- 1School of Public Policy and Management, Tsinghua University, Beijing, China
- 2School of Architecture, Harbin Institute of Technology (Shenzhen), Shenzhen, China
Introduction: Although the impact of neighborhood social capital on mental health has long been recognized, the extent to which the impact differs between immigrants and local residents remains a puzzle. This study aims to bridge the gap by comparing internal migrants who are restricted by their household registration (hukou) status, and urban natives in China.
Methods: Using self-rated mental health and social capital survey data collected in 26 neighborhoods in Beijing, this study examines the mental health outcomes of three types of neighborhood social capital, including social networks, shared norms and mutual trust, and social support.
Results: The study finds that the hukou status of immigrants moderates the effect of neighborhood social capital on mental health, and that the internal migrants in China experience less mental health benefit of neighborhood social capital than urban natives. Compared with urban natives, neighborhood social networks have less positive effect on migrants' mental health than that of urban natives.
Conclusion: The findings suggest that policy makers can improve the mental health of migrants through social capital building on the premise of eliminating the restrictions of hukou system on the migrants' right to participate in neighborhood activities and to access neighborhood services.
Introduction
The mental health of immigrants has been one of the most commonly discussed public health issues across disciplines (1, 2). Studies have showed that poverty, social stigma, discrimination in the job markets, and exclusion from local public services can cause substantial mental stresses for immigrants (3–6). These risk factors for mental stress may lead to a decline in the health advantage of immigrants over time, even if they generally report superior health conditions than natives at an early stage (7, 8).
In the past few years, a considerable body of literature has investigated the benefits of neighborhood-level social capital on residents' mental health (9–11). Neighborhood social capital refers to the features of social organization within a neighborhood, such as networks, trust, and support (9, 12–14). Recent studies also found that the same formation of social capital may have different effects on individuals with different social-demographic characteristics, such as gender and income (15). However, less is known about the extent to which their mental health impacts vary between immigrants and native residents. Immigrants often are segregated in enclaves with truncated social ties and supporting system (16–20). Even when living in the same neighborhood, immigrants remain largely marginalized from the mainstream society in their everyday lives (21–23). For immigrants, living in a mixed neighborhood with urban natives does not necessarily guarantee equal access to, nor fully utilize, the “stock” of neighborhood social capital as local neighbors to maintain mental health (21, 24).
Literature on the mental health of migrant populations in Chinese cities continues to emerge (5, 6, 25–27). It was recently reported that the number of internal migrants in urban China – residents who live in cities but do not possess an official urban residency status under the household registration system (hukou) – had reached 236 million in 2019 (28). Like immigrants in Western cities, internal migrants in China face higher mental health risks after relocating to receiving cities (29, 30).
Unlike ethnicity-based social etiologies in most western countries, the mental health of internal migrants in China is closely related to their hukou status (19, 31). Migrants without a local hukou are restricted from enjoying universal social welfare (32–35), and experience stereotypes and stigma in their daily interactions with urban natives (23, 36, 37). Hukou status marks different social groups, which may be not conducive to the positive impact of neighborhood social capital on the mental health of the internal migrants. However, the disparity between migrant and native residents within Chinese cities has not been fully studied.
In this article, we extend the line of inquiry on the mental health impacts of neighborhood social capital by exploring the heterogeneous effects between migrant and native residents in Chinese cities. Based on an empirical analysis of self-rated mental health and social capital survey collected in Beijing, we test the extent to which various dimensions of neighborhood social capital (i.e., social networks, shared norms and mutual trust, and social support) predict self-rated mental health, and the extent to which these effects are moderated by individual's residency status structured by China's unique hukou system.
The intellectual contribution of this analysis is twofold. First, we engage with the international literature on the effects of neighborhood social capital on mental health while highlighting the differential effects across social groups, thereby providing empirical evidence to better inform community development and public health strategies. Second, we combine the emerging literature on social capital determinants of migrants' mental health with empirical studies in urban China, while highlighting the social aspects of neighborhood environment.
Literature review
Neighborhood social capital and immigrants' mental health
Public health scholars have sought to understand the effects of neighborhood social capital on mental health, though conceptualization and measurement of social capital have varied in different studies (9, 38). Recognizing the influences of different disciplines (39–42), public health scholars have generally viewed neighborhood social capital as multi-dimensional concept that involves interpersonal networks developed within the neighborhood, shared norms and trust, as well as reciprocal social support developed through social interactions with neighbors (9, 12).
On the one hand, neighborhood social networks, defined as informal social relationships between neighbors developed in their everyday-life encounters, can procure predictable mental health benefits (38, 43). Residents can circulate health-relevant information from social networks with neighbors, which may help enhance their own mental health (4). Further interactions with neighbors may also directly contribute to a positive psychological experience, such as a sense of belonging and security, and recognition of self-worth (44, 45).
On the other hand, shared norms and mutual trust may benefit residents' mental health by providing a source of mutual connection and mutual respect and by improving residents' sense of purpose in life (46). Neighborhood social support is also an important form of neighborhood social capital that individuals can use to cope with everyday problems (47). Neighborhood social support plays an essential role in mental health by buffering the effects of psychological stress and promoting reciprocity, especially for vulnerable groups who are more likely to rely on neighborhood resources (43, 48).
However, research in Western Europe and the United States found that immigrants may not benefit from neighborhood social capital as much as their native neighbors. First, immigrants are considered as “outsiders”, marginalized in their receiving neighborhood. They change their residences frequently, hence having difficulties in expanding neighborhood social networks or having sustained social interactions with their neighbors (15, 24). In Netherlands, Fajth and Bilgili (24) found that immigrants do not interact with their local neighbors frequently, even though they have lived in their receiving neighborhoods for many years and acquainted with most of their neighbors. Without further social interactions, the impact of neighborhood social networks on immigrants' mental health is limited.
