
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 04 January 2023
Sec. Public Health and Nutrition
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1059677
Background: Food and nutrition literacy (FNLIT) is a relatively new term that is used to define the knowledge, skills, and behaviors necessary to achieve a healthy diet. Improving food and nutritional literacy in children is a necessary solution to eliminate nutritional disorders in this age group. The purpose of this study was to design, implement and evaluate an intervention to improve food and nutrition literacy in children aged 10–12 years old based on an intervention mapping (IM) approach.
Methods: This experimental study was performed in three phases. Through the first phase, an intervention was developed using the (IM) approach. In the second phase, the intervention was implemented for 6 months, and in the third phase, the intervention outcomes were evaluated and compared with the control group through a randomized controlled trial among 300 participants (each control and intervention group = 150).
Results: Before the intervention, there was no significant difference between the control and intervention groups in all subscales of FNLIT. After the intervention, there was a significant difference between the control and intervention groups in all subscales of FNLIT (P < 0/001). There were no differences between the two groups in terms of the FNLIT scores at baseline (P > 0.05). However, after 6 months of intervention, a significant difference was observed between the two groups (intra-group differences) (P < 0.001). Such a difference was not identified in the control group after 6 months also the results show the impact of socioeconomic factors and parental literacy on the average score of students' FNLIT and after the intervention, a significant difference was observed between the scores of control and intervention groups in all subscales of the FNLIT (P < 0.001).
Conclusions: The school-based intervention developed and evaluated in this study provides a basis for future programs targeting the improvement of FNLIT in children, especially in poor and deprived areas such as Kurdistan province.
Clinical trial registration: Iranian Clinical Trials Registry (IRCT) Code: 32094.
According to the latest World Health Organization report, non-communicable diseases are responsible for 36 million deaths annually, close to 80% (29 million people) of which occurs in low and middle-income countries (1). The main risk factors for chronic diseases are unhealthy nutrition, inadequate physical activity, and tobacco use (2). These risk factors often develop during childhood and adolescence and become institutionalized until adulthood (3). Among the four main risk factors of non-communicable diseases (NCDs), the diet has a greater role than the combination of physical activity, smoking, and alcohol consumption (4). Nutrition and diet have a major impact on population health and are associated with premature death and disability-adjusted life years (DALYs). The many years of life lost, poor quality of life, and NCDs impose an additional economic burden on society at high costs (5). Many risk factors for cancer and obesity worldwide are somehow linked to nutrition and diet (6).
Urbanization and its related lifestyle have resulted in major changes in the quantity and quality of nutritional patterns and physical activity, especially in children and adolescents (7, 8). In many parts of the world, these age groups supply about 50% of their calories from unhealthy food sources, highly processed foods, and drinks (9). Evidence in Iran also indicates the role of high-risk dietary behaviors in the prevalence of various nutritional problems, including malnutrition and communicable diseases (10, 11).
The basic point is that most of these health problems can be prevented through regular implementation of health promotion programs, including promoting healthy behaviors and changing lifestyles from early childhood (12). Childhood and adolescence are important periods for acquiring knowledge and skills related to food and nutrition (13).
Food and nutrition literacy (FNLIT) is a relatively new and multidimensional concept that may play an important role in establishing the overall dietary framework. It comprises a combination of necessary knowledge, skills, and practices relevant to nutritional recommendations (14–16), as well as a set of social, cultural, and ethnic factors (17, 18).
Despite conclusive evidence on the link between food literacy and diet quality (18–21), food literacy/nutrition literacy research focused on children is scarce (19, 20). Attention to FNLIT is very important in elementary school children because it is the starting point for food-related behaviors and skills education (21–23) and can empower them to choose healthy foods and adopt healthy eating behaviors throughout their lives (24, 25).
In Iran, interventions in nutrition education to enhance the nutritional knowledge of different age groups indicate the importance of paying attention to nutrition education. However, all aspects of FNLIT in children have not been provided formally and executively (18, 26–28). Given the effect of long-term contact with children at an early age and the interdependence between health and learning, schools are one of the most appropriate and important settings for preventive health promotion programs. School-based interventions provide access to young children early when unhealthy eating behavior has not yet begun (29, 30). Therefore, the present study aimed to design and evaluate an intervention to improve FNLIT in Iranian Kurdish primary school children using the IM approach. Intervention mapping (IM) is a process and unique approach for developing theory and evidence-based health education programs. Different studies have been performed to solve health problems using an interventional mapping approach, including a self-care training program for type 2 diabetic patients (31), designing educational interventions to promote food and nutrition literacy in primary school children (32), designing, implementing, and evaluation of community-based and school-based multifaceted intervention to sustainably increase fruit and vegetable consumption among children (33). The implementation of IM as a roadmap for designing and planning programs to address health problems has attracted the attention of researchers and planners in recent years (34).
