- 1Centre for Health Management and Policy Research, School of Public Health, Cheeloo College of Medicine (Key Lab of Health Economics and Policy, National Health Commission), Shandong University, Jinan, China
- 2Affiliated Hospital of Integrated Traditional Chinese and Western Medicine, Nanjing University of Chinese Medicine, Nanjing, China
- 3Department of Public Health Sciences, University of Virginia, Charlottesville, VA, United States
- 4Center for Cancer Control and Policy Research, School of Public Health, Shandong University, Jinan, China
- 5Shandong Academy of Medical Sciences, Shandong Cancer Hospital Affiliated to Shandong University, Jinan, China
- 6University of Virginia Cancer Center, Charlottesville, VA, United States
Objective: This study aimed to examine the urban-rural disparities and associated factors of health care utilization among cancer patients in China.
Methods: This study used the data collected from a cross-sectional survey conducted in China. A total of 1,570 cancer survivors from three urban districts and five rural counties were selected by using a multistage stratified random sampling method. We measured health care utilization with the way of cancer diagnosis, the number of hospitals visited, and receiving alternative therapies. Chi-square test was used to examine the differences between urban and rural cancer patients. Binary logistic regression analysis was performed to explore the determinants of health care utilization.
Results: Among 1,570 participants, 84.1% were diagnosed with cancer after developing symptoms, 55.6% had visited two and above hospitals, and 5.7% had received alternative therapies. Compared with urban cancer patients, rural ones were more likely to be diagnosed with cancer after developing symptoms (χ2 = 40.04, p < 0.001), while they were less likely to visit more than one hospital (χ2 = 27.14, p < 0.001). Residence area (urban/rural), health insurance type, household income, age at diagnosis, tumor site, stage of tumor, and survival years were significantly associated with health care utilization of cancer patients (p < 0.01).
Conclusions: Health care utilization was suboptimal among cancers patients in China. Rural cancer patients had less health care utilization including screenings and treatments than urban ones. Policymakers should implement specific strategies to ensure equitable utilization of cancer care. More attention should be paid to the disadvantaged groups and rural cancer patients. Prioritizing health resources allocation is needed to prevent, screen, and treat cancers in rural areas.
Introduction
Globalcancer statistics estimated 18.1 million new cancer cases around the world in 2018, and out of these cases, nearly one-half occurred in Asia, 23.4% occurred in Europe, and 21% occurred in America. Thereinto, ~24% of cancer cases occurred in China (1). With the increasing incidence of cancer, the population burden of cancer is being more and more significant in China. Southwest China has the highest cancer incidence rate, followed by North China and Northwest China, and Central China has the lowest incidence rate (2). Cancer has become the leading cause of death (126.9 deaths per 100,000 persons) and a major economic burden in China (2, 3). In 2011, five types of most prevalent cancers (lung, stomach, colorectal, female breast, and esophageal cancers) accounted for 56% of the cancer burden in China (4). Improved detection methods and more effective therapies for cancer have been developed and applied in clinical practice, which has also led to the increasing number of cancer survivors (5, 6). Thus, cancer has become one of the most significant public health issues in China (7).
Timely and effective utilization of cancer care including screening, diagnosis, and treatment, is essential to the health outcome of cancer patients. It has been shown that medical detection and effective treatment are significantly associated with improved experiences and outcome with cancer survivorship (8, 9). Early medical screening can detect some types of cancers (breast, colorectal, and so on) before the symptoms start to show (10, 11). Even after initial treatment has been completed, cancer survivors may still need a spectrum of long-term following treatment and rehabilitation care, including alternative therapies (12). Cancer patients require a coordinated and multidisciplinary approach to treatment and control their illness (13), so they may need to visit more than one hospital for cancer care utilization.
Rural cancer survivors were considered as having higher risk for decrements in health and well-being due to decreased access to health care, specialty services, and support resources in the United States (14). Substantial urban-rural disparities in the likelihood of financial hardship and non-adherence to surveillance colonoscopy existed in New Mexico (15). In China, cancer patients living in rural areas have more restricted access to health care due to limited cancer care resources and shortage of qualified providers (16). Moreover, people living in rural China are also more likely to be diagnosed at more advanced stages of cancers (17). There is noticeable urban-rural inequality in access to health care and health resources in China. Urban residents are likely to have more healthcare utilization, more healthcare resources, more access to government sponsored public programs/healthcare services and less risk to suffer from diseases (18). Rural populations also have more restricted access to health care than urban residents due to low funds for health insurance scheme (19).