Second, immigrants might be seen as the “others” and socially excluded by their local neighbors. Under high levels of social discrimination, frequent interactions between immigrants and native residents may lead to feelings of deprivation or mental stress (15, 49). Wutich et al. (49) research on Latino immigrants in the U.S found that those who have frequent social interactions with local neighbors report higher level of perceived stigma and worse mental health status in their ethnographic interviews. While these interactions with neighbors may also bring beneficial social capital to immigrants, i.e., trust and support, the negative emotions reinforced by neighborhood interactions may not be ameliorated by neighborhood social capital (38).
Hukou system and migrants' mental health in China
Although Chinese cities do not suffer from racial or ethnic divisions seen in Western cities, internal migrants in China still experience persistent discrimination and marginalization caused in large by the hukou system (36, 50, 51), which may also affect the mental health of residents (5, 52). Hukou-based residency status may potentially moderate the effect of neighborhood social capital on mental health. First, hukou-based residency status creates significant disparities in local citizenship and rights, defining access to welfare and services, including healthcare services (30, 53, 54). According to Gu et al. (53) and Lao et al. (54) nationwide study (53, 54), residents with local hukou enjoy access to better public services, while residents without local hukou are denied urban citizenship and benefits that normally accompany with the citizenship. Urban natives, born with local hukou, enjoy full access to local public resources and services, including care for mental health (50). A small group of internal migrants, typically more educated and privileged, manage to obtain local urban hukou upon or after migrating to receiving cities (33). These permanent migrants with urban hukou enjoy similar welfare entitlement as urban natives. However, a large number of internal migrants are temporary migrants, who do not hold official urban hukou despite having lived and worked in receiving cities and thus deprived of equal eligibility for urban health insurance, resulting in limited access to mental healthcare resources (35).
In addition to its direct influence on mental health, the hukou-based residency status also indicates different accessibilities to social capital living in urban neighborhoods (26, 29, 50), which may moderate the effect of neighborhood social capital on mental health. While neighborhood social capital is demonstrated to support urban natives' mental health (26), such effects can be more complicated for migrants. Previous studies have found that temporary migrants in China are experiencing discrimination and prejudice from local urbanites and thus are excluded from local social networks (37, 55). Although migrants may maintain social networks composed of strong ties with kinship relatives and other migrants of similar places of origin (19, 21, 52), these strong yet truncated social networks may not provide diversified information and resources that are critical for a positive living experience for disadvantaged migrants, but rather reinforce a sense of marginalization and exclusion among migrants. Compared to temporary migrants, permanent migrants have developed local ties and interact with local neighbors regularly (29). However, they are still experiencing discrimination and social exclusion, despite having obtained urban hukou (50). Such perceived experiences of social stigma and discrimination may contribute to the psychological distress of residents (52). Additionally, while neighborhood-based social capital provides an important source of material and psychological support to get by in daily life (40, 56), bonding social capital with kinship ties can also create a strong norm of reciprocity and can sometimes become emotionally draining (56), which may further increase the psychological stress among migrants.
Therefore, the empirical study aims to answer two research questions:
• The extent to which various dimensions of neighborhood social capital – neighborhood social networks, shared norms and mutual trust, and neighborhood social support – predict self-rated mental health of urban residents in China,
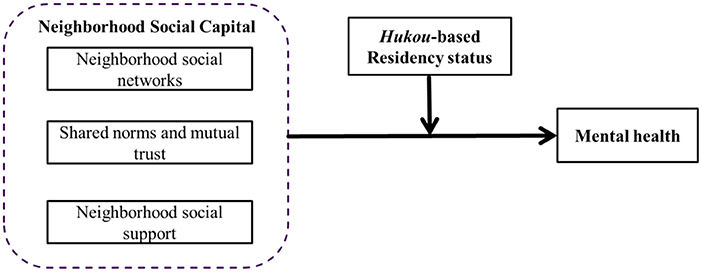
• To what extent the associations between neighborhood social capital and self-rated mental health are moderated by the hukou-based residency status (see Figure 1 for our conceptual framework).
Based on the above discussions, we hypothesize that:
• Various dimensions of neighborhood social capital – neighborhood social networks, shared norms and mutual trust, and neighborhood social support – may predict a positive mental health status for urban natives;
• The hukou-based residency status may moderate the effect of neighborhood social capital on self-rated mental health.
Data and methods
Data source
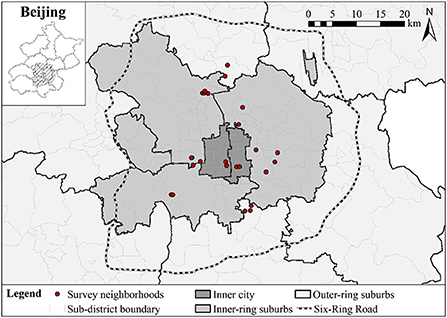
Our data was derived from a large-scale questionnaire survey conducted in 2017 that collected the mental health and neighborhood social capital data of 1,280 residents from 26 neighborhoods (shequ) in Beijing, China. Beijing has seen a massive influx of migrants over the past three decades. By 2017, Beijing had about 7.94 million migrants, accounting for 36.6% of the total population (57). Chinese municipalities typically include an urbanized core area (jianchengqu) and rural areas in the outskirt. Our study focuses only on the urbanized area of the Beijing Municipality, which primarily is located within the Six-Ring Road (Figure 2). Following Hu et al. (58), we divided our study area into the inner-city area (Xicheng and Dongcheng districts), the inner-ring suburb (Haidian, Chaoyang, Shijingshan, and Fengtai districts), and the outer-ring suburb (parts of Changping and Daxing distrcts).
