
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 08 February 2022
Sec. Public Mental Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.832819
This article is part of the Research Topic The Consequences of COVID-19 on the Mental Health of Students View all 71 articles
Background: The COVID-19 pandemic has led to observed increases in reported mental health issues, such as depression and anxiety symptoms. There is evidence attentional bias is associated with depression and anxiety, and it has been further suggested that anxiety sensitivity has a role in both the development and maintenance of depression and anxiety symptoms. Understanding these relationships may help inform preventative interventions for those at risk of mental health concerns. The present study explores the role of anxiety sensitivity, specifically physical and cognitive concerns, as a potential mediator of the relationship between attentional bias with depression and anxiety symptoms.
Method: Participants (n = 460) were recruited from the general population in China, and completed an online survey between February and March, 2020 which included the Attention to Positive and Negative Information Scale (APNI), Anxiety Sensitivity Index-3 (ASI-3) and Depression, Anxiety and Stress Scale (DASS-21). After exploring the correlations between the measures, mediation analysis was performed to explore the role of anxiety sensitivity (physical and cognitive subscales) in the relationship between attentional bias and depression and anxiety (as measured by the DASS-21).
Results: The results indicated that negative attention bias was significantly positively correlated with physical and cognitive concerns, physical and cognitive concerns were significantly positively correlated with depression and anxiety, and negative attention bias was significantly positively correlated with depression and anxiety (all ps < 0.001). Physical and cognitive anxiety sensitivity mediated the relationship between negative attention bias and both anxiety and depression symptoms.
Conclusion: Negative bias was associated with levels of anxiety and depression, and physical and cognitive anxiety sensitivity mediated associations between negative bias and anxiety and depression symptoms. The study provides theoretical support for intervention and guidance on individual mental health during the pandemic, and helps individuals increase their concern to negative emotions.
Public health issues such as COVID-19 will not only have a huge impact on social production, life and economic conditions, but also affect the physical and mental health of the public. COVID-19 is sudden, because of its fast-spreading speed, wide range, and strong infectivity, it seriously threatens the safety of human life, and has adverse health effects (1). On January 30, 2020, COVID-19 was listed by the World Health Organization (WHO) as a public health emergency of international concern. At present, COVID-19 has had an extraordinary threat on all aspects of individual life, such as safety, health, and wellbeing. The effects also extend to mental health, with associated effects on anxiety, depression, panic and other negative emotions (2). Anxiety and depression are significant indicators of poor mental health (3). Empirical research suggests that mental health disorder, especially negative emotions such as anxiety and depression, are very common, which not only reduces life satisfaction, but also impairs life functioning (4–6).
Studies have suggested that cognition and emotion have interactions at the functional and neurological levels, which together constitute the basis of behavior (7–9). Cognition is a necessary condition for emotion generation. Attention, as an early stage of cognitive processing, will affect individual emotional experience.
Attentional bias is an automatic and uncontrollable unconscious tendency, which refers to prioritizing certain types of stimuli to increase our ability to process this information (10). A number of studies have suggested (11, 12) that anxiety and depression are associated with increased attention allocation to negative stimuli compared to neutral stimuli (i.e., an attentional negativity bias). Attentional bias can be measured both objectively and subjectively. Objective measurement refers to the research conducted from the perspective of behavioral cognition through experimentation (13–15). It is usually inferred by measuring the tendency to pay attention to one type of stimulus over another, such as smoking-related stimuli and neutral control stimuli (16). While subjective measurement meanwhile is typically collected through self-report measures such as the attention to positive and negative information scale which has shown good reliability and validity (17–20).
The cognitive theory of anxiety suggests that attention bias plays an essential role in the maintenance of anxiety (21). Some studies indicated that attention bias is closely relevant to anxiety and depression (22). For example, Joormann and Gotlib found that depressed individuals tend to pay attention to negative material and avoid positive material (23). Koster et al. found that individuals with anxiety attend toward threatening images by using images (threatening images and neutral images) as experimental materials to test the responses of subjects (24). EEG study indicates that negativity biases produce hyper-activation of fear circuits during non-conscious processing of anxiety and conscious processing of depression (25).
However, previous studies have explored the relationship between attentional bias and anxiety and depression (26), but there is a lack of further research on the mediating variables between attentional bias and anxiety and depression. Since the COVID-19, there have been a large number of studies exploring the mental health of people, studying the psychological conditions of different groups, focusing on psychological interventions, etc. (27, 28), but few studies have explored their anxiety from the cognitive level of individuals. Therefore, this study introduced another variable, anxiety sensitivity, to study the indirect effects of attentional bias on anxiety and depression.
