
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 05 December 2022
Sec. Aging and Public Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1055699
This article is part of the Research Topic Innovations in Older Adult Care and Health Service Management: A Focus on the Asia-Pacific Region View all 15 articles
Objectives: The purpose of this study was to assess the bidirectional association between multimorbidity (MM) and functional disability among middle-aged and older adults in a longitudinal study in Thailand.
Methods: We analyzed longitudinal data of participants aged 45 years and older from two consecutive waves (in 2015 and 2017) of the Health, Aging, and Retirement in Thailand (HART). Functional disability was assessed with a 4-item activity of daily living (ADL) scale. Logistic regression analysis was conducted to assess the association between baseline functional disability and incident MM (≥2), and baseline morbidity and incident functional disability.
Results: The results indicate that a total of 1,716 individuals without morbidity at baseline and 3,529 without functional disability at baseline were included. At follow-up, 16.7 and 20.0% of functional disability cases and 7.1 and 3.6% of nonfunctional disability cases developed 2 morbidities and 3 or more morbidities, respectively, and 6.6% of MM cases and 4.0% of non-MM cases developed a functional disability. In the final logistic regression model adjusted for education, income, age, marital status, sex, smoking tobacco, body mass index (BMI), alcohol use, physical activity, and social engagement, functional disability at baseline was positively associated with incident MM (≥2) (adjusted odds ratio [aOR]: 2.58, 95% CI: 1.42–4.72), and MM (≥3) at baseline was positively associated with incident functional disability (aOR: 1.97, 95% CI: 1.13–3.43).
Conclusion: Multimorbidity and functional disability were bidirectionally associated.
There has been a demographic and epidemiological transition that has increased aging and chronic noncommunicable diseases in low- and middle-income countries (LMICs) (1) such as Thailand (2–5). This may include multimorbidity (MM) (co-existence of ≥2 chronic conditions) and functional disability in LMICs, including Thailand, which are an increasing burden on the healthcare systems (6–13). In a study among aging adults in six LMICs (i.e., China, India, Ghana, South Africa, Mexico, and Russia), the prevalence of MM was 45.5% (based on conditions: “angina, arthritis, asthma, chronic back pain, chronic lung disease, diabetes, edentulism, hearing problems, hypertension, stroke, visual impairment”) (14), and among older adults (≥50 years) in the six LMICs, the prevalence of MM (based on “arthritis, stroke, angina, diabetes, chronic lung disease, asthma, and hypertension”) was 17.4% in China, 25.2% in India, 16.6% in Ghana, 23.4% in South Africa, 45.3% in Mexico, and 23.6% in Russia (15). In a small community-based study among older adults (≥60 years) in southern Thailand, the prevalence of MM was 16.8% (16) and in national surveys, among older adults (≥60 years) in 2007 the prevalence of MM was 14.7% (“hypertension, heart disease, diabetes, cancer, stroke, and paralysis”) (17) and in 2018, 30.4% (MM: “cancer, diabetes, hypertension, stroke, asthma, or another self-named chronic disease) (18).
According to the World Health Organization (19), 15% of the global population is estimated to be disabled in 2011 (19). Among older adults (≥50 years) in the six LMICs, the prevalence of functional disability (1+ activities of daily living [ADLs] limitation) ranged from 16.2% in China to 55.7% in India (15). In a national survey among people aged 60 years and older in Thailand in 1997, the prevalence of long-term disability was 19% (20). Among older adults (60 years) in Thailand in 2011, 2.7% had difficulty with the ADL item dressing and 2.2% with eating (21); in 2014 and 2017, 7.6% had difficulty with at least one (of 8) ADL item (22, 23). In a small study in rural Thailand, the prevalence of severe disability among older adults was 11.9% (24).
Multimorbidity is implicated in various negative health outcomes, such as increased mental morbidity, disability, increased healthcare utilization, adverse drug events, and death (7, 25–27). Similarly, functional disability is associated with increased hospitalization (28), poor self-rated quality of life (29), and mortality (30, 31). Previous studies have shown that demographic factors, such as older age and female sex (32), lower socioeconomic status (6, 9), and lifestyle factors, such as smoking (33), alcohol use (32, 33), physical inactivity (32, 34), body weight status and obesity (32, 35), and lack of social engagement (36, 37) were associated with MM. Furthermore, demographic factors, such as older age (15, 29) and female sex (29, 38, 39), lower socioeconomic status (38, 40), lifestyle factors, such as smoking (41), alcohol use (42), physical inactivity (40, 43, 44), body weight status and obesity (40, 41), low social capital (15) and low social interaction (44) were associated with functional disability.
Most studies have investigated MM and incident functional disability (45–48), but few studies have investigated functional disability and incident MM, and bidirectional associations between MM and functional disability (7, 49). A study on the bidirectional association between MM and functional disability among older adults in China (including the chronic conditions: “hypertension, diabetes, cancer, chronic lung disease, cardiovascular disease, emotional or psychiatric disease, stomach or other digestive diseases, arthritis or rheumatism, kidney disease, liver disease, memory-related disease, and asthma”) and Europe (including 9 diseases: “hypertension, diabetes, cancer, chronic lung disease, cardiovascular disease, emotional of psychiatric disease, stomach or duodenal ulcer, and arthritis or rheumatism”) (7) found that across 2 longitudinal studies, functional disability and MM were bidirectionally associated. In the China (CHARLS) and Europe (SHARE) study, nationally representative cohorts were followed from 2011 to 2015, showing that participants with ADL/IADL disability at baseline were at a higher risk of developing MM and people with MM at baseline were at a higher risk of developing ADL/IADL disability in a dose-response fashion (7). Several longitudinal studies have investigated the determinants of MM and functional disability separately (49, 50), rather than studying both simultaneously (49). It is suggested that shared modifiable risk for both MM and functional disability exist, which should be further investigated (49).