This experimental field trial is part of a comprehensive study with three phases of intervention development, implementation, and evaluation. The study design was based on the IM approach. First introduced in 1998 by Bartholomew et al., IM comprises six steps, as follows: (1) needs assessment, (2) creating change goals matrix, (3) theory-based operational solutions, (4) program design, (5) program acceptance and implementation, and (6) program evaluation (35). Within the three phases of the study, four sub-studies were planned, comprising the six steps of the IM approach:
Phase 1, needs assessment and the first step of the IM, consisted of three sub-studies. In sub-study 1, the FNLIT questionnaire previously designed by Doustmohammadian et al. (18) for Tehran students was adapted for the Kurd-speaking subjects. Schools in Bane city, a city in the Kurdistan province, were chosen as the study setting. In sub-study 2, through a cross-sectional study, FNLIT status in a sample of 390 elementary students (grades 4–6) was assessed using the adapted questionnaire. In sub-study 3, through a qualitative phenomenological study, barriers and facilitators, the most important and practical measures, and the most appropriate channel(s) and intervention methods to promote FNLIT in the targeted population were identified. In the second phase, using the results obtained from the first phase studies steps 2–6 of the IM were implemented, leading to the development of an intervention. In the third phase, the effect of the designed intervention programs via a randomized controlled trial on 300 elementary school students aged 10–12 years in grades 4–6 (150 controls and 150 in the intervention group) was evaluated. Based on the needs assessment and resource review results, interventions to promote food and nutrition literacy in students were conducted in three sections, namely curriculum development, intervention implementation, and intervention evaluation, respectively.
The study followed the CONSORT guideline for the design and reporting of clinical trials (S1 CONSORT Checklist), and the CONSORT flow diagram for the study is shown in Figure 1.
Participants were fourth- to sixth-graders (10–12-year-olds) selected through stratified random sampling. The sample size was calculated considering the change in the mean and standard deviation of nutritional literacy scores based on the previous studies (36) using the following equation (37):
Significance level = 0.05, Study power = 80%, Number of time repeats = 2.
Effect size: 0.179 based on the study by Appleton et al. (36). Correlation between observations = 0.5.
Based on the above calculations, the sample size in each group was calculated at 131 individuals. A total of 300 participants (150 students for intervention and 150 controls) were selected to account for possible sample loss. The inclusion criteria were students' desire to participate in research, family's desire to cooperate in the study, study in the fourth, fifth and sixth grades of elementary school, having no chronic illness, having no physical disability, Iranian citizenship, and not participating in the sub-study 2.
After the random allocation of schools to two groups of intervention and control with similar characteristics, equal numbers of girls and boys schools were assigned to the intervention and control groups. Thus, a total of 20 schools (10 as controls and 10 as interventions) were randomly selected, four from each geographical district (north, south, east, west, and downtown) of Baneh city. Before the commencement of the study, coordination with the management of the city's education department and all school administrators was achieved through a written letter and attendance at schools. All 4, 5, and 6 graders were selected in each school. Then, the benefits of participating in the study, how the program was implemented, and how long it took were explained to the school authorities, students, and parents, and the written informed consent form was completed and signed by the students and their parents.
Further explanation is provided in the intervention method section. At the beginning of the study (October 2018), data on demographics and socioeconomic status, FNLIT subscales, including the understanding of food and nutrition information (UFNI), nutritional health knowledge (NHK), functional food and nutrition literacy (FFNL), interactive food and nutrition literacy (IFNL), food choice literacy (FCL), critical food and nutrition literacy (CFNL), food label literacy (FLL) were collected from students in both intervention and control groups by a questionnaire. After 6 months of implementation of the education program (March 2019), students in both control and intervention groups completed the same questionnaire.
Due to the nature of the treatment, it was impossible to blind subjects to educational and environmental interventions. The project coordinator and research assistants were also not blinded because they were responsible for implementing the intervention.
Using the results obtained from phases 1 and 2, which included designing steps 2–6 of the IM and considering the expected changes in knowledge, skills, and behaviors of the main and sub-target groups, the educational program content was designed. The final curriculums for children, parents, and school staff are presented in Table 1.
The designed intervention included two components: 1) nutrition education and 2) environmental interventions.
The education program targeted two groups: (1) parents and school staff and (2) students (main target).
Nutrition experts conducted parent and school staff training in three curriculum-based training sessions. For each session, a school health expert was appointed as the supervisor to oversee the sessions and provide a written report to the project manager at the end of the session. Three educational worksheets were prepared for each training session. Through these assignments that were supposed to be followed over 1 month, parents were obliged to follow the instructions as requested, and then the results were reviewed at the end of each month, and feedback was given to the parents.
Student training was planned in 16 sessions according to the educational curriculum for a period of 16 weeks in the fall and winter of the academic year 2018–2019. The sessions were held by teachers and supervised by a nutrition expert in the school classrooms. Teaching/learning strategies included the followings: (1) lecture, (2) group discussions, (3) questions and answers, (4) brainstorming, (5) demo games, (6) practical work, and (7) field trip and scientific tour. One week prior to each training session, coordination was made with the teacher and school staff, and all team members were informed of any possible changes.
