- 1Department of Internal Medicine, Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
- 2Department of Internal Medicine, Dow University of Health Sciences–Ojha Campus, Karachi, Pakistan
- 3Department of Nephrology, Dow University of Health Sciences–Ojha Campus, Karachi, Pakistan
- 4Department of Internal Medicine, Aga Khan University Hospital, Karachi, Pakistan
Background and Objectives: During the pandemic, the growing influence of social media, accessibility of over-the-counter medications, and fear of contracting the virus may have led to self-medication practices among the general public. Medical students are prone to such practices due to relevant background knowledge, and access to drugs. This study was carried out to determine and analyze the prevalence of self-medication practices among medical students in Pakistan.
Materials and Methods: This descriptive, cross-sectional study was conducted online in which the participants were asked about the general demographics, their self-medication practices and the reasons to use. All participants were currently enrolled in a medical college pursuing medical or pharmacy degree. Non-probability sampling technique was used to recruit participants.
Results: A total of 489 respondents were included in the final analysis. The response rate was 61%. Majority of the respondents were females and 18–20 years of age. Self-medication was quite prevalent in our study population with 406 out of 489 individuals (83.0%) were using any of the drugs since the start of pandemic. The most commonly utilized medications were Paracetamol (65.2%) and multivitamins (56.0%). The reasons reported for usage of these medications included cold/flu, or preventive measures for COVID-19. The common symptoms reported for self-medication included fever (67.9%), muscle pain (54.0%), fatigue (51.7%), sore throat (46.6%), and cough (44.4%). Paracetamol was the most commonly used drug for all symptoms. Female gender, being in 3rd year of medical studies, and individuals with good self-reported health were found more frequent users of self-medication practices.
Conclusion: Our study revealed common self-medication practices among medical and pharmacy students. It is a significant health issue especially during the pandemic times, with high consumption reported as a prevention or treating symptoms of COVID-19.
Introduction
The Coronavirus 2019 (COVID-19) was declared a pandemic by the World Health Organization on January 30th, 2020 (1). As of October 22nd, 2021, the global crisis has affected 242 million individuals and claimed over 4.9 million lives (2).
With clinical trials of multiple drugs in the pipeline, there are no definitive treatments with confirmed evidence against the severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2). Anti-malarial drugs, hydroxychloroquine, and chloroquine received emergency approval to treat prophylaxis in COVID-19 when a small non-randomized trial was initially promising (3). It was soon labeled controversial as randomized studies depicted an increased risk-to-benefit ratio (4). However, rapid medical research has developed, and massively rolled out COVID-19 vaccines prevented the adverse effects from symptoms of the disease in affected individuals (5). It is envisaged that vaccine advent and procurement by developed countries will soon create global inequity as middle-to-low income nations struggle to vaccinate healthcare workers and the older population (6). Economic recession in developing countries, like Pakistan has only managed to fully vaccinate less than half of its population (7).
The third wave of coronavirus had peaked, yet Pakistan's overburdened healthcare system reached a 90% occupancy of ventilators and hospital beds (8). Travel restrictions, oxygen shortage, and the risk of contracting the virus from crowded clinics and hospitals have inculcated fear in the public, allowing a nation prone to self-medication to rely more heavily on self-diagnosis (9, 10). Self-medication is the administering of medicines to treat self-recognized symptoms, psychological ailments, and first aid based on prior knowledge, without consulting a physician (11). The growing influence of social media has let individuals explore COVID-related symptoms, pain keywords, and treatments worldwide, as well as in Pakistan, as revealed by an infodemiological study on Google trends (12). Adding to this is the availability of over the counter (OTC) drugs in pharmacies across Pakistan which has been the highest contributor to a self-medicating prevalence of 81% in the populous Karachi. Easily accessible drugs in pharmacies across Pakistan range from analgesics, antibiotics, anti-diarrheal agents, antihistamines, antipyretics, cough-suppressants, vitamins to herbal medicines and homeopathy (10, 13). Though the primary reason was affordability, the greatest driver (47.8%) of self-medication was the belief that the illness was insignificant. This stems from poor health literacy amongst the general public which is easily influenced by the media (10). It is also well noted that preference for self-medication is cultural practice in Pakistan. The positive and negative effects of self-medication of Sanna Makki, a herbal laxative, which was widely used as a COVID-19 cure after mass-circulation on WhatsApp was a well-publicized example (14). The risks attached to self-medicated drugs include incorrect and improper dosage, and antibiotic abuse leading to drug resistance (15).
A trending worldwide practice of self-medication does not have enough literature on an ongoing pandemic, except studies conducted in Peru and Saudi Arabia (16, 17). However, no study reports the prevalence of self-medication in the highly affected medical student population in Pakistan—the future of the healthcare system. It is important to assess self-medication practices among medical students, because they have relevant knowledge, and are more likely to access to prescription as well as OTC drugs. Low tendency to consult health professionals, reliance on the internet for information on background medical knowledge, and treating self-diagnosed illnesses could be factors that promotes self-medication practice among medical students.
The primary objective was to determine and analyze the prevalence of self-medication practices among medical students for respiratory symptoms, from the onset of first COVID-19 symptom or in case of being positively tested for COVID-19. We further assessed the self-medicated drugs used for respiratory problems during the pandemic. A secondary aim was to evaluate the factors associated with self-medication of various drugs among medical students during the COVID-19 pandemic in Pakistan. This will allow the health ministries and educational administrations alike to undertake measures and address the gap of health negligence that can result from self-medication practices.
Materials and Methods
Study Design
This descriptive, cross-sectional study was conducted online from January 25th to February 20th, 2021. The design of the study and sample size was modified according to the pilot study carried out from December 11th to December 15th, 2020, under the expertise of professors and doctors. The questionnaire was developed in English, on Google survey, and distributed through social media platforms. The online survey questions were obtained after a thorough literature search and assessing the validity and reliability (16, 17). The responses were made anonymous to maintain confidentiality and reliability. Each participant received an email of their response to avoid duplication of data. Clarification of the contents and the purpose of the study were explained at the start of the survey followed by an informed consent. Data was anonymized and only the lead investigator had access to the responses.
