
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health, 11 March 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.766943
 Samira Behboudi-Gandevani1*
Samira Behboudi-Gandevani1* Razieh Bidhendi-Yarandi2
Razieh Bidhendi-Yarandi2 Mohammad Hossein Panahi3
Mohammad Hossein Panahi3 Abbas Mardani4
Abbas Mardani4 Christina Prinds5,6
Christina Prinds5,6 Mojtaba Vaismoradi1
Mojtaba Vaismoradi1Objectives: There are controversies regarding the risk of adverse pregnancy outcomes among immigrants from conflict-zone countries. This systematic review and meta-analysis aimed to investigate the risk of perinatal and neonatal outcomes among immigrants from conflict-zone countries compared to native-origin women in host countries.
Methods: A systematic search on the databases of PubMed/MEDLINE, Scopus, and Web of Science was carried out to retrieve studies on perinatal and neonatal outcomes among immigrants from Somalia, Iraq, Afghanistan, Yemen, Syria, Nigeria, Sudan, Ethiopia, Eritrea, Kosovo, Ukraine, and Pakistan. Only peer-reviewed articles published in the English language were included in the data analysis and research synthesis. The odds ratio and forest plots were constructed for assessing the outcomes of interests using the DerSimonian and Laird, and the inverse variance methods. The random-effects model and the Harbord test were used to account for heterogeneity between studies and assess publication bias, respectively. Further sensitivity analysis helped with the verification of the reliability and stability of our review results.
Results: The search process led to the identification of 40 eligible studies involving 215,718 pregnant women, with an immigration background from the conflict zone, and 12,806,469 women of native origin. The adverse neonatal outcomes of the risk of small for gestational age (Pooled OR = 1.8, 95% CI = 1.6, 2.1), a 5-min Apgar score <7 (Pooled OR = 1.4, 95% CI = 1.0, 2.1), stillbirth (Pooled OR = 1.9, 95% CI = 1.2, 3.0), and perinatal mortality (Pooled OR = 2, 95% CI = 1.6, 2.5) were significantly higher in the immigrant women compared to the women of native-origin. The risk of maternal outcomes, including the cesarean section (C-S) and emergency C-S, instrumental delivery, preeclampsia, and gestational diabetes was similar in both groups.
Conclusion: Although the risk of some adverse maternal outcomes was comparable in the groups, the immigrant women from conflict-zone countries had a higher risk of neonatal mortality and morbidity, including SGA, a 5-min Apgar score <7, stillbirth, and perinatal mortality compared to the native-origin population. Our review results show the need for the optimization of health care and further investigation of long-term adverse pregnancy outcomes among immigrant women.
The number of international immigrants, particularly asylum seekers and refugees from conflict-zone countries, continues to grow rapidly. In Europe, ~1 in 10 people, is currently an international immigrant (1). According to the U.N. High Commissioner for Refugees, at the end of 2019, at least 100 million people are forcibly displaced (2). Although there is no international consensus on the definition of immigrant (1), it could be defined by the length of settlement in the host country, documentation status, voluntary or forced movement, and underlying reasons for immigration (1, 3).
Immigration has been increasingly accepted as an important determinant of health (4, 5), but the association between immigration and health status is less understood. Additionally, incorporating the mixed definition for immigration has increased the extent and complexity of this association, which can negatively impact the health status of immigrants in host countries (6). These differences are more complicated by pregnancy (7).
Female immigrants from conflict-zone countries are one of the largest groups of immigrants and have been shown to be a vulnerable population. Given that they are mainly asylum seekers and undocumented immigrants, their access to maternal healthcare services is limited, which can lead to a higher risk of mortality and morbidity, particularly among pregnant women (8–10).
There is an abundance of research on maternal and newborn health, but the results of studies on these specific populations are heterogeneous and inconclusive (11–15). Therefore, this systematic review and meta-analysis aimed to investigate the risk of perinatal and neonatal outcomes among immigrants from conflict-zone countries compared to native-origin women in host countries.
For conducting this systematic review and meta-analysis, a review protocol was predesigned based on Cochrane's methods, which is available upon request. The review results were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (16). The search strategy was based on the population, intervention, comparison, outcome, and study (PICOS) design framework.
Population: pregnant women with an immigration background
Intervention: None.
Comparison: Pregnant women with a native origin background.
Outcome: Maternal and neonatal adverse outcomes.
Study design: Observational studies.
Studies were eligible for inclusion if they fulfilled the following criteria: original research; international immigration from conflict-zone countries of Somalia, Iraq, Afghanistan, Yemen, Syria, Nigeria, Sudan, Ethiopia, Eritrea, Kosovo, Ukraine, and Pakistan; presenting data on at least one of the perinatal or neonatal outcomes; having the reference group from host countries, and access to the full-text. However, only peer-reviewed articles published in the English language were included in the data analysis and research synthesis. Exclusion criteria were studies without accurate and clear data on research variables, duplicated data, and studies focusing on a specific minor population such as adolescents. However, no restrictions were applied on the status or length of time for the receiving country.
The studies were identified by searching electronic databases, such as PubMed (including Medline), Scopus, and Web of Science (from January 1, 2000, until September 1, 2020). Also, a manual search in the references lists of selected studies and other relevant reviews was performed. The search strategy was developed with the collaboration of a librarian. Search keywords regarding immigration from conflict-zone countries and adverse pregnancy outcomes were combined and used for search (Supplementary Table 1).
Potentially relevant papers were independently screened by two reviewers (SBG and RBY). The studies were excluded when their titles and abstracts did not meet our eligibility criteria. The full text of the remaining studies was evaluated. Discrepancies were resolved by discussion between the review authors and, if necessary, by appealing to the third reviewer (MV). The following data, including the origin of the study, publication year, study period, the size of the study population, population characteristics, including age and body mass index (BMI), outcome measurements, including the number, prevalence, or risk of adverse pregnancy events, were extracted from the studies that met our inclusion criteria. To prevent bias in the data extraction and data entry, the accuracy of data before the meta-analysis was assessed through double-checking the data extraction process.
According to the International Organization for Migration (IOM), the immigrant population has been defined as any person moving across an international border regardless of the person's legal status, whether it is voluntary or involuntary and what the causes of movement are, or how long the length of the stay is (17). In addition, conflict-zone refers to high-intensity conflict war or political instability that disrupts essential services, such as housing, transportation, communication, sanitation, water, and health care, which requires the response of people outside of the affected community. For the current study, conflict-zone counties consisted of Somalia, Iraq, Afghanistan, Yemen, Syria, Nigeria, Sudan, Ethiopia, Eritrea, Kosovo, Pakistan, and Ukraine.
