anxiety, depression with reference to other factors that have been found to compromise the mental wellbeing (53). They were mostly focused on the determination of a link between depression, anxiety and TB excluding confounding factors that may contribute to a compromised mental health (53). Considering general factors will help identify areas to be addressed so as to get a quick intervention in that area. The correlation of anxiety, depression, and TB has been established in most studies but factors have been poorly outlined (52).
Irrespective of the above-noted limitations to the quality of the articles, a review of the data collated by them is highly informative and good enough to inform treatment policy formation and upgrade. This review combined findings from a case report, qualitative and quantitative studies together thereby ensuring the capture of all relevant information on the topic making it one of the strengths.
Conclusion
The evidence of the effects of mental health on TB outcomes has been well captured in this review. Depression, anxiety and poor social support, and stigma evidently affect the mental well-being of individuals across the globe, irrespective of age, race, demographic characteristics, geographical location, and social status. Moreover, there is an urgent need to address TB in a multidisciplinary approach to combat the overall quality of treatment outcomes. Patients with all forms of TB may or may not experience optimum mental wellbeing depending on a variety of reasons influencing the patient and this needs further research.
Implication of Research
This review underscores the importance of studies in the field of mental health in relation to TB patients across the globe. Further research needs to be conducted in the field of mental health to outline strategies that will help promote the mental wellbeing of TB patients during treatment across the world. Furthermore, recent research on mental health and its association to medication adherence using causal inference analysis and meditational modeling will optimize treatment protocols for better outcomes as well as help understand limitations and pathways leading to default in TB treatment.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
CA and JW: conceptualization, methodology, and software. CA: formal analysis and visualization. CA, MM, BH, QL, and HS: investigation and writing—original draft preparation. MM, BH, QL, and HS: data curation and validation. JW: supervision, project administration, resources, writing—review and editing, and funding acquisition. All authors have given final approval of the version to be published and agreed on the journal to which the article has been submitted.
Funding
This study was funded by the National Natural Science Foundation of China (81973103), Nanjing Major Science and Technology Project (2021-11005), Medical Research Project of Jiangsu Health Commission (ZDB2020013), and Key Project of Philosophy and Social Science Research in Colleges and Universities in Jiangsu Province (2020SJZDA096). The funding agencies had no role in the study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
All authors of the manuscript thank and acknowledge their respective Universities and Institutes.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.855515/full#supplementary-material
References
1. Barberis I, Bragazzi NL, Galluzzo L, Martini M. The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus. J Prev Med Hyg. (2017) 58:E9–e12.
2. Kebede Y, Andargie G, Gebeyehu A, Awoke T, Yitayal M, Mekonnen S, et al. Tuberculosis and HIV are the leading causes of adult death in northwest Ethiopia: evidence from verbal autopsy data of Dabat health and demographic surveillance system, 2007-2013. Popul Health Metr. (2017) 15:27. doi: 10.1186/s12963-017-0139-z
3. Walker IF. Implementation of a psychosocial support package for people receiving treatment for multidrug-resistant tuberculosis in Nepal: a feasibility and acceptability study. Int J Behav Med. (2018) 13:e0201163. doi: 10.1371/journal.pone.0201163
4. endtb. (2018). Available online at: http://www.who.int/tb/strategy/en/ (accessed April 3, 2019).