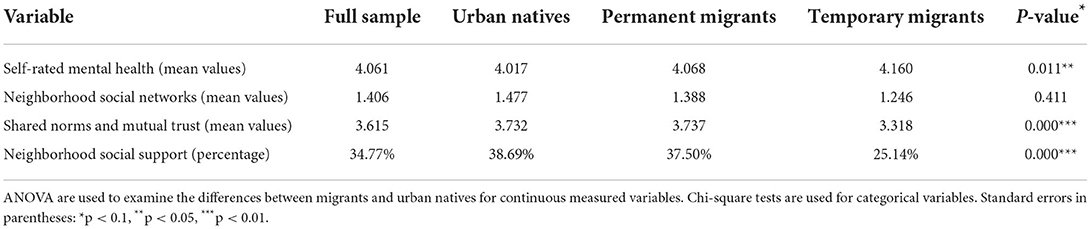
A multi-stage stratified sampling strategy was adopted to maximize the representativeness of diverse urban neighborhoods in different urban locations: four in the inner city, 16 in the inner-ring suburb, and six in the outer-ring suburb (Figure 2). From these 12 sub-districts, we selected a total of 26 neighborhoods (shequ) representing years of construction, housing characteristics, physical layout and environment, and socio-demographic structure. Finally, in each neighborhood we selected 50 residents (age 18–65) through a combination of systematic and stratified sampling strategies, according to the address list provided by the neighborhood resident committees. The survey eventually yielded a total of 1,280 valid samples (see Table 1 for the socio-demographic structure of the sample). To understand the effects of neighborhood social capital between migrants and urban natives on mental health, our sample did not include migrants living in other informal housing such as factory dorms or construction sites.
Variables and measures
Self-rated mental health
We use self-rated score to measure the overall mental health status of the participants. The question was asked as follows in the questionnaire. ‘What do you think about your mental health in the past year in general?' The self-rated scores range from 1-very unhealthy, 2-unhealthy, 3-neutral, 4-healthy, to 5-very healthy. This measurement has been used in a number of mental health studies [e.g., (44, 59)] and has been proven valid in capturing mental health status.
Neighborhood social capital
We included three variables to capture different dimensions of neighborhood social capital, namely social networks, shared norms and mutual trust, and social support.
Neighborhood social networks was measured by the number of non-kinship ties (i.e., friends and colleagues, excluding family members or relatives) that a respondent reported to have in the neighborhood. The second variable, i.e., shared norms and mutual trust, was measured by a composite index derived from five 1-5 Likert scale questions asking each respondent to rate the level of agreement to five statements, including: (1) I am familiar with my neighbors, (2) people in this neighborhood have similar values and views, (3) people in the neighborhood trust each other, (4) I am able to ask neighbors for help when in trouble, and (5) people in the neighborhood get along well with each other. We calculated the Principal Component Factor score of the five items as the value of neighborhood shared norms and mutual trust (Cronbach alpha = 0.878). Finally, neighborhood social support was generated from a multiple-choice question in the survey that reads “if you encounter any problem in your daily life (e.g. taking care of elders or picking up children when you are not free), who is your first choice to ask for help”. The choice of “neighbors” and “residents” committee were coded as 1 and other choices (e.g. relatives and friends in other neighborhoods, or hired domestic helpers) were coded as 0.
The hukou-based residency status
Unlike most existing studies on China's internal migration, which typically treats residency status as a binary situation of migrant versus local residents, we defined residency status into three categories – urban natives, permanent migrants, and temporary migrants – to explore the nuances created by the formal hukou institution and the informal everyday-life experiences of migrant social exclusion. The moderating variable – residency status – was captured from two survey questions asking the birth place and current hukou type of each respondent. Urban natives refer to residents who are born in Beijing and with local urban hukou; permanent migrants refer to residents who were born outside of Beijing city but have obtained Beijing urban hukou after migrating to the city; and temporary migrants refer to the residents who were born outside of Beijing city and have migrated to Beijing without obtaining local urban hukou. Our final sample included 827 urban natives (64.7%), 88 permanent migrants (6.9%) and 365 temporary migrants (28.5%). Only a small portion of migrants is able to acquire Beijing urban hukou and get the identity of permanent migrants.
Control variables
Following previous studies about Chinese resident's mental health, Chinese resident's mental health is proved to associated with age (5, 26, 58), gender (5, 26, 58), marital status (5, 58), educational level (5, 26, 58), employment status (5, 26, 58), homeownership (5), co-residence status (5), and household income (5, 26). Therefore, we controlled eight sociodemographic variables, including age, gender (male = 1, female = 0), marital status (married = 1, others = 0), educational level, employment status (employed = 1, others = 0), homeownership (owner = 1, renter = 0), co-residence status (living with family = 1, living alone = 0), and per capita monthly household income (natural logarithm value).
Analytic strategies
We used ordered logit regression models since our dependent variable – self-rated mental health – was rated on a 1-5 ordinal scale. Ordered logit model is utilized to estimate the probability of each categorical outcome from more than two discrete choices, in which the log odds of the outcomes are modeled as a linear combination of the predictor variables. The modeling process can be described as the estimation of coefficients β for independent variables x and a set of cutpoints k. For each sample j, an underlying score y* was estimated as a linear function of the independent variables x and random error ε:
Meanwhile, the probability of observing outcome i corresponds to the probability that underlying score y* lies within the range of the cutpoints computed for the outcome:
In our ordered logit model, cluster-robust standard errors were used to account for potential heteroscedasticity due to the nested nature of the survey data, given that the samples were clustered in 26 neighborhoods. We first examine the association between self-rated mental health and neighborhood social capital and residency status with Model 1, controlling eight socio-demographic variables. In Model 2, we further include the interaction terms between residency status and three neighborhood social capital variables to test whether the associations between mental health and neighborhood social capital were moderated by residency status. To ensure the robustness of the findings, we also ran binary logit regressions by recoding self-rated mental health into a binary variable, with the values of 1–3 recoded into zero and the value of 4–5 recoded into one. The results were largely similar to those of the ordered logit regressions.
