
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 04 January 2023
Sec. Public Health Policy
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1055898
This article is part of the Research TopicGlobal Surgery: The Next Frontier in Global Public HealthView all 15 articles
Background: One of the primary barriers to reducing maternal morbidity and mortality is disrespect and abuse during childbirth in biomedical facilities. Despite the serious consequences of disrespect and abuse during childbirth, there is no evidence of the prevalence of respectful maternity care in Southwest Ethiopia. This study aimed to assess the prevalence of respectful maternity care and associated factors among mothers who gave birth in three hospitals in Southwest Ethiopia.
Methods: An institution-based cross-sectional study was conducted among 348 mothers who gave birth in three hospitals in Southwest Ethiopia. Bivariable and multivariable binary logistic regression were used to identify the factors of respectful maternity care.
Results: In this study, 348 mothers with their newborns were included, making a response rate of 100%. The overall prevalence of respectful maternity care was 81.2%. Maternal age [AOR = 2.54; 95% CI (1.01–6.43)]; maternal occupation [AOR = 5.23; 95% CI (1.15–23.72)]; antenatal care follows-up [AOR = 2.86; 95% CI (1.01–8.20)]; and discussions with the provider about the place of delivery during antenatal care follow up [AOR = 5.58; 95% CI: (2.12–14.70)] were found to be the most significant components of respectful maternity care.
Conclusion: The provision of respectful maternity care was high, but there are complaints of disrespect and abuse still present in three hospitals in Southwest Ethiopia. Maternal age, maternal occupation, antenatal follow up, and discussion with the provider about the place of delivery during antenatal follow-up were associated with respectful maternity care. Thus, improving antenatal care service utilization and discussions with health care providers about the place of delivery during antenatal care follow-up should be focused on.
Pregnancy, labor, and delivery are crucial events in the lives of women and their families in all countries (1). The disrespect and abuse perpetrated on women in biomedical health facilities during childbirth is a global problem (2, 3). Respectful maternity care (RMC) is a person-centered strategy for maternity service that encourages procedures that reflect women's preferences and newborns' needs. It is based on ethical principles and respect for human rights (4, 5). We define disrespect and abuse (D&A) as any harsh care or thoughtless conduct directed toward a woman during childbirth (6).
Disrespectful maternity care has both direct and indirect impacts on women's birth outcomes, patient satisfaction, and future delivery plans (3, 7, 8).
The Ethiopian Minister of Health has launched a new compassionate, respectful maternity care (CRC) program based on WHO principles during childbirth and has given in-service training to all maternity care providers on CRC (9, 10). In addition, the establishment of maternal waiting rooms in biomedical health facilities, free labor and delivery service and transportation, pregnant women's conferences, and a media awareness campaign have all been attempted to promote SBA delivery (11). Despite these actions, 72% of Ethiopian women deliver their children at home, with a range of indicators depending on geography, economic status, and education levels (12). In addition, maternal and neonatal mortality rates remain at 412 per 100,000 and 29 per 1,000 live births, respectively (13). Furthermore, disrespectful maternity care at biomedical healthcare facilities is one of the key reasons for home delivery (14).
Despite RMC being the best and the key strategy to increase institutional delivery and reduce maternal and newborn mortality, there is no evidence of the prevalence and risk factors of RMC in the study area. Thus, this study aimed to assess the RMC and associated factors among women who gave birth in three public hospitals in Southwest Ethiopia.
The study was conducted at Mizan-Tepi University Teaching Hospital (MTUTH), Gebretsadik-Shawe General Hospital (GSGH), and Tepi General Hospital (TGH) in Southwest Ethiopia. Those hospitals are the only hospitals in the Southwest Ethiopia regional state and are located in Benchi-Sheko Zone, Kefa Zone, and Sheka Zone, respectively. The hospitals provide emergency obstetric care, maternal and neonatal health infrastructures, and a full complement of skilled health professionals, including obstetricians, anesthesiologists, radiologists, neonatologists, nurses, and midwives.
A facility-based cross-sectional study was conducted in these hospitals from 1 January to 30 February 2021.
The study population included women who gave birth in three hospitals in Southwest Ethiopia, while the source population included mothers who gave birth in three hospitals in Southwest Ethiopia during the study period.
Mothers in the postnatal care room during the study period were included in the study, whereas mothers who were critically ill and unable to communicate were excluded.
