- 1Department of Community Programs, Dhulikhel Hospital Kathmandu University Hospital, Kathmandu University, Dhulikhel, Nepal
- 2National Centre for Epidemiology and Population Health, Research School of Population Health, The Australian National University, Canberra, ACT, Australia
- 3Centre for Primary Health Care and Equity, University of New South Wales, Sydney, NSW, Australia
- 4School of Health, Medical and Applied Sciences, College of Science and Sustainability, Central Queensland University, Rockhampton, QLD, Australia
- 5Centre for Oral Health Outcomes & Research Translation (COHORT), School of Nursing and Midwifery, Western Sydney University, Sydney, NSW, Australia
- 6Department of International Affairs and Tropical Medicine, Tokyo Women's Medical University, Tokyo, Japan
- 7Physical Activity Research Group, Appleton Institute, Central Queensland University, Rockhampton, QLD, Australia
- 8Translational Health Research Institute, Western Sydney University, Sydney, NSW, Australia
Background: Nepal, in recent years, is witnessing an increasing problem of type 2 diabetes that has resulted significant premature deaths and disability. Prevention and management of non-communicable diseases (NCDs) including diabetes have been prioritized in the national policies and guidelines of the Nepal Government. However, research looking at the overview of the implementation of the existing policies and guidelines for diabetes prevention and control is scarce. Hence, this study reviewed diabetes related existing policies and its implementation process at the primary health care level in Nepal.
Methods: This study involved two phases: Phase I: situation analyses through review of documents and Phase II: qualitative exploratory study. In phase I, four databases (Medline, Web of Science, Embase and PubMed) were systematically searched using key search terms related to diabetes care and policies between January 2000 and June 2021. Also, relevant gray literature was reviewed to understand the trajectory of policy development and its translation with regards to diabetes prevention and management at primary health care level in Nepal. Following the phase I, we conducted in-depth interviews (IDI) and key informant interviews (KII) with health care providers, policy makers, and managers (IDI = 13, and KII = 7) at peripheral and central levels in Kavrepalanchowk and Nuwakot districts of Nepal. The in-depth interviews were audio recorded, transcribed, and coded. The triangulation of data from document review and interviews was done and presented in themes.
Results: Four key themes were identified through triangulating findings from the document review and interviews including (i) limited implementation of policies into practices; (ii) lack of coordination among the different levels of service providers; (iii) lack of trained human resources for health and inadequate quality services at the primary health care level, and (iv) inadequate access and utilization of diabetes care services at primary health care level. Specifically, this study identified some key pertinent challenges to the implementation of policies and programs including inadequate resources, limited engagement of stakeholders in service design and delivery, lack of trained health care providers, lack of financial resources to strengthen peripheral health services, fragmented health governance, and weak reporting and monitoring systems.
Conclusion: This study revealed that the policies, plans, and strategies for prevention and management of NCDs in Nepal recognized the importance of diabetes prevention and control. However, a major gap remains with adequate and lack of clarity in terms of implementation of available policies, plans, strategies, and programs to address the problem of diabetes. We suggest the need for multisectoral approach (engaging both health and non-health sectors) at central as well as peripheral levels to strengthen the policies implementation process, building capacity of health care providers, ensuring adequate financial and non-financial resources, and improving quality of services at primary health care levels.
Introduction
Diabetes mellitus is one of the most prevalent chronic conditions associated with increasing morbidity, mortality, and economic burden worldwide (1). In 2019, there were 463 million adults living with diabetes worldwide, and this number is estimated to reach 700 million by the year 2045 (2). An additional 374 million people had prediabetes and were at a risk of developing type 2 diabetes (2) The burden of diabetes and its impact on life of the people is substantially higher in low middle income countries (LMICs), in comparison to high-income countries (3). The United Nations (UN) Sustainable Development Goals (SDG-3 Health and Wellbeing); target 4 that focuses on prevention and treatment of non-communicable diseases (NCDs), has prioritized in reducing the global burden of NCDs including diabetes. Likewise, the WHO (World Health Organization) Global Action Plan on NCDs (2013–2020) has emphasized to raise the priority in the national and international agendas and goals to the prevention and control of NCDs, through strengthened international cooperation and advocacy” (4).
South Asia, where a quarter of the world population resides, has a majority of all global diabetes cases (5). Nepal, a South Asian developing country has a high prevalence of both prediabetes (9.2%) and diabetes (8.5%) cases (6). However, the burden of diabetes is likely underreported because the peripheral health system of Nepal has not yet been well equipped with the infrastructure to screen, diagnose, and treat the cases with diabetes (7–10). Despite the polices and guidelines in prevention and management of diabetes in Nepal, there are significant challenges, including limited health care facilities and medications within the current health care system and lack of awareness about diabetes and healthy lifestyle related behaviors among people (8–10).
Being cognizant of the impacts of NCDs including diabetes, the Government of Nepal (GoN), in recent years, has developed some policies, guidelines, and manuals to guide the prevention and management of NCDs including diabetes. The Government of Nepal annual report shows that different level of NCDs related services are being provided at local health facilities, such as services for hypertension and diabetes detection, counseling, referral, follow up services for NCDs patients including diabetes, drugs refilling, and health promotion related services (11). This initiative reflects the greater effort of the Government of Nepal toward the prevention and control of diabetes. The Government of Nepal, in recent years, has launched a multisectoral Action Plan for the prevention and control of NCDs and implemented PEN (package of essential non-communicable disease) in selected districts of Nepal.
Despite the development of policies and strategies on NCDs including diabetes prevention and control in the country, the evidence on the implementation of these policies remained largely unexplored. Therefore, in this study, we systematically reviewed the existing literature that included both academic literature and policies specific to diabetes in Nepal and then conducted a qualitative study, to explore the implementation aspects of policies and strategies related to diabetes prevention and management in Nepal. The study aimed to answer two research questions: (i) What are the policies and guidelines being developed to prevent and control type 2 diabetes in Nepal (ii) what is the implementation status of the existing policies and guidelines for diabetes prevention and control in Nepal?
Methods
This study adopted an approach of combining documents review and in-depth interviews (IDI) and key informant interviews (KII) to answer the research questions. This approach has been widely adopted in the previous studies to identify the factors in the inclusion and prioritization of NCDs in polices, guidelines, and actions plans (12–15). In phase I, we systematically searched and reviewed the relevant published academic literature and gray literature from websites of Ministry of Health to understand the trajectory of policy development and its translation with regards to diabetes in real world settings in Nepal. In phase II, we conducted in-depth interviews and key informant interviews with health care providers, policy makers, and managers. Details of the phase wise study are as follows.
Phase I: Situation Analyses Through Literature Review
In this phase, a systematic search was conducted in four key electronic databases including Medline, Web of Science, Embase, and PubMed to identify peer-reviewed journal articles and government documents (plans, policies, and guidelines). Also, gray literature was searched through google and webpage of the Ministry of Health and Population, Government of Nepal. The literature search was limited to the academic and gray literature published between 01 January 2000 and 31 June 2021. Most policies for NCDs prevention and control in Nepal have been formulated in recent decades (11). The National Nutrition Policy and Strategy initiated in 2004 also highlights the healthy eating pattern including household food security, improved dietary habits, and preventing lifestyle related diseases (16). We searched gray literature (particularly NCDs) related policies, and plans published in English as well as Nepali.
