
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 22 July 2022
Sec. Health Economics
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.853438
Background: The prevalence of cigarette smoking in China is high and the utilization of smoking cessation clinics is very low. Multicomponent smoking cessation interventions involving community and hospital collaboration have the potential to increase the smoking cessation rate. However, the cost-effectiveness of this intervention model is unknown.
Methods: We conducted a smoking cessation intervention trial in 19 community health service centers in Beijing, China. A cost-effectiveness analysis was performed from a societal perspective to compare three strategies of smoking cessation: no intervention (NI), pharmacological intervention (PI), and comprehensive intervention (CI) (PI plus online health promotion). A Markov model, with a time horizon of 20 years, was used to simulate the natural progression of estimated 10,000 male smokers. A cross-sectional survey was conducted to obtain data on costs and quality-adjusted life years (QALYs) by using the five-level EuroQol-5-dimension (EQ-5D-5L) questionnaire. Probabilistic sensitivity analysis was performed to explore parameters of uncertainty in the model.
Results: A total of 680 participants were included in this study, including 283 in the PI group and 397 in the CI group. After 6 months of follow-up, the smoking cessation rate reached 30.0% in the CI group and 21.2% in the PI group. Using the Markov model, compared with the NI group, the intervention strategies of the PI group and the CI group were found to be cost-effective, with an incremental cost-effectiveness ratio (ICER) of $535.62/QALY and $366.19/QALY, respectively. The probabilistic sensitivity analysis indicated that the CI strategy was always the most cost-effective intervention.
Conclusion: CI for smoking cessation, based in hospital and community in China, is more cost-effective than PI alone. Therefore, this smoking cessation model should be considered to be implemented in healthcare settings.
Tobacco use remains the world's leading preventable cause of morbidity and mortality, resulting in more than 8 million deaths each year worldwide (1). China, the world's largest tobacco producer and consumer, has more than 350 million smokers (2). More than 1 million people die each year from smoking-related diseases, and about 100,000 people die from secondhand smoke exposure in China (3). Worse still, tobacco-related deaths in China are expected to reach 3 million by 2050 if effective measures are not taken to control tobacco use (4). The tobacco epidemic is a major threat to public health in China.
Smoking cessation is one of the most important measures to reduce harm from cigarettes. The Healthy China 2030 Action Plan requires that the prevalence of adult smoking be decreased to 20% by 2030 (5). However, quitting smoking is a complex and difficult process for smokers due to nicotine dependence. The Global Adult Tobacco Survey, Fact Sheet, China, 2018 showed that the smoking rate among people aged 15 and above in China was 26.6%, of which 50.5% of men and 2.1% of women were current smokers (6). Among smokers, only 16.1% of current smokers planned to or were thinking about quitting in the next 12 months, and 90.1% of smokers who tried to quit in the past 12 months did not use any quitting assistance for at least one quit attempt (6). When smokers quit smoking without help, it was difficult to maintain abstinence in long term (7).
In 1998, the World Health Organization (WHO) officially included tobacco dependence as a chronic and highly recurrent disease in the International Classification of Diseases (ICD-10; code F17.2). Therefore, quitting smoking requires scientific and professional guidance, which can strengthen smokers' confidence and determination to quit and help them relieve withdrawal symptoms. Common smoking cessation methods include clinic consultation, pharmacological therapy, nicotine replacement therapy, behavioral intervention, and multi-component smoking cessation treatment. There is ample evidence that the combination of behavioral interventions and pharmacotherapy could improve the effectiveness of smoking cessation (8). In order to meet the demand for smoking cessation services, China has launched a centrally subsidized local smoking cessation clinic project since 2014, which has supported the creation of 586 smoking cessation clinics nationwide (9). However, 57% of the clinics only provide cessation advice and behavioral support, and the utilization rate of these clinics is poor due to a lack of public awareness of their availability (10).
To promote adequate treatment for tobacco dependence, WHO recommends that each country should take appropriate, comprehensive, and integrated measures including establishing population-level and individual level approaches, considering novel approaches and media, and integrating brief advice into the existing primary healthcare system (11). Therefore, it is imperative to offer smoking cessation services in primary healthcare settings, which could achieve better population coverage at a relatively low cost (12). Implementing a smoking cessation program based in the community could mobilize local resources and improve access to smoking cessation services. Several foreign studies have confirmed the feasibility and short-term effectiveness of involving community health workers in smoking cessation (13–15), while there are inadequate studies on long-term effectiveness.