Health care utilization is the individuals' behaviors of choosing from a range of services and optional health care providers to meet their health demands (20). Health care utilization and its patterns are reflected by health care seeking behaviors (21, 22). Thus, health care can be well provided based on related information in terms of health care utilization and their associated factors (23). Many studies have used Andersen's behavioral models to examine the determinants of health care utilization, including predisposing factors, enabling factors, and need factors (23, 24). Existed literature has showed that health care utilization were affected by determinants at multiple levels, including individual and household factors (income, knowledge, education, age, gender, insurance coverage, distance to health facilities) (21, 25), as well as characteristics of health care system (availability, affordability and accessibility of drugs and healthcare services) (26). Furthermore, it has been revealed that urban-rural regional difference was also one important predictor of health care utilization (27).
Numerous studies have examined the incidence and mortality rates of cancer and their determining factors (2, 28). Also, many studies have highlighted issues related to cancer treatment, the cost of treatment, economic burden of cancer, and the lasting effects of treatment (29–31). Nevertheless, few studies have focused on cancer care utilization and its associated factors, especially among cancer survivors in China. Reliable information on patterns and determining factors of health care utilization is required to provide further insight for policy makers to take measures for cancer control and reduce the heavy burdens of cancers in China. Therefore, this study aimed to examine the urban-rural disparities and associated factors of health care utilization among cancer patients in China.
Materials and Methods
Data and Sample
This study used the data collected from a cross-sectional survey conducted from March 2015 to March 2016 in Shandong province of China, which used a modified questionnaire referred to the Cancer Supplement of the Medical Expenditure Panel Survey (32). A multistage stratified random sampling method was used in this survey. In the first stage, three urban districts and five rural counties were selected based on demographic context and socioeconomic development. The sample was stratified by rural vs. urban status. Counties and urban districts are at the same level in the Chinese administrative division system (32).
The survey selected patients with cancer identified in the cancer registry system as participants. The inclusion criteria of eligible participants were: (1) diagnosed with lung, stomach, colorectal, or female breast cancers between 2011 and 2013; (2) at least 18 years old at the time of their cancer diagnosis; and (3) having willingness to participate in the survey. Those patients were excluded if they were diagnosed with multiple cancers (33). In each county or district, about 200 eligible cancer patients were randomly chosen to complete the questionnaire by face-to-face interview. Finally, the survey assigned 1,600 cancer cases to interviewers, while a total of 1,570 cancer survivors were included in the final analysis of this study.
Variables and Measurement
We measured health care utilization with the way of cancer diagnosis, the number of hospitals visited, and receiving alternative therapies. The three dependent variables were selected based on previous literatures and the profile of health care utilization among cancer patients in Chinese community. The way of cancer diagnosis can help us to provide evidence on the status of early detection of cancer. The number of hospitals visited can help us to understand the twists and turns during the cancer patients' diagnoses and treatments. The variable of receiving alternative therapies is lack of analysis in the majority of literatures, but alternative therapies are helpful for rehabilitation of cancer patients. The way of cancer diagnosis was measured based on the question: “How was your cancer diagnosed,” with answers (1, health checkup; 2, after developing symptom; 3, by testing for other illness; 4, cancer screening). The number of hospitals visited was the total number of visiting hospitals for the participant's treatment since diagnosed with cancer. Receiving alternative therapies was measured based on the question: “Have you tried alternative therapies besides hospital medical treatment.” To explore the influencing factors of cancer care utilization using logistic regression models, those dependent variables were all collapsed into binary variables, including the way of cancer diagnosis (1, after developing symptom; 0, others), the number of hospitals visited (1, more than one hospital; 0, one hospital), receiving alternative therapies (1, yes; 0, no).
According to the Andersen behavior model, the determinants influencing health care utilization consisted of predisposing factors, enabling factors and need factors (34). Predisposing factors included gender (1, female; 2, male), age at diagnosis (1, <50 year; 2, 50–59 year; 3, 60–69 year; 4, ≥70 year), educational level (1, < primary school; 2, primary school; 3, middle school; 4, ≥high school), marital status (1, married; 2, single/divorced/widowed), and employment status (1, employee; 2, farmer; 3, retired; 4, unemployed). Enabling factors included residence area (1, urban community; 2, rural village), health insurance type (1, UEBMI = Urban Employee Basic Medical Insurance; 2, URBMI = Urban Resident Basic Medical Insurance; 3, NCMS=New Cooperative Medical Scheme; 4, other), and annual household income (CNY) (1, <5000; 2, 5,000–20,000; 3, 20,000–50,000; 4, ≥50,000). Need variables included tumor site (1, breast; 2, lung; 3, colorectal; 4, stomach), cancer stage (1, early; 2, medium; 3, later; 4, unknown), and survival time (years) (1, <1 year; 2, 1–2 year; 3, 2–3 year; 4, ≥3year).
