- 1Institute for Health Research, University of Bedfordshire, Luton, United Kingdom
- 2Quality Improvement, Northampton General Hospital NHS Trust, Northampton, United Kingdom
- 3Institute for Sport and Physical Activity Research, Centre for Health, Wellbeing and Behaviour Change, University of Bedfordshire, Bedford, United Kingdom
- 4Division of Sport, Health and Exercise Sciences, Department of Life Sciences, Brunel University London, Uxbridge, United Kingdom
- 5Centre for Physical Activity in Health and Disease, Brunel University London, Uxbridge, United Kingdom
- 6Centre for Behaviour Change, University College London, London, United Kingdom
The workplace is a major contributor to excessive sitting in office workers. There are a wide array of adverse effects of high volumes of sitting time, including an increased risk of type 2 diabetes and depression. Active workstations can be used in effective interventions to decrease workplace sitting. However, there are a lack of interventions that have been developed using a systematic process that is informed by participant needs and a framework for identifying the most appropriate content for the intervention. Applying these methods could increase adherence and potential effectiveness of the intervention. Therefore, the purpose of this pilot study is to examine the feasibility, acceptability, and efficacy of a tailored workplace intervention to reduce and break up sitting in office workers that has been developed using the Behavior Change Wheel and the APEASE (Acceptability, Practicability, Effectiveness/cost-effectiveness, Affordability, Safety/side-effects, Equity) criteria. This article reports the protocol for this study that is currently ongoing. Participants will be cluster-randomized (by offices) to control and intervention groups. The evaluation of the intervention includes determining feasibility by assessing participant recruitment, retention and data completion rates. Adherence to the intervention will be assessed based on daily sitting and standing time relative to guidelines provided to participants as part of the intervention. Outcome measures also include productivity measured using Ecological Momentary Assessment, absenteeism, presenteeism, cardiometabolic risk markers, and wellbeing. The findings of this study will inform the effective design and implementation of interventions for reducing and breaking up sitting in office workers.
Introduction
Sedentary behavior has been described as any waking behavior in a sitting, reclining or lying posture that has an energy expenditure of ≤ 1.5 metabolic equivalents (METs) (1). In the United Kingdom, high levels of sedentary behavior have been reported with male and female employees sitting more than 11 h/day on average (2). Studies have identified the workplace as a major contributor to excessive sitting (3) with one study reporting that office workers spent 79% of their working day sitting and 42% of their work hours engaging in prolonged sitting (i.e., sitting bouts ≥ 30 min) (4).
Individuals who spend prolonged periods being sedentary have an increased risk of adverse health outcomes, including type 2 diabetes, cardiovascular disease, some cancers, and mental health problems such as depression and anxiety (5–9). This has led to incorporating a focus on reducing and breaking up sedentary behavior in national and international physical activity guidelines (10, 11). As high amounts of sitting are accumulated in the office workplace, this is a key setting where interventions could be implemented to improve occupational and public health. Indeed, an expert consensus statement recommended that workers who are in predominantly desk-based occupations should start by accumulating 2 h of standing and light activity during working hours each day, and progress to reaching a target of 4 h per day (12).
There is a growing body of evidence that suggests height-adjustable workstations (i.e., a workstation that permits the user to interchangeably work in a seated or standing posture) could be effective for decreasing sitting in the workplace (13). When height-adjustable workstations are provided as part of multi-component interventions that also include strategies such as education, manager support, standing meetings, self-monitoring and social support, workplace sitting has been significantly reduced by 45 to 83 min/work shift after 12 months (14, 15). Although these interventions appear promising, management of organizations might be reluctant to implement them if productivity is negatively affected (16). With respect to productivity concerns, a systematic review reported that productivity is likely to be unaffected by using a height-adjustable workstation (17). There are also limited studies that have reported taking employee's perceptions and experiences into account when developing interventions to reduce workplace sitting (18), which may limit intervention adherence and effectiveness. By involving the target audience in the development of interventions, this will help to ensure their needs are met and enhance their adherence and engagement (19). The Behavior Change Wheel (BCW) (20, 21) has been recommended for guiding the systematic process of developing an intervention using a framework that takes into account the needs of the target audience. To the author's knowledge, only one previous office workplace intervention has been developed using the BCW (18); the SMArT Work intervention in National Health Service employees led to significant reductions in sitting at work and improvements in job performance, work engagement, occupational fatigue, sickness presenteeism, anxiety and quality of life over 12 months (15). Further research is required in other occupational groups to strengthen the evidence base for incorporating a focus on reducing and breaking up sitting in workplace policy and practice. Demonstrating the effectiveness of such interventions for improving work-related outcomes, such as worker productivity, will be important for encouraging the adoption of such changes in policy and practice. The use of ecological momentary assessment (EMA) facilitated through smartphone technology provides the opportunity to collect simultaneous time-stamped data with limited recall bias to elucidate on the temporal effects of posture and activities on work performance throughout the workday (22, 23). However, the effects of workplace sitting interventions on EMA measures of work-related outcomes is limited.
This article describes the protocol for a pilot cluster-randomized controlled trial (RCT) to evaluate the feasibility and efficacy of a multi-component intervention to reduce and break up workplace sitting, including the systematic process for identifying the content of the intervention using the BCW. The effects of the intervention on a range of sitting, activity, health, wellbeing and work-related outcomes (including EMA assessment) will be evaluated.
Methods
Study Design and Overview
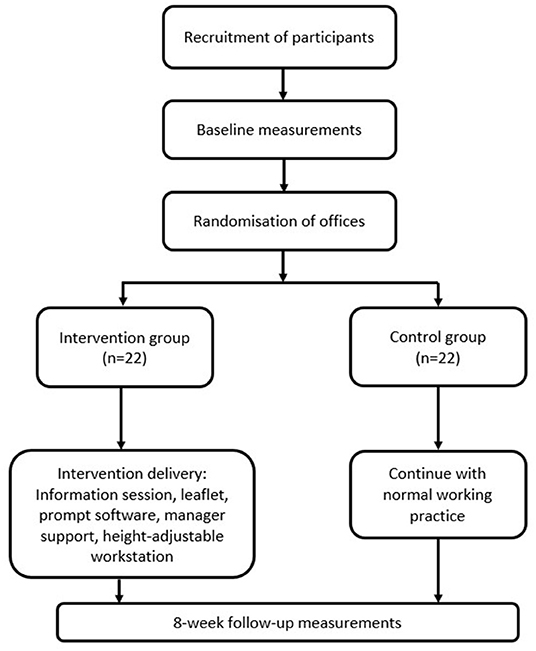
The study adopts an 8-week, two-arm cluster RCT design that is planned to be conducted during Spring and Summer months (see Figure 1 for overview of study design). The unit of randomization will be the workers' offices in line with previous research (24). Participants will be randomly allocated into clusters with each cluster being in either the control or intervention group for a period of 8 weeks. Given the nature of the intervention, blinding from participants or the core research team is not possible.
