
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 04 April 2022
Sec. Public Mental Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.829362
Background: The COVID-19 pandemic and the associated infection prevention and control measures had a negative impact on the mental health of many people. In the United Arab Emirates (UAE), infection control measures implemented after March 24th, 2020, placed necessary restrictions on people's freedom of movement.
Aim: This study aimed to assess the association between levels of daytime vs. nighttime outdoor activity and mental health among a sample of UAE residents during the lockdown period.
Method: An opportunity sample of 245 participants completed an online survey assessing levels of depression, somatic symptoms, daytime and nighttime activity levels.
Results: Multivariate logistic regression revealed that daytime activity, but not nighttime activity, was associated with a lower risk of clinically significant depressive and somatic symptomatology.
Conclusion: The association of better mental health with daytime not nighttime outdoor activity could be possibly attributed to vitamin D, but further studies are needed to confirm this speculation.
The COVID-19 pandemic disrupted many aspects of routine life, adversely impacting physical and mental health, social activity, and economic status (1). Once the World Health Organization declared the disease a global pandemic in March 2020, many countries began implementing stringent infection prevention and control measures. Attempting to curtail the transmission of the virus and to prevent deaths and the catastrophic over-burdening of their healthcare systems, several governments including that of the United Arab Emirates (UAE) UAE, placed restriction on freedom of movement via the implementation of population-wide curfews and lockdowns (2, 3). The UAE enforced mandatory masking, social distancing and quarantine, suspended air travel, and closed all educational and public entities, except for vital services such as supermarkets, pharmacies, and healthcare facilities. Additionally, the UAE implemented a nation-wide 8 pm to 6 am curfew, requiring people to remain in their homes or face significant financial penalties.
The pandemic and the above-mentioned infection prevention and control measures have adversely affected mental health (4). At the most basic level, the grief related to COVID-19 deaths, and the fear of infection are highly likely to lead to an elevated risk of developing an associated mental health problem. In addition to the direct fear of the virus, the essential limitations on the freedom-of-movement, including social/physical distancing and quarantine, can also have undesirable impacts on psychological wellbeing (4).
Recent research across different countries worldwide and in the UAE have reportednegative changes in diet during the lockdown including consuming more calories, eating more snacks and less of fresh fruits and vegetables, and hence gaining weight (5–7). In addition, physical activity levels; which were already low in the UAE before COVID-19; have been reduced and negatively impacted by quarantine (8). COVID-19 had also increased the level of anxiety and depressive mental health symptoms drastically and unfavorably affected people's sleeping patterns along with dietary habits and physical activity levels (4, 9).
Several researchers have recently highlighted that the immune system could be supported by important micronutrients which could lower the risk of COVID-19 infection (10). Among those, vitamin D is the most attractive for research. An adequate intake of vitamins is crucial to fight against infections and inflammations, especially during COVID-19 pandemic. One important vitamin is vitamin D, which is well known to boost the immune system and to modulate the body's response to infections (11). Therefore, in such critical times a healthy balanced lifestyle containing vitamins and minerals is essential to overcome Covid19 and strengthen immunity. When infected by COVID-19 virus, the body increases the release of pro-inflammatory cytokines and C-reactive protein (12, 13). Vitamin D reduces the severity of the COVID-19 infection by minimizing the cytokine storm caused by the innate system. Based on the most recent evidence, vitamin D supplementation can reduce risk and severity of respiratory infections (14). Casual sun exposure by individuals could secure adequate vitamin D levels (15, 16). There is sufficient evidence during the COVID-19 pandemic to support recommending vitamin D given that many people are spending more time indoors and may not get the sufficient amount of vitamin D they need for optimal bone and overall health (17).
In this study, we aimed to examine the relationship between outdoor physical activity levels (daytime vs. nighttime) and mental health during COVID-19 lockdown among an opportunity sample of citizens and residents of the UAE. Our research could contribute important findings about mental health in the UAE and guide future intervention studies given the high prevalence of depression in the gulf region (18).
This cross-sectional study utilized an online survey to assess mental health (depressive and somatic symptomatology) in a community sample of adults (N = 245) in the UAE between April 8th and April 18th, 2020. Respondents completed standardized assessments for symptom measures of depression and somatization, along with psychosocial and demographic variables including daytime and nighttime physical activity levels that might potentially influence such symptoms. Moreover, data about the use of vitamin D supplements during the Curfew was recorded. Bivariate and multivariate associations were calculated for the main study variables.
A-priori sample size estimates for regression analysis (19) with a medium effect size suggested a sample of size of 103. The final sample of participants (N = 245) were an opportunity sample recruited through the social media and email networks of UAE's National Program for Happiness and Wellbeing. For inclusion, participants were required to be adult (at least 18 years old) residents/citizens of the UAE residing in the country during April 2020. Participants who did not complete the battery fully (n = 8) were excluded. The final sample included both genders (199 females and 46 males) and broadly reflected the multiethnic and international nature of the UAE population. Ages ranged from 18 to 73 with a mean age of 33.47 ± 12.88. All participants undertook a survey that involved questions related to mental health status assessment (depression and somatization), demographics and psychosocial variables.
