
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 08 March 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.809568
This article is part of the Research TopicOral Health, Oral Diseases and Nutrition in ChildrenView all 5 articles
Background: Oral health literacy (OHL) has been recognized as a component of oral health disparities; however, the precise relationship between literacy and oral health outcomes has not been established. To explore the role of parents' OHL for their own subjective oral health, related behavior, and for the proxy assessment of their child's oral health, oral health-related behavior.
Methods: Survey data were collected from 406 parents of 4- to 7-year-old children in Beijing, China. The background characteristics, oral health assessment, oral health-related behavior, knowledge and attitudes, and diet-related questions of parents and their children were surveyed by a questionnaire. OHL was assessed with the Hong Kong Rapid Estimate of Adult Literacy in Dentistry (HKREAL-30) Scale and a revised version that asked the respondents to indicate if they understood the words (HKREALD-30-Understand).
Results: The HKREALD-30 responses correlated with the HKREALD-30-Understand responses. The higher the parents' HKREALD-30-Understand scores, the better they described the health of their own teeth and gums, the greater their child's diet was influenced by the protein, sugar and calories of the food, and the more positive their oral health-related attitudes were. The higher the parent's HKREALD-30 scores, the healthier they described their child's teeth and gums.
Conclusions: Both the HKREALD-30 and HKREALD-30-Understand Scores correlate with parents' self and proxy oral health-related responses. Chinese parents could understand that the word would add predictive value to the prediction of how parents' oral health literacy affects their own oral health care, children's oral health and other related aspects.
Previous evidence has proven the prevalence of low literacy in health care settings and its adverse influence on health outcomes (1, 2). Low general health literacy is associated directly and indirectly with a range of poor health outcomes, not only because it is related to risk factors for poor health care but also because it affects patients' utilization of health care services, their cooperation with treatment recommendations, and their health-related behavior in general (3–6). Oral health-related literacy studies began later and were especially influenced by the fact that an oral health literacy instrument was developed in 2007, the Rapid Estimate of Adult literacy in Dentistry (REALD-30) (7).
One very important consideration was how parents' level of oral health literacy would affect their own oral health and the oral health of their children. Although the precise relationship between literacy and oral health outcomes has not been established (8–11), OHL has been increasingly recognized as a component of oral health disparities. Related studies revealed that the better parents' oral health literacy was, the better their own oral health (12, 13), and the better their children's oral health (10, 14). Low parental OHL was associated with low oral conditions among their children (9, 15–18). Studies have also demonstrated an association between decreased parental OHL and worse oral health behaviors, which had an adverse impact on children's oral health-related quality of life (19). Meanwhile, only a few studies have explored oral health-related behaviors. Common oral health-related behaviors such as brushing, flossing and regular dental visits need to be further evaluated.
Diet-related behavior has been studied extensively in the medical field. Because adults with limited literacy skills have difficulty interpreting and acting on health information that could reduce their risk factors and related symptoms, it is not surprising that people with low health literacy have poor disease management and diet-related behaviors in chronic illnesses (20, 21). Studies have also shown that diet-related attitudes are associated with health literacy and could predict diet-related behaviors and dietary quality (22). Less well educated, poorer and sicker people know less about where to look for dieted-related information and are less likely to attempt finding it (23). Therefore, we hypothesized that the poor oral health literacy population would not have a healthy diet-related attitude and behavior toward keeping their teeth healthy.
The importance of literacy in dentistry has attracted increasing attention. However, limited research has focused on oral health literacy among the Chinese population (24). The majority of oral health literacy instruments, such as REALD-30, were developed in English for North American contexts and cannot be used directly in Chinese-speaking groups, which limited the related studies. In 2012, Wong et al. (25) developed a measurement instrument, the Hong Kong Rapid Estimate of Adult Literacy in Dentistry (HKREALD-30), which is valid and reliable for the basic screening of oral health literacy among Chinese people. Therefore, it is a perfect time to utilize this instrument to see if oral health literacy in China would also be related.
Based on these considerations, the objectives of this study are to explore the role of parents' OHL in their own subjective oral health and related behavior and for the proxy assessment of their child's oral health, oral health-related behavior.