We considered search of literatures by using combinations of different keywords, namely “diabetes,” “people with diabetes,” “diabetes mellitus,” “sugar,” “guidelines,” “protocol,” “policy,” “guide,” standard practice,” “strategy,” “implementation,” “intervention,” “Nepal,” “health post,” “primary health care center,” “peripheral health system,” “facilitators,” “Barriers,” and “community health workers.”
Inclusion Criteria
The inclusion criteria of this study is:(i) The primary or secondary studies (both quantitative and qualitative) focused on diabetes prevention only, or management or prevention and management in Nepal; (ii) programs that cover health promotion, prevention, treatment, or rehabilitation activities for people with diabetes at the primary health care center or health post or community level (iii) Primary or secondary studies that focused on barriers and facilitators for management of diabetes in Nepal, and (iv) policies and plans documents focusing on NCDs in Nepal.
Exclusion Criteria
The exclusion criteria is: (i) studies including Gestational Diabetes Mellitus or Diabetes Insipidus (ii) studies that solely focused on estimating prevalence of diabetes in Nepal, (iii) clinical interventions studies of diabetes prevention or management, and (iv) studies based on hospital settings.
Data Extraction and Synthesis
The data extraction and synthesis process as recommended and by Heller et al. (12) and other researchers (13, 14) was adopted. The data obtained from the search and review of documents were extracted and presented in the narrative form. The key components/areas of the documents review were identified according to the objectives of the study. These include implementation of policies and strategies into practice, coordination among the different level of health care providers, primary health care challenges in delivering comprehensive care, and boundaries for the people with diabetes to access diabetes care at primary health care.
The results of document review guided the development of interview guide and inform the identification of the potential participants needed for the study to explore the implementation process of the existing policies and guidelines for diabetes management from the perspective of health care workers working with peripheral health system of Nepal.
Phase II: Exploratory Study
Study Setting
The qualitative study was conducted in Kavrepalanchowk and Nuwakot districts of Nepal. Kavre is one of the 77 districts of Nepal with Dhulikhel as its district headquarters and covers an area of 1,396 km2 (539 sq mi). Kavrepalanchok with an area of 1,396 sq.ft. is situated at a mid-hilly area majorly, having the subtropical climate with an elevation range of 280–3,018 m, bordered to the east by Ramechhap and Dolakha, west by Kathmandu valley, north by Sindhupalchok, and south by Sindhuli and Makawanpur. According to CBS, 2068, the total number of households is 80,720 with a total population of 381,937 including the number of men 182,936 (47.90%) and women 199,001 (52.10%). The adult literacy percentage is 62.77% and per capita income is $1399 (17). The people in this district rely upon income from the business and agricultural farming (18).
Nuwakot district is located in the Bagmati zone, covering an area of 1,121 km2 in the mid development region of Nepal. According to the national census 2011, the total population of the district is 2,77,471 comprising 1,32,787 men and 1,44,684 women. Of these, 54.6 spoke Nepali, 39.9 Tamang, 2.0 Newari, and 0.9% Lepcha as their first language (19). Agriculture, service, and industry are the major activities performed by the people of this district. A little over half of the (51.25%) population in this district is engaged in agriculture and 14.43% in some form of employment (20).
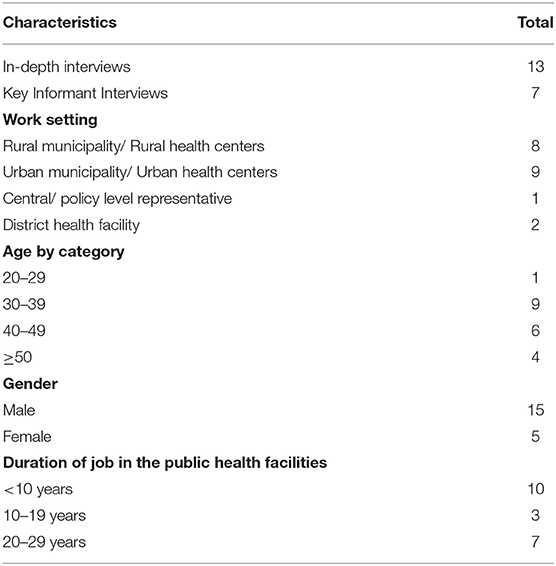
In this phase, IDIs (n = 13) and KIIs (n = 7) were conducted in two districts namely Kavrepalanchowk (n = 13) and Nuwakot (n = 7). These two districts were chosen due to the convenience for the researchers to access, where the study team has been implementing diabetes management intervention using the Randomized Controlled Trial. The interviews included 13 IDIs with health care providers at community level and 7 KIIs with health policy makers and program managers at central and district levels. The general characteristics of the participants involved in in-depth and key informant interviews are presented in Table 1.
We adopted purposive sampling to recruit the participants. A semistructured interview guide was used to obtain the data. The focus areas included in the interview schedule were (i) access, availability, and utilization of services for prevention and management of diabetes; (ii) facilitators and barriers to the prevention and management of diabetes; (iii) potentials to developing culturally appropriate and context specific intervention approaches to prevention and management of diabetes. Telephone interviews were conducted due to the COVID-19 restrictions. All the interviews were conducted in the Nepali language by two members of the research team (RS and DM). All in depth interviews and key informant interviews were audio recorded and were transcribed verbatim. The transcripts were then translated into English by a research team member (RS) and checked for accuracy by another team member (UNY). Three interview transcripts were randomly selected and checked by additional team members (UNY and LR) to ensure reliability of the transcription.
Data Processing and Analysis
The transcripts were individually read and re-read several times in order to become familiar with the data and to record initial ideas then organized into a coding framework, informed by the interview topic guide. A thematic analysis using an inductive approach was used to identify the emerging patterns and themes within the data (2017) (21). Themes were identified by comparing and contrasting the patterns and meanings as expressed by the participants. Two researchers (RS and DM) independently coded the transcripts and identified the themes which were further checked by another two researchers (UNY and AS) for accuracy. All project team members reviewed the final themes, and a consensus was achieved resolving the discrepancies through discussion. A final set of three major themes was identified and the qualitative findings are presented, accordingly. These include (i) access to and utilization of NCDs including the diabetes related programs in Nepal, (ii) challenges and enablers for prevention and management of diabetes in Nepal, and (iii) potentials to developing culturally appropriate and context specific intervention approaches to prevention and control of diabetes in Nepal. The triangulation of data from document review and interviews was guided by the data extraction and synthesis process as recommended by Heller et.al (12) and other researchers (13, 14).