The survey was a self-report survey [rarely vs. frequently (yes/no), do you do this?]. All demographic and COVID-related measures were available in the two main languages commonly used in the UAE, namely Arabic and English. The developed survey was part of a larger ongoing national survey exploring the impact of COVID-19 in the UAE. Ethical clearance was obtained from Zayed University Research Ethics Committee (R201213) and from the Ministry of Health and Prevention's Research Ethics Committee (MOHAP/DXB-REC/ MMM/No. 49/2020). Data collection took place online and all participants consented prior to answering the survey.
The COVID-related items were adapted from Shevlin et al. (20). Moreover, some items related to outdoor activity were adapted from the previously validated Sun Avoidance Inventory which was an indicator of vitamin D lifestyle related factors among the UAE population (21–23). The questions were related to being on outdoor balcony, in a garden or yard, on a roof or terrace, walking or exercising outdoors. All items were duplicated for both daytime and nighttime sections.
The PHQ-8 (24) is a commonly utilized standardized tool for assessing the prevalence and severity of depressive symptoms. The psychometric properties of the PHQ-8 scores had been widely supported and it consists of eight questions that examine the frequency of depressive symptoms over past 2 weeks. Responses can range from 0 to 3 (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day). Total added scores range from 0 to 24 with scores below 5 indicating absence of considerable depressive symptoms. The presence of moderate depression (clinically significant depressive symptoms) was noted when the cut-off score of ≥10 was exceeded up to 14 as scores of 15 and above indicated severe levels of depression. The reliability of the scale among the current sample was excellent (α = 0.915).
We used the PHQ15 to assess somatic symptoms (25). The inclusion of this measure follows the finding that psychological symptoms are often somatized, some individuals are more likely to experience or report distress in somatic terms (vague aches and pains, insomnia, headaches etc.,) rather than the psychological ones (26). Previous research suggests that among Arab populations depression is very frequently described in terms of psychosomatic symptoms (27). The PHQ-15 is a 15-item self-report measure, asking respondents about the degree of distress in relation to physical health problems (insomnia, headaches, stomach aches etc.) over the last 2 weeks. All items are rated on a 3-point Likert scale: 0 (not bothered at all) to 2 (bothered a lot). We excluded the item focused on ‘menstrual problems' due to its gender-specific content. The total scale scores were used, where scores of 10 and above are viewed as clinically significant. Multiple previous studies attest to the reliability and validity of the PHQ-15 (28).
The United Arab Emirates (UAE) enacted several infection prevention and control measures, including social distancing, quarantine, curfews, the closure of educational/recreational facilities, and the cessation of in and outbound passenger air travel. Supplementary Table 1, based on UAE governmental sources, provides a timeline of the nation's primary infection prevention and control measures around the time that this study was planned and undertaken. Adapted from Thomas et al., 2020 (29).
Bivariate and multiple logistic regressions were done with R (R Core Team, 2020), using generalized linear models in the base package. Two binary logistic regression models were used to predict Somatization (PHQ-15) and Depression (PHQ-8), computing bivariate odds ratios (OR) and multivariate adjusted odds ratios (AOR) for all predictor variables. The predictor variables were age, gender, citizenship, outdoor activity (day and night) and VTD supplement use.
Daytime outdoor activity levels (M = 3.97 SD = 3.72) were higher than nighttime activity levels (M = 3.51, SD = 3.96); indicating that participants were more engaged in daytime outdoor activity as compared to nighttime. This difference was statistically significant t (241) = 1.86, p = 0.032. Table 1 details the mean score for each outdoor activity. Walking outdoors was the most highly endorsed outdoor activity for both daytime and nighttime.
In response to the question “To reduce your risk of being infected by the coronavirus COVID-19 have you recently taken vitamin D supplement”. Participants gave the following responses No (N = 142, 56%), Occasionally (N = 38, 15.2%) and Regularly (N = 67, 26.8%).
Psychopathology scores were elevated with 47.95% of the participants scoring above the cut-off of the PHQ-8 for depressive symptoms. Similarly, high levels of clinically significant somatic symptomatology were also observed with 34.31% of participants scoring above the cut-off of the PH-Q15 for somatic symptoms. Table 2 details the mean score for psychopathology symptoms of depression and somatization for the study participants.
Only outdoor activity in the daytime was associated with lower levels of depression and somatization as revealed by the significant negative correlation with PH-Q8 depression and PH-Q15 somatization scores (p <.01 and p <.001, respectively). Table 3 details the bivariate correlations between the study's key variables. Nighttime outdoor activity and use of vitamin D supplements however were uncorrelated with levels of psychopathology.
The results of bivariate and multiple logistic regression analyses to predict likelihood of depression (PHQ-8) in Table 4 reveal the significance of prediction with daytime outdoor activity levels (p < 0.01).
Low levels of daytime outdoor activity were associated with higher risk of clinically significant depressive symptoms. This effect remained even after controlling for age, gender and citizenship status. Figure 1 details the AOR for all variables in the multivariate logistic regression model.