Statistical Analysis
The hypotheses to be tested in this study are that there are significant disparities of cancer care utilizations (in terms of way of cancer diagnosis, number of hospitals visited and receiving alternative therapies) between urban rural areas, and many associated factors influencing health care utilization among cancer patients in China. Firstly, descriptive analysis was conducted to summarize basic characteristics and clinical characteristics of the respondents. The frequency and percentage were calculated and presented for categorical variables. Chi-square (χ2) test was used to examine the differences of proportions between urban and rural areas. Secondly, we used descriptive analysis to examine the frequency and percentage of health care utilization among the selected respondents. Chi-square (χ2) test was used to examine the differences of proportions between urban and rural cancer patients. Thirdly, binary logistic regression analysis was performed to explore the determinants of health care utilization (being diagnosed after developing symptom, visiting more than one hospital, receiving alternative therapies). We presented Odds Ratios (ORs) and their 95% Confidence Intervals (CIs). All statistical analyses were conducted using STATA 15. The significance level for statistics was set at p < 0.05 and p < 0.01.
Results
Basic Characteristics of The Participants and Urban-Rural Disparities
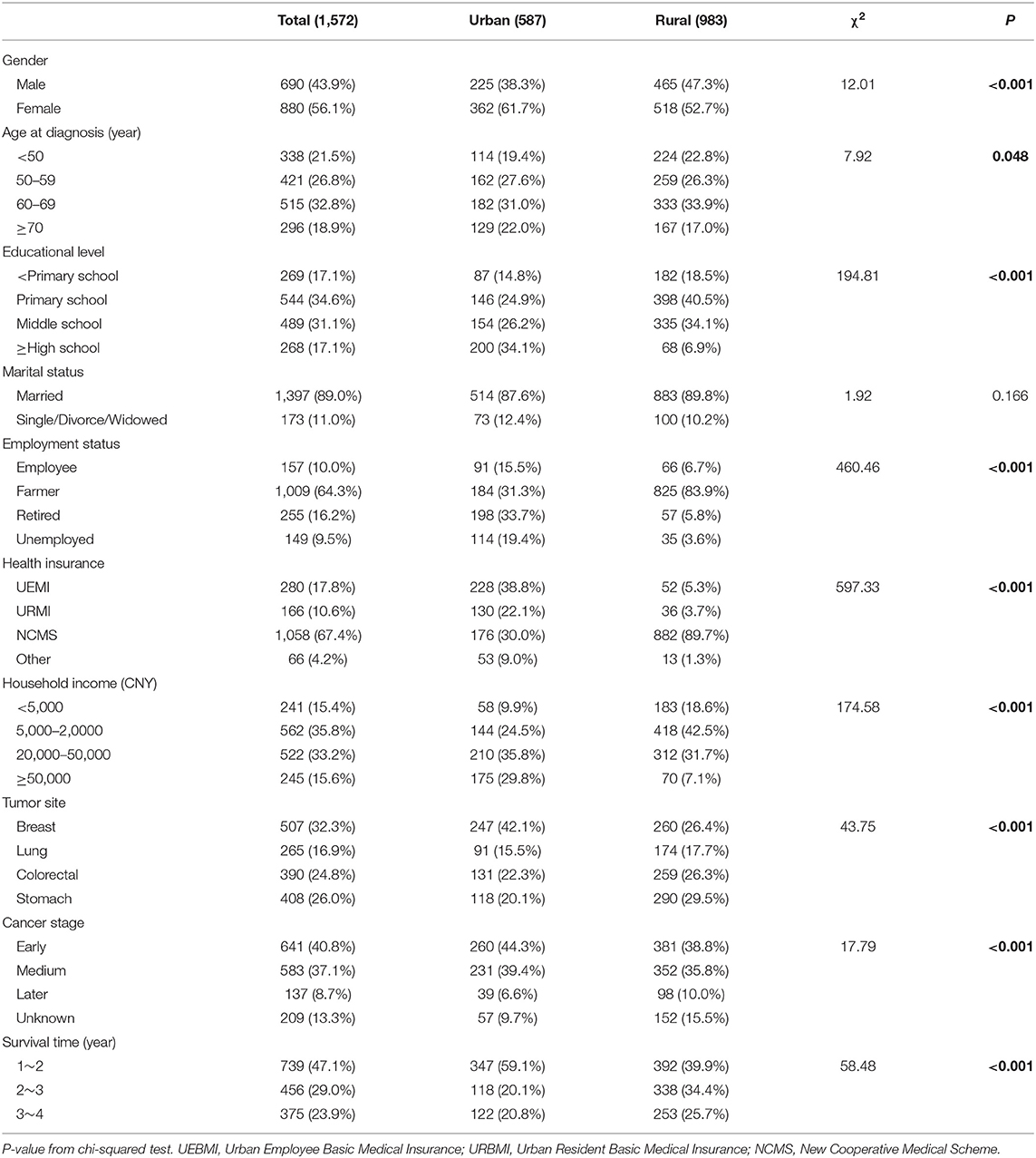
Basic characteristics were listed for the overall sample and by urban and rural participants (Table 1). Among 1,570 cancer patients, 983 (62.6%) were from rural areas. The majorities of them were females (56.1%), more than 50 years at diagnosis (78.5%), married (89.0%), farmers (64.3%), and covered by NCMS (67.4%). Only 17.1% of the participants had the education level of high school and above. More than half of the respondents had a low annual household income of <20,000 CNY. Cancer sites of the patients included breast (32.3%), stomach (26.0%), colorectal (24.8%), and lung (16.9%). More than a half of them had lived more than 2 years since their cancer diagnosis. Compared with urban cancer patients, rural ones were more likely to have low educational level (χ2 = 194.81, p < 0.001) and low household income (χ2 = 174.58, p < 0.001), to be at later cancer stage (χ2 = 17.79, p < 0.001), and to survive more than 2 years (χ2 = 58.48, p < 0.001). There were also statistical differences of gender, age at diagnosis, employment status and tumor site between urban and rural participants (all p < 0.05).