This study followed the STROBE guideline checklist (26), with ethical approval obtained from the Peking University School and Hospital of Stomatology Ethics Committee (PKUSSIRB-201839139).
Data were collected from five hundred and one parent of children who participated in the regular dental examination, which was held in the daycare by dentists from Peking University School and Hospital of Stomatology in 2018. The parents were informed that a regular dental examination would be held at the daycare by dentists from Peking University School and Hospital of Stomatology and that an anonymous survey would be handed out after the examination. The parents who wanted to participate received the survey when they picked up their child, responded at home and returned the survey back the next day.
The survey mainly consisted of three variables: OHL, parent's oral health status, and children's oral health status. The detailed questionnaire is supplied in the Supplementary Materials. The variables extracted from the questionnaires were representative oral health assessment and related factors, which were further statistically analyzed with regard to their relationships with OHL score. Detailed information on the grading standard of each variable is presented in Supplementary Table 1. OHL was assessed by the HKREAL-30 Scale, which contains 30 Chinese words and was developed to assess oral health literacy among Chinese people. The parents were asked to check the words they could pronounce correctly and the words they understood the meaning. The mean score of each item and the mean sum score were calculated. The oral health status and related factors of parents and their children were assessed by their background characteristics, self-reported oral health, oral health-related behavior, knowledge and attitudes. The background characteristics included their gender, age, and years of education. Oral health-related behavior, knowledge and attitudes consisted of questions concerning parents' and their children's oral health, their frequency of brushing, flossing and dental visits, and the types of dental treatments they had received. The score ranges from 1 to 5, and a higher score indicates more positive. The mean and standard deviation of these questions were calculated. Furthermore, we survey the children's diet-related questions. The parents were asked to check on a list of 25 different foods and beverages that were often seen in the Chinese diet that their child had consumed during the past 24 hours. In addition, an open-ended question asked which other food their child had eaten in the past 24 hours; other questions inquired whether the child usually ate breakfast and how the costs and information about the food influenced their decision when ate out.
The parents' paper-pencil survey responses were entered into SPSS (Version 22). Descriptive statistics such as frequency distributions, percentages, means, standard deviations, and ranges were computed to provide an overview of the responses. Pearson correlation coefficients were used to determine the relationship between the constructs of interest. P < 0.05 was considered as significant.
There were 406 valid responses among 501 returned survey questionnaires. The respondents ranged in age from 26 to 48 years (Mean: 35.86, SD: 3.68). When the parents responded concerning the children's background characteristics, 52% were male, and the children ranged in age from 4 to 7 years (mean: 5.12, SD: 1.05). A detailed overview of the parents' and children's background characteristics is supplied in Supplementary Table 2.
Table 1 provides an overview of the respondents' answer scores concerning their own and their child's oral health and oral health-related knowledge, attitudes, and attitudes toward children's diet. The score ranges from 1 to 5, and a higher score indicates a more positive result. The parent self-reported health of teeth was 3.59, and their self-reported health of their gums was 3.67. Nearly 50% responded that they had very good or excellent oral health. Concerning that the proxy response was about their child's health of teeth and gums, the scores were 3.76 and 4.11, respectively. The absolute majority of the parents (83%) brushed their teeth more than once a day. However, only 15% flossed once per day or two times per day or more. Sixty-four percent of the children brushed their teeth two or more per day. However, only 5% flossed once per day to two times per day. The fluoride and sealant knowledge scores were 3.34 and 2.12, respectively.