Anxiety sensitivity (AS) refers to the fear of anxiety and sensations related to anxiety (29). Individuals with high AS tended to experience various negative emotions (30). AS is a key cognitive factor in the generation and maintenance of anxiety and depression, which can theoretically increase the risk of anxious and depressive psychopathology (31). Studies have found that individuals with high AS have an attention bias toward threat stimuli, which may trigger deeper negative emotions, which in turn deepens their attention to threat stimuli (32). Most research has focused on AS as a whole, and few studies have specifically explored its specific dimensions. AS has three dimensions: cognitive, physical and social concerns (33). Cognitive concern reflect fear of cognitive dyscontrol, physical concern reflect the fear of physical sensations accompanying anxiety, and social concern reflect the fear that an observable anxiety response will lead to social exclusion (34). Many studies have suggested that physical and cognitive mediate the relationship, but social concern was not found to be a significant mediator (35). Guo et al. (36) found that the mediating effect of social concern on anxiety and attentional control is not significant. But the study did not explore the mediating role of different dimensions of anxiety sensitivity between attention bias and other negative emotions.
Previous literature has not been clear on the relationship between attention bias, AS, anxiety and depression. To further the existing literature and integrating existing research results, the study examined the influence of negative bias on anxiety and depression, and further investigated the mediating role of physical and cognitive concerns. Furthermore, the study also investigated the mediating role of social concerns. Based on the above review, the following hypotheses for this study were: negative attention bias would be associated with anxiety and depression symptoms; physical and cognitive AS would mediate relations between negative attention bias and both anxiety and depression symptoms. This study has potential significance for understanding how attentional processing is related to anxiety sensitivity, and then lead to depression and anxiety symptoms during the COVID-19 pandemic. This understanding might be used to support public health messaging, and identify people at risk of poorer mental health during public health emergencies.
The study conducted a cross-sectional internet-based survey of Chinese adults from February to March 2020. This study used the widely popular Chinese social media application “WeChat” to invite participants (37). WeChat has location-based online communities. We arranged for WeChat community moderators from a large city in central China (within Henan province) to invite their residents through the app. It also includes some participants from other provinces, including Beijing, Sichuan, Zhejiang, etc. The present study used the Survey Star online questionnaire. Electronic consent of all participants was obtained in this study. Before obtaining participant consent, they were informed that the survey was anonymous and confidential. And inform the participants that the purpose of this survey is to investigate your mental health, the results of the survey are only used for statistics and not for other purposes. All procedures in this study conformed to the ethical standards of the Chinese Psychological Association (https://www.cpsbeijing.org/) and are in line with the 1964 Helsinki Declaration and subsequent amendments or similar ethical standards. The study was approved by the Tianjin Normal University ethics committee (XL2020-21).
A total of 529 people participated and completed all scales. All the participants had normal vision or corrected vision, without any history of mental disorder. Survey Star provides a feature that prevents participants from answering the questionnaire multiple times, and it prompts participants to complete skipped items, so there is no missing data. We removed participants who were considered to not have given the study proper attention by either providing the same response to all items, or who completed the full questionnaire battery in <180 s. A total of 460 valid questionnaires were retained, with an effective rate of 86.96%. The average age of the participants was 25.38 years (SD = 8.73). There were 154 male participants (33.5%) and 306 female participants (66.5%).
The APNI was developed by Noguchi et al. to measure attention bias toward positive or negative information (38). Lv et al. adapted a Chinese scale version, with a total of 30 items, divided into two dimensions: positive attention bias (19 items in total) and negative attention bias (11 items in total) (20). Items are rated on a 5-point Likert scale from 1 (“strongly disagree”) to 5 (“strongly agree”). In this study, the negative attention bias dimension was used to measure attention bias toward negative information. Internal consistency for the sample was 0.878.
The ASI-3 was developed by Taylor et al., mainly used to measure fear of anxiety-related symptoms based on the belief that they may have harmful personal consequences (33). The scale consists of three dimensions of physical, cognitive and social concerns. Each dimension has six items, for a total of 18 items. Items are rated on a 5-point Likert scale from 0 (“very little”) to 4 (“very much”) (39). Internal consistency for the present sample was 0.940 for the physical concern subscale, 0.924 for the cognitive concern subscale, and 0.888 for the cognitive concern subscale.
The DASS-21 was initially developed by Lovibond et al. and the Chinese version was developed by Gong et al. (3, 40). The questionnaire has good reliability and validity among Chinese adults, with a wide range of applicability (41). Twenty-one items are rated over the past week on a 4-point Likert scale from 0 (“not applicable”) to 3 (“very applicable”); higher scores reflect greater symptoms. The anxiety and depression sub-scales were used in this study, with Internal consistency of 0.890 and 0.917, respectively.