The environmental interventions included activities aimed at creating a healthy food environment both at home and school. The goals of home interventions included: (1) increasing students' access to healthy food and limiting unhealthy food access at home; (2) increasing students' involvement in food shopping, preparation, and cooking at home, (3) involving students in home food decisions, (4) involving students in planting vegetables at home parents. The school environment intervention targeted the socio-cultural, physical, economic, and political environment, as follows: (1) modifying the school's Socio-Cultural environment through implementing simple and healthy food competitions, food and nutrition festivals, healthy nutrition painting contests among children; (2) improving the school's physical environment through distributing healthy snacks and hygienic foodstuffs at the school canteen; (3) modifying the school's economic environment by distributing healthy school meals at an affordable price or partially free-of-charge in the canteen; and (4) improving the school's political environment by initiating a School Food and Nutrition Committee composed of teachers, school food service staff, school health personnel, and delegates from students, parents, and other stakeholders to coordinate and support promotion activities, such as: installing banners, posters, and flyers to promote FNLIT, and changing school policies regarding food and nutrition education, as well as the type and characteristics of nutritional snacks available at the school store (Table 2).
During the implementation phase, in order to refine and improve educational sessions and their final effect, teaching methods and quality of the trainers, the degree of students' participation in the discussions, the ability to understand the content, the participant's satisfaction with the number, time and place of the training sessions, innovation in the content and among students, parents, and school staff were assessed by a checklist. Study participants were asked to indicate their final evaluation and satisfaction regarding the school and home environment in terms of healthy eating and nutrition before and after the program using a checklist.
The main outcome measure of this intervention study was students' FNLIT scores. Using the FNLIT questionnaire, students' scores before and after intervention regarding different subscales, including understanding of food and nutrition information, nutritional health knowledge, functional food and nutrition literacy, interactive food and nutrition literacy, food choice literacy, critical food and nutrition literacy, food label literacy and total food and nutrition literacy were compared.
The normality of the data was evaluated by the Kolmogorov-Smirnov test. Since the data distribution in both control and intervention groups was not normal, we used the Wilcoxon, Man-Whitney U, and Kruskal-Wallis H statistical tests for data analysis. In order to compare the FNLIT subscales before and after the intervention within and between groups, Wilcoxon and Mann-Whitney U tests were used, respectively. Wilcoxon and Mann-Whitney U tests were used to determine the relationship between FNLIT status with demographic variables in dichotomous variables such as gender before and after the intervention within and between groups. Wilcoxon and Kruskal-Wallis H tests were used in multi-state variables such as the number of family members before and after the intervention within and between groups.
The demographic and social characteristics of the participants are shown in Table 3. There were no differences between the two groups regarding the FNLIT scores at baseline (P > 0.05). However, after 6 months of intervention, a significant difference was observed between the two groups (Intra-group differences) (P < 0.001). Such a difference was not identified in the control group after 6 months.
Since more than 98% of the participants were Kurds and spoke Kurdish, ethnicity and language were excluded from the list of confounding variables for FNLIT in the analysis. Age of half of the parents was 44–35 years (control = 52% and intervention = 47.4%). Most participants were the first children in the family (control = 35.4% and intervention = 45.2%). The four-person families had the highest number in both groups (control = 46.8% and intervention = 43.4%). Moreover, the parental education level of most participants was at the elementary level, and based on the results obtained from the Kruskal Wallis test listed in Table 4, it shows the impact of socioeconomic factors and parental literacy on the average score of students' food and nutrition literacy.
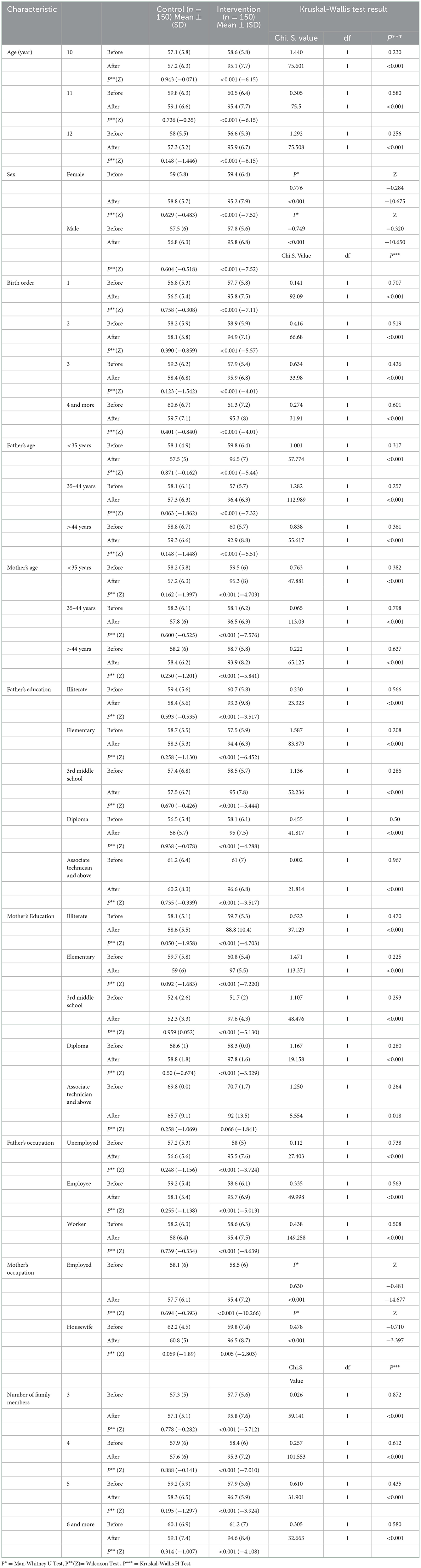
Table 4. Comparison of FNLIT scores based on the demographic and social characteristics in both groups before and after the intervention.
