- 1School of Medicine, Texas Tech University Health Sciences Center, Lubbock, TX, United States
- 2Julia Jones Matthews Department of Public Health, Graduate School of Biomedical Sciences, Texas Tech University Health Sciences Center, Lubbock, TX, United States
- 3Center of Excellence for Integrative Health, Lubbock, TX, United States
- 4Julia Jones Matthews Department of Public Health, Graduate School of Biomedical Sciences, Texas Tech University Health Sciences Center, Abilene, TX, United States
- 5Center of Excellence for Translational Neuroscience and Therapeutics, Lubbock, TX, United States
- 6Department of Pathology, School of Medicine, Texas Tech University Health Sciences Center, Lubbock, TX, United States
Introduction: Approximately half of adult Americans suffer from musculoskeletal disorders (MSD). Significant risk factors for musculoskeletal disorders include poor diet, obesity, and insufficient physical activity. Studies show that lifestyle change education and interventions reduce MSD risk factors. However, little is known about the relationship between physician advice for behavior change and reported behavior change by MSD patients. This study explored the association between physician advice for lifestyle change and reported change in MSD patients, as well as the effects that patient education levels have on compliance.
Methods: This study used data from the 2017 National Health Interview Survey, a nationally representative cross-sectional survey of non-institutionalized US adults. The research team limited analysis to adults who reported a limitation due to musculoskeletal problems (n = 2,672). Outcomes included physician recommendations to increase physical activity, reduce fat/calories, or lose weight, and whether they enacted these behavioral changes. Adjusted logistic regression models examined whether compliance with doctor's instructions differed by education level.
Results: Adjusted models show patients advised to change physical activity, diet, and weight were more likely to report attempted behavior change. Education was positively associated with likelihood of complying with physician advice to increase physical activity. Among patients not advised to change behaviors by a physician, education was positively associated with current behavior change attempts.
Conclusion: This study suggests that physician recommendations are relevant predictors of reported behavior change in individuals with MSD. Although education plays an important role in this association, the relationship is complex and multifaceted. Future studies should explore how compliance may be impacted by other factors, such as physician message type.
Introduction
Musculoskeletal disorders (MSDs) affect ~124 million adult Americans, which accounts for one in every two adults, greater than the prevalence of cardiovascular and respiratory diseases combined (1). MSDs also have large economic implications, costing the US $213 billion in 2011 through lost productivity and more than $300 billion in 2009 through lost work earnings and health care costs (2). Pain and disability from MSDs are significant barriers to independent living in the community. Interventions need to include both clinical and population-based approaches to improve the prevention and treatment of MSDs for a better quality of life.
One of the most important areas for prevention and treatment is modifying risk factors (3). Numerous risk factors are associated with musculoskeletal conditions, including MSDs. Smoking, unhealthy diet, obesity, sleep deprivation, stress, and inactivity all contribute to a higher risk of developing MSDs (4). Minimizing the occurrence of these factors is well-accepted in reducing the risk and severity of MSDs as well as decreasing pain (5–7). However, long-term behavioral changes are essential for risk reduction and management of MSDs (8). Therefore, individuals need to focus on developing healthy choices with their physicians and maintaining them in their absence. Physician advice that is complemented with resources, such as community health programs, may improve prevention and risk factor management strategies (9).
Studies have shown that physicians play a significant role in educating and promoting healthier lifestyles in their patients (10, 11). Educational interventions in individuals with MSDs demonstrated effectiveness in reducing risk factors, improving productivity, and reducing pain and anxiety (12–14). However, non-compliance thwarts many effective treatment plans regardless of disease (15). Poor compliance is widespread, exhibited by ~30–50% of all patients and accounting for between $100 and $300 billion of avoidable health care costs (16). The relationship between physician advice for lifestyle change and MSD patient compliance has not been well-established. Appreciation of the factors that affect patients' decisions to perform and comply with advice is useful for healthcare providers and public health messaging to develop more efficient methods to maximize compliance and decrease risk factors in their patients. Further, an extension of compliance in the clinical setting can be applied to how people understand and respond to health initiatives in the community setting (17). In other words, the ability to understand the causes that help patients make better decisions with their physicians may also be a target for prevention strategies in the community.