The sample size was calculated using the single population proportion formula based on the assumptions below. The 95% confidence interval (CI), (Z/2 = 1.96), marginal error (d) = 0.05, and proportion of RMC p = 71% are based on a study conducted in Jimma, Ethiopia. As a result, 348 mothers were included in the study after allowing for a 10% non-response rate (15).
The study was conducted simultaneously at MTUTH, GSGH, and TGH. A proportional sample allocation was applied to each hospital based on the number of deliveries performed in the 2 months before data collection. A total of 348 mothers (139, 113, and 96 from MTUTH, GSGH, and TPGH, respectively) participated in the study. For each hospital, the study participants were identified by systematic random sampling technique from the postnatal registration book. Participants were recruited within 12 h of delivery in the postnatal room.
An accredited health professional such as a midwife, doctor, or nurse who has been educated and trained to proficiency in the skills needed to manage normal pregnancy, childbirth, and the immediate postnatal period, and in the identification, management, and referral of complications in women and newborns (16).
The mothers were interviewed and their medical records were reviewed using an Amharic version interviewer-administered questionnaire and an English version checklist. Previous literature was used to construct the structured questionnaire and extraction checklist (17).
For the prevalence of RMC, 15 interviewer-administered questionnaires that contain dichotomous (yes/no) questions were used. It was determined that a mother was receiving RMC if she answered yes to all 15 questions. If a mother responded negatively (no) to at least one question, we have considered that she had disrespectful delivery care (17).
The data on maternal age, religion, marital status, occupation, educational level, residence, income, ethnicity, antenatal care (ANC) follow-up, the reason to deliver in the hospital, admission to the maternity waiting room before labor started, the duration of labor, the gender of the maternity care provider attending the birth, and a face-to-face interviewer-administered questionnaire in the postnatal room were used to collect information from providers on the place of birth during ANC. Healthcare providers attending labor and delivery, companion during labor, labor outcome, and labor started spontaneously/ induced were collected an extract checklist used when reviewing their medical records.
Technical training for data collectors was provided before the actual data collection, and a pretest on 5% of the total sample size outside the study area with similar characteristics to the study population was conducted to ensure the quality of the data. The adapted English questionnaire was translated into Amharic, the local language, and then back to English by a language expert for consistency checks. We used six trained and degreed midwives as data collectors and two physicians as supervisors to collect all the requisite sample sizes. Each completed questionnaire was double-checked for accuracy, consistency, and completeness by the supervisors every day.
The data were double-checked, coded, and entered into Epi Data version 3.1 software packages before being exported to SPSS software for analysis. Frequency tables and percentages were also used to present the descriptive analysis. To explain the data, the mean and standard deviations were calculated and used for applicable variables. For the multivariable regression model, bivariable regression analysis with a p < 0.25 was used to select candidate variables. The AOR with their 95% confidence CI was calculated after a multivariable logistic regression was fitted using the centering method. Finally, variables in the multivariable regression analysis with a p < 0.05 were considered significant.
A total of 348 mothers with newborns were included in the study, making a response rate of 100%. 149 (42.8%) of respondents fall in the 20–24 years age group. Nearly one-third of the study participants, 133 (38.2%) were from the Bench ethnic group and 149 (42.8%) were followers of the Protestant religion. About two-thirds of the mothers, 257 (73.9%), were married. Around half of them, 201 (57.8%) were housewives, and one-third of them, 112 (32.2%), had a monthly family income of 10–30 US dollars (USD). Above half of the respondents, 200 (57.5%) were non-educated (Table 1).