Methodological structures and result presentation in the studies were assessed using the Newcastle–Ottawa scale (18). Three domains of study selection and a comparability outcome of studies were scored. Studies with quality scores above 6 were judged high quality, 4–6 moderate quality, and <4 low quality.
The association between immigration status and pregnancy outcomes was examined using the calculation of the pooled odds ratio (OR) (with 95% CI) as the effect size and the p < 0.05 were considered statistically significant.
The random-effects model described by DerSimonian and Laird was used for analysis (19). The corresponding forest plots were constructed for both the pooled prevalence and the OR of the outcomes. Study heterogeneity was assessed using the inconsistency index (I2-statistic), and > 50% was considered substantial heterogeneityw. In addition, sensitivity analysis was performed to show the influence of each study on the overall meta-analyses' estimates. Publication bias was assessed through the Harbord test. In case of publication bias, the trim and fill correction was applied for adjustment. Data analyses were conducted using Stata (version 14; STATA Inc., College Station, TX, USA).
The search yielded 337 citations, including 122 duplicates (Figure 1). The screening of titles and abstracts resulted in the exclusion of 134 studies. After a full-text appraisal of 81 studies, 40 studies were included (3, 13, 20–57), involving 215,718 pregnant women with an immigration background from conflict-zone countries and 12,806,469 native-origin women. The manual search yielded no additional study. Characteristics of the included studies were summarized in Table 1. The quality appraisal of the included studies has been presented in Supplementary Tables 2, 3. A total of 30 studies were judged as high quality (3, 13, 20, 22–26, 28, 30, 32, 34, 36–38, 40–44, 46–50, 52, 54–56); 10 for moderate quality (21, 29, 31, 33, 35, 39, 45, 51, 53, 57); and no study had low quality.
A total of 77.5% of studies were conducted in Europe [n = 31, including Norway (3, 34, 42, 43, 49, 50, 52, 54, 56), Finland (23, 24), Israel (28, 40), Turkey (26–31, 33, 35, 37, 39, 45, 51), Sweden (32, 36, 38, 48), Finland (41), Denmark (44, 47), Netherlands (53), UK (57)], 7.5% in Asia [n = 3, including Lebanon (20), Jordan (21), Pakistan (22)], and 12.5% in others (n = 5, including USA (13, 56), Canada (46), and Australia (25–27)].
The pooled OR and estimation of heterogeneity and publication bias have been shown in Table 2. However, no substantial publication bias based on the Harbord test was observed, except for macrosomia, which was corrected using the trim and fill method of publication bias adjustment. The risk of most serious adverse neonatal outcomes, analyzed using the random-effects model in the immigrant women, was significantly higher compared to the native pregnant women. In this respect, the risk of small for gestational age (SGA) (Pooled OR = 1.8, 95% CI = 1.6, 2.1), a 5-min Apgar score <7 (Pooled OR = 1.4, 95% CI = 1.0, 2.1), stillbirth (Pooled OR = 1.9, 95% CI = 1.2, 3.0), and perinatal mortality (Pooled OR = 2.0, 95% CI = 1.6, 2.5) were all significantly higher in the immigrant women compared to the native-origin women (Figures 2–5). In contrast, the immigrant women had a lower risk of macrosomia (Pooled OR = 0.6, 95% CI = 0.5–0.7), large for gestational age (LGA) (Pooled OR = 0.5, 95% CI = 0.4–0.7), and preterm birth (Pooled OR = 0.9, 95% CI = 0.8–0.9) compared to their native counterparts (Figures 6–8). However, the risk of all maternal outcomes, including the cesarean section (C-S) and emergency C-S, instrumental delivery, preeclampsia, and gestational diabetes mellitus (GDM), were similar in both groups (Supplementary Figures 1–5).
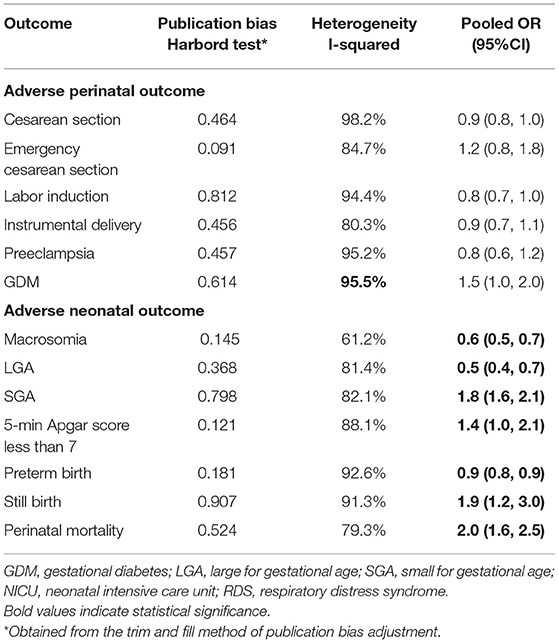
Table 2. Heterogeneity, estimation of publication bias, and meta-analysis of the included studies on the prevalence of adverse maternal and neonatal outcomes.
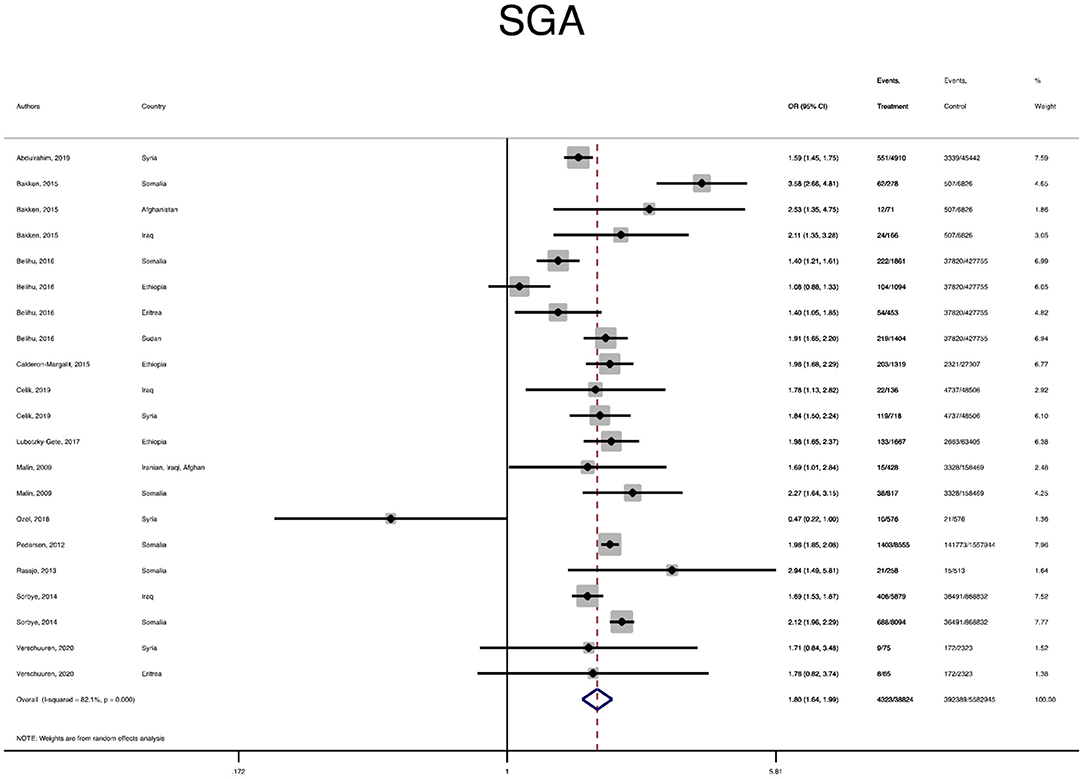
Figure 2. A forest plot of the pooled odds ratio of small for gestational age (SGA) in the immigrant and native-origin populations.