One such factor is patient education level, which is a major social determinant of health essential for understanding and following a healthcare professional's advice (18–21). There is limited knowledge on how patient education levels are associated with compliance to healthcare providers' advice for lifestyle change to treat MSDs. Understanding this relationship may serve as a platform for further discoveries, such as determining how educational interventions affect lower educated patients (22). This may also aid the design of community outreach programs that help bring more attention to lifestyle choices and preventative measures. This study aimed to explore the association between patient behaviors for increasing physical activity, eating healthier, and enrolling in a weight loss program and physician advice for these lifestyle changes in MSD patients. Secondly, we examined the effects that background education level has on this compliance. We hypothesized a positive association between physician advice for behavior change and self-reported engagement in those behaviors and a positive association between education levels and compliance with physician's advice.
Methods
This study analyzed data from the 2017 National Health Interview Survey (NHIS). The NHIS is a nationally representative cross-sectional survey of non-institutionalized US residents conducted yearly (23). Respondents aged 18 and up were used for this study, with data merged from the Person and Sample Adult files of the 2017 NHIS. The Sample Adult survey was administered to a subsample of the full NHIS sample, resulting in a sample size of 26,742. These respondents were asked, “What condition or health problem causes you to have difficulty with activities?” Those who answered that musculoskeletal or connective tissue problems caused such limitations represent the subpopulation of interest for the study (n = 2,672).
Outcomes of interest included respondent self-reports that a physician has instructed the person to participate in a weight loss program, increase physical activity, or reduce fat or calories. Additionally, the respondent self-reported if they are currently engaging in those three activities. Education was coded into four categories based on reported years of education completed: less than high school, high school diploma, some college, and college or more. Control variables included age group, race/ethnicity, gender, body mass index, marital status, and employment status.
The research team conducted the analysis using Stata 16.1. Chi square tests compared categorical variable distributions between education level and physician recommendations or health behavior efforts. The six binary outcomes in this study, including three self-reports of physician recommendation and three self-reports of current health behavior activity, had prevalence well above 10% in the population of interest. As such, these outcomes were not appropriate for logistic regression, which may overestimate effect size when the outcome occurs more than 10% of the time (24). Therefore, this study applied Poisson regression with robust error variance (calculated using population weights in Stata) to estimate the relative risk of each outcome (25, 26). Given that language of “risk” may be less palatable for discussing an outcome of favorable health behaviors, we report these as prevalence ratios (27). Although the prevalence of individuals saying they are currently engaged in a weight loss program is slightly <10% in the subpopulation (9.2%), prevalence ratios were reported for all outcomes for consistency. Population weights, using the “svy” command in Stata, were used to account for NHIS complex survey design. Statistical significance was set at alpha <0.05.
Results
This study focuses on the 8.9% (n = 2,672) of 2017 adult NHIS respondents reporting that musculoskeletal or connective tissue problems cause limitations in activities. The average age for this subpopulation was older than the rest of the NHIS sample (56.4 years compared to 46.5 years, respectively). The MSD subsample was also more likely to be female than the rest of the NHIS sample (61.1 vs. 50.8%, respectively). The sample was also disproportionately non-Hispanic white relative to the rest of the NHIS sample (72.1 vs. 63.4%, respectively).
The proportion of adult respondents with MSD who reported being told by a physician to reduce fat and calories in their diet significantly differed by education level, where 48.73% with less than high school education reported receiving this advice, compared to 33.07% with a college degree or higher (Table 1). Education level was not associated with physician advice to increase physical activity or participate in a weight loss program.
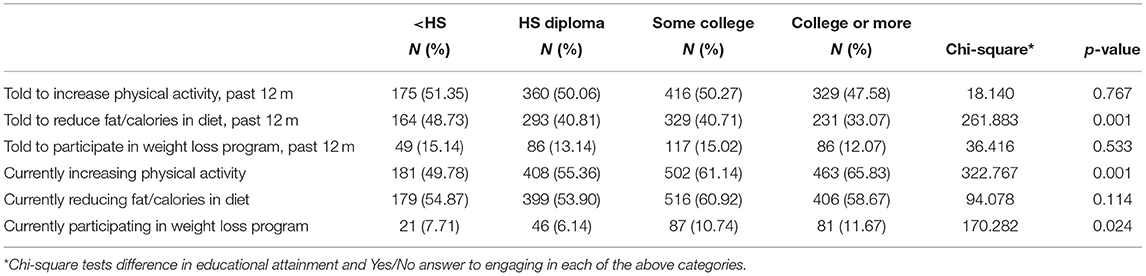
Table 1. Education effects on the proportions of adults with musculoskeletal disorders receiving physician advice for behavior change and reporting performing those changes.
