- 1School of Public Health, Southern Medical University, Guangzhou, China
- 2School of Health Management, Southern Medical University, Guangzhou, China
- 3Department of Healthcare, Guangdong Women and Children Hospital, Guangzhou, China
- 4Department of Preventive Medicine, Shantou University Medical College, Shantou, China
Background: Congenital heart defects are the most common type of birth defects and bring a heavy disease burden in China. Examining the temporal and spatial trends of congenital heart defects epidemics can give some elementary knowledge for succeeding studies.
Objective: To characterize the spatial-temporal patterns of the prevalence of congenital heart defects based on a substantial cohort of the perinatal fetus in south China in 2016–2020.
Methods: This study was a retrospective population-based cohort study conducted in Guangdong, China from 2016 to 2020. Pregnant women and their infants received birth defect surveillance during pregnancy and seven days after delivery in more than 1,900 midwifery hospitals in 21 cities. Perinatal infants with congenital heart defects were identified and enrolled. The prevalence of congenital heart defects was calculated according to cities, years, urban and rural areas, regions of Guangdong, categories of maternal age at delivery, seasons of delivery, and infant's gender.
Results: A total of 8,653,206 perinatal infants and 53,912 total congenital heart defects were monitored in Guangdong, including 46,716 (86.65%) without other defects and 7,736 (13.35%) with other defects. The average prevalence of total congenital heart defects was 62.30/10,000 (95% CI, 61.78/10,000–62.83/10,000), congenital heart defects without other defects was 53.36/10,000 (95% CI, 52.88/10,000–53.85/10,000), and congenital heart defects with other defects was 8.94/10,000 (95%CI, 8.74/10,000–9.14/10,000). From 2016 to 2020, the prevalence of total congenital heart defects was 54.92/10,000, 54.23/10,000, 63.79/10,000, 73.11/10,000, 68.20/10,000, respectively. We observed geographical variations within the prevalence of congenital heart defects. The prevalence of congenital heart defects was much higher in the Pearl River Delta region than in the non-Pearl River Delta region, as well as higher in urban areas than in rural areas.
Conclusion: The findings of this study are helpful to the understanding of the etiology and epidemiology characteristics of congenital heart defects in south China. Our data likely reflect a better estimate of the spatiotemporal trends in congenital heart defects prevalence than reported previously.
Introduction
Congenital heart defects (CHDs), the most common type of congenital disability, are defined as clinically significant structural heart and/or great vessels disease present at birth (1). About 1/4 of infants born with a heart defect have a critical CHD (2). As medical care and treatment have advanced, infants with CHDs have longer and healthier lives, but the effects of CHDs on infants are lifelong (3). CHDs can develop different health issues in patients over time, depending on their specific heart defect, the number of heart defects they have, and the severity of their heart defect (4).
A previous study showed that the prevalence of CHDs increased worldwide from 1930 to 2009, with the highest prevalence in Asia (93/10,000), followed by Europe (82/10,000), and the lowest in Africa (19/10,000) (5). Further, Wu et al. suggested that the prevalence of CHDs rose in urban and rural populations in Guangdong province from 2008 to 2012 (6). CHDs had become a worldwide major public health problem that seriously affects the quality of the birth population and is particularly severe in Asian regions (5). According to the China Birth Defect Prevention and Control Report, the prevalence of total CHDs in China was 40.95/10,000 in 2011, accounting for 26.70% of all birth defects (7). However, China has a vast territory, and the prevalence of total CHDs shows significant geographical distribution differences between different provinces. Economically developed coastal areas are higher than other inland areas in most cases (8). In addition, previous research on risk factors of four class characteristics or conditions (parental characteristics or conditions, maternal therapeutic drug exposures, parental non-therapeutic drug exposures, and parental environmental exposures.) of a variety of risk factors and that there were significant associations between multiple risk factors and CHDs, but little information is available on the potential adverse effects of these factors on fetal heart rate (4).
Guangdong province, located in southern China, has the largest GDP and resident population among all provinces in China (9). Guangdong began to carry out a birth defects surveillance project in 58 hospitals in 1986, and according to the statistics of 58 hospitals, the prevalence of total CHDs in Guangdong was 52.41/10,000 from 2008 to 2012 (6). Since 2015, Guangdong had initiated a comprehensive prevention and control project for birth defects, the surveillance scope had been extended from the previous 58 hospitals to all midwifery hospitals. All pregnant women and their infants in Guangdong should receive birth defect surveillance during pregnancy and seven days after delivery. When any midwifery hospital found perinatal birth defects, it was necessary to report the “Birth Defect Registration Card” through the Guangdong Provincial Birth Defect Surveillance System (9). Thus, based on the provincial birth defects data from 2016 to 2020, this study can accurately obtain the prevalence of total CHDs and its spatiotemporal and demographic characteristics in Guangdong, which can provide evidence for further prevention and treatment of CHDs or the development of health policies.
Methods
Data Sources and Data Collection
We used data from the Guangdong Provincial Birth Defect Surveillance System. We collected the mother's information (age, ethnicity, education level, income level, date of last menstruation, gestational week, gravidity, parity), and the perinatal infant's information (method of delivery, infant gender, birth weight, prognosis status).
