
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 15 December 2022
Sec. Occupational Health and Safety
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1053703
This article is part of the Research Topic Insights in Occupational Health and Safety: 2022 View all 16 articles
 Ayahito Ito1,2,3*
Ayahito Ito1,2,3* Daisuke Sawamura3*
Daisuke Sawamura3* Shogo Kajimura4
Shogo Kajimura4 Hideki Miyaguchi5
Hideki Miyaguchi5 Haruki Nakamura6
Haruki Nakamura6 Toshiyuki Ishioka7*
Toshiyuki Ishioka7*Introduction: The coronavirus disease of 2019 (COVID-19) has had a severe psychological impact on occupational therapists. Clarifying the mental health status of occupational therapists and its relationship with therapy quality is essential for maintaining the quality of care and patients' quality of life. Therefore, the present study aimed to investigate whether and how mental health problems are related to the quality of occupational therapy.
Methods: A nationwide cross-sectional online survey was conducted during Japan's second national state of emergency (January 2021). A total of 4,418 registered occupational therapists who were members of the Japanese Association of Occupational Therapists participated in this study. After screening for the exclusion criteria, data from 1,966 participants were analyzed.
Results: Path analysis showed that insufficient information provision by the workplace and increased workload were associated with depression, anxiety, and insomnia. Specifically, depression was associated with decreased therapy quality. Furthermore, one's therapy quality showed a strong positive correlation with colleagues' therapy quality.
Discussion: These results demonstrated a direct link between therapists' mental health conditions and therapy quality and suggested that decreased therapy quality might occur at the institutional rather than individual level. A reassessment of the support system and prompt detection and support for professionals with psychological symptoms may be the key to enhancing therapy quality and patients' quality of life. The present results contribute to the understanding of these relationships, considering the current pandemic context for occupational therapists.
The coronavirus disease 2019 (COVID-19) pandemic has had an unprecedented impact on society and is viewed as a global stressor induced by widespread voluntary restrictions and social distancing (1). The psychological effects of the COVID-19 outbreak on medical workers who have been fighting on the frontlines and on the general population have recently been documented (2, 3). The importance of physical and psychological support, such as the provision of precautionary items and information, has been emphasized (4). In this critical situation, medical workers who are directly or indirectly involved in diagnosis or treatment are at risk of developing psychological problems due to changes in workloads and/or work contents (3, 5).
Psychological impacts of COVID-19 on second-line healthcare professionals have been documented (5–8). Occupational therapists are classified as second-line medical professionals who do not directly care for patients with COVID-19 during the early stages (9). However, the work environment has changed due to the current pandemic, and this has had a negative impact on their mental health (6, 9). Although such psychological stress can negatively affect therapy quality and lead to client dissatisfaction (10), little is known about the relationship between mental health problems and the therapy quality of occupational therapists. Previous studies identified the relationship between mental health problems and job performance (11–19). For example, Shirom et al. (17) revealed that emotional exhaustion caused by overload is a critical factor in decreasing care quality, suggesting the importance of caring for the mental health of medical professionals to maintain the quality of care. Thus, the purpose of the present study was to clarify the psychological impact of the COVID-19 outbreak on occupational therapists and examine whether their mental health problems are related to decreased quality of therapy. By conducting a cross-sectional web-based survey targeted at registered occupational therapists in Japan, we investigated the relationships among the changes in work and life due to COVID-19, mental health problems, and quality of therapy. As mentioned below, we focused on the following four factors that can affect mental health conditions: efforts to avoid being infected, information provision from the workplace, workload, and working hours.
Previous studies investigating the effects of quarantine on mental health conditions have documented that healthcare workers, compared with the general public, exhibited concerns about being infected by others and reported substantially more negative feelings, such as anger and loneliness, after quarantine (20). A previous report showed that 98.3% of occupational therapists showed more significant efforts to avoid infection, and 94.7% of them refrained from unnecessary outings (6). As a decrease in social connectedness is related to perceived stress (1), these results raise the possibility that efforts to avoid being infected would be related to adverse psychological effects. Information provision from the workplace also has a critical role in addressing mental health conditions. A recent report suggested that sufficient information from the workplace significantly reduced the risk of mental health problems (6, 21), and this finding is consistent with previous evidence that showed the effectiveness of information provision for mental support during previous infectious outbreaks such as H1N1 and SARS (22–24). Other recent reports suggested that social connectedness was associated with a lower level of perceived stress and COVID-19-related burnout (1, 25). Thus, the information provided may improve mental health conditions by enhancing the sense of social connectedness.