To gain better knowledge of the association between MM and functional disability in Southeast Asia, the aim of this study was to assess the bidirectional association between MM and functional disability among middle-aged and older adults in a longitudinal study in Thailand. In particular, the study had two objectives, namely, (1) to estimate the association between functional disability at baseline and incident MM and (2) to estimate the association between morbidity counts at baseline and incident functional disability.
This study analyzed longitudinal data from two consecutive waves (2015 and 2017) of the Health, Aging, and Retirement in Thailand (HART). In a national sample from five regions and Bangkok and its vicinity, one adult (≥45 years) per household was randomly selected using a multistage sampling design [refer to (51) for further details]. The 2015 (N = 5,616) and 2017 surveys included 3,708 members of the 2015 HART cohort (92 died during a follow-up or 4.3% of the baseline respondents were in the study area; 1,554 moved away from the study area; 270 declined participation; and the response rate: 72.3% and the retention rate: 66.03%). A total of 3,708 participants who responded to the 2015 and 2017 surveys were included in the study, and 3,646 had complete information on our variables of interest (MM and functional disability). Participants were interviewed at their homes by trained field workers using the paper-and-pencil (PAPI) questionnaire in wave 1 and computer-assisted personal interviewing (CAPI) in wave 2.
Chronic physical conditions were evaluated by self-reported healthcare provider diagnosed conditions, including hypertension, diabetes, lung diseases, emphysema, cardiovascular diseases, heart disease, heart failure, rheumatism, arthritis, bone diseases, low bone density, osteoporosis, kidney diseases, cancer, liver diseases, emotional/nervous or psychiatric disease, brain diseases, Alzheimer's disease, and visual and hearing impairment. MM was defined as having two or more chronic diseases, and non-MM as having none or one physical chronic disease.
Functional disability was measured based on a 4-item (eating, bathing, dressing, and washing) modified ADL index (52). Responses ranged from 0 = “able to do it all by myself” to 3 = “need help for all steps.” Functional disability was defined as any of the four items not being able to do all by themselves (Cronbach's α = 0.94 at wave 1 and 0.90 at wave 2).
Sociodemographic data included educational level, sex, age, marital status, and income quartile. Education was grouped into (1) no formal education, (2) elementary school, and (3) more than elementary school (middle school, high school, vocational diploma or 2-year diploma degree, bachelor's degree, or higher than bachelor's degree). “The income quartile was calculated based on annual income from employment, own business, agricultural/livestock/fishing business, short-term or contract work, financial support from family, remuneration/pension income from the government fund, occupational pension fund, private pension fund, social security/welfare income, income e from government living allowance, veteran's welfare benefit, other welfare assistance income, and income from other sources, into four groups 1 = 0 to <13,000 Thai Baht, 2 = 13,000 to <50,000, 3 = 50,000 to <140,000, 4 = ≥140,000 Thai Baht (Average exchange rate in 2015: 1 US=34.2 Baht)” (53).
Tobacco smoking was sourced from the item, “Have you ever smoked cigarettes?” (response options: “1 = yes, and still smoke now, 2 = yes, but quit smoking, and 3 = never”).
Alcohol use was assessed with the question, “Have you ever drunk alcoholic beverages such as liquor, beer, or wine?” (response options: 1 = yes, and still drinking now, 2 = yes, but do not drink now, and 3 = never).
Past week physical activity or exercise (frequency: “How often do you exercise?” (days a week) and duration of any type: “On the day you exercise, how long do you exercise?” (minutes) (54)) was grouped into “none = inactivity, 1–149 min/week = low activity, and ≥150 min/week = high activity.” (55).
Body mass index (BMI) was based on self-reported body weight and height and was classified using Asian cutoff criteria into “underweight (<18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), and obesity (25+ kg/m2)” (56).
Social engagement included six items of formal and one item of informal social engagement (defined as at least one activity in the past month) (53, 57). Formal social engagement included religious, occupational, and cultural organizations; alumni or parent association or association of people from the same hometown; volunteer; and political organizations. Responses were coded as “1 = daily to at least once a month” and “0 = once a year or never.” Informal social engagement was determined with the following questions: (1) “In the past year, do you have any close friends or relatives who live nearby and have a close relationship with? (Please refer to the only person whom you meet most often)” and (2) “If so, how often do you meet with them in person (number of times per day, week, month, year, other, never)?” Informal social engagement was defined as “1 = having a close friend or relative who lives nearby and have a close relationship with and having met that person at least in the past 1 month” and “0 = not having a close friend or relative or meeting a close friend less than once a month in the past year” (53).