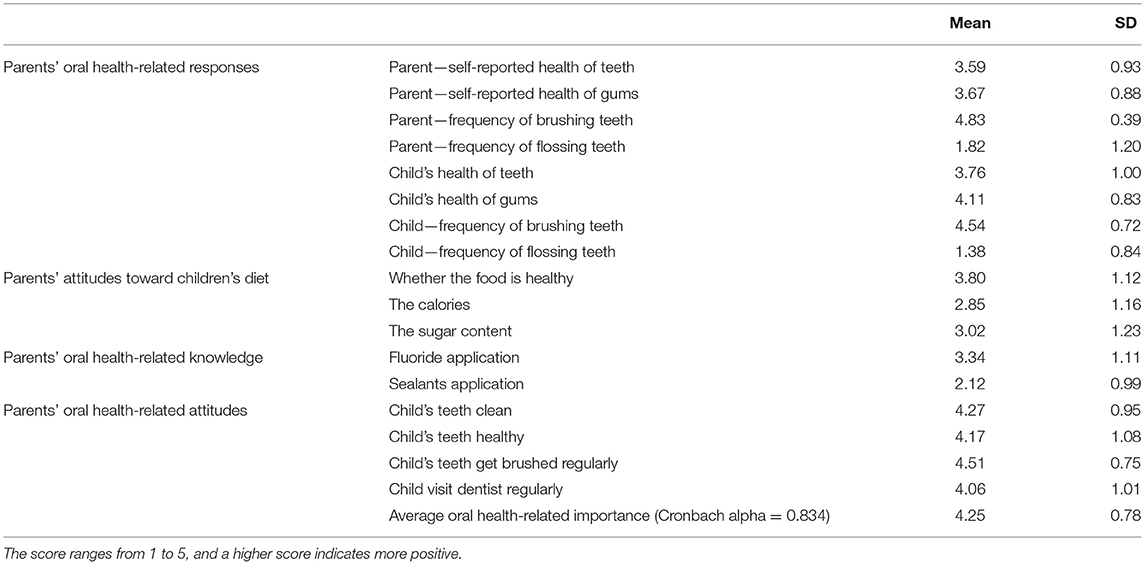
Table 1. The mean score of parents' oral health-related responses, knowledge, attitudes, and attitudes toward children's diet.
The parents' oral health-related attitudes were measured with four items that asked them how important it is for them that their child has clean teeth and healthy teeth, that the child's teeth are brushed regularly, and that the child sees a dentist regularly for check-up visits. Table 1 shows that the absolute majority of the parents held positive attitudes toward oral health.
Table 2 shows that 42% of parents had a dental visit in the past year, and on average, the majority had received checkups, cleaning, and fillings in the past. Concerning the children with dental treatment in the past, the data show that 87% had received a check-up in the past and 41% had fillings.
The parents were asked how frequently their children had one of nine protein-containing foods on all five different carbohydrate-rich foods and seven sugar-rich foods. Table 3 shows that on average, the sum of protein-rich food on the day was 4.00 in the last 24 h, the sum of carbohydrate-rich food was 2.43, and the sum of sugar-rich food was 1.18. In addition, Table 1 indicates that the scores of whether the food was healthy, the calories, and the sugar content were 3.80, 2.85, and 3.02, respectively.
To assess the parents' oral health literacy score, HKREAL-30 was provided twice. First, parents were asked if they could read each of the 30 words. Then, they were asked if they could understand each of the 30 words and understand the meaning. Table 4 shows that from these 30 items on average, the parents answered that they could read 23.91 and that they understood 17.08. Their responses concerning whether they could read the word and understand a word were significantly different in 17/30 words. Their reading and understanding overall scores correlated significantly and were equal to 0.44.
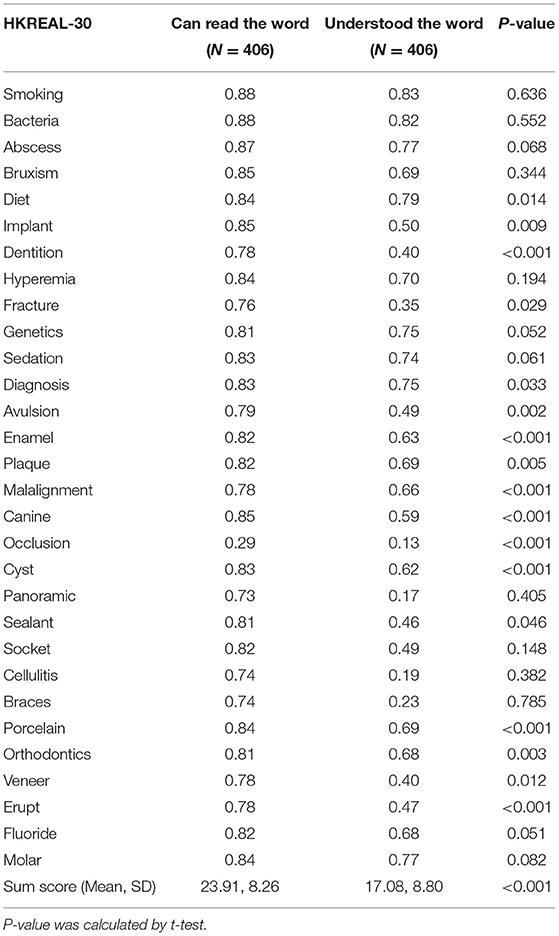
Table 4. Parents' responses concerning the Hong Kong Rapid Estimate of Adult Literacy in Dentistry (HKREAL-30) Scale.