The increased workload and working hours negatively impact mental health conditions (6, 26–30). For example, previous literature showed that workload is positively related to depression and that its relationship was mediated by emotional distress (29), and long working hours are also associated with depression (31) and further associated with poor patient safety and decreased care quality (30). In addition to this physical overload, the present pandemic forces medical professionals to work in high-pressure environments (26).
To replicate these findings (i.e., the link between environmental factors and mental health) and further examine whether these mental health problems negatively affect the quality of therapy, we used path analysis in the present study. Because of the close relationships among mental health problems, including depression, anxiety, and insomnia (32, 33), in our hypothesized model, we assume that the four factors (i.e., efforts to avoid being infected, information provision from the workplace, workload, and working hours) are linked to each psychological symptom, and all three psychological symptoms would be related to therapy quality. Based on previous findings, which showed relationships among workload, mental health, and job performance (11, 17, 18), we designed a hypothesized path model (Figure 1A). This model focused on the relationships between (1) the changes in work and life due to COVID-19, (2) mental health problems, including depression, anxiety, and insomnia, and (3) the quality of therapy. Based on recent literature that has documented (perceived) social isolation (20, 23), we proposed “efforts to avoid being infected” and “less information provision from the workplace” as candidates that may increase mental health problems. Second, based on literature that focused on the relationship between mental health and job performance (11, 17, 18, 27, 30), we hypothesized that the increase in mental health problems would be related to a decrease in therapy quality. Based on previous reports that showed a close link between perceptions of caregiver and client (34, 35), in the present study, we employed self-report of one's therapy quality as an index of therapy quality. Further, to examine whether one's therapy quality is closely related to colleagues' therapy quality (i.e., to determine if the change in quality is beyond personal problems), we performed a simple correlation analysis.
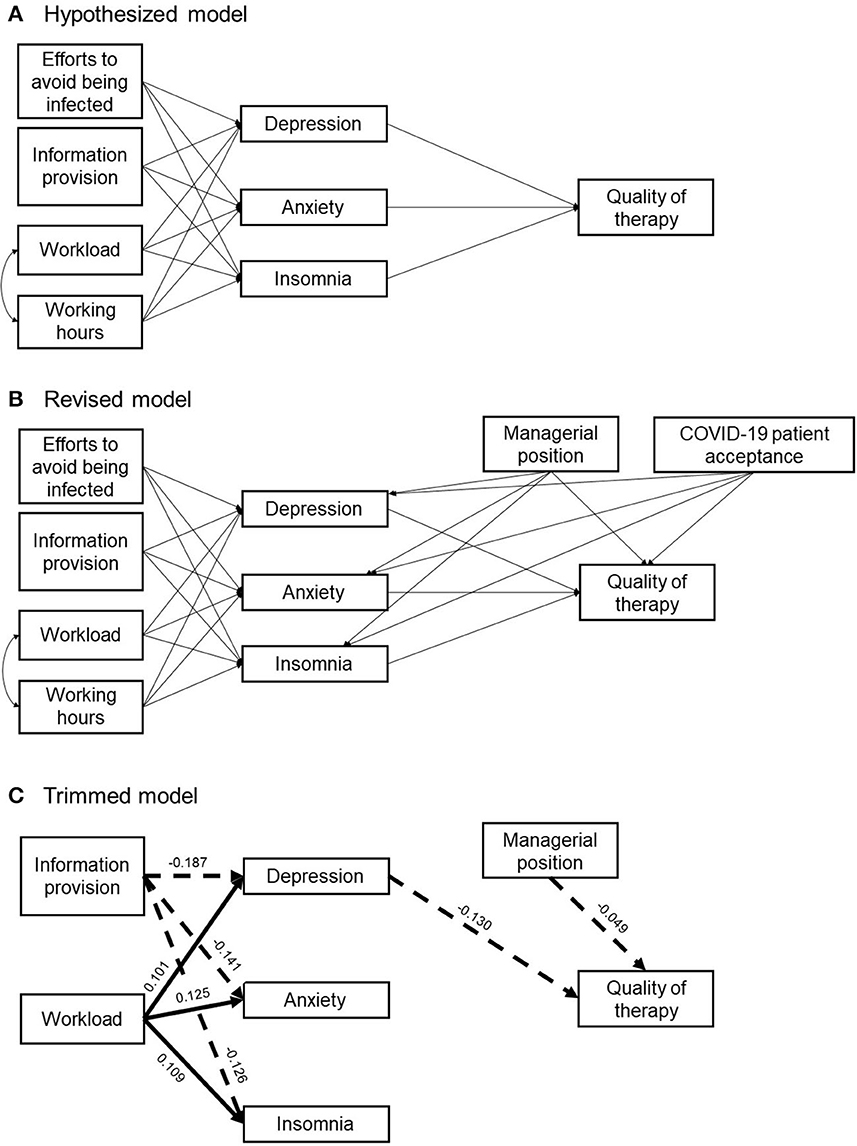
Figure 1. A hypothesized path model (A), revised model (B), and trimmed model (C). In the trimmed model, the straight line depicts a significantly positive relationship, and the dashed line depicts a significantly negative relationship.