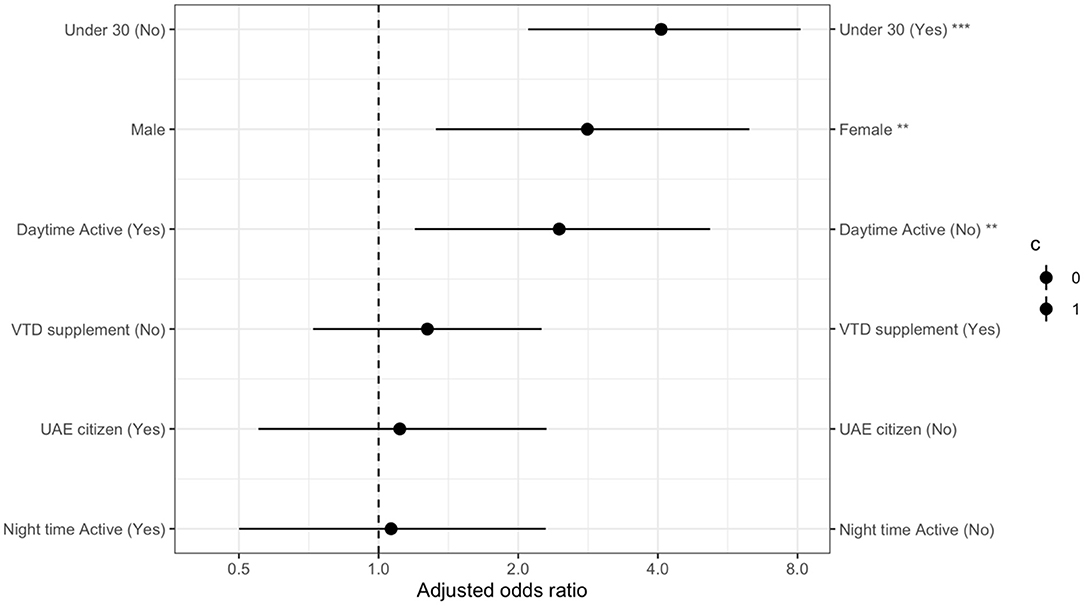
Figure 1. Multivariate logistic regression model analysis for higher risk of clinically significant depressive symptoms with adjusted odds ratios for all variables.
The results of the bivariate and multivariate analysis for the risk of developing clinically significant levels of somatic symptoms are shown in Table 5. The data demonstrates the significance of prediction with only daytime outdoor activity levels (p < 0.05).
Low levels of daytime outdoor activity were also associated with higher risk of clinically significant somatic symptoms. This effect remained even after controlling for age, gender, and citizenship status. Figure 2 details the AOR ratios for all variables in the multivariate logistic regression model.
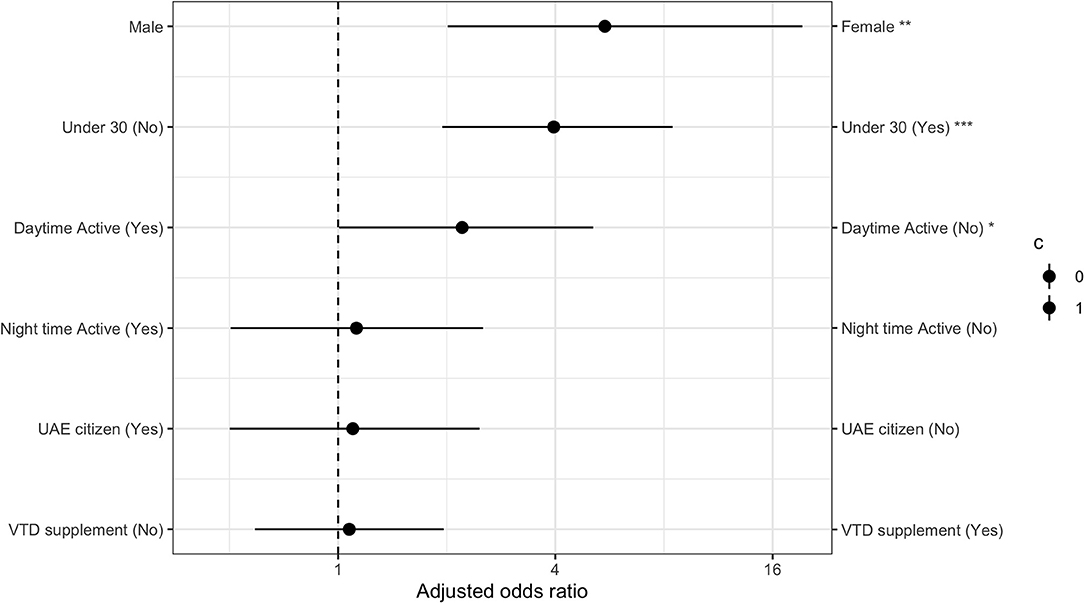
Figure 2. Multivariate logistic regression model analysis for higher risk of clinically significant somatic symptoms with adjusted odds ratios for all variables.