The Urban-Rural Disparity of Health Care Seeking Behaviors
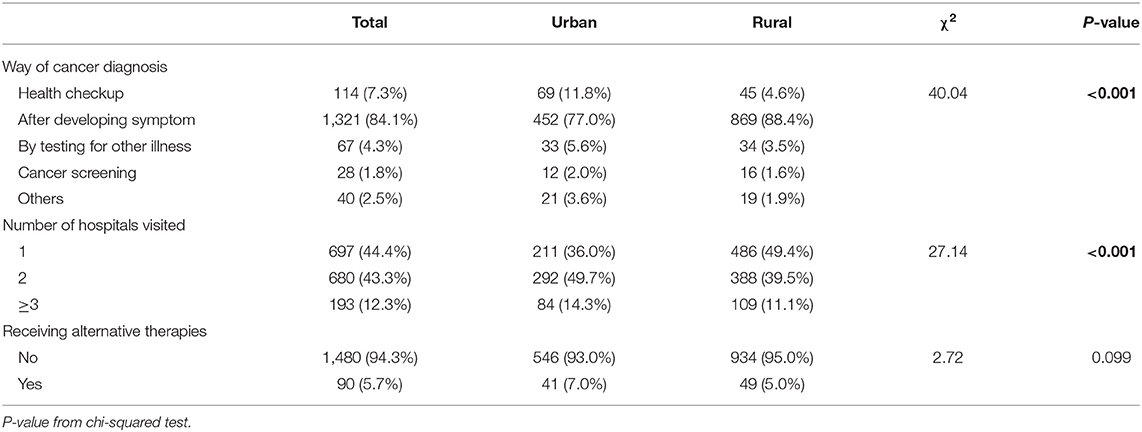
Table 2 presented the urban-rural disparities of health care utilization of the participants. Among 1,570 cancer patients, 84.1% were diagnosed with cancer after developing symptoms. Approximately 43.3% of the participants had visited two hospitals for treatments, while 12.3% had visited three and above hospitals. Only 5.7% of them had received alternative therapies for cancer. Compared with urban cancer patients, rural ones were more likely to be diagnosed with cancer after developing symptom (χ2 = 40.04, p < 0.001), while were less likely to visit more than one hospital (χ2 = 27.14, p < 0.001).
Determinants of Health Care Utilization by Logistic Regression Models
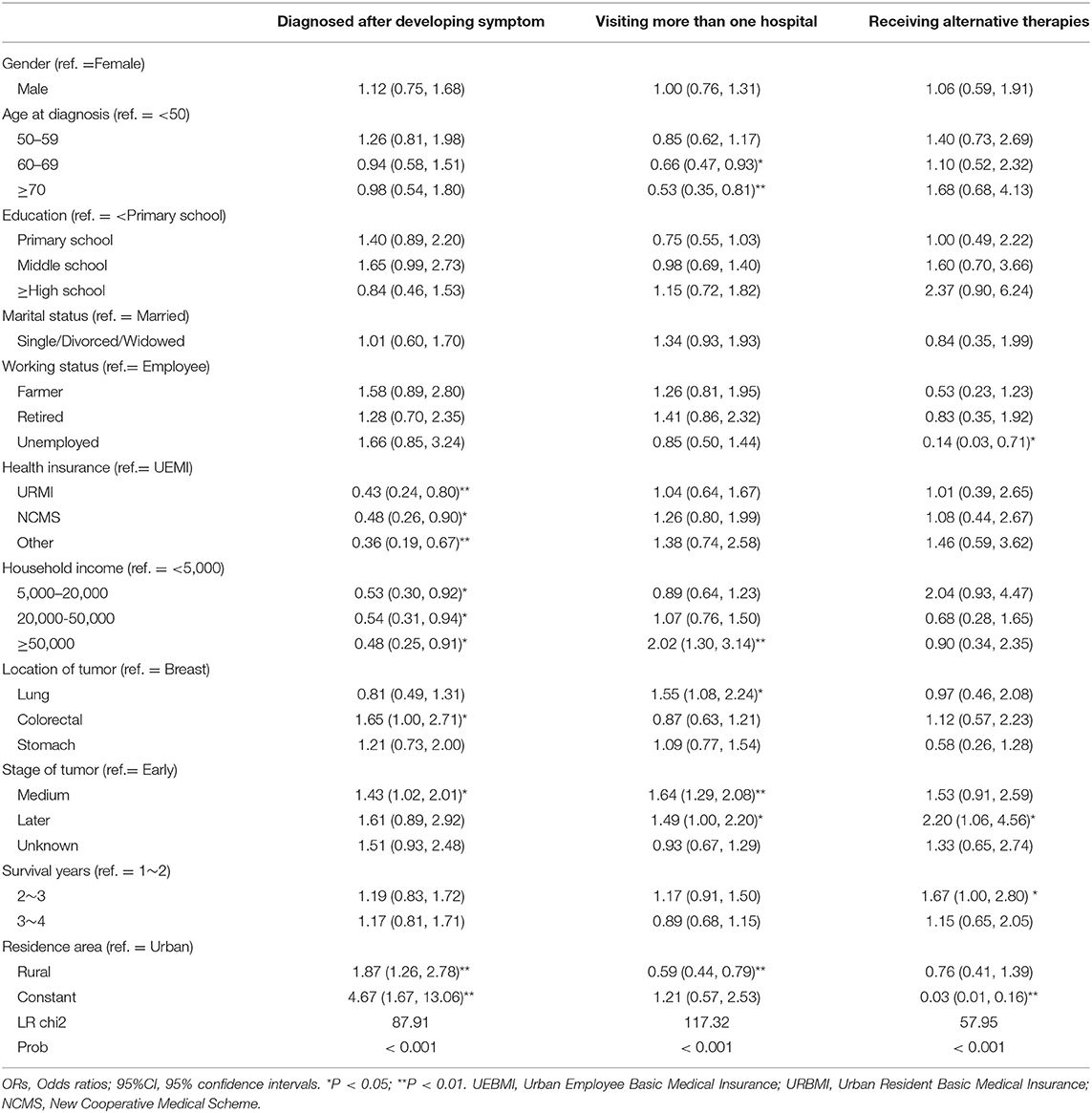
Table 3 displayed the determinants of health care utilization by binary logistic regression analyses. Older cancer patients were less likely to visit more than one hospital (OR = 0.66, p < 0.05; OR = 0.53, p < 0.01). Compared with cancer patients having UEMI, those having URMI or NCMS were less likely to be diagnosed with cancer after developing symptoms (OR = 0.43, p < 0.01; OR = 0.48, p < 0.05). Cancer patients having higher household income were less likely to be diagnosed with cancer after developing symptoms (OR = 0.53, p < 0.05; OR = 0.54, p < 0.05; OR = 0.48, p < 0.05), while were more likely to visit more than one hospitals (OR = 2.02, p < 0.01). Compared with urban cancer patients, rural ones were more likely to be diagnosed with cancer after developing symptom (OR = 1.87, p < 0.01), but were less likely to visit two and above hospitals (OR = 0.59, p < 0.01).