The cost-effectiveness of smoking cessation interventions is increasingly becoming a primary consideration for the public health sector. Some previous literature has been published reporting the cost-effectiveness of different smoking cessation interventions, such as pharmacotherapy, nicotine replacement therapy, and cell phone intervention (15–17). Also, there are various studies using the Markov simulation model to evaluate the cost-effectiveness of tobacco control campaigns in different countries (18–20). To our knowledge, there is little smoking cessation program based on hospital and community collaboration in China. Few studies have demonstrated the cost-effectiveness of this intervention model, which is a good way to examine both the costs and effects of interventions. Therefore, it is imperative to investigate the cost-effectiveness of interventions within the context of China.
This study aims to perform a cost-effectiveness analysis (CEA) of comprehensive smoking-cessation interventions based in the community and hospitals in China to provide economic evidence for the public health program.
This study is guided by the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement (21). The completed CHEERS checklist is provided in Supplementary File 1.
This project developed a comprehensive tobacco dependence management model based on community and hospital collaboration and conducted a parallel-controlled community intervention trial to evaluate the effectiveness of the model. The intervention program was implemented by our team at the Capital Medical University, the Respiratory Smoking Cessation Clinic of Sino-Japanese Friendship Hospital, and the community health service centers, which were the intervention sites. Community smoking cessation management groups were formed to be responsible for project implementation. Each group included 20~30 participants, 1 physician from the smoking cessation clinic, 1 community family doctor, 1 community manager, 8~10 volunteers selected from the credible people in the community, and 1 psychological counselor. We compared the cost-effectiveness of three smoking cessation intervention strategies: no intervention (NI), pharmacological intervention (PI), and comprehensive intervention (CI) (PI plus online health promotion). PI and CI were conducted based on community and hospital collaboration. The intervention trial lasted for 6 months, and our team followed up with participants to monitor outcomes such as smoking status, drug use, and smoking cessation willingness. Figure 1 shows the specific measures for each intervention at different time points. For details of the intervention, please see Supplementary File 2.
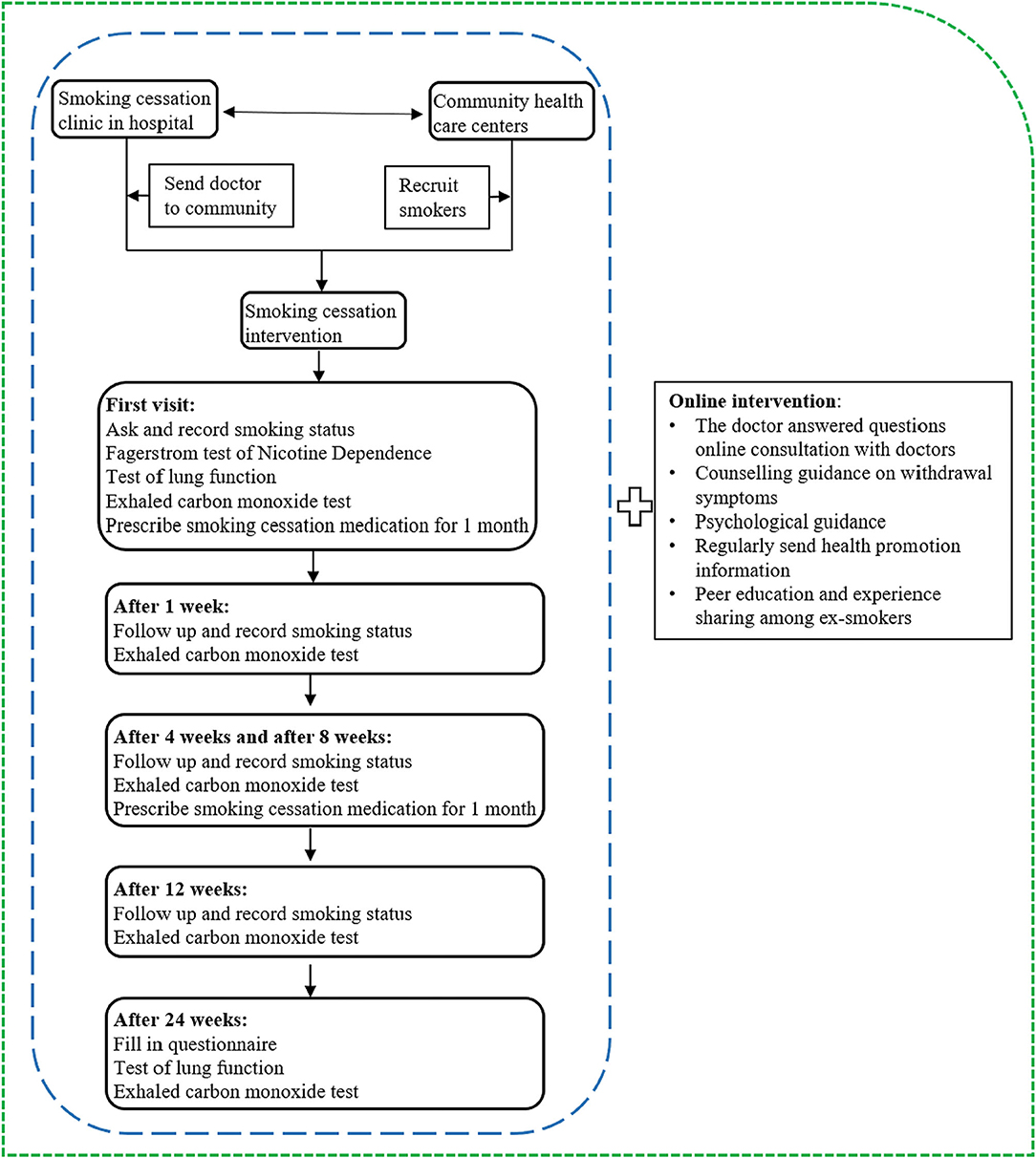
Figure 1. The content of the intervention program. The blue circle and green circle respresent the specific measures of PI and CI, respectively.
This study has been approved by the Medical Ethics Committee of Capital Medical University (Z2019SY007). Written informed consent was obtained from all the participants.