Empirical findings
Descriptive analysis
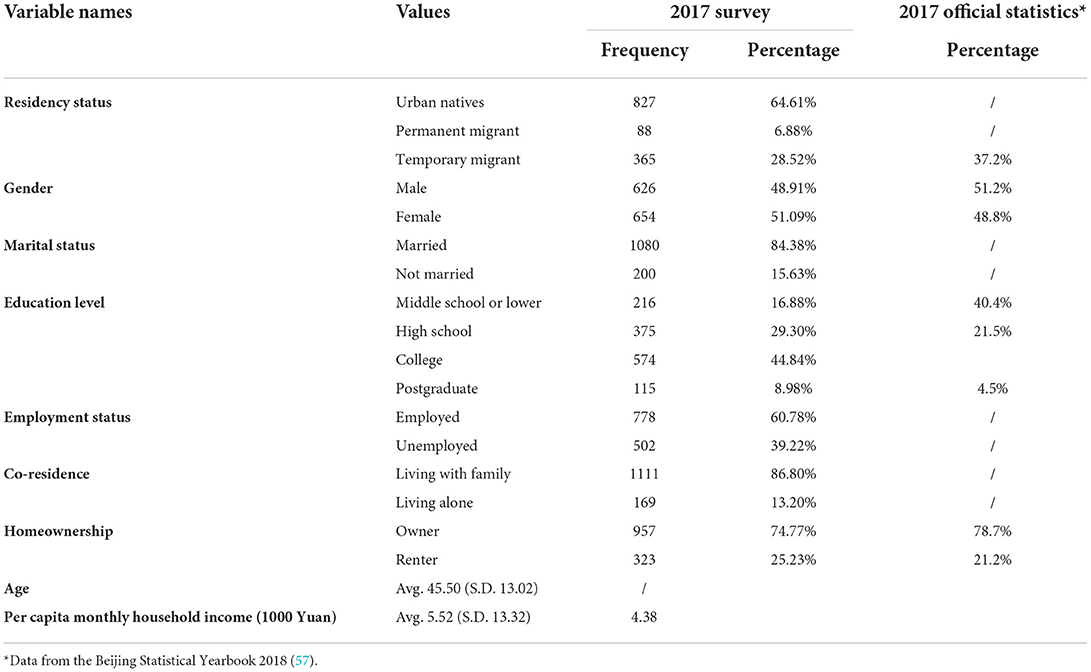
Table 2 shows the descriptive analysis of self-rated mental health and neighborhood social capital variables, stratified by residency status. ANOVA-tests and Chi-square tests were performed to test if significant differences exist between temporary migrants, permanent migrants, and urban natives. The self-rated mental health score of migrants (Temporary migrants: Mean = 4.160; Permanent migrants: Mean = 4.068) is slightly higher than that of urban natives (Mean = 4.017). Yet temporary migrants are significantly disadvantaged in the access to most neighborhood social capital compared with urban natives, as shown by the lower scores in all three dimensions of neighborhood social capital, although permanent migrants generally enjoy similar levels of neighborhood social capital as urban natives (Table 2).
Association between self-rated mental health and neighborhood social capital
Table 3 presents the results of the ordered logit regression model. Model 1 presents the main effects of neighborhood social capital without the interaction terms. The average VIF value for all independent variables in model 1 was 1.61, with no VIF value of any individual independent variable exceeding 10, which indicated no serious multicollinearity issue.
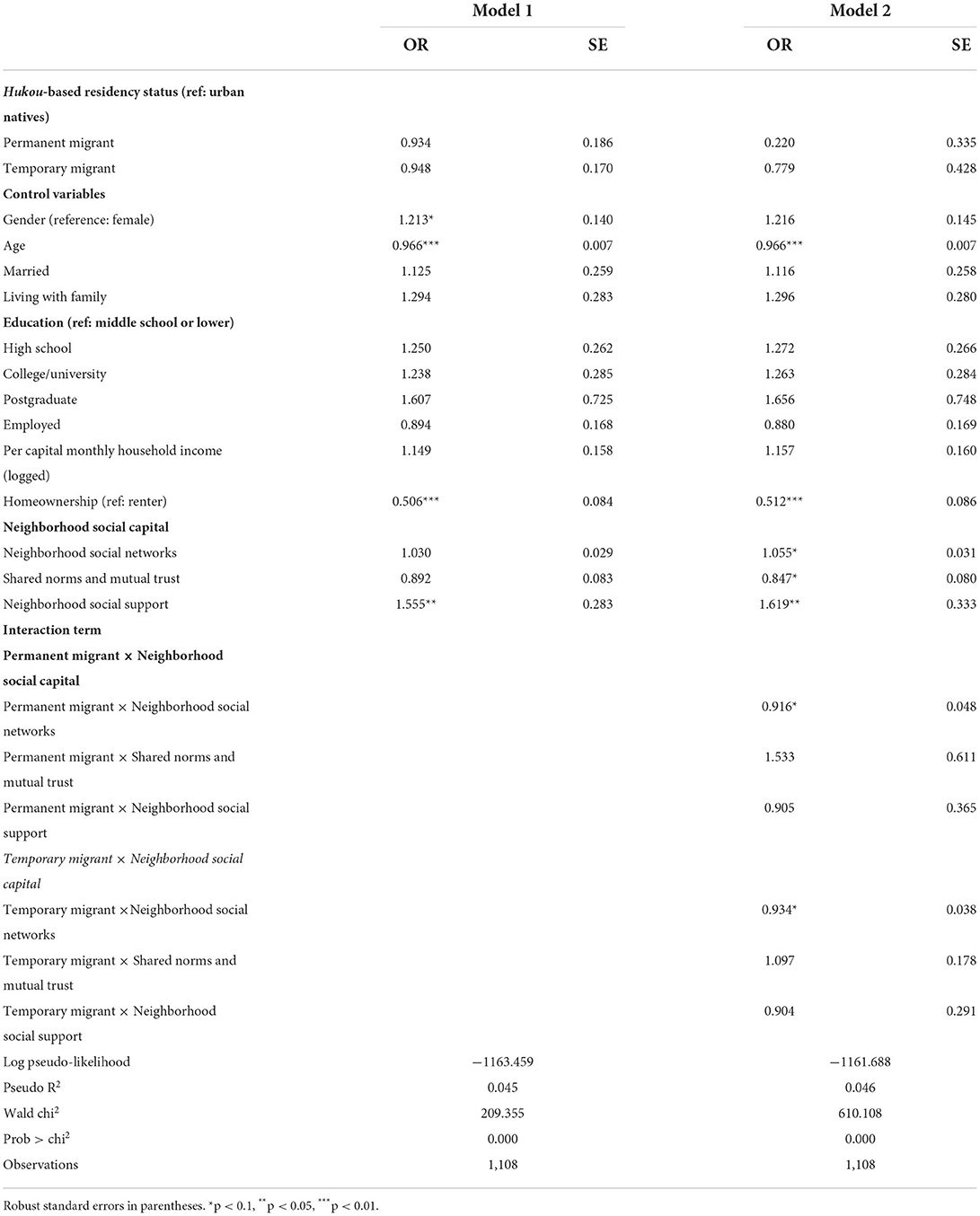
Table 3. Ordered logit regression results: Association between neighborhood social capital and self-rated mental health.