The study is registered on ClinicalTrials.gov (NCT03560544). Ethical approval for the procedures detailed below was obtained from the University of Bedfordshire Institute for Health Research Ethics Committee (lHREC836). Participants will provide written informed consent prior to any testing procedures and the study is being conducted in accordance with the Declaration of Helsinki.
Study Setting
The study will be conducted with office workers employed across a university campus and a local council, both located in the East of England region, UK. Participants were recruited from one campus at the university and employees at the council worked within offices at a single site. Clusters of participants will be recruited from both organizations who will be randomly allocated to the intervention or control group i.e., there will be intervention and control clusters located at each organization.
Participant Recruitment
Management approval will be sought and obtained for the recruitment of the employees, changes to the workplace environment, and for study testing and communications to take place during work time. The project will be advertised to staff as part of a workplace wellbeing programme via internal mail, staff meetings, information fliers in offices and other strategic places within the participating organizations.
Eligibility Criteria
Participants will be full-time desk-based office employees between the ages of 18 and 60 years employed in any job type and from any ethnic background. Individuals will be excluded from the study if they are pregnant, have a history of musculoskeletal complaints, non-ambulatory, or have a planned holiday that would mean they would not be at work for more than 2 weeks during the 8-week intervention period.
Sample Size
There is no standard procedure for determining the sample size for pilot studies as their main purpose is to obtain an estimate of the standard deviation that could be used to determine the likely effect size to inform a full trial (25). Thus, the proposed study will recruit a total of 44 participants in two groups of 18 allowing for an attrition rate of 20%. This is in line with sample size recommendations for pilot studies (26) and that used in a previous related pilot study of a workplace intervention to reduce sitting (27).
Randomization
To minimize contamination between groups in open plan offices, a cluster randomization approach will be used with offices being the unit of randomization i.e., randomization into either the intervention or control group will be assigned on an office basis (28). The number of clusters is projected to be approximately eight with an average cluster size of six (29). Randomization will be achieved by assigning a cluster ID to each office and clusters then being allocated to intervention or control group using an online randomization tool (https://www.randomlists.com/team-generator) by an independent researcher (30). Randomization will take place before the collection of baseline measurements and group allocation will not be disclosed to participants until the completion of baseline assessment (28).
Intervention Development, Content and Delivery
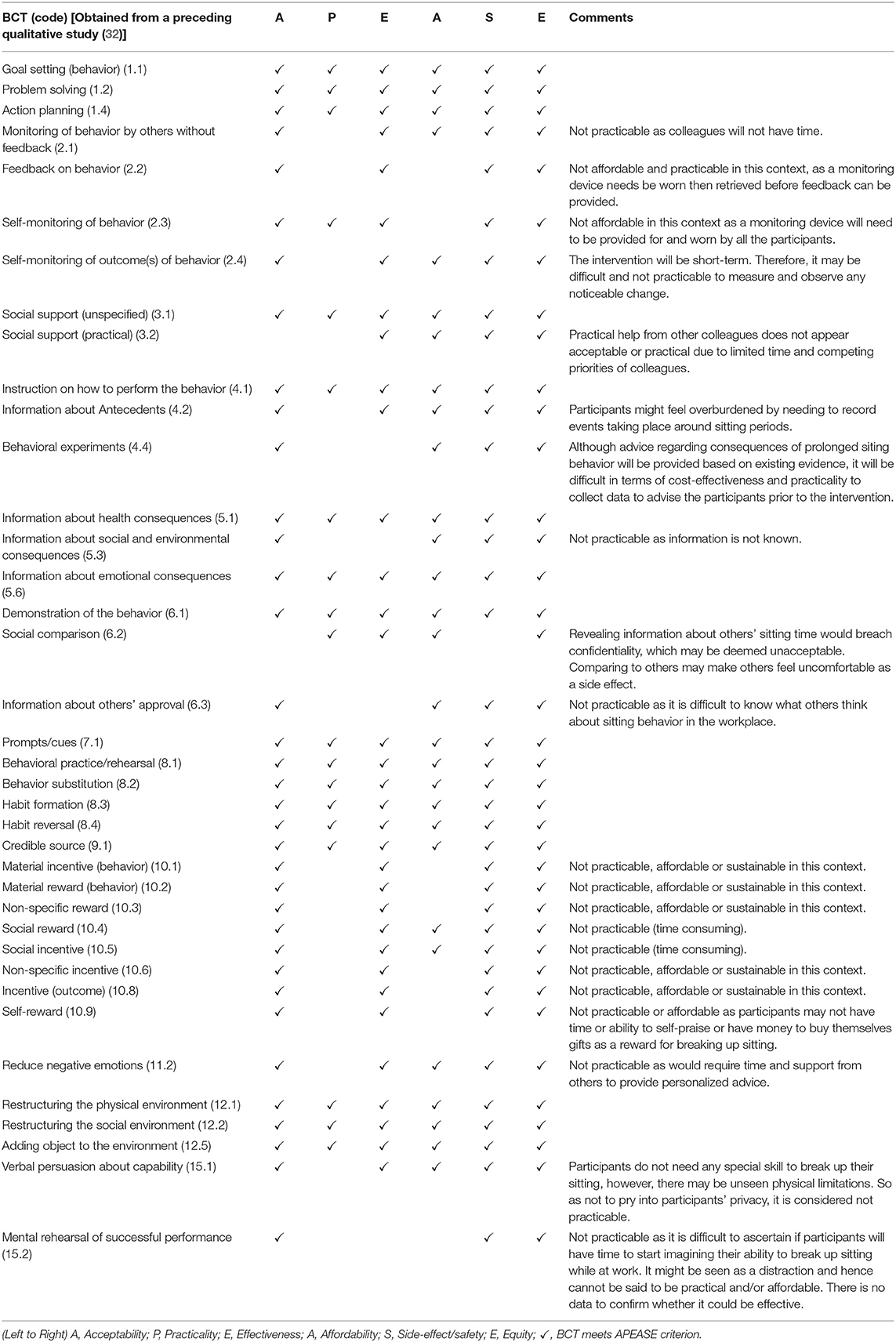
The intervention described in this study protocol was developed by systematically following the BCW framework (20, 31). The first step was to identify the problem (health and cardiovascular disease risk) in behavioral terms (sedentary behavior) and specify the target behavior to be changed (sitting at work). This was then followed by a COM-B (Capability, Opportunity and Motivation-Behavior) behavioral analysis conducted for the identification of barriers and facilitators to breaking up workplace sitting in office workers (32). The analysis led to the identification of seven core themes [“Knowledge-deficit sitting behavior,” “Willingness to change,” “Inadequate cognitive resources for action,” “Tied to the desk,” “Competing motivations,” “Emotional influences,” and “Organizational support and interpersonal influences” (32)], which linked to five of the six COM constructs and 12 domains of the Theoretical Domains Framework (TDF) (33). The TDF serves as a theoretical lens for understanding the cognitive, affective, social and environmental influences on behavior (33, 34). Subsequently, seven possible intervention functions, three policy categories and 38 behavior change techniques (BCTs) based on the BCT Taxonomy version 1 (35) that could be considered for inclusion in an intervention for reducing and breaking up workplace sitting were identified (36).