The proportion of older adults with incident MM (those who have MM at wave 2 and are without morbidity at wave 1) and incident functional disability (those who have a functional disability at wave 2 and are without functional disability at wave 1) is presented with frequencies and percentages. Pearson's chi-square tests are used to compare baseline characteristics among groups. The first logistic regression model estimated odds ratios (ORs) and confidence intervals (CIs) between functional disability at baseline and incident MM, and the second model compared morbidity counts at baseline and incident functional disability. Three models are presented for incident MM and incident functional disability. The first model is unadjusted; in the second model, adjustments are made for age, income, sex, education, and marital status, and in the third model, adjustments are made for model 2 variables plus smoking, physical activity, BMI, alcohol use, and social engagement. The selection of covariates is based on a previous review of the literature (6–8, 14, 15, 25, 29, 32–44). A value of p ≤ 0.05 was considered statistically significant. All statistical analyses were performed using StataSE version 15.0 (College Station, TX, USA).
The analytic baseline sample included 3,638 individuals aged 45 years and older. The prevalence of MM was 23.5%, and the prevalence of functional disability was 3.2%. Both MM and functional disability increased with age, decreased with higher education, decreased with higher income, decreased with alcohol use and smoking, and decreased with being married or cohabiting. MM was higher in women than in men but functional disability did not differ by sex. MM increased with increased body weight and functional disability was greater among those with underweight and who were physically inactive. The social engagement did not significantly differ by MM and functional disability (refer to Table 1).
In the first model that estimates incident morbidity, a total of 1,716 individuals without morbidity were included from baseline, with 30 (1.8%) having a functional disability at baseline. At follow-up, 16.7% and 20.0% of functional disability cases and 7.1 and 3.6% of nonfunctional disability cases developed 2 morbidities and 3 or more morbidities, respectively. Middle-aged and older adults with functional disability at baseline had a significantly higher prevalence of morbidity counts at follow-up (p < 0.001). Those with higher incident morbidity counts were likely older, were unmarried, had less income, had no social engagement, and were not currently smoking tobacco or using alcohol than those without or with lower morbidity counts (refer to Table 2).
In the second model that estimates incident functional disability, a total of 3,529 individuals without a functional disability were included from baseline, with 1,115 (30.1%), 607 (16.4%), and 270 (7.3%) having 1, 2, and 3 or more morbidities at baseline. At follow-up, 6.6% of MM cases and 4.0% of non-MM cases developed a functional disability. Furthermore, 3.4% of 0, 4.9% of 1, 5.5% of 2, and 9.4% of 3 or more morbidity cases developed a functional disability. Middle-aged and older adults with physical MM at baseline had a significantly higher prevalence of functional disability at follow-up (p < 0.002), and those with higher morbidity counts at baseline had a significantly higher prevalence of functional disability at follow-up (p < 0.001). Those with incident functional disability were likely to be older, had lower education, were unmarried, had lower income, were not currently using alcohol, were less physically active, and were more likely underweight than those without functional disability (refer to Table 3).
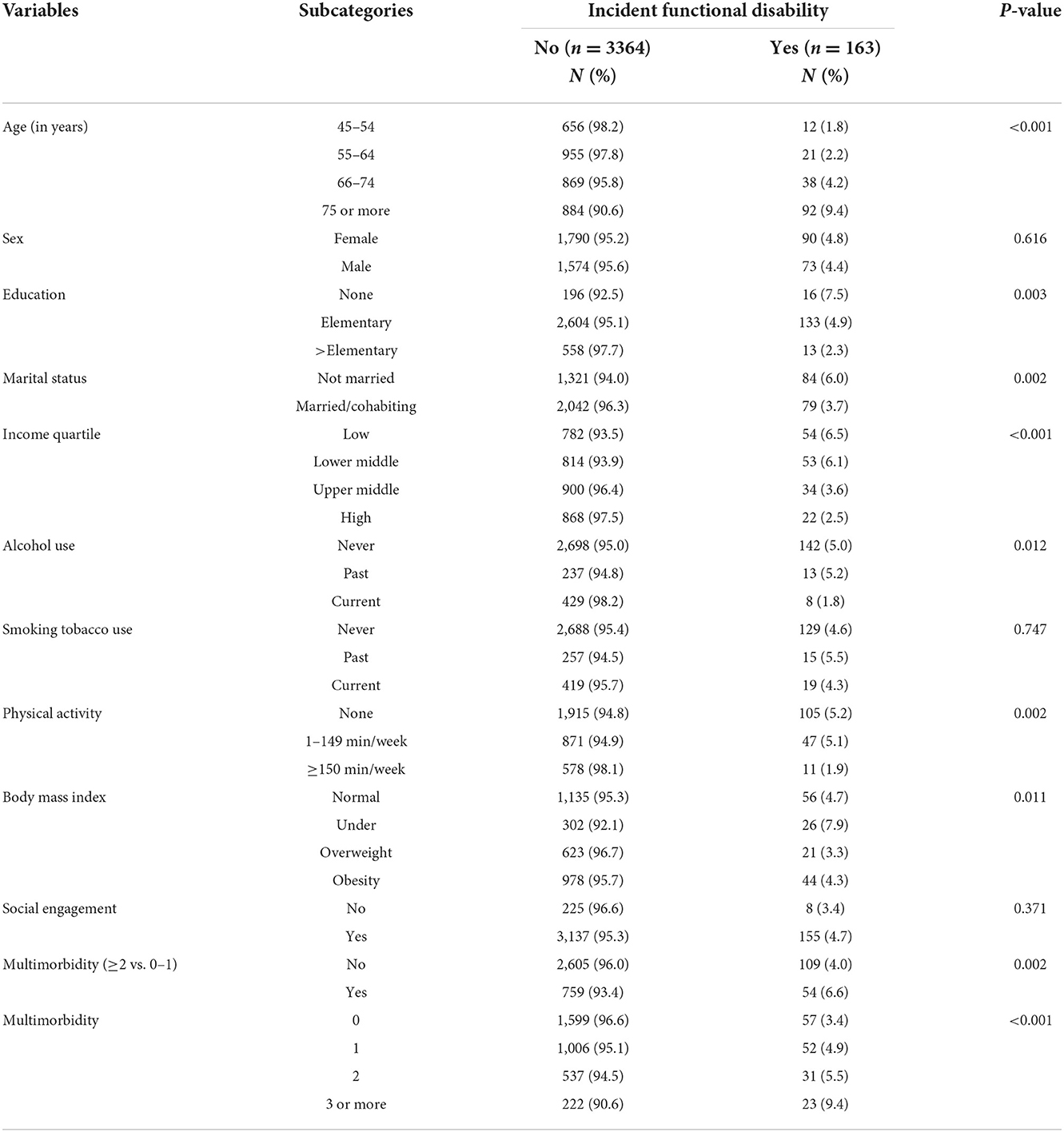
Table 3. Sample characteristics of participants with incident functional disability, Thailand, 2015–2017.