The number of subjects studied in both control and intervention groups was equal and they were identical in terms of age, gender, and educational levels in order to eliminate the confounding effect. Based on the results, the birth rank of one has the highest frequency in both control (35.3%) and intervention (45.3%) groups. Family size of four in both control (46.7%) and intervention (43.3%) groups were more frequent than others. The parents' age of most of the participants in both the control and intervention groups was between 35 and 44 years. The parent's education of most of the participants in both the control and intervention groups was the elementary level.
In both the control and intervention groups, the fathers of the study subject were mostly workers, and the mothers were housewives. In both the control and intervention groups, the breadwinner of the family were their father. Most of the participants in the study in both groups did not have support resources. In terms of housing ownership status, most of the study participants in both the control and intervention groups stated that they owned their housing.
At baseline, the FNLIT scores were not significantly different between the control and intervention groups (58.6 in the intervention and 58.3 in the control groups) (P = 0.75). However, after the intervention, a significant difference was observed between the scores of control and intervention groups in all subscales of the FNLIT (P < 0.001) (inter-group difference). In the intervention group, the highest and the lowest scores were related to the “food choice literacy (FCL)” (99.1) and “food label literacy (FLL)” (86.3) subscales, respectively.
After the intervention, the total FNLIT score was 57.8 in the control group compared to 95.5 in the intervention group (P < 0.001). The mean score of FNLIT in the control group before and after the intervention was not significantly different in all subscales, except for the “FLL” subscale (no intra-group difference), which significantly decreased in the control group (P = 0.009) (Table 5).
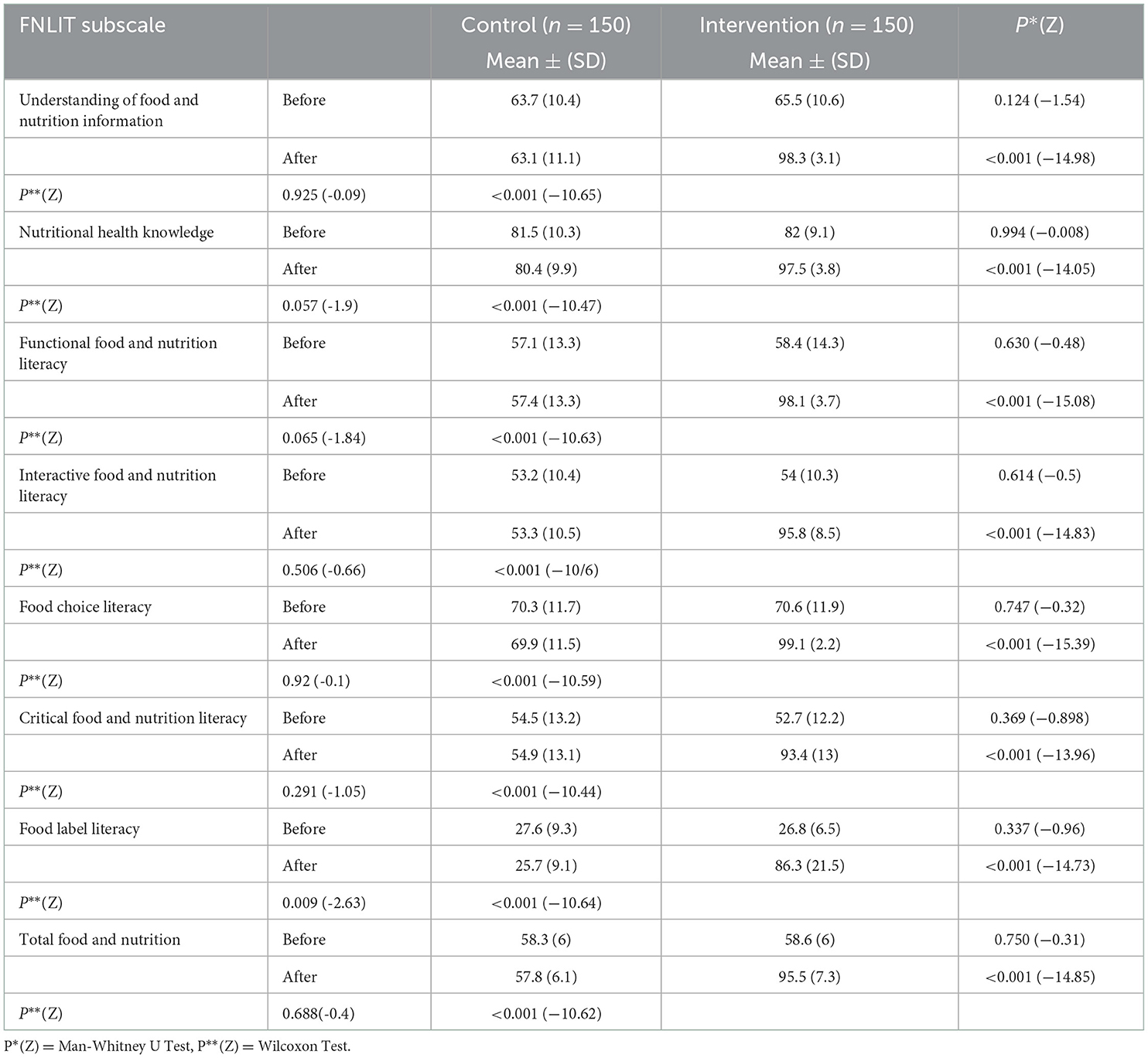
Table 5. Mean and standard deviation scores of FNLIT subscales in both control and intervention groups.