The sample size for this study was calculated by using the corresponding formula of a two-armed parallel control trial as shown here. The α was 0.05, and the test efficiency was 0.9, which means the β was 0.1. Since the smoking cessation rate of daily smokers over 15 years of age in China was 14.4% according to the 2015 China Adult Tobacco Survey Report, p2 was 14.4% which reflected the positive rate of the control group. The p1, the expected positive rate in the test group, was set at 24.4% with the goal of increasing the smoking cessation rate by 10% through intervention. The δ2 is the difference between p1 and p2, which was 0.102. The required sample size was calculated to be 262. To account for dropout of 5%, we aimed to recruit 276 participants to each group, with a total of 582 participants.
In total, eight community health service centers with a stable population and good basic conditions for chronic disease management were selected as the sites to conduct CI. Matching the characteristics of social economy, population health, and medical services of community health service centers in the CI group, 11 centers were selected as sites to conduct PI. In total, 19 community health service centers in Beijing were selected (Figure 2). Community doctors and community managers were responsible for recruiting smokers who were willing to participate in the smoking cessation intervention program.
Inclusion criteria for the participants were current smokers living in the community who (a) had smoked for 6 months or more in their lifetime and had smoked within 30 days prior to the survey, (b) were not currently using other methods to quit smoking, (c) and could communicate fluently and were willing to take part in the follow-up. Smokers were excluded if they (a) had participated in another smoking cessation program, (b) were pregnant or breast feeding, or (c) were suffering from a serious illness that prevented them from being able to participate physically or mentally.
Prior to the intervention, the investigators were trained by team members. At the intervention site, investigators and doctors from the hospital conducted face-to-face questionnaires, carbon monoxide blow tests, and lung function tests on study participants. Based on these test results, the doctor developed specific smoking cessation plans for each participant, including whether to take smoking cessation drugs, daily doses of the drug, etc. In total, 680 tobacco-dependent smokers were enrolled in our project from 19 communities.
We created a state-transition Markov model to compare three smoking–cessation intervention strategies by using TreeAge Pro software. Figure 3 illustrates the various states and the potential transitions between these states. The model constructed in this study included four states: healthy smoker, healthy quitter, ischemic stroke, and death. Smoking is a risk factor for a variety of diseases, including cardiovascular disease which is the main smoking-related cause of death globally. In China, the stroke incidence and particularly the incidence of ischemic stroke was higher than in other countries (22). Smoking is a major risk factor for stroke with 10.8% of strokes in men attributed to smoking (23). Thus, in this study, ischemic stroke was selected to represent smoking-related disease and was included in the model.