The Guangdong Provincial Birth Defect Surveillance System monitored 8,653,206 perinatal infants in Guangdong, China from 2016 to 2020. Among them, we identified and enrolled a total of 53,912 perinatal infants with CHDs (ICD 10: Q20.0–Q26.4), including live births, stillbirths, and neonatal deaths within seven days.
Statistical Analysis
The prevalence of CHDs was calculated according to years, urban and rural areas, regions of Guangdong, categories of maternal age at delivery, season of delivery, and infant's gender. Descriptive statistics were used to show the essential characteristics of CHDs in infants and their mothers, including the mother's ethnicity, gravidity, parity, income level, education level, and infant's weight, gender, single or multiple births, time of diagnosis, and prognosis status. For differences in the prevalence among characteristics, the χ2 test was used to compare the prevalence of unordered categorical variables. In addition, as for the prevalence trend, because the Cochran-Armitage test is sensitive to population base, compared with linear regression analysis, the Cochran-Armitage test has more advantages when the population is large and the ordered classification variables (years) are minor. Therefore, the Cochran-Armitage test was used to explore the trend in the context of substantial monitoring data of congenital heart defects. A map was used to depict the geographical location of Guangdong in China and the geographical distribution of the four major regions in Guangdong (the Pearl River Delta (PRD) region, Eastern, Western and Northern Guangdong). We used a dot-line diagram to demonstrate the annual prevalence trend of CHDs in Guangdong from 2016 to 2020. We used maps to demonstrate the annual prevalence trend of total CHDs in 21 cities of Guangdong from 2016 to 2020. All statistical analyses were performed within the SPSS v27.0 software, and diagrams and maps were drawn by R v4.1.0 software.
Results
Figure 1 can manifest the geographical location of Guangdong as well as the four divided regions of Guangdong (Pearl River Delta, Eastern, Western, and Northern). The Pearl River Delta region is a developed region with better medical resources, while Eastern, Western, and Northern Guangdong regions are relatively underdeveloped, with insufficient and uneven distribution of medical resources.
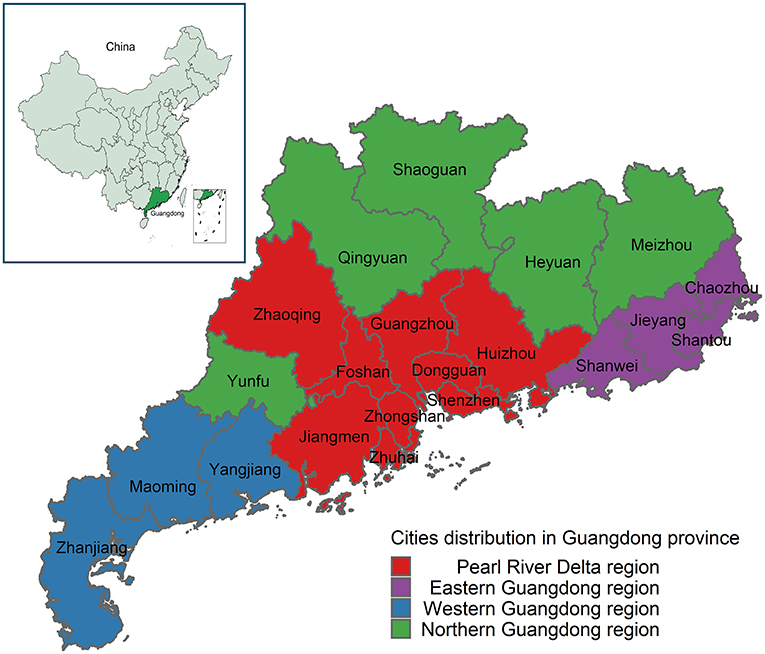
Figure 1. Geographical locations of the study area. Guangdong, which located in southern China, includes 21 cities, and divided into four regions. The Pearl River Delta region includes Guangzhou, Dongguan, Shenzhen, Huizhou, Zhaoqing, Foshan, Zhongshan, Zhuhai, and Jiangmen; Eastern Guangdong includes Shanwei, Jieyang, Shantou, and Chaozhou; Western Guangdong includes Yangjiang, Maoming, and Zhangjiang; Northern Guangdong includes Yunfu, Qingyuan, Shaoguan, Heyuan, and Meizhou.
Table 1 and Figure 2 show the prevalence trend of total CHDs in Guangdong from 2016 to 2020. During the study period, a total of 8,653,206 perinatal infants and 53,912 total CHDs were monitored in Guangdong, including 46,716 (86.65%) without other defects and 7,736 (13.35%) with other defects. The prevalence of total CHDs was 62.30/10,000 (95% CI, 61.78/10,000–62.83/10,000). The prevalence of CHDs without other defects was 53.36/10,000 (95% CI, 52.88/10,000–53.85/10,000), and the prevalence of CHDs with other defects was 8.94/10,000 (95%CI, 8.74/10,000–9.14/10,000), the prevalence of CHDs with no other defects was significantly higher than that with other defects (P < 0.001). In terms of annual prevalence, the prevalence of total CHDs showed an increasing trend (P < 0.001), with the highest prevalence in 2019 (73.11/10,000) and the lowest prevalence in 2017 (54.23/10,000). The trend in the prevalence of CHDs without other defects was similar to that of total CHDs (P < 0.001), with the highest prevalence in 2019 (62.13/10,000) and the lowest prevalence in 2017 (46.27/10,000). The prevalence of CHDs with other defects increased year by year (P < 0.001), with the highest prevalence in 2019 (10.98/10,000) and the lowest prevalence in 2016 (6.43/10,000).