In the final logistic regression model adjusted for education, income, age, marital status, sex, smoking tobacco, BMI, alcohol use, physical activity, and social engagement, functional disability at baseline was positively associated with incident MM (≥2) (adjusted OR [aOR]: 2.58, 95% CI: 1.42–4.72), and MM (≥3) at baseline was positively associated with incident functional disability (aOR: 1.97, 95% CI: 1.13–3.43) (refer to Table 4).
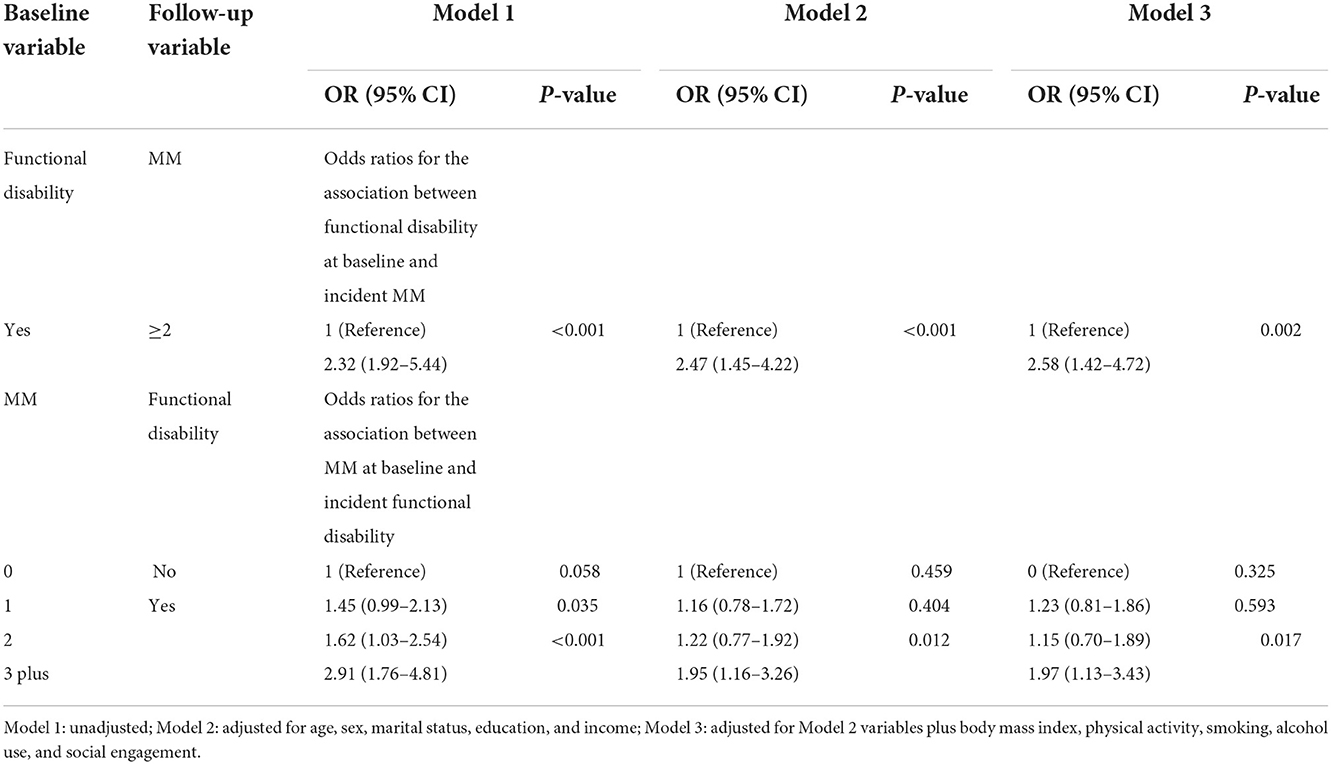
Table 4. Odds ratios for bidirectional associations between functional disability and multimorbidity (MM).
