
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health, 12 April 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.821781
Objective: To evaluate the effects of Tuina (massage) vs. non-Tuina traditional Chinese medicine (TCM) treatments on nocturnal enuresis in children.
Methods: A systematic review and meta-analysis of randomized controlled trials (RCTs) was conducted following the Preferred Reported Items for Systematic Review and Meta-analysis (PRISMA) guidelines. RevMan 5.3 software was used for meta-analysis.
Results: Twelve RCTs recruiting a total of 1,007 children were included. Meta-analysis results showed that, compared with non-Tuina TCM treatments, Tuina could significantly improve the total effective rate of children's enuresis [RR = 1.29, 95%CI (1.22–1.36), P < 0.00001]. The results of subgroup analyses indicated that the total effective rate of Tuina combined with acupuncture in the treatment of nocturnal enuresis was higher than acupuncture alone [RR = 1.24, 95%CI (1.12–1.37), P < 0.0001]. The total effective rate of Tuina in the treatment of enuresis in children was better than that of herbal medicine alone [RR = 1.45, 95%CI (1.31–1.61), P < 0.00001]. The total effective rate of Tuina combined with herbal medicine in the treatment of enuresis in children was better than that of herbal medicine alone [RR = 1.16, 95%CI (1.06–1.26), P = 0.0007]. No adverse reactions of Tuina were reported in all included studies.
Conclusion: From the available evidence, Tuina, or Tuina combined with non-Tuina TCM treatments (acupuncture, or herbal medicine) can improve the clinical outcome of children with enuresis, indicating Tuina is a promising treatment choice for children's enuresis. However, because of the intrinsic limitations of the included studies, more high-quality randomized controlled trials with longer follow-up are still needed to further confirm the efficacy and safety of Tuina in the treatment of nocturnal enuresis in children.
Enuresis, also known as “bed-wetting”, is defined as intermittent urinary incontinence during sleep in children older than age 3, which is also the definition recognized and adopted by traditional Chinese medicine (TCM) (1, 2). Primary enuresis in children is a common childhood disease with heterogeneous and complex etiology. The delay of central nervous system function maturation, genetic factors, sleep disorders, and abnormal secretion of the antidiuretic hormone can lead to the occurrence of primary enuresis in children (3). Children with long-term enuresis may have impaired immune function, psychological disorders, low self-esteem, and other problems, which also lead to negative effects on the quality of life of their parents (4).
Clinically, anticholinergic drugs, tricyclic antidepressants, artificial antidiuretics, and central stimulants are often used for the treatment of enuresis, but their efficacy is poor and often leads to many side effects (5). Desmopressin, for example, has the most important side effects of water poisoning and hyponatremia, and a high relapse rate once discontinued (6). TCM treatments, such as herbal medicine, acupuncture and moxibustion, and Tuina are commonly used for the treatment of nocturnal enuresis, and many clinical studies have shown that they are effective and have great potential in the treatment of this disorder (7–11). However, due to the unpleasant taste or invasiveness, non-Tuina TCM treatments including herbal medicine, acupuncture and moxibustion have unsatisfactory compliance in young children (12, 13), on the contrary, Tuina is non-invasive, safe, and comfortable, making it more suitable and acceptable for children with nocturnal enuresis (14). Tuina for children originated from adult Tuina, but because children's body is immature, their skin and flesh are tender, the force of Tuina for children is much gentler than that for adults (15). However, whether Tuina is more or less effective than non-Tuina TCM treatments for the treatment of children's enuresis remains unknown, therefore, this systematic review and meta-analysis included the related randomized controlled trials (RCT) to investigate the difference in the effects of Tuina vs. non-Tuina TCM treatments for enuresis in children, aiming to provide evidence for clinicaldecision-making.
This systematic review and meta-analysis were performed following the PRISMA (Preferred Reported Items for Systematic Review and Meta-analysis) guidelines (16).
The electronic databases including China national knowledge infrastructure (CNKI), Wanfang Database, Chongqing VIP, The Cochrane Library, and PubMed were searched for potentially eligible studies.
A combination of the following English terms was used to search the English databases: (“enuresis” OR “bed-wetting”) AND (“pediatric” OR “pediatric” OR “adolescent” AND “child” OR “children” OR “kid” OR “youngster”) AND (“Tuina” OR “massage”). For the Chinese databases, the following keywords were used in combined ways: [“yiniao (enuresis)” OR “Niaochuang (bed-wetting)” AND (“Xiaoer (children)” OR “ertong (children)” OR “qingshaonian (adolescent)”) AND (“Tuina” OR “Anmo (massage)”]. The retrieval time was from the establishment to July 2021.