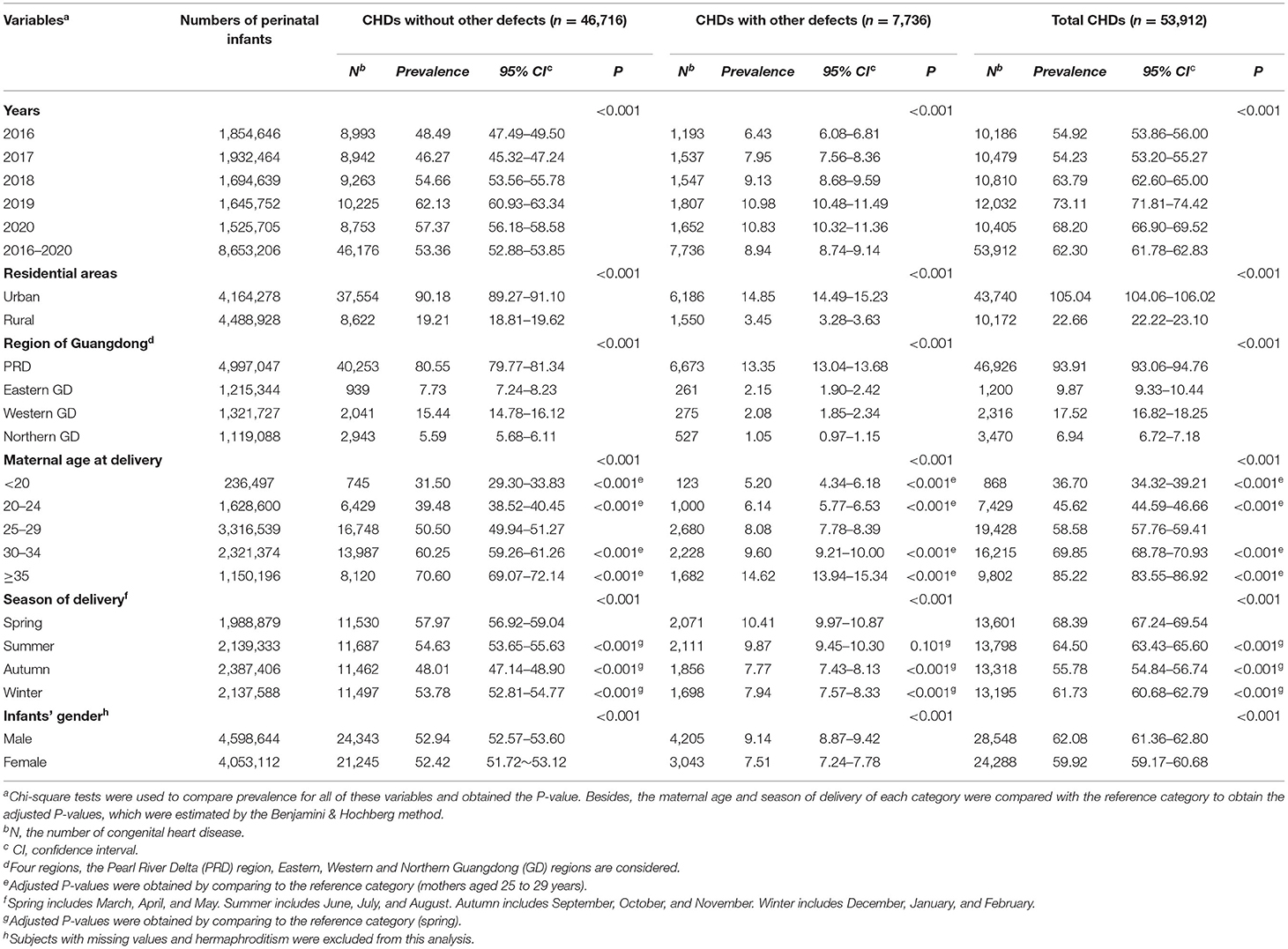
Table 1. Prevalence of congenital heart defects (CHDs) (per 10,000 perinatal infants) in Guangdong, China, 2016–2020.