The ultimate question of this manuscript is how oral health literacy is related to parents' and children's oral health, oral health-related behavior and parents' oral health knowledge and attitudes. Table 5 shows that when the number of words that the parents indicated they could read was significantly correlated with the child's subjective health of teeth and gums. The higher the reading oral health related literature score was, the healthier the parents described their child's health of teeth and health of gums, the more previous dental procedures that the parents had, but the fewer previous dental procedures the children had, the less sugar rich food the children ate, and the more important it was to the parents that they ate healthy food when they ate out, that they watched the calories when they ate out, and they watched the amount of sugar when they ate out. The better their reading-related oral health literacy score was, the less they thought that it is not true that fluoride can prevent caries, that it is not sure that sealant can prevent carriers, that they agreed that they know how to protect their child's teeth, and that they had positive attitudes.
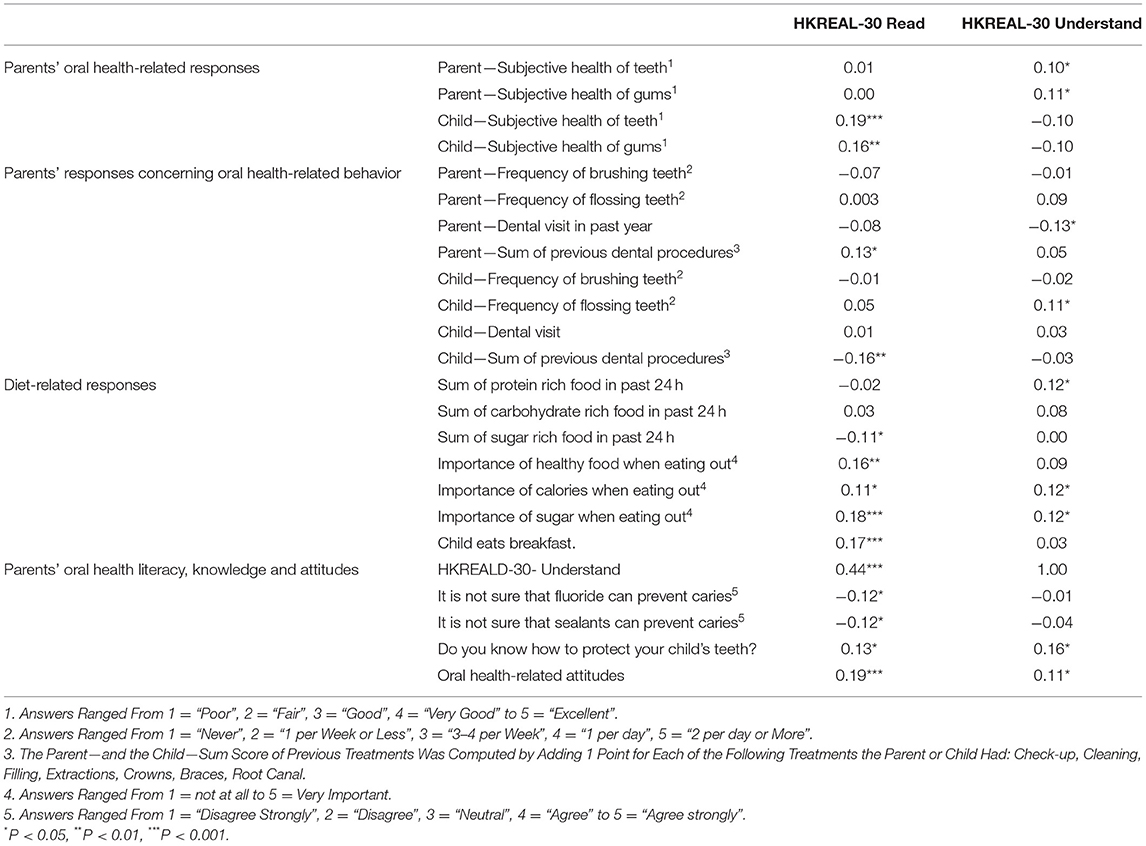
Table 5. Relationships between parents' oral health literacy and their own and their child's subjective oral health and oral health-related behavior, knowledge and attitudes.