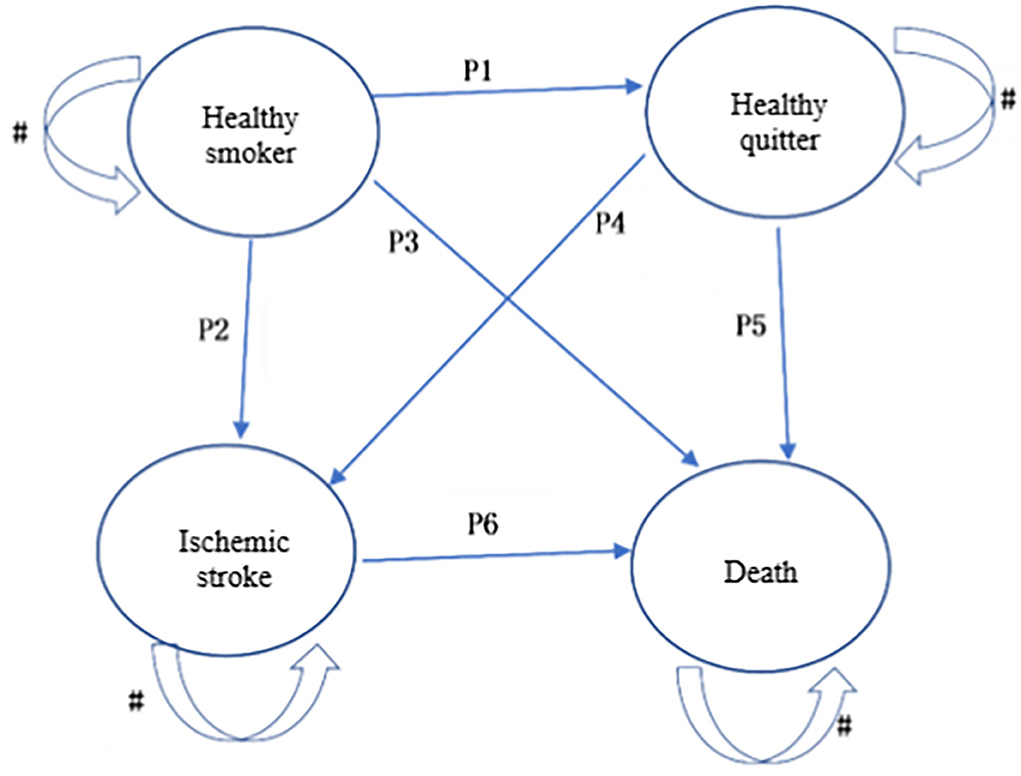
Figure 3. Markov model structure. # indicates that there is a certain probability of remaining within the state.
The base case is 10,000 adult male smokers who were willing to quit smoking. This model, with a time horizon of 20 years, could predict the lifetime costs and quality adjusted life years (QALYs) of different smoking cessation intervention strategies. The model runs on two basic assumptions: (1) a participant can only be in one state in each Markov cycle, and (2) the 'smoker's transition from one state to the next occurs randomly based on probability, regardless of which state the smoker was in before entering the new state. The simulation queue established by this model was 10,000 people with a cycle period of 1 year and a total of 20 cycles. When the time unit of the parameter is inconsistent with the cycle, it is converted to the formula P=(Pt)1/t, where P is the probability of transfer within a cycle. The Markov model framework could be found in Supplementary Figure S1.
Probabilities data were obtained from the Global Study of the Economic Burden of Disease and the results of domestic epidemiological surveys, and related literature studies are shown in Table 1.
The costs of different smoking cessation intervention strategies were calculated using the work decomposition structure (WBS) and the operation cost method to count the input of each group of resources in the community intervention trial. The average cost of hospitalization for ischemic stroke comes from the China Stroke Prevention and Control Report 2019. The cost estimates in this study are divided into average direct costs and average indirect costs. The average direct costs include inspection costs, smoking cessation drug costs, and other material costs. The average indirect costs include medical “personnel's lost work expense,” smoker's lost work expense, and transportation cost. The total costs of the different smoking cessation strategies are shown in Table 1. All the costs were inflated to 2019 using the China Consumer Price Index and converted to US dollars using official exchange rates as of 2019 (US$1 = ¥6.90).
Quality-adjusted life years as a measurement reflecting both health-related quality of life and mortality is recommended by China Guidelines for Pharmacoeconomic Evaluations as the most suitable measure for the economic evaluation of health outcomes. QALYs are equal to time spent in the relevant health states multiplied by an appropriate utility score. In this study, a cross-sectional survey was conducted to identify the utility scores for smokers, in which participants completed EuroQol five-dimensional questionnaires (EQ-5D-5L). The EQ-5D-5L utility scores are shown in Table 1.