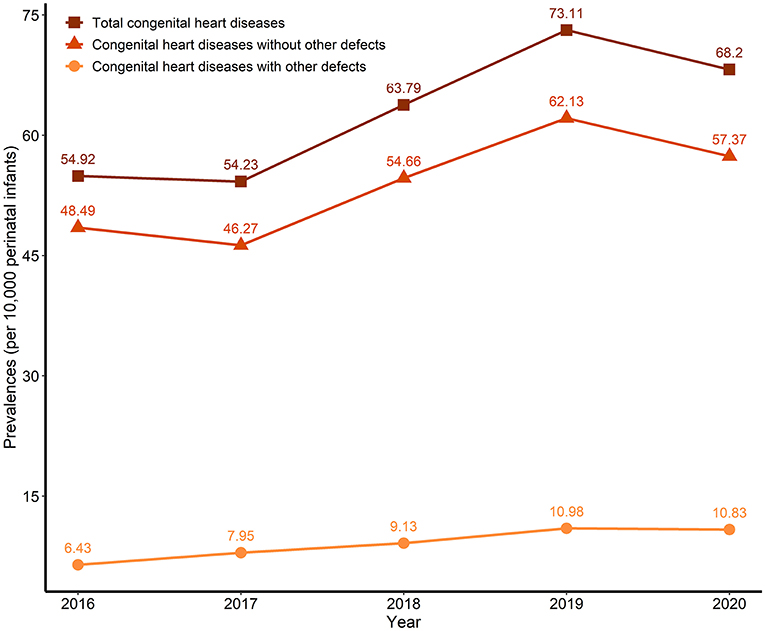
Figure 2. Trends of the prevalence of congenital heart defects (CHDs) (per 10,000 perinatal infants) in Guangdong, China, 2016–2020.
Table 1 and Supplementary Figure 1 also show the prevalence of CHDs stratified by residential areas, regions of Guangdong, maternal age at delivery, season of delivery, infants' gender. The prevalence of total CHDs was higher in urban residents than in rural residents (105.04/10,000 vs. 22.66/10,000, respectively; P < 0.001). The prevalence of total CHDs was highest in the Pearl River Delta region, followed by western Guangdong, eastern Guangdong, and lowest in northern Guangdong (93.91/10,000 vs. 17.52/10,000 vs. 9.87/10,000 vs. 6.94/10,000, respectively; P < 0.001). The prevalence of total CHDs increased with maternal age, with the highest in the ≥35 years, followed by the 30–34 years, the 25–29 years, the 20–24 years, and the lowest in the <20 years (85.22/10,000 vs. 69.85/10,000 vs. 58.58/10,000 vs. 45.62/10,000 vs. 36.70/10,000, respectively; P < 0.001). The prevalence of total CHDs was highest in spring, followed by summer, winter, and lowest in autumn (68.39/10,000 vs. 64.50/10,000 vs. 61.73/10,000 vs. 55.78/10,000, respectively; P < 0.001). Females had a higher prevalence of total CHDs than males (62.08/10,000 vs. 59.92/10,000, respectively; P < 0.001). Comparisons between different stratifications of the prevalence of CHDs without or with other defects were similar to that of total CHDs.
Table 2 shows the percentage of CHDs across different stratifications separated by characteristics of mothers and infants. Among the mothers, Han had the highest percentage in terms of ethnicity, followed by ethnic minorities (96.79 vs. 2.44%, respectively; P < 0.001). Regarding the number of pregnancies, the percentage of pregnancies ≥2 was the highest, followed by pregnancy one times (67.38 vs. 32.55%, respectively; P < 0.001). In terms of parity, the percentage of primiparous women was the highest, followed by multiparous women (55.52 vs. 42.92%, respectively; P < 0.001). In terms of season, there was little difference in the four seasons, with the highest percentage in summer, followed by spring and autumn, and the lowest in winter (25.59 vs. 25.23 vs. 24.70 vs. 24.48%, respectively; P < 0.001). In terms of income level, the percentage of ≥8,000 yuan was the highest, followed by 4,000–8,000 yuan, and the lowest was <4,000 yuan (53.57 vs. 20.73 vs. 7.76%, respectively; P < 0.001). In terms of education level, the percentage of undergraduate and above was the highest, followed by high school, and the lowest was middle school and below (32.82 vs. 26.62 vs. 23.60%, respectively; P < 0.001). Among infants with CHDs, in terms of gestational age, the percentage was highest at ≥37 weeks, followed by 28–36 weeks, and the lowest was <28 weeks (63.05 vs. 19.80 vs. 17.04%, respectively; P < 0.001). In terms of birth weight, the percentage was highest at 2,500–4,000 g, followed by <2,500 g, and the lowest was ≥4,000 g (56.90 vs. 33.08 vs. 3.59%, respectively; P < 0.001). In terms of infant gender, the percentage was highest in males, followed by females, and the lowest was hermaphroditism (52.95 vs. 45.05 vs. 0.17%, respectively; P < 0.001). In terms of multiple births, the percentage was higher in singletons than in multiple births (93.69 vs. 5.66, respectively; P < 0.001). In terms of time of diagnosis, the percentage diagnosed within seven days after delivery was higher than that diagnosed during pregnancy (69.98 vs. 26.35%, respectively; P < 0.001). In terms of prognostic outcome, the percentage of live births was highest, followed by stillbirths, and the lowest was death within seven days after delivery (77.75 vs. 18.03 vs. 0.29%, respectively; P < 0.001). Comparisons between different stratifications of the percentage of CHDs without or with other defects were similar to that of total CHDs.