5. Health. (2018). Available online at: https://en.wikipedia.org/wiki/Health (accessed April 3, 2019).
6. Dos Santos AP, Lazzari TK, Silva DR. Health-related quality of life, depression and anxiety in hospitalized patients with tuberculosis. Tuberc Respir Dis. (2017) 80:69–76. doi: 10.4046/trd.2017.80.1.69
7. Peltzer K, Pengpid S. Anxiety and depressive features in chronic disease patients in Cambodia, Myanmar and Vietnam. S Afr J Psychiatr. (2016) 22:940. doi: 10.4102/sajpsychiatry.v22i1.940
8. Wang XB Li XL, Zhang Q, Zhang J, Chen HY, Xu WY, et al. A survey of anxiety and depressive symptoms in pulmonary tuberculosis patients with and without tracheobronchial tuberculosis. Front Psychiatry. (2018) 9:308. doi: 10.3389/fpsyt.2018.00308
9. Kumar K, Kumar A, Chandra P, Kansal HM. A study of prevalence of depression and anxiety in patients suffering from tuberculosis. J Family Med Prim. (2016) 5:150–3. doi: 10.4103/2249-4863.184641
10. Anxiety. (2018). Available online at: https://www.mentalhealth.org.uk/statistics/mental-health-statistics-anxiety (accessed April 11, 2019).
11. Mental Health. (2018). Available online at: https://www.mentalhealth.org.uk/statistics (accessed April 11, 2019).
12. Depression. (2018). Available online at: http://www.who.int/news-room/fact-sheets/detail/depression (accessed April 15, 2019).
13. Alene KA, Clements ACA, McBryde ES, Jaramillo E, Lonnroth K, Shaweno D, et al. Mental health disorders, social stressors, and health-related quality of life in patients with multidrug-resistant tuberculosis: a systematic review and meta-analysis. J infect. (2018). 77:357–67. doi: 10.1016/j.jinf.2018.07.007
14. Turner J, Kelly B. Emotional dimensions of chronic disease. West J Med. (2000) 172:124–8. doi: 10.1136/ewjm.172.2.124
15. Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. (Washington, DC: 1974). (2010) 125:34–42. doi: 10.1177/00333549101250S407
16. Social Support. (2018). Available online at: http://psychology.iresearchnet.com/social-psychology/interpersonal-relationships/social-support/ (accessed April 17, 2019).
17. Paz-Soldan VA, Alban RE, Jones CD, Oberhelman RA. The provision of and need for social support among adult and pediatric patients with tuberculosis in Lima, Peru: a qualitative study. BMC Health Serv Res. (2013) 13:290. doi: 10.1186/1472-6963-13-290
18. Pungrassami P, Kipp AM, Stewart PW, Chongsuvivatwong V, Strauss RP, Van Rie A. Tuberculosis and AIDS stigma among patients who delay seeking care for tuberculosis symptoms. Int J Tuberc Lung Dis. (2010) 14:181–7.
19. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
20. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implementat. Sci. (2010) 5:69. doi: 10.1186/1748-5908-5-69
21. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
22. Strobe Checklist. Available online at: https://www.strobe-statement.org/fileadmin/Strobe/uploads/checklists/STROBE_checklist_v4_combined.pdf (accessed April 19, 2019).
23. PICO ELEMENT. Available online at: https://canberra.libguides.com/c.php?g=599346&p=4149722 (accessed April 19, 2019).
24. Qualitative Checklist. (2018). Available online at: https://www.gla.ac.uk/media/media_64038_en.pdf (accessed April 19, 2019).