Based on the findings, the intervention designed and implemented in elementary schools in Baneh resulted in a significant improvement in total food and nutrition literacy (FNLIT) score and almost all its subscales in the intervention group compared to the controls. The FNLIT scores in both groups were moderate or low in more subscales before the intervention, except for the two subscales of the cognitive domain: understanding of food and nutrition information and nutritional health knowledge. The scores of both groups were moderate to low in all other subscales, especially in interactive food and nutrition literacy and food label literacy subscales. In the intervention group, the highest and the lowest scores were related to the “food choice literacy” and “food label literacy” subscales, respectively. These results are consistent with those reported by Doustumohammadian et al. in Tehran (19), indicating moderate literacy scores in the cognitive domain but low scores in almost all skill subscales. Also, analysis of the content of primary school textbooks in Iran has shown that there is more emphasis on cognitive aspects of food and nutrition, with little emphasis on developing practical food and nutrition skills (38, 39). Similar results have been reported in other studies, and this finding reemphasizes the need to reform educational approaches to focus more on hands-on practice experiences, specifically when it comes to everyday life skills (40–42).
The present study indicates a considerable gap between FNLIT in the cognitive and skill domains in children aged 10–12 years. These findings reemphasize the need to reform educational approaches to focus more on hands-on practice experiences, specifically when it comes to everyday life skills (43–45). A comprehensive educational program should provide strategies to improve learners' knowledge, as well as skills needed to develop and practice intended behaviors, including healthy nutrition behaviors (39). Combining food and nutrition literacy encompasses a broad range of skills and abilities considered in food literacy (skill in food choice and preparation), as well as skills in nutrition literacy, such as how to access sound nutritional information and interaction and communication skills with others (46). Such skills can complement food skills and may improve the total impact. Therefore, the present study combines and utilizes both aspects of food literacy and nutrition literacy to cover the range of issues that needs to be addressed by both. Also, special attention was given to the community ethnic culture (47). Recent studies consider FNLIT rather than a one-dimensional view as an integrated structure encompassing various socioeconomic and ecological dimensions (43, 46, 48). Beatrice Velpini and others obtained almost heterogeneous results that showed different spectra. The effective types of food and nutrition literacy interventions included the following characteristics: technology components, involvement of different methods, time period of more than 1 month, and face-to-face meetings (44). Furthermore, West et al., in a before-and-after study that investigated the value of a 6-week program called OzHarvest NEST (Education and training of nutrition skills) in promoting food security and nutritional literacy, concluded that achieving food security requires multifaceted features and upstream determinants (45).
Using the IM approach was a strength of the present study. The advantage of using the intervention mapping approach has been demonstrated in various studies. A literature review suggests that the intervention mapping approach, with emphasis on evidence and theory, provides an appropriate conceptual framework for guiding the content and strategies used to design health promotion interventions, and interventions designed using this framework positively affect health outcomes. Krolner et al. (33), conducted a study aimed at designing, implementing, and evaluating a community-based and school-based multifaceted intervention to sustainably increase fruit and vegetable intake among 13-year-olds (seventh grade). This study used an interventional approach to guide the intervention design. The results showed that the approach taken had provided insights into effective strategies for increasing fruit and vegetable intake among adolescents. The systematic and theory-based approach used in this study can guide the design of process evaluations in future interventional studies and practices (33). Other studies that used IM to design and implement nutrition interventions have reported positive effects on improving short-term outcomes (22, 31). Based on such evidence, the present study applied the steps of the intervention mapping approach to design, implement and evaluate the intervention (17, 22, 31, 32).
In Iran, school food environments do not usually support students' healthy food choices. Often school staff and peers, as students' main role models, do not have appropriate eating patterns most of the time, and school stores generally do not adhere to healthy nutrition policies (49, 50). Therefore, it is necessary not only to reevaluate curriculums regarding FNLIT but also to reemphasize healthy food environment policies in Iranian schools. This approach will provide a supportive environment to back up what is being learned in the classroom.
Children have a strong interest in food and nutrition information and learning and practicing food and nutrition skills, and they usually welcome happy, varied, inexperienced, and multifaceted intervention programs, and they consider the school a good place to start these programs.
Based on the evidence, multi-level and multi-component interventions have often been successful (51–53). Several intervention studies in Iranian schools have previously aimed at teaching healthy eating topics (26–28); however, this is the first attempt to promote FNLIT in Iranian children.
Although this study presents new findings on promoting FNLIT in primary children, it also has some limitations. The most important of these limitations are the following. First, the inconsistency of some unhealthy food advertising on national media with the nature of the study curriculum, that the effect of unhealthy food advertisements on ongoing and sustained training, group discussions, and criticism of unhealthy food advertising in the national media counteracted the target group.