Furthermore, the reference lists of all the related articles were reviewed to identify potential RCTs. There were no trials excluded due to their publication status or language.
(1) Participants: All the participants should meet the following diagnostic criteria of pediatric enuresis (17): The onset age is 3–18 years old, bed-wetting every night or every few days, or even countless bed-wetting overnight (1, 2, 18). (2) Interventions: The experimental group was treated with Tuina, or Tuina combined with non-Tuina TCM treatment (herbal medicine, acupuncture, etc.); the control group was treated with non-Tuina TCM treatment alone. Except for the Tuina treatment, other treatments were the same in the control group and the experimental group. (3) Type of studies: Randomized controlled trials, whether or not allocation concealment, blinding methods were used. (4) Outcome measures: There were clear and well-recognized criteria for efficacy evaluation, the total effective rate (TER) was regarded as the primary outcome, and adverse reactions were the secondary outcome.
(1) Non-randomized controlled trials (non-RCTs); (2) Tuina was not the intervention; (3) Literature of missing outcome indicators; (4) Duplicated studies, reviews, studies with incomplete data and unable to obtain the full text; (5) Enuresis caused by urinary tract infection, or severe liver and kidney dysfunction.
According to the standards for diagnosis and efficacy of diseases and syndromes of traditional chinese medicine (17), the treatment efficacy was evaluated and graded after treatment:
a) Complete remission (CR): The patient's enuresis disappeared and no recurrence within one month;
b) Significantly effective (SE): Enuresis symptoms were significantly relieved, and recurrence occurred within a month, but less than 1 time per week;
c) Partial remission (PR): Enuresis frequency decreased, more than once a week;
d) Ineffective: No change in enuresis frequency compared with that before treatment.
The total effective rate was defined as the percentage of patients who achieved CR or SE or PR.
Retinal hemorrhage, fracture, hematoma, ecthyma, vomiting, etc., related to the treatments (19).
All the candidate articles were screened by two independent investigators (C.I. TONG and M.I. HO) based on the title and abstract. The full texts were retrieved for further evaluation according to the inclusion and exclusion criteria. All inclusion disagreements were resolved by consensus.
The included studies were assessed for risk bias using the Review Manager5.3 software built-in risk bias assessment tool provided by the Cochrane Handbook V.5.1.0 (Cochrane Collaboration) (20). The evaluation items included the generation of random sequences, allocation concealment, blinding of investigators and subjects, blind evaluation of study outcomes, the integrity of outcome data, selective reporting of study results, and other sources of risk bias. The bias risk was assessed as low risk, unknown risk, and high risk according to the quality of the included studies. The characteristics of all included RCTs are summarized in Table 1.
The included studies were analyzed using Review Manager 5.3 software provided by the Cochrane Collaboration. The I2 statistic and Chi2 test were used to determine statistical heterogeneity. If P > 0.1 and I2 <50%, the heterogeneity was considered acceptable and the fixed-effect model was adopted. If P ≤ 0.1 and I2≥ 50%, substantial heterogeneity was considered, and the random-effects model was used to calculate the pooled effect size, and the source of heterogeneity would be analyzed. According to data types, the risk ratio (RR) or odds ratio (OR) were used for dichotomous data, and the weighted mean difference (WMD) or standardized mean difference (SMD) for continuous data. In total 95% confidence interval (CI) was calculated for both (32–34).
The funnel plots and Egger's test were carried out to assess the potential bias when there were more than 10 trials included in a meta-analysis (20, 35, 36).
Table 2 summarizes the results of the meta-analysis.
A total of 184 articles in Chinese and English were retrieved. In total 124 duplicates studies, Summary and review studies, did not meet the inclusion criteria and empirical articles. According to the inclusion and exclusion criteria, 12 references were finally obtained. After reading the full texts, the final number of studies included in quantitative analysis was 12 (21–31, 37). The literature screening process is shown in Figure 1. The characteristics of the tests are shown in Table 1.
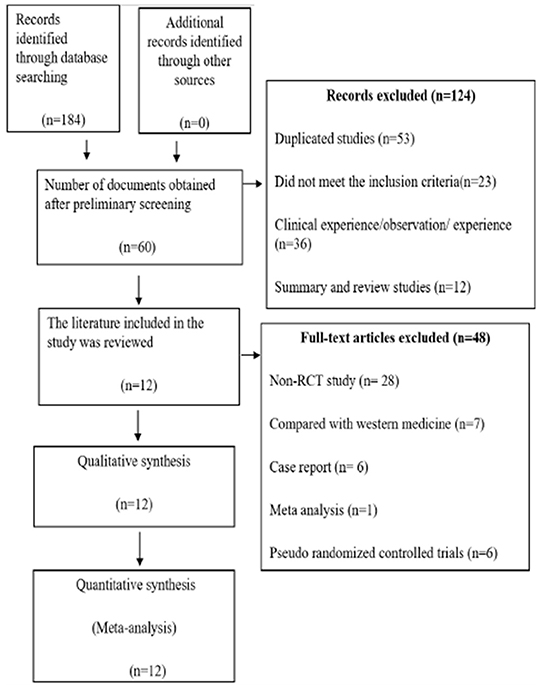
Figure 1. Preferred reporting items for systematic reviews and meta-analysis (PRISMA) search diagram.