Compared with breast cancer patients, lung cancer patients were more likely to visit more than one hospitals (OR = 1.55, p < 0.05); colorectal cancer patients were more likely to be diagnosed with cancer after developing symptoms (OR = 1.65, p < 0.05). Compared with cancer patients at early stage, those at medium stage were more likely to be diagnosed with cancer after developing symptoms (OR = 1.43, p < 0.05), to visit more than one hospitals (OR = 1.64, p < 0.01); and those at later stage, were more likely to visit more than one hospitals (OR = 1.49, p < 0.05) and to receive alternative therapies (OR = 2.20, p < 0.05). Compared with cancer patients surviving 1~2 years, those surviving 2~3 years were more likely to receive alternative therapies (OR = 1.67, p < 0.05).
Discussion
This is the first study to provide a snapshot regarding the urban-rural disparity and determining factors of health care utilization among cancer patients in China. Information on the utilization of health care is essential to reform health policies based on the demands and influencing factors. The findings in this study revealed that, the majority of cancer patients were diagnosed after developing symptoms, and more than a half of them visited two and above hospitals for cancer treatments, while only a few of them received alternative therapies for cancer. Comparatively speaking, rural cancer patients had less health care utilization than urban ones. Health care utilization of cancer patients were mainly determined by both socioeconomic characteristics (health insurance types, household income) and clinical characteristics (age at diagnosis, tumor site, stage of tumor, survival years).