Table 2. Percentage of congenital heart defects (CHDs) across different stratifications separated by characteristics of mothers and infants.
Figure 3, Supplementary Figure 2 and Supplementary Table 1 show the spatial distribution of the prevalence of total CHDs in 21 cities of Guangdong from 2016 to 2020. The prevalence of total CHDs among 21 cities in Guangdong showed significant temporal variation and spatial distribution heterogeneity throughout the study period. From 2016 to 2020, the overall prevalence of cities in the Pearl River Delta region was higher than that in other regions. Five cities were higher than the provincial average level (62.30/10,000), which were Foshan (220.05/10,000), Zhongshan (137.28/10,000), Zhuhai (101.59/10,000), Guangzhou (99.74/10,000) and Shenzhen (77.75/10,000), while the other 16 cities were lower than the provincial average level, and the lowest was Chaozhou (3.36/10,000). In 2016, the prevalence of five cities was higher than the provincial average level (54.92/10,000), which were Foshan, Zhongshan, Guangzhou, Zhuhai, and Shenzhen (186.48/10,000, 162.81/10,000, 120.94/10,000, 98.27/10,000, and 88.73/10,000, respectively), and the lowest was Chaozhou (1.82/10,000). In 2017, the prevalence of Foshan, Zhongshan, Guangzhou, Zhuhai, and Shenzhen (168.12/10,000, 126.14/10,000, 91.70/10,000, 83.08/10,000, and 71.62/10,000, respectively) were higher than the provincial average level (54.23%), and the lowest was Chaozhou (1.63/10,000). In 2018, the prevalence of Foshan, Zhongshan, Guangzhou, Zhuhai, and Shenzhen (246.53/10,000, 140.52/10,000, 100.05/10,000, 89.15/10,000, and 64.04/10,000, respectively) were higher than the provincial average level (63.79/10,000), and the lowest was Shanwei (2.78/10,000). In 2019, the prevalence of Foshan, Zhongshan, Shenzhen, Zhuhai, and Guangzhou (280.46/10,000, 140.38/10,000, 106.43/10,000, 96.83/10,000, and 82.50/10,000, respectively) were higher than the provincial average level (73.11/10,000), and the lowest was Shanwei (1.93/10,000). In 2020, the prevalence of Foshan, Zhuhai, Zhongshan, Guangzhou, Jiangmen, Heyuan, Qingyuan, and Huizhou (232.61/10,000, 161.99/10,000, 112.50/10,000, 105.81/10,000, 97.26/10,000, 83.21/10,000, 71.83/10,000, and 68.66/10,000, respectively) were higher than the provincial average level (68.20/10,000), another 13 cities were lower than the provincial average level, and the lowest was Shanwei (2.95/10,000).
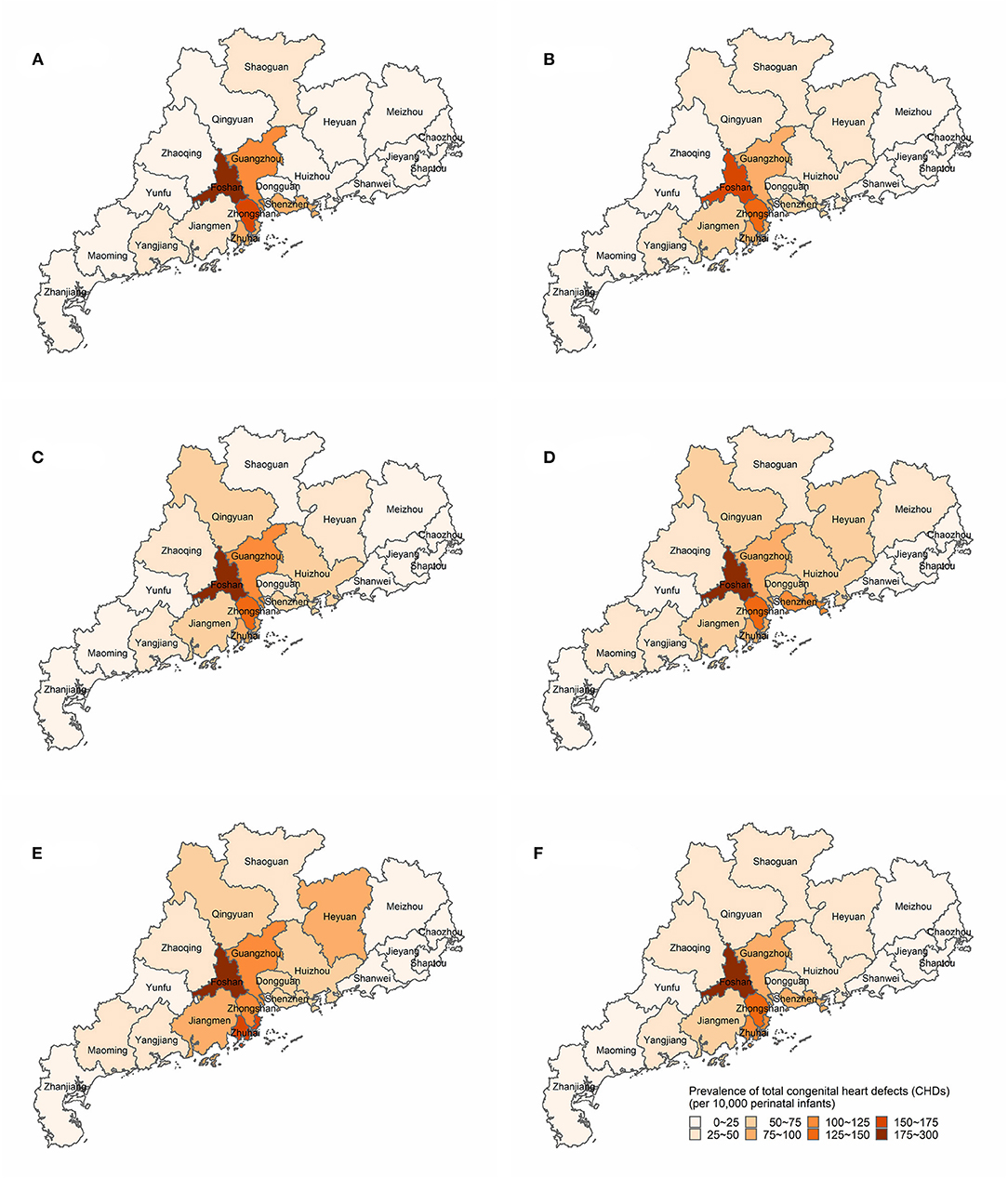
Figure 3. Spatial distributions of the prevalence of total congenital heart defects (CHDs) (per 10,000 perinatal infants) in Guangdong, China, 2016–2020. (A) Spatial distributions of total CHDs prevalence in 2016. (B) Spatial distributions of total CHDs prevalence in 2017. (C) Spatial distributions of total CHDs prevalence in 2018. (D) Spatial distributions of total CHDs prevalence in 2019. (E) Spatial distributions of total CHDs prevalence in 2020. (F) Spatial distributions of total CHDs prevalence in 2016–2020.
Discussion