Development of Survey Questionnaire and Operationalization of Variables
The questionnaire included a total of 11 questions. Seven questions were dedicated to the general demographics including the city of residence, gender, age, marital status, level of education/medical, and comorbid conditions. The next 4 questions were based on self-medication of drugs for prevention and treatment of respiratory symptoms: drug selection, reasoning for self-medication, symptoms they were looking to improve, and if any of the drugs improved those symptoms. The participants were asked if they consulted any physician before starting these medications, were they been using these medications before COVID-19 pandemic, and do they have any comorbid conditions that warrant the use of these medications. All these questions if answered as a No have been considered as self-medication during the pandemic. The drugs listed in the survey included acetaminophen, ibuprofen, azithromycin, hydroxychloroquine, ivermectin, doxycycline, antivirals (lopinavir, ritonavir, remdesivir, and others), cetirizine, multivitamin compounds or any other drug (open question) for respiratory symptoms. All drugs were classified according to the Anatomical Therapeutic Chemical (ATC) (18). This selection of drugs was based on the existing literature, and reports from the local media. COVID-19 can present with a range of symptoms. Frequently reported symptoms were obtained from CDC's guidelines (19). The list of symptoms included fever, fatigue, cough, muscle ache, nasal congestion, sore throat, headache, breathing difficulty, no symptom, and other symptom (open question). Anosmia was omitted as being controversial at the time of inception of this study (16). To assess the reason for drug use, participants had seven options listed as cold/flu, no symptoms, COVID-19 prevention, had COVID-19 symptoms, COVID-19 positive, consume the drug regularly, other reason (open question). The following 5-point Likert scale was used to identify and list the improvement in symptoms if any: improved all symptoms, improved most of the symptoms, improved a few of the symptoms, improved only one symptom, did not alleviate any of the symptoms.
Sample Size/Sampling Technique
The sample size of the survey was obtained from the pilot study determined using the power analysis. The minimum sample size was 385, with a statistical power of 80% and a confidence interval of 95%. We hypothesized that at least 50% of the participants would practice self-medication, with a 5% margin of error. The formula for sample size estimation was n = N ×/((N-1) E2 + x), where N is the population size and n is sample size estimation. A non-probability sampling technique was used to recruit participants from social media platforms, including WhatsApp, Facebook, and Messenger.
Inclusion/Exclusion Criteria
Inclusion criteria included completed responses, and the respondent i.e., male or a female medical student pursuing MBBS or Pharm D degree from a medical college in Pakistan, having the ability to understand English, and being technologically adept and have access to Internet. While exclusion criteria included respondents from other than the medical field.
Ethical Approval
The study received ethical approval from the Institution's Ethics Committee of the Dow University Ojha Hospital. Each participant had the right to withdraw from the study at any time. The possible risks and the purpose of the survey were thoroughly explained. Participants had to provide consent before filling out the questionnaire.
Data Analysis
Microsoft Excel 2016 was used for data collection and assembled in to Statistical Package for Social Sciences (SPSS) version 25.0 for data analysis. A multivariate analysis estimated the preference of self-medication for the surveyed drugs using the baseline demographics i.e., sex, age, marital status, educational status, region, presence of comorbid conditions, and self-reported health as control variables. Categorical variables were assessed using frequencies and percentages, through univariate analysis. Analytical statistics were performed with 95% confidence intervals (CI) and odds ratios (OR), which were obtained using logistic regression.
Results
A total of 374 medical and 115 pharmacy students were included in the final analysis. The response rate was 61%. Majority of the respondents were of 18–20 years of age (58.5%). More than three-fourths were females. 34.0% of medical students were in first year, 20.6% in second year, 20.3% in third year, 13.9% in fourth year, and 11.2% were in final year of their medical education. Most respondents were from province Sindh and Punjab (combined 85.7%). Only 4.5% reported previous comorbid conditions, while majority (60.5%) were in good state of self-reported health. While reporting the risk of acquiring COVID-19 infection, 43.8% were unbothered. Another 38.0% admitted mild risk while only 2.9% reported severe risk. 15.3% of participants were already infected with the virus. The socio-demographic characteristics of the participants are described in Table 1.
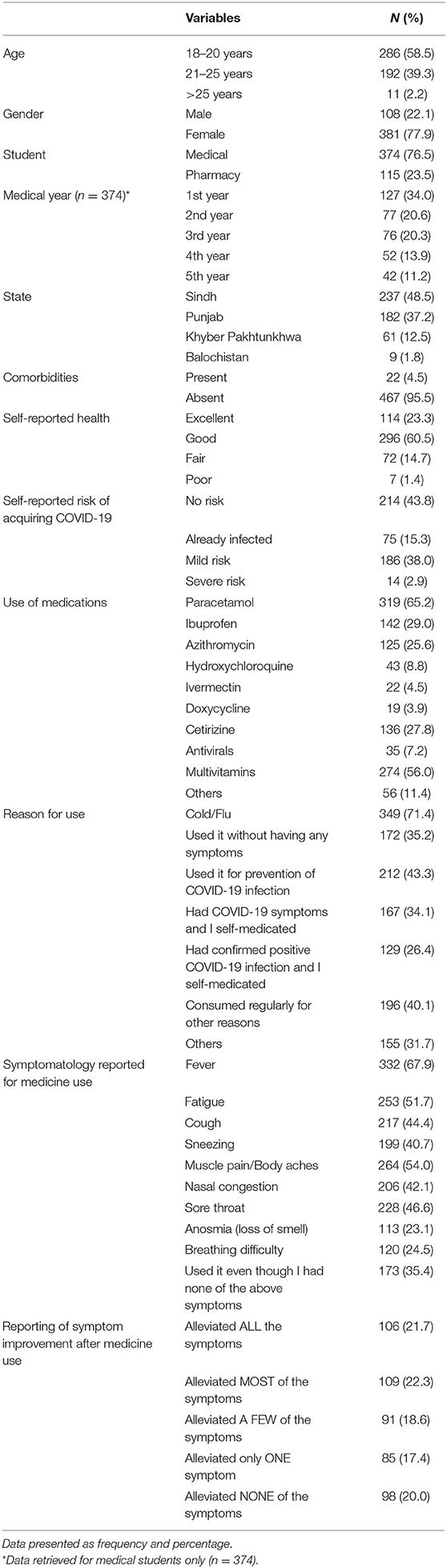
Table 1. Sociodemographic characteristic of medical students during the COVID-19 lockdown (n = 489).