The reporting of this qualitative research adhered to the Standards for Reporting Qualitative Research (SRQR) (22). Several strategies were employed to enhance the trustworthiness (credibility, transferability, dependability, confirmability, and transferability) of the study findings (23, 24). This included checking the data for accuracy, organizing debriefings for completeness of data (RS, DM, UNY and, LR). See Supplementary Material, SRQR Checklist.
Ethics Approval
This study is a part of an ongoing larger research project in Nepal, which uses a randomized controlled trial for diabetes self-management in Nepal. Ethics approval of the main study has been obtained from the Ethics Review Committees of Nepal Health Research Council, Nepal, Tokyo Women's Medical University and Central Queensland University Australia. Informed verbal consent was obtained from all participants prior to audio recordings of the interview.
Results
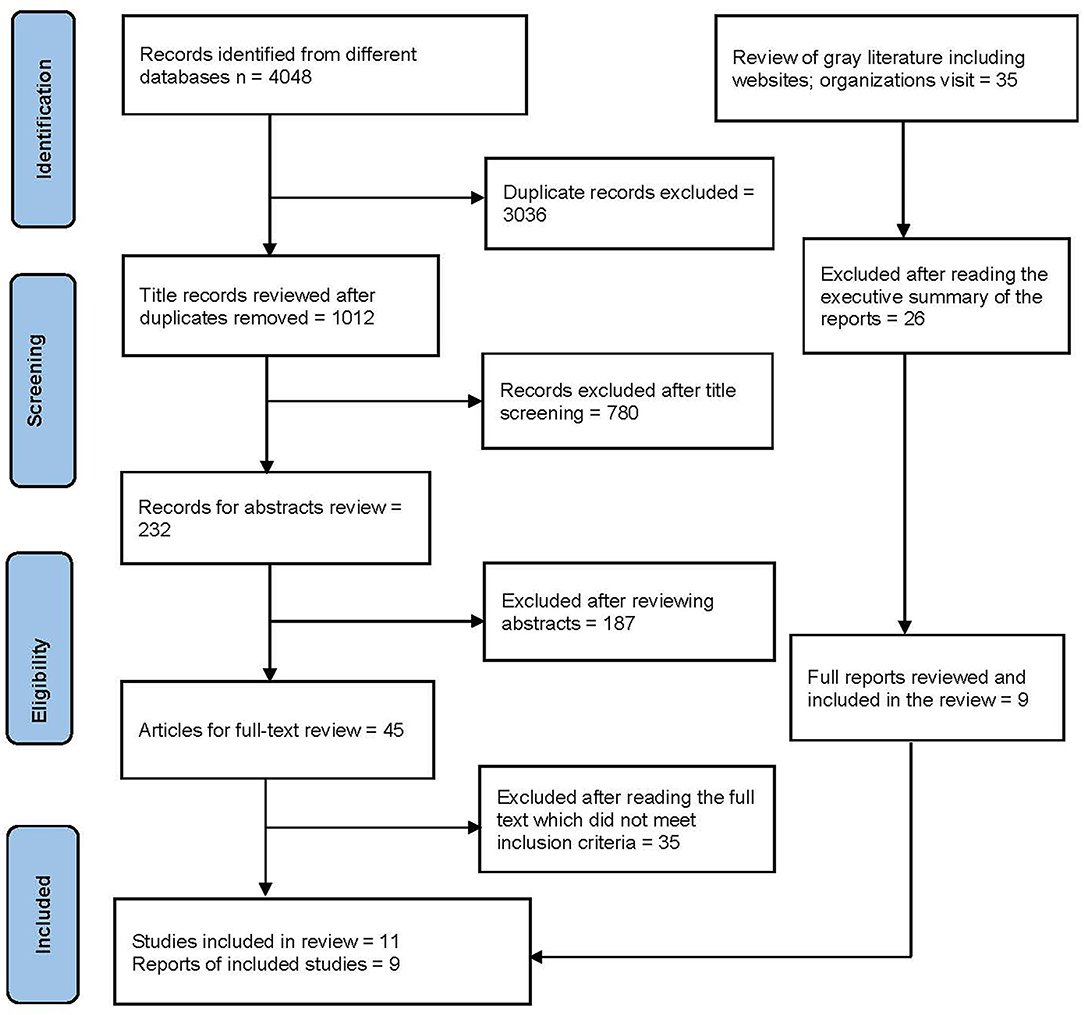
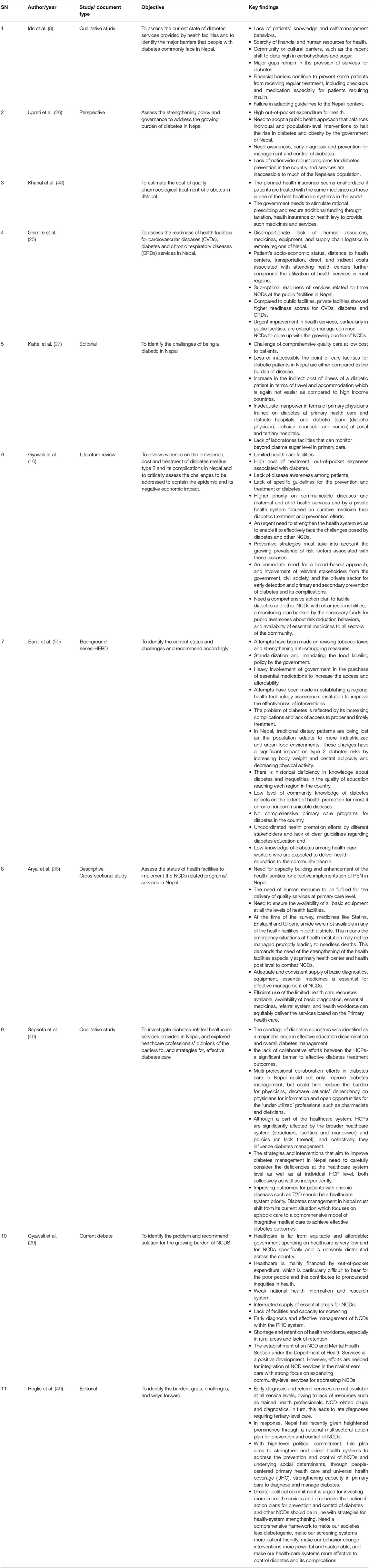
The systematic search of different databases yielded 4,048 studies. A total of 1,012 (not duplicated) publications were screened. The titles and abstracts were screened for 232 studies and after removing the publications/ reports that did not meet inclusion criteria, 45 studies met full-text review criteria. The full text records/documents were reviewed and further assessed for eligibility and finally, 11 records met the inclusion criteria and were included in this review. In addition, a total of 9 records were retrieved from the gray literature search and review of citations/reference lists. Altogether, 20 relevant studies and policy documents were included in the review (see Figure 1). We have also summarized the findings obtained from the documents review in the tables (see Tables 2, 3), the data obtained from documents review and exploratory research were triangulated, and the findings are presented in key thematic forms.