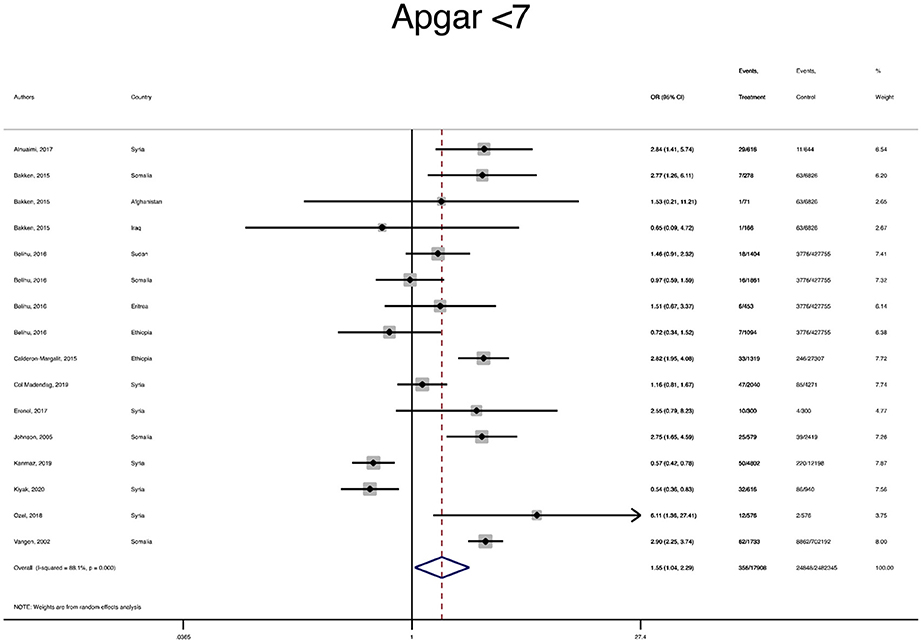
Figure 3. A forest plot of the pooled odds ratio of a 5-min Apgar score less than 7 in the immigrant and native-origin populations.
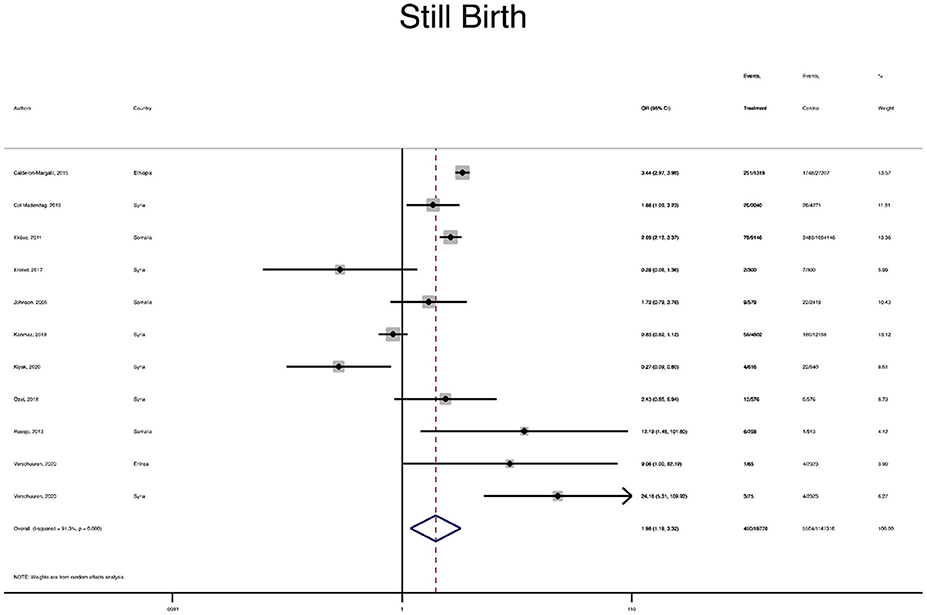
Figure 4. A forest plot of the pooled odds ratio of still birth in the immigrant and native-origin populations.
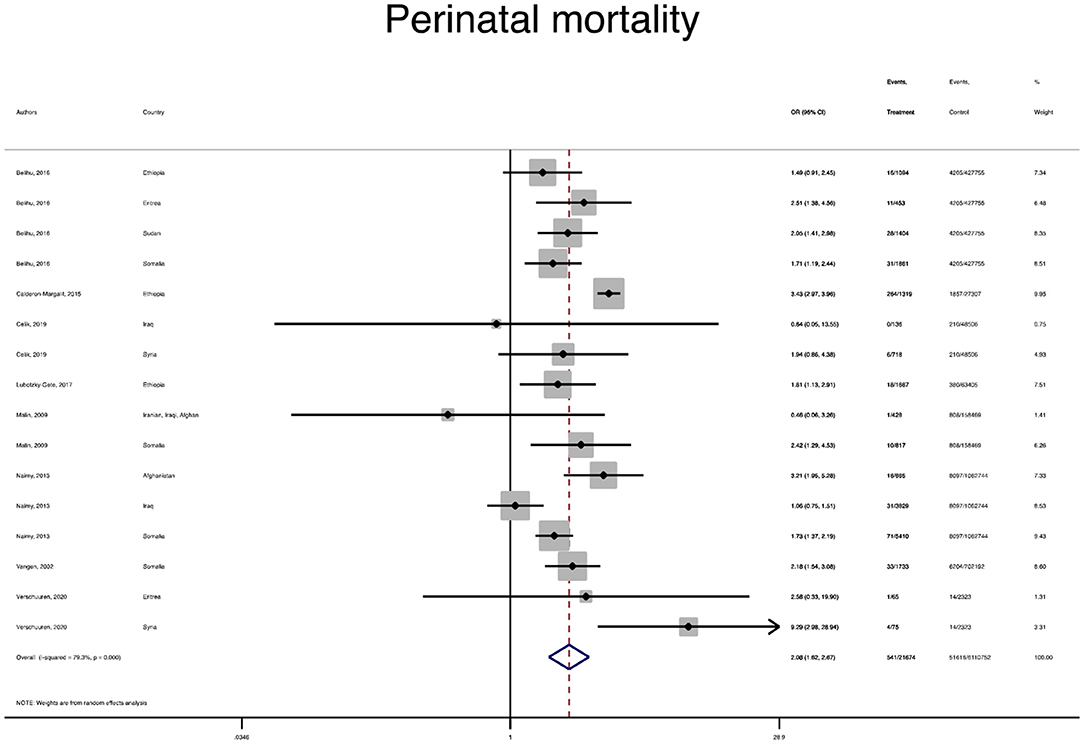
Figure 5. A forest plot of the pooled odds ratio of perinatal mortality in the immigrant and native-origin populations.