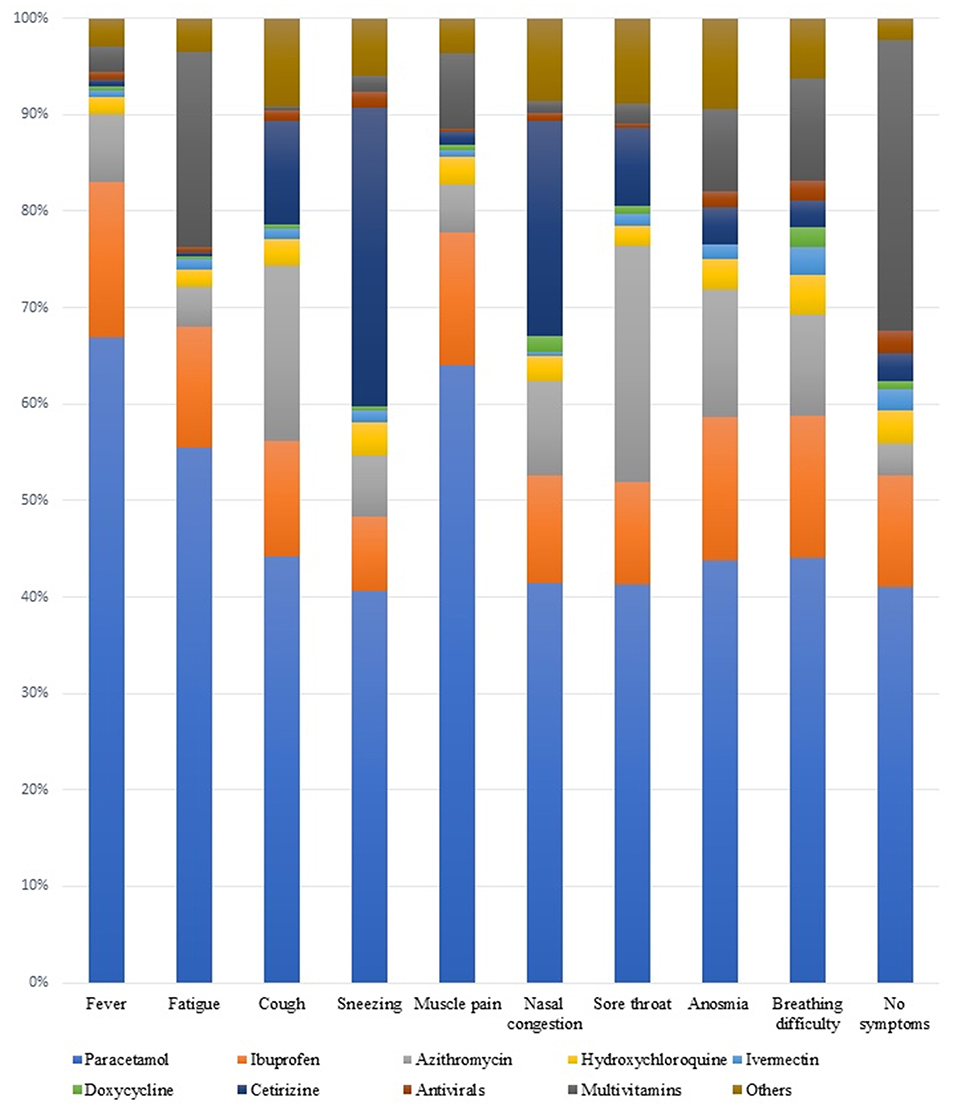
Self-medication was prevalent in our study population with 316 out of 374 medical students (84.5%) and 90 out of 115 pharmacy students (78.3%) were using any of the drugs since the start of pandemic. The most commonly utilized medications were Paracetamol (65.2%), multivitamins (56.0%), Ibuprofen (29.0%), Cetirizine (27.8%), and Azithromycin (25.6%) among others. The reasons reported for usage of these medications included cold/flu (71.4%), as preventive measures for COVID-19 (43.3%), or a self-medication for COVID-19 symptoms (34.1%). However, 35.2% reported taking these medications without any reason or symptoms, while another 40.1% consumed them regularly for other reasons. The symptoms reported for self-medication included fever (67.9%), fatigue (51.7%), cough (44.4%), sneezing (40.7%), muscle pain/body aches (54.0%), nasal congestion (42.1%), sore throat (46.6%) anosmia (23.1%), and breathing difficulty (24.5%) as shown in Table 1. Paracetamol was the most commonly used drug for all symptoms including fever, fatigue, cough, sneezing, myalgia, nasal congestion, sore throat, anosmia, and shortness of breath. Figure 1 demonstrates the relative proportions of drug use for each specific symptomatology.
Paracetamol use was common in individuals >21 years, final year medical students, those already infected with COVID-19, and having flu, fever, and fatigue. 45.4% shown all or most symptoms resolved with its use as shown in Table 2. Azithromycin use was common in age >21 years, 5th year medical students, inhabitants of Khyber Pakhtunkhwa/Balochistan, as well as those already infected with COVID-19. Cetirizine use was frequent among pharmacy students, final year medical students and those with self-reported risk of COVID-19 infection. Use of antivirals was prevalent among males of above 21 years of age. Use of multivitamins was also common in individuals >21 years, females, residents of Khyber Pakhtunkhwa/Balochistan and those either already infected with COVID-19 or reported mild to severe risk of acquiring infection. Individuals from province Punjab were more likely to use ivermectin and less likely to use cetirizine as self-medication. Doxycycline use was found prevalent in males. Use of ivermectin was not shown to improve any of the self -reported symptoms. Other medications were more common among those having comorbid conditions and self-reported as fair/poor. All these factors showed significant association when conducted on a logistic regression model with reported odds ratios and p-values as shown in Table 3.