The study results suggest that mental health among the UAE population had been adversely affected during the COVID-19 curfew period. Psychopathology scores were elevated beyond pre-pandemic norms, with close to half the participants scoring above the cut-off of the PHQ-8. Similarly, high levels of somatic symptomatology were also reported on the PHQ-15. Such results during a time of crisis were expected since the current COVID-19 pandemic has influenced the psychological health of individuals all over the world due to the necessary infection-prevention and control measures, such as lockdowns. Several other studies concur, each reporting alarmingly elevated rates of mental conditions during the COVID-19 (30–32) and worsened clinical symptoms for those who already suffered from mental conditions (33).
In the present study, citizens (Emirati nationals) generally reported higher rates of depression and somatization compared to non-Emirati residents. They were also more likely to score above the PHQ8 and PHQ15 cut-offs. This effect, however, disappears when we adjust for other variables (age in particular). The Emirati section of the sample is significantly younger than the non-Emirati resident counterpart, hence age rather than nationality is associated with elevated symptoms of somatization and depression. Similar age-related findings had been reported in other national (34) and international studies (20) undertaken around the same time.
It had been widely demonstrated that moderate to vigorous physical activity can improve overall health, encompassing both physical and mental wellbeing (35). Ample research has shown that physical activity could enhance sleep quality and reduce risks of developing stress, anxiety and depression as it increases the level of endorphins, dopamine, adrenaline, myokines, serotonin and endocannaboids (36, 37). meta A meta-analysis of prospective studies encompassing 1,837,794 person-years concluded that physical activity was a protective factor against depression across different age groups and geographical locations across the world (38). Similarly, physical activity was shown to confer protection against anxiety after examining evidence from studies with 3,57,424 person-years (39).
During COVID-19 pandemic, physical activity had been reported to be associated with less depression and anxiety across different parts of the globe (40). Conversely, the reduction in physical activity levels due to COVID-19 lockdowns had a negative impact on overall health and wellbeing (41–45). The findings in our study are in line with reports from other studies examining the life style behaviors of individuals in the Middle East and North Africa (MENA) region during quarantine (46). A study by Cheikh Ismail et al. (2020) demonstrated that the UAE population had experienced higher levels of anxiety and depressive mental health symptoms during COVID-19 along with unfavorable sleeping patterns, eating habits, and physical activity levels (47). A similar study by Abouzid et al., (2021), showed a remarkable increase in sedentary lifestyle and reduction in physical activities due to people's tendency to spend more time on social media and television during quarantine (46).
In our current study, daytime activity, but not nighttime activity, was significantly correlated with lower depressive and somatic symptoms. Multivariate regression analysis revealed that outdoor physical activity; during the day; was a strong predictor of both depression and somatization and that such power remained upon adjustment for other variables. During the COVID-19 pandemic, confinement and spending more time indoors restricted outdoor physical activity and shifted the life styles of many individuals toward being more sedentary. Such changes were associated with a reduced ability to fight the viral infection and also negative effects on the brain health and immune system (48). Specific Outdoor physical activity in natural environments was correlated with reduced odds of depression when compared to inactivity and indoor activity among 88,522 individuals (49). Although the mechanism behind this finding is not fully elucidated, it is suggested that exposure to sunlight and bonding with nature might be a contributing factor since it could create a more pleasant experience (50). A systematic review conducted by Thompson et al., (2011) tested the hypothesis that there are additional benefits attained from performing physical activity outdoors in natural spaces vs. indoor settings. The review demonstrated some additional positive effects on self-reported mental wellbeing immediately following exercise in nature which are not seen following the same exercise indoors (51).
Our findings regarding the robust correlation of lower levels of depression and somatization with daytime but not nighttime outdoor physical activity could be interpreted in the context of other results from previous research in the UAE regarding depression, vitamin D deficiency and sun avoidance which demonstrated that high levels of sun avoidance are associated with higher risk of both depression and vitamin D deficiency (22, 23). The fact that nighttime outdoor activity levels did not show a correlation with depressive and somatic symptoms further makes this suggestion about a possible role for vitamin D more plausible.
Good nutrition and active lifestyle are the two chief elements in maintaining a good immunity to fight the SARS-CoV-2 virus. However, outdoor activity and access to healthy food have been impaired across several countries by either total or partial lockdowns during the COVID-19 pandemic. This had consequently reduced people's intake of vitamins and minerals and their sunlight exposure. Ultraviolet B (UV-B) light from sunlight exposure is the main factor for producing the active form of vitamin D in the body (52). As more than 80% of the body's requirement of vitamin D is supplied from UV-B sunlight exposure (53, 54) the lowered levels of outdoor activities due to COVID-19 lockdowns might hence contribute to a higher prevalence of vitamin D deficiency (55).
Vitamin D has an important physiological role in the brain including brain development, synaptic plasticity, neuroprotection, neurotransmission, and neuroimmunomodulation (56). studies have found low levels of vitamin D in patients with major depressive disorder (MDD) and bipolar disorder (BD) (57–59); however, its clinical and therapeutic effects on mental health is still under study (60, 61).