When the parents' oral health literacy as measured with how many words they indicated they understood, the data showed that the more words they understood, the better the parents' objective health of their teeth and of gums, the more likely they had a dental visit in last year and the more likely their child's teeth get flossed, the more protein rich food their child had in the last 24 h, the more important it was to watch the calories and sugar when they ate out, and the greater they agreed that they knew how to protect their child's teeth and the more positive their oral health related attitudes.
The research contains 406 subjects, which is a good size that enabled us to test the hypothesis that we were interested in. The heterogeneity of the respondents' background characteristics was also satisfactory, as 125 fathers, which is a considerable number, participated in this research. There was a wide range in the educational degree. However, on the whole, the sample was highly educated, which may potentially limit the range of responses to oral health literacy skills, as research has proven that a higher education level is strongly associated with parents' oral health-related behavior and children's health of teeth (27–31). In addition, the income level range varies widely, meaning that the socioeconomic background of the parents ranges from a very low combined family income to a very high combined family income. Given that there is a strong relationship between oral health literacy and the family's socioeconomic status (32–36), the variety of socioeconomic backgrounds in our research would also provide us with a wide range of oral health literacy levels. There were approximately half males and half females, and they ranged in age from 4 to 7 years, with most children having primary dentition. The gender and age of our subjects also provide an ideal outlook for our study.
Parents' oral health behavior has been substantiated to affect their children's oral health behavior and oral health status (37). In our study, 83% of parents said they bush one to two times per day, meaning most of the parents were very good with brushing. However, the children did not brush as frequently as the parents. The frequency of flossing of both parents and children was very low. As reported by parents, we have a wide range of food-related responses, which allows us to look if all oral health literacy would be correlated with how much protein-, carbohydrate- and sugar-rich food they ate. The health-related attitude was evaluated by asking questions regarding when eating out what factors of parents considered important. However, only a low proportion of parents paid attention to the food composition. This phenomenon may be because of the features of Chinese food. The main components of Chinese meal are rice, flour, and various vegetables. Therefore, people are not used to pay attention to this aspect.
As shown in our study, parents' reading and understanding-based OHL was correlated with children's subjective health of teeth and gums and parents' oral health-related behaviors. The reading and understanding sum scores were correlated at the level of 0.44, which showed that what parents could read and what they understood were not necessarily correlated. When we have a closer look at each of the words we tested parents, we can see that the reading score and the understanding score of words: diet, implant, dentition, fracture, diagnosis, avulsion, enamel, plaque, mal-alignment, canine, occlusion, cyst, sealant, porcelain, orthodontics, veneer, and erupt are significantly correlated. There might be two circumstances that caused this result. The first was when the word was very uncommonly used in daily life, such as occlusion. People did not know either how to read or the meaning. Therefore, the two scores were significantly correlated. The second circumstance was that the word was composed of easy-reading characters, the term was used wildly, and even laypeople were familiar with them. Therefore, parents who could read the word also understood them. It is notable that Chinese is character-based rather than word-based, and a single character can be used as a word or meaning unit. This feature means that the examinee may read the word correctly without knowing its meaning, which is usually unlikely for English-speaking persons.