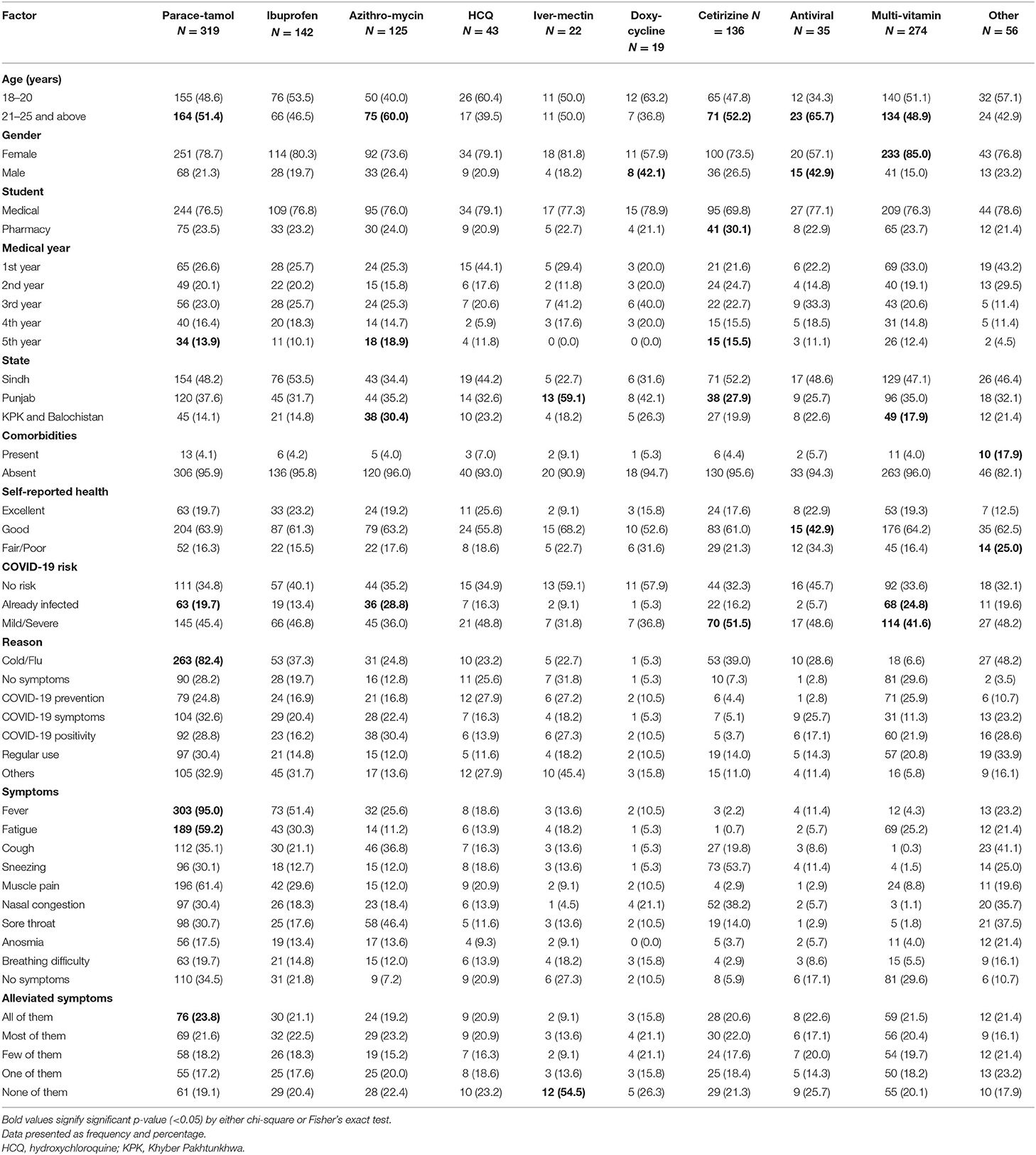
Table 2. Factors associated with self-medication of various drugs among medical students during the COVID-19 lockdown (n = 489).
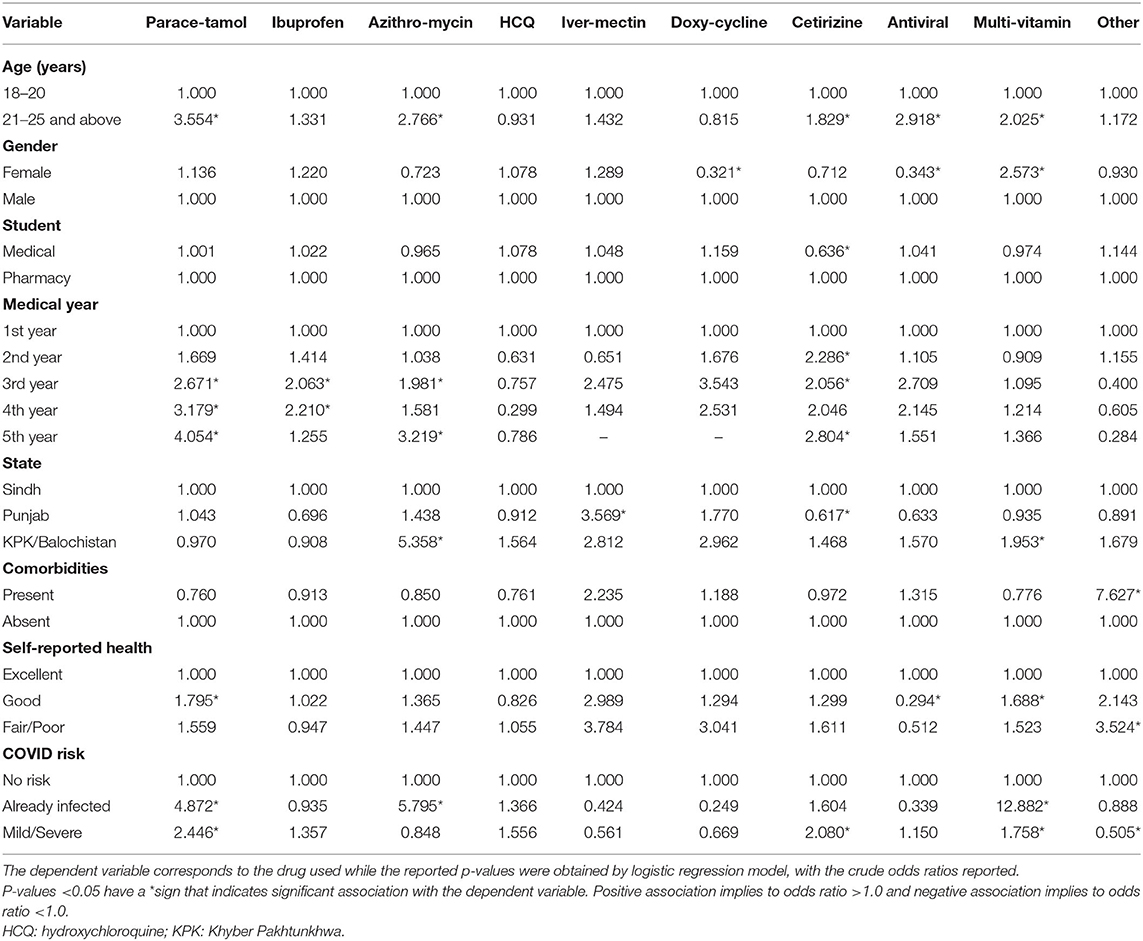
Table 3. Bivariate analysis of the factors associated with the self-medication of various drugs during the COVID-19 lockdown among medical students (n = 489).
The following variables were significantly associated with self-medication practice in logistic regression (Supplementary Figure 1; Table 4): female sex (p < 0.001), third-year medical students (p = 0.022), self-reported health as good (p = 0.029), and those previously infected with COVID-19 (p = 0.050). In multivariate analysis, female gender (<0.001), those in third year of medical studies (p = 0.031) and those students who perceived their self-reported health as “good” were more likely to adopt self-medication practices (p = 0.032).