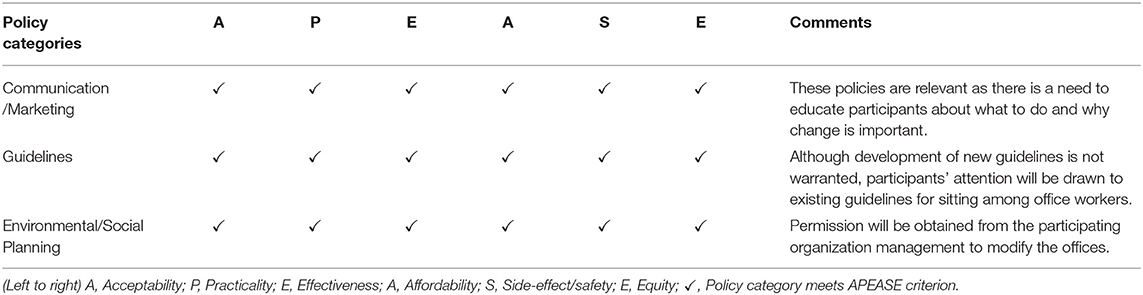
In deciding which intervention functions, policy categories and BCTs were most appropriate or have the highest possibility of success in delivering the desired change in this context, the Acceptability, Practicability, Effectiveness/cost-effectiveness, Affordability, Safety/side-effects, Equity (APEASE) criteria was applied. This is line with recommendations for using the BCW in practice (21, 37). Initial judgments using the APEASE criteria were made by the first author and reviewed by the co-authors (AC, DB and DH) until consensus regarding acceptance or rejection was reached. This led to identifying for inclusion, five intervention functions (Education, Persuasion, Enablement, Training and Environmental Restructuring; see Table 1), three policy categories (Communication/Marketing, Guidelines, and Environmental/Social Planning; Table 2) and 17 BCTs [Goal setting (behavior), Action planning, Problem solving, Instruction on how to perform the behavior, Credible source, Information about health consequences, Information about emotional consequences, Prompts/cues, Social support [unspecified], Restructuring the physical environment, Restructuring the social environment, Adding objects to the environment, Behavioral practice/rehearsal, Behavior substitution, Habit formation, Habit reversal and Demonstration of the behavior; see Table 3]. Table 4 shows a logic model, whereby the intervention content specified by BCTs is mapped onto components of the TDF and COM-B model. It also includes description of the delivery mode for the intervention content. The intervention thus includes a combination of education, persuasion, training, enablement, and environmental restructuring with the aim of addressing all of the identified constructs of the COM-B model and TDF. The intervention strategies and modes of delivery consist of an information session provided by a researcher and a leaflet covering the health consequences of prolonged sitting and the benefits of breaking up sitting, goal setting, action planning; computer prompt software; line manager support; and a height-adjustable workstation at each individual's desk. The computer prompt Google Chrome extension “Marinara: Pomodoro Assistant” will be installed on participant's computers. This prompt software has a customisable timer that can be used to set prompt alerts that appear as pop-up messages on the screen to remind the user to take a break. The break duration is customisable and the user is notified when the break has ended.
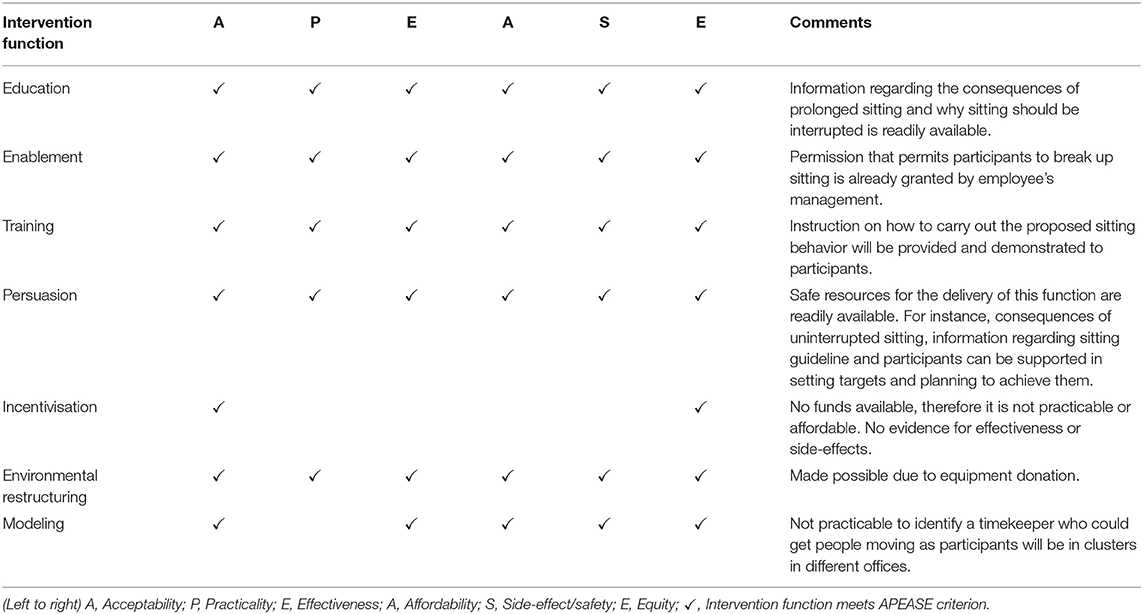
Table 1. Selection of intervention functions to cause a change in sitting behavior in desk-based employees.