Having both reading and understanding skills measured could provide us with two different levels of inside. One would be how well they were trained to read symbols in Chinese. The other would be to understand the underlying meaning and what it means, which would be correlated with other aspects of their life. Therefore, they were both are significant. There are some findings that were completely different, such as the subjective health of the teeth and gums. The difference reveals that when parents truly have a deeper understanding, they might be better prepared to take care of their teeth and gums. Therefore, Chinese parents could understand that the word would add predictive value to the prediction of how parents' oral health literacy affects their own oral health care, children's oral health and other related aspects.
This study had some limitations. First, when testing respondents' reading-based oral health literacy, parents were asked to self-report. The accuracy of their pronunciation was not checked by one study, which might result in error. The second limitation was that the research was conducted in several university-affiliated childcare centers in the capital of Beijing. The overall educational level was high. With most parents working, the family income differed widely, but overall, it was definitely more weight toward people who potentially have higher literacy. As place of residency is also a significant factor that influences oral health-related quality of life (29), the sample was not a completely representative of the Chinese population. It would be worthwhile to look more into it in future studies, and a random sample across the spectrum of social demographic background or social status, such as low education and low-income populations, would be included.
Studies regarding health literacy in China are limited. From the handful of studies, we found that a low health literacy level in China may lead to the ignorance of risk factors and poor utilization of medical resources when having chronic diseases (38). Health literacy is the main factor affecting health promotion, and lower health literacy may lead to no treatment seeking and poor cooperation with the treatment recommendation (39, 40). It is warningly important for Chinese dentists to realize and understand the importance of oral health literacy to help patients with poor oral health literacy and ensure better oral health outcomes.
Both HKREALD-30 and HKREALD-30-Understand Scores correlate with parents' self and proxy oral health-related responses. Chinese parents could understand that the word would add predictive value to the prediction of how parents' oral health literacy affects their own oral health care, children's oral health and other related aspects.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Biomedical Ethics Committee of Peking University School and Hospital of Stomatology (PKUSSIRB-201839139). The patients/participants provided their written informed consent to participate in this study.
YW, MI, and CY conceptualized the study, performed the data analysis, wrote the manuscript, and critically revised the manuscript. CY collected the data. All authors participated in the design, interpretation of the studies, analysis of the data, and review of the manuscript.
This study was funded by Peking University School and Hospital of Stomatology (Grant Number: PKUSSNCT-20Y02) and Peking University International Strategic Partnership Fund (Medical science, 2021).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank all children and parents who participated in this research and all the dentists, nurses, and teachers who helped in conducting this project.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.809568/full#supplementary-material
OHL, Oral health literacy; HKREAL-30, Hong Kong Rapid Estimate of Adult literacy in Dentistry; HKREALD-30-Understand, Understand the words in the Hong Kong Rapid Estimate of Adult Literacy in Dentistry; REALD-30, Rapid Estimate of Adult literacy in Dentistry.
1. Kirsch I, Jungeblut A, Jenkins L, Kolstat A. Adult Literacy in America: A First Look at the Results of the National Adult Literacy Survey. Washington, DC: National Center for Education Statistics. U.S. Department of Education (1993). p. xiv.