We conducted our analysis from a societal perspective in accordance with the China Guidelines for Pharmacoeconomic Evaluations. A hypothetical cohort of base case adult smokers was simulated over a 20-year time horizon with each cycle lasting 1 year. We discounted future costs and future benefits at 3%. Outcome measures were reported in incremental cost-effectiveness ratios (ICERs) with a Cost-Effectiveness Threshold (CET) of 1–3 times GDP per capita in China (10,279.12 ~ 30837.36) (30), which was the most common approach to set CET (31). The intervention strategy would be considered to be “very” cost-effective if ICER was less than GDP per capita, and could still count as cost-effective if the ICER did not exceed 3 times of GDP per capita (32). By using the probabilistic sensitivity analyses, we explored the uncertainty of model parameters, including incidence rate of ischemic stroke, and utility values. A Cost-effectiveness acceptability curve was generated to illustrate the percentage of curves estimated by ICER that were cost-effective at different values of willingness to pay per quit.
Of all the 680 smokers who participated across communities, 283 were randomly assigned to the PI group and 397 to the CI group (Table 2). In the PI group, there were 251 male smokers (88.7%), and most participants had a secondary education level and above (89.7%). In the CI group, 366 participants (92.2%) were male, and about 193 smokers (49.0%) had retired. About two-thirds of participants had at least moderate FTND defined nicotine dependence in both the PI group (62.6%) and CI group (62.9%). Baseline characteristics between the two groups were similar.
Table 3 shows the short-term effects in the CI and PI groups after receiving the smoking cessation intervention. After 1 month, 54 participants in the CI group and 26 in the PI group successfully quit smoking, and the difference between the two groups was not statistically significant (p > 0.05). After 3 months of the intervention, 81 people in the CI group and 38 people in the PI group successfully quit smoking, and the results showed a statistically significant difference in the distribution of intervention effect between the two groups (p < 0.05). After 6 months, the smoking cessation rate of the CI and PI groups was 30.0 and 21.2%, respectively (p < 0.05).
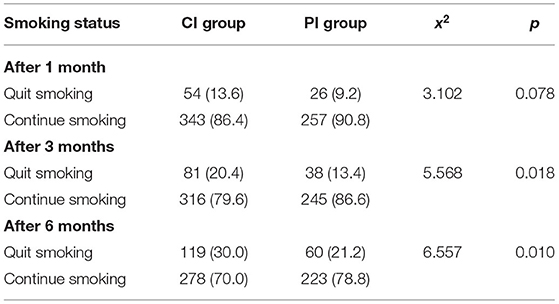
Table 3. Short-term effects in the intervention groups after receiving smoking cessation intervention.
Table 4 shows the cost, QALYs, incremental costs, and the ICER of different intervention strategies. Compared with the NI group, the intervention strategy of the PI group and the CI group were both found to be very cost-effective with ICER of $535.62/QALY and $366.19/QALY, respectively, which were well below our CET ($10279.12/QALY).
In this study, the probability sensitivity of incidence rate and utility indicators including age-standardized incidence rate of ischemic stroke, the utility of smoker, quitter, and patients with ischemic stroke, respectively, in Table 1 were analyzed. Sensitivity analysis results suggest that when the willingness to pay threshold was >$0/QALY, the CI strategy was always the most cost-effective intervention plan, while the PI strategy was considered to be more costly and less effective (Figure 4).
To our knowledge, this study is the first to compare the relative costs and outcomes of different smoking cessation intervention strategies based on community and hospital collaboration, in China. Our findings indicate that compared with NI, the CI program based on hospital and community collaboration is cost-effective. Through sensitivity analysis simulating the effects of adjusting for a range of bias parameters, we found that our model has good stability statistically. These findings should inform the formulation of effective tobacco control policies in China.
In 2013, the WHO proposed that primary healthcare should play an important role in tobacco control (33). According to WHO estimates, the possible effects of integrating smoking cessation interventions for all smokers into basic healthcare services include: more than 80% of all smokers would be served each year, 40% of smokers would be encouraged to try to quit, and 2~3% of smokers would quit smoking successfully. This indicates that providing smoking cessation services in primary healthcare is effective for tobacco control. In the UK, smoking cessation interventions and clinical treatment referrals for smoking cessation by community GPs were introduced for specific groups, in 2002 (34). In the United States, Australia, and other countries, community-oriented tobacco control interventions have also been carried out for many years (13, 35, 36). Unlike foreign countries that rely on community pharmacy personnel to provide smoking cessation services (37), family doctors and physicians from smoking cessation clinics were responsible to provide services in this study, due to the family doctor contract services (FDCSs) in China. Based on institutional characteristics in China, this approach could not only save costs but also improve the effects of smoking cessation. In recent years, the chronic disease management model of a hospital–community linkage has been applied to the intervention management of many chronic diseases and has achieved good management results (38). However, community health service centers, as the provider of primary healthcare services, have delivered little in terms of services for tobacco control in China.