25. Organization WH. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division (2019). Available online at: https://apps.who.int/iris/handle/10665/327595
26. Koyanagi A, Vancampfort D, Carvalho AF, DeVylder JE, Haro JM, Pizzol D, et al. Depression comorbid with tuberculosis and its impact on health status: cross-sectional analysis of community-based data from 48 low- and middle-income countries. BMC Med. (2017) 15:209. doi: 10.1186/s12916-017-0975-5
27. Peltzer K, Naidoo P, Matseke G, Louw J, McHunu G, Tutshana B. Prevalence of psychological distress and associated factors in tuberculosis patients in public primary care clinics in South Africa. BMC Psychiatry. (2012) 12:89. doi: 10.1186/1471-244X-12-89
28. Das M, Isaakidis P, Van den Bergh R, Kumar AM, Nagaraja SB, Valikayath A, et al. HIV, multidrug-resistant TB and depressive symptoms: when three conditions collide. Glob Health Action. (2014) 7:24912. doi: 10.3402/gha.v7.24912
29. Theron G, Peter J, Zijenah L, Chanda D, Mangu C, Clowes P, et al. Psychological distress and its relationship with non-adherence to TB treatment: a multicentre study. BMC Infect Dis. (2015) 15:253. doi: 10.1186/s12879-015-0964-2
30. Thomas BE, Shanmugam P, Malaisamy M, Ovung S, Suresh C, Subbaraman R, et al. Psycho-socio-economic issues challenging multidrug resistant tuberculosis patients: a systematic review. PLoS ONE. (2016) 11:e0147397. doi: 10.1371/journal.pone.0147397
31. Ugarte-Gil C, Ruiz P, Zamudio C, Canaza L, Otero L, Kruger H, et al. Association of major depressive episode with negative outcomes of tuberculosis treatment. PLoS ONE. (2013) 8:e69514. doi: 10.1371/journal.pone.0069514
32. Yan S, Zhang S, Tong Y, Yin X, Lu Z, Gong Y. Nonadherence to antituberculosis medications: the impact of stigma and depressive symptoms. Am J Trop Med Hyg. (2018) 98:262–5. doi: 10.4269/ajtmh.17-0383
33. Xavier PB, Peixoto B. Emotional distress in Angolan patients with several types of tuberculosis. Afr Health Sci. (2015) 15:378–84. doi: 10.4314/ahs.v15i2.10
34. Alosaimi FD, Alkharboush FA, Altuwariqi MH. A case of anxiety associated with miliary tuberculosis. Int Med Case Rep J. (2014) 7:111–5. doi: 10.2147/IMCRJ.S64855
35. Husain MO, Dearman SP, Chaudhry IB, Rizvi N, Waheed W. The relationship between anxiety, depression and illness perception in tberculosis patients in Pakistan. CP & EMH. (2008) 4:4. doi: 10.1186/1745-0179-4-4
36. Yin J, Wang X, Zhou L, Wei X. The relationship between social support, treatment interruption and treatment outcome in patients with multidrug-resistant tuberculosis in China: a mixed-methods study. TM & IH. (2018) 23:668–77. doi: 10.1111/tmi.13066
37. Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. (2013) 103:813–21. doi: 10.2105/AJPH.2012.301069
38. Zarova C, Chiwaridzo M, Tadyanemhandu C, Machando D, Dambi JM. The impact of social support on the health-related quality of life of adult patients with tuberculosis in Harare, Zimbabwe: a cross-sectional survey. BMC Res Notes. (2018) 11:795. doi: 10.1186/s13104-018-3904-6
39. Craig GM, Daftary A, Engel N, O'Driscoll S, Ioannaki A. Tuberculosis stigma as a social determinant of health: a systematic mapping review of research in low incidence countries. Int J Infect Dis. (2017) 56:90–100. doi: 10.1016/j.ijid.2016.10.011
40. Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: a qualitative study. BMC Public Health. (2007) 7:211. doi: 10.1186/1471-2458-7-211
41. Chalco K, Wu DY, Mestanza L, Munoz M, Llaro K, Guerra D, et al. Nurses as providers of emotional support to patients with MDR-TB. Int Nurs Rev. (2006) 53:253–60. doi: 10.1111/j.1466-7657.2006.00490.x