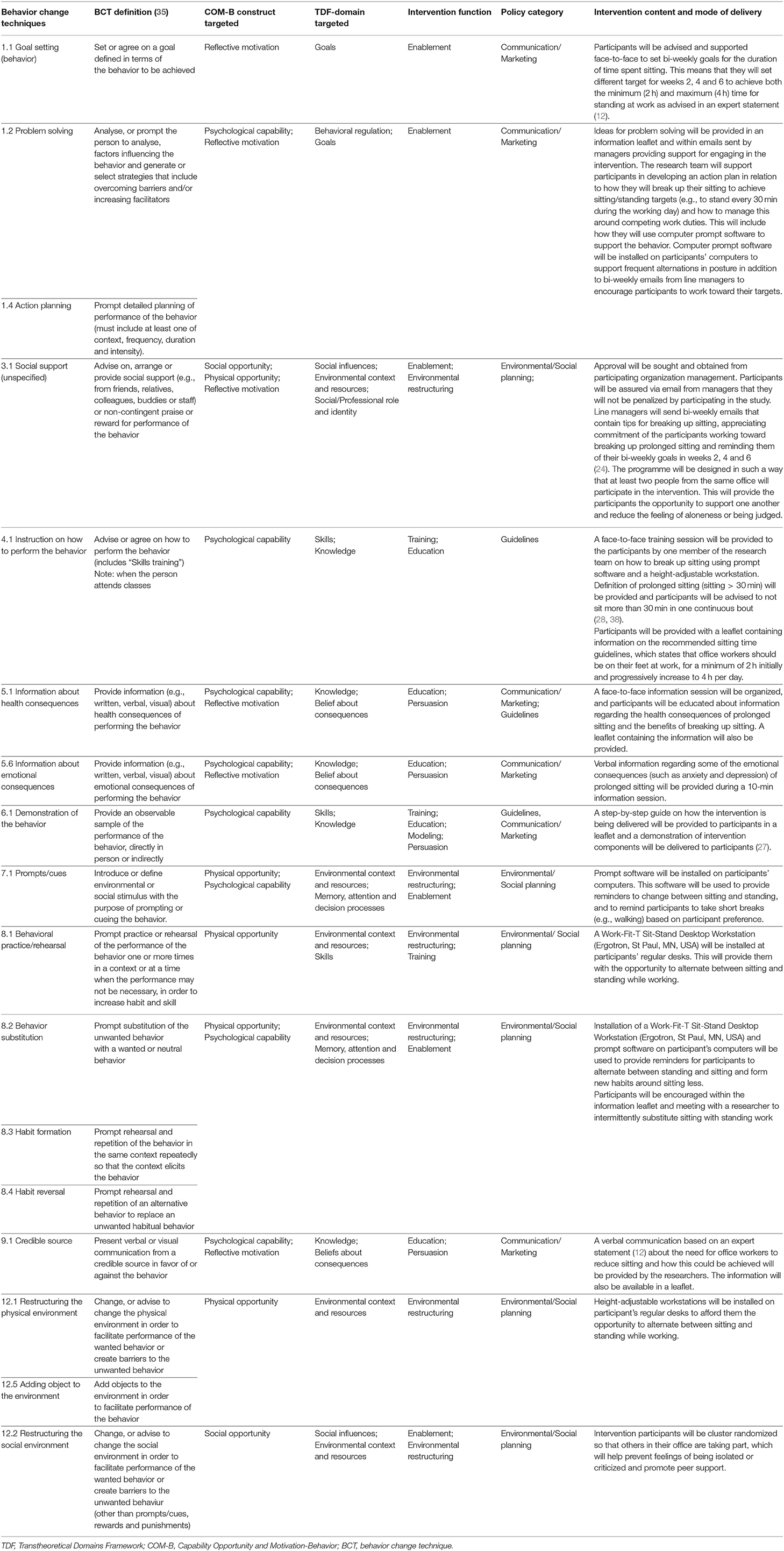
Table 4. Intervention content specified by behavior change techniques mapped onto components of TDF and COM-B model.
Control Group
The control group will continue to work as normal with no changes in their routine or environment. They will complete the same measurements as the intervention group.
Measurements
All measures for both intervention and control groups will be performed at baseline and during the final week of the 8-week study period. Questionnaires will be completed online using Qualtrics survey software (Qualtrics, Provo, Utah, USA) with physical measures taking place at participant's workplaces in a private room.
Primary Outcome Measure: Workplace Sitting Time
The primary outcome measure is sitting time at work, which will be measured using an activPAL3 activity monitor (PAL Technologies Ltd., Glasgow, UK). The activPAL is a portable lightweight device, which is usually worn on the front of the mid-thigh to take measurement of postural information by recognizing periods of lying down/sitting, standing, and stepping based on the inclination of the thigh (39, 40). The activPAL has high reliability and validity for assessing sitting, standing and stepping (41). In this study, the device will be worn on the right thigh for seven full consecutive days (42) at baseline and during the last week of the intervention. The device will be waterproofed by wrapping it within a nitrile sleeve and an adhesive medical dressing. In addition, participants will complete a diary to keep record of their waking time, working hours and time they go to bed while wearing the device to enable calculation of waking and working time wear periods (42). Data from the activPAL will be considered valid only if the device is worn for a minimum of 75% of the workplace monitoring time (39, 40). The sitting time at work variable will be normalized by expressing it as a percentage of the duration of the working day for each participant.
Secondary Outcome Measures
Sitting, Standing and Stepping
In addition to workplace sitting, the activPAL will be used to measure total daily sitting time and the following variables for working hours and across the waking day: time spent in sitting bouts <30 min and ≥30 min, the number of sitting bouts <30 min and ≥30 min, standing time, number of sit-to-upright transitions, number steps and stepping time. Processing PAL (v1.1, University of Leicester, Leicester, UK) will be used to process the data. A validated algorithm (43) will be used to identify valid waking wear data with heat maps being generated to visually check classifications of waking wear time against information provided in the participant's diaries. Waking bout corrections will be made where errors are identified (42). A valid day for daily data will be accepted if wear time is ≥10 h per day; ≥500 steps per day and if not recording > 95% data in one activity category (i.e., sitting, standing or stepping). The resulting data for all primary and secondary activPAL outcome measures will be averaged across all valid days. All time variables for the working day will be normalized by expressing them as a percentage of the work shift duration. All count variables, such as the number of sitting bouts, will be normalized by expressing them as counts per hour.