Statistical analyses were conducted using the SPSS (v. 22.0 for Windows; IBM Corporation), the data were analyzed for descriptive statistical analysis, Pearson correlations and regression analysis. The study used deviation-corrected percentile bootstrapping to test the mediating effect. The mediation analyses were conducted using the Hayes Process Macro for SPSS with 95% bias corrected confidence interval (CI) based on 5,000 bootstrap samples (42). The mediating effect exists if the confidence interval does not include 0. According to the hypothesis of this research negative attention bias would be associated with anxiety and depression symptoms; physical and cognitive AS would mediate relations between negative attention bias and both anxiety and depression symptoms. The study have run two analyses, one without the social concern and one with to check for the effect.
In order to explore relationships between negative attention bias and physical and cognitive concerns, anxiety and depression symptoms, Pearson correlations were conducted, and results are shown in Table 1. Specifically, negative attention bias was significantly positively correlated with physical concern (r = 0.408, p < 0.001) and cognitive concern (r = 0.449, p < 0.001), physical concern (r = 0.731, p < 0.001) and cognitive concern (r = 0.747, p < 0.001) were significantly positively correlated with depression, physical concern (r = 0.783, p < 0.001), and cognitive concern were significantly positively correlated with anxiety, and negative attention bias was significantly positively correlated with depression (r = 0.399, p < 0.001) and anxiety (r = 0.431, p < 0.001).
With negative attention bias as independent variable, cognitive and physical concerns as mediating variables, anxiety and depression as dependent variables separately, multiple mediation analysis were conducted. The results indicate that negative attention bias was significantly associated with depression and anxiety symptoms (β = 0.078, p = 0.022; β = 0.103, p = 0.001, respectively). Physical and cognitive concerns were significantly associated with depression (β = 0.304, p < 0.001; β = 0.444, p < 0.001, respectively), and physical and cognitive concerns were associated with anxiety (β = 0.450, p < 0.001; β = 0.327, p < 0.001, respectively). Results are reported in Table 2. From the model, negative attention bias not only directly predicted depression and anxiety, but also indirectly predicted depression and anxiety through physical and cognitive concerns.
The study analyzed the mediating effect of physical and cognitive concerns between attention bias and depression severity. Results suggested that the indirect effect of physical concern on the influence of negative attention bias on depression was 0.081. Its bootstrapped 95% confidence interval for the indirect effect of “negative attention bias → physical concern → depression” was (0.044, 0.126). The 95% confidence interval did not contain 0, indicating that physical concern had a significant mediating effect. The indirect effect of cognitive concern on the influence of negative bias on depression was 0.128, and the bootstrapped 95% confidence interval for the indirect effect of “negative attention bias → cognitive concern → depression” was (0.083, 0.179).The 95% confidence interval did not contain 0, indicating that cognitive concern had a significant mediating effect (see Table 3 and Figure 1). The finding indicates that physical concern and cognitive concern have significant mediating effects between negative attention bias and depression.
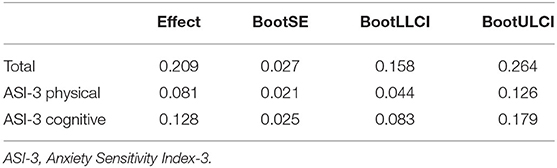
Table 3. Analysis of the mediating effect of physical concern and cognitive concern on negative bias affecting depression.
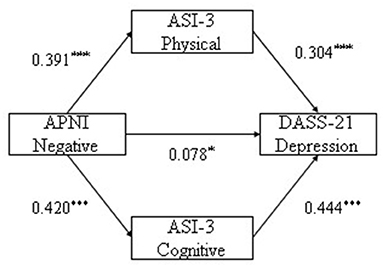
Figure 1. The mediating pathway of physical and cognitive concerns in negative bias influence depression. *p < 0.05, **p < 0.01, ***p < 0.001.
BootSE, BootLLCI, and BootULCI refer to the standard error, lower limit and upper limit of the 95% confidence intervals of the indirect effects estimated by the percentile bootstrap method corrected by deviation, respectively, as follows.