2. Nutbeam D. Health promotion glossary. Health Promo Int. (1998) 13:349–64. doi: 10.1093/heapro/13.4.349
3. Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. (1995)10:537–41. doi: 10.1007/BF02640361
4. Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. (1995) 274:1677–82. doi: 10.1001/jama.1995.03530210031026
5. Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, et al. Health literacy among medicare enrollees in a managed care organization. JAMA. (1999) 281:545–51. doi: 10.1001/jama.281.6.545
6. Ruth P. Health literacy: a challenge for American patients and their health care providers. Health Promo Int. (2000) 15:277–83. doi.org/10.1093/heapro/15.4.277 doi: 10.1093/heapro/15.4.277
7. Lee JY, Rozier RG, Lee SY, Bender D, Ruiz RE. Development of a word recognition instrument to test health literacy in dentistry: the REALD-30–a brief communication. J Public Health Dent. (2010) 67:94–8. doi: 10.1111/j.1752-7325.2007.00021.x
8. U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. Washington, DC: U.S. Government Printing Office (2000). Available online at: http://www.health.gov/healthypeople/
9. Firmino RT, Martins CC, Faria LDS, Martins Paiva S, Granville-Garcia AF, Fraiz FC, et al. Association of oral health literacy with oral health behaviors, perception, knowledge, and dental treatment related outcomes: a systematic review and meta-analysis. J Public Health Dent. (2018) 78:231–45. doi: 10.1111/jphd.12266
10. Firmino RT, Ferreira FM, Martins CC, Granville-Garcia AF, Fraiz FC, Paiva SM. Is parental oral health literacy a predictor of children's oral health outcomes? Systematic review of the literature. Int J Paediatr. (2018) 8:459–71. doi: 10.1111/ipd.12378
11. Macek MD, Atchison KA, Watson MR, Holtzman J, Wells W, Braun B, et al. Assessing health literacy and oral health: preliminary results of a multi-site investigation. J Public Health Dent. (2016) 76:303–13. doi: 10.1111/jphd.12156
12. Parker EJ, Jamieson LM. Associations between Indigenous Australian oral health literacy and self-reported oral health outcomes. BMC Oral Health. (2010) 10:1–8. doi: 10.1186/1472-6831-10-3
13. Miller E, Lee JY, DeWalt DA, Vann WF. Impact of caregiver literacy on children's oral health outcomes. Pediatrics. (2010) 126:107–14. doi: 10.1542/peds.2009-2887
14. Lee JY, Divaris K, Baker AD, Rozier RG, Vann WF Jr. The relationship of oral health literacy and self-efficacy with oral health status and dental neglect. Am J Public Health. (2012) 102:923–9. doi: 10.2105/AJPH.2011.300291
15. Bridges SM, Parthasarathy DS, Wong HM, Yiu CK, Au TK, McGrath CP. The relationship between caregiver functional oral health literacy and child oral health status. Patient Educ Couns. (2014) 94:411–6. doi: 10.1016/j.pec.2013.10.018
16. Garrett GM. Parental functional health literacy relates to skip pattern questionnaire error and to child oral health. J Calf Dent Assoc. (2012) 40:423–30.
17. Horowitz AM, Kleinman DV. Oral health literacy: a pathway to reducing oral health disparities in Maryland. J Public Health Dent. (2012) 72:S26–30. doi: 10.1111/j.1752-7325.2012.00316.x
18. Vann WF Jr, Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: impact on oral health outcomes in early childhood. J Dent Res. (2010) 89:1395–400. doi: 10.1177/0022034510379601
19. Divaris K, Lee JY, Baker AD, Vann WF. Caregivers' oral health literacy and their young children's oral health-related quality-of-life. Acta Odontologica Scandinavica. (2012) 70:390–7. doi: 10.3109/00016357.2011.629627
20. Kim S, Love F, Quistberg DA, Shea JA. Association of Health Literacy With Self-Management Behavior in Patients With Diabetes. Diabetes Care. (2004) 27:2980–2. doi: 10.2337/diacare.27.12.2980
21. Carbone ET, Zoellner JM. Nutrition and health literacy: a systematic review to inform nutrition research and practice. J Acad Nutr Diet. (2012) 112:254–65. doi: 10.1016/j.jada.2011.08.042
22. Cha E, Kim KH, Lerner HM, Dawkins CR, Bello MK, Umpierrez G, et al. Health literacy, self-efficacy, food label use, and diet in young adults. Am J Health Behav. (2014) 39:331–9. doi: 10.5993/AJHB.38.3.2
23. Niedzwiedzka B, Mazzocchi M, Aschemann WJ, Gennaro L, Verbeke W, Traill WB. Determinants of information behaviour and information literacy related to healthy eating among Internet user in five European countries. Inform Res. (2014) 19:633.