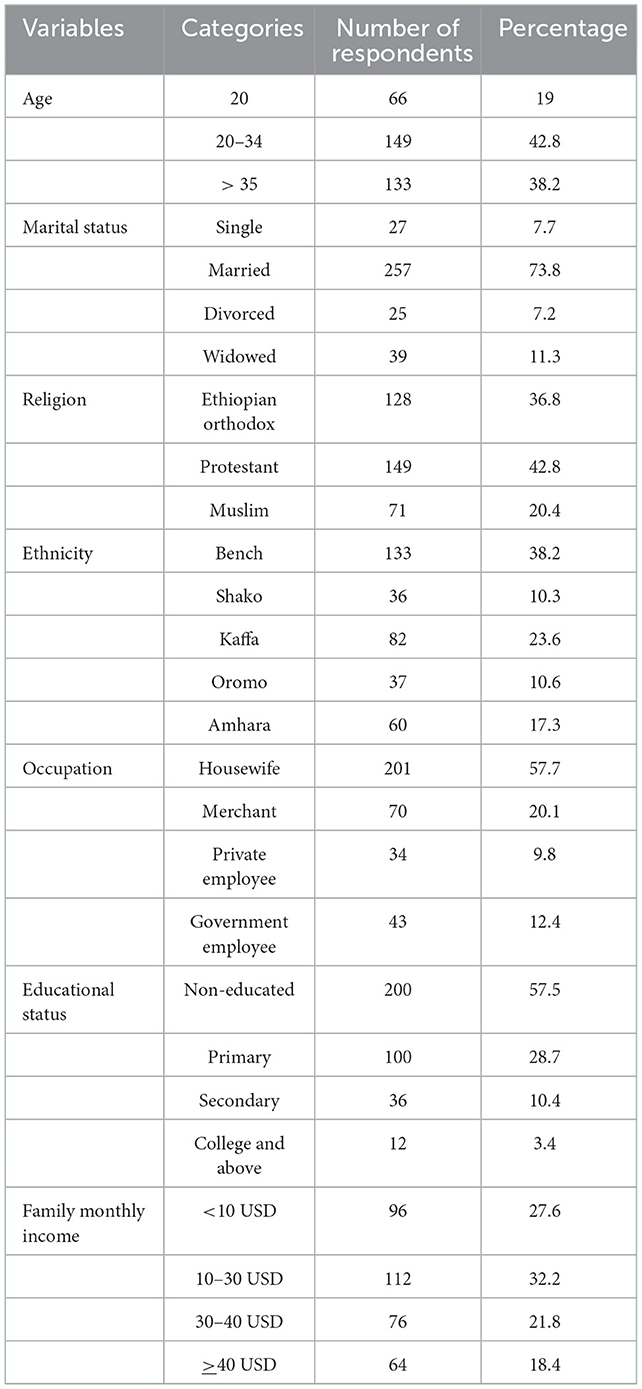
Table 1. The socioeconomic characteristics of mothers at three public hospitals in Southwest Ethiopia in 2021 (n = 348).
Of the total respondents, 317 (91.1%) had a history of ANC follow-up for recent childbirth; 266 (76.4%) of the mothers were attended by a midwife; 271 (77.9%) of mothers gave birth through spontaneous vaginal delivery, and more than half of 201 (57.8%) healthcare providers were males. The majority of mothers (281) (80.7%) were admitted to maternity waiting homes, which are designed to improve access to obstetric care for high-risk pregnant women or those who live very far away from health facilities before delivery. More than half, 184 (52.9%), mothers discussed delivery with a provider, and 276 (79.3%) did not have complications during delivery (Table 2).