Education and self-reports of current efforts to increase physical activity were positively associated, with 49.78% of adults with less than a high school degree reporting increased physical activity attempt, compared to 65.83% of adults with college or greater degrees (Table 1). A similar trend was true for respondents participating in a weight loss program, where 7.71% with less than a high school degree participated compared to 11.67% of college graduates. Education was not associated with current efforts to reduce fat or calories.
Adjusted prevalence ratios predicting physician recommendations for behavior change show few significant associations (Table 2). Education was not associated with physician recommendations except in the case of calorie reduction, where those with a college degree exhibited a lower prevalence of being told to reduce calories compared to those with less than a high school degree (OR = 0.78, 95% CI−0.64–0.95).
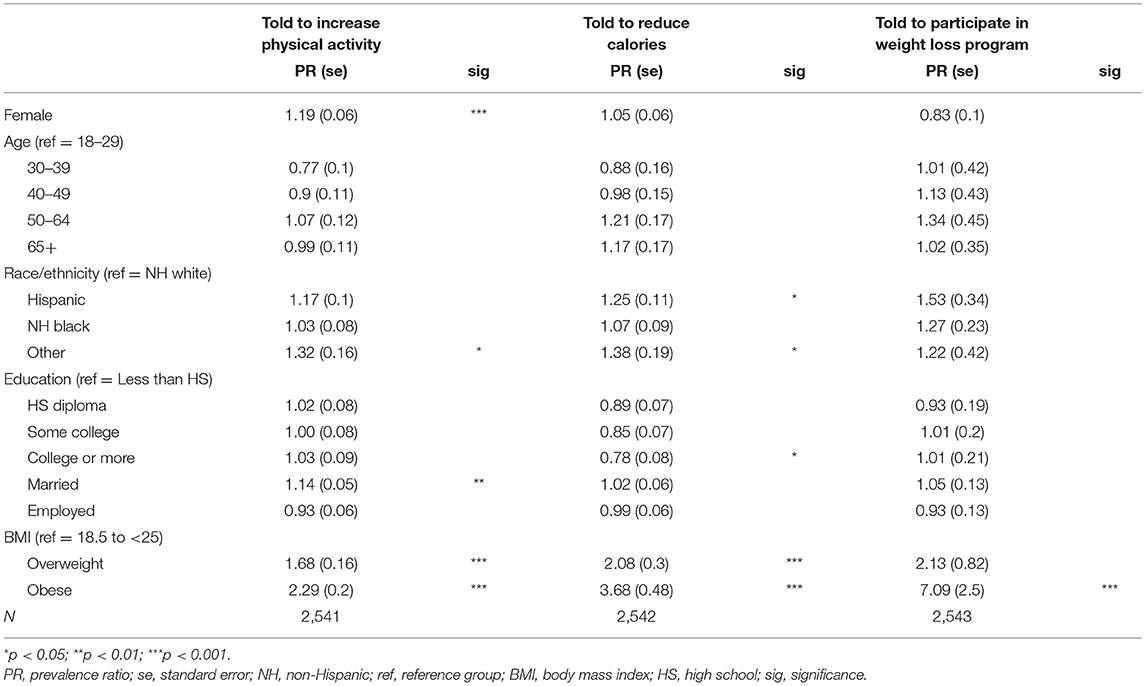
Table 2. Adjusted prevalence ratios predicting physician recommendations for behavior change in individuals reporting musculoskeletal disorders.
Education was positively associated with alignment of behavior change efforts and self-reported physician recommendations to increase physical activity (Table 3). Significant interaction effects demonstrate that efforts to increase physical activity vary by education level and self-reported physician recommendations (Figure 1). There was also a positive trend between education level and the likelihood of attempting physical activity among those who were not advised to do so by a physician. The physician recommendation group exhibited overall higher efforts to increase physical activity and narrower disparities between high and low education groups.