Interestingly, there was an increase in the intake of dietary supplements during the COVID-19 pandemic, particularly vitamin D supplement intake (increase rate of 31.8%) (46). In our study, we did not determine the increase rate prior to COVID-19, however 31.6% of the participants were taking Vitamin D (D3) supplements regularly/occasionally during the pandemic. The available over the counter dose in the country ranges from 1,000 to 50,000 IU for vitamin D. Previous studies from the UAE reported a low level of dietary and supplementary intake for vitamin D among the UAE population prior to COVID-19 (22, 62–64). Despite the abundance of sunshine in the UAE, there is an alarmingly high prevalence (around 80% among the population) for vitamin-D deficiency due to multiple reasons including cultural sartorial, religious and habitual which mainly reduce sun exposure and limit obtaining adequate vitamin D through UV-B (63).
A study by Di Nicola et al., 2020, showed that low 25-hydroxyvitamin D serum levels were significantly correlated with greater mental disturbance in patients with mood illnesses during the COVID-19 pandemic (65). Similar results were reported by Chen et al. demonstrated a significant association between low serum 25 (OH) D levels and poor mental health in a large sample of young adults (66). Moreover, many studies have found some positive impacts of vitamin D supplementation in individuals with clinical depression and vitamin D deficiency (60, 61, 67). Despite the positive associations obtained from observational studies, a large longitudinal randomized trial that has recently studied the effect of treatment with vitamin D3 supplementation on the rate and frequency of depression didn't achieve any significant difference in clinically relevant depressive symptoms or mood scores (61). This warrants further investigation and additional trials using different dosages and regimen.
In this study, we propose a preliminary understanding of the psychosocial factors associated with elevated levels of depression and somatization among the UAE population during COVID-19 pandemic in the context of daytime vs. outdoor activity levels. To our knowledge, this is the first study in the UAE to ever examine the relationship between outdoor physical activity levels (daytime vs. nighttime) and mental health during COVID-19 lockdown among citizens and residents of the UAE. Such studies aiming to assess the impact of the pandemic on mental health and wellbeing are essential in order to fully decipher the implications and outcomes and pave way for the development of future intervention programs.
Despite the interesting results of this study, there are several important limitations. Given the need for a prompt data collection method to complete the study within a critical period during a rapidly evolving pandemic, we resorted to snowball and convenience sampling using internet and social media platform to invite participants. Such a sampling method might introduce bias and limit the generalizability of the findings. Hence, the results might not be fully projected to be representative of all the UAE population. Moreover, the serum 25 (OH) D levels which are frequently used as clinical indicators for the assessment of vitamin D status had not been measured. Another limitation pertains to data about sun exposure which was estimated by outdoor activity, however, sartorial style during exposure had not been recorded. Nevertheless, the findings of our study should encourage other researchers to further investigate the role of vitamin D as a potential resilience factor associated with psychological wellbeing during COVID-19 pandemic and recovery phase.
Our study attempted to explore the impact of COVID-19 on mental health of population in the UAE. The data in our study had demonstrated that daytime outdoor activity levels during COVID-19 curfew in the UAE were significantly associated with lower depressive and somatic symptoms. Nighttime outdoor activity levels in contrast where not correlated with depression and somatic symptoms. We speculate that differences in results between daytime and nighttime outdoor activities could be attributed tothe positive effects of bonding with nature and exposure to sun which raises the levels of vitamin D. Such assumption however, requires much further investigation and additional research.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Zayed University and Ministry of Health. The patients/participants provided their written informed consent to participate in this study. Ethical clearance was obtained from Zayed University Research Ethics Committee (R201213) and from the Ministry of Health and Prevention's Research Ethics Committee (MOHAP/DXB-REC/MMM/No. 49/2020).
JT and FA led the concept and design and initial draft write up. SK and NE contributed to the discussion. All the authors contributed to writing the draft manuscript and read and agreed to the published version of the manuscript.
This study was funded by the Cluster Grant R21001 awarded by Zayed University, United Arab Emirates. The funding body was not involved in the design of the study and collection, analysis, and interpretation of data or in writing the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the participants of the study for their time and effort to advance our understanding of mental health impact during COVID-19 lockdown. We also are grateful to Ms. Sirine Zahran for her help with editing.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.829362/full#supplementary-material
1. Barro RJ, Ursúa JF, Weng J. The Coronavirus and the Great Influenza Pandemic: Lessons From the “Spanish flu” for the Coronavirus's Potential Effects on Mortality and Economic Activity. Cambridge, MA: National Bureau of Economic Research (2020).
2. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel med. (2020) 27:taaa020. doi: 10.1093/jtm/taaa020
3. Koh D. COVID-19 lockdowns throughout the world. Occup Med. (2020) 70:322. doi: 10.1093/occmed/kqaa073
4. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020). doi: 10.1016/S2215-0366(20)30168-1
5. Deschasaux-Tanguy M, Druesne-Pecollo N, Esseddik Y, Szabo de Edelenyi F, Alles B, Andreeva VA, et al. Diet and physical activity during the COVID-19 lockdown period (March-May 2020): results from the French NutriNet-Sante cohort study. medRxiv. (2020) 924–38. doi: 10.1101/2020.06.04.20121855
6. Zachary Z, Brianna F, Brianna L, Garrett P, Jade W, Alyssa D, et al. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes Res Clin Pract. (2020) 210–6. doi: 10.1016/j.orcp.2020.05.004
7. Radwan H, Al Kitbi M, Hasan H, Al Hilali M, Abbas N, Hamadeh R, et al. (2021). Indirect health effects of COVID-19: unhealthy lifestyle behaviors during the lockdown in the United Arab Emirates. Int J Environ Res Public Health. 18:1964. doi: 10.3390/ijerph18041964
8. Yammine K. The prevalence of physical activity among the young population of UAE: a meta-analysis. Perspect public health. (2017) 137:275–80. doi: 10.1177/1757913916675388
9. Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Social Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
10. Gombart AF, Pierre A, Maggini S. A review of micronutrients and the immune system–working in harmony to reduce the risk of infection. Nutrients. (2020) 12:236. doi: 10.3390/nu12010236
11. Rossetti M, Martucci G, Starchl C, Amrein K. Micronutrients in sepsis and COVID-19: a narrative review on what we have learned and what we want to know in future trials. Medicina. (2021) 57:419. doi: 10.3390/medicina57050419
12. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirusinfected pneumonia in wuhan, China. J Am Med Assoc. (2020) 1061–9. doi: 10.1001/jama.2020.1585
13. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020). doi: 10.1016/S0140-6736(20)30183-5
14. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. (2020) 12:988. doi: 10.3390/nu12040988
15. Dawodu A, Dawson KP, Amirlak I, Kochiyil J, Agarwal M, Badrinath P. Diet, clothing, sunshine exposure and micronutrient status of Arab infants and young children. Ann Trop Paediatr. (2001) 21:39–44. doi: 10.1080/02724930124951
16. Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. (2004) 80(Suppl. 6):1678S−88S. doi: 10.1093/ajcn/80.6.1678S
17. Grigoriou EV, Trovas G, Papaioannou N, Makras P, Kokkoris P, Dontas I, et al. Serum 25-hydroxyvitamin D status, quantitative ultrasound parameters, and their determinants in Greek population. Arch Osteoporos. (2018) 13:111. doi: 10.1007/s11657-018-0526-5
18. Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJL, et al. Burden of 392 depressive disorders by country, sex, age, and year: findings from the global burden of disease 393 study 2010. PLoS Med. (2013) 10:e1001547. doi: 10.1371/journal.pmed.1001547
19. Soper D.S. A-priori Sample Size Calculator for Multiple Regression. (2020). Available online at: https://www.danielsoper.com/statcalc (accessed September 16, 2021).
20. Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L. Anxiety, Depression, Traumatic Stress, COVID-19 Related Anxiety in the UK General Population During the COVID-19 Pandemic. PsyArXiv (2020). Available online at: https://psyarxiv.com (accessed September 16, 2021).
21. Thomas J, Alanouti F, Campbell C, Al Ameri S. Exploring sun avoidant attitudes and behaviors in the United Arab Emirates. Social Behavior and Personality: An Int J. (2010) 38:1111–8. doi: 10.2224/sbp.2010.38.8.1111
22. Justin Thomas Fatme Al Anouti Sara Al Hasani Laila Abdel-Wareth & Afrozul Haq Sunshine Sadness and Seasonality. 25-Hydroxyvitamin D, and depressive symptoms in the United Arab Emirates (UAE). Int J Ment Health Promot. (2011) 13:23–6. doi: 10.1080/14623730.2011.9715647
23. Al Anouti F, Thomas J, Abdel-Wareth L, Rajah J, Grant WB, Haq A. Vitamin D deficiency and sun avoidance among university students at Abu Dhabi, United Arab Emirates. Dermatoendocrinol. (2011) 3:235–9. doi: 10.4161/derm.3.4.16881
24. Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. (2009) 114:163–73. doi: 10.1016/j.jad.2008.06.026
25. Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. (2002) 64:258–66. doi: 10.1097/00006842-200203000-00008