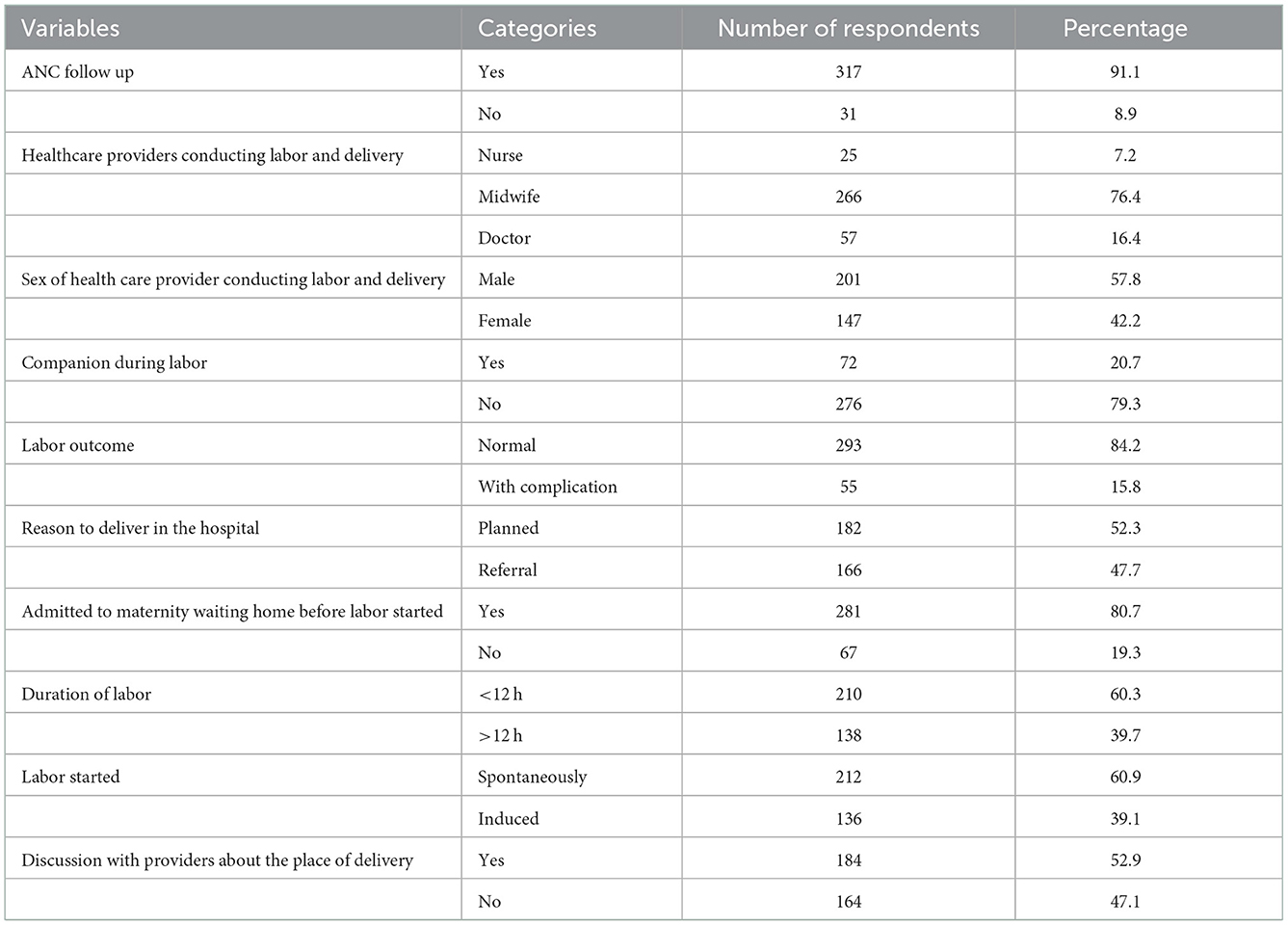
Table 2. The obstetric characteristics of mothers in three public hospitals in Southwest Ethiopia in 2021 (n = 348).
Of the proportion of RMC out of 348 mothers who gave birth in three public hospitals in Southwest Ethiopia, 283 (81.2%) mothers received RMC, but the remaining 65 (18.8) mothers were disrespected during labor and delivery (Figure 1). Out of the 348 respondents, 82.6%, 77.0%, 84.1% and 79.3% received friendly, abuse-free, timely, and discrimination-free care, respectively (Table 3).
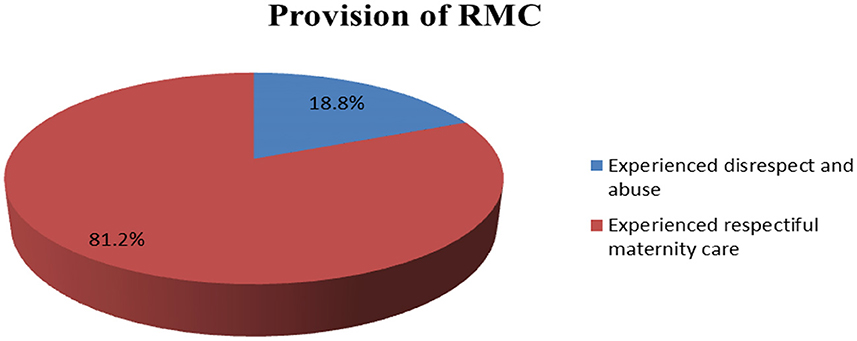
Figure 1. Provision of RMC during labor and delivery in three public hospitals of Southwest Ethiopia (n = 348).