The findings from the document review and IDIs and KIIs were triangulated. Four major themes emerged that were directly relevant to the implementation process of the existing policies and guidelines for diabetes management in the peripheral health system in Nepal. The key themes identified are: (i) limited implementation of policies into practice, (ii) lack of coordination among the different level of provider, (iii) lack of human resources for health and comprehensive quality services at the primary health care level, and (iv) boundaries for the people with diabetes to access diabetes care at primary health care and engagement to promote diabetes self-management.
Implementation of Policies and Strategies Into Practice
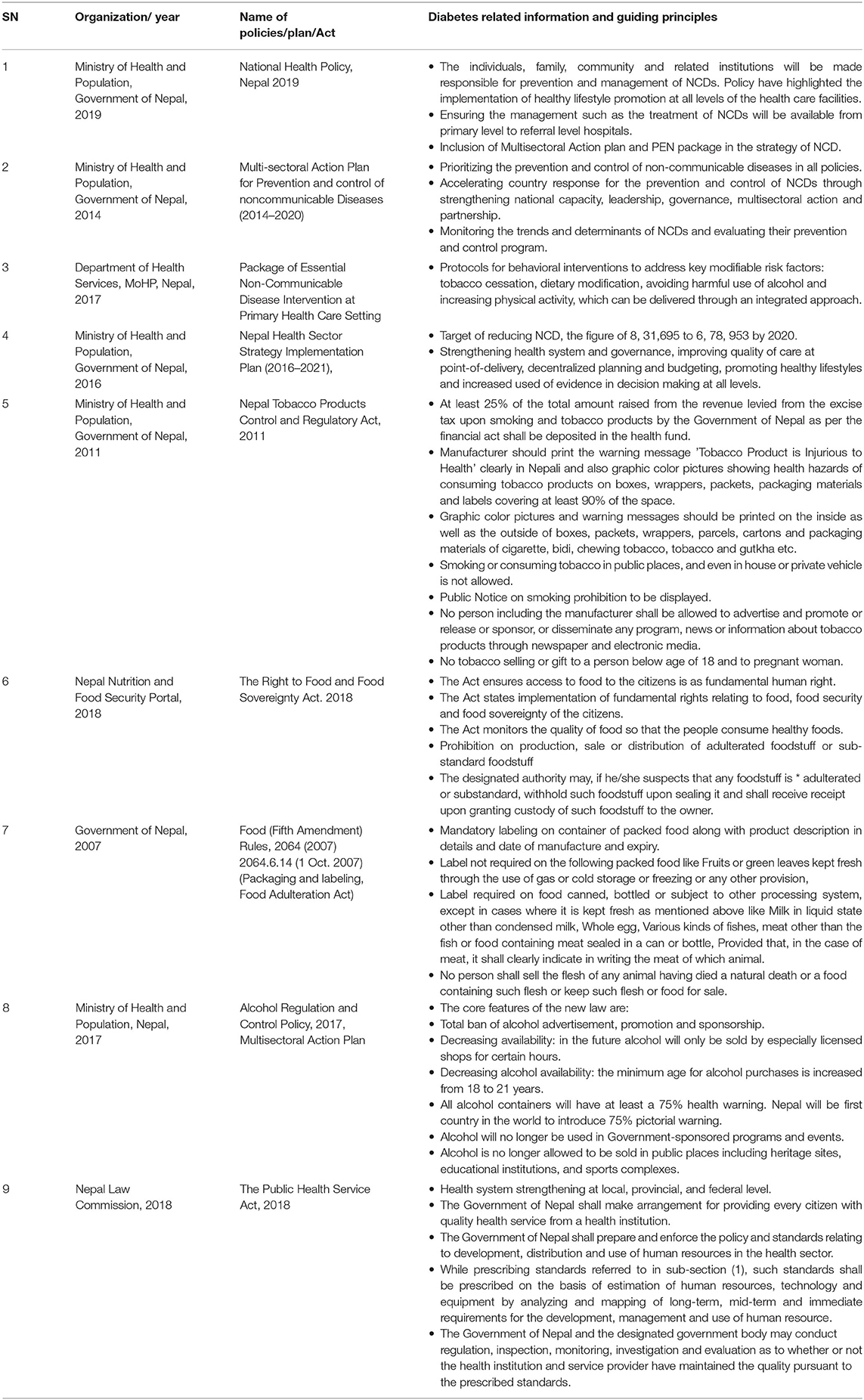
In recent years, Nepal has developed policies for NCDs prevention and control. However, to date, no specific policies exist for the diabetes prevention and control. Some of the policies related to NCDs include (i) National Health Policy 2019, (ii) Multisectoral Action Plan for the Prevention and Control of Non-communicable Diseases (2014–2020), (iii) Nepal Health Sector Strategy (NHSS) Implementation Plan 2016–21, (iv) WHO's Package of Essential NCDs (PEN) Intervention at PHC setting, (v) Nepal Tobacco Products Control and Regulatory Act, 2011 (Smoke free zones/Tobacco Advertising), (vi) Food (Fifth Amendment) Rules, 2064 (2007) 2064.6.14 (1 Oct. 2007) (Packaging and labeling, (vii) Food Adulteration Act/), (viii) Alcohol Regulation and Control Policy, 2017, and (ix) The Public Health Service Act, 2018 (see Table 2).
The qualitative findings showed that most of the community health workers reported not using any protocol or guidelines in the management of diabetes. The understanding of package of essential NCDs (PEN) protocols was limited to few health care providers who received training on the PEN package in Nuwakot and Kavrepalanchowk districts. Most interviewed health care providers mentioned that they were unaware about any guidelines for diabetes management at the primary health care level, while few expressed that they had received basic training on PEN 2–3 years back in other districts. Some of the senior peripheral health care providers mentioned that there is a lack of guidelines for engaging community health workers for diabetes care in Nepal.
One of the participants said, “We do not have such type of guidelines, protocols; however, we have heard from others or based on our own experiences, we have been providing some kind of diabetes relates services in particularly diabetes screening and distribution of basic medication” (ID: K003, CHW, Kavrepalanchowk).
Few health care providers mentioned that training for management of non-communicable disease including diabetes should focus on skill development rather than educating them on disease prevention and control and improving healthy behavior. Some participants expressed that the selection criteria for sending people for any training is not as per the guidelines for training and capacity building, rather selection of participant done solely based on nepotism and favoritism. This reflected the lack of implementation of National Health Training Center protocols. One health care provider reported- “Two to three people have training on PEN package but there is no translation of learnings from training. I would say it's crucial to strengthen primary health system while providing training to the community health workers.” (NOO4, CHW, Nuwakot).
Coordination and Collaborations Among the Different Level of Health Care Providers
Two studies suggested the need to improve the coordination among the different levels of the stakeholders (10, 25) with a greater involvement of relevant stakeholders from the government, civil society, and the private sector for early detection and management of diabetes in Nepal. This is also supported by our qualitative findings where majority of the participants reported the lack of coordination among the concerned stakeholders as a major problem for implementing any programs. Majority of the participants highlighted the need for an active engagement of all end-users from the inception to delivery and effective monitoring of the program. Some participants blamed the stakeholders for not being concerned for people's health. Additionally, few other stated political and vested interest of stakeholders as the impeding factor for coordination.