Second, the lack of inter-sectoral cooperation between the Ministry of Health and the Ministry of Education to provide children with proper education on healthy nutrition and promote their food and nutrition literacy has exacerbated the dilemma and should be addressed at the national level by health policymakers. Third, children usually prefer unhealthy foods to natural and healthy ones because of their flavors/taste. Many children know healthy foods and may have access to them but still choose to eat unhealthy ones. In order to change this, the issue must be addressed in a multifaceted and inclusive way, and all the different sections involved should take part in resolving it. Finally, the generalizability of the results was limited to Iranian primary school students in the Baneh region in Kurdistan.
The results of the present study showed that the educational interventions designed and implemented could effectively promote FNLIT at the elementary school level, even in a deprived community, in terms of educational and nutrition facilities. This may indicate the value and importance of teamwork as well as active and practical classroom activities. Also, the active participation of the participants and systematic, ecologically-, fact-based planning of the intervention may have affected its results. Due to the achievements of the study and as a result of advocacy made by the schools' staff, it was approved by the Health Committee of the general director of education in Baneh to include the intervention in the curriculum of all elementary schools for the coming academic year.
This FNLIT promotion study, using the intervention mapping approach, involved students, parents, and school personnel and utilized an ecological perspective. We designed the intervention based on indigenous culture and utilized the native potentials and capabilities of the local community. This should be emphasized in future interventions to promote children's food and nutrition literacy. The extensive use of national and social media is also suggested to cover a large group of people.
The need to include food and nutrition literacy, including its analytical, interactive, and functional aspects, in the current school curricula is highly emphasized.
This is part of a Mixed Methods Study for a Ph.D. thesis of the first investigator (MA) at the Department of Health Education and Promotion, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by School of Public Health and Allied Medical Sciences, Tehran University of Medical Sciences. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
ES and NO were joint supervisors of the thesis. AR and AD were the study advisors. All authors contributed to all aspects of the investigation. All authors read and approved the final version.
This research was funded by the Tehran University of Medical Sciences as a Ph.D. student dissertation (Dissertation Code: 9511108004).
The authors would like to thank the participating schools, students, their parents, teachers, school healthcare providers, and the research staff who participated in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1059677/full#supplementary-material
FNLIT, Food and Nutrition Literacy; IM, Intervention Mapping; NCDs, Non-Communicable Diseases.
1. Organization WH, Unit WHOMoSA. Global Status Report on Alcohol and Health, 2014. Geneva: World Health Organization (2014).
2. O'Grady M, Capretta J. Health-care cost projections for diabetes and other chronic diseases: the current context and potential enhancements. Partnership Fight Chronic Dis. (2009) 15. Available online at: https://www.silverbook.org/reference/health-care-cost-projections-for-diabetes-and-other-chronic-diseases-the-current-context-and-potential-enhancements/
3. Nugent R, Bertram MY, Jan S, Niessen LW, Sassi F, Jamison DT, et al. Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. Lancet. (2018) 391:2029–35. doi: 10.1016/S0140-6736(18)30667-6
4. Hyseni L, Atkinson M, Bromley H, Orton L, Lloyd-Williams F, McGill R, et al. The effects of policy actions to improve population dietary patterns and prevent diet-related non-communicable diseases: scoping review. Eur J Clin Nutr. (2017) 71:694. doi: 10.1038/ejcn.2016.234
5. Fernandez MA. Food Literacy and Healthy Diets of Canadian parents: Associations and Evaluation of the Eat Well Campaign. Ph.D. Thesis, Université Laval, Québec, QC (2019).
6. Research WCRFAIfC. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. Continuous Update Project Expert Report (2018).
7. Popkin BM, Gordon-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes. (2004) 28:S2. doi: 10.1038/sj.ijo.0802804
8. Ghassemi H, Harrison G, Mohammad K. An accelerated nutrition transition in Iran. Public Health Nutr. (2002) 5:149–55. doi: 10.1079/PHN2001287
9. Rehm C, Drewnowski A. Trends in consumption of solid fats, added sugars, sodium, sugar-sweetened beverages, and fruit from fast food restaurants and by fast food restaurant type among US children, 2003–2010. Nutrients. (2016) 8:804. doi: 10.3390/nu8120804
10. Kelishadi R, Pour MH, Zadegan NS, Kahbazi M, Sadry G, Amani A, et al. Dietary fat intake and lipid profiles of Iranian adolescents: Isfahan Healthy Heart Program-heart health promotion from childhood. Prev Med. (2004) 39:760–6. doi: 10.1016/j.ypmed.2004.02.047
11. Azadbakht L, Esmaillzadeh A. Macro and micro-nutrients intake, food groups consumption and dietary habits among female students in Isfahan University of Medical Sciences. Iran Red Crescent Med J. (2012) 14:204.