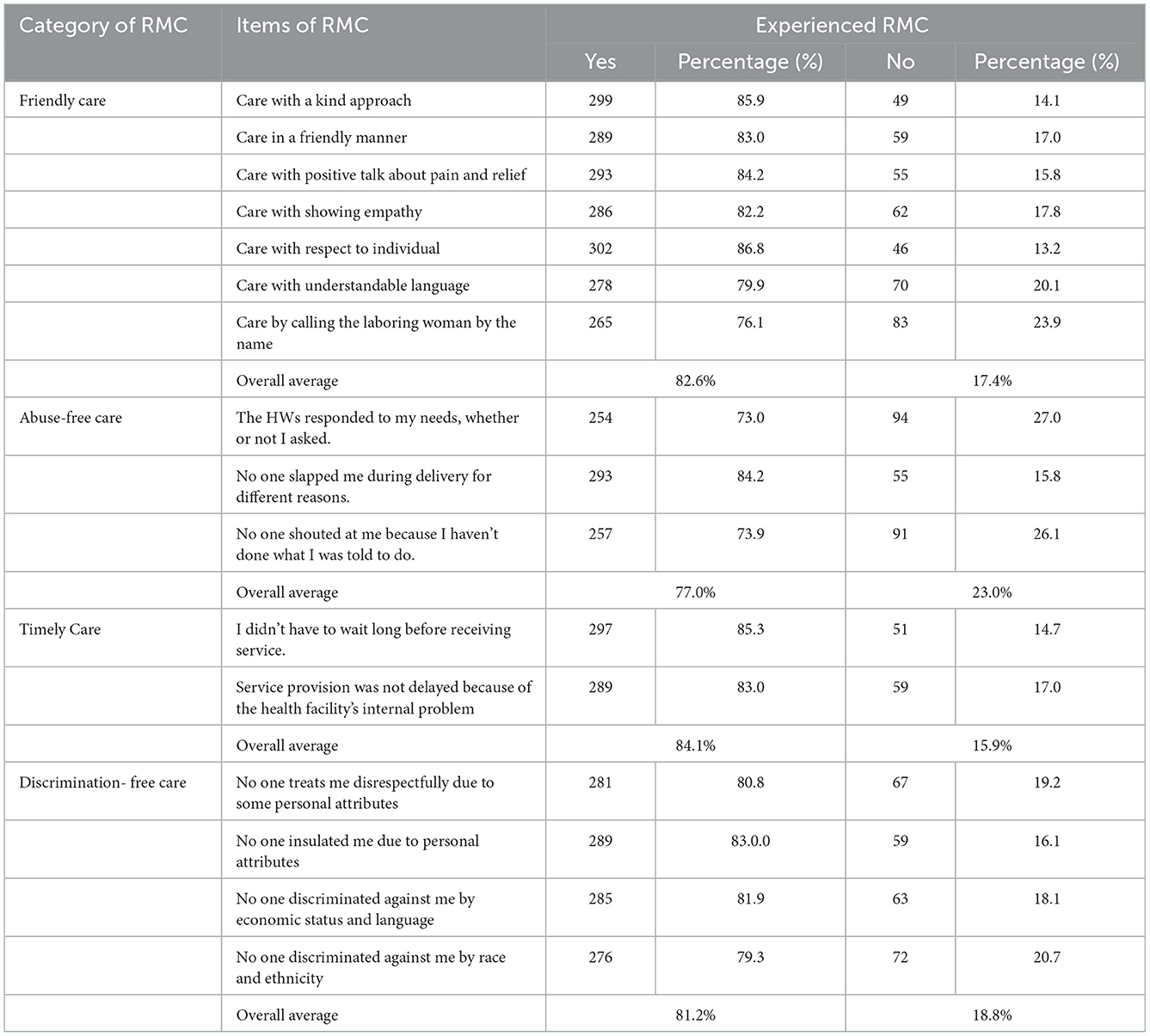
Table 3. Provision of RMC during childbirth at three public hospitals in Southwest Ethiopia, 2021 (n = 348).
In the bivariable logistic regression model, maternal age, maternal occupation, ANC follow-up, the provider who attended the labor and delivery, companion during labor, labor outcome, a reason to deliver in the hospital, admission to maternity waiting home before labor started, duration of labor, how labor started (spontaneously vs. induced) and discussion about the place of delivery with a provider during ANC follow up were the main components of RMC. After adjusting for confounding variables in a multivariable logistic regression model, maternal age, maternal occupation, ANC follow up and discussion about the place of delivery with a provider during ANC follow-up were identified as the significant predicates of RMC.
Mothers who were <20 years old were 2.5 times more likely to receive respectful maternity care than those whose age was more than or equal to 35 years [AOR = 2.54; 95% CI (1.01–6.43)]. Mothers who had private work were 5.2 times more likely to receive respectful maternity care than women who had governmental work [AOR = 5.23; 95% CI (1.15–23.72)]. Mothers who had at least one history of ANC follow-up in their current pregnancy were 2.8 times more likely to receive RMC as compared to their counterparts [AOR = 2.86; 95%CI (1.01–8.20)]. The odds of experiencing RMC were higher among mothers who discussed the place of delivery with healthcare providers during their current pregnancy as compared to their counterparts (AOR = 5.58; 95% CI: [2.12–14.70]) (Table 4).