Our study performed a comprehensive analysis of spatial-temporal and demographic characteristics of CHDs in Guangdong from 2016 to 2020. The main finding is that there was heterogeneity in the temporal and spatial distribution of the prevalence of CHDs, and the average prevalence of total CHDs was 62.30/10,000 in Guangdong in the past 5 years. From 2016 to 2020, the prevalence of total CHDs was increasing year by year as a whole, peaking in 2019 and slightly decreasing in 2020, but it was still at a high level. The prevalence of CHDs in urban residents was significantly higher than that in rural residents. There were also significant differences among regions in Guangdong, with the highest prevalence of CHDs in the Pearl River Delta region, followed by the western, eastern, and northern regions of Guangdong. The prevalence of CHDs increased with maternal age at delivery, and the prevalence of ≥35 years was almost twice as higher than the <25 years. The prevalence of CHDs was highest in spring, followed by summer, winter, and lowest in autumn. The prevalence of CHDs was higher in male than female infants.
The comprehensive prevention and control project of birth defects is a public health project that requires a tremendous amount of workforce, material, and financial resources. Guangdong was one of the few provinces in China to carry out this project throughout the province. In our study, the prevalence of total CHDs in Guangdong in 2016–2020 was higher than the prevalence obtained by Wu et al. using the data analysis of 58 hospitals in Guangdong in 2008–2012 (62.30/10,000 vs. 52.41/10,000, respectively), and was more accurate and comprehensive (6). Previous studies have shown that the global prevalence of CHDs is generally estimated to be 80/10,000 worldwide, but there was wide variation between countries or regions (5, 10). A study based on the European Surveillance of Congenital Anomalies Central Database found that the average prevalence of perinatal CHDs in Europe from 2000 to 2005 was about 80/10,000 (11). A Perinatal Health Surveillance Report for Congenital Defects issued by the Public Health Agency of Canada showed that the prevalence of CHDs in Canada was 85/10,000 in 2009 (12). According to the Chinese national report on birth defects (2012), the prevalence of total CHDs in China was 40.95/10,000 (7). The prevalence of total CHDs in Guangdong was slightly lower than that in Europe and the North American regions but slightly higher than the average level in China.
In terms of temporal changes, our study showed that the prevalence of total CHDs in Guangdong slightly decreased in 2017, but began to increase significantly in 2018, reached a peak in 2019, and began to decrease slightly again in 2020. This phenomenon may be related to the universal two-child policy issued by China since 2016 (13). From 2016, the number of perinatal infants began to increase considerably, reaching the peak in 2017, but the policy had not produced a cumulative effect, and the number of perinatal infants decreased year by year from 2018. Due to plenty of perinatal infants, the prevalence of CHDs slightly decreased in 2017. However, with the decrease in the number of perinatal infants and the increase in the elderly pregnant women, the prevalence of CHDs began to increase from 2018.