This study performed a cost-effectiveness analysis alongside a randomized controlled quasi-experiment involving the community and hospital. From the societal perspective, our findings suggest that the CI program based on community and hospital collaboration is cost saving, which means that the cost of the intervention program is lower compared with the cost of smoking-related diseases. This indicates that health policymakers should consider putting part of the budget allocations for tobacco control into community healthcare centers. In addition, this study confirmed the significance of online health promotion intervention in smoking cessation, which is consistent with previous findings (39). Paying attention to the smokers' quitting needs and obstacles they encountered at different stages and providing the social support they need is critical to increasing the smoking cessation rate (40). Online health promotion services can provide smokers with the information and emotional support they need timely and conveniently, and thus, may be considered a great way to assist smoking cessation.
Our findings indicate that the smoking cessation model based on hospital and community collaboration may be feasible and acceptable for tobacco control. In view of the prevalence of tobacco use, in order to better control smoking, it is recommended to promote hospital-community multisectoral cooperation with the tobacco dependence management model. First, we should establish a multi-sectoral cooperative smoking cessation support system with the community as the place and the hospital as the support system. Training is required to strengthen the knowledge and skills of relevant community medical personnel. Also, we should establish shared online resources containing relevant health promotion materials by using the Internet, WeChat group, which is one of the most popular social media in China, and other new media. This resource would support follow-up management, enrich the community smoking cessation intervention system, and strengthen the implementation of relevant policies to promote the sustainable development of hospital–community smoking cessation interventions.
Several limitations of our study should be carefully considered. First, in the community intervention trial, the investigation of re-smoking after smoking cessation was not studied, so the effect of smoking cessation and relapse on the smoking cessation population was not considered within the model. This may have magnified the effect of quitting smoking, resulting in a certain degree of bias. In addition, this study only selected ischemic stroke to predict smoking-related diseases in the model, and only accounted for the direct treatment cost of ischemic stroke. Smoking is a strong risk factor for many diseases. Therefore, other diseases should also be considered in states prediction for further studies and simulations. The model in this study is based on adult smoking men, and the model prediction is not specific to different age groups. Since there may be some differences in the effects and long-term benefits of smoking cessation in different age groups, further research is required to investigate this.
In summary, the CI for smoking cessation based on hospital and community collaboration in China has been shown to be very cost-effective. This smoking cessation model should be further implemented and evaluated to more strongly establish the potential benefit to public health in China.
This study has been registered on the official website of the China Clinical Trial Registration Centre (ChiCTR1900024991).
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of Capital Medical University. The patients/participants provided their written informed consent to participate in this study.
TQ: conceptualization, methodology, formal analysis, writing—original draft, and writing—review and editing. QJ: conceptualization, methodology, data curation, and formal analysis. XL: conceptualization, methodology, investigation, resources, supervision, project administration, and writing—review and editing. XB: investigation, project administration, and data acquisition. KQ: conceptualization, investigation, and data curation. MG: investigation and writing—review and editing. YW: investigation, resources, and project administration. All authors contributed to the article and approved the submitted version.
This research was supported by the Foundation of the National Key R&D Program of China (2017YFC1309404).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors thank all the local participants for their support and hard work in launching and implementing this study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.853438/full#supplementary-material
1. (WHO) WHO. Tobacco Fact Sheet Information. (2020). Available online at: https://wwwwhoint/news-room/fact-sheets/detail/tobacco (accessed March 22, 2020).
2. Yang G, Fan L, Tan J, Qi G, Zhang Y, Samet JM, et al. Smoking in China: findings of the 1996 National Prevalence Survey. JAMA. (1999) 282:1247–53. doi: 10.1001/jama.282.13.1247
3. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
4. Chen Z, Peto R, Zhou M, Iona A, Smith M, Yang L, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. (2015) 386:1447–56. doi: 10.1016/S0140-6736(15)00340-2
5. China SCotPsRo. Opinion on Implementing Healthy China 2030 Initiative. State Council Document No 13. Beijing: Government of China (2019).