42. Gibson N, Cave A, Doering D, Ortiz L, Harms P. Socio-cultural factors influencing prevention and treatment of tuberculosis in immigrant and Aboriginal communities in Canada. Soc Sci Med. (2005) 61:931–42. doi: 10.1016/j.socscimed.2004.10.026
43. Grede N, Claros JM, de Pee S, Bloem M. Is there a need to mitigate the social and financial consequences of tuberculosis at the individual and household level? AIDS Behav. (2014) 18 Suppl 5:S542–53. doi: 10.1007/s10461-014-0732-0
44. Zhang S, Li X, Zhang T, Fan Y, Li Y. The experiences of high school students with pulmonary tuberculosis in China: a qualitative study. BMC Infect Dis. (2016) 16:758. doi: 10.1186/s12879-016-2077-y
45. Zhang SR, Yan H, Zhang JJ, Zhang TH Li XH, Zhang YP. The experience of college students with pulmonary tuberculosis in Shaanxi, China: a qualitative study. BMC Infect Dis. (2010) 10:174. doi: 10.1186/1471-2334-10-174
46. Atif M, Sulaiman SA, Shafie AA, Asif M, Sarfraz MK, Low HC, et al. Impact of tuberculosis treatment on health-related quality of life of pulmonary tuberculosis patients: a follow-up study. Health Qual Life Outcomes. (2014) 12:19. doi: 10.1186/1477-7525-12-19
47. Lee G, Scuffell J, Galea JT, Shin SS, Magill E, Jaramillo E, et al. Impact of mental disorders on active TB treatment outcomes: A systematic review and meta-analysis. Int J Tuberculosis Lung Dis. (2020) 24:1279–84. doi: 10.5588/ijtld.20.0458
48. Isaakidis P, Rangan S, Pradhan A, Ladomirska J, Reid T, Kielmann K. 'I cry every day': experiences of patients co-infected with HIV and multidrug-resistant tuberculosis. TM & IH. (2013) 18:1128–33. doi: 10.1111/tmi.12146
49. Van Rie A, Sengupta S, Pungrassami P, Balthip Q, Choonuan S, Kasetjaroen Y, et al. Measuring stigma associated with tuberculosis and HIV/AIDS in southern Thailand: exploratory and confirmatory factor analyses of two new scales. TM & IH. (2008) 13:21–30. doi: 10.1111/j.1365-3156.2007.01971.x
50. Volmink J, Garner P. Interventions for promoting adherence to tuberculosis management. Cochrane Database Syst Rev. (2000) 4:Cd000010. doi: 10.1002/14651858.CD000010
51. Ambaw F, Mayston R, Hanlon C, Alem A. Depression among patients with tuberculosis: determinants, course and impact on pathways to care and treatment outcomes in a primary care setting in southern Ethiopia–a study protocol. BMJ Open. (2015) 5:e007653. doi: 10.1136/bmjopen-2015-007653
52. Duko B, Gebeyehu A, Ayano G. Prevalence and correlates of depression and anxiety among patients with tuberculosis at WolaitaSodo University Hospital and Sodo Health Center, WolaitaSodo, South Ethiopia, Cross sectional study. BMC Psychiatry. (2015) 15:214. doi: 10.1186/s12888-015-0598-3
53. Scuffell J, Boccia D, Garcia Velarde F, Leon SR, Raviola G, Lecca L, et al. Mental disorders and drug/alcohol use in patients commencing extensively drug-resistant tuberculosis treatment. Public Health Action. (2017) 7:237–9. doi: 10.5588/pha.17.0044
Keywords: tuberculosis, mental health, health-related quality of life, treatment, adherence
Citation: Agbeko CK, Mallah MA, He B, Liu Q, Song H and Wang J (2022) Mental Health Status and Its Impact on TB Treatment and Its Outcomes: A Scoping Literature Review. Front. Public Health 10:855515. doi: 10.3389/fpubh.2022.855515
Received: 15 January 2022; Accepted: 25 April 2022;
Published: 31 May 2022.
Edited by:
Harshavardhan Sampath, Sikkim Manipal University, IndiaReviewed by:
Anmol Pradhan, Sikkim Manipal University, IndiaShijo Joseph, Mar Sleeva Medicity, India
Copyright © 2022 Agbeko, Mallah, He, Liu, Song and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianming Wang, am13YW5nQG5qbXUuZWR1LmNu
 Charles Kwaku Agbeko
Charles Kwaku Agbeko Manthar Ali Mallah
Manthar Ali Mallah Biyu He1
Biyu He1