26. Keedwell P. How Sadness Survived:The Evolutionary Basis of Depression. Radcliffe: Oxford (2008).
27. Hinz A, Ernst J, Glaesmer H, Brähler E, Rauscher FG, Petrowski K, Kocalevent RD. Frequency of somatic symptoms in the general population: Normative values for the Patient Health Questionnaire-15 (PHQ-15). Journal of psychosomatic research, 96, 27-31. doi: 10.1016/j.jpsychores.2016.12.017
28. Becker S. M. (2004). Detection of somatization and depression in primary care in Saudi Arabia. Soc Psychiatry Psychiatr Epidemiol. (2017) 39:962–6. doi: 10.1007/s00127-004-0835-4
29. Thomas J, Barbato M, Verlinden M, Gaspar C, Moussa M, Ghorayeb J, et al. Psychosocial correlates of depression and anxiety in the United Arab Emirates during the COVID-19 pandemic. Front Psychiatry. (2020) 11:564172. doi: 10.3389/fpsyt.2020.564172
30. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
31. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
32. Sani G, Janiri D, Di Nicola M, Janiri L, Ferretti S, Chieffo D. Mental health during and after the COVID-19 emergency in Italy. Psychiatry Clin Neurosci. (2020) 74:372. doi: 10.1111/pcn.13004
33. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID19 epidemic. Lancet Psychiatry. (2020) 7:e21. doi: 10.1016/S2215-0366(20)30090-0
34. Barbato M, Thomas J. In this together: psychological wellbeing of foreign workers in the United Arab Emirates during the COVID-19 pandemic. Int J Psychol. 56:825–33. doi: 10.1002/ijop.12786
35. CDC. Benefits of physical activity. (2021). Centers for Disease Control and Prevention. Available online at: https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm (accessed November 30, 2021).
36. Ströhle A. Physical activity, exercise, depression and anxiety disorders. J Neural Transm. (2009) 116:777–84. doi: 10.1007/s00702-008-0092-x
37. Di Liegro CM, Schiera G, Proia P, Di Liegro I. Physical activity and brain health. Genes. (2019) 10:720. doi: 10.3390/genes10090720
38. Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a -analysis of prospective cohort studies. Am J Psychiatry. (2018) 175:631–48. doi: 10.1176/appi.ajp.2018.17111194
39. Schuch FB, Stubbs B, Meyer J, Heissel A, Zech P, Vancampfort D, et al. Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress Anxiety. (2019) 36:846–58. doi: 10.1002/da.22915
40. Wolf S, Seiffer B, Zeibig JM, Welkerling J, Brokmeier L, Atrott B, et al. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? A rapid systematic review. Sports Med. (2021) 51:1771–83. doi: 10.1007/s40279-021-01468-z
41. Lesser IA, Nienhuis CP. The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int J Environ Res Public Health. (2020) 17:3899. doi: 10.3390/ijerph17113899
42. Maugeri G, Castrogiovanni P, Battaglia G, Pippi RD, Agata V, Palma A, et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. (2020) 6:e04315. doi: 10.1016/j.heliyon.2020.e04315
43. Hosen I, Al-Mamun F, Mamun MA. Prevalence and risk factors of the symptoms of depression, anxiety, and stress during the COVID-19 pandemic in Bangladesh: a systematic review and meta-analysis. Glob Ment Health. (2021) 8:e47. doi: 10.1017/gmh.2021.49
44. Auny FM, Akter T, Guo T, Mamun MA. How has the COVID-19 pandemic changed bmi status and physical activity - its associations with mental health conditions, suicidality: an exploratory study. Risk Manag Healthc Policy. (2021) 14:2527–36. doi: 10.2147/RMHP.S308691
45. Hosen F, Al Mamun F, Mamun MA. The role of sociodemographics, behavioral factors, and internet use behaviors in students' psychological health amid COVID-19 pandemic in Bangladesh. Health Sci Rep. (2021) 4:e398. doi: 10.1002/hsr2.398
46. Abouzid M, El-Sherif DM, Eltewacy NK, Dahman NBH, Okasha SA, Ghozy S, et al. Influence of COVID-19 on lifestyle behaviors in the Middle East and North Africa region: a survey of 5896 individuals. J Transl Med. (2021) 19:129. doi: 10.1186/s12967-021-02767-9
47. Cheikh Ismail L, Osaili TM, Mohamad MN, Al Marzouqi A, Jarrar AH, Abu Jamous DO, et al. Eating habits and lifestyle during COVID-19 lockdown in the United Arab Emirates: a cross-sectional study. Nutrients. (2020) 12:3314. doi: 10.3390/nu12113314
48. Woods JA, Hutchinson NT, Powers SK, Roberts WO, Gomez-Cabrera MC, Radak Z, et al. The COVID- 19 pandemic and physical activity. Sports Med Health Sci. (2020) 2:55–64. doi: 10.1016/j.smhs.2020.05.006
49. Matias TS, Lopes MVV, da Costa BGG, Silva KS, Schuch FB. Relationship between types of physical activity and depression among 88,522 adults. J Affect Disord. (2022) 297:415–20. doi: 10.1016/j.jad.2021.10.051
50. Kelly P, Williamson C, Niven AG, Hunter R, Mutrie N, Richards J. Walking on sunshine: scoping review of the evidence for walking and mental health. Br J Sports Med. (2018) 52:800–6. doi: 10.1136/bjsports-2017-098827
51. Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol. (2011) 45:1761–72. doi: 10.1021/es102947t
52. Lippi G, Cervellin G, Danese E. Indoor tanning a Gianus Bifrons: vitamin D and human cancer. Adv Clin Chem. (2018) 83:183–96.