This cross-sectional online survey was conducted in Japan from 20 to 25 January 2021. The data were collected through Google Forms (https://www.google.com/forms/about/). All the respondents were registered occupational therapists who were members of the Japanese Association of Occupational Therapists. A request for participation was sent to all registered members via email on 20 January 2021. The study protocol was approved by the ethical committee at Saitama Prefectural University (acceptance number: 20003). All participants provided written, informed consent. Email addresses were collected to ensure that the same respondent did not take the questionnaire multiple times.
Participants were asked to report their sociodemographic characteristics: age, gender, academic background, marital status (married or unmarried), history of psychiatric disorders (yes or no), employment type (full-time/part-time), managerial position (yes or no), and years of service. As the participants had to answer each question before proceeding, no missing data existed. Participants who reported a history of psychiatric disorders were excluded from the analysis. Based on previous findings (5, 6, 23), we focused on loneliness, depression, anxiety, and insomnia. Three validated questionnaires were used: the Japanese version of the three-item loneliness scale (36), the Zung Self-Rating Anxiety Scale (SAS) (37), the Zung Self-Rating Depression Scale (SDS) (38), and the Japanese version of the Insomnia Severity Index (ISI-J) (39). The three-item loneliness scale measures overall with three items (“I feel that I lack companionship,” “I feel left out,” and “I feel isolated from others”) and is known to identify loneliness quite well (40). The total score ranged from 3 to 9, and higher scores reflected greater loneliness (40). The SAS and SDS had 20 items each that measured anxiety and depression, respectively. The SAS included negative statements such as “I get upset easily or feel panicky” (37). The SDS contained 10 negative statements, such as “I feel down-hearted and blue,” and 10 reverse-scored positive statements, such as “My life is pretty full” (38). The ISI-J contained seven questions assessing the nature, severity, and impact of insomnia, rated on a five-point Likert scale (0 = no problem; 4 = very severe problem) (6, 41). These questionnaires have been widely used for non-clinical samples, and the cutoffs for detecting the presence or absence of loneliness, anxiety, depression, and insomnia were ≥ 6 for the three-item loneliness scale (42–44), ≥ 40 for the SAS (45), ≥ 50 for the SDS (46), and ≥ 10 for the ISI-J (39, 47).
Participants were also asked to answer the following items concerning the work environment: acceptance of patients with COVID-19 at their workplace (yes or no), provision of information on COVID-19 by the workplace (7-point rating scale ranging from 1 = insufficient to 7 = sufficient), changes in one's therapy quality compared to the period before COVID-19 (decreased, unchanged, or increased), colleagues' therapy quality compared with the period before COVID-19 (worse, unchanged, or better), changes in working hours compared to the period before COVID-19 (increase, decrease, or no change), changes in workload with the period before COVID-19 (increase, decrease, or no change), work from home (yes or no), and free description (fill-in-the-blank question).
Concerning daily life, participants were asked to respond to the following items concerning everyday life: efforts to avoid being infected (7-point rating scale ranging from 1 = never to 7 = frequent), efforts to not transmit the virus to others (7-point rating scale), frequency of contact with family (7-point rating), frequency of contact with friends (7-point rating), changes in daily step count compared to the period before COVID-19 (which was evaluated using records automatically logged in healthcare applications implemented in the respondents' phones), fewer outings (yes or no), attempts to avoid face-to-face conversations (yes or no), increased standard precautions at home (handwashing and gargling) (yes or no), increased frequency of mask-wearing (yes or no), increased social networking site usage (yes or no), and free description (fill-in-the-blank question).