Adherence Analysis
Adherence to the intervention will be assessed using activPAL data for the working day. Participants will be classified into one of three groups at baseline and follow-up in line with recommendations from an expert statement on reducing sedentary time in the workplace (12): (1) meeting the recommended guidelines (MEETING) for standing and/or stepping at work of ≥4 h per work day, (2) meeting the minimal guidelines (MINIMAL) for standing and/or stepping at work of ≥2 h but <4 h per work day, or (3) sedentary (SED) i.e., not meeting MINIMAL or MEETING guidelines.
Feasibility
Feasibility will be assessed based on recruitment response rate (percentage of people who express interest in participating in the study / number of invitations sent out to individuals x 100) and eligibility rate (percentage of individuals who are screened / number of individuals eligible to take part x 100). Retention rate will be calculated as number of participants who complete 8-week measures / number of participants enrolled into the study x 100. Data completion rates will be calculated as the number of complete datasets for each outcome measure / number of participants enrolled ×100.
Intervention Acceptability
Acceptability of the intervention will be assessed using semi-structured interviews with intervention participants. Data will be analyzed using thematic analysis as well as deductive charting using the APEASE (Acceptability, Practicality, Effectiveness, Affordability, Side effects, Equity) criteria (44).
Productivity
Work productivity will be assessed using measures of absenteeism, presenteeism, and ecological momentary assessment (EMA) at baseline and during week eight of the study. Absenteeism will be measured using self-report at baseline and at the end of the eighth week. Three questions to assess unsanctioned absences will be used from a previous study (45). This includes the number of days off work in the last 2 weeks for sickness (colds, flu, etc.), the number of days off work for mental health reasons (stress, burnout, etc.), and the number of days excused work (e.g., compassionate leave, educational leave, parental leave). Self-reported absenteeism will be calculated by summing the number of days reported across all three questions. Presenteeism will be measured using the 8-item Work Limitations Questionnaire (WLQ), which is a short version of the original 25-item WLQ (46). This version of the WLQ is a reliable and valid alternative to the longer questionnaire (47). The WLQ requires participants to self-report their level of difficulty (or ability) to perform eight specific job demands in the last 2 weeks, with answers grouped into four work limitation scales on time management, physical, mental, and output demands.
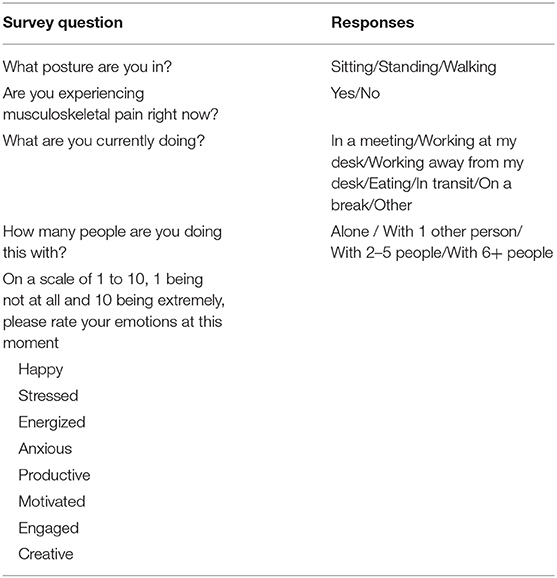
The final measure of productivity is EMA, which has been used previously in a variety of different contexts to measure physical activity and sedentary behavior (48–50). Prompt software will be installed on participant's smartphones to deliver the EMA. Prompts to complete the EMA will occur at random, four times each week day between 9 am to 5 pm (51). In total, participants will be requested to respond to and complete a maximum of 12 EMA surveys in a week. Once a participant has completed 12 surveys, the prompt software will no longer prompt that participant to respond (51). The questionnaire includes items about posture, musculoskeletal issues, task being performed, social interactions, mood, and perception of engagement and productivity (Table 5), typically taking <1 min to complete each time.
Cardiometabolic Risk Biomarkers
All cardiometabolic risk biomarker measures will be taken at baseline and within 5 days post-intervention. This includes the following:
Fasting Blood Glucose and Lipid Profile. Blood samples taken after an overnight fast of at least 10 h using a finger prick method with a lancet (52). Blood samples will be analyzed with a Cholestech LDX analyzer (Cholestech Corp., Hayward, CA., USA) to provide measures of total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides and blood glucose (52).
Blood Pressure. Resting systolic and diastolic blood pressure will be measured on the right arm after resting for at least 10 min in a seated position using an automated blood pressure monitor (Omron HEM705 CP, Omron Healthcare UK Limited, Milton Keynes, UK) validated by the European Society of Hypertension (53). The average of two blood pressure readings with a 2-min rest between each will be used for analysis.
Anthropometry. The standardized procedure of Lohman et al., (54) will be used. Height is measured with a stadiometer (Horltain Ltd., Crymych, UK) to the nearest 0.1 cm, while mass is measured with an electronic weighing scale (Tanita Corp., Tokyo, Japan) to the nearest 0.1 kg. Waist circumference is recorded to the nearest 0.1 cm measured around the waist at navel-level while participants are standing (55, 56). All measures will be taken by the same investigator to avoid inter-investigator variability. Body mass index will be calculated as: weight / height2.
Psychological and Mental Wellbeing
Perceived levels of stress will be measured using the Cohen Perceived Stress Scale (57), which evaluates the unpredictability, uncontrollability and overload of an individual's life, and has high validity and reliability (57). The questionnaire requires participants to rank the frequency of feelings and thoughts using a five-point Likert scale ranging from 1 “Never” to 5 “Very often”. Participant's mood states will be measured using the Positive and Negative Affect Schedule (PANAS), which is a 20-item self-report measure of positive affect and negative affect (58). The questionnaire makes use of words that describe feelings and emotions on a scale from 1 “Very slightly or Not at all” to 5 “Extremely.” The PANAS positive and negative affect scales have high reliability (59). Changes in participants' mental wellbeing will be assessed using the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) (60), which is a 14-item scale that explores feelings and thoughts over the last 2 weeks. This study was registered to obtain permission to use WEMWBS (ID: 448654978) on warwick.ac.uk. The WEMWBS classifies individuals as having low, average or high mental wellbeing and can measure changes over time. The questionnaire asks questions such as “I have been feeling confident” and participants will need to rate themselves on a scale from 1 “None of the time” to 5 “All of the time.” It has been reported to have high test-retest reliability (61).