12. Abel-Smith B. An Introduction to Health: Policy, Planning and Financing. London: Routledge (2018). doi: 10.4324/9781315843421
13. Shin K-H, Lee Y, Cho W. Survey on foodservice satisfaction and dietary education needs for improvement of school foodservice in middle school students in Seoul. Korean J Commun Nutr. (2017) 22:127–35. doi: 10.5720/kjcn.2017.22.2.127
14. Truman E, Raine K, Mrklas K, Prowse R, Den Hoed RC, Watson-Jarvis K, et al. Promoting children's health: toward a consensus statement on food literacy. Can J Public Health. (2017) 108:e211–e3. doi: 10.17269/CJPH.108.5909
15. Amin SA, Lehnerd M, Cash SB, Economos CD, Sacheck JM. Development of a tool for food literacy assessment in children (TFLAC). J Nutr Educ Behav. (2019) 51:364–9. doi: 10.1016/j.jneb.2018.12.006
16. Doustmohammadian A, Omidvar N, Keshavarz-Mohammadi N, Eini-Zinab H, Amini M, Abdollahi M. Development of a conceptual framework of food and nutrition literacy in children. BMC Nutr. (2022) 8:1–11. doi: 10.1186/s40795-022-00590-z
17. Cullerton K, Vidgen HA, Gallegos D. A Review of Food Literacy Interventions Targeting Disadvantaged Young People. QUT ePrints: Queensland (2012).
18. Doustmohammadian A, Omidvar N, Keshavarz-Mohammadi N, Abdollahi M, Amini M, Eini-Zinab H. Developing and validating a scale to measure Food and Nutrition Literacy (FNLIT) in elementary school children in Iran. PLoS ONE. (2017) 12:e0179196. doi: 10.1371/journal.pone.0179196
19. Doustmohammadian A, Keshavarz Mohammadi N, Omidvar N, Amini M, Abdollahi M, Eini-Zinab H, et al. Food and nutrition literacy (FNLIT) and its predictors in primary schoolchildren in Iran. Health Promot Int. (2018) 34:1002–13. doi: 10.1037/t65724-000
20. O'Sullivan T. Measuring Food Literacy in 9 and 10 Year Old New Zealand Children: Questionnaire Development, Validity and Reliability. Otago: University of Otago (2015).
22. Mollborn S, Lawrence E. Family, peer, and school influences on children's developing health lifestyles. J Health Soc Behav. (2018) 59:133–50. doi: 10.1177/0022146517750637
23. Doustmohammadian A, Omidvar N, Keshavarz-Mohammadi N, Eini-Zinab H, Amini M, Abdollahi M. The association and mediation role of Food and Nutrition Literacy (FNLIT) with eating behaviors, academic achievement and overweight in 10-12 years old students: a structural equation modeling. Nutr J. (2022) 21:1–16. doi: 10.1186/s12937-022-00796-8
24. Velardo S. The nuances of health literacy, nutrition literacy, and food literacy. J Nutr Educ Behav. (2015) 47:385–9.e1. doi: 10.1016/j.jneb.2015.04.328
25. Hayes-Conroy A. Doing Nutrition Differently: Critical Approaches to Diet and Dietary Intervention. London: Routledge (2016). doi: 10.4324/9781315577913
26. Hosseini M, Shojaeizadeh D, Chaleshgar M, Pishva H. A study of educational intervention on knowledge, attitude, practice about iron deficiency anemia in female adolescent students. J Gorgan Univ Med Sci. (2006) 8:37–42.
27. Hamayeli Mehrabani H, Mirmiranl P, Alaiin F, Azizi F. Changes in nutritional knowledge, attitude, and practices of adolescents in district 13 of Tehran after 4 years of education. Iranian J Endocrinol Metab. (2009) 11:235–43.
28. Mehrabani HH, Mirimiran P, Alaiin F, Azizi F. Changes in nutritional knowledge, attitude, and practices of adolescents in district 13 of Tehran after 4 years of education. Iranian J Endocrinol Metab. (2009) 11:235–43.
29. De Bourdeaudhuij I, Van Cauwenberghe E, Spittaels H, Oppert JM, Rostami C, Brug J, et al. School-based interventions promoting both physical activity and healthy eating in Europe: a systematic review within the HOPE project. Obesity Rev. (2011) 12:205–16. doi: 10.1111/j.1467-789X.2009.00711.x
30. Control CfD, Prevention. School health guidelines to promote healthy eating and physical activity. MMWR Recommend Rep. (2011) 60(RR-5):1.
31. Shakibazadeh E, Bartholomew LK, Rashidian A, Larijani B. Persian diabetes self-management education (PDSME) program: evaluation of effectiveness in Iran. Health Promot Int. (2015) 31:623–34. doi: 10.1093/heapro/dav006
32. Ahmadpour M, Omidvar N, Doustmohammadian A, Rahimiforoushani A, Shakibazadeh E. Children food and nutrition literacy—a new challenge in daily health and life, the new solution: using intervention mapping model through a mixed methods protocol. J Med Life. (2020) 13:175. doi: 10.25122/jml-2019-0025
33. Krølner R, Jørgensen TS, Aarestrup AK, Christiansen AH, Christensen AM, Due P. The Boost study: design of a school-and community-based randomised trial to promote fruit and vegetable consumption among teenagers. BMC Public Health. (2012) 12:191. doi: 10.1186/1471-2458-12-191
34. Eldredge LKB, Markham CM, Ruiter RA, Fernández ME, Kok G, Parcel GS. Planning Health Promotion Programs: An Intervention Mapping Approach. New York, NY: Wiley (2016).