Randomized method was used in all the 12 included studies (21–31, 37), but only 7 (21–26, 28–31) clearly described the randomized methods (table of random numbers). No studies clearly described the allocation concealment, the blind method of investigator, participants, and outcome assessment. There was no case of patient withdrawal or loss of follow-up in all the studies. The overall quality of RCTs was not high. The risk of bias and methodological quality of the included RCTs was assessed and shown in Tables 1, 3 and Figures 2, 3.
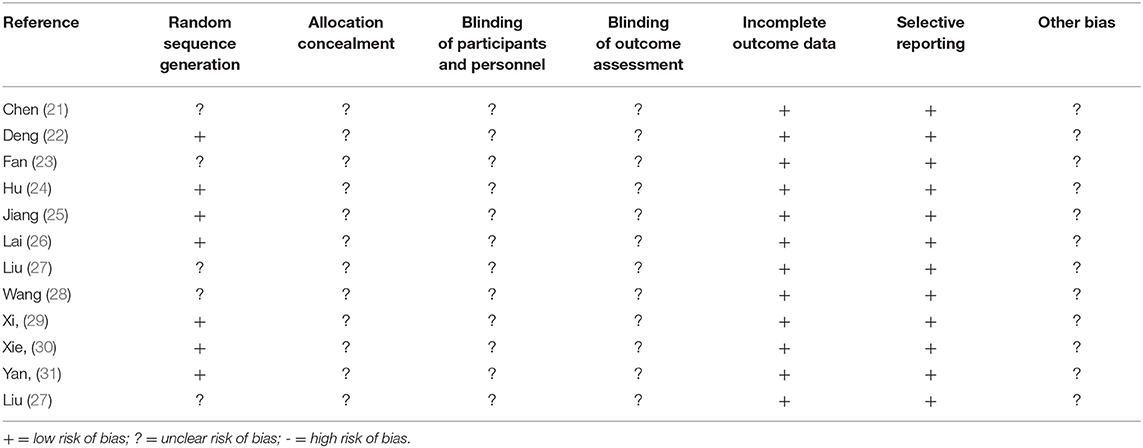
Table 3. The methodologic quality of the included trials was assessed using the Cochrane risk of bias tool.
There were 12 trials involving 1,007 patients (21–31, 37) that compared the total effective rate of Tuina vs. non-Tuina TCM treatments in the treatment of pediatric enuresis. There was no significant heterogeneity among the included studies (I2 = 49%), the fixed effects model was used for meta-analysis. The results showed that the total effective rate of the Tuina treatment group was higher than that of the non-Tuina control group [RR = 1.29, 95%CI (1.22–1.36), P < 0.00001], and the difference between the two groups was statistically significant. As shown in Figure 4.
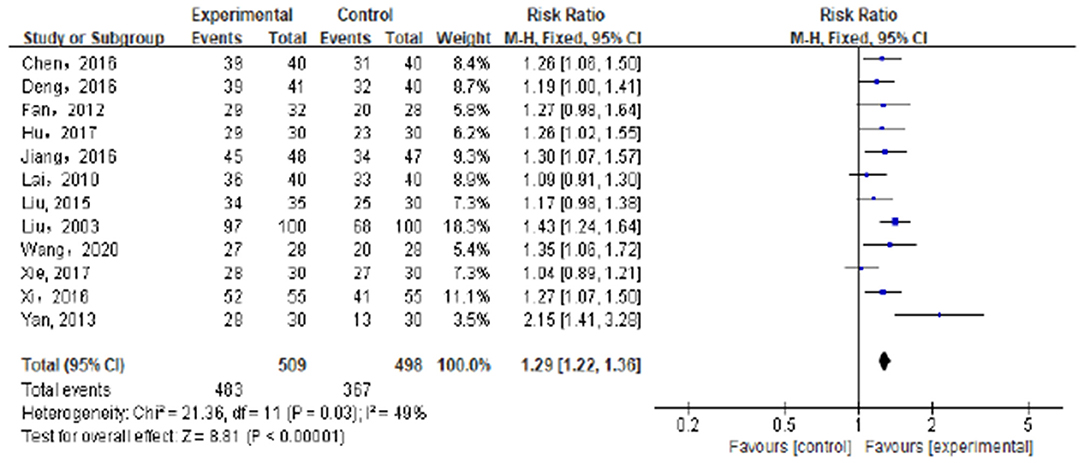
Figure 4. Compared with the control group, the total effective rate of the experimental group was significantly improved.