In terms of spatial distribution, there was significant spatial heterogeneity in the prevalence of total CHDs in Guangdong. Previous studies had shown that the distribution of the disease was not balanced, and there was spatial variability worldwide (5, 10). For instance, the prevalence of total CHDs was usually lower in North Africa, Australia, and some provinces of northern China than in South African states, Central Asia and Southeast Asia. Similarly, there were differences in the spatial distribution of prevalence in 34 provinces in China (8). Compared with some provinces in China, the prevalence of CHDs in Guangdong was lower than that in Shanghai from 2014 to 2015 (187.00/10,000) (14), but higher than that in Hunan province from 2016 to 2019 (46.00/10,000) (15). A meta-analysis study showed that the prevalence of total CHDs in China from 2015 to 2019 was 49.05/10,000, slightly lower than that in Guangdong, which may be related to the phenomenon that China has a vast territory, the prevalence in economically developed areas of the south China was higher than that in the north China, and that in the east China was higher than that in the west China (8). Moreover, the prevalence in the Pearl River Delta region was higher than that in the non-Pearl River Delta region, and the prevalence of CHDs in the areas around the Pearl River Delta region showed dynamic changes, which may be related to the local healthcare level and referral system (16). However, it is worth noting that the prevalence of CHDs in Foshan had remained high, and the prevalence was two or three times the provincial average level. The high prevalence should arouse the vigilance of health administrative authorities, find the relevant influencing factors, and take complementary strategies to reduce the prevalence. The prevalence in Chaozhou and Shanwei in eastern Guangdong were too low, suggesting that it may be that the local surveillance ability was insufficient and the diagnosis and treatment ability of CHDs needs to be further improved.
There were significant differences between maternal age at delivery, urban and rural areas, and infant gender in Guangdong for different stratifications. Our findings indicated that with increasing maternal age at delivery, the prevalence of CHDs increases, which was consistent with a study in the United States as well as the study in Hunan province (15, 17). At the same time, significant risk factors for CHDs in perinatal infants may also include increased parental age, but this speculation does not have sufficient evidence of association (18, 19). In addition, in our study, the prevalence of CHDs was significantly lower in rural areas than in urban areas, and female infants had a lower prevalence of CHDs than male infants, which are consistent with the study in Hunan province (15). This may be due to the insufficient surveillance ability of CHDs in rural areas, or due to the developed transportation network, referral network and tiered diagnosis and treatment system in Guangdong, pregnant women in rural areas mostly choose to visit large hospitals in urban areas when they found fetuses with CHDs (20, 21).
Strengths and Limitations
The advantage of this study was that based on the data of all midwifery hospitals throughout Guangdong, including live births, stillbirths, and perinatal infants who died within seven days after delivery, the trend and spatial distribution of the prevalence of CHDs over the years can be accurately obtained, which can help provide evidence to formulate targeted public health policies, carry out unique prevention and control projects for CHDs, and improve the prevention awareness of the majority of women at childbearing age in the future.
However, this research does have some limitations. Above all, this study was only a descriptive analysis in order to investigate the spatiotemporal distribution of CHDs in Guangdong. Thus, it does not provide a definite causal relationship between the disease and those spatiotemporal features. In addition, because it is challenging to perform precise measurements of some exposures (e.g., occupational and environmental exposures), such potential factors were not included in this study, although they might affect the spatiotemporal distribution of the disease (4).
Conclusions
In conclusion, our study analyzed a total of 8,653,206 perinatal infants to reveal the spatial-temporal and demographic characteristics of the prevalence of CHDs in Guangdong, China from 2016 to 2020. Further studies should be devoted to strengthening the prevention and treatment of CHDs, which will help reduce the prevalence of the disease and improve the life quality of patients.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Guangdong Women and Children Hospital. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
YZ, HM, QZ, ZS, YX, LS, and DC: acquisition, analysis, or interpretation of data. HM, QZ, and ZS: drafting of the manuscript. HM: statistical analysis. DW and YZ: obtained funding and supervision. PG: anadministrative, technical, or material support. All authors: concept and design. All authors contributed to the article and approved the submitted version.