Statistical Analysis
All statistical analyses will be performed using SPSS (IBM Corp, Armonk, New York, USA). Data will be assessed for normality using the Shapiro-Wilk test owing to the relatively small sample size. Linear mixed models will be used with arm and time as fixed effects, participant ID and cluster ID as random effects, and the baseline value of each variable as a covariate. An additional linear mixed model will be used to compare the effect of standing vs. sitting posture for the EMA variables at follow-up with posture and arm as fixed effects, participant ID and cluster ID as random effects, and the baseline value of each variable as a covariate. The Sidak post-hoc adjustment will be used to adjust for multiple comparisons in all models. Adjustments for missing data will be made using the estimated marginal means procedure of the linear mixed models. If there was a large number of non-normally distributed variables, the bias-corrected and accelerated (BCa) bootstrap method will be used to produce unbiased estimates of the confidence limits for all data (62). Data will be presented as mean and 95% confidence intervals of the bootstrapping procedure. The level of statistical significance will be p ≤ 0.05 for two-tailed tests. Magnitude of effects will be reported as Hedges' g, which is a corrected effect size based on Cohen's d that is suitable for use in small sample sizes of 20 or less per group to produce an unbiased estimate of the population effect size (63). The magnitude of the effect sizes will be considered to be small if they are ≥ 0.2, moderate if ≥ 0.6, and large if ≥ 1.2, using the scale proposed by Hopkins et al. (64). Adherence to the intervention will be assessed using the Wilcoxon signed rank test to compare baseline and follow-up classifications. The standardized test statistic of the Wilcoxon test will be converted to an effect statistic by dividing it by the square root of N (65), which can then be interpreted as r using the scales of Cohen (66) and Hopkins et al. (64).
Discussion
This pilot cluster-randomized controlled trial will evaluate the efficacy of a tailored workplace intervention for reducing and breaking up sitting, productivity, wellbeing and cardiometabolic risk biomarkers. The multi-component intervention protocol was designed using a participatory approach informed by the BCW and identification of intervention functions, policy categories and BCTs using the APEASE criteria to enhance the intervention's adherence and effectiveness. In addition to employing this systematic and evidence-based process for developing the intervention, further strengths of this study include the cluster-randomized design to minimize contamination between groups that are located within the same organization. The study will also be conducted within an ecologically valid office environment, thus enhancing its real-world application. Ecological momentary assessment will be used to assess temporal effects of the intervention on productivity during specific postures and work activities; this may provide important evidence to encourage changes in workplace policy and practice. Potential limitations include sample representativeness of the general office worker population as the study is being conducted only within two organizations. It will also not be possible to determine the effects of each individual strategy used as part of the intervention, which could help in determining their suitability for inclusion in occupational health promotion programmes. Furthermore, physical activity levels prior to taking blood samples will not be standardized. This may be a limitation as there is the potential for carryover effects of prior exercise on glucose and lipid levels.
In conclusion, this study will provide important evidence regarding the efficacy of a systematically developed tailored workplace intervention. This will include evaluating the effects of the intervention on a range of health and work-related outcomes, including an ecological momentary assessment of productivity that has been seldom employed in office workplace studies; this may be key in promoting the adoption and implementation of such interventions in workplace practice and policies. The findings of this study can be used to inform a future fully powered RCT to determine the effectiveness of this multi-component intervention for reducing sitting and improving health in office workers.
Ethics Statement
The studies involving human participants were reviewed and approved by the University of Bedfordshire Institute for Health Research Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
SO contributed to the concept, development of intervention, and drafting the manuscript. DB, DH, and AC contributed to the concept, development of intervention, and manuscript review. All authors reviewed and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Ergotron Inc., for donating the height-adjustable workstations for use in this study.
References
1. Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary behavior research network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Physical Activity. (2017) 14:75. doi: 10.1186/s12966-017-0525-8
2. Kazi A, Duncan M, Clemes S, Haslam C. A survey of sitting time among UK employees. Occup Med.. (2014) 64:497–502. doi: 10.1093/occmed/kqu099
3. Bennie JA, Pedisic Z, Timperio A, Crawford D, Dunstan D, Bauman A, et al. Total and domain-specific sitting time among employees in desk-based work settings in Australia. Aust N Z J Public Health. (2015) 39:237–42. doi: 10.1111/1753-6405.12293
4. Hadgraft NT, Healy GN, Owen N, Winkler EAH, Lynch BM, Sethi P, et al. Office workers' objectively assessed total and prolonged sitting time: Individual-level correlates and worksite variations. Prev Med Rep. (2016) 4:184–91. doi: 10.1016/j.pmedr.2016.06.011
5. Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. (2012) 55:2895–905. doi: 10.1007/s00125-012-2677-z
6. Teychenne M, Costigan SA, Parker K. The association between sedentary behaviour and risk of anxiety: a systematic review. BMC Public Health. (2015) 15. doi: 10.1186/s12889-015-1843-x
7. Bailey DP, Hewson DJ, Champion RB, Sayegh SM. Sitting time and risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. Am J Prev Med. (2019) 57:408–16. doi: 10.1016/j.amepre.2019.04.015
8. Chong F, Wang Y, Song M, Sun Q, Xie W, Song C. Sedentary behavior and risk of breast cancer: a dose–response meta-analysis from prospective studies. Breast Cancer. (2020) 28:48–59. doi: 10.1007/s12282-020-01126-8
9. Biddle SJH, Henson J, Davies MJ, Khunti K, Sutton S, Yates T, et al. Device-assessed total and prolonged sitting time: associations with anxiety. depression, and health-related quality of life in adults. J Affect Disord. (2021) 287:107–14. doi: 10.1016/j.jad.2021.03.037
11. Bull FC, Al-Ansari S, Biddle S, Borodulin K, Buman K, Cardon MP, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
12. Buckley JP, Hedge A, Yates T, Copeland RJ, Loosemore M, Hamer M, et al. The sedentary office: an expert statement on the growing case for change towards better health and productivity. Br J Sports Med. (2015) 49:1357–62. doi: 10.1136/bjsports-2015-094618
13. Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Pedisic Z. Workplace interventions for reducing sitting at work. Cochrane Database Syst Rev. (2018) 12:CD010912. doi: 10.1002/14651858.CD010912.pub5
14. Healy GN, Eakin EG, Owen N, Lamontagne AD, Moodie M, Winkler EAH, et al. A cluster randomized controlled trial to reduce office workers' sitting time: effect on activity outcomes. Med Sci Sports Exerc. (2016) 48:1787–97. doi: 10.1249/MSS.0000000000000972
15. Edwardson CL, Yates T, Biddle SJH, Davies MJ, Dunstan DW, Esliger DW, et al. Effectiveness of the stand more AT (SMArT) work intervention: cluster randomised controlled trial. BMJ. (2018) 363:k3870. doi: 10.1136/bmj.k3870
16. Ben-Ner A, Hamann DJ, Koepp G, Manohar CU, Levine JA. Treadmill workstations: the effects of walking while working on physical activity and work performance. PLoS ONE. (2014) 9:e88620. doi: 10.1371/journal.pone.0088620
17. Ojo SO, Bailey DP, Chater AM, Hewson DJ. The impact of active workstations on workplace productivity and performance: a systematic review. Int J Environ Res Public Health. (2018) 15:417. doi: 10.3390/ijerph15030417
18. Munir F, Biddle SJH, Davies MJ, Dunstan D, Esliger D, Gray LJ, et al. Stand more at work (SMArT Work): using the behaviour change wheel to develop an intervention to reduce sitting time in the workplace. BMC Public Health. (2018) 18:319. doi: 10.1186/s12889-018-5187-1
19. Leask CF, Sandlund M, Skelton DA, Chastin SFM. Co-creating a tailored public health intervention to reduce older adults' sedentary behaviour. Health Edu J. (2017) 76:595–608. doi: 10.1177/0017896917707785
20. Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
21. Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. London: Silverback Publishing (2014).