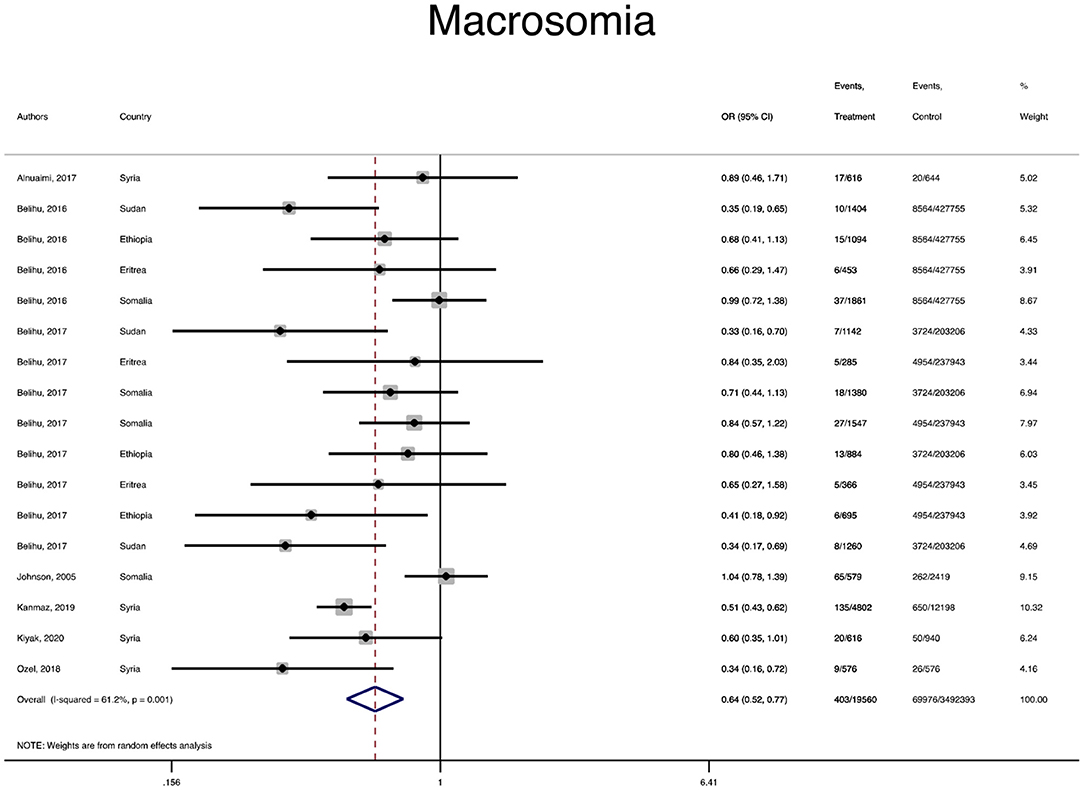
Figure 6. A forest plot of the pooled odds ratio of macrosomia in the immigrant and native-origin populations.
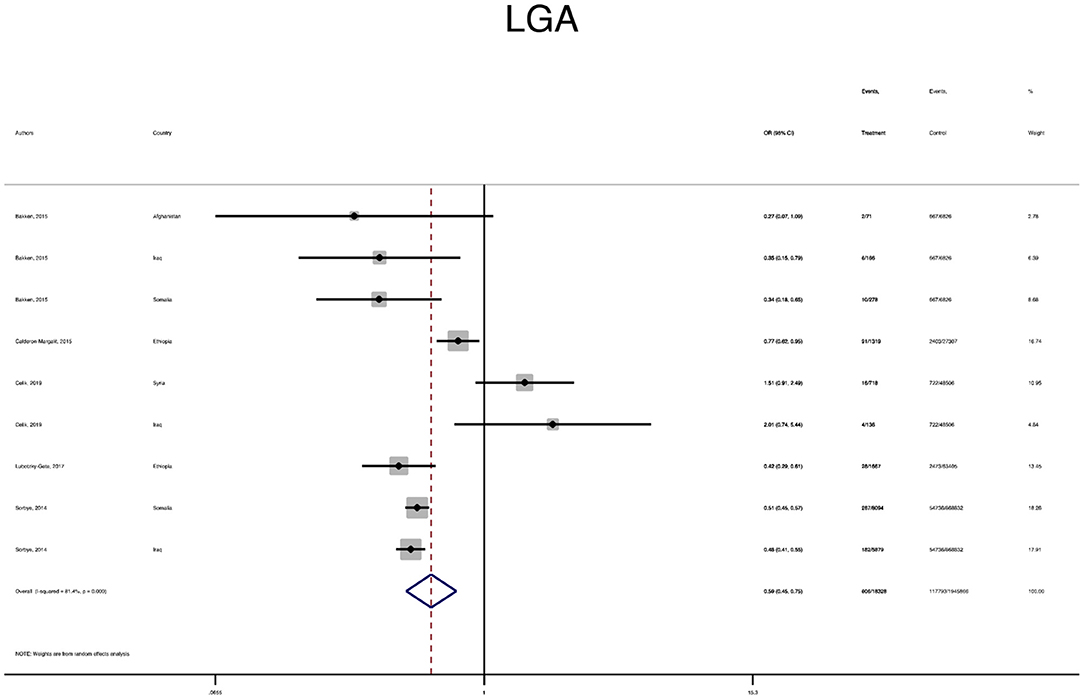
Figure 7. A forest plot of the pooled odds ratio of large for gestational age (LGA) in the immigrant and native-origin populations.