Funding
The study was partly funded by the Project of the accounting of total health expenditure in Guangdong Province, the Philosophy and Social Sciences Research Project of Guangdong College (No. 2015WSYS0010), the Public Health Service System Construction Research Foundation of Guangzhou (2021–2023), and Medical Scientific Research Foundation of Guangdong of China (Nos. A2021094 and C2020032). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.813916/full#supplementary-material
References
1. Bernier PL, Stefanescu A, Samoukovic G, Tchervenkov CI. The challenge of congenital heart disease worldwide: epidemiologic and demographic facts. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. (2010) 13:26–34. doi: 10.1053/j.pcsu.2010.02.005
2. Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics. (2013) 131:e1502–8. doi: 10.1542/peds.2012-3435
3. Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, et al. Non-inherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American heart association council on cardiovascular disease in the young: endorsed by the American academy of pediatrics. Circulation. (2007) 115:2995–3014. doi: 10.1161/CIRCULATIONAHA.106.183216
4. Patel SS, Burns TL. Non-genetic risk factors and congenital heart defects. Pediatr Cardiol. (2013) 34:1535–55. doi: 10.1007/s00246-013-0775-4
5. van Der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. (2011) 58:2241–7. doi: 10.1016/j.jacc.2011.08.025
6. Wu L, Li B, Xia J, Ji C, Liang Z, Ma Y, et al. Prevalence of congenital heart defect in Guangdong, 2008–2012. BMC Public Health. (2014) 14:152. doi: 10.1186/1471-2458-14-152
7. Ministry of Health of the People's Republic of China. The Chinese national report on birth defects (2012). Available online at: http://www.gov.cn/gzdt/att/att/site1/20120912/1c6f6506c7f811bacf9301.pdf (accessed October 10, 2021)
8. Zhao L, Chen L, Yang T, Wang T, Zhang S, Chen L, et al. Birth prevalence of congenital heart disease in China, 1980–2019: a systematic review and meta-analysis of 617 studies. Eur J Epidemiol. (2020) 35:631–42. doi: 10.1007/s10654-020-00653-0
9. Zhu Y, Miao H, Zeng Q, Li B, Wang D, Yu X, et al. Prevalence of cleft lip and/or cleft palate in Guangdong, China, 2015–2018: a spatio-temporal descriptive analysis. BMJ Open. (2021) 11:e046430. doi: 10.1136/bmjopen-2020-046430
10. GBD 2017 Congenital Heart Disease Collaborators. Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Child Adolesc Health. (2020) 4:185–200. doi: 10.1016/S2352-4642(19)30402-X
11. Dolk H, Loane M, Garne E. Congenital heart defects in Europe: prevalence and perinatal mortality, 2000 to 2005. Circulation. (2011) 123:841–9. doi: 10.1161/CIRCULATIONAHA.110.958405
12. Irvine B, Luo W, León JA. Congenital anomalies in Canada 2013: a perinatal health surveillance report by the public health agency of canada's canadian perinatal surveillance system. Health Promot Chronic Dis Prev Can. (2015) 35:21–2. doi: 10.24095/hpcdp.35.1.04
13. Zang S, OuYang J, Zhao M, Zhu Y, Liu J, Wang X. Factors associated with child delivery expenditure during the transition to the national implementation of the two-child policy in China. Health Qual Life Outcomes. (2021) 19:30. doi: 10.1186/s12955-021-01678-z
14. Zhang Y, Riehle-Colarusso T, Correa A, Li S, Feng X, Gindler J, et al. Observed prevalence of congenital heart defects from a surveillance study in China. J Ultrasound Med. (2011) 30:989–95. doi: 10.7863/jum.2011.30.7.989
15. Xie D, Fang J, Liu Z, Wang H, Yang T, Sun Z, et al. Epidemiology and major subtypes of congenital heart defects in Hunan Province, China. Medicine. (2018) 97:e11770. doi: 10.1097/MD.0000000000011770
16. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. (2002) 39:1890–900. doi: 10.1016/s0735-1097(02)01886-7
17. Miller A, Riehle-Colarusso T, Siffel C, Frías JL, Correa A. Maternal age and prevalence of isolated congenital heart defects in an urban area of the United States. Am J Med Genet A. (2011) 155A:2137–45. doi: 10.1002/ajmg.a.34130
18. Olshan AF, Schnitzer PG, Baird PA. Paternal age and the risk of congenital heart defects. Teratology. (1994) 50:80–4. doi: 10.1002/tera.1420500111
19. Joinau-Zoulovits F, Bertille N, Cohen JF, Khoshnood B. Association between advanced paternal age and congenital heart defects: a systematic review and meta-analysis. Hum Reprod. (2020) 35:2113. doi: 10.1093/humrep/deaa105
20. Wu Y, Zhou H, Wang Q, Cao M, Medina A, Rozelle S. Use of maternal health services among women in the ethnic rural areas of western China. BMC Health Serv Res. (2019) 19:179. doi: 10.1186/s12913-019-3996-2
Keywords: congenital heart diseases, perinatal infants, spatial, temporal, prevalence
Citation: Miao H, Zeng Q, Shi Z, Xia Y, Shi L, Chen D, Guo P, Zhu Y and Wang D (2022) Spatio-Temporal Distribution and Demographic Characteristics of Congenital Heart Defects in Guangdong, China, 2016–2020. Front. Public Health 10:813916. doi: 10.3389/fpubh.2022.813916
Received: 12 November 2021; Accepted: 01 April 2022;
Published: 26 April 2022.
Edited by:
Muhammad Tariq, University of Tabuk, Saudi ArabiaReviewed by:
Lifei Wang, University of Toronto, CanadaRashid Mir, University of Tabuk, Saudi Arabia
Copyright © 2022 Miao, Zeng, Shi, Xia, Shi, Chen, Guo, Zhu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yingxian Zhu, emh1eXgyMDIxQDE2My5jb20=; Dong Wang, ZG9uZ3c5NkBzbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Huazhang Miao
Huazhang Miao Qinghui Zeng
Qinghui Zeng Zengping Shi
Zengping Shi Yi Xia
Yi Xia Lushaobo Shi
Lushaobo Shi Dongxue Chen
Dongxue Chen Pi Guo
Pi Guo Yingxian Zhu
Yingxian Zhu Dong Wang
Dong Wang