“Engaging Management committee, health management committee, political representatives, teachers, health worker, FCHVs, etc. from the inception to delivery of the program will create ownership and trust toward the program activities. But unfortunately, INGOs/NGOs just collaborate with some powerful political leader or government representative and implement the program.” (ID:N003, CHW, Nuwakot)
“Though such programs are being carried out by many INGOs/NGOs, I think it should be carried out mobilizing employee by Nepal Government. If those programs can be conducted in collaboration with the Nepal government, INGOs, and NGOs it would be more fruitful and achievable.” (ID: N004, CHW Nuwakot)
“In community level we need to coordinate with FCHVs, our management committee which we have here, likewise health management committee, representatives, teachers, health workers etc. to make sustainable programs” (ID: K007, CHW, Kavrepalanchowk)
Some health care providers from the Nuwakot district mentioned that there is a lack of monitoring and supervision of program related to NCDs. As such, one expressed- “We have the PEN program, but nobody knows what we are doing. Focal person for NCDs does not have enough idea on NCDs. Honestly speaking, I think there isn't any monitoring done specifically for NCDs.” (N004, CHW, Nuwakot).
Few participants also cited lack of sensitization of issues related to NCDs, along with lack of technical and economic resources as major problems to deal with growing problem of diabetes and other NCDs.
Primary Health Care Challenges in Delivering Comprehensive Care
All the included studies discussed the challenges that are prevalent with health care system in delivering diabetes care at primary health care level. Five out of eight studies mainly discussed the unavailability of the health resources and human resources at the primary health care system (9, 10, 25–27). Three studies reported sub-optimal readiness of public health care facilities in delivering services related to NCDs including diabetes (9, 25, 28). A literature review conducted by Gyawali et al. highlighted that public health facilities still highly prioritize communicable disease and maternal and child health services and are not well-prepared to deliver service for the people with NCDs including diabetes (10). Similarly, the study reported that the readiness of services to deliver comprehensive services in Nepal was sub-optimal because of lack of trained human resources, equipment, drugs, and standard guidelines for effective management of NCDs including diabetes (10). Likewise, an editorial paper highlighted several challenges such as, insufficient and/or inaccessible health care facilities offering diabetes services, inadequate diabetes trained manpower at primary health care and districts hospitals, inadequate team (medical office assigned for NCD, dietician, diabetes educator and nurses) at zonal and tertiary hospitals, and insufficient laboratories facilities to monitor beyond plasma sugar level in primary care in Nepal (27).
Moreover, WHO PEN program is the only nationwide robust program implemented in Nepal till date, however, it's implementation across the country is taking longer (26). Awareness, early diagnosis and prevention are the keys to diabetes management and control. Therefore, the government of Nepal has recognized a need to adopt a public health approach to halt the rise of diabetes and obesity (26). The management of diabetes in the peripheral health system is not comprehensive and are less focused on lifestyle modification, rather they are focused on providing the listed essential medicines (9).
Similarly, the findings of our study also noted the inadequate human resources for health and supplies of glucometers and strips required for screening of the diabetes cases. Likewise, higher proportion of the study participants reported the diabetes medicine, metformin, are unavailable in most of the health centers. However, few reported a limited stock of metformin in PHC level.
One health care provider said, “Metformin was supplied by province government since last year, but not now and I don't know the reason” (ID: N004, CHW, Nuwakot).
Similarly, another health care provider expressed - “We used to do glucometer testing previously but now we are out of strips.” (ID: N002, CHW, Nuwakot).
Majority of the health care providers expressed dissatisfaction with supply chain management system. Participants cited lack of co-ordination between health care coordinator and logistic division representative of district, inability of officials to forecast demand of medicines, inadequate funding and an inefficient purchasing system as the major reasons for inefficient supply chain management system. Most of the senior level health care professionals mentioned the lack of trained doctor or health care providers to manage Diabetes and other NCDs. One senior health care provider mentioned that- “We envisioned the recruitment of human resources for health, such as doctor and health assistants but we cannot do anything because of lack of resources from federal and provincial government. District health office does not have budget to tackle NCDs specifically.” (DHO2, Nuwakot).
Boundaries for the People With Diabetes to Access Diabetes Care at Primary Health Care
Three studies highlighted that people had low level of awareness on diabetes and its management (9, 10, 26). Studies included in this review showed that several challenges that impeded access to the diabetes care at the public health facility including PHC in Nepal, including the financial burden like out-of-pocket expenditures, inadequate essential drugs, lack of trust of people on government services, limited health care facilities and ineffective government-initiated health insurance system. Although primary health care is considered the backbone of health service delivery, this lacked adequate preventive and curative services for diabetes. Likewise the management of type 2 diabetes mellitus (T2DM) and its complications found to be a formidable challenge to the government owing to lack of appropriate infrastructure and financing scheme required to provide diabetes management services (10). Few health care providers also highlighted that there is lack of recognition of diabetes and major health related problems.
One said “NCDs are a major health problem globally. Lack of recognition of these problems by them (ward / local government), not realizing that it's a major problem and design programs accordingly.” (ID: N004, CHW, Nuwakot)
Similarly, barriers to engage in diabetes self-management practices included modifying the dietary habits that are deep rooted to cultural practices, unavailability of space for physical activity, lack of motivation toward lifestyle management, poor adherence to lifelong medication for diabetes and lack of family support in changing the behavior (9).
One participant expressed “The major challenge is to change people's behavior. Most of the people are aware about the consequences and knowledgeable but they don't implement in their life. The main problem is the negligence or not prioritizing diabetes as a major health problem” (ID: K002, CHW, Kavrepalanchowk).
Some participants perceived a lower trust in the medicines supplied by the government because they believed that free medicines will not be effective on disease management. Few participants also perceived poor health literacy as a major challenge for diabetes prevention and management at the primary health care (PHC) level. One said:
“Limited health literacy on diabetes among people is unaddressed issues. There is greater need of transforming the community through health literacy program. This could develop trust among people for government health facilities among those who do not feel so.” (ID:UM1, HC, Kavrepalanchowk)
Discussion
This study identified several key policies, strategies, and plans that have been formulated by the Government of Nepal and have aimed at addressing the problem of NCDs including diabetes in Nepal. The Government of Nepal has launched multisectoral Action Plan for the prevention and control of NCDs and implemented PEN package in selected districts of Nepal, there is still a lack of programs that emphasize screening, diagnosis of diabetes, and providing comprehensive self-management and care.
Given the increasing problem of NCDs including diabetes in Nepal, there has been a critical need for developing and implementing effective policies and strategies into affordable and feasible programs that can detect individuals at risk of developing diabetes, provide health services at the local level and can support people with diabetes in self-management of conditions. Examining available public health policies with regard to diabetes prevention and control is crucial, given the social and economic burden that diabetes creates for the individuals, communities and the health system as a whole. At present, Nepal has introduced a range of NCDs related policies, however they lack the specifics for diabetes prevention and control and the implementation of existing policies is weak.