Based on previous findings, which showed relationships among workload, mental health, and job performance (11, 17, 18), we designed a hypothesized path model (Figure 1A). This model focused on the relationships between the changes in work and life due to COVID-19, mental health problems including depression, anxiety, and insomnia, and the quality of therapy. Based on recent literature that has documented (perceived) social isolation and loneliness (20, 23), we chose “efforts to avoid being infected” and “less information provision from the workplace” as candidates that can exacerbate mental health problems. Second, based on literature that focused on the relationship between mental health and job performance (11, 17, 18, 27, 30), we hypothesized that the exacerbation of mental health problems would be related to a decrease in therapy quality. Based on previous reports that showed a close link between the perceptions of caregiver and client (34, 35), in the present study, we employed self-report of one's therapy quality as an index of therapy quality. Further, to examine whether one's therapy quality was closely related to colleagues' therapy quality (i.e., check if the change in quality is beyond personal problems), we performed a simple correlation analysis. Path analyses were performed using AMOS 28 (48). To assess the goodness of fit, we employed the chi-square value, the comparative fit index (CFI), and the root-mean-squared error of approximation (RMSEA). The chi-square value of < 0.05, the CFI value of ≥ 0.95, and the RMSEA value of < 0.06 are considered to indicate good model fit (49–52). The data were evaluated for estimation methods that assume multivariate normality using Bollen-Stine bootstrapping. Skewness and kurtosis were also examined (Supplementary Table 1).
Sample characteristics and questionnaire results are shown in Table 1. Cutoff scores for the four questionnaires were determined based on previous literature (39, 42, 45, 46). The total number of respondents was 4,418. Data from respondents with a history of psychiatric disorders (n = 481), inconsistent answers between yes or no questions and rating (e.g., “yes” to the change in outing frequency but rated the frequency as unchanged) (n = 1,336), a declaration that they do not actively see clients (n = 475), and inconsistent answers to working hours (n = 160) were excluded. The remaining respondents were 1,966 (1,106 women and 860 men).
The results of bivariate correlations among study variables are shown in Table 2. Information provision is negatively associated with the three psychological symptoms, supporting previous evidence that insufficient information provision is related to mental health problems. Information provision and the three psychological symptoms were significantly related to one's quality of therapy (all p-values < 0.01). In other words, an increase in information provision is positively related to the quality of therapy, whereas a decrease in psychological symptoms is positively related to the quality of therapy. Efforts to avoid being infected, workload, and working hours did not show a significant relationship with the quality of therapy.
Furthermore, efforts to avoid being infected and working hours were not significantly associated with any psychological symptoms. We also performed correlation analysis using the data of one's therapy quality and colleagues' therapy quality. This analysis showed a strong positive correlation (Pearson's r = 0.79, p < 0.01, 95% confidence interval [0.78, 0.81]), suggesting that changes in therapy quality during the pandemic mainly occur at the institutional rather than the individual level.
First, we examined whether the demographic variables, including gender, managerial position, marital status, and acceptance of patients with COVID-19, needed to be considered as control variables using multigroup analysis. The four types of multigroup analysis revealed that managerial position and acceptance of patients with COVID-19 needed to be considered as control variables, whereas gender and marital status did not make significant group differences (Supplementary Figures 1–8). Therefore, we revised the model to include managerial position and acceptance of patients with COVID-19 as control variables and performed the path analysis (Figure 1B). The path analysis for the revised model (Table 3, Figure 1B) showed a significant chi-square value (χ2 = 117.22, df = 9, p < 0.001) and a discrepancy between the model and data (Bollen-Stine bootstrapping, p < 0.05), but the other goodness-of-fit indicators showed that this model had a good fit (CFI = 0.96, RMSEA = 0.078). Next, we designed a trimmed model based on the results of the revised model. In this trimmed model, exogenous variables, “efforts to avoid being infected” and “working hours,” and a control variable, “acceptance of patients with COVID-19,” which was not related to any other variables and had insignificant paths, were removed (Figure 1C). Although, this model showed a significant chi-square value (χ2 = 42.48, df = 7, p < 0.05), and the discrepancy between the model and data (Bollen-Stine bootstrapping, p < 0.05), the other goodness-of-fit indices showed that this model had a better fit (CFI = 0.99, RMSEA = 0.05). These results suggested that insufficient information provision by the workplace and that increased workload are critically associated with mental health problems, and therapists in managerial positions tend to feel that the quality of their therapy has decreased during the COVID-19 pandemic. Furthermore, although the bivariate correlation revealed that all mental health problems were significantly associated with the quality of therapy, depression may be especially important in maintaining the quality of therapy.