The first longitudinal study investigates the bidirectional associations between MM and functional disability in Southeast Asia. Consistent with two studies in China and Europe (7), we found that MM (hypertension, diabetes, lung diseases, emphysema, cardiovascular diseases, heart diseases, heart failure, rheumatism, arthritis, bone diseases, low bone density, osteoporosis, kidney diseases, cancer, liver diseases, emotional/nervous or psychiatric diseases, brain diseases, Alzheimer's disease, and visual and hearing impairment) and functional disability were bidirectionally associated with middle-aged and older adults in Thailand. These associations were independent of BMI, sex, marital status, age, education, income, smoking, physical activity, alcohol use, and social engagement.
We found some differences between the present study and the two previous studies (CHARLS and SHARE), namely, the associations between baseline functional disability and incident MM, and the associations between baseline MM and incident functional disability were weaker in this study than in CHARLS and SHARE (7). We believe that the major contributor to this difference was due to the significantly lower sample size in our study compared to CHARLS and SHARE, which includes a shorter follow-up period (2 years) compared to the CHARLS and SHARE study (4 years). In addition, although the type and number of morbidities and covariates assessed in this study were similar to CHARLS and SHARE, covariates in our study may have had a differential effect. For example, after including all covariates in the model, the effect of MM (3+) on functional disability was reduced from 2.9 to 2.0.
In a systematic review, the main consequences of MM were disability and functional decline (48), which may occur due to damage in multiple organs and systems (7, 58). Conversely, older adults with a functional disability may engage in less health behavior, such as physical activity, are less likely to access and adhere to medical care independently, have a higher BMI, and experience more psychological distress than those without functional disability (7). Another possibility is that specific mechanisms of biological aging influence both MM and functional disability. For example, physical inactivity increases both MM and functional disability (49). This leaves the question of possible shared modifiable risk factors for both functional disability and MM, which is subject to further research.
This study found among individuals aged 45 years and older, a prevalence of MM of 23.5%, which is higher than in a study among older adults (≥60 years) in southern Thailand (16.8%) (16) and in a national survey among older adults (≥60 years) in Thailand (14.7%) (17). The lower rate of MM in the latter study may be attributed to fewer morbidities (six) included in the survey (17). The prevalence of MM (23.5%) was higher than in China (17.4%) and Ghana (16.6%), similar to South Africa (23.4%) and Russia (23.6%), lower than in India (25.2%) and Mexico (45.3%) (15), and much lower than among predominantly older adults from six LMICs (45.5%) (14). Reasons for some of these differences are attributable to the different number of morbidities included; for example, in the six-country study, a lower prevalence of MM was found with fewer conditions, and in the same study, a higher prevalence was found with a higher number of MM (e.g., the inclusion of vision and hearing impairment). Moreover, a higher morbidity rate may be related to the symptom-based and physical measurements of morbidities, while our study relied only on self-reported healthcare provider diagnosed morbidities.
Furthermore, this study found among individuals aged 45 years and older, a prevalence of functional disability of 3.2% (4.3% of individuals aged 60 years and older), which is lower than in two national surveys in Thailand in 2014 and 2017 (7.6%) (22, 23). A major reason for the almost double higher prevalence of functional disability in these two latter surveys compared to our study may be attributed to the difference in the number of items of the functional disability measure (our study only used 4 items, while the two surveys reported here used 8 items). Measuring functional disability with more items increases the likelihood of finding more functional limitations. Compared to these prevalence rates of functional disability in Thailand (<10%), much higher rates were found among older adults (≥50 years) in the six LMICs, namely, China (16.2%), India (55.7%), Ghana (44.0%), South Africa (38.6%), Mexico (38.8%), and Russia (43.1%) (15).
Furthermore, we found that consistent with previous research (6, 9, 15, 29, 32, 38, 40), both MM and functional disability increased with age, decreased with higher education, and decreased with higher income. In line with previous studies (32), the prevalence of MM was higher in women than in men, while functional disability did not differ by sex, as found previously (29, 38, 39). The prevalence of MM and functional disability was higher among those who were physically inactive, which is consistent with previous research (32, 34, 40, 43, 44). Consistent with previous studies (32, 35), MM was higher among those with a higher BMI (obesity) and consistent with a study in India (59), underweight was higher among those with functional disabilities. Furthermore, we found that past smoking and past alcohol use were higher among those with MM and functional disability, meaning that individuals with MM and/or functional disability may have stopped smoking and/or alcohol use. Contrary to some previous research (15, 36, 37, 44), we did not find that MM and functional disability decreased social engagement. This result may be related to the overall very high prevalence of social engagement (>93%), and a stricter measure of social engagement could have produced different results.
The study used a national cohort study with large sample size and adjusted for various confounding social, health, and demographic factors. Study limitations include that MM was assessed by self-reported diagnosed chronic conditions, and functional disability was only measured with a modified shorter version of the ADL scale. We could have distinguished between milder and more severe functional disabilities due to the small sample sizes. Moreover, this study had a 2-year follow-up period, hindering us from measuring long-term associations.
Baseline MM (≥3) increases the risk of incident functional disability and baseline functional disability increases the risk of incident MM (≥2) among middle-aged and older adults in Thailand. Given these findings, health services should be reoriented to tailor interventions to people with MM to prevent and control future functional disabilities, and interventions targeting people with functional disabilities may help prevent and control MM in middle and late adulthood in Thailand.
Publicly available datasets were analyzed in this study. This data can be found here: Data is publicly available at Gateway to Global Aging Data, Health, Aging, and Retirement in Thailand: https://g2aging.org/?section=study&studyid=44.
The studies involving human participants were reviewed and approved by Ethics Committee in Human Research, National Institute of Development Administration—ECNIDA (ECNIDA 2020/00012). The patients/participants provided their written informed consent to participate in this study.