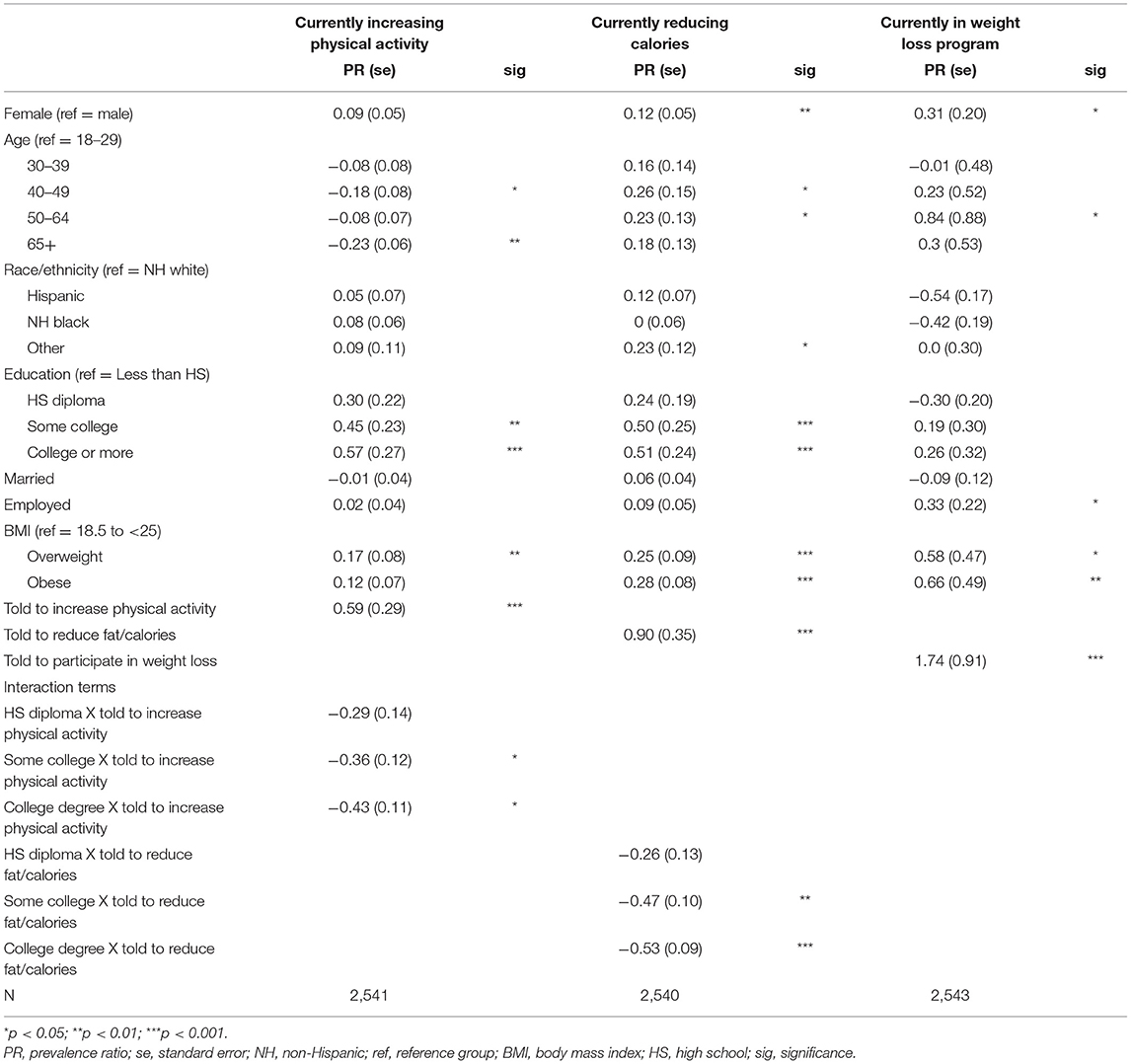
Table 3. Adjusted prevalence ratios predicting current behavior change efforts in individuals reporting musculoskeletal disorders.

Figure 1. Prevalence ratios of attempting to increase physical activity, by education and whether doctor advised to increase physical activity. < HS, less than high school diploma; HS, high school diploma; Some coll, some college; College+, college degree or higher; Prevalence ratio for each bar derived from interaction of poisson regression coefficients between doctor's recommendation to increase physical activity and education level; Reference group, less than a HS diploma who were not told to increase physical activity.