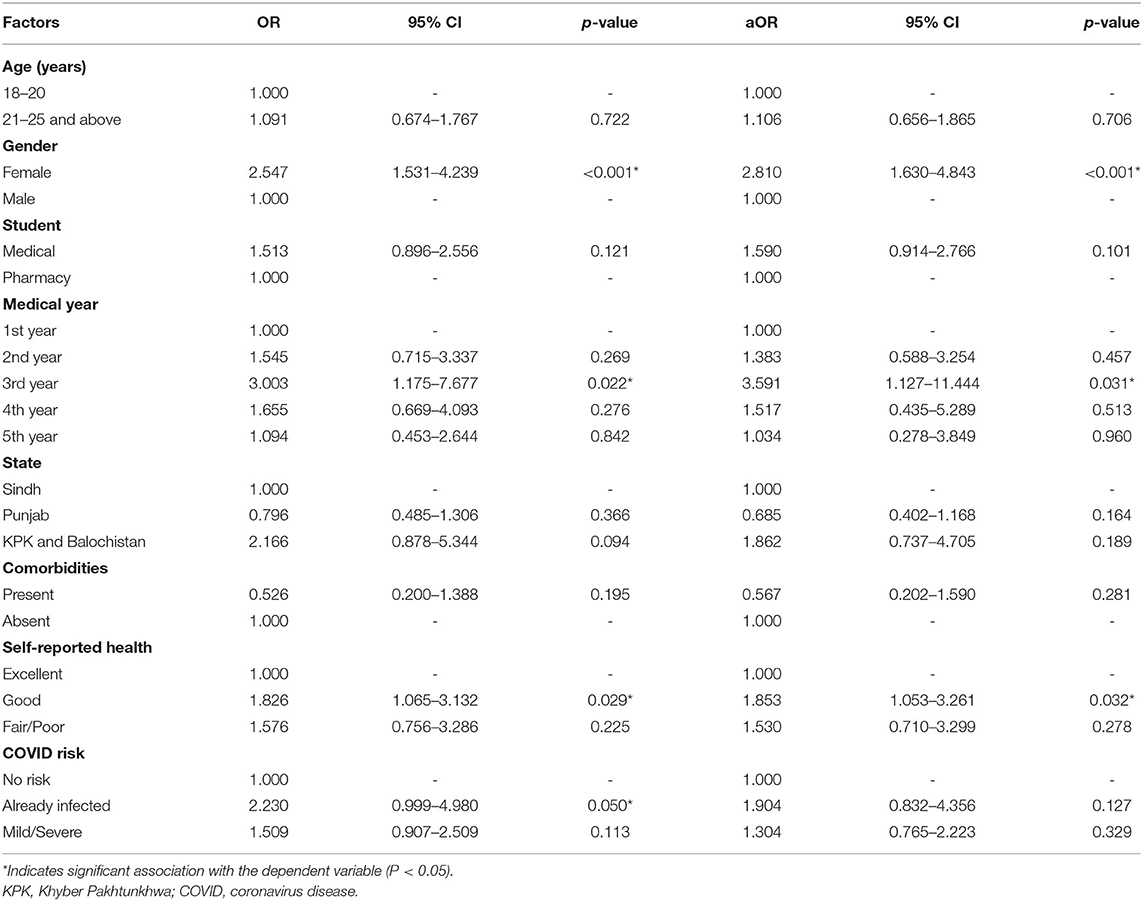
Table 4. Multivariate analysis of the factors associated with the self-medication practice during the COVID-19 lockdown among medical students (n = 489).
Discussion
Self-medication is often considered as an ambiguous phenomenon and the practice is commonplace in developed and developing countries alike. However, it has not been extensively qualitatively or quantitatively studied, especially in Pakistan (20). Self-medication with antibiotics rates were generally low in middle income countries, according to a 2020 review, however, among affected countries, Pakistan had one of the highest prevalence of 81.23%, with only 7.3% in Indonesia and 26.9% in Bangladesh (21). A study conducted by the Aga Khan University, Karachi in 2008 revealed 76% self-medication rates among the medical and non-medical university students surveyed (22), while another survey from pre-COVID times, consisting of a small segment of medical students in Pakistan found 99% of them to be engaged in practicing self-medication (23). To the best of our knowledge, our study is the first of its kind within the current pool of literature available, that has evaluated self-medication among medical students in the context of COVID-19, encompassing most provinces of Pakistan.
The incidence of self-medication revealed in our results is around 83%, a finding that is comparable to self-medication occurrence rates during COVID-19 reported in studies conducted abroad. Among the nursing undergraduates in Saudi Arabia, self-medication practice with antibiotics and analgesics was found to be 87% (5) while In Kenya, health care self-medication prevalence was 60.4% among healthcare workers, indicating an increase from pre pandemic results (24). Another study assessing self-medication prevalence in the Nigerian population during the pandemic reported a finding of 41% (25). In Togo, 34.1 % of the participants that belonged to healthcare, air transport, police, road transport and informal sectors reported to self-medicate and healthcare division had the highest of 51.9% against all sectors (26). Conversely, in Peru, the number of responders not engaging in self-medication was higher than those that did, for all drugs including Acetaminophen, Ibuprofen, Azithromycin, Hydroxychloroquine, Penicillin, Antiretrovirals, which were evaluated (16). Multivariate logistic regression model showed that being female gender, medical school year 3rd, having been already infected with COVID-19 or having already infected with COVID-19 were factors that were associated respondents expected to self-medicate the most.
Paracetamol was the highest used drug in our study, respondents 21–25 years and above, 5th year medical students, those already infected with COVID-19, and stating symptoms of cold/flu, fever and fatigue showed significant use. High use of Paracetamol aligns with results from the nursing undergraduates in Saudi Arabia (17) and from the Peru adult population (16) where it was also the most consumed drug. As a widely used first line pharmacotherapy analgesic for tackling pain disorders and different pyrexia, Paracetamol use is widely reported in studies comprising of medical students. Health science major students in Nigeria commonly used it as a pain reliever (25), while medical students in Iran were also frequent users of this drug (27). An Indian study found medical students to be more likely to self-medicate than paramedical students and for this purpose, Paracetamol was consumed mostly (28). Paracetamol has been known to have negligible anti-inflammatory action (28) and guidelines issued during the initial months of the pandemic state that it can be used for treating mild COVID-19 symptoms when managing patients at home (29) or for self-medication, especially for fever or headache (30). This is consistent with our results corresponding to Paracetamol use as it was greatly used to treat “fever” in our study population, and its use also showed improvement in all or most of the symptoms experienced by the responders who employed Paracetamol. However, some instances report the drug to be exacerbating COVID-19 symptoms, likely due to activation of prothrombotic mechanisms which is known as one of the leading pathogenic causes of COVID-19 (29). Single or repeated high Paracetamol dose, or chronic ingestion above therapeutic doses can result in hepatotoxicity (17). Hepatotoxicity from intentional or non-intentional Paracetamol overdose is the most common cause of drug-induced liver injury and is a global issue (17). The medicine's toxic dosage effects must be known to students utilizing it.