Next the study analyzed the mediating effect of physical and cognitive concerns between negative attention bias and anxiety. Results indicated that the indirect effect of physical concern on the influence of negative attention bias on anxiety was 0.117, and its bootstrapped 95% confidence interval for the indirect effect of “negative attention bias → physical concern → anxiety” was (0.079, 0.163). The 95% confidence interval did not contain 0, indicating that physical concern had a significant mediating effect. The indirect effect of cognitive concern on the influence between negative bias on anxiety was 0.092, and the bootstrapped 95% confidence interval for the indirect effect of “negative attention bias → cognitive concern → anxiety” was (0.054, 0.136). The 95% confidence interval did not contain 0, indicating that cognitive concern had a significant mediating effect (see Table 4 and Figure 2). The finding indicates that physical concern and cognitive concern have significant mediating effects between negative attention bias and anxiety.
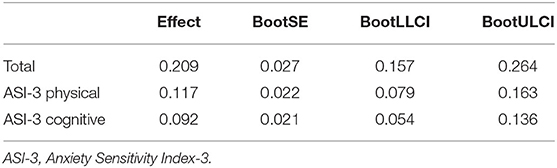
Table 4. Analysis of the mediating effect of physical concern and cognitive concern on negative bias affecting anxiety.
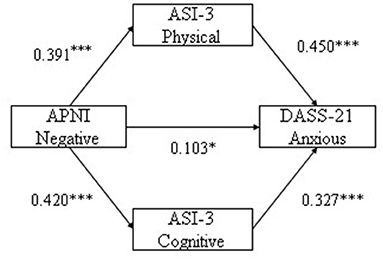
Figure 2. The mediating pathway of physical and cognitive concerns in negative bias influence anxious. *p < 0.05, ***p < 0.001.
In addition, the study also explored the mediating role of physical concern, cognitive concern, and social concern between negative bias and depression and anxiety, respectively. The results indicated that the regression coefficient of social concern was not significant (see Table 5), and the bootstrapped 95% confidence interval for the indirect effect of “negative attention bias → social concern → depression” was (−0.068, 0.001) (see Table 6). The 95% confidence interval of each parth contained 0. The bootstrapped 95% confidence interval for the indirect effect of “negative attention bias → social concern → anxiety” was (−0.034, 0.030) (see Table 7). The 95% confidence interval of each parth contained 0. These indicated the mediating effect of social concern was not significant.
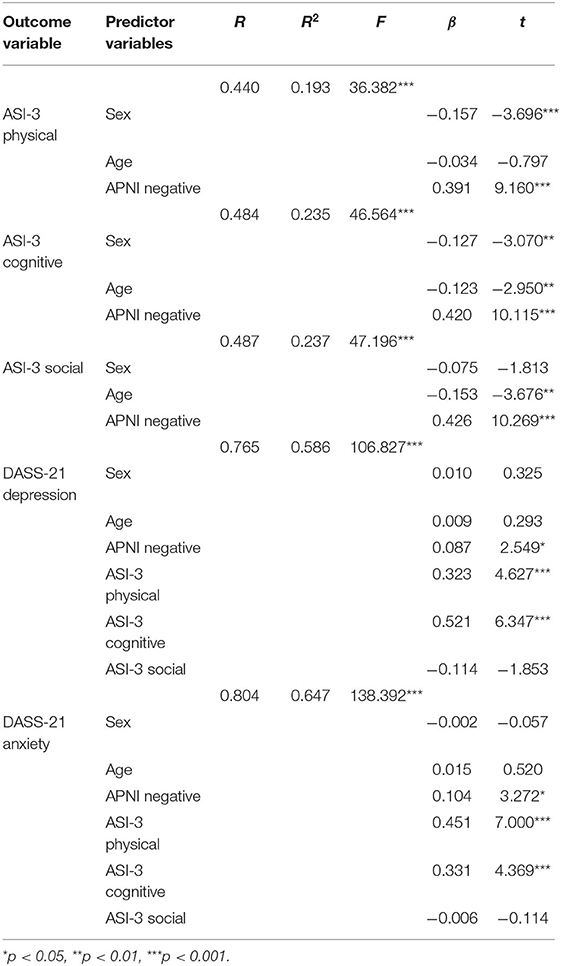
Table 5. Regression analysis of variable relationships in models (physical, cognitive, and social concerns as mediating variables).
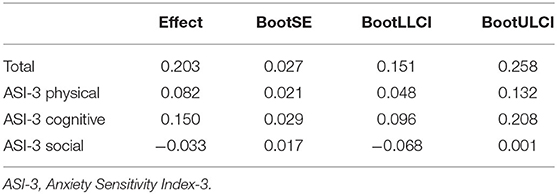
Table 6. Analysis of the mediating effect of physical, cognitive, and social concerns on negative bias affecting depression.