Education was also positively associated with self-reported attempts to reduce calories, although the interaction effects demonstrate that this relationship was primarily rooted in the group not told to reduce calories (Table 3). The MSD group told to reduce calories by a physician exhibited no meaningful differences by education level (Figure 2). Interactions between education and physician recommendations for participation in a weight loss program were not statistically significant and were dropped from the final model. Individuals who self-reported that their physician recommended a weight loss program were 1.74 times more likely to report participating in one.
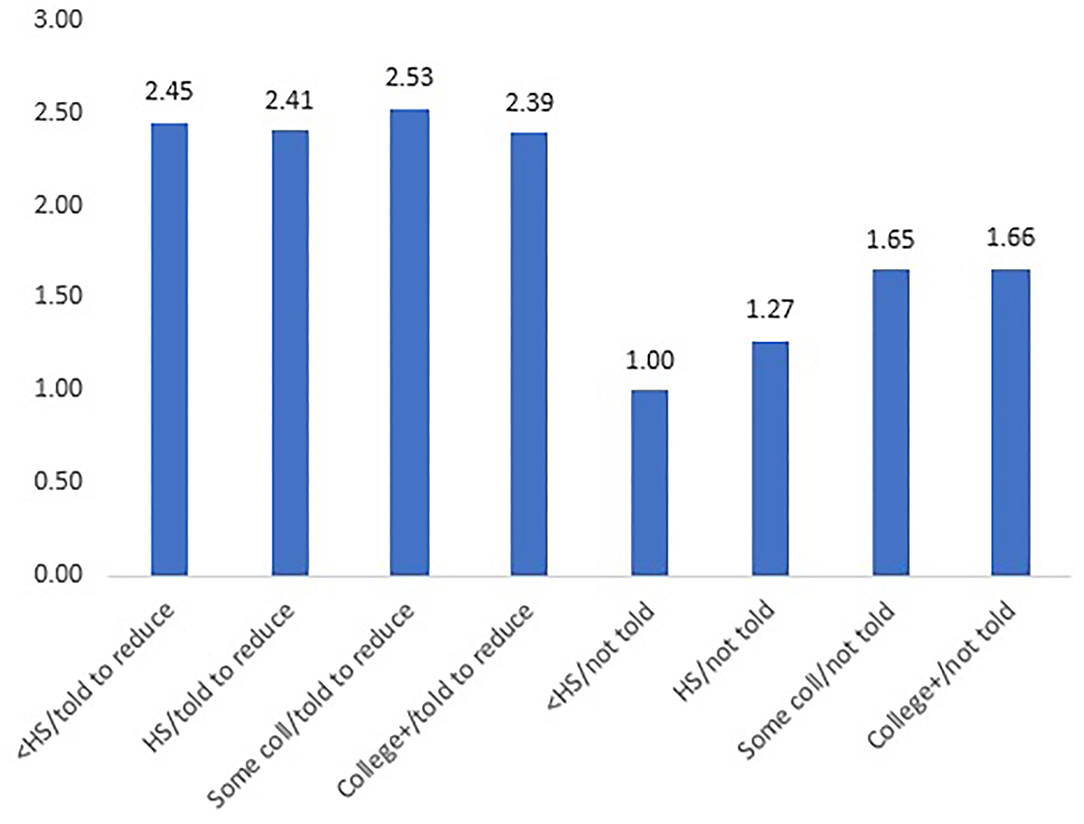
Figure 2. Prevalence ratios of attempting to reduce calories, by education and whether doctor advised to decrease calories. < HS, less than high school diploma; HS, high school diploma; Some coll, some college; College+, college degree or higher; Prevalence ratio for each bar derived from interaction of poisson regression coefficients between doctor's recommendation to reduce calories and education level; Reference group, less than a HS diploma who were not told to reduce calories.
Discussion
This cross-sectional study highlighted the modest, yet meaningful, role of physician advice for behavior changes among MSD patients. Those who were advised to exercise more, participate in weight loss programs, and reduce calories and fat were more likely to do so compared to patients who were not. These findings are consistent with previous research addressing non-musculoskeletal patient compliance to similar health promoting behavior changes (10, 11, 28). For increasing physical activity and reducing calories, physician recommendation for behavior change was an important factor that attenuated educational disparities in these behaviors.