After controlling social-demographic variables, no significant difference was founded between self-rated mental health of permanent migrants, that of temporary migrants and that of urban natives. Neighborhood social support were positively associated with mental health: all else equal, a resident is more likely to report a higher mental health score if he or she perceives availability of social support in the neighborhood (OR = 1.555, p = 0.015; Table 3). However, neither neighborhood social networks nor mutual trust was significantly associated with self-rated mental health.
Several socio-demographic control variables were also found significant in predicting self-rated mental health (Table 3). On a 0.10 significance level, men were more likely than women to report positive mental health status (OR = 1.213, p = 0.093). Not surprisingly, older residents were less likely to report positive mental health status (OR = 0.966, p = 0.000). Interestingly, homeowners were significantly less likely than renters to report positive mental health status (OR = 0.506, p = 0.000), which is contrary to the findings in international literature about positive correlation between housing tenure and mental health (60). This might be related with high housing prices in Chinese large cities. Compared to renters, most of houseowners have no other options but to pay large amount of monthly mortgage after purchasing a house, therefore suffering from continuous mental stress (5).
Moderating effects of residency status
Model 2 in Table 3 presents results from the second ordered logit regression model with the interaction terms to further test the moderating effects of residency status on the mental health outcomes of neighborhood social capital.
In model 2, as for the baseline levels of neighborhood social capital effects, all the three types of neighborhood social capital are significant associated with mental health for urban natives. In specific, urban natives with more access to neighborhood social support (OR = 1.619, p = 0.019) and social networks (OR = 1.055, p = 0.063) report higher level of positive mental health status. In contrast, those urban natives perceiving higher level of mutual trust and shared norms report worse mental health status (OR = 0.847, p = 0.079). The significance of neighborhood social support is consistent with model 1, which is more robust than social networks and shared norms and mutual trust.
There is significant difference in the mental health impact of neighborhood social networks between migrants and native residents. Model results also indicate that resident status significantly moderates the mental health impacts for one dimension of neighborhood social capital – i.e., social networks, but not for neighborhood social support and shared norms and trust. Migrants are less likely to report the same level of self-rated mental health as urban natives, despite having the same size of neighborhood social networks. As shown in in Table 3, the OR for the interaction term between neighborhood social networks and residency status is 0.916 (p = 0.095) for permanent migrants and is 0.934 (p = 0.089) for temporary migrants. In other words, whereas urban natives are more likely to report better mental health with increased neighborhood social networks, such a positive association is significantly reduced for permanent and temporary migrants. Figure 3 illustrates the estimated associations between neighborhood social networks and respondents' self-rated mental health across different residency status. For both permanent and temporary migrants, larger neighborhood social networks predict lower level of self-rated mental health. We also estimated the difference between two migrant subgroups by setting permanent migrants as the baseline reference in interaction terms. The OR of interaction term reveals a stronger effect of neighborhood social networks for temporary migrants compared to permanent migrants, but the difference is not significant.
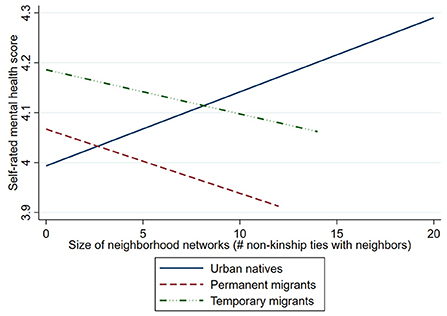
Figure 3. Predicted relationships between neighborhood social capital and self-rated mental health by different residency status.
Discussion and conclusion
Based on the cross-sectional questionnaire survey data of 26 neighborhoods in Beijing, China, this study examines the heterogenous effects of neighborhood social capital on the mental health between migrants and urban natives in the institutional context of the hukou system. Although migrants may have access to formal housing in socially mixed urban neighborhoods, they have relatively less neighborhood social capital than their native neighbors. The residency status of migrants plays a negative role in moderating the association between neighborhood social capital and mental health.
The positive effect of neighborhood social support and social networks on mental health for urban natives are consistent with previous findings (11, 26, 27). Comparatively, shared norms and mutual trust is negatively associated with mental health for urban natives, which is consistent with some findings in previous studies (15). This potential downside of social capital is more obvious in the context of population fluidity. For instance, one study in Japan found that the gap between positive mutual trust and negative experience of social interaction with dissimilar neighbors may cause psychological distress, which in turn affect mental health (61). Chinese urban neighborhoods have experienced the disbanding of social relationships over the years, partly due to the influx of migrants (62, 63). Compared with internal migrants, urban natives are more likely to have positive expectation on mutual trust and thus experiencing a significant gap between positive mutual trust and negative experience of social interaction with dissimilar neighbors (64, 65), which leads to poor self-rated mental health.
According to the second model which examines the interaction terms between residency status and three neighborhood social capital variables, immigrants did not gain as many mental health benefits from increased neighborhood social networks as their native neighbors. While previous studies found the importance of neighborhood social networks in improving mental health outcomes (11, 38, 43), this study suggests that the mental health benefits of neighborhood social networks can be attenuated by particular hukou-based residency status. Temporary migrants without local hukou may create stereotypes in the minds of urban natives, leading to self-isolation behaviors and avoidance of interaction with natives (36). Although some migrants have already developed social networks in their neighborhoods, their interaction with neighbors are relatively limited in improving their mental wellbeings (18). For those migrants who feel social marginalized and institutionally excluded, building greater social networks with local neighbors does not confer mental health benefits, but rather negative perceptions of social status (21) leading to worsening mental health outcomes. Despite having local hukou, permanent migrants who have not lived long enough in local urban society are less likely to develop close ties and interactions with the receiving neighborhoods (66). Their interactions with neighbors tend to be instrumental rather than emotional, which does not do much help to relieve their stress or anxiety, and thus appears to be less effective in improving mental health (67).