Using data from an online questionnaire from registered occupational therapists, we investigated the relationships among work life, mental health conditions, and quality of therapy. The results from the path analysis showed that insufficient information provision at the workplace and increased workload were related to depression, anxiety, and insomnia. Depression was associated with decreased self-evaluation of one's quality of therapy. Furthermore, the evaluation of one's quality of therapy showed a strong positive correlation with the evaluation of a colleague's quality of therapy, suggesting the possibility that changes in therapy quality occur on an institutional basis rather than on an individual basis. However, the majority of participants thought that they obtained information from the workplace at a higher level than average; it is considered that qualitatively novel supporting systems and reassessment of workload are important.
A total of 50.4% of the respondents reported an increased workload due to the pandemic, and the increase in workload was significantly related to an increase in depression, anxiety, and insomnia. These findings are consistent with a recent meta-analysis focusing on burnout and the mental health of medical professionals (53). The path analysis showed a specific link between depression and therapy quality. Although depression showed a strong positive correlation with the other two symptoms (r = 0.73 with anxiety and r = 0.52 with insomnia), anxiety and insomnia showed relatively smaller correlations with therapy quality, which could be negligible (r = −0.1 for anxiety and r = −0.06 for insomnia) (54). Depression showed a relatively larger correlation with therapy quality (r = −0.13), highlighting the relationship between depression and the quality of therapy. Contrary to our hypothesis, efforts to avoid being infected did not show a significant link with other variables and were excluded from our trimmed model. This may be because there is an extremely high number of therapists who do not want to be infected. In fact, 99.2% of the respondents said that their efforts to avoid being infected were above average. The data might indicate the professionalism of occupational therapists.
During the second state of emergency, 24.4, 16.5, 15.1, and 14.5% of occupational therapists presented symptoms of loneliness, depression, anxiety, and insomnia, respectively. Although the prevalence of psychological symptoms varies across countries, especially due to the pandemic (55), the ratio of respondents who showed depression and anxiety increased, and the ratio of insomnia decreased in comparison with the previous online survey, which was conducted during the initial state of emergency (10.9 to 16.5% for depression, 11.3 to 15.1% for anxiety, and 16.8 to 14.5% for insomnia) (6). Although the number of people with insomnia decreased, mental health condition among therapists seems to be getting worse, and additional mental support is needed. Taken together with the finding of the bivariate correlation, which showed a negative relationship between the increase in psychological symptoms and therapy quality, there is a possibility that therapy quality has decreased throughout the pandemic in some institutions. Although additional direct and causal evidence is needed, insufficient information provision and overload might negatively affect therapy quality, resulting in decreased quality of life of patients.
It should be noted that 74.4% of respondents answered that the information provided was above average, and only 9.4% answered that the information provided was below average. Thus, most workplaces seem to have been trying to support therapists, and therapists acknowledge the effort. However, in addition to typical support for workers, such as providing personal protective equipment and information, individual psychological support would be needed. For example, one possible way is to identify therapists with psychological symptoms using validated questionnaires (9) and monitor and care for them (26). Burnout among healthcare professionals has been a severe problem for a long time (10, 30), and it is becoming more serious in these challenging times. As burnout is linked to decreased therapy quality, such an approach is essential for therapists and patients.
Another possible idea to support therapists can be drawn from a recent randomized clinical trial that demonstrated the effectiveness of a layperson-delivered, empathy-focused program (56). In this study, callers who were briefly trained in empathetic conversational techniques using a 1-h videoconference talked to participants over the telephone for 4 weeks, and this intervention improved depression, loneliness, and anxiety in at-risk adults (56). If managers are trained to have empathetic conversations using short material, such an intervention can be implemented in each workplace, and it would have the potential to support therapists and further maintain therapy quality during pandemics. However, it should be noted that the managerial position has a negative relationship with therapy quality, and care for the managers is also essential. The findings of this study revealed that one's therapy quality showed a strong positive correlation with colleagues' therapy quality. Thus, it is plausible that therapy quality can change at the institutional level. As a first step, it is crucial to reassess the work and mental health conditions of each professional and the supporting system in each institution. Then, it might be helpful to consider employing such additional approaches.