Physicians have a vital role in counseling patients and have the opportunity at each encounter to educate their patients. In a study using National Health and Nutrition Examination Survey, Pool et al. reported that patients who had their obesity addressed by their physicians were two times more likely to report a 5% weight loss compared to patients whose physicians did not (29). The current study shows that about half of respondents report that their physician has told them to increase physical activity, whereas about 12–15% report their physician has recommended a weight loss program. This suggests that some physicians may be missing opportunities to advise MSD patients on the benefits of lifestyle changes or patients are not receiving messages that are conveyed to them. More comprehensive dissemination of these recommendations can produce significant risk factor reductions and thus serves as an important method for helping prevent and treat MSDs (5–7, 30).
Several studies have supported that educational interventions mitigating risk factors help prevent workers from developing MSDs (12–14). The current study supports the idea that the educational baseline of patients has an impact on compliance with physician advice. However, this association is complex and further investigation is needed to understand the factors that may cause the positive trend between educational background and compliance. For example, if misunderstanding of advice or patient distrust with their doctors are different among the education groups, which may impact compliance (31, 32). More targeted approaches based on education level may increase the efficacy of physician recommendations for behavioral change.
Patient perception also complicates compliance relationships. Whereas, healthcare providers may prioritize compliance, patients may have higher priorities such as controlling symptoms, preventing medical emergencies, maintaining financial stability, or enjoying a quality lifestyle (33). Lifestyle behavior change recommendations for patients suffering especially from chronic diseases may not all align with their best interests (33). Variations in patient perception for what is best for them may help explain why there was a significant impact of education on increasing physical activity and decreasing fat/calories, but not enrolling in a weight loss program. Further investigation is needed to understand the patient perspective on following advice and how educational attainment may impact how patients perceive what is best for them. As our models indicate, understanding reported patient compliance with physician recommendation may also be impacted by gender, race/ethnicity, and age. Previous investigations have indicated that men exhibit a lower degree of medical compliance compared to women (34). Additionally, race/ethnicity analyses showed that European Americans reported significantly better compliance than Asian Americans and Hispanics (34). Such factors add to the complexity of understanding patient perception and thus compliance.
This study is limited by its survey-based self-report nature, and therefore, recall bias may be possible in relation to patient recall of doctor's recommendations and patient reports of health behaviors. The cross-sectional nature of this study does not allow us to establish causation among reported advice, reported behavior change, or education level, as we do not know the timing of the recommendation relative to the report of attempted behavior change. Additionally, other factors such as age, race/ethnicity, and gender may impact the efficacy of behavior change recommendations and deserve exploration in future studies. Lastly, patients may have received more than one behavior change advice. Separating the three advice categories such that there was no overlap in advice given to subjects was not possible due to issues with sample size. The strength of this study is that the subpopulation of individuals whose musculoskeletal symptoms cause difficulty with daily activities is derived from a large, nationally representative sample of non-institutionalized US adults. As such, the sample may be more representative of US adults broadly experiencing such symptoms, including those actively being treated and those who have not or will not seek treatment for their symptoms.
The findings suggest that physician advice for risk factor management to prevent MSDs and improve patient outcomes should not be discounted. Doctors should strive to provide their patients with a sufficient understanding of the benefits of a regimen and how to follow the proposed regimen. This compliance may also apply to beyond the clinic. Spreading awareness of modifying behaviors to reduce risk factors in the community may greatly reduce the prevalence of musculoskeletal conditions. The educational background of a patient should also be considered when treating for MSD, and different approaches may be needed when addressing differently educated patients to maximize their compliance and understanding of advice.
Conclusion
Physician advice for lifestyle behavior change increased the likelihood for MSD patients to increase physical activity, decrease fat and calories, and participate in a weight loss program. Additionally, education differences were attenuated when patients were told by their physician to increase physical activity or decrease fat and calories. This demonstrates the importance of physician communication with their patients for advocating healthy behaviors, regardless of education level. Compliance with advice was affected by education for increasing physical activity. This relationship is complex and warrants future investigation for possible explanations.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found at: https://www.cdc.gov/nchs/nhis/nhis_2017_data_release.htm.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JC: conceptualization, methodology, validation, investigation, writing—original draft, and writing—review and editing. JD: conceptualization, methodology, formal analysis, investigation, writing—original draft, and writing—review and editing. JS: conceptualization and writing—review and editing. C-LS: conceptualization, writing—review and editing, and supervision. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the Texas Tech University Health Sciences Center Office of the School of Medicine Dean for helping cover the publication cost.