In the present study, 84.1% of the participants reported that they were diagnosed with cancer patients after developing symptoms, and only 13.4% of cancer patients were detected via health checkups, by testing for other illness, or tumor screening. Some reasons might explain this phenomenon: firstly, many of the respondents may have no adequate knowledge about cancer risk factors and symptoms. Cancer patients could not seek timely diagnoses at the specialized health institutions if they had no appropriate interpretation of early symptoms (35). Secondly, health checkups and cancer screening services have not been covered by social health insurance schemes for the general population in China (32), although several big public health programs have been implemented among high risk population. Therefore, promoting diagnoses at early stage is still a big challenge in China. On one hand, there is a big need of health education interventions to increase the cancer knowledge and diagnostic acumen of both healthcare professionals and high-risk population. On the other hand, if the benefit packages of social health insurance schemes can be expanded to cover some major cancer screening services, more cancer cases will be timely diagnosed and treated to reduce the incidence of cancer at advanced stages.
This study showed that 55.6% of participants had visited two or more hospitals for cancer treatments. After the detection of primary cancer signals, the patients should be referred to the specialized cancer facilities for further diagnosis and treatment. However, they often postpone health care utilization and miss appointments for their treatments due to lack of money or other reasons. Social health insurance should play a greater role in reducing out-of-pocket expenditure on healthcare services for cancer patients. Cancer patients usually use health care in specialized cancer treatment facilities. Specialized cancer treatment facilities that are closer to the patients would facilitate health care utilization and adherence to treatment regimens (35). Ongoing efforts should be taken to integrate cancer care between oncology and primary care settings. The study also found that only a few of them had received alternative therapies for cancer. Models for the integration of care for cancer survivors, including self-management, wellness and healthy lifestyle promotion, and cancer rehabilitation, should be developed and applied (6).
The findings indicated that there were differences in health care utilization between urban and rural cancer patients. Rural cancer patients were more likely to be diagnosed with cancer after developing symptoms and less likely to visit two or more hospitals than urban ones. This discrepancy is mainly because there are obvious disparities in healthcare resources including infrastructure and human resource between rural and urban areas (18). It was reported that in 2015, the number of health technicians and hospital beds per thousand persons in urban areas was nearly 2.62 times and 2.23 times more than those in rural areas in China, respectively (36). Therefore, patients in rural areas may have less access to specialist medical care, and this should be an important consideration when defining future healthcare investment and policy (37). It is vital to reduce the disparity of healthcare resources between rural and urban areas by improving the capacity of rural healthcare institutions in China (18). During the study period, rural residents were mostly insured by the New Rural Cooperative Medical System, which had less coverage and higher coinsurance rates than the insurance that covered urban employees and residents (19).
Furthermore, the results suggested that health care utilization of cancer patients were influenced by both socioeconomic characteristics and clinical characteristics. Consistent with previous studies, health care utilization were influenced by health insurance and household income (21, 38). Cancer survivors may be at greatest risks for financial hardship due to the high expenditures on health services and medicines for cancer. If the burden of financial hardship from cancer is not addressed, the consequent impact on medical care access and utilization may lead to poor health outcomes among individuals with poor socioeconomic status (38, 39). This study also found that health care utilization of cancer patients were affected by age at diagnosis, location of tumor, stage of tumor, and survival years. Understanding personal socioeconomic and clinical features can help to identify sub-groups of cancer survivors with barriers to receipt of necessary cancer care, and to develop potential intervention points that ensure access to care across populations (40).
This is the first representative study that examined the urban-rural disparity and associated factors of health care utilization among cancer patients in China. However, there are several limitations to acknowledge in this study. Firstly, given the cross-sectional survey, the present analysis cannot identify the causal relationship between the identified determinants and health care utilization. Further research should investigate the causality with longitudinal survey data. Secondly, although we explored a broad set of individual factors associated with health care utilization from the demand side, no related information on health care system (availability, affordability and accessibility of healthcare services) from the supply side which might also influence health care utilization were involved, which will be explored in future study. Thirdly, our data were collected using a structured interviewer-administered questionnaire based on self-reported information of the participants, which might be subjected to recall bias.
In conclusion, health care utilization was suboptimal among patients with cancers in China. There were evident disparities in health care utilization between urban and rural cancer survivors. Health care utilization was determined by health insurance types, household income and clinical characteristics. The findings highlighted the needs of systematic collection of information on health care utilization of cancer patients. This would help policymakers to implement specific strategies for ensuring equitable utilization of health care, and to enforce the sufficient delivery of cancer care services in the country. More attention should be paid to the disadvantaged groups and rural cancer patients. Prioritizing health resources allocation is needed to prevent, screen, and treat cancers in rural areas in the future.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
This study was reviewed and approved by the Ethics Review Board of the School of Public Health, Shandong University (No. 20140201). All included participants provided written informed consent forms for participation in the survey before starting the interviews.
Author Contributions
HW and XS conceived and designed the study. XH and HW did the data analysis. HW wrote the first draft of the paper. XS supervised and revised the first draft. All authors reviewed and approved the final manuscript submitted for publication.