Multivitamins were the second highest consumed drug in our study, which have also been the drug of choice as divulged in a population-based survey during COVID-19 in Nigeria with 51.8% reporting to use this group of medicine (25). In Togo, 27.6% used Vitamin C when self-medicating (26), while in Egypt, 27% used vitamin C and 17.7% used vitamin D (31). A study from 2015 involving healthcare and non-healthcare university students from South India found multivitamins to be among the most commonly self-medicated drugs (32). Multivitamins include multiple vitamins and minerals, trace elements all of which possess antioxidant properties and have a crucial role in regulating immune function and can reduce risk of respiratory infection (33). A large observational study conducted in US, UK, and Sweden during first waves of COVID-19 demonstrated a modest protective effect among those taking multivitamin supplements with a reduced risk for testing positive for SARS-CoV-2 (33). Hence, these might explain the significant use of multivitamins by females and participants 21–25 years and above. Additionally, individuals with COVID-19 can experience weight loss; having adequate amounts of vitamins and minerals can prevent this unintended reduction in weight (34). Moreover, a deficiency in certain micronutrients such as Vitamin A, Vitamin D, Zinc can be deleterious during viral infections (33). These factors might elucidate why those infected with COVID-19 in our research resorted to a significantly high rate of multivitamin use.
Ibuprofen was the third highest self-medicated drug in our population. Previously, it has been reported to be the most preferred NSAID for analgesic purposes among nursing undergraduates in Saudi Arabia (20%) (17). As a non-steroidal anti-inflammatory drug (NSAID), it is well tolerated and effective during pain and inflammation and has minor side effects (17). Alongside Paracetamol, it is one of the most extensively used antipyretic (35). Since the start of the pandemic, Ibuprofen use has been subject to debate (36). Initially discouraged for use as it was suspected to aggravate infections (37), such claims were later rejected. A study analyzing data from ISARIC Clinical Characterization Protocol UK cohort found NSAIDS use not disposing to any poor COVID-19 outcome (38). A 2021 systematic review and meta-analysis reiterated similar findings and revealed no negative association between use of NSAIDS, including Ibuprofen, with SARS-CoV-2 infection or its outcomes (39). Ibuprofen has been known to have a better analgesic response in men while higher threshold and greater tolerance for electrically induced pain, responded significantly to ibuprofen in contrast to women (40). Nevertheless, the high use of this drug during COVID-19 can be linked to its efficacy in relieving fever, infection (35). However, users must be wary that disproportionate use of the drug can cause adverse drug reactions (ADRs) (17).
Hydroxychloroquine and ivermectin, the sales of which escalated globally in wake of COVID-19 were found to be consumed in low amounts in our study (41). Other frequently used drugs were Cetirizine and Azithromycin. Azithromycin has been popular amongst antibiotics that have been used for self-medication in Pakistan (21) and has also been an alternative for self-medication in other countries such as Saudi Arabia (17) and Peru (16). Using antibiotics during self-medication is the leading cause of antimicrobial resistance (42) thus its intake must be regulated, its appropriate use and disposal ensured especially by medical students.
The most common reason for use of the respective drug was “cold/flu”, consistent with results from studies of including medical students from Iran (29, 43) and Brazil (44). “Fever”, one of the most common COVID-19 symptom (19), followed by “Muscle Pain” were the highest symptomologies reported for medicine use. Analgesic use for muscular pain at any site was also highly common among undergraduate medical and paramedical students in India (28). Studies evaluating medical students' attitudes toward self-medication delineate sufficient knowledge, familiarity with disease, and time constraints which can also be cited as motives for self-medication among our participants in this pandemic scenario (17). In the early days of SARS-CoV-2 outbreak, when the disease was a source of fear and stigma, knowledge and access to prescription-only medicines while trying to keep one's health status, especially if infected with COVID-19, could be accounted for self-medication rates among the medical students' community (26). Furthermore, practicing self-medication allowed the students to exercise freedom in managing their health and wellbeing instilling a sense of independence (24). The overall high self-medication rate throughout all year groups can be ascribed to the extensive educational load upon these students and stressful circumstances which results in distress and compels them to seek OTC drugs (45). Another study conducted in Poland highlighted such behaviors increased during lockdown (46). According to a study from Jordan, factors such as female gender, working in the medical field, and history of COVID-19 infection were reportedly associated with self-medication similar to our findings (47).
While the high self-medication percentage suggests medical students' confidence while self-prescribing, the possibility that students' knowledge about drug pharmacology, cultural prevalence, and limited experience at the current student level can make them susceptible to unfavorable outcomes, must not be undermined (28). Drug addiction and drug dependence (29) can also be induced by repeated self-medication, which students must be aware of. Lockdown and isolation guidelines have prevented the population from visiting hospitals and clinics and have altered health-seeking behavior. As different SARS-CoV-2 variants keep emerging, people are likely to self-medicate (48). Medical students are also probable to keep self-medicating, which could be helpful in obtaining benefits of self-care, and alleviating burden on the healthcare system of the country by reducing number of physician visits (49). By practicing self-medication wisely themselves, staying mindful of the pharmacological and taxological risks of improper drug use (25), they could facilitate the lay population to treat themselves for minor ailments which could further relieve pressure on health care setups.
The study is important as questions specific to the drug trends in the local population were incorporated, and responses from all parts of the country were received. However, as online platforms were used for disseminating the questionnaire, students in remote areas with no access to the internet could not be a part of the survey. Other limitation included non-random sampling method and generalizability of study results. Besides, due to recall bias, some responders might have answered incorrectly.
Conclusion
Our study revealed common self-medication practices among medical and pharmacy students. It is a significant health issue especially during the pandemic times, with high consumption reported as a prevention or treating symptoms of COVID-19. Further measures are needed to improve healthcare policies regarding awareness and sensitization about the risks of self-medication. Future studies should also assess students' attitude toward self-medication, their knowledge regarding drug dosage and potential side effects, and the role of medical colleges to better ascertain their approach toward self-medication.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Approval was taken in this study from Institutional Review Board of Dow University Ojha Hospital (Approval No. IRB (DUH)-2020/174/021), and content to participate was obtained from all the individuals through online platform. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
FY: conceptualization. UN, HNaj, HNau, and AK: data curation. MSA: formal analysis. FY and MNA: funding acquisition. FY, UN, and HNaj: investigation. MSA and AK: methodology. FY, UN, and AK: project administration. UN, HNaj, and HNau: resources. MSA and HNau: software. MSA, HNau, and AK: validation. HNaj and HNau: visualization. UN and HNau: writing—original draft. FY, MSA, MNA, and AK: writing—review and editing. All authors approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.803937/full#supplementary-material
Supplementary Figure 1. Crude and Adjusted level analysis of factors associated with self-medication among medical students.
References
1. WHO. Director-General's Opening Remarks at the Media Briefing on COVID-19. (2020). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 (accessed May 16, 2021).