The subgroup analyses were conducted to determine the causes of heterogeneity among the results of studies. The subgroup analysis based on the method of TCM treatments showed that different method of TCM treatments was the cause of heterogeneity and the clinical efficacy of Tuina was better than other non-Tuina TCM treatments in the management of children's enuresis.
Four experiments (21, 23, 24, 37) compared the effective rate of Tuina combined with acupuncture in the treatment of pediatric enuresis. A total of 265 patients were included, including 137 cases in the Tuina plus acupuncture group and 128 cases in the acupuncture group. The results showed that the total effective rate of Tuina plus acupuncture was higher than that of acupuncture alone, and the difference was statistically significant [RR = 1.24, 95%CI (1.12–1.37), P < 0.0001]. As shown in Figure 5.
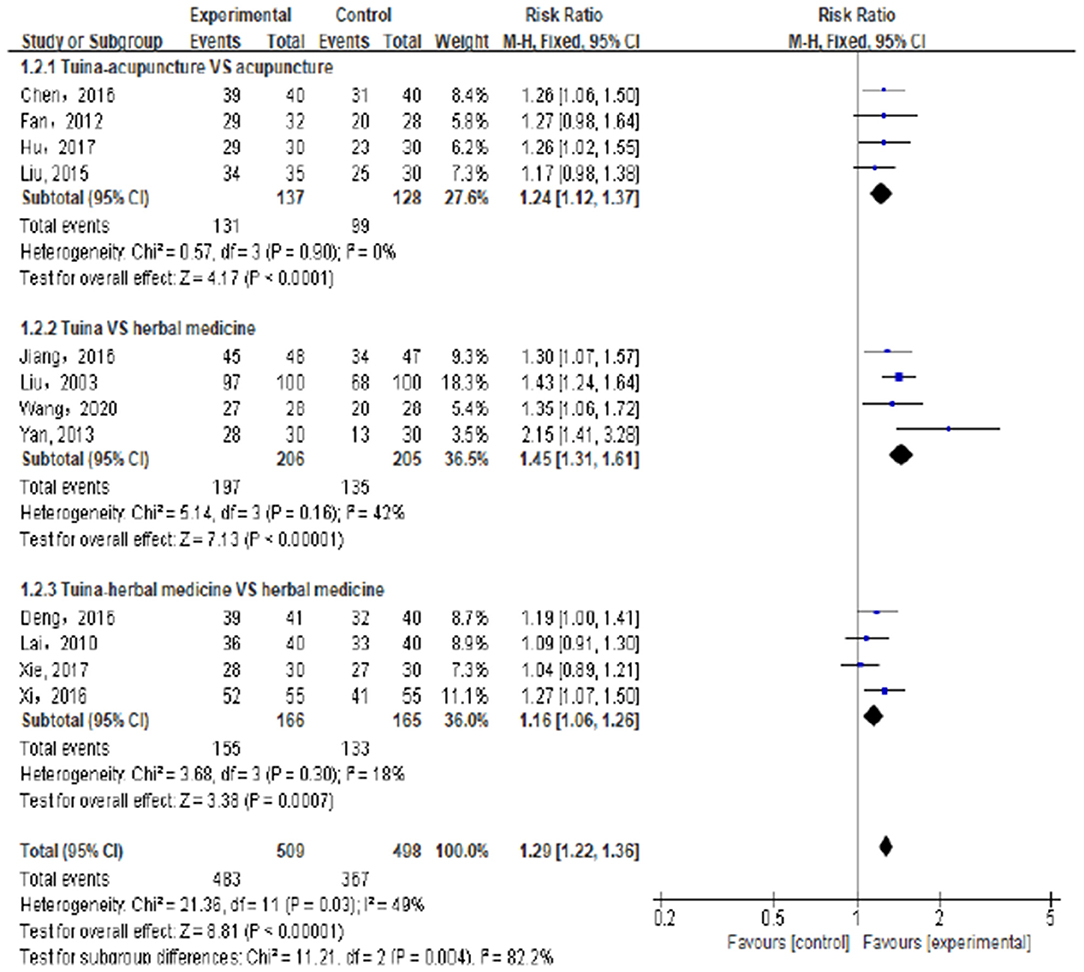
Figure 5. Subgroup analysis showed that compared with the control group, the total effective rate of the experimental group was significantly improved.