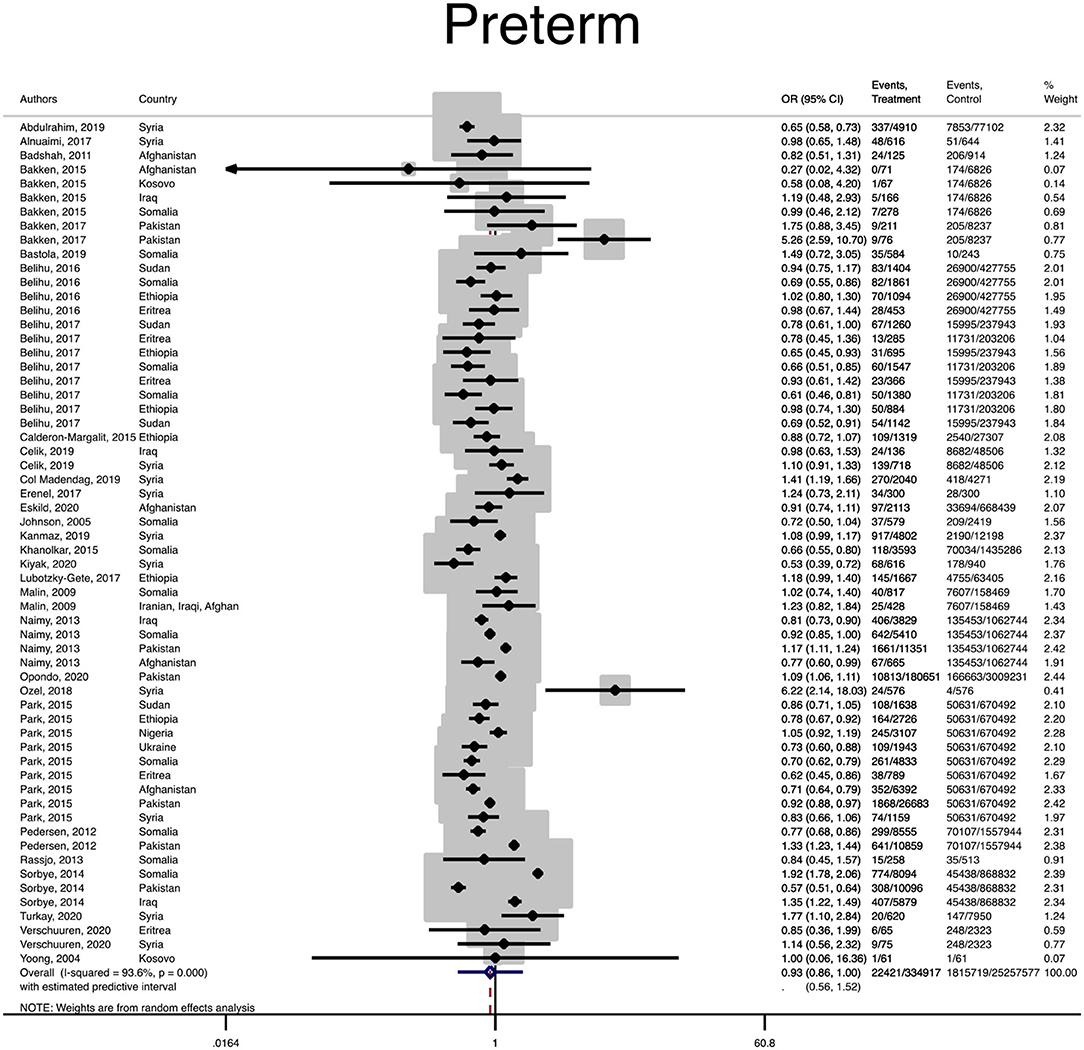
Figure 8. Forest plot of the pooled odds ratio of preterm birth in the immigrant and native-origin populations.
The results were highly consistent with the main results of data analysis, and no substantial modification of the estimates of change was reported after the exclusion of individual studies (Supplementary Figures 6A–M).
This systematic review and meta-analysis showed that, among the immigrants from conflict-zone countries, the risk of adverse neonatal outcomes, including SGA, a 5-min Apgar score <7, stillbirth, and perinatal mortality, was higher compared with the native-origin women. However, the risk of adverse maternal outcomes such as C-S and emergency C-S, labor induction, instrumental delivery, preeclampsia, and GDM was similar in both groups.
There is no consensus on the definition of an immigrant in the international literature. Immigration has a significant impact on public health outcomes (58). It is well-documented that diversity in genetics, environment, behavior, and, also, the disparity in the socioeconomics situation at both individual and societal levels can influence the health status of immigrants (6). However, the health effects of armed conflicts have remained unexplored (59). Generally, some studies have reported similar pre-migration exposures to armed conflicts and post-migration health problems among immigrants, which are both generally poorer than the population of host counties (60, 61). However, it is argued that pregnancy may increase the risk of health problems among immigrants. Our review revealed that the risk of maternal outcomes was comparable, but the risk of most serious adverse neonatal outcomes among the immigrant women from conflict-zone countries was significantly higher than those women in host countries. In this respect, being an immigrant from a conflict-zone country does not guarantee that he or she has been exposed to trauma or violence. Nevertheless, he or she has greater exposure to perceived threats of violence, chronic stress, and physical violence (62, 63), which may have led to health problems (64).
Female refugees of child-bearing age are more vulnerable to stress exposure, which can increase the risk of preventable adverse neonatal outcomes. Moreover, many of these adverse neonatal outcomes are related to preventable risk factors such as difficulties in access to timely prenatal care in host countries (65). However, due to multiple underlying reasons such as language and cultural barriers, and the policy and social systems in host countries, these women tend to initiate prenatal care lately and have fewer prenatal visits (66). It should be noted that many of these adverse outcomes not only have immediate adverse effects on neonates but also can have long-lasting consequences on the growth and development of the newborn well into adulthood (66, 67).
We found that the risk of adverse maternal outcomes among the immigrants was similar to the native population. Some studies have found a “healthy-migrant effect” among immigrants, which is a similar or a better health status than the population in host countries (68). It is hypothesized that immigrants represent a selectively healthy and young group of people, and, therefore, their health status stands out compared to the general native population in host countries (69–71). The effect of the healthy immigrants may be translated across some maternal outcomes among immigrants' mothers from conflict-zone countries. In addition, Bakken et al. (3) argued that women originating from various conflict-zone countries may experience different risks of adverse perinatal outcomes. They reported that immigrant women from Somalia needed more targeted care during pregnancy and childbirth than those from Kozovo (3).
Despite our review results that exclusively focus on pregnant women from conflict-zone countries, our meta-analysis summarized available evidence regarding the perinatal health issues among these groups of women. The quality of the included studies was either moderate or high. Since no study was considered to be of poor quality, it helped us to represent the acceptable quality of evidence in this meta-analysis.