2. WHO. Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. Available online at: https://covid19.who.int/ (accessed October 23, 2021).
3. Yadav UCS. Vaccines and drugs under clinical trials for prevention and treatment of COVID-19. Virusdisease. (2021) 32:13–9. doi: 10.1007/s13337-020-00650-7
4. Echeverría-Esnal D, Martin-Ontiyuelo C, Navarrete-Rouco ME, De-Antonio Cuscó M, Ferrández O, Horcajada JP, et al. Azithromycin in the treatment of COVID-19: a review. Expert Rev Anti Infect Ther. (2021) 19:147–63. doi: 10.1080/14787210.2020.1813024
5. COVID Vaccines Protect Against Top Variants WHO Says. Available online at: https://www.medscape.com/viewarticle/951657 (accessed May 23, 2021).
6. Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. (2021) 397:1023–34. doi: 10.1016/S0140-6736 (21)00306-8
7. Coronavirus, (COVID-19),. Google News. Available online at: https://news.google.com/covid19/map?hl=en-PK&state=7&mid=%2Fm%2F05sb1&gl=PK&ceid=PK%3Aen (accessed May 23, 2021).
8. COVID-19–Pakistan. Available online at: https://covid19.who.int/region/emro/country/pk (accessed October 23, 2021).
9. Pakistan Heading Towards Acute Oxygen Shortage Warn Producers. Available online at: https://www.thenews.com.pk/print/825221-pakistan-heading-towards-acute-oxygen-shortage-warn-producers (accessed May 23, 2021).
10. Aziz MM, Masood I, Yousaf M, Saleem H, Ye D, Fang Y. Pattern of medication selling and self-medication practices: a study from Punjab, Pakistan. PLoS ONE. (2018) 13:e0194240. doi: 10.1371/journal.pone.0194240
11. WHO Guidelines for the regulatory assessment of medicinal products for use in self-medication. WHO Drug Inf. (2000) 14:18–26. Available online at: https://apps.who.int/iris/handle/10665/57624
12. Szilagyi IS, Ulrich T, Lang-Illievich K, Klivinyi C, Schittek GA, Simonis H, et al. Google Trends for pain search terms in the world's most populated areas before and after the first recorded COVID-19 case: an infodemiological study. J Med Internet Res. (2021) 23:e27214. doi: 10.2196/27214
13. Afridi MI, Rasool G, Tabassum R, Shaheen M, Siddiqullah Shujauddin M. Prevalence and pattern of self-medication in Karachi: a community survey. Pakistan J Med Sci. (2015) 31:1241–5. doi: 10.12669/pjms.315.8216
14. Fact-check: “Sanna Makki” NOT a Cure for Coronavirus Overdose Can Be Harmful. Available online at: https://www.geo.tv/latest/292182-fact-check-sanna-makki-not-a-cure-for-coronavirus-can-cause-harm-if-overdosed (accessed May 23, 2021).
15. Ruiz ME. Risks of self-medication practices. Curr Drug Saf. (2010) 5:315–23. doi: 10.2174/157488610792245966
16. Quispe-Cañari JF, Fidel-Rosales E, Manrique D, Mascaró-Zan J, Huamán-Castillón KM. Chamorro–Espinoza SE, et al. Self-medication practices during the COVID-19 pandemic among the adult population in Peru: a cross-sectional survey. Saudi Pharm J. (2021) 29:1–11. doi: 10.1016/j.jsps.2020.12.001
17. Faqihi AHMA, Sayed SF. Self-medication practice with analgesics (NSAIDs and acetaminophen), and antibiotics among nursing undergraduates in University College Farasan Campus, Jazan University, KSA. Ann Pharm Fr. (2020) 79:275–85. doi: 10.1016/j.pharma.2020.10.012
18. WHOCC. Structure and Principles. Available online at: https://www.whocc.no/atc/structure_and_principles/ (accessed May 23, 2021).
19. Symptoms of COVID-19 | CDC. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html (accessed May 23, 2021).
20. Anwar M, Green J, Norris P. Health-seeking behaviour in Pakistan: a narrative review of the existing literature. Public Health. (2012) 126:507–17. doi: 10.1016/j.puhe.2012.02.006
21. Aslam A, Gajdács M, Zin CS, Ab Rahman NS, Ahmed SI, Zafar MZ, et al. Evidence of the practice of self-medication with antibiotics among the lay public in low- and middle-income countries: a scoping review. Antibiotics. (2020) 9:1–17. doi: 10.3390/antibiotics9090597
22. Zafar SN, Syed R, Waqar S, Zubairi AJ, Vaqar T, Shaikh M, et al. Self-medication amongst university students of Karachi: prevalence, knowledge and attitudes. J Pak Med Assoc. (2008) 58:214–7. Available online at: https://jpma.org.pk/article-details/1378?article_id=1378
23. Kanwal ZG, Nighat F, Azhar S, Chohan O, Jabeen M, Yameen MA. Implications of self-medication among medical students-A dilemma. J Pakistan Med Assoc. (2018) 68:1363–7. Available online at: https://jpma.org.pk/article-details/8852?article_id=8852
24. Onchonga D, Omwoyo J, Nyamamba D. Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharm J. (2020) 28:1149–54. doi: 10.1016/j.jsps.2020.08.003
25. Wegbom AI, Edet CK, Raimi O, Fagbamigbe AF, Kiri VA. Self-medication practices and associated factors in the prevention and/or treatment of COVID-19 virus: a population-based survey in Nigeria. Front Public Heal. (2021) 9:606801. doi: 10.3389/fpubh.2021.606801
26. Sadio AJ, Gbeasor-Komlanvi FA, Konu RY, Bakoubayi AW, Tchankoni MK, Bitty-Anderson AM, et al. Assessment of self-medication practices in the context of the COVID-19 outbreak in Togo. BMC Public Health. (2021) 21:58. doi: 10.1186/s12889-020-10145-1
27. Abdi A, Faraji A, Dehghan F, Khatony A. Prevalence of self-medication practice among health sciences students in Kermanshah, Iran. BMC Pharmacol Toxicol. (2018) 19:36. doi: 10.1186/s40360-018-0231-4
28. Chindhalore CA, Dakhale GN, Giradkar AB. Comparison of self-medication practices with analgesics among undergraduate medical and paramedical students of a tertiary care teaching institute in Central India – a questionnaire-based study. J Educ Health Promot. (2020) 9:309. doi: 10.4103/jehp.jehp_378_20
29. Pandolfi S, Simonetti V, Ricevuti G, Chirumbolo S. Paracetamol in the home treatment of early COVID-19 symptoms: a possible foe rather than a friend for elderly patients? J Med Virol. (2021) 93:5704–6. doi: 10.1002/jmv.27158
30. Paracetamol Paracetamol or ibuprofen can be used to treat the symptoms of COVID-19 says NHS, England,. Pharm J. Available online at: https://pharmaceutical-journal.com/article/news/paracetamol-or-ibuprofen-can-be-used-to-treat-the-symptoms-of-covid-19-says-nhs-england (accessed April 20, 2020).