Four experiments (25, 27, 28, 31) compared the effective rates of Tuina vs. herbal medicine in the treatment of enuresis in children. A total of 411 cases were included, 206 cases in the Tuina group and 205 cases in the herbal medicine group. The results showed that the effective rate of the Tuina group was better than that of the herbal medicine group, and the difference was statistically significant [RR = 1.45, 95%CI (1.31–1.61), P < 0.00001]. As shown in Figure 5.
Four trials (22, 26, 29, 30) compared the effective rates of Tuina combined with herbal medicine vs. herbal medicine alone in the treatment of enuresis in children. A total of 331 cases were included. The results showed that the total effective rate of Tuina combined with herbal medicine was significantly higher than that of herbal medicine alone, and the difference was statistically significant [RR = 1.16, 95%CI (1.06–1.26), P = 0.0007]. As shown in Figure 5.
There was no significant heterogeneity for the above subgroup analyses outcomes (I2 = 0, 42, and 18%, respectively), and the fixed effects model was applied to combine the trials.
No adverse reactions related to Tuina were reported in the included trials.
Between all included clinical trials, there was generally good homogeneity.
Regarding TER, the primary outcome, the pooled data showed that Tuina, or Tuina combined with other TCM treatments significantly increased TER by 21.2% (RR = 1.29, 95% CI 1.22–1.36, P < 0.00001). The results were similar when the sensitivity and subgroup analyses were conducted based on the quality of the study (only included the studies clearly describing randomization methods) (22, 24–26, 29–31) [RR = 1.26, 95%CI (1.17–1.36), P < 0.0001], duration of Tuina treatment (≥ 15 days) (22–26, 29, 31) [RR = 1.31, 95%CI (1.20–1.43), P < 0.0001]; Year of publication (only studies published in the last 6 years were included) (21, 22, 24, 25, 28–30) [RR = 1.24, 95%CI (1.15-1.33, P < 0.00001], subject size (≥ 40 subjects in each group) (21, 22, 25–27, 29) [RR = 1.28, 95%CI (1.20–1.37), P < 0.00001]. The results of the sensitivity and subgroup analyses suggested that the results of the meta-analysis were reliable and robust.
The funnel plots of the total effective rate, the primary outcome, suggested possible publication bias in small trials (Figure 6).
According to modern medicine theory, enuresis in children is related to psychological factors, genetic factors, imperfect neurodevelopment (38), abnormal bladder function, and other factors. Invisible spina bifida can also cause bed-wetting in children. In the theory of TCM, enuresis is related to congenital deficiency, the pathogenesis of enuresis in children is complex and its etiology has not yet been fully elucidated. The main etiology and pathogenesis of enuresis in children are the asthenia and coldness of the Xia Yuan (primordial qi of lower energizer), the deficiency of spleen, lung, and kidney, the dampness and heat of the liver meridian, and the incompatibility of the heart and kidney (39). Western medicine treatments mainly include functional exercise, psychological support, and clinical medications (mainly desmopressin) (40, 41). Long-term medications for children may cause greater side effects, such as psychological burdens and even serious psychological disorders. Increasing reports have shown that TCM might play a promising role in the management of children's enuresis, it shows good clinical effectiveness without notable side effects. TCM treatment methods include herbal medicine, acupuncture, Tuina, etc. Tuina has been broadly used for the treatment of enuresis in children, a master's thesis (42) reported a meta-analysis of Tuina in the treatment of enuresis in children (42). The main differences between this thesis and our study included: a) Wen's study included the studies that used other non-TCM treatments, such as western medicine, physical therapy, etc. In our study, only TCM treatments were used for both the control group and the treatment group. b) Wen's study did not evaluate the overall effects of Tuina vs. other treatments, only subgroup analyses were performed, in situations where no overall effects were evaluated, subgroup analyses were unreliable. It was not wise to draw confirmatory conclusions from subgroup findings (43, 44). There is a need to perform a meta-analysis to systematically evaluate the overall effects of Tuina for enuresis in children, and compare the effects of Tuina vs. non-Tuina TCM treatments. The present study is the first systematic review and meta-analysis comparing the difference in the clinical efficacy of Tuina vs. non-Tuina TCM treatments for enuresis in children.
According to the TCM etiology and pathogenesis of enuresis in children, the basic therapeutic principles of Tuina are balancing yin and yang, supplementing the insufficiency and reducing the excess, etc (45). Based on the TCM syndrome differentiation with meridian and acupoints as the outline (46), the individualized treatment regimes are also different, commonly used regimes include Tuina on the acupoints Baihui (GV20) and Qihai (CV6) to warm the yang and dispel cold, pinching the ridge of the Du Channel to facilitate the conduction of qi through the meridians to tonify qi, pushing Tianheshui acupoint (PC9- PC3 direction) to clear the liver and dispel dampness, kneading the Neiguan (PC6) and Shenmen (HT7) acupoints to clear the heart and warm the kidneys, etc. (47, 48).