The current findings have limitations. First, as the present results were based on a cross-sectional online questionnaire and data were gathered only from occupational therapists in Japan, further studies are needed to examine whether these results can be applied to other populations (e.g., physiotherapists) and across borders. Second, the evaluation of one's own and colleagues' therapy quality in the present study was based on the participants' self-reports. Thus, there is a possibility that those self-evaluations are biased to some extent based on social desirability (a tendency to present oneself as socially desirable or acceptable rather than to present one's true thoughts or feelings) or by decreased self-esteem, which might be related to a personal mental health condition. Although the evaluation between one's therapy quality and that of colleagues' were correlated, and it is plausible that a decrease in therapy quality happens to some extent, these results are reported with caution. Future studies are needed to collect patient data relating to the quality of therapy and personality assessment, which may yield greater objectivity than self-reports. Finally, and most importantly, studies are required that directly examine whether interventions to support therapists' mental health, such as an empathy-focused program, are effective in terms of improving the quality of therapy and patients' quality of life. Nevertheless, we believe the findings from this study would be the cornerstone of a novel support system for therapists.
In conclusion, a nationwide cross-sectional online survey was conducted to investigate whether and how mental health problems are related to the therapy quality of occupational therapists. The results showed that insufficient information provision at the workplace and increased workload were positively related to psychological symptoms. Only depression was associated with decreased self-evaluation of one's quality of therapy. Evaluations of one's own quality and a colleague's quality of therapy showed a strong positive correlation, suggesting that improvements in therapy quality may occur at the institutional rather than the individual level.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethical Committee in Saitama Prefectural University. The patients/participants provided their written informed consent to participate in this study.
AI, DS, HM, HN, and TI: study conception, design, and data acquisition. AI, DS, SK, and TI: analysis, interpretation of data, and writing—review and editing. AI: writing—original draft. All authors approved final version of the article.
This research was supported by the Saitama Prefectural University Grant (200070).
We greatly appreciate the Japanese Association of Occupational Therapists for their support in data collection and all occupational therapists for their participation.
Author HN was employed by the Japanese Association of Occupational Therapists.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1053703/full#supplementary-material
1. Nitschke JP, Forbes PAG, Ali N, Cutler J, Apps MAJ, Lockwood PL, et al. Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br J Health Psychol. (2021) 26:553–69. doi: 10.1111/bjhp.12485
2. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
3. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
4. Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry. (2020) 7:e15–6. doi: 10.1016/S2215-0366(20)30078-X
5. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
6. Ishioka T, Ito A, Miyaguchi H, Nakamura H, Sawamura D. Psychological impact of COVID-19 on occupational therapists: an online survey in Japan. Am J Occup Ther. (2021) 75. doi: 10.5014/ajot.2021.046813
7. Tahara, M., Mashizume, Y, Takahashi K. Coping mechanisms: exploring strategies utilized by Japanese healthcare workers to reduce stress and improve mental health during the COVID-19 pandemic. Int J Env Res Public Health. (2021) 18:1. doi: 10.3390/ijerph18010131
8. Tanaka K, Tahara M, Mashizume Y, Takahashi K. Effects of lifestyle changes on the mental health of healthcare workers with different sense of coherence levels in the era of COVID-19 pandemic. Int J Env Res Public Health. (2021) 18:6. doi: 10.3390/ijerph18062801
9. Ito A, Ishioka T. Exploring the impact of the COVID-19 pandemic on the mental health of rehabilitation therapists. Jpn Soc Brain Function Rehabil. (2020) 10:24799. doi: 10.24799/jrehabilneurosci.200512
10. Escudero-Escudero, AC, Segura-Fragoso A, Cantero-Garlito PA. Burnout syndrome in occupational therapists in Spain: prevalence and risk factors. Int J Env Res Public Health. (2020) 17:3164. doi: 10.3390/ijerph17093164
11. Adler DA, McLaughlin TJ, Rogers WH, Chang H, Lapitsky L, Lerner D, et al. Job performance deficits due to depression. Am J Psychiatry. (2006) 8. doi: 10.1176/ajp.2006.163.9.1569
12. Darvishmotevali M, Ali F. Job insecurity, subjective well-being and job performance: the moderating role of psychological capital. Int J Hosp Manag. (2020) 87:102462. doi: 10.1016/j.ijhm.2020.102462