53. O'Sullivan F, Laird E, Kelly D, van Geffen J, van Weele M, McNulty H, et al. Ambient UVB dose and sun enjoyment are important predictors of vitamin D status in an older population. J Nutr. (2017) 147:858–68. doi: 10.3945/jn.116.244079
54. Datta P, Philipsen PA, Olsen P, Bogh MK, Johansen P, Schmedes AV, et al. The half-life of 25(OH) D after UVB exposure depends on gender and vitamin D receptor polymorphism but mainly on the start level. Photochem Photobiol Sci. (2017) 16:985–95. doi: 10.1039/C6PP00258G
55. Abdulateef DS, Rahman HS, Salih JM, Osman SM, Mahmood TA, Omer SHS, et al. COVID-19 severity in relation to sociodemographics and vitamin D use. Open Med. (2021) 16:591–609. doi: 10.1515/med-2021-0273
56. Groves NJ, McGrath JJ, Burne TH. Vitamin D as a neurosteroid affecting the developing and adult brain. Annu Rev Nutr. (2014) 34:117–141. doi: 10.1146/annurev-nutr-071813-105557
57. Belzeaux R, Boyer L, Ibrahim EC, F'eron F, Leboyer M, Fond G. Mood disorders are associated with a more severe hypovitaminosis D than schizophrenia. Psychiatry Res. (2015) 229:613–6. doi: 10.1016/j.psychres.2015.04.039
58. Boerman R, Cohen D, Schulte PF, Nugter A. Prevalence of vitamin D deficiency in adult outpatients with bipolar disorder or schizophrenia. J Clin Psychopharmacol. (2016) 36:588–92. doi: 10.1097/JCP.0000000000000580
59. Cuomo A, Maina G, Bolognesi S, Rosso G, Beccarini Crescenzi B, Zanobini F, et al. Prevalence and correlates of vitamin d deficiency in a sample of 290 inpatients with mental illness. Front Psychiatry. (2019) 10:167. doi: 10.3389/fpsyt.2019.00167
60. Jamilian H, Amirani E, Milajerdi A, Kolahdooz F, Mirzaei H, Zaroudi M, et al. The effects of vitamin D supplementation on mental health, and biomarkers of inflammation and oxidative stress in patients with psychiatric disorders: a systematic review and meta-analysis of randomized controlled trials. Prog Neuropsychopharmacol Biol Psychiatry. (2019) 94:109651. doi: 10.1016/j.pnpbp.2019.109651
61. Okereke OI, Reynolds CF 3rd, Mischoulon D, Chang G, Vyas CM, Cook NR, et al. Effect of long-term vitamin D3 supplementation vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA. (2020) 324:471–80. doi: 10.1001/jama.2020.10224
62. Haq A, Svobodová J, Imran S, Stanford C, Razzaque MS. Vitamin D deficiency: A single centre analysis of patients from 136 countries. J Steroid Biochem Mol Biol. (2016) 164:209–13. doi: 10.1016/j.jsbmb.2016.02.007
63. Haq A, Wimalawansa SJ, Pludowski P, Anouti FA. Clinical practice guidelines for vitamin D in the United Arab Emirates. J Steroid Biochem Mol Biol. (2018) 175:4-11. doi: 10.1016/j.jsbmb.2016.09.021
64. Al Saleh Y, Beshyah SA, Hussein W, Almadani A, Hassoun A, Al Mamari A, et al. Diagnosis and management of vitamin D deficiency in the Gulf cooperative management of vitamin D deficiency in the Gulf cooperative from the GCC vitamin D advisory board. Arch Osteoporos. (2020) 15:35. doi: 10.1007/s11657-020-0709-8
65. Di Nicola M, Dattoli L, Moccia L, Pepe M, Janiri D, Fiorillo A, et al. Serum 25-hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID-19 pandemic. Psychoneuroendocrinology. (2020) 122:104869. doi: 10.1016/j.psyneuen.2020.104869
66. Chen L, Zhu H, Harshfield GA, Treiber FA, Pollock JS, Pollock D, et al. 2020. Serum 25-hydroxyvitamin D concentrations are associated with mental health and psychosocial stress in young adults. Nutrients. (2020) 12:1938. doi: 10.3390/nu12071938
Keywords: COVID-19, depressive symptoms, somatization, vitamin D, United Arab Emirates
Citation: Al Anouti F, Thomas J, Karras S and El Asswad N (2022) Outdoor Activity in the Daytime, but Not the Nighttime, Predicts Better Mental Health Status During the COVID-19 Curfew in the United Arab Emirates. Front. Public Health 10:829362. doi: 10.3389/fpubh.2022.829362
Received: 05 December 2021; Accepted: 23 February 2022;
Published: 04 April 2022.
Edited by:
Mohammed A. Mamun, CHINTA Research Bangladesh, BangladeshReviewed by:
Amjad Hasan Jarrar, United Arab Emirates University, United Arab EmiratesCopyright © 2022 Al Anouti, Thomas, Karras and El Asswad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fatme Al Anouti, ZmF0bWUuQWxBbm91dGlAenUuYWMuYWU=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.