In this study, 12 RCTs were finally included. The results of this meta-analysis indicate that, compared with non-Tuina TCM treatments, Tuina could significantly improve the total effective rate of enuresis in children by 21.2% [RR = 1.29, 95%CI (1.22–1.36), P < 0.00001], no adverse reactions were reported in the included studies, indicating that Tuina appears to be effective and safe for the treatment of enuresis in children and might bring clinical benefits to them.
Enuresis is more common in very young children, so it is also called pediatric enuresis. Although herbal medicine and acupuncture are also effective for pediatric enuresis, herbal medicine is not very suitable for very young kids because it usually tastes bitter, and acupuncture is an invasive treatment. Therefore, as a non-invasive treatment, Tuina is more suitable for young children, Tuina therapy is well tolerated by children and has better compliance for long-term therapy. The results of subgroup analyses showed that Tuina was more effective than herbal medicine in the treatment of enuresis in children (P< 0.00001), Tuina combined with herbal medicine or acupuncture in the treatment of nocturnal enuresis was more effective than herbal medicine (P = 0.0007) or acupuncture (P< 0.0001) alone, suggesting that Tuina is an optimal treatment choice for enuresis in children, if the kids could accept herbal medicine or acupuncture treatment, Tuina combined with herbal medicine, or Tuina combined with acupuncture are also preferred than herbal medicine or acupuncture alone.
This meta-analysis has some limitations:
(a) The quality of 4 included RCTs in this study was not high, and there were potential risks of bias due to the lack of randomization methods, and methods of blinding, etc.
(b) The treatment duration and follow-up time were relatively short, the long-term outcomes of Tuina could not be evaluated.
(c) Individual data were insufficient, subgroup and sensitivity analyses based on country, age, sex, severity, specific method of Tuina, the pathogenesis of enuresis, etc. were not performed.
(d) Adverse reactions were not reported in any included studies. Therefore, only efficacy evaluation can be carried out, and the safety of tuina could not be evaluated. Further studies in this area should be strengthened in the future.
(e) There was potential publication bias.
From the available evidence, Tuina, or Tuina combined with non-Tuina TCM treatments (acupuncture, or herbal medicine) can improve the clinical outcome of children with enuresis, indicating Tuina is a promising treatment choice for children's enuresis. However, because of the intrinsic limitations of the included studies, more high-quality randomized controlled trials with longer follow-up are still needed to further confirm the efficacy and safety of Tuina in the treatment of nocturnal enuresis in children.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
CT and QH methodology, investigation, verification, analysis, and manuscript writing. MH verification, investigation, and formal analysis. ZZ writing review and editing. QW and MC verification, investigation, design, review, and supervision. All authors contributed to the article and approved the submitted version.
This study was funded by the Science and Technology Development Fund, Macau SAR (file No.: 0010/2019/A, 0099/2018/A3, 0098/2021/A2, and 130/2017/A3), Science and Technology Planning Project of Guangdong Province (2020B1212030008).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.821781/full#supplementary-material
1. Shen Q, Liu XM, Yao Y, et al. The management of unisymptomatic nocturnal enuresis in children in China. J Clin Pediatr. (2014) 32:970–5.
2. ZY/T001.1-001.9-94, Criteria for diagnosis and curative effect of TCM diseases and syndromes [S].
4. Collis D, Kennedy-Behr A, Kearney L. The impact of bowel and bladder problems on children's quality of life and their parents: a scoping review. Child Care Health Dev. (2019) 45:1–14. doi: 10.1111/cch.12620
5. Pan L. Treatment of 31 children with enuresis (kidney qi deficiency syndrome) by invigorating spleen and nourishing kidney Tuina combined with Suoquan pill. J External Treat Tradit Chin Med. (2018) 5:27–8.