Impact of some policies such as graphic warnings on tobacco packaging and alcohol products, diabetes risk factors survey, ban of alcohol advertisement and promotion and sponsorship are laudable but the implementation of policies for the prevention and management of type 2 diabetes at primary health care level is not yet well-organized. The poor implementation of policies for preventing and managing diabetes at the primary health care level have been largely reflected in recently published studies from Nepal (9, 29). The emerging evidence from Nepal during the COVID-19 pandemic have captured stories of people with diabetes who were deprived of basic primary health care services. This reflects poor implementation of different policies and programs to curb diabetes in Nepal. This argument is supported by a recent study which noted weak implementation of NCD related policies in LMICs compared to high-income countries (30). The success of the policies is determined based on the implementation process. There are many reasons for poor implementation of policies and strategies in low-income countries, including financial constraints, poor recognition of NCDs as the key priority health problem, inadequate trained human resources, and lack of guidelines and standard operating procedures, etc. (7). Therefore, the government should identify the strategies to facilitate an effective translation of the existing policies into practice. To start with, the government should engage external developmental partners, international non-governmental organizations, research and implementation organizations to put emphasis on strategies to curb growing burden of NCDs including diabetes (31). Moreover, political interest and support are essential to strengthening the implementation process of the existing NCD and diabetes related policies.
Studies have shown that delivery of diabetes care through strong PHC has resulted in lower health costs, better health outcomes, higher satisfaction of people with diabetes, fewer hospitalization rate, and greater socioeconomic equity (32–35). While the prevalence of diabetes and its impact on health and overall quality of life is high in Nepal, low institutional capacity of primary health care center, inadequate human resources for health, lack of resources/funding and priority for diabetes and other NCDs and poor intersectoral coordination are some key challenges to implementing programs for prevention and control of diabetes. Previous studies have noted lack of regular supply of medications, lack of glucometers required to screen diabetes, health education materials, and limited skills of health care providers for management of diabetes as major concerns at PHC level that impede delivery of diabetes care (7, 36, 37).
Lack of trained or poor retention of human resources for health is a pertinent issue in LMICs including Nepal, that needs to be addressed effectively in order to delivering diabetes prevention and care services in low-income settings (38, 39). These all can leave people with diabetes with no choice other than to seek medical services from a poorly regulated private sector which is generally means higher cost and is hence unaffordable for poor people (40, 41). Therefore, revitalization of primary health care is greatly required to deliver comprehensive diabetes prevention and management services along with appropriate support systems (in terms of guidelines, budget, trained human resources and logistics and supplies etc.) available at the primary care level. Also, it is crucial to establish referral services for the complicated diabetes cases from the PHC to secondary and tertiary level hospitals. Similarly, a comprehensive action plan to tackle diabetes with clear responsibilities and a monitoring plan backed by the necessary funds to support diabetes prevention and management programs at the community level is required. Further, monitoring and evaluation are vital for the quality of the care provided at the primary health care level along with strong national health information and research system in place in order to keep track of the ongoing services and patient follow up.
Previous studies have identified that importance of health literacy in improving behavioral, clinical, patient–provider communication, and other outcomes among people with diabetes (42, 43). It is obvious that people with adequate health literacy seek available health services, can effectively communicate with health care providers and manage their lifestyle required for maintaining good health. Evidence also suggests that health literacy is an important determinant of inequities in health (44). In most cases, poor health literacy is viewed as patient problem that can hinder obtaining information or communicating with health care providers. This would need further research in the case of Nepal. Therefore, diabetes prevention and control programs require comprehensive intervention strategies to tackle various issues related to prevention and care. This strategy would also help to reduce health disparities and establish people center care at primary health care center (44). Addressing the problem of diabetes across people of different strata, particularly among those with poor economic status, would need revisiting the existing health insurance policy of Nepal and improving the implementation process. The current health insurance policy in Nepal aims to address social inequity and breaking barriers to quality of care. The overall findings of the study suggest the need for developing context-specific cost-effective intervention approaches to prevention and control of NCDs including diabetes. Further, co-designing approach (45) could be adopted that will address the concerns of all stakeholders and design the people centered interventions that could be scalable to primary care level across the country.
Research Implications
The findings of this study are useful for the policy makers in Nepal to map the gaps in formulation and implementation of NCDs related policies in Nepal, particularly diabetes prevention and control at the peripheral level. The findings are also helpful to strengthen the ongoing implementation of PEN package at the peripheral level. The lack of screening and awareness at the community level implies the greater need of people centered health literacy intervention (46) required to improve the health outcomes of the people living with diabetes through comprehensive self-management program. Similarly, there is a need for continuity of care for the people with diabetes which could include primary, secondary, and tertiary preventive approaches to maintain their blood sugar level and reduce the potential complications due to uncontrolled diabetes.
The primary health care has a significant role to play for the prevention and management of NCDs (47) including diabetes at the community level; however, resources and support provided to these care services now are inadequate. Given the importance of providing NCDs and diabetes related programs at the primary care level, there is a need for revitalizing the primary health care systems that effectively integrates the NCDs and diabetes related programs within the current health care systems.
Study Strengths and Limitations
As like other studies, this study does have strengths and some limitation. The strengths include: (i) study triangulated the findings from both literature review and a qualitative study conducted with health care providers and policy makers, (ii) findings gathered add to the literature on policy translation research on diabetes, and (iii) the gaps identified in the current study might guide the decision makers to take appropriate steps for diabetes prevention and management at primary health care setting of Nepal. Our study had some key limitations. First, search of literature was done in selected databases which may not have captured all the evidence. Second, some studies may have been missed to be included because of language bias as we did not include articles or policies available in Nepali language. Thirdly, the findings from a qualitative study cannot be generalized to other study settings of Nepal as they each constitute a small number of respondents.
Conclusion
Our findings suggests that despite the formulation of a range of policies and strategies for the prevention and control of NCDs including diabetes in Nepal, there has been a poor translation of these policies into practices. Integrating NCDs including diabetes related programs within the current health care systems and revitalizing primary health care systems along with effective implementation of such programs are essential to achieving SDG-3, health, and wellbeing and ensuring universal access to health services by 2030. There is also a need for developing and implementing effective, context specific, and cost-effective intervention required for prevention and control of NCDs including diabetes in Nepal. In order to improve and strengthen implementation aspect of policies and strategies to NCDs and diabetes prevention and control in Nepal, there is a need for engaging wider stakeholders such as government, health care professionals, local community leaders, political leaders, private sectors etc.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Human research Ethics Committee of Nepal Health Research Council Nepal. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
RS, UY, AbS, GP, and LR contributed conceptualizing the study, drafting the manuscript, and finalization. RS, AbS, DM, GP, BK, HI, UY, LR, and RK contributed to data collection, processing, analyses, and results' write up. UY, PP, YH, AbS, ArS, YH, BK, RK, TS, and LR thoroughly reviewed the manuscript and contributed substantially for necessary revision. RS, UY, AbS, GP, and LR final reviewed the manuscript and prepared for submission. All authors contributed to the article and approved the submitted version.