This research has several policy implications. Firstly, in parallel with other studies in Western countries, our findings indicate that neighborhood social capitals can make a significant contribution to residents' mental health. Therefore, to make residential areas a healing place for promoting mental wellness, planners and policy makers should pay more attention to the neighborhood social environment and foster a friendly neighborhood atmosphere. Secondly, migrants, especially temporary migrants without local hukou, are vulnerable to the negative impacts of neighborhood social capital on mental health. Therefore, this study calls on social organizations in local neighborhoods to abandon the restrictions of the household registration system, and provide permanent and temporary migrants with more opportunities to involve in neighborhood collectives and foster a sense of belonging. Building a healthy city for the mental wellness of all citizens requires integration between urban natives and immigrants, which needs the supports from China's macro-level institutions and micro-level community development efforts.
Several limitations of this study need to be acknowledged. First, our study relied on cross-sectional survey data. It is difficult to either infer causality from association, or to fully capture the multi-faceted causal mechanisms of neighborhood social capital and mental health. Longitudinal data and ethnographic materials with more detailed information should be used in future research. Second, with Beijing as research site, other types of Chinese cities, including medium-sized cities, were not considered. As the household registration policy is less stringent, the situation of immigrants in medium-sized cites might be different. Therefore, it is necessary to conduct a cross-city study to better understand the effects of neighborhood social capital on mental health of migrants in urban China. Finally, using one self-rated question to measure mental health has limitations in accuracy compared to using standard mental health questionnaires such as PHQ-9. The use of standard mental health questionnaires is thus encouraged to precisely assess mental health status.
In conclusion, this study finds neighborhood social capital has different effects on the mental health of migrants than urban natives in mixed urban neighborhoods. Our empirical evidence engages in the theoretical debate about how the effect of neighborhood social capitals on immigrant mental health are attenuated, extending the implications of neighborhood social capital in the migrant and mental health literature. In future research, a mixed-method approach should be taken to better understand the specific mechanisms by which individual life experiences, neighborhood social capital, and macro-social institutions jointly determine the mental health of floating populations.
Data availability statement
The datasets presented in this article are not readily available because the data collected for this study is confidential. Requests to access the datasets should be directed to ZL, emhpbGlubGl1QHRzaW5naHVhLmVkdS5jbg==.
Ethics statement
This study does not involve medical experiments. Ethical approval for the survey was obtained from the Ethics Committee of the School of Public Policy and Management, Tsinghua University. Informed, oral consent was obtained from all survey participants. Written consent for participation was not required for this study in accordance with national legislation and the institutional requirement.
Author contributions
XW, PZ, and ZL: study conception, design, and analysis and interpretation of data. XW and ZL: acquisition of data. XW and PZ: drafting of manuscript. PZ and ZL: critical revision. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the National Natural Science Foundation of China under Grant Number 41901185 and 4207120. This research also received support from the Shenzhen Science and Technology Innovation Commission under Grant number GXWD20201230155427003-20200821180448001, and the Startup Foundation for High-Level Talents of Harbin Institute of Technology (Shenzhen).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lecerof SS, Stafström M, Westerling R, Östergren P-O. Does social capital protect mental health among migrants in Sweden? Health Promot Int. (2016) 31:644–52. doi: 10.1093/heapro/dav048
2. Wolffers I, Verghis S, Marin M. Migration, human rights, and health. Lancet. (2003) 362:2019–20. doi: 10.1016/S0140-6736(03)15026-X
3. Chen J, Chen S. Mental health effects of perceived living environment and neighborhood safety in urbanizing China. Habitat Int. (2015) 46:101–10. doi: 10.1016/j.habitatint.2014.11.002
4. Daoud N, Haque N, Gao M, Nisenbaum R, Muntaner C, O'Campo P. Neighborhood settings, types of social capital and depression among immigrants in Toronto. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:529–38. doi: 10.1007/s00127-016-1173-z
5. Li J, Liu Z. Housing stress and mental health of migrant populations in urban China. Cities. (2018) 81:172–9. doi: 10.1016/j.cities.2018.04.006
6. Ma Z, Xia Y. Acculturation strategies, age at migration, and self-rated health: an empirical study on internal migrants in China. Soc Sci Res. (2021) 93:102487. doi: 10.1016/j.ssresearch.2020.102487
7. Chiswick BR, Lee YEWL, Miller PW. Immigrant selection systems and immigrant health. Contemp Econ Policy. (2008) 26:555–78. doi: 10.1111/j.1465-7287.2008.00099.x
8. Urquia ML, O'Campo PJ, Heaman MI. Revisiting the immigrant paradox in reproductive health: the roles of duration of residence and ethnicity. Soc Sci Med. (2012) 74:1610–21. doi: 10.1016/j.socscimed.2012.02.013
9. Carpiano RM. Toward a neighborhood resource-based theory of social capital for health: Can Bourdieu and sociology help? Soc Sci Med. (2006) 62:165–75. doi: 10.1016/j.socscimed.2005.05.020