SP, KP, and DA contributed to the design, implementation of the research, and wrote the manuscript. KP analyzed the results. All authors contributed to the article and approved the submitted version.
The Health, Aging, and Retirement in Thailand (HART) study is sponsored by the Thailand Science Research and Innovation (TSRI) and the National Research Council of Thailand (NRCT).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. National National Institute on Aging National National Institutes of Health (2011). Global Health and Ageing. NIH Publication no. 11-7737. Available online at: file:///C:/Users/user/Downloads/global_health.pdf (accessed on December 5, 2021).
2. Anantanasuwong D. Population ageing in Thailand: critical issues in the twenty-first century. In: Narot P, Kiettikunwong N, (eds.) Education for the Elderly in the Asia Pacific, Education in the Asia-Pacific Region: Issues, Concerns and Prospects. (2021). p. 59.
3. Prasartkul P, Thaweesit S, Chuanwan S. Prospects and contexts of demographic transitions in Thailand. JPSS. (2019) 27:1–22. doi: 10.25133/JPSSv27n1.001
4. Kaufman ND, Chasombat S, Tanomsingh S, Rajataramya B, Potempa K. Public health in Thailand: emerging focus on non-communicable diseases. Int J Health Plann Manage. (2011) 26:e197–212. doi: 10.1002/hpm.1078
5. Senanarong V, Harnphadungkit K, Poungvarin N, Vannasaeng S, Chongwisal S, Chakorn T, et al. The dementia and disability project in Thai elderly: rational, design, methodology and early results. BMC Neurol. (2013) 13:3. doi: 10.1186/1471-2377-13-3
6. Arokiasamy P, Uttamacharya U, Jain K, Biritwum RB, Yawson AE, Wu F, et al. The impact of multimorbidity on adult physical and mental health in low- and middle-income countries: what does the study on global ageing and adult health (SAGE) reveal? BMC Med. (2015) 13:178. doi: 10.1186/s12916-015-0402-8
7. Qiao Y, Liu S, Li G, Lu Y, Wu Y, Shen Y, et al. Longitudinal follow-up studies on the bidirectional association between ADL/IADL disability and multimorbidity: results from two national sample cohorts of middle-aged and elderly adults. Gerontology. (2021) 67:563–71. doi: 10.1159/000513930
8. Pati S, Swain S, Knottnerus JA, Metsemakers JFM, van den Akker M. Magnitude and determinants of multimorbidity and health care utilization among patients attending public versus private primary care: a cross-sectional study from Odisha, India. Int J Equity Health. (2020) 19:57. doi: 10.1186/s12939-020-01170-y
9. Pengpid S, Peltzer K. Multimorbidity in chronic conditions: public primary care patients in four greater Mekong Countries. Int J Environ Res Public Health. (2017) 14:1019. doi: 10.3390/ijerph14091019
10. Pengpid S, Peltzer K. Chronic conditions, multimorbidity, and quality of life among patients attending monk healers and primary care clinics in Thailand. Health Qual Life Outcomes. (2021) 19:61. doi: 10.1186/s12955-021-01707-x
11. Limpawattana P, Theeranut A, Chindaprasirt J, Sawanyawisuth K, Pimporm J. Caregivers burden of older adults with chronic illnesses in the community: a cross-sectional study. J Commun Health. (2013) 38:40–5. doi: 10.1007/s10900-012-9576-6
12. Chiaranai C, Chularee S, Srithongluang S. Older people living with chronic illness. Geriatr Nurs. (2018) 39:513–20. doi: 10.1016/j.gerinurse.2018.02.004
13. Yiengprugsawan V, Healy J, Kendig H, Neelamegam M, Karunapema P, Kasemsup V. Reorienting health services to people with chronic health conditions: diabetes and stroke services in Malaysia, Sri Lanka and Thailand. Health Syst Reform. (2017) 3:171–81. doi: 10.1080/23288604.2017.1356428
14. Vancampfort D, Stubbs B, Koyanagi A. Physical chronic conditions, multimorbidity and sedentary behavior amongst middle-aged and older adults in six low- and middle-income countries. Int J Behav Nutr Phys Act. (2017) 14:147. doi: 10.1186/s12966-017-0602-z
15. Lestari SK, Ng N, Kowal P, Santosa A. Diversity in the factors associated with ADL-related disability among older people in six middle-income countries: a cross-country comparison. Int J Environ Res Public Health. (2019) 16:1341. doi: 10.3390/ijerph16081341
16. Sukchan P, Chemoh W, Payanglee K. Morbidity and multi-morbidity among the elderly population in southernmost Thailand: cox proportional hazards regression model of survival approach. PNUJR. (2019) 12:89–105. https://li01.tci-thaijo.org/index.php/pnujr/article/view/213939
17. Haseen F, Adhikari R, Soonthorndhada K. Self-assessed health among Thai elderly. BMC Geriatr. (2010) 10:30. doi: 10.1186/1471-2318-10-30
18. Phulkerd S, Thapsuwan S, Chamratrithirong A, Gray RS. Influence of healthy lifestyle behaviors on life satisfaction in the aging population of Thailand: a national population-based survey. BMC Public Health. (2021) 21:43. doi: 10.1186/s12889-020-10032-9
19. World Health Organization (WHO). World Report on Disability. Geneva, Switzerland: World Health Organization (2011). ISBN 978-92-4 068521-5
20. Jitapunkul S, Kunanusont C, Phoolcharoen W, Suriyawongpaisal P, Ebrahim S. Determining public health priorities for an ageing population: the value of a disability survey. Southeast Asian J Trop Med Public Health. (2003) 34:929–36.