35. Bartholomew LK, Parcel GS, Kok G. Intervention mapping: a process for developing theory and evidence-based health education programs. Health Educ Behav. (1998) 25:545–63. doi: 10.1177/109019819802500502
36. Appleton AA. Promoting Health Literacy Through the School Nutrition Environment. Iowa State University (2010).
37. Diggle P, Diggle PJ, Heagerty P, Liang K-Y, Heagerty PJ, Zeger S. Analysis of Longitudinal Data. Oxford: Oxford University Press (2002).
38. Sadegholvad S, Yeatman H, Omidvar N, Parrish A-M, Worsley A. Essential nutrition and food systems components for school curricula: views from experts in Iran. Iran J Public Health. (2017) 46:938. doi: 10.4103/2008-7802.193094
39. Brener ND, Demissie Z, McManus T, Shanklin SL, Queen B, Kann L. School Health Profiles 2016: Characteristics of Health Programs Among Secondary Schools (2017). Available online at: https://www.cdc.gov/healthyyouth/data/profiles/pdf/2016/2016_Profiles_Report.pdf (accessed December 11, 2022).
40. Jung T, Huang J, Eagan L, Oldenburg D. Influence of school-based nutrition education program on healthy eating literacy and healthy food choice among primary school children. Int J Health Promot Educ. (2019) 57:67–81. doi: 10.1080/14635240.2018.1552177
41. Bedoyan J, Jadhav A, Melanson K, Larson S, Greene G. P14 increasing critical nutrition literacy through a college-level, introductory nutrition course. J Nutr Educ Behav. (2019) 51:S38–S9. doi: 10.1016/j.jneb.2019.05.390
42. Tabacchi G, Battaglia G, Alesi M, Paoli A, Palma A, Bellafiore M. Food literacy predictors and associations with physical and emergent literacy in pre-schoolers: results from the Training-to-Health Project. Public Health Nutr. (2019) 2019:1–10. doi: 10.1017/S1368980019002404
43. Perry EA, Thomas H, Samra HR, Edmonstone S, Davidson L, Faulkner A, et al. Identifying attributes of food literacy: a scoping review. Public Health Nutr. (2017) 20:2406–15. doi: 10.1017/S1368980017001276
44. Velpini B, Vaccaro G, Vettori V, Lorini C, Bonaccorsi G. What is the impact of nutrition literacy interventions on children's food habits and nutrition security? A scoping review of the literature. Int J Environ Res Public Health. (2022) 19:3839. doi: 10.3390/ijerph19073839
45. West EG, Lindberg R, Ball K, McNaughton SA. The role of a food literacy intervention in promoting food security and food literacy-OzHarvest's NEST Program. Nutrients. (2020) 12:2197. doi: 10.3390/nu12082197
46. Krause C, Sommerhalder K, Beer-Borst S, Abel T. Just a subtle difference? Findings from a systematic review on definitions of nutrition literacy and food literacy. Health Promotion Int. (2016) 33:378–89. doi: 10.1093/heapro/daw084
47. Vidgen HA, Gallegos D. Defining food literacy and its components. Appetite. (2014) 76:50–9. doi: 10.1016/j.appet.2014.01.010
48. Cullen T, Hatch J, Martin W, Higgins JW, Sheppard R. Food literacy: definition and framework for action. Can J Dietetic Practice Res. (2015) 76:140–5. doi: 10.3148/cjdpr-2015-010
49. Majdabadi HA, Montazeri A, Shojaeizadeh D, Nedjat S, Farahani FK, Djazayeri A, et al. Parents' and stakeholders' perspectives on strategies to reduce fast food consumption among Iranian adolescents: a qualitative study. Iranian Red Crescent Med J. (2017) 19:e26614. doi: 10.5812/ircmj.26614
50. Esfarjani F, Khalafi M, Mohammadi F, Mansour A, Roustaee R, Zamani-Nour N, et al. Family-based intervention for controlling childhood obesity: an experience among Iranian children. Int J Prev Med. (2013) 4:358.
51. Brooks N, Begley A. Adolescent food literacy programmes: a review of the literature. Nutr Dietetics. (2014) 71:158–71. doi: 10.1111/1747-0080.12096
52. Johnston CA, Tyler C, McFarlin BK, Poston WS, Haddock CK, Reeves R, et al. Weight loss in overweight Mexican American children: a randomized, controlled trial. Pediatrics. (2007) 120:e1450–e7. doi: 10.1542/peds.2006-3321
Keywords: intervention, food and nutrition literacy, Iran, Kurdish, primary children, intervention mapping
Citation: Ahmadpour M, Omidvar N, Shakibazadeh E, Doustmohammadian A and Rahimiforoushani A (2023) Development and evaluation of an intervention to improve food and nutrition literacy among Iranian Kurdish primary school children: An application of intervention mapping approach. Front. Public Health 10:1059677. doi: 10.3389/fpubh.2022.1059677
Received: 01 October 2022; Accepted: 12 December 2022;
Published: 04 January 2023.
Edited by:
Maria Luisa Garmendia, University of Chile, ChileReviewed by:
Joanne Karam, University of Balamand, LebanonCopyright © 2023 Ahmadpour, Omidvar, Shakibazadeh, Doustmohammadian and Rahimiforoushani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nasrin Omidvar,  b21pZHZhci5uYXNyaW5AZ21haWwuY29t
b21pZHZhci5uYXNyaW5AZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.