6. WHO. Global Adult Tobacco Survey Fact Sheet. (2018). Available online at: https://wwwwhoint/docs/default-source/wpro—documents/countries/china/2018-gats-china-factsheet-cn-enpdf?sfvrsn=3f4e2da9_2 (accessed March 22, 2021).
7. Cooper J, Borland R, Yong H-H, McNeill A, Murray RL, O'Connor RJ, et al. To what extent do smokers make spontaneous quit attempts and what are the implications for smoking cessation maintenance? Findings from the International Tobacco Control Four country survey. Nicotine Tob Res. (2010) 12(Suppl. 1):S51–7. doi: 10.1093/ntr/ntq052
8. Sealock T, Sharma S. Smoking cessation. In: StatPearls. Treasure Island, FL: StatPearls Publishing (2022).
9. Xie L, Xiao L, Kuang D, Jiang Y, Yang Y. Analysis of the factors influencing the smoking cessation rate during the follow-up of the first visit of the smoking cessation clinic patients of the central supplement project in 2015–2018. Chin J Epidemiol. (2020) 41:890–5.
10. Lin H, Xiao D, Liu Z, Shi Q, Hajek P, Wang C. National survey of smoking cessation provision in China. Tob Induc Dis. (2019) 17:25. doi: 10.18332/tid/104726
11. World Health Organization. WHO Framework Convention on Tobacco Control. Geneva: World Health Organization (2003).
12. Piné-Abata H, McNeill A, Murray R, Bitton A, Rigotti N, Raw M. A survey of tobacco dependence treatment services in 121 countries. Addiction. (2013) 108:1476–84. doi: 10.1111/add.12172
13. Bryant J, Bonevski B, Paul C, Hull P, O'Brien J. Implementing a smoking cessation program in social and community service organisations: a feasibility and acceptability trial. Drug Alcohol Rev. (2012) 31:678–84. doi: 10.1111/j.1465-3362.2011.00391.x
14. Zulkiply SH, Ramli LF, Fisal ZAM, Tabassum B, Abdul Manaf R. Effectiveness of community health workers involvement in smoking cessation programme: a systematic review. PLoS ONE. (2020) 15:e0242691. doi: 10.1371/journal.pone.0242691
15. Thavorn K, Chaiyakunapruk N. A cost-effectiveness analysis of a community pharmacist-based smoking cessation programme in Thailand. Tob Control. (2008) 17:177–82. doi: 10.1136/tc.2007.022368
16. Zhuang T, Ku S, Shapiro LM, Hu SS, Cabell A, Kamal RN. A cost-effectiveness analysis of smoking-cessation interventions prior to posterolateral lumbar fusion. J Bone Joint Surg Am Vol. (2020) 102:2032–42. doi: 10.2106/JBJS.20.00393
17. Daly AT, Deshmukh AA, Vidrine DJ, Prokhorov AV, Frank SG, Tahay PD, et al. Cost-effectiveness analysis of smoking cessation interventions using cell phones in a low-income population. Tob Control. (2019) 28:88–94. doi: 10.1136/tobaccocontrol-2017-054229
18. Hurley SF, Matthews JP. Cost-effectiveness of the Australian national tobacco campaign. Tob Control. (2008) 17:379–84. doi: 10.1136/tc.2008.025213
19. Murukutla N, Yan H, Wang S, Negi NS, Kotov A, Mullin S, et al. Cost-effectiveness of a smokeless tobacco control mass media campaign in India. Tob Control. (2018) 27:547–51. doi: 10.1136/tobaccocontrol-2016-053564
20. Tosanguan J, Chaiyakunapruk N. Cost-effectiveness analysis of clinical smoking cessation interventions in Thailand. Addiction. (2016) 111:340–50. doi: 10.1111/add.13166
21. Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ. (2013) 346:f1049. doi: 10.1136/bmj.f1049
22. Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, Incidence, and Mortality of Stroke in China: results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation. (2017) 135:759–771. doi: 10.1161/CIRCULATIONAHA.116.025250
23. Gu D, Kelly TN, Wu X, Chen J, Samet JM, Huang J, et al. Mortality attributable to smoking in China. N Engl J Med. (2009) 360:150–9. doi: 10.1056/NEJMsa0802902
24. Global Burden of Diseases. Injuries and Risk Factors Study (GBD). Available online at: https://www.thelancet.com/gbd (accessed November 21, 2021).