21. Khongboon P, Pongpanich S, Chapman RS. Risk Factors for Six Types of Disability among the Older People in Thailand in 2002, 2007, and 2011. J Aging Res. (2016) 2016:6475029. doi: 10.1155/2016/6475029
22. Knodel J, Teerawichitchainan B, Prachuabmoh V, Pothisiri W. The situation of Thailand's older population: An update based on the 2014 survey of older persons in Thailand. Chiang Mai: Help Age International, East Asia/Pacific Regional Office (2015).
23. Teerawitchitchainan, B., Pothisiri W, Knodel J, Prachuabmoh V (2019). The Situation of Thailand's Older Population: An Update Based on the 2017 Survey. London: HelpAge International.
24. Sihapark S, Kuhirunyaratn P, Chen, H. Severe Disability Among Elderly Community Dwellers in Rural Thailand: Prevalence and Associated Factors. Ageing Int 39, 210–220 (2014). doi: 10.1007/s12126-013-9190-7
25. Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA. Multimorbidity and mortality in older adults: A systematic review and meta-analysis. Arch Gerontol Geriatr. (2016) 67:130–8. doi: 10.1016/j.archger.2016.07.008
26. Pati S, Swain S, Hussain MA, van den Akker M, Metsemakers J, Knottnerus JA, et al. Prevalence and outcomes of multimorbidity in South Asia: a systematic review. BMJ Open. (2015) 5:e007235. doi: 10.1136/bmjopen-2014-007235
27. Salive ME. Multimorbidity in older adults. Epidemiol Rev. (2013) 35:75–83. doi: 10.1093/epirev/mxs009
28. Chen C, Lim JT, Chia NC, Wang L, Tysinger B, Zissimopolous J, et al. The Long-term impact of functional disability on hospitalization spending in Singapore. J Econ Ageing. (2019) 14:100193. doi: 10.1016/j.jeoa.2019.02.002
29. Yau PN, Foo CJ, Cheah NL, Tang KF, Lee SW. The prevalence of functional disability and its impact on older adults in ASEAN region: a systematic review and meta-analysis. Epidemiol Health. (2022) 2022:e2022058. doi: 10.4178/epih.e2022058
30. Forman-Hoffman VL, Ault KL, Anderson WL, Weiner JM, Stevens A, Campbell VA, et al. Disability status, mortality, and leading causes of death in the United States community population. Med Care. (2015) 53:346–54. doi: 10.1097/MLR.0000000000000321
31. Langballe EM, Tangen GG, Engdahl B, Strand BH. Increased mortality risk for adults aged 25-44 years with long-term disability: A prospective cohort study with a 35-year follow-up of 30,080 individuals from 1984-2019 in the population-based HUNT study. Lancet Reg Health Eur. (2022) 22:100482. doi: 10.1016/j.lanepe.2022.100482
32. Kaluvu L, Asogwa OA, Marzà-Florensa A, Kyobutungi C, Levitt NS, Boateng D, et al. Multimorbidity of communicable and non-communicable diseases in low- and middle-income countries: A systematic review. J Multimorb Comorb. (2022) 12:26335565221112593. doi: 10.1177/26335565221112593
33. Mishra VK, Srivastava STM, Murthy PV. Population attributable risk for multimorbidity among adult women in India: Do smoking tobacco, chewing tobacco and consuming alcohol make a difference? PLoS ONE. (2021) 16:e0259578. doi: 10.1371/journal.pone.0259578
34. Vancampfort D, Koyanagi A, Ward PB, Rosenbaum S, Schuch FB, Mugisha J, et al. Chronic physical conditions, multimorbidity and physical activity across 46 low- and middle-income countries. Int J Behav Nutr Phys Act. (2017) 14:6. doi: 10.1186/s12966-017-0463-5
35. Agrawal S, Agrawal PK. Association between body mass index and prevalence of multimorbidity in low-and middle-income countries: a cross-sectional study. Int J Med Public Health. (2016) 6:73–83. doi: 10.5530/ijmedph.2016.2.5
36. Ma R, Romano E, Vancampfort D, Firth J, Stubbs B, Koyanagi A. Physical multimorbidity and social participation in adult aged 65 years and older from six low- and middle-income countries. J Gerontol B Psychol Sci Soc Sci. (2021) 76:1452–62. doi: 10.1093/geronb/gbab056
37. Ronaldson A, Arias de la Torre J, Bendayan R, Yadegarfar ME, Rhead R, Douiri A, et al. Physical multimorbidity, depressive symptoms, and social participation in adults over 50 years of age: findings from the English Longitudinal Study of Ageing. Aging Ment Health. (2022) 2022:1–11. doi: 10.1080/13607863.2021.2017847
38. Hosseinpoor AR, Williams JS, Jann B, Kowal P, Officer A, Posarac A, et al. Social determinants of sex differences in disability among older adults: a multi-country decomposition analysis using the World Health Survey. Int J Equity Health. (2012) 11:52. doi: 10.1186/1475-9276-11-52
39. Zheng PP, Guo ZL, Du XJ, Yang HM, Wang ZJ. Prevalence of Disability among the Chinese Older Population: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. (2022) 19:1656. doi: 10.3390/ijerph19031656
40. Rodrigues MA, Facchini LA, Thumé E, Maia F. Gender and incidence of functional disability in the elderly: a systematic review. Cad Saude Publica. (2009) 25:S464–76. doi: 10.1590/S0102-311X2009001500011