The main limitation of this study was the lack of data on potential risk factors in included studies, which might have potentially affected the outcomes of interest. In addition, the rate of iatrogenic C-S due to GDM and pre-eclampsia was not reported due to the lack of data in the included original manuscripts. Although many war immigrants are undocumented, the lack of data on the maternal duration of residence in host countries, as well as heterogeneity between immigrants, asylum seekers, and refugees did not let us perform subgroup analysis among them.
In conclusion, our systematic review and meta-analysis demonstrated that the risk of some adverse maternal outcomes was comparable, but the immigrant women from conflict-zone countries had a higher risk of neonatal mortality and morbidity, including SGA, a 5-min Apgar score <7, stillbirth, and perinatal mortality compared to the native-origin population. This study shows the need for the application of preventive strategies to prevent missing valuable opportunities and to optimize health across two generations. Further investigation into long-term adverse pregnancy outcomes for this population is warranted.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Nord University, Bodø, Norway covered the processing charge to this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.766943/full#supplementary-material
1. World Health Organization. Report on the Health of Refugees and Migrants in the WHO European Region: No Public Health Without Refugee and Migrant Health. (2018). World Health Organization: Copenhagen. https://www.euro.who.int/en/publications/abstracts/report-on-the-health-of-refugees-and-migrants-in-the-who-european-region-no-public-health-without-refugee-and-migrant-health-2018 (accessed August 10, 2021).
2. UNHCR. United Nations High Commissioner for Refugees, Global Trends for Forced Displacement in 2019. (2019). Available online at: https://www.unhcr.org/flagship-reports/globaltrends/globaltrends2019/ (accessed August 10, 2021).
3. Bakken KS, Skjeldal OH, Stray-Pedersen B. Immigrants from conflict-zone countries: an observational comparison study of obstetric outcomes in a low-risk maternity ward in Norway. BMC Pregnancy Childbirth. (2015) 15:163. doi: 10.1186/s12884-015-0603-3
4. Castañeda H, Holmes SM, Madrigal DS, Young ME, Beyeler N, Quesada J. Immigration as a social determinant of health. Annu Rev Public Health. (2015) 36:375–92. doi: 10.1146/annurev-publhealth-032013-182419
5. Elisabeth M, Maneesh PS, Katarina SF, Slobodan Z, Michael S. Antimicrobial resistance and migrants in Sweden: poor living conditions enforced by migration control policies as a risk factor for optimal public health management. Front Public Health. (2021) 9:642983. doi: 10.3389/fpubh.2021.642983
6. Wickramage K, Vearey J, Zwi AB, Robinson C, Knipper M. Migration and health: a global public health research priority. BMC Public Health. (2018) 18:987. doi: 10.1186/s12889-018-5932-5
7. Gieles NC, Tankink JB, van Midde M, Düker J, van der Lans P, Wessels CM, et al. Maternal and perinatal outcomes of asylum seekers and undocumented migrants in Europe: a systematic review. Eur J Public Health. (2019) 29:714–23. doi: 10.1093/eurpub/ckz042
8. Dopfer C, Vakilzadeh A, Happle C, Kleinert E, Müller F, Ernst D, et al. Pregnancy related health care needs in refugees-a current three center experience in Europe. Int J Environ Res Public Health. (2018) 15:1934. doi: 10.3390/ijerph15091934
9. Ekmekci PE. Syrian refugees, health and migration legislation in Turkey. J Immigr Minor Health. (2017) 19:1434–41. doi: 10.1007/s10903-016-0405-3
10. Alemi Q, Stempel C, Koga PM, Smith V, Danis D, Baek K, et al. Determinants of health care services utilization among first generation Afghan migrants in Istanbul. Int J Environ Res Public Health. (2017) 14:201. doi: 10.3390/ijerph14020201
11. Wanigaratne S, Cole DC, Bassil K, Hyman I, Moineddin R, Shakya Y, et al. Severe neonatal morbidity among births to refugee women. Matern Child Health J. (2016) 20:2189–98. doi: 10.1007/s10995-016-2047-4
12. Dadras O, Nakayama T, Kihara M, Ono-Kihara M, Seyedalinaghi S, Dadras F. The prevalence and associated factors of adverse pregnancy outcomes among Afghan women in Iran; Findings from community-based survey. PLoS ONE. (2021) 16:e0245007-e. doi: 10.1371/journal.pone.0245007
13. Johnson EB, Reed SD, Hitti J, Batra M. Increased risk of adverse pregnancy outcome among Somali immigrants in Washington state. Am J Obstet Gynecol. (2005) 193:475–82. doi: 10.1016/j.ajog.2004.12.003
14. Liu C, Ahlberg M, Hjern A, Stephansson O. Perinatal health of refugee and asylum-seeking women in Sweden 2014-17: a register-based cohort study. Eur J Public Health. (2019) 29:1048–55. doi: 10.1093/eurpub/ckz120
15. Small R, Gagnon A, Gissler M, Zeitlin J, Bennis M, Glazier R, et al. Somali women and their pregnancy outcomes postmigration: data from six receiving countries. BJOG. (2008) 115:1630–40. doi: 10.1111/j.1471-0528.2008.01942.x
16. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
17. International Organization for Migration (IOM). World Migration Report 2020. Available online at: https://publications.iom.int/system/files/pdf/wmr_2020.pdf (accessed March 09, 2021).
18. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
19. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
20. Abdulrahim S, El Rafei R, Beydoun Z, El Hayek GY, Nakad P, Yunis K, et al. Test of the epidemiological paradox in a context of forced migration: low birthweight among Syrian newborns in Lebanon. Int J Epidemiol. (2019) 48:275–86. doi: 10.1093/ije/dyy200
21. Alnuaimi K, Kassab M, Ali R, Mohammad K, Shattnawi K. Pregnancy outcomes among Syrian refugee and Jordanian women: a comparative study. Int Nurs Rev. (2017) 64:584–92. doi: 10.1111/inr.12382
22. Badshah S, Mason L, Mckelvie K, Payne R, Lisboa PJ. Maternal risk factors in Afghan-refugees compared to Pakistani mothers in Peshawar, NWFP Pakistan. J Pak Med Assoc. (2011) 61:161–4.