22. Yang YS, Ryu GW, Han I, Oh S, Choi M. Ecological momentary assessment using smartphone-based mobile application for affect and stress assessment. Health Inf Res. (2018) 24:381–6. doi: 10.4258/hir.2018.24.4.381
23. Engelen L, Held F. Understanding the office: using ecological momentary assessment to measure activities. posture, social interactions, mood, and work performance at the workplace. Buildings. (2019) 9:54. doi: 10.3390/buildings9020054
24. Dunstan DW, Wiesner G, Eakin EG, Neuhaus M, Owen NAD, LaMontagne M, et al. Reducing office workers' sitting time: rationale and study design for the Stand Up Victoria cluster randomized trial. BMC Public Health. (2013) 13:1057. doi: 10.1186/1471-2458-13-1057
25. Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res. (2016) 25:1057–73. doi: 10.1177/0962280215588241
26. National Institute for Health Research. Justifying Samsple Size For a Feasibility Study. (2018). Available online at: https://www.rds-london.nihr.ac.uk/wpcms/wp-content/uploads/2019/02/Justifying-sample-size-for-feasibility-study-updated-22-Feb-2019.pdf (accessed October 28, 2019).
27. Healy GN, Eakin EGAD, LaMontagne N, Owen EAH, Winkler G, Wiesner L, et al. Reducing sitting time in office workers: short-term efficacy of a multicomponent intervention. Prev Med. (2013) 57:43–8. doi: 10.1016/j.ypmed.2013.04.004
28. Danquah IH, Kloster S, Holtermann A, Aadahl M, Bauman A, Ersboll AK, et al. Take a stand!-a multi-component intervention aimed at reducing sitting time among office workers-a cluster randomized trial. Int J Epidemiol. (2017) 46:128–40. doi: 10.1093/ije/dyw009
29. Maylor BD, Edwardson CL, Zakrzewski-Fruer JK, Champion RB, Bailey DP. Efficacy of a multi-component cluster randomised controlled trial to reduce workplace sedentary behaviour in office workers. J Occup Environ Med. (2018) 60:787–95. doi: 10.1097/JOM.0000000000001366
30. Kennedy ADM, Torgerson DJ, Campbell MK, Grant AM. Subversion of allocation concealment in a randomised controlled trial: a historical case study. Trials. (2017) 18. doi: 10.1186/s13063-017-1946-z
31. Michie S, Johnston M, West R, Abraham C, Hardeman W, Wood C. Designing behaviour change interventions: the behaviour change wheel and behaviour change techniques. Ann Behav Med. (2014) 47:S157.
32. Ojo SO, Bailey DP, Brierley ML, Hewson DJ, Chater AM. Breaking barriers: using the behavior change wheel to develop a tailored intervention to overcome workplace inhibitors to breaking up sitting time. BMC Public Health. (2019) 19:1–17. doi: 10.1186/s12889-019-7468-8
33. Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. (2012) 7:37. doi: 10.1186/1748-5908-7-37
34. Atkins L, Francis J, Islam R, O'Connor D, Patey A, Ivers N, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. (2017) 12:77. doi: 10.1186/s13012-017-0605-9
35. Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. (2013) 46:81–95. doi: 10.1007/s12160-013-9486-6
36. Ojo SO, Bailey DP, Hewson DJ, Chater AM. Perceived Barriers and Facilitators to Breaking Up Sitting Time among Desk-Based Office Workers: A Qualitative Investigation Using the TDF and COM-B. Int J Environ Res Public Health. (2019) 16:2903. doi: 10.3390/ijerph16162903
37. West R, Michie S, Atkins L, Chadwick P, Lorencatto F. Achieving Behaviour Change: A Guide For Local Government And Partners. London: Public Health England (2019).