41. Townsend TN, Mehta NK. Contributions of obesity and cigarette smoking to incident disability: a longitudinal analysis. Prev Med. (2020) 141:106226. doi: 10.1016/j.ypmed.2020.106226
42. Dent OF, Grayson DA., Waite LM, Cullen JS, Creasey H, Bennett HP, et al. A longitudinal study of alcohol consumption and functional disability in a community sample of older people. Aust J Ageing. (2000) 19:185–9. doi: 10.1111/j.1741-6612.2000.tb00233.x
43. Heiland EG, Welmer AK, Wang R, Santoni G, Fratiglioni L, Qiu C. Cardiovascular Risk Factors and the Risk of Disability in Older Adults: Variation by Age and Functional Status. J Am Med Dir Assoc. (2019) 20:208–12.e3. doi: 10.1016/j.jamda.2018.05.013
44. Seino S, Nofuji Y, Yokoyama Y, Abe T, Nishi M, Yamashita M, et al. Combined impacts of physical activity, dietary variety, and social interaction on incident functional disability in older Japanese adults. J Epidemiol. (2021). doi: 10.2188/jea.JE20210392
45. Calderón-Larrañaga A, Santoni G, Wang HX, Welmer AK, Rizzuto D, Vetrano DL, et al. Rapidly developing multimorbidity and disability in older adults: does social background matter? J Intern Med. (2018) 283:489–99. doi: 10.1111/joim.12739
46. Marengoni A, von Strauss E, Rizzuto D, Winblad B, Fratiglioni L. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med. (2009) 265:288–95. doi: 10.1111/j.1365-2796.2008.02017.x
47. Sheridan PE, Mair CA, Quiñones AR. Associations between prevalent multimorbidity combinations and prospective disability and self-rated health among older adults in Europe. BMC Geriatr. (2019) 19:198. doi: 10.1186/s12877-019-1214-z
48. Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. (2011) 10:430–9. doi: 10.1016/j.arr.2011.03.003
49. Calderón-Larrañaga A, Vetrano DL, Ferrucci L, Mercer SW, Marengoni A, Onder G, et al. Multimorbidity and functional impairment-bidirectional interplay, synergistic effects and common pathways. J Intern Med. (2019) 285:255–71. doi: 10.1111/joim.12843
50. Ryan A, Wallace E, O'Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. (2015) 13:168. doi: 10.1186/s12955-015-0355-9
51. Anantanasuwong D, Theerawanviwat D, Siripanich P. Panel survey and study on health and aging, and retirement in Thailand. In: Gu D, Dupre M (Eds) Encyclopedia of Gerontology And Population Aging. Cham: Springer (2019).
52. Katz S, Ford AB, Heiple KG, Newill VA. Studies of illness in the aged: Recovery after fracture of the hip. J Gerontol. (1964) 19:285–93. doi: 10.1093/geronj/19.3.285
53. Anantanasuwong D, Pengpid S, Peltzer K. Prevalence and associated factors of successful ageing among people 50 years and older in a national community sample in Thailand. Int J Environ Res Public Health. (2022) 19:10705. doi: 10.3390/ijerph191710705
54. Kim SH, Park S, A. Meta-analysis of the correlates of successful aging in older adults. Res Aging. (2017) 39:657–77. doi: 10.1177/0164027516656040
55. WHO. World Health Organization (WHO) guidelines on physical activity and sedentary behaviour. Licence: CC BY-NC- SA3.0 IGO. (2020). Available online at: file:///C:/Users/user/Downloads/9789240015128-eng%20(2).pdf (accessed July, 21, 2021).
56. Wen CP, David Cheng TY., Tsai SP, Chan HT, Hsu HL, Hsu CC, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. (2009) 12:497–506. doi: 10.1017/S1368980008002802
57. Berkman LF, Sekher TV, Capistrant B, Zheng Y. Social networks, family, and care giving among older adults in India. In: Smith JP, Majmundar M (eds). Aging in Asia: Findings from New and Emerging Data Initiatives. Washington DC: The National Academic Press (2012). p. 261–78.
58. Bi YH, Pei JJ, Hao C, Yao W, Wang HX. The relationship between chronic diseases and depression in middle-aged and older adults: A 4-year follow-up study from the China Health and Retirement Longitudinal Study. J Affect Disord. (2021) 289:160–6. doi: 10.1016/j.jad.2021.04.032
Keywords: multimorbidity, functional disability, longitudinal study, Thailand, bidirectional
Citation: Pengpid S, Peltzer K and Anantanasuwong D (2022) Bidirectional association between functional disability and multimorbidity among middle-aged and older adults in Thailand. Front. Public Health 10:1055699. doi: 10.3389/fpubh.2022.1055699
Received: 28 September 2022; Accepted: 14 November 2022;
Published: 05 December 2022.
Edited by:
Nai Peng Tey, University of Malaya, MalaysiaReviewed by:
Matthew Kelly, Australian National University, AustraliaCopyright © 2022 Pengpid, Peltzer and Anantanasuwong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karl Peltzer, a2ZwZWx0emVyQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.