Funding
This work was supported by the China Medical Board (CMB 13-160).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are grateful to the students who participated in the survey for their cooperation. The authors acknowledge all staff involved in this research.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2018) 68:394–424. doi: 10.3322/caac.21492
2. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. (2016) 66:115–32. doi: 10.3322/caac.21338
3. Huang H, Shi J, Guo L, Zhu X, Wang L, Liao X, et al. Expenditure and financial burden for common cancers in China: a hospital-based multicentre cross-sectional study. Lancet. (2016) 388:S10. doi: 10.1016/S0140-6736(16)31937-7
4. Zheng R, Zeng H, Zhang S, Chen T, Chen W. National estimates of cancer prevalence in China, 2011. Cancer Lett. (2016) 370:33–8. doi: 10.1016/j.canlet.2015.10.003
5. Shih YC, Smieliauskas F, Geynisman DM, Kelly RJ, Smith TJ. Trends in the cost and use of targeted cancer therapies for the privately insured nonelderly: 2001 to 2011. J Clin Oncol. (2015) 33:2190–6. doi: 10.1200/JCO.2014.58.2320
6. Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. (2016) 66:271–89. doi: 10.3322/caac.21349
7. Varghese C, Shin HR. Strengthening cancer control in China. Lancet Oncol. (2014) 15: 484–5. doi: 10.1016/S1470-2045(14)70056-7
8. Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. (2005) 353:1784–92. doi: 10.1056/NEJMoa050518
9. Yabroff KR, Dowling E, Rodriguez J, Ekwueme DU, Meissner H, Soni A, et al. The Medical Expenditure Panel Survey (MEPS) Experiences with Cancer Survivorship Supplement. Journal of Cancer Survivorship. (2012) 6:407–19. doi: 10.1007/s11764-012-0221-2
10. Calonge N, Petitti DB, DeWitt TG, Dietrich AJ, Gregory K, Grossman D, et al. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. (2009) 151:716–26, W-236. doi: 10.7326/0003-4819-151-10-200911170-00008
11. Calonge N, Petitti DB, DeWitt TG, Dietrich AJ, Gregory K, Harris R, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. (2008) 149:627–37. doi: 10.7326/0003-4819-149-9-200811040-00243
12. Mayer DK, Nasso SF, Earp JA. Defining cancer survivors, their needs, and perspectives on survivorship health care in the USA. Lancet Oncol. (2017) 18:e11. doi: 10.1016/S1470-2045(16)30573-3
13. Yao N, Wang J, Cai Y, Yuan J, Wang H, Gong J, et al. Patterns of cancer screening, incidence and treatment disparities in China: protocol for a population-based study. BMJ Open. (2016) 6:e012028. doi: 10.1136/bmjopen-2016-012028
14. McNulty JA, Nail L. Cancer survivorship in rural and urban adults: a descriptive and mixed methods study. J Rural Health. (2015) 31:282–91. doi: 10.1111/jrh.12106
15. McDougall JA, Banegas MP, Wiggins CL, Chiu VK, Rajput A, Kinney AY. Rural disparities in treatment-related financial hardship and adherence to surveillance colonoscopy in diverse colorectal cancer survivors. Cancer Epidemiol Biomarkers Prev. (2018) 3:1275–82. doi: 10.1158/1055-9965.EPI-17-1083
16. Su M, Zhang N, Cai Y, Wang J, Anderson R, Yao N, et al. Work and income changes after cancer in rural China: a cross-sectional survey. Cancer Med. (2019) 8:7859–68. doi: 10.1002/cam4.2627
17. Huo Q, Cai C, Zhang Y, Kong X, Jiang L, Ma T, et al. Delay in diagnosis and treatment of symptomatic breast cancer in China. Ann Surg Oncol. (2015) 22:883–8. doi: 10.1245/s10434-014-4076-9
18. Zhao D, Zhou Z, Shen C, Nawaz R, Li D, Ren Y, et al. Rural and urban differences in patient experience in China: a coarsened exact matching study from the perspective of residents. BMC Health Serv Res. (2021) 21:330. doi: 10.1186/s12913-021-06328-0
19. Meng Q, Fang H, Liu X, Yuan B, Xu J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. (2015) 386:1484–92. doi: 10.1016/S0140-6736(15)00342-6
20. Jin Y, Zhu W, Yuan B, Meng Q. Impact of health workforce availability on health care seeking behavior of patients with diabetes mellitus in China. Int J Equity Health. (2017) 16:80. doi: 10.1186/s12939-017-0576-0
21. Abuduxike G, Aşut Ö, Vaizoglu SA, Cali S. Health-seeking behaviors and its determinants: a facility-based cross-sectional study in the Turkish Republic of Northern Cyprus. Int J Health Policy Manag. (2020) 9:240–9. doi: 10.15171/ijhpm.2019.106