31. Khabour OF, Hassanein SFM. Use of vitamin/zinc supplements, medicinal plants, and immune boosting drinks during COVID-19 pandemic: a pilot study from Benha city, Egypt. Heliyon. (2021) 7:e06538. doi: 10.1016/j.heliyon.2021.e06538
32. Sharma A, Oommen S, Topno I, Saya RP. Perceptions and practices of self-medication in healthcare and nonhealthcare university students in South India. J Basic Clin Physiol Pharmacol. (2015) 26:633–40. doi: 10.1515/jbcpp-2015-0025
33. Louca P, Murray B, Klaser K, Graham MS, Mazidi M, Leeming ER, et al. Modest effects of dietary supplements during the COVID-19 pandemic: insights from 445 850 users of the COVID-19 Symptom Study app. BMJ Nutr Prev Heal. (2021) 4:149–57. doi: 10.1136/bmjnph-2021-000250
34. Harvard TH, ,. Chan School of Public Health. Ask the Expert: The Role of Diet and Nutritional Supplements During COVID-19 | The Nutrition Source. 2020. Available online at: https://www.hsph.harvard.edu/nutritionsource/2020/04/01/ask-the-expert-the-role-of-diet-and-nutritional-supplements-during-covid-19/ (accessed August 24, 2021).
35. Esba LCA, Alqahtani RA, Thomas A, Shamas N, Alswaidan L, Mardawi G. Ibuprofen and NSAID use in COVID-19 infected patients is not associated with worse outcomes: a prospective cohort study. Infect Dis Ther. (2021) 10:253–68. doi: 10.1007/s40121-020-00363-w
36. Carius BM, Schauer SG. Ibuprofen during the COVID-19 pandemic: social media precautions and implications. West J Emerg Med. (2020) 21:497–8. doi: 10.5811/westjem.2020.4.47686
37. Rinott E, Kozer E, Shapira Y, Bar-Haim A, Youngster I. Ibuprofen use and clinical outcomes in COVID-19 patients. Clin Microbiol Infect. (2020) 26:1259. doi: 10.1016/j.cmi.2020.06.003
38. Kragholm K, Torp-Pedersen C, Fosbol E. Non-steroidal anti-inflammatory drug use in COVID-19. Lancet Rheumatol. (2021) 3:e465–6. doi: 10.1016/S2665-9913 (21)00144-2
39. Moore N, Bosco-Levy P, Thurin N, Blin P, Droz-Perroteau C. NSAIDs and COVID-19: a systematic review and meta-analysis. Drug Saf. (2021) 44:929–38. doi: 10.1007/s40264-021-01089-5
40. Farkouh A, Baumgärtel C, Gottardi R, Hemetsberger M, Czejka M, Kautzky-Willer A. Sex-related differences in drugs with anti-inflammatory properties. J Clin Med. (2021) 10:1441. doi: 10.3390/jcm10071441
41. Hashmi FK, Atif N, Malik UR, Riboua Z, Saleem F, Khan YH, et al. Misinformation in wake of the COVID-19 outbreak: fueling shortage and misuse of lifesaving drugs in Pakistan. Disaster Med Public Health Prep. (2021) 15:e32–3. doi: 10.1017/dmp.2020.400
42. Rather IA, Kim B-C, Bajpai VK, Park Y-H. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci. (2017) 24:808–12. doi: 10.1016/j.sjbs.2017.01.004
43. Hashemzaei M, Afshari M, Koohkan Z, Bazi A, Rezaee R, Tabrizian K. Knowledge, attitude, and practice of pharmacy and medical students regarding self-medication, a study in Zabol University of Medical Sciences; Sistan and Baluchestan province in south-east of Iran. BMC Med Educ. (2021) 21:49. doi: 10.1186/s12909-020-02374-0
44. Corrêa Da Silva MG, Soares MCF, Muccillo-Baisch AL. Self-medication in university students from the city of Rio Grande, Brazil. BMC Public Health. (2012) 12:339. doi: 10.1186/1471-2458-12-339
45. Bekele KM, Abay AM, Mengistu KA, Atsbeha BW, Demeke CA, Belay WS, et al. Knowledge, attitude, and practice on over-the-counter drugs among pharmacy and medical students: a facility-based cross-sectional study. Integr Pharm Res Pract. (2020) 9:135–46. doi: 10.2147/IPRP.S266786
46. Makowska M, Boguszewki R, Nowakowski M, Podkowińska M. Self-medication-related behaviors and Poland's COVID-19 lockdown. Int J Environ Res Public Health. (2020) 17:8344. doi: 10.3390/ijerph17228344
47. Elayeh E, Akour A, Haddadin RN. Prevalence and predictors of self-medication drugs to prevent or treat COVID-19: experience from a Middle Eastern country. Int J Clin Pract. (2021) 75:e14860. doi: 10.1111/ijcp.14860
48. Rafiq K, Nesar S, Anser H, Leghari QA, Hassan A, Rizvi A, et al. Self-medication in the COVID-19 pandemic: survival of the fittest. Disaster Med Public Health Prep. (2021) 8:1–5. doi: 10.1017/dmp.2021.173
Keywords: self-medication, medical students, COVID-19, pandemic, public health, Pakistan
Citation: Yasmin F, Asghar MS, Naeem U, Najeeb H, Nauman H, Ahsan MN and Khattak AK (2022) Self-Medication Practices in Medical Students During the COVID-19 Pandemic: A Cross-Sectional Analysis. Front. Public Health 10:803937. doi: 10.3389/fpubh.2022.803937
Received: 28 October 2021; Accepted: 07 February 2022;
Published: 09 March 2022.
Edited by:
Chantal M. Morel, Université de Genève, SwitzerlandReviewed by:
Hashaam Akhtar, Yusra Institute of Pharmaceutical Sciences Islamabad, PakistanSarosh Iqbal, University of the Punjab, Pakistan
Ali Hassan Gillani, Xi'an Jiaotong University, China
Amal Akour, The University of Jordan, Jordan
Copyright © 2022 Yasmin, Asghar, Naeem, Najeeb, Nauman, Ahsan and Khattak. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muhammad Sohaib Asghar, c29oYWliX2FzZ2hhcjEyM0B5YWhvby5jb20=
 Farah Yasmin
Farah Yasmin Muhammad Sohaib Asghar
Muhammad Sohaib Asghar Unaiza Naeem
Unaiza Naeem Hala Najeeb1
Hala Najeeb1