6. Kuwertz-Bröking E, von Gontard A. Clinical management of nocturnal enuresis. Pediatr Nephrol. (2018) 7:1145–54. doi: 10.1007/s00467-017-3778-1
7. Bower WF, Diao M, Tang JL, Zhang HW, Yeung CK. Acupuncture for bladder dysfunction and nocturnal enuresis in children: a systematic review and exploration of rationale. Neurourol Urodyn. (2005) 24:267–72. doi: 10.1002/nau.20108
8. Bower WF, Diao M. Acupuncture as a treatment for nocturnal enuresis. Auton Neurosci. (2010) 157:63–7. doi: 10.1016/j.autneu.2010.07.003
9. Zhang YH, Gu Q. Fifty cases of primary nocturnal enuresis in children treated with herbal-partition moxibustion and finger pressure. Zhongguo Zhen Jiu. (2014) 34:831–2. doi: 10.13703/j.0255-2930.2014.08.033
10. Ma Y, Liu X, Shen Y. Effect of traditional Chinese and Western medicine on nocturnal enuresis in children and indicators of treatment success: Randomized controlled trial. Pediatr Int. (2017) 59:1183–8. doi: 10.1111/ped.13417
11. Wang D. Progress of traditional Chinese and western medicine in the treatment of pediatric enuresis. Chin Health Standard Manage. (2016) 7:124–25.
12. Bao C, Lu B, Wu X. Clinical observation on 30 cases of pediatric enuresis treated by acupuncture and moxibustion tongdu and Wenyang. Jiangsu J Tradit Chin Med. (2015) 47:49–50.
13. Rong P, Zhao YS, Ma R, Hu SY, Zhong CL, Zhao JS. Systematic evaluation of traditional Chinese medicine treatment of pediatric enuresis. Chin J Tradit Chin Med. (2012) 27:1818–22.
14. Zhang Cd, Zhang JR. Effective evaluation on treating pediatric enuresis of the Shenqi Buzu type by the Yi'nao Bushen Tuina therapy. Clin Res Tradit Chin Med. (2017) 9:73–4.
15. Dong DR. Characteristics of pediatric massage J Chengdu College Tradit Chin Med. (1987) 03:59–60.
16. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:7. doi: 10.1371/journal.pmed.1000097
17. Wang ZY, Du K, Li C, Xi Z, Zhang F. Guidelines for the clinical diagnosis and treatment of pediatric enuresis. Chin J Pediatr. (2018) 14:4–8. doi: 10.16840/j.issn1673-4297.2018.01.02
18. Wu RP, Hu YM, Jiang ZF. Zhufutang Practical Pediatrics. 6th Ed. Beijing: People's Medical Publishing House (1996) p. 1896.
19. Wang SS, Liu F, Yang H, Wang DD. Reflection on the safety of pediatric massage. China J Tradit Chin Med. (2020) 35:4808–11.
20. Wang X, Liu Z, Sui X, Wu Q, Wang J, Xu C. Elemene injection as adjunctive treatment to platinum-based chemotherapy in patients with stage III/IV non-small cell lung cancer: A meta-analysis following the PRISMA guidelines. Phytomedicine. (2019) 59:152787. doi: 10.1016/j.phymed.2018.12.010
21. Chen YH. linical analysis of acupuncture combined with chiropractic therapy in the treatment of 40 children with enuresis. Gansu Sci Technol. (2016) 32:111–2.
22. Deng CX. Effect of chiropractic in the treatment of enuresis in children. Yunnan J Tradit Chin Med. (2016) 37:39–40. doi: 10.16254/j.cnki.53-1120/r.2016.10.017
23. Fan HY. Clinical analysis of acupuncture combined with Tuina in treatment of enuresis in 60 cases. China's Health Ind. (2012) 9:173–173. doi: 10.16659/j.cnki.1672-5654.2012.26.025
24. Hu AF. Clinical study of Baihui acupuncture combined with chiropractic in the treatment of enuresis in children. Tradit Asian Pacific Med. (2017) 13:107–8. Available online at: https://tra-oversea-cnki-net.libezproxy.must.edu.mo/kns/detail/detail.aspx?FileName=YTCT201713051&DbName=CJFQ2017
25. Jiang CY. Clinical observation on the treatment of enuresis with nephroqi deficiency in children by Tuina of warming kidney and strengthening spleen. New Traditional Chin Med. (2016) 48:127–8. doi: 10.13457/j.cnki.jncm.2016.09.057
26. Lai CJ. Treatment of 40 children with enuresis by internal administration of traditional Chinese medicine combined with three-part Tuina. Massage Rehabilit Med. (2010) 1:36–7. doi: 10.3969/j.issn.1008-1879.2010.07.017