38. Henson J, Davies MJ, Bodicoat DH, Edwardson CL, Gill JMR, Stensel DJ, et al. Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in postmenopausal women: a randomized acute study. Diabetes Care. (2016) 39:130–8. doi: 10.2337/dc15-1240
39. van der Ploeg HP, Merom D, Chau JY, Bittman M, Trost SG, Bauman AE. Advances in population surveillance for physical activity and sedentary behavior: reliability and validity of time use surveys. Am J Epidemiol. (2010) 172:1199–206. doi: 10.1093/aje/kwq265
40. Chau JY, Sukala W, Fedel K, Do A, Engelen L, Kingham M, et al. More standing and just as productive: Effects of a sit-stand desk intervention on call center workers' sitting. standing, and productivity at work in the Opt to Stand pilot study. Prev Med Rep. (2016) 3:68–74. doi: 10.1016/j.pmedr.2015.12.003
41. Grant PM, Ryan CG, Tigbe WW, Granat MH. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med. (2006) 40:992–7. doi: 10.1136/bjsm.2006.030262
42. Edwardson CL, Winkler EAH, Bodicoat DH, Yates T, Davies MJ, Dunstan DW, et al. Considerations when using the activPAL monitor in field-based research with adult populations. J Sport Health Sci. (2017) 6:162–78. doi: 10.1016/j.jshs.2016.02.002
43. Winkler EAH, Bodicoat DH, Healy GN, Bakrania K, Yates T, Owen N, et al. Identifying adults' valid waking wear time by automated estimation in activPAL data collected with a 24 h wear protocol. Physiol Meas. (2016) 37:1653–68. doi: 10.1088/0967-3334/37/10/1653
44. Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. (2019) 11:589–97. doi: 10.1080/2159676X.2019.1628806
45. Gaudine A, Gregory C. The accuracy of nurses' estimates of their absenteeism. J Nurs Manag. (2010) 18:599–605. doi: 10.1111/j.1365-2834.2010.01107.x
46. Lerner D, Amick BC, Rogers WH, Bungay K, Cynn D. The work limitations questionnaire. Med Care. (2001) 39:72–85. doi: 10.1097/00005650-200101000-00009
47. Walker TJ, Tullar JM, Diamond PM, Kohl HW, Amick BC. Validity and reliability of the 8-item work limitations questionnaire. J Occup Rehabil. (2017) 27:576–83. doi: 10.1007/s10926-016-9687-5
48. Runyan JD, Steenbergh TA, Bainbridge C, Daugherty DA, Oke L, Fry BN. A smartphone ecological momentary assessment/intervention app” for collecting real-time data and promoting self-awareness. PLoS ONE. (2013) 8:e71325. doi: 10.1371/journal.pone.0071325
49. Dunton GF. Ecological momentary assessment in physical activity research. Exerc Sport Sci Rev. (2017) 45:48–54. doi: 10.1249/JES.0000000000000092
50. Degroote LD, De Bourdeaudhuij A, Van Dyck I, Crombez DG. Content validity and methodological considerations in ecological momentary assessment studies on physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. (2020) 17:35. doi: 10.1186/s12966-020-00932-9
51. Engelen L, Chaua JY, Burks-Young S, Bauman A. Application of ecological momentary assessment in workplace health evaluation. Health Promot J Austr. (2016) 27:259–63. doi: 10.1071/HE16043
52. Bailey DP, Boddy LM, Savory LA, Denton SJ, Kerr CJ. Choice of activity-intensity classification thresholds impacts upon accelerometer-assessed physical activity-health relationships in children. PLoS ONE. (2013) 8:e57101. doi: 10.1371/journal.pone.0057101
53. El Assaad MA, Topouchian JA, Asmar RG. Evaluation of two devices for self-measurement of blood pressure according to the international protocol: the Omron M5-I and the Omron 705IT. Blood Press Monit. (2003) 8:127–33. doi: 10.1097/00126097-200306000-00006
54. Lohman TG, Roche AF, Martorell R. Anthropometric Standardisation Reference Manual. Champaign, IL: Human Kinetics Books (1988).
55. Jackson C, Lewis K, Conner M, Lawton R, McEachan RRC. Are incremental changes in physical activity and sedentary behaviours associated with improved employee health?: a 12-month prospective study in five organisations. Int J Workplace Health Manag. (2014) 7:16–39. doi: 10.1108/IJWHM-03-2013-0013
56. Boyle T, Vallance JK, Buman MP, Lynch BM. Reallocating time to sleep. sedentary time, or physical activity: associations with waist circumference and body mass index in breast cancer survivors. Cancer Epidemiol Biomarkers Prev. (2017) 26:254–60. doi: 10.1158/1055-9965.EPI-16-0545
57. Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. Soc Psychol Health. (1988) 31–67.
58. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect - the PANAS scales. J Pers Soc Psychol. (1988) 54:1063–70. doi: 10.1037/0022-3514.54.6.1063
59. Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): Construct validity. measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol. (2004) 43:245–65. doi: 10.1348/0144665031752934
60. Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. (2007) 5:63. doi: 10.1186/1477-7525-5-63
61. Stewart-Brown SL, Platt S, Tennant A, Maheswaran H, Parkinson J, Weich S, et al. The warwick-edinburgh mental well-being scale (WEMWBS): a valid and reliable tool for measuring mental well-being in diverse populations and projects. J Epidemiol Commun Health. (2011) 65:A38–9. doi: 10.1136/jech.2011.143586.86
62. Kelley K. The effects of nonnormal distributions on confidence intervals around the standardized mean difference: bootstrap and parametric confidence intervals. Educ Psychol Meas. (2005) 65:51–69. doi: 10.1177/0013164404264850
63. Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. (2013) 4:863. doi: 10.3389/fpsyg.2013.00863
64. Hopkins WG, Marshall SW, Batterham AM, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. (2009) 41:3–12. doi: 10.1249/MSS.0b013e31818cb278
65. Fritz COM, Richler PEJJ. Effect size estimates: current use. calculations, and interpretation. J Exp Psychol Gen. (2012) 141:17. doi: 10.1037/a0024338
Keywords: sedentary behavior, Behavior Change Wheel, intervention, desk-based employees, office workers, pilot study, protocol
Citation: Ojo SO, Bailey DP, Chater AM and Hewson DJ (2022) Workplace Intervention for Reducing Sitting Time in Sedentary Workers: Protocol for a Pilot Study Using the Behavior Change Wheel. Front. Public Health 10:832374. doi: 10.3389/fpubh.2022.832374
Received: 09 December 2021; Accepted: 03 February 2022;
Published: 12 April 2022.
Edited by:
Yan Li, Icahn School of Medicine at Mount Sinai, United StatesReviewed by:
Sophie Carter, York St John University, United KingdomSiti Munira Yasin, MARA University of Technology, Malaysia
Copyright © 2022 Ojo, Bailey, Chater and Hewson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel P. Bailey, ZGFuaWVsLmJhaWxleUBicnVuZWwuYWMudWs=; Angel M. Chater, YW5nZWwuY2hhdGVyQGJlZHMuYWMudWs=; YS5jaGF0ZXJAdWNsLmFjLnVr
 Samson O. Ojo
Samson O. Ojo Daniel P. Bailey
Daniel P. Bailey Angel M. Chater
Angel M. Chater David J. Hewson
David J. Hewson