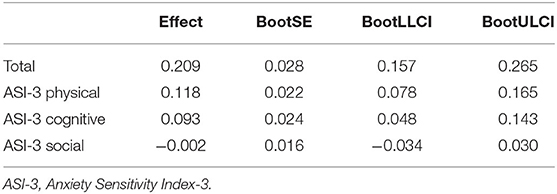
Table 7. Analysis of the mediating effect of physical, cognitive and social concerns on negative bias affecting anxiety.
Since December 2019, the COVID-19 has affected social production and personal life to varying degrees. With the development of society and economy, in the face of public emergencies, the public's ability to protect against risks economically has increased, but the psychological impact cannot be ignored. Therefore, more and more scholars have begun to explore the public's psychological conditions and risk perceptions behind public events from a psychological perspective (32). In February 2020, Guo et al. (43) surveyed the mental health status of 26,000 Chinese people through an online questionnaire, and found that 33% of the participants had a certain degree of depression, and 22.4% of the participants had obvious anxiety. During the pandemic, the incidence of public anxiety and depression has increased (44).
The present study focus on the relationship between cognition and emotion, especially explored the relationship between negative attention bias and anxiety and depression through physical and cognitive concerns (45). The results indicated that negative bias was significantly positively correlated with anxiety and depression, suggesting that negative bias is a potential influencing factor of anxiety and depression, which would induce negative emotion and have a negative influence on mental health development. During the pandemic, people will receive a lot of news about the COVID-19. Compared with individuals who pay more attention to positive information related to the pandemic, individuals who are biased toward negative news will have more negative emotions such as anxiety or depression. From the perspective of cognition, different cognitive styles will lead to differences in attention bias and affect individual emotional health to varying degrees, thus enhancing negative emotions such as anxiety and depression (46). This may also be one of the reasons why different individuals experience different anxiety and depression in the same context of the pandemic.
Negative attention bias and AS subscales were significantly positively correlated, indicating that when individuals have attention bias to negative information, their worries and fears about their own physical feelings and cognitions increase. The onion model of cognition suggests that cognitive processes and personality factors are interrelated and interact with each other (47). Consistent with previous studies, individual cognitive differences, such as attention bias to negative information, are reasons leading to high AS (27). During the pandemic, some individuals may pay too much attention to the negative information about the pandemic rather than the positive information. As shown in the results of this study, on the one hand, the attentional bias toward negative information will cause individuals to have stronger fears of their own physical sensations (such as sweating, shaking, etc.); on the other hand, it will also cause individuals to have a fear of cognitive dissonance.
According to correlation and regression results excessive worry about physiology and cognition were associated with negative emotions. As cognitive susceptibility factors of mental disorders, AS and its subscales are not only considered as risk factors leading to anxiety disorders, but also as important influencing factors of anxiety and depression (48). They are malleable and easy to be evaluated (49). In view of this, people with high AS may have a low tolerance for emotions such as anxiety, whereas individuals with low AS may have high tolerance (50). Previous studies have also suggested that there is a positive correlation between AS and negative emotions, and individuals with high AS tend to experience various negative emotional states (51). It can be inferred that during the pandemic, individuals with high AS tend to experience more negative emotions such as anxiety or depression. Results of the present study suggest that negative bias may affect anxiety and depression through the mediating effects of physical concern and cognitive concern, respectively. When an individual has attention bias toward negative information, the individual will have a fear of impaired cognitive control, and the individual's cognitive concern will further increase their negative emotional experiences such as anxiety and depression. Researchers believe that cognitive attention will trigger one's negative emotions by amplifying anxiety symptoms, thereby driving the relationship between AS and anxiety and depression (52). This is consistent with results of previous studies (53). Prior work has suggested that cognitive AS can increase anxiety and depression. Individuals with high cognitive concern believe that their symptoms, such as attentional decline or psychological incompetence will cause individuals to feel more uncomfortable, thus further enhancing negative emotional experience (35). The current research lacks evidence that social concern has mediating effect between negative bias and depression and anxiety. It indicates that, individuals pay less attention to society than their physical and cognitive concerns during the pandemic, that is, external evaluations may not trigger individual fear. It is consistent with the results of the previous studies, among the three dimensions of AS, only social concern does not work (36).
The current research on mental health is very necessary, and it is necessary to continue to strengthen public mental health science publicity and psychological counseling during the COVID-19. All sectors of society should gradually start to prevent and respond to mental health problems after the pandemic, and strengthen the construction of the social psychological service system and improve the public's mental health development in the future.