13. Dyrbye LN, West CP, Hunderfund AL, Sinsky CA, Trockel M, Tutty M, et al. Relationship between burnout, professional behaviors, and cost-conscious attitudes among US physicians. J Gen Int Med. (2020) 35:1465–76. doi: 10.1007/s11606-019-05376-x
14. Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA. (2011) 305:2009–10. doi: 10.1001/jama.2011.652
15. Ignacio J, Dolmans D, Scherpbier A, Rethans JJ, Chan S, Liaw SY, et al. Stress and anxiety management strategies in health professions' simulation training: a review of the literature. BMJ Simul Technol Enhanc Learn. (2016) 2:42–6. doi: 10.1136/bmjstel-2015-000097
16. Obrenovic B, Jianguo D, Khudaykulov A, Khan MAS. Work-family conflict impact on psychological safety and psychological well-being: a job performance model. Front Psychol. (2020) 11:475. doi: 10.3389/fpsyg.2020.00475
17. Shirom A, Nirel N, Vinokur AD. Overload, autonomy, and burnout as predictors of physicians' quality of care. J Occup Health Psychol. (2006) 11:328–42. doi: 10.1037/1076-8998.11.4.328
18. Wang PS, Beck AL, Berglund P, McKenas DK, Pronk NP, Simon GE, et al. Effects of major depression on moment-in-time work performance. Am J Psychiatry. (2004) 7. doi: 10.1176/ajp.161.10.1885
19. Yu J, Park J, Hyun SS. Impacts of the COVID-19 pandemic on employees' work stress, well-being, mental health, organizational citizenship behavior, and employee-customer identification. J Hosp Mark Manag. (2021) 30:529–48. doi: 10.1080/19368623.2021.1867283
20. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
21. Sawamura D, Ito A, Miyaguchi H, Nakamura H, Ishioka T. Different impacts of COVID-19 on quality of therapy, psychological condition, and work life among occupational therapists in physical and mental health fields. Front Public Health. (2022) 10:7069. doi: 10.3389/fpubh.2022.887069
22. Imai H, Matsuishi K, Ito A, Mouri K, Kitamura N, Akimoto K, et al. Factors associated with motivation and hesitation to work among health professionals during a public crisis: a cross sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC Public Health. (2010) 10:672. doi: 10.1186/1471-2458-10-672
23. Matsuishi K, Kawazoe A, Imai H, Ito A, Mouri K, Kitamura N, et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin Neurosci. (2012) 66:353–60. doi: 10.1111/j.1440-1819.2012.02336.x
24. Sin SS, Huak CY. Psychological impact of the SARS outbreak on a Singaporean rehabilitation department. Int J Ther Rehabil. (2004) 11:417–24 doi: 10.12968/ijtr.2004.11.9.19589
25. Yildirim M, Çiçek I, Sanli ME. Coronavirus stress and COVID-19 burnout among healthcare staffs: the mediating role of optimism and social connectedness. Curr Psychol. (2021) 3:1781. doi: 10.1007/s12144-021-01781-w
26. Greenberg N. Mental health of health-care workers in the COVID-19 era. Nat Rev Nephrology. (2020) 16:425–6. doi: 10.1038/s41581-020-0314-5
27. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ m. (2020). doi: 10.1136/bmj.m1211
28. Greenglass ER, Burke RJ, Fiksenbaum L. Workload and burnout in nurses. J Community Appl Soc Psychol. (2001) 11:211–5. doi: 10.1002/casp.614
29. Greenglass ER, Burke RJ, Moore KA. Reactions to increased workload: Effects on professional efficacy of nurses. Appl Psychol. (2003) 52:580–97. doi: 10.1111/1464-0597.00152
30. Griffiths P, Dall'Ora C, Simon M, Ball J, Lindqvist R, Rafferty AM, et al. Nurses' shift length and overtime working in 12 European countries: the association with perceived quality of care and patient safety. Med Care. (2014) 52:975–981. doi: 10.1097/MLR.0000000000000233
31. Ogawa R, Seo E, Maeno T, Ito M, Sanuki M, Maeno T, et al. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Edu. (2018) 18:50. doi: 10.1186/s12909-018-1171-9
32. Caplan SE. Relations among loneliness, social anxiety, and problematic internet use. CyberPsychology and Behav. (2007) 10:234–42. doi: 10.1089/cpb.2006.9963
33. Staner L. Comorbidity of insomnia and depression. Sleep Med Rev. (2010) 14:35–46. doi: 10.1016/j.smrv.2009.09.003
34. Jimmieson NL, Griffin MA. Linking client and employee perceptions of the organization: a study of client satisfaction with health care services. J Occup Organ Psychol. (1998) 71:81–96. doi: 10.1111/j.2044-8325.1998.tb00664.x
35. Schneider B, White SS, Paul MC. Linking service climate and customer perceptions of service quality: test of a causal model. J Appl Psychol. (1998) 83:150–63. doi: 10.1037/0021-9010.83.2.150
36. Igarashi T. Development of the Japanese version of the three-item loneliness scale. BMC Psychol. (2019) 7:20. doi: 10.1186/s40359-019-0285-0
37. Zung WW. A rating instrument for anxiety disorders. Psychosom. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
38. Zung WW. A self-rating depression scale. Arch Gen Psychiatry. (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
39. Munezawa T. Development of the Japanese version of the insomnia severity index (ISI-J). Jpn J Psychiatric Treat. (2009) 24:219–25.
40. Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. (2004) 26:655–72. doi: 10.1177/0164027504268574
41. Bastien CH, Vallières A, Morin Cm. validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/s1389-9457(00)00065-4
42. Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the Natl Acad Sci. (2013) 110:5797–801. doi: 10.1073/pnas.1219686110
43. Stickley A, Ueda M. Loneliness in Japan during the COVID-19 pandemic: prevalence, correlates and association with mental health. Psychiatry Res. (2022) 307:114318. doi: 10.1016/j.psychres.2021.114318
44. Victor CR, Pikhartova J. Lonely places or lonely people? Investigating the relationship between loneliness and place of residence. BMC Public Health. (2020) 20:778. doi: 10.1186/s12889-020-08703-8
45. Dunstan DA, Scott N. Norms for Zung's self-rating anxiety scale. BMC Psychiatry. (2020) 20:90. doi: 10.1186/s12888-019-2427-6
46. Dunstan DA, Scott N. Clarification of the cut-off score for Zung's self-rating depression scale. BMC Psychiatry. (2019) 19:177. doi: 10.1186/s12888-019-2161-0
47. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
49. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling. Multidisciplinary J. (1999) 6:1–55. doi: 10.1080/10705519909540118
50. Kline R. Principles and Practice of Structural Equation Modeling, Fourth Edition. New York, NY: The Guilford Press (2015).
51. Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: a review. J Edu Res. (2006) 99:323–38. doi: 10.3200/JOER.99.6.323-338
52. Volkert D, Candela L, Bernacki M. Student motivation, stressors, and intent to leave nursing doctoral study: a national study using path analysis. Nurse Edu Today. (2018) 61:210–5. doi: 10.1016/j.nedt.2017.11.033
53. O'Connor, K, Muller Neff D, Pitman S. Burnout in mental health professionals: a systematic review and meta-analysis of prevalence and determinants. Eur Psychiatry J Assoc Eur Psychiatrists. (2018) 53:74–99. doi: 10.1016/j.eurpsy.2018.06.003
54. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. (2018) 126:1763–8. doi: 10.1213/ANE.0000000000002864
55. Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M, et al. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuro-Psychopharmaco Biol Psychiatry. (2021) 107:110247. doi: 10.1016/j.pnpbp.2021.110247
56. Kahlon MK, Aksan N, Aubrey R, Clark N, Cowley-Morillo M, Jacobs EA, et al. Effect of layperson-delivered, empathy-focused program of telephone calls on loneliness, depression, and anxiety among adults during the COVID-19 pandemic: a randomized clinical trial. JAMA Psychiatry. (2021) 3:113. doi: 10.1001./jamapsychiatry.2021.0113
Keywords: COVID-19, occupational therapy, anxiety, depression, insomnia
Citation: Ito A, Sawamura D, Kajimura S, Miyaguchi H, Nakamura H and Ishioka T (2022) Quality of therapy and mental health among occupational therapists during the COVID-19 pandemic. Front. Public Health 10:1053703. doi: 10.3389/fpubh.2022.1053703
Received: 26 September 2022; Accepted: 24 November 2022;
Published: 15 December 2022.
Edited by:
Antonio Caputi, University of Bari Aldo Moro, ItalyReviewed by:
Kai-Shuen Pheh, Tunku Abdul Rahman University, MalaysiaCopyright © 2022 Ito, Sawamura, Kajimura, Miyaguchi, Nakamura and Ishioka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ayahito Ito, YXlhaGl0by5pdG9AZ21haWwuY29t; Daisuke Sawamura, ZC5zYXdhbXVyYUBwb3AubWVkLmhva3VkYWkuYWMuanA=; Toshiyuki Ishioka, aXNoaW9rYS10b3NoaXl1a2lAc3B1LmFjLmpw
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.