27. Liu RJ. Treatment of 100 children with enuresis by Tuina. Sichuan Tradit Chin Med. (2003) 09:92.
28. Wang YF. Clinical observation of pediatric Tuina treatment of 56 children's enuresis. Clin Res. (2020) 8:142. Available online at: https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjIwMzIyEhJ6Z2JqeXkta3AyMDIwMjIyNDIaCHk5d3dwZHht
29. Xi Z. Clinical study of massage combined with Feng's kneading technique in the treatment of spleen and kidney deficiency syndrome in children with enuresis. Beijing Univ Chin Med. (2016) 35:370–3. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD201701&filename=1017014828.nh
30. Xie TL. Clinical observation of Xuanfei Yishen Decoction combined with pediatric massage in the treatment of pediatric enuresis, lung and kidney qi deficiency syndrome. Changchun Univ Chin Med. (2017) Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD201801&filename=1018006738.nh
31. Yan JF. Clinical study on the treatment of enuresis in children with renal qi deficiency by massage of warming kidney and strengthening spleen. Shandong Univ Chin Med. (2013). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD201401&filename=1014115785.nh
32. Chen H, Yao X, Li T, Lam CW, Zhang R, Zhang H, et al. Compound Kushen injection combined with platinum-based chemotherapy for stage III/IV non-small cell lung cancer: A meta-analysis of 37 RCTs following the PRISMA guidelines. J Cancer. (2020) 11:1883–98. doi: 10.7150/jca.40267
33. Zhang YW, Zhang J, Hu JQ, Wen CL Dai SY, Yang DF, et al. Neuraxial adjuvants for prevention of perioperative shivering during cesarean section: A network meta-analysis following the PRISMA guidelines. World J Clin Cases. (2019) 7:2287–301. doi: 10.12998/wjcc.v7.i16.2287
34. Wu Q, Yao X, Chen H, Liu Z, Li T, Fan X, et al. Long-term aspirin use for primary cancer prevention: an updated systematic review and subgroup meta-analysis of 29 randomized clinical trials. J Cancer. (2020) 11:6460–73. doi: 10.7150/jca.49001
35. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
36. Chen H, Yao X, Liu Z, Li T, Xu C, Wang J, et al. Efficacy and safety of Shenqi Fuzheng injection combined with platinum-based chemotherapy for stage III/IV non-small cell lung cancer: A protocol for systematic review and meta-analysis of randomized controlled trials. Medicine. (2019) 98:39. doi: 10.1097/MD.0000000000017350
37. Dong DR. Characteristics of pediatric massage J Chengdu College Tradit Chin Med. (1987) 03:59–60.
38. Banakhar MA, Al-Shaiji TF, Hassouna MM. Pathophysiology of overactive bladder. Int Urogynecol J. (2012) 23:975–982. doi: 10.1007/s00192-012-1682-6
39. Xu MM, Xu L. The clinical research progress of massage in the treatment of pediatric enuresis, China. Rural Med. (2020) 27:72–4. doi: 10.19542/j.cnki.1006-5180.004270
40. Zhang Q, Si Dm. Effect of desmopressin combined with oxbubnin on primary enuresis. Modern Drug Application in China. (2015) 9:123–5. doi: 10.14164/j.cnki.cn11-5581/r.2015.16.085
41. Wang H, Wang SM, Wan MT, Hao HW. Study on the rule of traditional Chinese medicine in the treatment of children's enuresis based on modern literature. Chinese J Exper Form. (2016) 22:200–3. doi: 10.13422/j.cnki.syfjx.2016060200
42. Wen YH. Systematic evaluation of clinical research on massage in the treatment of pediatric enuresis (Thesis). Chengdu Univ Tradit Chin Med. (2016). Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD201701&filename=1017032808.nh
43. Wu QB, Leung LH. Association of dietary fiber and yogurt consumption with lung cancer risk. JAMA Oncol. (2020) 6:788. doi: 10.1001/jamaoncol.2020.0261
44. Wu QB, Leung LH. The evidence strength of a meta-analysis of aspirin for primary prevention of cancer. J Cancer Res Clin Oncol. (2020) 146:2173–5. doi: 10.1007/s00432-019-03069-w
45. Li PF. Yang Jindou's theory of balancing Yin and Yang Tuina. Beijing Tradit Chin Med. (2011) 30:362–6. doi: 10.16025/j.1674-1307.2011.05.014
46. Sun DR, Chen BR. The application of skin massage theory in children. Chin J Tradit Chin Med. (2020) 35:1531–3.
Keywords: Tuina, massage, enuresis in children, randomized controlled trial, meta-analysis
Citation: Tong C, He Q, Ho M, Zhong Z, Wu Q and Chen M (2022) Tuina for Enuresis in Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Public Health 10:821781. doi: 10.3389/fpubh.2022.821781
Received: 24 November 2021; Accepted: 14 March 2022;
Published: 12 April 2022.
Edited by:
Li Wu, Hunan University of Chinese Medicine, ChinaReviewed by:
Lu Ping, Shanghai University of Traditional Chinese Medicine, ChinaCopyright © 2022 Tong, He, Ho, Zhong, Wu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qibiao Wu, cWJ3dUBtdXN0LmVkdS5tbw==; Min Chen, bWNoZW5AbXVzdC5lZHUubW8=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.