The current study investigated attention bias to negative information applied to the mediation effect of anxiety and depression, it still has several limitations. On the one hand, as a cross-sectional study, it is impossible to determine the causal relationship and direction between variables, and the self-reports cannot guarantee the objectivity and authenticity of the data. Future research can use longitudinal research to further study causality. On the other hand, besides the mediating effect of physical and cognitive concerns, there may also be some regulatory variables affecting the relationship between individual negative bias, anxiety and depression. Future studies may consider further exploring the relations of negative bias on mental health in more complex models.
In sum, the current study found that negative bias was associated with levels of anxiety and depression, and physical and cognitive AS mediated associations between negative bias and anxiety and depression symptoms. The findings of this study provide theoretical support for intervention and guidance on individual mental health during the pandemic, and helps individuals increase their concern to negative emotions.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Tianjin Normal University. The patients/participants provided their written informed consent to participate in this study.
SL designed the study protocol. XL conducted data collection, data management, cleaning, and analysis. SL and XL wrote the first draft of the paper. All authors contributed to the article and approved the submitted version.
This research receives a grant from the Natural Science Foundation of China (Grant number 31800921).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Xie DD, Yang Y, Cheng LJ. The impact of home quarantine and physical exercise on mental health during COVID-19. Chinese J Clin Psychol. (2021) 29:1343–7. doi: 10.16128/j.cnki.1005-3611.2021.06.045
2. Pfefferbaum B, North CS. Mental health and the covid-19 pandemic. N Engl J Med. (2020) 383:510–2. doi: 10.1056/NEJMp2008017
3. Gong X, Xie XY, Xu R, Luo YJ. Psychometric properties of the Chinese versions of DASS-21 in Chinese College Students. Chinese J Clin Psychol. (2010) 18:443–6. doi: 10.16128/j.cnki.1005-3611.2010.04.020
4. Mackenzie S, Wiegel JR, Mundt M, Brown D, Saewyc E, Heiligenstein E, et al. Depression and suicide ideation among students accessing campus health care. Am J Orthopsychiatr. (2011) 81:101–7. doi: 10.1111/j.1939-0025.2010.01077.x
5. Li DP, Xu L, Bao ZY, Chen Y, Su XH. Family financial strain and adolescents' depression: the effects of perceived discrimination and parent-adolescent attachment. Psychol Dev Educ. (2015) 31:342–9. doi: 10.1002/cad.20098
6. Luo YC, Bian YF, Chen XY, Wang L. Effect of parental rejection on adolescents' depression: a moderated mediation effect. Chinese J Clin Psychol. (2015) 23:268–72. doi: 10.16128/j.cnki.1005-3611.2015.02.017
7. Dolan RJ. Emotion, cognition, and behavior. Science. (2002) 298:1191–4. doi: 10.1126/science.1076358
8. Phelps EA. Emotion and cognition: insights from studies of the human amygdala. Annu Rev Psychol. (2006) 57:27– 53. doi: 10.1146/annurev.psych.56.091103.070234
9. Pessoa L. On the relationship between emotion and cognition. Nat Rev Neurosci. (2008) 9:148–58. doi: 10.1038/nrn2317
10. Robinson TE, Berridge KC. The neural basis of drug craving: an incentive–sensitization theory of addiction. Brain Res Rev. (1993) 18:247–91. doi: 10.1016/0165-0173(93)90013-P
11. Wu L, Lin BX, Liu L. Difficulties of highly anxious individuals in removing attention from emotionally negative information. J Psychol Sci. (2017) 40:310–4. doi: 10.16719/j.cnki.1671-6981.20170209
12. Zhou Z, Cao S, Li H, Li Y. Treatment with escitalopram improves the attentional bias toward negative facial expressions in patients with major depressive disorders. J Clin Neurosci. (2015) 22:1609–13. doi: 10.1016/j.jocn.2015.03.036
13. De Mathis MA, Batistuzzo MC, Bar-Haim Y, Abend R, Miguel EC, Morais I, et al. Attentional bias in specific symmetry and cleaning dimensions of obsessive-compulsive disorder. J Anxiety Disord. (2020) 73:1–7. doi: 10.1016/j.janxdis.2020.102238