23. Bastola K, Koponen P, Härkänen T, Luoto R, Gissler M, Kinnunen TI. Delivery and its complications among women of Somali, Kurdish, and Russian origin, and women in the general population in Finland. Birth. (2019) 46:35–41. doi: 10.1111/birt.12357
24. Bastola K, Koponen P, Härkänen T, Luoto R, Gissler M, Kinnunen TI. Pregnancy complications in women of Russian, Somali, and Kurdish origin and women in the general population in Finland. Womens Health. (2020) 16:1745506520910911. doi: 10.1177/1745506520910911
25. Belihu FB, Davey MA, Small R. Perinatal health outcomes of East African immigrant populations in Victoria, Australia: a population based study. BMC Preg Childbirth. (2016) 16:86. doi: 10.1186/s12884-016-0886-z
26. Belihu FB, Small R, Davey MA. Episiotomy and severe perineal trauma among Eastern African immigrant women giving birth in public maternity care: a population based study in Victoria, Australia. Women Birth. (2017) 30:282–90. doi: 10.1016/j.wombi.2016.11.008
27. Belihu FB, Small R, Davey MA. Variations in first-time caesarean birth between Eastern African immigrants and Australian-born women in public care: A population-based investigation in Victoria. Aust N Z J Obstet Gynaecol. (2017) 57:294–301. doi: 10.1111/ajo.12491
28. Calderon-Margalit R, Sherman D, Manor O, Kurzweil Y. Adverse perinatal outcomes among immigrant women from Ethiopia in Israel. Birth. (2015) 42:125–31. doi: 10.1111/birt.12163
29. Çelik IH, Arslan Z, Ulubaş Işik D, Tapisiz ÖL, Mollamahmutoglu L, Baş AY, et al. Neonatal outcomes in Syrian and other refugees treated in a tertiary hospital in Turkey. Turk J Med Sci. (2019) 49:815–20. doi: 10.3906/sag-1806-86
30. Col Madendag I, Eraslan Sahin M, Madendag Y, Sahin E, Demir MB, Ozdemir F, et al. The effect of immigration on adverse perinatal outcomes: analysis of experiences at a Turkish Tertiary Hospital. Biomed Res Int. (2019) 2019:2326797. doi: 10.1155/2019/2326797
31. Demirci H, Yildirim Topak N, Ocakoglu G, Karakulak Gomleksiz M, Ustunyurt E, Ulku Turker A. Birth characteristics of Syrian refugees and Turkish citizens in Turkey in 2015. Int J Gynaecol Obstet. (2017) 137:63–6. doi: 10.1002/ijgo.12088
32. Ekéus C, Cnattingius S, Essén B, Hjern A. Stillbirth among foreign-born women in Sweden. Eur J Public Health. (2011) 21:788–92. doi: 10.1093/eurpub/ckq200
33. Erenel H, Aydogan Mathyk B, Sal V, Ayhan I, Karatas S, Koc Bebek A. Clinical characteristics and pregnancy outcomes of Syrian refugees: a case-control study in a tertiary care hospital in Istanbul, Turkey. Arch Gynecol Obstet. (2017) 295:45–50. doi: 10.1007/s00404-016-4188-5
34. Eskild A, Sommerfelt S, Skau I, Grytten J. Offspring birthweight and placental weight in immigrant women from conflict-zone countries; does length of residence in the host country matter? A population study in Norway. Acta Obstet Gynecol Scand. (2020) 99:615–22. doi: 10.1111/aogs.13777
35. Güngör ES, Seval O, Ilhan G, Verit FF. Do Syrian refugees have increased risk for worser pregnancy outcomes? Results of a tertiary center in Istanbul Turk J Obstet Gynecol. (2018) 15:23–7. doi: 10.4274/tjod.64022
36. Juárez SP, Small R, Hjern A, Schytt E. Caesarean birth is associated with both maternal and paternal origin in immigrants in Sweden: a population-based study. Paediatr Perinat Epidemiol. (2017) 31:509–21. doi: 10.1111/ppe.12399
37. Kanmaz AG, Inan AH, Beyan E, Özgür S, Budak A. Obstetric outcomes of Syrian refugees and Turkish citizens. Arch Iran Med. (2019) 22:482–8.
38. Khanolkar AR, Wedrén S, Essén B, Sparén P, Koupil I. Preterm and postterm birth in immigrant- and Swedish-born parents: a population register-based study. Eur J Epidemiol. (2015)30:435–47. doi: 10.1007/s10654-014-9986-0
39. Kiyak H, Gezer S, Ozdemir C, Gunkaya S, Karacan T, Gedikbasi A. Comparison of delivery characteristics and early obstetric outcomes between Turkish women and Syrian refugee pregnancies. Niger J Clin Pract. (2020) 23:12–7. doi: 10.4103/njcp.njcp_10_18
40. Lubotzky-Gete S, Shoham-Vardi I, Sheiner E. Comparing pregnancy outcomes of immigrants from Ethiopia and the Former Soviet Union to Israel, to those of Native-Born Israelis. J Immigr Minor Health. (2017) 19:1296–303. doi: 10.1007/s10903-016-0484-1
41. Malin M, Gissler M. Maternal care and birth outcomes among ethnic minority women in Finland. BMC Public Health. (2009) 9:84. doi: 10.1186/1471-2458-9-84
42. Naimy Z, Grytten J, Monkerud L, Eskild A. Perinatal mortality in non-western migrants in Norway as compared to their countries of birth and to Norwegian women. BMC Public Health. (2013) 13:37. doi: 10.1186/1471-2458-13-37
43. Naimy Z, Grytten J, Monkerud L, Eskild A. The prevalence of pre-eclampsia in migrant relative to native Norwegian women: a population-based study. BJOG. (2015) 122:859–65. doi: 10.1111/1471-0528.12978
44. Kragelund Nielsen K, Andersen GS, Damm P, Andersen AN. Gestational diabetes risk in migrants. a nationwide, register-based study of all births in Denmark 2004 to 2015. J Clin Endocrinol Metab. (2020) 105:dgaa024. doi: 10.1210/clinem/dgaa024
45. Ozel S, Yaman S, Kansu-Celik H, Hancerliogullari N, Balci N, Engin-Ustun Y. Obstetric outcomes among Syrian refugees: a comparative study at a tertiary care maternity hospital in Turkey. Rev Bras Ginecol Obstet. (2018) 40:673–9. doi: 10.1055/s-0038-1673427
46. Park AL, Urquia ML, Ray JG. Risk of preterm birth according to maternal and paternal country of birth: a population-based study. J Obstet Gynaecol Can. (2015) 37:1053–62. doi: 10.1016/S1701-2163(16)30070-6
47. Pedersen GS, Mortensen LH, Gerster M, Rich-Edwards J, Andersen AM. Preterm birth and birthweight-for-gestational age among immigrant women in Denmark 1978-2007: a nationwide registry study. Paediatr Perinat Epidemiol. (2012) 26:534–42. doi: 10.1111/ppe.12010