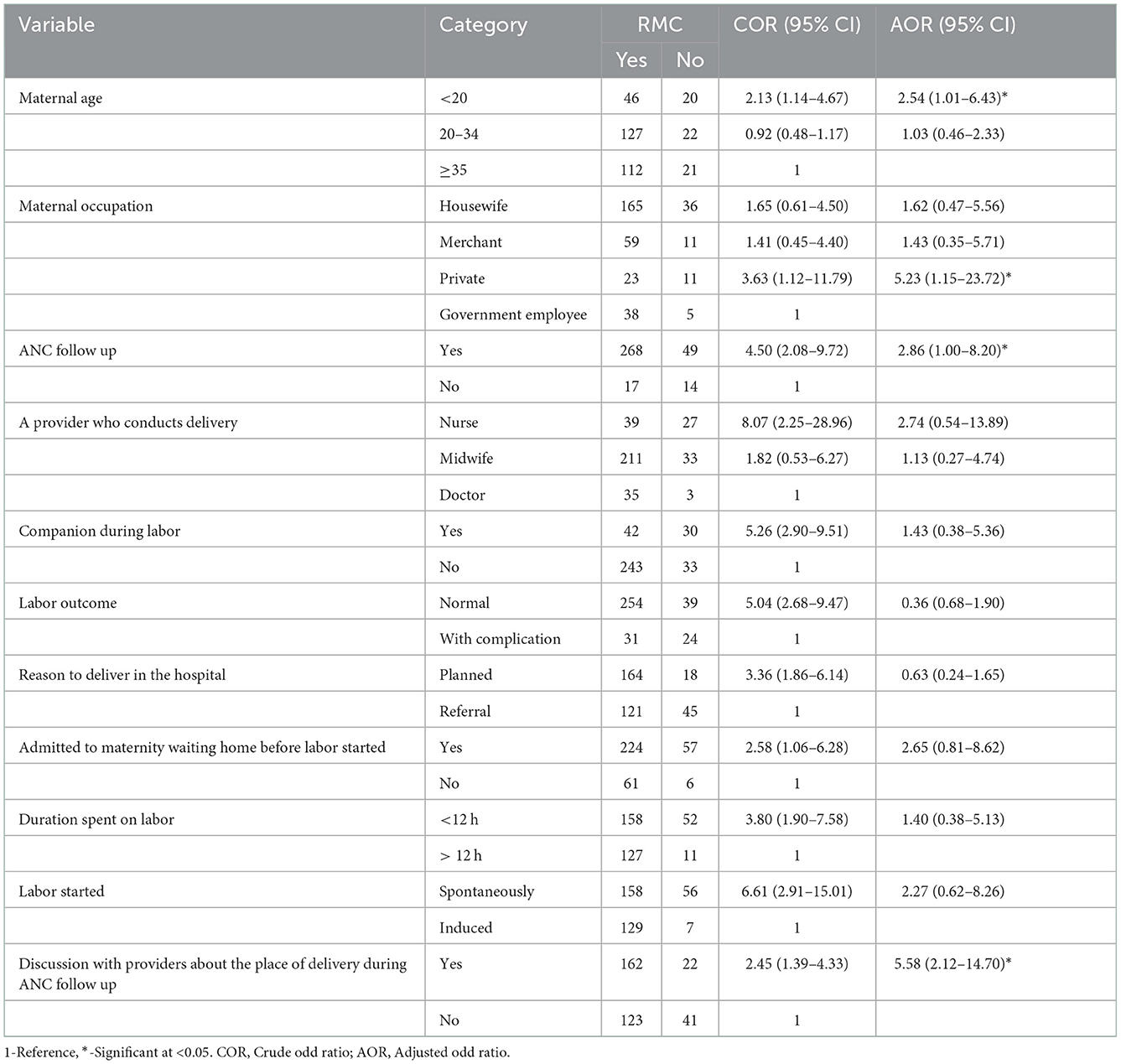
Table 4. Bivariable and multivariable analyses showing crude and adjusted odds ratios for an association between RMC and risk factors among mothers who give birth in three public hospitals in Southwest Ethiopia, 2021 (n = 348).
An important approach to minimizing maternal and neonatal morbidity and mortality is to increase pregnant women's access to skilled care during childbirth (5). The study aimed to assess the provision of RMC and related characteristics among birthgiving mothers in three public hospitals in Southwest Ethiopia.