10. Fraser T, Naquin N. Better together? The role of social capital in urban social vulnerability. Habitat Int. (2022) 124:102561. doi: 10.1016/j.habitatint.2022.102561
11. Liu Y, Zhang F, Liu Y, Li Z, Wu F. The effect of neighbourhood social ties on migrants' subjective wellbeing in Chinese cities. Habitat Int. (2017) 66:86–94. doi: 10.1016/j.habitatint.2017.05.011
12. Carpiano RM. Neighborhood social capital and adult health: an empirical test of a Bourdieu-based model. Health Place. (2007) 13:639–55. doi: 10.1016/j.healthplace.2006.09.001
13. Hays RA, Kogl AM. Neighborhood attachment, social capital building, and political participation: a case study of low-and moderate-income residents of Waterloo, Iowa. J Urban Aff. (2007) 29:181–205. doi: 10.1111/j.1467-9906.2007.00333.x
14. Manturuk K, Lindblad M, Quercia R. Friends and neighbors: Homeownership and social capital among low- to moderate-income families. J Urban Aff. (2010) 32:471–88. doi: 10.1111/j.1467-9906.2010.00494.x
15. Villalonga-Olives E, Kawachi I. The dark side of social capital: a systematic review of the negative health effects of social capital. Soc Sci Med. (2017) 194:105–27. doi: 10.1016/j.socscimed.2017.10.020
16. Bi L, Fan Y, Gao M, Lee CL, Yin G. Spatial mismatch, enclave effects and employment outcomes for rural migrant workers: empirical evidence from Yunnan Province, China. Habitat Int. (2019) 86:48–60. doi: 10.1016/j.habitatint.2019.02.008
17. Lin S, Gaubatz P. Socio-spatial segregation in China and migrants' everyday life experiences: the case of Wenzhou. Urban Geogr. (2017) 38:1019–38. doi: 10.1080/02723638.2016.1182287
18. Liu Y, Li Z, Breitung W. The social networks of new-generation migrants in China's urbanized villages: a case study of Guangzhou. Habitat Int. (2012) 36:192–200. doi: 10.1016/j.habitatint.2011.08.008
19. Liu Z, Wang Y, Tao R. Social Capital and migrant housing experiences in urban China: a structural equation modeling analysis. Hous Stud. (2013) 28:1155–74. doi: 10.1080/02673037.2013.818620
20. Liu Z. Supporting or dragging? effects of neighbourhood social ties on social integration of rural-to-urban migrants in China. Hous Stud. (2019) 34:1–18. doi: 10.1080/02673037.2019.1577955
21. Jin L, Wen M, Fan JX, Wang G. Trans-local ties, local ties and psychological well-being among rural-to-urban migrants in Shanghai. Soc Sci Med. (2012) 75:288–96. doi: 10.1016/j.socscimed.2012.03.014
22. Pan SW, Carpiano RM. Immigrant density, sense of community belonging, and suicidal ideation among racial minority and white immigrants in Canada. J Immigr Minor Heal. (2013) 15:34–42. doi: 10.1007/s10903-012-9657-8
23. Liu Z, Tan Y, Chai Y. Neighbourhood-scale public spaces, inter-group attitudes and migrant integration in Beijing, China. Urban Stud. (2020) 57:2491–509. doi: 10.1177/0042098019879376
24. Fajth V, Bilgili Ö. Beyond the isolation thesis: exploring the links between residential concentration and immigrant integration in the Netherlands. J Ethn Migr Stud. (2020) 46:3252–76. doi: 10.1080/1369183X.2018.1544067
25. Li J, Rose N. Urban social exclusion and mental health of China's rural-urban migrants – a review and call for research. Heal Place. (2017) 48:20–30. doi: 10.1016/j.healthplace.2017.08.009
26. Wen M, Fan J, Jin L, Wang G. Neighborhood effects on health among migrants and natives in Shanghai, China. Health Place. (2010) 16:452–60. doi: 10.1016/j.healthplace.2009.12.001
27. Xiao Y, Miao S, Sarkar C. Social ties, spatial migration paradigm, and mental health among two generations of migrants in China. Popul Space Place. (2021) 27:1–16. doi: 10.1002/psp.2389
28. China NB. National Bulletin of Economic and Social Development of China 2019. Beijing: National Bureau of Statistics (2019).
29. Hou B, Nazroo J, Banks J, Marshall A. Impacts of migration on health and well-being in later life in China: Evidence from the China Health and Retirement Longitudinal Study (CHARLS). Health Place. (2019) 58:102073. doi: 10.1016/j.healthplace.2019.01.003
30. Zhong BL, Liu TB, Chan SSM, Jin D, Hu CY, Dai J, et al. Common mental health problems in rural-to-urban migrant workers in Shenzhen, China: prevalence and risk factors. Epidemiol Psychiatr Sci. (2018) 27:256–65. doi: 10.1017/S2045796016001141
31. Liu T, Shi Q. Acquiring a beijing hukou : who is eligible and who is successful? China Q. (2020) 243:855–68. doi: 10.1017/S0305741019001541
32. Chan KW. The Chinese hukou system at 50. Eurasian Geogr Econ. (2009) 50:197–221. doi: 10.2747/1539-7216.50.2.197
33. Chan KW. The household registration system and migrant labor in China: notes on a debate. Popul Dev Rev. (2010) 36:357–64. doi: 10.1111/j.1728-4457.2010.00333.x
34. Wu W, Wang G. Together but unequal: citizenship rights for migrants and locals in urban China. Urban Aff Rev. (2014) 50:781–805. doi: 10.1177/1078087413518172
35. Zhou J, Lin L, Tang S, Zhang S. To settle but not convert hukou among rural migrants in urban China: How does family-level eligibility for citizenship benefits matter? Habitat Int. (2022) 120:102511. doi: 10.1016/j.habitatint.2022.102511
36. Orum AM, Bata S, Shumei L, Jiewei T, Yang S, Trung NT. Public man and public space in Shanghai today. City Community. (2009) 8:369–89. doi: 10.1111/j.1540-6040.2009.01298.x
37. Wang X, Liu Z. Neighborhood environments and inclusive cities: an empirical study of local residents' attitudes toward migrant social integration in Beijing, China. Landsc Urban Plan. (2022) 226:104495. doi: 10.1016/j.landurbplan.2022.104495
38. Kawachi I. Social Ties and Mental Health. J Urban Heal Bull New York Acad Med. (2001) 78:458–67. doi: 10.1093/jurban/78.3.458
39. Bourdieu P. The Forms of Capital. Dans: Handbook of Theory and Research for the Sociology of Education. New York: Greenwood (1986), p. 241–58.
40. Coleman JS. Social capital in the creation of human capital. Am J Sociol. (1988) 94:S95–120. doi: 10.1086/228943
41. Putnam RD. Making Democracy Work: Civic Traditions in Modern Italy. Princeton, N.J: Princeton University Press (1993).