Funding
RS, DM, and HI are regular project staff of the project funded by Japan Agency for Medical Research and Development (AMED). LR, TS, BK, AbS, ArS and RK are research investigators of the ongoing project funded by AMED Japan (Grant Number JP21jk0110020) under the Global Alliance for Chronic Disease (GACD) Call and funding mechanism.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.763784/full#supplementary-material
References
1. Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2197–223. doi: 10.1016/S0140-6736(12)61689-4
2. International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels, Belgium; International Diabetes Federation.
3. Zhou B, Lu Y, Hajifathalian K, Bentham J, Di Cesare M, Danaei G, et al. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. (2016) 387:1513–30. doi: 10.1016/S0140-6736(16)00618-8
4. World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. Geneva: World Health Organization (2013). Available online at: http://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf;jsessionid=A4B0D1B6267E645B43E2A08A28E79133?sequence=1 (accessed December 31, 2021).
5. Hills AP, Misra A, Gill JM, Byrne NM, Soares MJ, Ramachandran A, et al. Public health and health systems: implications for the prevention and management of type 2 diabetes in south Asia. Lancet Diabetes Endocrinol. (2018) 6:992–1002. doi: 10.1016/S2213-8587(18)30203-1
6. Shrestha N, Mishra SR, Ghimire S, Gyawali B, Mehata S. Burden of diabetes and prediabetes in nepal: a systematic review and meta-analysis. Diabetes Therapy. (2020) 11:1935–46. doi: 10.1007/s13300-020-00884-0
7. Rawal LB, Kharel C, Yadav UN, Kanda K, Biswas T, Vandelanotte C, et al. Community health workers for non-communicable disease prevention and control in Nepal: a qualitative study. BMJ Open. (2020) 10:e040350. doi: 10.1136/bmjopen-2020-040350
8. Ghimire S. Barriers to diet and exercise among Nepalese type 2 diabetic patients. Int Sch Res Notices. (2017) 2017:1273084. doi: 10.1155/2017/1273084
9. Ide N, LoGerfo JP, Karmacharya B. Barriers and facilitators of diabetes services in Nepal: a qualitative evaluation. Health Policy Plan. (2018) 33:474–82. doi: 10.1093/heapol/czy011
10. Gyawali B, Ferrario A, van Teijlingen E, Kallestrup P. Challenges in diabetes mellitus type 2 management in Nepal: a literature review. Glob Health Action. (2016) 9:31704. doi: 10.3402/gha.v9.31704
11. Government of Nepal. Non Communicable Diseases. Ministry of Health and Population. Available online at: https://www.mohp.gov.np/eng/index.php/ncd (accessed May 29, 2021).
12. Heller O, Somerville C, Suggs LS, Lachat S, Piper J, Aya Pastrana N, et al. The process of prioritization of non-communicable diseases in the global health policy arena. Health Policy Plan. (2019) 34:370–83. doi: 10.1093/heapol/czz043
13. Shiffman J, Smith S. Generation of political priority for global health initiatives: a framework and case study of maternal mortality. Lancet. (2007) 370:1370–9. doi: 10.1016/S0140-6736(07)61579-7
14. Shawar Y, Shiffman J, Spiegel D. Generation of political priority for global surgery: a qualitative policy analysis. Lancet Glob Health. (2015) 3:e487–95. doi: 10.1016/S2214-109X(15)00098-4
15. Shawar YR, Crane LG. Generating global political priority for urban health: the role of the urban health epistemic community. Health Policy Plan. (2017) 32:1161–73. doi: 10.1093/heapol/czx065
16. National Nutrition Policy and Strategy 2004. Nutrition Section, Child Health Division, Department of Health Services, Ministry of Health and Population. Available online at: http://dohs.gov.np/wp-content/uploads/chd/Nutrition/Nutrition_Policy_and_Strategy_2004.pdf (accessed December 31, 2021).
17. Government of Nepal. District Coordination Committee Office, Kavrepalanchowk, Nepal. Available online at: https://dcckavre.gov.np/en/ (accessed December 31, 2021).
18. Regmi S, Gautam UK. A Comparative Analysis of Micro Finances: An Economic Impact of Micro Finance upon Income Level of People in Kavrepalanchok District, Nepal: Universitetet i Agder; University of Agder (2016).
19. Government of Nepal. District Coordination Committee Office, Nuwakot, Nepal. Available online at: https://dccnuwakot.gov.np/en/brief-introduction/ (accessed December 31, 2021).
20. Sakchyam Programme, Nuwakot district, Nepal. Available online at: https://sakchyam.com.np/nuwakot-2/ (accessed December 31, 2021).
21. Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis:striving to meet the trustworthiness criteria. Int J Qual Methods. (2017) 16:1–13. doi: 10.1177/1609406917733847
22. O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. (2014) 89:1245–51. doi: 10.1097/ACM.0000000000000388
23. Shenton A. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf. (2004) 22:63–75. doi: 10.3233/EFI-2004-22201
24. Houghton C, Casey D, Shaw D, Murphy K. Rigour in qualitative case-study research. Nurse Res. (2013) 20:12–7. doi: 10.7748/nr2013.03.20.4.12.e326
25. Ghimire U, Shrestha N, Adhikari B, Mehata S, Pokharel Y, Mishra SR. Health system's readiness to provide cardiovascular, diabetes and chronic respiratory disease related services in Nepal: analysis using 2015 health facility survey. BMC Public Health. (2020) 20:1–15. doi: 10.1186/s12889-020-09279-z
26. Upreti SR, Lohani GR, Magtymova A, Dixit LP. Strengthening policy and governance to address the growing burden of diabetes in Nepal. WHO South East Asia J Public Health. (2016) 5:40–3. doi: 10.4103/2224-3151.206551
27. Kattel V, Maskey R, Lavaju P, Taparia R, Agrawal Y. Challenges of being a diabetic in Nepal. J Diabetes Endocrinol Assoc Nepal. (2018) 2:1–2. doi: 10.3126/jdean.v2i2.22352
28. Mishra SR, Khanal P, Karki DK, Kallestrup P, Enemark U. National health insurance policy in Nepal: challenges for implementation. Glob Health Action. (2015) 8:28763. doi: 10.3402/gha.v8.28763
29. Gyawali B, Khanal P, Mishra SR, van Teijlingen E, Wolf Meyrowitsch D. Building strong primary health care to tackle the growing burden of non-communicable diseases in Nepal. Glob Health Action. (2020) 13:1788262. doi: 10.1080/16549716.2020.1788262
30. Allen LN, Nicholson BD, Yeung BYT. Goiana-da-Silva F. Implementation of non-communicable disease policies: a geopolitical analysis of 151 countries. Lancet Glob Health. (2020) 8:e50–8. doi: 10.1016/S2214-109X(19)30446-2