The overall provision of RMC was 81.2%, according to the findings of this study. This result is higher than the studies found in Ethiopia (57%), and Kenya (80 %) (18, 19). However, the result is lower than a study conducted in Tanzania (20). This difference could be due to time differences associated with current accelerated reproductive health promotion activities, women-friendly programs, and various supportive types of training in some health institutions in the study area, as well as the small sample size of previous studies and different study areas.
In the current study, a variety of factors affected RMC. In this regard, the study found that mothers who were younger than 20 years old were more likely to have RMC than older mothers. This finding was supported by research conducted in Kenya (19). The reason for this association could be that women under the age of 20 are more educated than their counterparts; these mothers may have a greater understanding of healthcare facilities, as well as of their rights and privileges.
Mothers who had at least one history of ANC follow-up in their current pregnancies were more likely to receive RMC as compared to their counterparts. This finding is in line with findings from recent studies in Ethiopia's southern and eastern regions (21, 22). ANC follow-up enhances RMC provision. The pregnant women's adaptation to the services and close relationships with the healthcare staff are critical in creating trust in the facility's services.
Last but not least, RMC was part of a pregnant woman's discussion with healthcare providers about the place of birth. In this context, women who discussed a birthplace with maternity care providers during ANC were more likely to receive RMC than those who did not. This evidence supports research conducted in Oromia, Ethiopia, which found that mothers who had not received ANC visits were more likely to be disrespected and abused than those who had received ANC visits (23). This could be because women who had ANC and discussed a birthplace were more likely to know the healthcare professionals who would attend them during their labors and births.
The provision of RMC was high, but there are complaints of disrespect and abuse still present in three hospitals in Southwest Ethiopia. Maternal age, maternal occupation, antenatal follow up and discussion with the provider about the place of delivery during antenatal follow-up were associated with respectful maternity care. Thus, improving ANC service utilization and discussion with healthcare providers about the place of delivery during ANC follow-up should be focused on.
Our research might have the following limitations: Our research might have been subject to social desirability bias and fear of reporting abusive care, since the data were collected within the hospital setting. The other limitation is that meanwhile, the data were collected in the early postpartum period; thereby some women were too exhausted to respond to some questions.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Mizan Tepi University. The patients/participants provided their written informed consent to participate in this study.
AA developed the conception of the idea, wrote the proposal, and participated in the data collection and analysis. KK participated in data analysis, report writing, and prepared the manuscript. GA approved the proposal with some revisions and participated in manuscript development. All authors read and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ANC, Antenatal Care; D&A, Disrespect and Abuse; AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; GSGH, Gebretsadik-Shawe General Hospital; HWs, Health Workers; MTUTH, Mizan Tepi University Teaching Hospital; RMC, Respectful maternity care; SBA, Skilled Birth Attendant; TGH, Tepi General Hospital; WHO, World Health Organization.
1. Windau-Melmer T. A Guide for Advocating for Respectful Maternity Care. Washington, DC: Futures Group Health Policy Project (2013). p. 1–8.
2. Browser D, Hill K. Exploring Evidence for Disrespect Abuse in Facility Based Childbirth: Report of a Landscape Analysis-USAID. (2015). Available online at: http://www.mhtf.org/document/exploring-evidence-for-disrespect-and-abuse-in-facility-based-childbirth
3. Fekadu GA, Ambaw F, Kidanie SA. Facility delivery and postnatal care services use among mothers who attended four or more antenatal care visits in Ethiopia: further analysis of the 2016 demographic and health survey. BMC Pregnancy Childbirth. (2019) 19:1–9. doi: 10.1186/s12884-019-2216-8
4. Reis V, Deller B, Carr C, Smith J. Respectful Maternity Care: Country Experiences, Survey Report. Washington DC: United States Agency for International Development (2012).
5. Reis V, Deller B, Catherine Carr C, Smith J. Respectful Maternity Care. Washington DC: USAID (2012).
6. Wassihun B, Deribe L, Worede N, Gultie T. Prevalence of disrespect and abuse of women during childbirth and associated factors in Bahir Dar town, Ethiopia. Epidemiol Health. (2018) 40:e2018029. doi: 10.4178/epih.e2018029
7. Kruk ME, Kujawski S, Mbaruku G, Ramsey K, Moyo W, Freedman LP. Disrespectful and abusive treatment during facility delivery in Tanzania: a facility and community survey. Health Policy Plan. (2018) 33:e26–33. doi: 10.1093/heapol/czu079
8. Nyamtema AS, de Jong AB, Urassa DP, Van Roosmalen J. Using audit to enhance quality of maternity care in resource limited countries: lessons learnt from rural Tanzania. BMC Pregnancy Childbirth. (2011) 11:1–8. doi: 10.1186/1471-2393-11-94
9. World Health Organization. The Prevention and Elimination of Disrespect and Abuse During Facility-Based Childbirth: Geneva, Switzerland, WHO Statement. World Health Organization (2014).