25. Rücker V, Heuschmann PU, O'Flaherty M, Weingärtner M, Hess M, Sedlak C, et al. Twenty-year time trends in long-term case-fatality and recurrence rates after ischemic stroke stratified by etiology. Stroke. (2020) 51:2778–85. doi: 10.1161/STROKEAHA.120.029972
26. Council NH. 2019 China Health Statistics Yearbook. Beijing: China Concord Medical University Press (2019).
28. Wang YL, Pan YS, Zhao XQ, Wang D, Johnston SC, Liu LP, et al. Recurrent stroke was associated with poor quality of life in patients with transient ischemic attack or minor stroke: finding from the CHANCE trial. CNS Neurosci Ther. (2014) 20:1029–35. doi: 10.1111/cns.12329
29. Pan Y, Cai X, Huo X, Zhao X, Liu L, Wang Y, et al. Cost-effectiveness of mechanical thrombectomy within 6 hours of acute ischaemic stroke in China. BMJ Open. (2018) 8:e018951. doi: 10.1136/bmjopen-2017-018951
30. China Statistical Yearbook. (2020). Available online at: http://www.stats.gov.cn/tjsj/ndsj/2020/indexch.htm (accessed October 12, 2020).
31. Leech AA, Kim DD, Cohen JT, Neumann PJ. Use and misuse of cost-effectiveness analysis thresholds in low- and middle-income countries: trends in cost-per-DALY studies. Value Health. (2018) 21:759–61. doi: 10.1016/j.jval.2017.12.016
32. World Health Organization Commission on Macroeconomics and Health: Macroeconomics and Health: Investing in Health for Economic Development. Geneva: World Health Organization (2001).
33. World Health Organization. Strengthening Health Systems for Treating Tobacco Dependence in Primary Care. France: World Health Organization (2013). Available online at: https://apps.who.int/iris/bitstream/handle/10665/84388/9789241505413_eng_Part-III_service_providers.pdf?sequence=4 (accessed February 16, 2021).
34. Gillam S, Schamroth A. The community-oriented primary care experience in the United kingdom. Am J Public Health. (2002) 92:1721–5. doi: 10.2105/AJPH.92.11.1721
35. Dent LA, Harris KJ, Noonan CW. Randomized trial assessing the effectiveness of a pharmacist-delivered program for smoking cessation. Ann Pharmacother. (2009) 43:194–201. doi: 10.1345/aph.1L556
36. Asvat Y, Cao D, Africk JJ, Matthews A, King A. Feasibility and effectiveness of a community-based smoking cessation intervention in a racially diverse, urban smoker cohort. Am J Public Health. (2014) 104(Suppl. 4):S620–7. doi: 10.2105/AJPH.2014.302097
37. Carson-Chahhoud KV, Livingstone-Banks J, Sharrad KJ, Kopsaftis Z, Brinn MP, To-A-Nan R, et al. Community pharmacy personnel interventions for smoking cessation. Cochrane Database Syst Rev. (2019) 2019:CD003698. doi: 10.1002/14651858.CD003698.pub3
38. Hu H, Liang H, Wang H. Longitudinal study of the earliest pilot of tiered healthcare system reforms in China: will the new type of chronic disease management be effective? Soc Sci Med. (2021) 285:114284. doi: 10.1016/j.socscimed.2021.114284
39. Qian Y, Gui W, Ma F, Dong Q. Exploring features of social support in a Chinese online smoking cessation community: a multidimensional content analysis of user interaction data. Health Informatics J. (2021) 27:14604582211021472. doi: 10.1177/14604582211021472
Keywords: cost-effectiveness, smoking cessation, pharmacological intervention, online health promotion, community health centers
Citation: Qin T, Jin Q, Li X, Bai X, Qiao K, Gu M and Wang Y (2022) A Cost-Effectiveness Analysis of Comprehensive Smoking-Cessation Interventions Based on the Community and Hospital Collaboration. Front. Public Health 10:853438. doi: 10.3389/fpubh.2022.853438
Received: 13 January 2022; Accepted: 17 June 2022;
Published: 22 July 2022.
Edited by:
Kyriakos Souliotis, University of Peloponnese, GreeceReviewed by:
Chiranjivi Adhikari, Indian Institute of Public Health Gandhinagar (IIPHG), IndiaCopyright © 2022 Qin, Jin, Li, Bai, Qiao, Gu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xingming Li, eGluZ21pbmdsaUBjY211LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.