31. Hudson B, Hunter D, Peckham S. Policy failure and the policy-implementation gap: can policy support programs help? Policy Design and Practice. (2019) 2:1–14. doi: 10.1080/25741292.2018.1540378
32. Faruqi N, Thomas L, Parker S, Harris-Roxas B, Taggart J, Spooner C, et al. Primary health care provider-focused interventions for improving outcomes for people with type 2 diabetes: a rapid review. Public Health Res Pract. (2019) 29:e29121903. doi: 10.17061/phrp29121903
33. Reichert SM, Harris SB, Tompkins JW, Belle-Brown J, Fournie M, Green M, et al. Impact of a primary healthcare quality improvement program on diabetes in Canada: evaluation of the Quality Improvement and Innovation Partnership (QIIP). BMJ Open Diabetes Res Care. (2017) 5:e000392. doi: 10.1136/bmjdrc-2017-000392
34. Flood D, Hane J, Dunn M, Brown SJ, Wagenaar BH, Rogers EA, et al. Health system interventions for adults with type 2 diabetes in low-and middle-income countries: a systematic review and meta-analysis. PLoS Med. (2020) 17:e1003434. doi: 10.1371/journal.pmed.1003434
35. van Weel C, Kidd MR. Why strengthening primary health care is essential to achieving universal health coverage. Can Med Assoc J. (2018) 190:E463. doi: 10.1503/cmaj.170784
36. Aryal BK, Daud M, Thapa A, Mahotra A, Ale Magar S, Malla CK. Assesssment of Health Facilities for Implementation of Non-communicable Disease Package. J Nepal Health Res Counc. (2018) 16:149–55. doi: 10.3126/jnhrc.v16i2.20301
37. Yadav UN, Lloyd J, Hosseinzadeh H, Baral KP, Dahal S, Bhatta N, et al. Facilitators and barriers to the self-management of COPD: a qualitative study from rural Nepal. BMJ Open. (2020) 10:e035700. doi: 10.1136/bmjopen-2019-035700
38. Karachaliou F, Simatos G, Simatou A. The challenges in the development of diabetes prevention and care models in low-income settings. Front Endocrinol. (2020) 11:518. doi: 10.3389/fendo.2020.00518
40. Sapkota S, Brien J-aE, Aslani P. Diabetes-related healthcare services in nepal—a qualitative exploration of healthcare professionals' opinions. Pharmacy. (2020) 8:131. doi: 10.3390/pharmacy8030131
41. Herman WH, Ye W, Griffin SJ, Simmons RK, Davies MJ, Khunti K, et al. Early detection and treatment of type 2 diabetes reduce cardiovascular morbidity and mortality: a simulation of the results of the anglo-danish-dutch study of intensive treatment in people with screen-detected diabetes in primary care (ADDITION-Europe). Diabetes Care. (2015) 38:1449–55. doi: 10.2337/dc14-2459
42. Stormacq C, Wosinski J, Boillat E, Van den Broucke S. Effects of health literacy interventions on health-related outcomes in socioeconomically disadvantaged adults living in the community: a systematic review. JBI Evidence Synthesis. (2020) 18:1389–469. doi: 10.11124/JBISRIR-D-18-00023
43. Marciano L, Camerini A-L, Schulz PJ. The role of health literacy in diabetes knowledge, self-care, and glycemic control: a meta-analysis. J Gen Intern Med. (2019) 34:1007–17. doi: 10.1007/s11606-019-04832-y
44. Hasnain-Wynia R, Wolf MS. Promoting health care equity: is health literacy a missing link? Health Serv Res. (2010) 45:897–903. doi: 10.1111/j.1475-6773.2010.01134.x
45. Yadav UN, Lloyd J, Baral KP, Bhatta N, Mehta S, Harris MF. Using a co-design process to develop an integrated model of care for delivering self-management intervention to multi-morbid COPD people in rural Nepal. Health Res Policy Syst. (2021) 19:17. doi: 10.1186/s12961-020-00664-z
46. Yadav UN, Lloyd J, Hosseinzadeh H, Baral KP, Bhatta N, Harris MF. Levels and determinants of health literacy and patient activation among multi-morbid COPD people in rural Nepal: findings from a cross-sectional study. PLoS ONE. (2020) 15:e0233488. doi: 10.1371/journal.pone.0233488
47. Yadav UN, Mistry SK, Ghimire S, Schneider CH, Rawal LB, Acharya SP, et al. Recognizing the roles of primary health care in addressing non-communicable diseases in low-and middle-income countries: lesson from COVID-19, implications for the future. J Glob Health. (2021) 11:03120. doi: 10.7189/jogh.11.03120
48. Khanal S, Veerman L, Nissen L, Hollingworth S. Forecasting the amount and cost of medicine to treat type 2 diabetes mellitus in Nepal using knowledge on medicine usage from a developed country. J Pharm Health Serv Res. (2018) 10:91–9. doi: 10.1111/jphs.12265
49. Roglic G, Varghese C, Thamarangsi T. Diabetes in South-East Asia: burden, gaps, challenges and ways forward. WHO South-East Asia J Public Health. (2016) 5:1–4. doi: 10.4103/2224-3151.206546
50. Baral S, Uprety S, Lamichhane B. Backgrounder series: Diabetes. Kathmandu: Health Research Social Development Forum (2016). Available online at: https://www.herd.org.np/uploads/frontend/Publications/PublicationsAttachments1/1480578900-Backgrounder%20on%20DIABETES.pdf (accessed Dec 31, 2021).
Keywords: guidelines, implementation, Nepal, policy, type 2 diabetes, prevention, management
Citation: Shrestha R, Yadav UN, Shrestha A, Paudel G, Makaju D, Poudel P, Iwashita H, Harada Y, Shrestha A, Karmacharya B, Koju R, Sugishita T and Rawal L (2022) Analyzing the Implementation of Policies and Guidelines for the Prevention and Management of Type 2 Diabetes at Primary Health Care Level in Nepal. Front. Public Health 10:763784. doi: 10.3389/fpubh.2022.763784
Received: 24 August 2021; Accepted: 07 January 2022;
Published: 09 February 2022.
Edited by:
Kingston Rajiah, Gandhi Institute of Technology and Management University, IndiaReviewed by:
Mohamed Izham Mohamed Ibrahim, Qatar University, QatarNouf Sahal Alharbi, King Saud University, Saudi Arabia
Copyright © 2022 Shrestha, Yadav, Shrestha, Paudel, Makaju, Poudel, Iwashita, Harada, Shrestha, Karmacharya, Koju, Sugishita and Rawal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lal Rawal, ZHIubGFscmF3YWwmI3gwMDA0MDtnbWFpbC5jb20=; TC5yYXdhbCYjeDAwMDQwO2NxdS5lZHUuYXU=
†These authors have contributed equally to this work and share first authorship
 Rabina Shrestha
Rabina Shrestha Uday Narayan Yadav2,3†
Uday Narayan Yadav2,3† Prakash Poudel
Prakash Poudel Hanako Iwashita
Hanako Iwashita Tomohiko Sugishita
Tomohiko Sugishita Lal Rawal
Lal Rawal