10. FMOH. Federal Democratic Republic of Ethiopia, Federal Ministry of Health; Health Sector Transformation Plan (HSTP) 2015/16-2019/20.
11. Gurara MK, Jacquemyn Y, Ukke GG, Van Geertruyden J-P, Draulans V. Benefits, barriers and enablers of maternity waiting homes utilization in Ethiopia: an integrative review of national implementation experience to date. BMC Pregnancy Childbirth. (2022) 22:1–23. doi: 10.1186/s12884-022-04954-y
12. UNICEF. National Situation Analysis of Children and Women in Ethiopia. Addis Ababa, Ethiopia: Ministry of Finance/UNICE (2017).
13. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey. Addis Ababa; Rockville, MD: CSA and ICF (2016)
14. Wolde HF, Gonete KA, Akalu TY, Baraki AG, Lakew AM. Factors affecting neonatal mortality in the general population: evidence from the 2016 Ethiopian Demographic and Health Survey (EDHS)—multilevel analysis. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4668-3
15. Hurissa B, Getinet T. Assessment of provision of women friendly care and associated factors among postnatal mothers at three public hospitals of Jimma Zone, Oromia Region, Ethiopia, 2016. J Biomed Sci. (2017) 6:26. doi: 10.4172/2254-609X.100070
16. World Health Organization. Proportion of Births Attended by a Skilled Attendant: Geneva, Switzerland, 2008 Updates. World Health Organization (2008).
17. Wubetu YA, Sharew NT, Mohammed OY. Respectful Delivery Care and Associated Factors Among Mothers Delivered in Debre Berhan Town Public Health Facilities, Ethiopia. (2020). doi: 10.21203/rs.3.rs-62205/v1
18. Wassihun B, Zeleke S. Compassionate and respectful maternity care during facility based child birth and women's intent to use maternity service in Bahir Dar, Ethiopia. BMC Pregnancy Childbirth. (2018) 18:1–9. doi: 10.1186/s12884-018-1909-8
19. Abuya T, Ndwiga C, Ritter J, Kanya L, Bellows B, Binkin N, et al. The effect of a multi-component intervention on disrespect and abuse during childbirth in Kenya. BMC Pregnancy Childbirth. (2015) 15:1–14. doi: 10.1186/s12884-015-0645-6
20. Sando D, Ratcliffe H, McDonald K, Spiegelman D, Lyatuu G, Mwanyika-Sando M, et al. The prevalence of disrespect and abuse during facility-based childbirth in urban Tanzania. BMC Pregnancy Childbirth. (2016) 16:1–10. doi: 10.1186/s12884-016-1019-4
21. Dewana Z, Fikadu T, Abdulahi M. Client perspective assessment of women's satisfaction towards labour and delivery care service in public health facilities at Arba Minch town and the surrounding district, Gamo Gofa zone, south Ethiopia. Reprod Health. (2016) 13:1–6. doi: 10.1186/s12978-016-0125-0
22. Bante A, Teji K, Seyoum B, Mersha A. Respectful maternity care and associated factors among women who delivered at Harar hospitals, eastern Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. (2020) 20:1–9. doi: 10.1186/s12884-020-2757-x
Keywords: abuse, disrespect, Mizan Tepi University, respectful maternity care, associated factors
Citation: Adugna A, Kindie K and Abebe GF (2023) Respectful maternity care and associated factors among mothers who gave birth in three hospitals of Southwest Ethiopia: A cross-sectional study. Front. Public Health 10:1055898. doi: 10.3389/fpubh.2022.1055898
Received: 28 September 2022; Accepted: 08 December 2022;
Published: 04 January 2023.
Edited by:
Kwasi Torpey, University of Ghana, GhanaReviewed by:
Robbie Elizabeth Davis-Floyd, Rice University, United StatesCopyright © 2023 Adugna, Kindie and Abebe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amanuel Adugna,  YW1hbnVlbGFkdWduYTIxQGdtYWlsLmNvbQ==
YW1hbnVlbGFkdWduYTIxQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.