References
1. United States Bone and Joint Initiative: The Burden of Musculoskeletal Diseases in the United States (BMUS). 4th ed. Rosemont, IL (2020). Available online at: https://www.boneandjointburden.org/fourth-edition/ib0/prevalence-select-medical-conditions (accessed May 15, 2021).
2. Perruccio AV, Yip C, Badley EM, Power JD. Musculoskeletal disorders: a neglected group at public health and epidemiology meetings? Am J Public Health. (2017) 107:1584–5. doi: 10.2105/AJPH.2017.303990
3. Sullivan MJ, Ward LC, Tripp D, French DJ, Adams H, Stanish WD. Secondary prevention of work disability: community-based psychosocial intervention for musculoskeletal disorders. J Occup Rehabil. (2005) 15:377–92. doi: 10.1007/s10926-005-5944-7
4. Dean E, Soderlund A. What is the role of lifestyle behaviour change associated with non-communicable disease risk in managing musculoskeletal health conditions with special reference to chronic pain? BMC Musculoskelet Disord. (2015) 16:87. doi: 10.1186/s12891-015-0545-y
5. Jones G, Winzenberg TM, Callisaya ML, Laslett LL. Lifestyle modifications to improve musculoskeletal and bone health and reduce disability–a life-course approach. Best Pract Res Clin Rheumatol. (2014) 28:461–78. doi: 10.1016/j.berh.2014.07.004
6. Kirsch Micheletti J, Blafoss R, Sundstrup E, Bay H, Pastre CM, Andersen LL. Association between lifestyle and musculoskeletal pain: cross-sectional study among 10,000 adults from the general working population. BMC Musculoskelet Disord. (2019) 20:609. doi: 10.1186/s12891-019-3002-5
7. Kotowski SE, Davis KG. Influence of weight loss on musculoskeletal pain: potential short-term relevance. Work. (2010) 36:295–304. doi: 10.3233/WOR-2010-1031
8. Hutting N, Johnston V, Staal JB, Heerkens YF. Promoting the use of self-management strategies for people with persistent musculoskeletal disorders: the role of physical therapists. J Orthop Sports Phys Ther. (2019) 49:212–5. doi: 10.2519/jospt.2019.0605
9. Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care–the growing importance of the community health center. N Engl J Med. (2010) 362:2047–50. doi: 10.1056/NEJMp1003729
10. Rose SA, Poynter PS, Anderson JW, Noar SM, Conigliaro J. Physician weight loss advice and patient weight loss behavior change: a literature review and meta-analysis of survey data. Int J Obes. (2013) 37:118–28. doi: 10.1038/ijo.2012.24
11. Levesque A, Li HZ, Pahal JS. Factors related to patients' adherence to medication and lifestyle change recommendations: data from Canada. Int J Psychol Stud. (2012) 4:42–55. doi: 10.5539/ijps.v4n2p42
12. Abareshi F, Yarahmadi R, Solhi M, Farshad AA. Educational intervention for reducing work-related musculoskeletal disorders and promoting productivity. Int J Occup Saf Ergon. (2015) 21:480–5. doi: 10.1080/10803548.2015.1087729
13. Wong EM, Chan SW, Chair SY. Effectiveness of an educational intervention on levels of pain, anxiety and self-efficacy for patients with musculoskeletal trauma. J Adv Nurs. (2010) 66:1120–31. doi: 10.1111/j.1365-2648.2010.05273.x
14. Vyas R. Mitigation of musculoskeletal problems and body discomfort of agricultural workers through educational intervention. Work. (2012) 41(Suppl. 1):2398–404. doi: 10.3233/WOR-2012-0473-2398
15. Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. (2001) 26:331–42. doi: 10.1046/j.1365-2710.2001.00363.x
16. Iuga AO, McGuire MJ. Adherence and health care costs. Risk Manag Healthc Policy. (2014) 7:35–44. doi: 10.2147/RMHP.S19801
17. Hoffmann RL, Rohrer WM III, South-Paul JE, Burdett R, Watzlaf VJ. The effects of barriers on Health Related Quality of Life (HRQL) and compliance in adult asthmatics who are followed in an urban community health care facility. J Community Health. (2008) 33:374–83. doi: 10.1007/s10900-008-9108-6
18. Buchbinder R, Hall S, Youd JM. Functional health literacy of patients with rheumatoid arthritis attending a community-based rheumatology practice. J Rheumatol. (2006) 33:879–86.