42. Putnam RD. Bowling Alone: the Collapse and Revival of American Community. New York: New York : Simon and Schuster (2000).
43. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
44. Carpiano RM, Fitterer LM. Questions of trust in health research on social capital: what aspects of personal network social capital do they measure? Soc Sci Med. (2014) 116:225–34. doi: 10.1016/j.socscimed.2014.03.017
45. Ziersch AM, Baum FE, MacDougall C, Putland C. Neighbourhood life and social capital: THE implications for health. Soc Sci Med. (2005) 60:71–86. doi: 10.1016/j.socscimed.2004.04.027
46. Gale CR, Dennison EM, Cooper C, Sayer AA. Neighbourhood environment and positive mental health in older people: the hertfordshire cohort study. Health Place. (2011) 17:867–74. doi: 10.1016/j.healthplace.2011.05.003
47. Chadwick KA, Collins PA. Examining the relationship between social support availability, urban center size, and self-perceived mental health of recent immigrants to Canada: a mixed-methods analysis. Soc Sci Med. (2015) 128:220–30. doi: 10.1016/j.socscimed.2015.01.036
48. O'Campo P, Salmon C, Burke J. Neighbourhoods and mental well-being: what are the pathways? Health Place. (2009) 15:56–68. doi: 10.1016/j.healthplace.2008.02.004
49. Wutich A, Ruth A, Brewis A, Boone C. Stigmatized neighborhoods, social bonding, and health. Med Anthropol Q. (2014) 28:556–77. doi: 10.1111/maq.12124
50. Wang WW, Fan CC. Migrant workers' integration in Urban China: experiences in employment, social adaptation, and self-identity. Eurasian Geogr Econ. (2012) 53:731–49. doi: 10.2747/1539-7216.53.6.731
51. Du H, Li S, Hao P. ‘Anyway, you are an outsider': Temporary migrants in urban China. Urban Stud. (2017) 55:3185–201. doi: 10.1177/0042098017691464
52. Wang YP, Wang Y, Wu J. Housing migrant workers in rapidly urbanizing regions: a study of the chinese model in Shenzhen. Hous Stud. (2010) 25:83–100. doi: 10.1080/02673030903362019
53. Lao X, Zhao Z, Gu H. Revisiting hukou transfer intentions among floating population in chinese cities: spatial differences and multi-level determinants. SAGE Open. (2022) 12:215824402210979. doi: 10.1177/21582440221097926
54. Gu H, Ling Y, Shen T, Yang L. How does rural homestead influence the hukou transfer intention of rural-urban migrants in China? Habitat Int. (2020) 105:102267. doi: 10.1016/j.habitatint.2020.102267
55. Xin L, Hengyu G, Qiang G, Guoju A, Junhui W. Unraveling the geography of intercity flows of migrants' hukou conversion intentions: a spatial econometric origin-destination flow analysis. J Urban Plan Dev. (2022) 148:5022032. doi: 10.1061/(ASCE)UP.1943-5444.0000875
56. Curley AM. Draining or gaining? The social networks of public housing movers in Boston. J Soc Pers Relat. (2009) 26:227–47. doi: 10.1177/0265407509106716
58. Wang R, Xue D, Liu Y, Chen H, Qiu Y. The relationship between urbanization and depression in China: the mediating role of neighborhood social capital. Int J Equity Health. (2018) 17:1–10. doi: 10.1186/s12939-018-0825-x
59. Mulvaney-Day NE, Alegría M, Sribney W. Social cohesion, social support, and health among Latinos in the United States. Soc Sci Med. (2007) 64:477–95. doi: 10.1016/j.socscimed.2006.08.030
60. Pierse N, Carter K, Bierre S, Law D, Howden-Chapman P. Examining the role of tenure, household crowding and housing affordability on psychological distress, using longitudinal data. J Epidemiol Community Heal. (2016) 70:961–6. doi: 10.1136/jech-2015-206716
61. Murayama H, Wakui T, Arami R, Sugawara I, Yoshie S. Contextual effect of different components of social capital on health in a suburban city of the greater Tokyo area: A multilevel analysis. Soc Sci Med. (2012) 75:2472–80. doi: 10.1016/j.socscimed.2012.09.027
62. Forrest R, Yip N-M. Neighbourhood and Neighbouring in Contemporary Guangzhou. J Contemp China. (2007) 16:47–64. doi: 10.1080/10670560601026736
63. Hazelzet A, Wissink B. Neighborhoods, social networks, and trust in post-reform china: the case of Guangzhou. Urban Geogr. (2012) 33:204–20. doi: 10.2747/0272-3638.33.2.204
64. Wang Z, Zhang F, Wu F. Social trust between rural migrants and urban locals in China - exploring the effects of residential diversity and neighbourhood deprivation. Popul Space Place. (2017) 23:e2008. doi: 10.1002/psp.2008
65. Wang Z, Zhang F, Wu F. Affective neighbourly relations between migrant and local residents in Shanghai. Urban Geogr. (2017) 38:1182–202. doi: 10.1080/02723638.2016.1206700
66. Knight J, Gunatilaka R. Great expectations? the subjective well-being of rural-urban migrants in China. World Dev. (2010) 38:113–24. doi: 10.1016/j.worlddev.2009.03.002
Keywords: mental health, neighborhood social capital, hukou, migrants, China
Citation: Wang X, Zhou P and Liu Z (2022) Neighborhood social capital and self-rated mental health: Disparities between migrants and native residents in Beijing. Front. Public Health 10:1055712. doi: 10.3389/fpubh.2022.1055712
Received: 28 September 2022; Accepted: 31 October 2022;
Published: 18 November 2022.
Edited by:
Linchuan Yang, Southwest Jiaotong University, ChinaReviewed by:
Hengyu Gu, The Chinese University of Hong Kong, Hong Kong SAR, ChinaZhuolin Tao, Beijing Normal University, China
Copyright © 2022 Wang, Zhou and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peiling Zhou, emhvdXBlaWxpbmdAaGl0LmVkdS5jbg==
 Xiaomeng Wang
Xiaomeng Wang Peiling Zhou
Peiling Zhou Zhilin Liu
Zhilin Liu