14. Godara M, Sanchez-Lopez A, De Raedt R. Manipulating avoidance motivation to modulate attention bias for negative information in dysphoria: an eye-tracking study. J Behav Ther Exp Psychiatry. (2021) 70:1–8. doi: 10.1016/j.jbtep.2020.101613
15. Jiang YX, Chen H. Attention and recognition bias towards body-related cues among self-objectified female. J Psychol Sci. (2019) 42:1462–9. doi: 10.16719/j.cnki.1671-6981.20190627
16. Wilcockson TD, Pothos EM, Osborne AM, Crawford TJ. Top-down and bottom-up attentional biases for smoking-related stimuli: comparing dependent and non-dependent smokers. Addict Behav. (2021) 118:106886. doi: 10.1016/j.addbeh.2021.106886
17. Wang ZW, Li FZ, Wan XC, Shi M, Xiao W. Attention bias and emotion regulation: mediating of emotional complexity. China J Health Psychol. (2020) 28:1723–7. doi: 10.13342/j.cnki.cjhp.2020.11.026
18. Xie JP, Xu S, Peng L, Shao YF, Li Xiong JX. Multiple mediation effects of attention bias on depression and negative affective neuroscience personality of army new recruits. Occup and Health. (2020) 36:1943–7. doi: 10.13329/j.cnki.zyyjk.2020.0518
19. Alamdar S, Lv Y, Guo J, Lu J, Zhang Y. Attentional bias effect on post-traumatic outcomes in children after earthquake: mediation role of rumination. PsyCh J. (2020) 2020:1–11. doi: 10.1002/pchj.360
20. Lv YD, Guo J, Zhang YQ. A revision of the attention to positive and negative information scale (APNI) in Chinese children. Chinese J Clin Psychol. (2016) 24:861–4. doi: 10.16128/j.cnki.1005-3611.2016.05.021
21. Beck AT, Clark DA. An information processing model of anxiety: automatic and strategic processes. Behav Res Ther. (1997) 35:49–58. doi: 10.1016/S0005-7967(96)00069-1
22. Sheppes G, Luria R, Fukuda K, Gross JJ. There's more to anxiety than meets the eye: isolating threat-related attentional engagement and disengagement biases. Emotion. (2013) 13:520–8. doi: 10.1037/a0031236
23. Joormann J, Gotlib IH. Selective attention to emotional faces following recovery from depression. J Abnorm Psychol. (2007) 116:80–5. doi: 10.1037/0021-843X.116.1.80
24. Koster EHW, Crombez G, Verschuere B. Components of attentional bias to threat in high trait anxiety: facilitated engagement, impaired disengagement, and attentional avoidance. Behav Res Ther. (2006) 44:1757–71. doi: 10.1016/j.brat.2005.12.011
25. Williams LM, Kemp AH, Felmingham K, Liddell BJ, Palmer DM, Bryant RA. Neural biases to covert and overt signals of fear: dissociation by trait anxiety and depression. J Cogn Neurosci. (2007) 19:1595–608. doi: 10.1162/jocn.2007.19.10.1595
26. Yu YJ. Effects of anxiety and depression on attentional bias: the mediating role of attentional control. Stud Psychol Behav. (2020) 18:121–7.
27. Bai XJ. How to strengthen the capacity building of psychological service institutions in China under the normal epidemic prevention and control. Stud Psychol Behav. (2020) 18:730–1.
28. Xu Y. Social and psychological response in the post-epidemic era. Stud Psychol Behav. (2020) 18:724–6.
29. McNally RJ. Anxiety sensitivity and panic disorder. Biol Psychiatry. (2002) 52:938–46. doi: 10.1016/S0006-3223(02)01475-0
30. Cai WP,. Attention Bias in High Anxiety Sensitivity Military Personnel Modification. (Dissertation), The Second Military Medical University, Shanghai, China (2018). Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CDFD&dbname=CDFDLAST2019&filename=1018084026.nh&uniplatform=NZKPT&v=YjeZd5Jj-hPxbxCCk83jPO-n834css2tvMFAb8qw-dvj15xE9tKuKZI_dRB6IizL
31. Olatunji BO, Wolitzky, Taylor K. Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychol Bullet. (2009) 135:974–99. doi: 10.1037/a0017428
32. Zhao XY. Attentional Bias of Individuals With Different Anxiety Sensitivities to Medical-Related Information. (Dissertation), Tianjin Normal University, Tianjin, China (2021). doi: 10.27363/d.cnki.gtsfu.2021.000206
33. Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess. (2007) 19:176–88. doi: 10.1037/1040-3590.19.2.176
34. Taylor S. Anxiety Sensitivity: Theory, Research, and Treatment of the Fear of Anxiety. Mahwah, NJ: Lawrence Erlbaum Associates (1999).