48. Råssjö EB, Byrskog U, Samir R, Klingberg-Allvin M. Somali women's use of maternity health services and the outcome of their pregnancies: a descriptive study comparing Somali immigrants with native-born Swedish women. Sex Reprod Healthc. (2013) 4:99–106. doi: 10.1016/j.srhc.2013.06.001
49. Sørbye IK, Daltveit AK, Sundby J, Stoltenberg C, Vangen S. Caesarean section by immigrants' length of residence in Norway: a population-based study. Eur J Public Health. (2015) 25:78–84. doi: 10.1093/eurpub/cku135
50. Sørbye IK, Daltveit AK, Sundby J, Vangen S. Preterm subtypes by immigrants' length of residence in Norway: a population-based study. BMC Pregnancy Childbirth. (2014) 14:239. doi: 10.1186/1471-2393-14-239
51. Turkay Ü, Aydin Ü, Salici M, Çalişkan E, Terzi H, Astepe BS, et al. Comparison of pregnant Turkish women and Syrian refugees: Does living as a refugee have an unfavorable effect on pregnancy outcomes? Int J Gynaecol Obstet. (2020) 149:160–5. doi: 10.1002/ijgo.13117
52. Vangen S, Stoltenberg C, Johansen RE, Sundby J, Stray-Pedersen B. Perinatal complications among ethnic Somalis in Norway. Acta Obstet Gynecol Scand. (2002) 81:317–22. doi: 10.1034/j.1600-0412.2002.810407.x
53. Verschuuren AEH, Postma IR, Riksen ZM, Nott RL, Feijen-de Jong EI, Stekelenburg J. Pregnancy outcomes in asylum seekers in the North of the Netherlands: a retrospective documentary analysis. BMC Pregnancy Childbirth. (2020) 20:320. doi: 10.1186/s12884-020-02985-x
54. Bakken KS, Skjeldal OH, Stray-Pedersen B. Obstetric outcomes of first- and second-generation Pakistani immigrants: a comparison study at a low-risk maternity ward in Norway. J Immigr Minor Health. (2017) 19:33–40. doi: 10.1007/s10903-015-0329-3
55. Sanchalika A, Teresa J. Risk of gestational diabetes among south Asian immigrants living in New Jersey–a retrospective data review. J Racial Ethn Health Disparities. (2015) 2:510–6. doi: 10.1007/s40615-015-0099-6
56. Vangen S, Stoltenberg C, Skrondal A, Magnus P, Stray-Pedersen B. Cesarean section among immigrants in Norway. Acta Obstet Gynecol Scand. (2000) 79:553–8. doi: 10.1080/j.1600-0412.2000.079007553.x
57. Yoong W, Wagley A, Fong C, Chukwuma C, Nauta M. Obstetric performance of ethnic Kosovo Albanian asylum seekers in London: a case-control study. J Obstet Gynaecol. (2004) 24:510–2. doi: 10.1080/01443610410001722527
58. Gushulak B, Weekers J, Macpherson D. Migrants and emerging public health issues in a globalized world: threats, risks and challenges, an evidence-based framework. Emerg Health Threats J. (2009) 2:e10-e. doi: 10.3134/ehtj.09.010
59. Green JC, BeLue R, Boakye EA, Choi E, Vaughn MG. Armed conflict in Central America and immigrant health in the United States. Ann Glob Health. (2018) 84:654–62. doi: 10.29024/aogh.2373
60. Fazel M, Reed RV, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in high-income countries: risk and protective factors. Lancet. (2012) 379:266–82. doi: 10.1016/S0140-6736(11)60051-2
61. Bohra-Mishra P, Massey DS. Individual decisions to migrate during civil conflict. Demography. (2011) 48:401–24. doi: 10.1007/s13524-011-0016-5
62. Nissen AF, Sengoelge M, Solberg Ø. Post-migration stressors and subjective well-being in adult Syrian refugees resettled in Sweden: a gender perspective. Front Public Health. (2021) 9:717353. doi: 10.3389/fpubh.2021.717353
63. Liu C, Urquia M, Cnattingius S, Hjern A. Migration and preterm birth in war refugees: a Swedish cohort study. Eur J Epidemiol. (2014) 29:141–3. doi: 10.1007/s10654-013-9877-9
64. Hollander AC, Bruce D, Burström B, Ekblad S. Gender-related mental health differences between refugees and non-refugee immigrants—a cross-sectional register-based study. BMC Public Health. (2011) 11:180. doi: 10.1186/1471-2458-11-180
65. Heslehurst N, Brown H, Pemu A, Coleman H, Rankin J. Perinatal health outcomes and care among asylum seekers and refugees: a systematic review of systematic reviews. BMC Med. (2018) 16:89. doi: 10.1186/s12916-018-1064-0
66. Malebranche M, Nerenberg K, Metcalfe A, Fabreau GE. Addressing vulnerability of pregnant refugees. Bull World Health Organ. (2017) 95:611-A. doi: 10.2471/BLT.17.193664
67. Bains S, Sundby J, Lindskog BV, Vangen S, Sørbye IK. Newly arrived migrant women's experience of maternity health information: a face-to-face Questionnaire study in Norway. Int J Environ Res Public Health. (2021) 18:7523. doi: 10.3390/ijerph18147523
68. Helgesson M, Johansson B, Nordquist T, Vingård E, Svartengren M. Healthy migrant effect in the Swedish context: a register-based, longitudinal cohort study. BMJ Open. (2019) 9:e026972-e. doi: 10.1136/bmjopen-2018-026972
69. Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic paradox: demographic and epidemiologic approaches. Ann N Y Acad Sci. (2001) 954:140–74. doi: 10.1111/j.1749-6632.2001.tb02751.x
70. Miller LS, Robinson JA, Cibula DA. Healthy immigrant effect: preterm births among immigrants and refugees in Syracuse, NY. Matern Child Health J. (2016) 20:484–93. doi: 10.1007/s10995-015-1846-3
Keywords: conflict-zone countries, immigrant, neonatal outcomes, perinatal outcomes, meta-analysis
Citation: Behboudi-Gandevani S, Bidhendi-Yarandi R, Panahi MH, Mardani A, Prinds C and Vaismoradi M (2022) Perinatal and Neonatal Outcomes in Immigrants From Conflict-Zone Countries: A Systematic Review and Meta-Analysis of Observational Studies. Front. Public Health 10:766943. doi: 10.3389/fpubh.2022.766943
Received: 30 August 2021; Accepted: 03 February 2022;
Published: 11 March 2022.
Edited by:
Amanda Rodrigues Amorim Adegboye, Coventry University, United KingdomReviewed by:
Matthias David, Charité University Medicine Berlin, GermanyCopyright © 2022 Behboudi-Gandevani, Bidhendi-Yarandi, Panahi, Mardani, Prinds and Vaismoradi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samira Behboudi-Gandevani, c2FtaXJhLmJlaGJvdWRpLWdhbmRldmFuaUBub3JkLm5v
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.