22. Clewley D, Rhon D, Flynn T, Koppenhaver S, Cook C. Health seeking behavior as a predictor of healthcare utilization in a population of patients with spinal pain. PLoS ONE. (2018) 13:14. doi: 10.1371/journal.pone.0201348
23. Shaikh BT, Hatcher J. Health seeking behaviour and health service utilization in Pakistan: Challenging the policy makers. J Public Health (Oxf). (2005) 27:49–54. doi: 10.1093/pubmed/fdh207
24. Kim HK, Lee M. Factors associated with health services utilization between the years 2010 and 2012 in Korea: Using Andersen's Behavioral model. Osong Public Health Res Perspect. (2016) 7:18–25. doi: 10.1016/j.phrp.2015.11.007
25. O'Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cad Saude Publica. (2007) 23:2820–34. doi: 10.1590/S0102-311X2007001200003
26. Haque R, Parr N, Muhidin S. Parents' healthcare-seeking behavior for their children among the climate-related displaced population of rural Bangladesh. Soc Sci Med. (2019) 226:9–20. doi: 10.1016/j.socscimed.2019.02.032
27. Srivastava S, Gill A. Untreated morbidity and treatment-seeking behaviour among the elderly in India: Analysis based on National Sample Survey 2004 and 2014. SSM-Population Health. (2020) 10:100557. doi: 10.1016/j.ssmph.2020.100557
28. Chen W, Zheng R, Zhang S, Zhao P, Zeng H, Zou X, et al. Annual report on status of cancer in China, 2010. Chin J Cancer Res. (2014) 26:48–58. doi: 10.3978/j.issn.1000-9604.2014.01.08
29. Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin. (2018) 68:153–65. doi: 10.3322/caac.21443
30. Bestvina CM, Zullig LL, Yousuf ZS. The implications of out-of-pocket cost of cancer treatment in the USA: a critical appraisal of the literature. Future Oncol. (2014) 10:2189–99. doi: 10.2217/fon.14.130
31. Sun X, Shi J, Guo L, Huang H, Yao N, Gong J, et al. Medical expenses of urban Chinese patients with stomach cancer during 2002–2011: a hospital-based multicenter retrospective study. BMC Cancer. (2018) 18:435. doi: 10.1186/s12885-018-4357-y
32. Yao N, Zhang N, Wang J, Anderson RT, Liu X, Lyu J, et al. Experiences with cancer survey in China. Cancer. (2019) 125:3068–78. doi: 10.1002/cncr.32164
33. Su M, Lao J, Zhang N, Wang J, Anderson RT, Sun X, et al. Financial hardship in Chinese cancer survivors. Cancer. (2020) 126:3312–21. doi: 10.1002/cncr.32943
34. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
35. Esther N, Julius S, Deogratius MA. Understanding health-seeking and adherence to treatment by patients with esophageal cancer at the Uganda cancer Institute: a qualitative study. BMC Health Serv Res. (2021) 21:159. doi: 10.1186/s12913-021-06163-3
36. NHaFPCo C. Health and Family Planning Statistics Yearbook. (2016). Beijing: Peking Union Medical College Press (2016).
37. Liu G, Xue Y, Qian Z, Yang L, Yang Y, Geng Q, et al. Healthcare-seeking behavior among pregnant women in the Chinese hierarchical medical system: a cross-sectional study. Int J Equity Health. (2019) 18:129. doi: 10.1186/s12939-019-1037-8
38. Banegas MP, Dickerson JF, Kent EE, de Moor JS, Virgo KS, Guy GP Jr, et al. Exploring barriers to the receipt of necessary medical care among cancer survivors under age 65 years. J Cancer Surviv. (2018) 12:28–37. doi: 10.1007/s11764-017-0640-1
39. Kent EE, Forsythe LP, Yabroff KR, Weaver KE, de Moor JS, Rodriguez JL, et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. (2013) 119:3710–7. doi: 10.1002/cncr.28262
Keywords: health care utilization, cancer patients, urban-rural disparities, associated factors, China
Citation: Wang H, Hua X, Yao N, Zhang N, Wang J, Anderson R and Sun X (2022) The Urban-Rural Disparities and Associated Factors of Health Care Utilization Among Cancer Patients in China. Front. Public Health 10:842837. doi: 10.3389/fpubh.2022.842837
Received: 24 December 2021; Accepted: 10 February 2022;
Published: 04 March 2022.
Edited by:
Asankha Pallegedara, Wayamba University of Sri Lanka, Sri LankaReviewed by:
Jayasens Dissanayake, Wayamba University of Sri Lanka, Sri LankaN. Soysa, Wayamba University of Sri Lanka, Sri Lanka
Copyright © 2022 Wang, Hua, Yao, Zhang, Wang, Anderson and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaojie Sun, eGlhb2ppZXN1bkBzZHUuZWR1LmNu
 Haipeng Wang
Haipeng Wang Xingxing Hua2
Xingxing Hua2 Xiaojie Sun
Xiaojie Sun