35. Olthuis JV, Watt MC, Stewart SH. Anxiety sensitivity index (asi-3) subscales predict unique variance in anxiety and depressive symptoms. J Anxiety Disord. (2014) 28:115–24. doi: 10.1016/j.janxdis.2013.04.009
36. Guo Y, Yang H, Elhai J, McKay D. Anxiety regarding COVID-19 is related to attentional control: the mediating role of anxiety sensitivity. Front Psychiatry. (2021) 12:713279. doi: 10.3389/fpsyt.2021.713279
37. Montag C, Becker B, Gan C. The multipurpose application WeChat: a review on recent research. Front Psychol. (2018) 9:1–8. doi: 10.3389/fpsyg.2018.02247
38. Noguchi K, Gohm CL, Dalsky DJ. Cognitive tendencies of focusing on positive and negative information. J Res Pers. (2006) 40:891–910. doi: 10.1016/j.jrp.2005.09.008
39. Wang L, Liu W, Zhu X, Wang Y, Li L, Yang Y, et al. Validity and reliability of the Chinese Version of the Anxiety Sensitivity Index-3 in healthy adult women. Chinese Mental Health J. (2014) 28:767–71. doi: 10.3969/j.issn.1000-6729.2014.10.008
40. Lobvibnd PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
41. Wen Y, Wu DX, Lv XJ, Li HG, Liu XC, Yang YP. Psychometric properties of the Chinese Short Version of Depression Anxiety and Stress Scale in Chinese adults. Chin J Public Health. (2012) 28:436–1438.
42. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. 2nd ed. New York, NY: Guilford (2018).
43. Guo F, Cai Y, Wang YX, Li YY, Chen ZY. Emotional health status and social mentality of the Chinese general public during the 2019 novel coronavirus pneumonia pandemic. Sci Techol Rev. (2020) 38:68–76. doi: 10.3981/j.issn.1000-7857.2020.04.009
44. Gavin B, Lyne J, McNicholas F. Mental health and the COVID19 pandemic. Irish J Psychol Med. (2020) 2020:1–7. doi: 10.1017/ipm.2020.72
45. Chang JH, Yuan YX, Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. J Southern Med Univ. (2020) 40:171–6. doi: 10.12122/j.issn.1673-4254.2020.02.06
46. Zhong JJ, Chen ZY, Fang FX. The mechanism of cognitive styles and operations influencing on individual difference of intelligence level. Psychol Expl. (2012) 32:231–5.
47. Xue WF. The basic function of consciousness and the basic logic of personality type. Technol Enterprise. (2013) 13:296. doi: 10.13751/j.cnki.kjyqy.2013.13.298
48. Capron DW, Kotov R, Schmidt NB. A cross-cultural replication of an interactive model of anxiety sensitivity relevant to suicide. Psychiatry Res. (2012) 205:74–8. doi: 10.1016/j.jpsychires.2011.10.009
49. Schmidt NB, Norr AM, Allan NP, Raines AM, Capron DW. A randomized clinical trial targeting anxiety sensitivity for patients with suicidal ideation. J Consult Clin Psychol. (2017) 85:596–610. doi: 10.1037/ccp0000195
50. Weems CF. Anxiety sensitivity as a specific form of distress tolerance in youth: Developmental assessment, origins, and applied applications. Distr Toler Theor Res Clin Appl. (2010) 2010:29–51. Available online at: https://www.researchgate.net/profile/Carl-Weems/publication/261025895_Anxiety_sensitivity_as_a_specific_form_of_distress_tolerance_in_youth_Developmental_assessment_origins_and_applied_applications/links/00b7d53305aba111fc000000/Anxiety-sensitivity-as-a-specific-form-of-distress-tolerance-in-youth-Developmental-assessment-origins-and-applied-applications.pdf
51. Cox BJ, Borger SC, Taylor S, Fuentes K, Ross LM. Anxiety sensitivity and the five-factor model of personality. Behav Res Ther. (1999) 37:633–41. doi: 10.1016/S0005-7967(98)00174-0
52. Capron DW, Norr AM, Macatee RJ, Schmidt NB. Distress tolerance and anxiety sensitivity cognitive concerns: testing the incremental contributions of affect dysregulation constructs on suicidal ideation and suicide attempt. Behav Ther. (2013) 44:349–58. doi: 10.1016/j.beth.2012.12.002
Keywords: anxiety sensitivity, physical concerns, cognitive concerns, mental health, attention bias
Citation: Li S and Li X (2022) The Relationship Between Attentional Bias, Anxiety Sensitivity, and Depression and Anxiety Symptoms: Evidence From the COVID-19 Pandemic in China. Front. Public Health 10:832819. doi: 10.3389/fpubh.2022.832819
Received: 10 December 2021; Accepted: 13 January 2022;
Published: 08 February 2022.
Edited by:
Li Wang, Institute of Psychology (CAS), ChinaReviewed by:
Rob Saunders, University College London, United KingdomCopyright © 2022 Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao Li, bGl4aWFvaG4xMDE4QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.