24. Gao J, Ruan J, Zhao L, Zhou H, Huang R, Tian J. Oral health status and oral health knowledge, attitudes and behavior among rural children in Shaanxi, western China: a cross-sectional survey. BMC Oral Health. (2014) 14:144. doi: 10.1186/1472-6831-14-144
25. Wong HM, Bridges SM, Yiu CK, McGrath CP, Au TK, Parthasarathy DS. Development and validation of Hong Kong Rapid Estimate of Adult Literacy in Dentistry. J Investig Clin Dent. (2012) 3:118–27. doi: 10.1111/j.2041-1626.2012.00113.x
26. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
27. Ashkanani F, Al-Sane M. Knowledge attitudes and practices of caregivers in relation to oral health of preschool children. Med Princ Pract. (2013) 22:167–72. doi: 10.1159/000341764
28. Born CD, Divaris K, Zeldin LP, Rozier RG. Influences on preschool children's oral health-related quality of life as reported by English and Spanish-speaking parents and caregivers. J Public Health Dent. (2016) 76:276–86. doi: 10.1111/jphd.12152
29. Gaber A, Galarneau C, Feine JS, Emami E. Rural-urban disparity in oral health-related quality of life. Community Dent Oral Epidemiol. (2018) 46:132–42. doi: 10.1111/cdoe.12344
30. Horowitz AM, Kleinman DV, Wang MQ. What Maryland adults with young children know and do about preventing dental caries. Am J Public Health. (2013) 103:e69–76. doi: 10.2105/AJPH.2012.301038
31. Lee CY, Ting CC, Wu JH, Lee KT, Chen HS, Chang YY. Dental visiting behaviours among primary schoolchildren: Application of the health belief model. Int J Dent Hyg. (2018) 16:e88–95. doi: 10.1111/idh.12319
32. Wong HM, Bridges SM, Yiu CK, McGrath CP, Au TK, Parthasarathy DS. Validation of the Hong Kong Oral Health Literacy Assessment Task for Paediatric Dentistry (HKOHLAT-P). Int J Paediatr Dent. (2013) 23:366–75. doi: 10.1111/ipd.12021
33. Renzaho A, de Silva-Sanigorski A. The importance of family functioning, metal health and social and emotional well-being on child oral health. Child Care Health Dev. (2014) 40:543–52. doi: 10.1111/cch.12053
34. Mak KK, Day JR. Dental health behaviours among early adolescents in Hong Kong. Int J Dent Hyg. (2011) 9:122–6. doi: 10.1111/j.1601-5037.2010.00452.x
35. Pakpour AH, Lin CY, Kumar S, Fridlund B, Jansson H. Predictors of oral health-related quality of life in Iranian adolescents: a prospective study. J Investig Clin Dent. (2018) 9:e12264. doi: 10.1111/jicd.12264
36. Perera I, Ekanayake L. Influence of oral health-related behaviours on income inequalities in oral health among adolescents. Community Dent Oral Epidemiol. (2011) 39:345–51. doi: 10.1111/j.1600-0528.2010.00606.x
37. Okada M, Kawamura M, Kaihara Y, Matsuzaki Y, Kuwahara S, Ishidori H, et al. Influence of parents' oral health behaviour on oral health status of their school children: an exploratory study employing a causal modelling technique. Int J Paediatr Dent. (2002) 12:101–8. doi: 10.1046/j.1365-263X.2002.00338.x
38. Li X, Ning N. Hao, Y, Sun H, Gao L, Jiao M, Wu Q, Quan H. Health literacy in rural areas of China: hypertension knowledge survey. Int J Environ Res Public Health. (2013) 10:1125–38. doi: 10.3390/ijerph10031125
39. Li CY, Lee O, Shin GS Li XW. Health literacy and health status of Korean-Chinese elderly people living in Yanbian, China. J Korean Acad Nurs. (2009) 39:386–92. doi: 10.4040/jkan.2009.39.3.386
Keywords: oral health literacy, parents, children, diet, behavior
Citation: Wang Y, Inglehart MR and Yuan C (2022) Impact of Parents' Oral Health Literacy on Their Own and Their Children's Oral Health in Chinese Population. Front. Public Health 10:809568. doi: 10.3389/fpubh.2022.809568
Received: 05 November 2021; Accepted: 04 February 2022;
Published: 08 March 2022.
Edited by:
Raffaella Docimo, University of Rome Tor Vergata, ItalyReviewed by:
Huabin Luo, East Carolina University, United StatesCopyright © 2022 Wang, Inglehart and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chao Yuan, Y2hhb3l1YW5AYmptdS5lZHUuY24=
†Present address: Yu Wang, Private Practice, Boston, MA, United States
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.