19. Gordon MM, Hampson R, Capell HA, Madhok R. Illiteracy in rheumatoid arthritis patients as determined by the Rapid Estimate of Adult Literacy in Medicine (REALM) score. Rheumatology. (2002) 41:750–4. doi: 10.1093/rheumatology/41.7.750
20. Swearingen CJ, McCollum L, Daltroy LH, Pincus T, Dewalt DA, Davis TC. Screening for low literacy in a rheumatology setting: more than 10% of patients cannot read “cartilage,” “diagnosis,” “rheumatologist,” or “symptom”. J Clin Rheumatol. (2010) 16:359–64. doi: 10.1097/RHU.0b013e3181fe8ab1
21. Hirsh JM, Boyle DJ, Collier DH, Oxenfeld AJ, Nash A, Quinzanos I, et al. Limited health literacy is a common finding in a public health hospital's rheumatology clinic and is predictive of disease severity. J Clin Rheumatol. (2011) 17:236–41. doi: 10.1097/RHU.0b013e318226a01f
22. Lowe W, Ballinger C, Protheroe J, Lueddeke J, Nutbeam D, Armstrong R, et al. Effectiveness of musculoskeletal education interventions in people with low literacy levels: a systematic review. Arthritis Care Res. (2013) 65:1976–85. doi: 10.1002/acr.22085
23. About the National Health Interview Survey. Available online at: https://www.cdc.gov/nchs/nhis/about_nhis.htm (accessed May 10, 2021).
25. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. (2004) 159:702–6. doi: 10.1093/aje/kwh090
26. Stata svy Estimation. Available online at: https://www.stata.com/manuals13/svysvyestimation.pdf (accessed June 2, 2021).
27. Martinez BAF, Leotti VB, Silva GSE, Nunes LN, Machado G, Corbellini LG. Odds ratio or prevalence ratio? An overview of reported statistical methods and appropriateness of interpretations in cross-sectional studies with dichotomous outcomes in veterinary medicine. Front Vet Sci. (2017) 4:193. doi: 10.3389/fvets.2017.00193
28. Dorsey R, Songer T. Lifestyle behaviors and physician advice for change among overweight and obese adults with prediabetes and diabetes in the United States, 2006. Prev Chronic Dis. (2011) 8:A132.
29. Pool AC, Kraschnewski JL, Cover LA, Lehman EB, Stuckey HL, Hwang KO, et al. The impact of physician weight discussion on weight loss in US adults. Obes Res Clin Pract. (2014) 8:e131–9. doi: 10.1016/j.orcp.2013.03.003
30. da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med. (2010) 53:285–323. doi: 10.1002/ajim.20750
32. Association AM. 8 reasons patients don't take their medications American Medical Association. American Medical Association (2020). Available online at: https://www.ama-assn.org/delivering-care/patient-support-advocacy/8-reasons-patients-dont-take-their-medications (accessed June 2, 2021).
33. Roberson MHB. The meaning of compliance: patient perspectives. Qualit Health Res. (1992) 2:7–26. doi: 10.1177/104973239200200102
Keywords: lifestyle medicine, education, compliance, behavior change, musculoskeletal disorder (MSD)
Citation: Chen JN, Dennis JA, St. John JA and Shen C-L (2022) Self-Reported Patient Compliance With Physician Advised Lifestyle Behavior Changes Among Adults With Musculoskeletal Conditions. Front. Public Health 10:821150. doi: 10.3389/fpubh.2022.821150
Received: 23 November 2021; Accepted: 31 January 2022;
Published: 24 February 2022.
Edited by:
William Ka Fai Tse, Kyushu University, JapanReviewed by:
Brian Kinslow, Northern Arizona University, United StatesSandul Yasobant, Indian Institute of Public Health Gandhinagar (IIPHG), India
Copyright © 2022 Chen, Dennis, St. John and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jason N. Chen, amFzb24uY2hlbkB0dHVoc2MuZWR1
 Jason N. Chen
Jason N. Chen Jeff A. Dennis
Jeff A. Dennis Julie A. St. John
Julie A. St. John Chwan-Li Shen
Chwan-Li Shen