
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 26 January 2023
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1053302
 Desalegn Tesfa1*
Desalegn Tesfa1* Sofonyas Abebaw Tiruneh1
Sofonyas Abebaw Tiruneh1 Alemayehu Digssie Gebremariam1
Alemayehu Digssie Gebremariam1 Melkalem Mamuye Azanaw1
Melkalem Mamuye Azanaw1 Melaku Tadege Engidaw1
Melaku Tadege Engidaw1 Belayneh Kefale2†
Belayneh Kefale2† Bedilu Abebe1
Bedilu Abebe1 Tsion Dessalegn1
Tsion Dessalegn1 Mulu Tiruneh1
Mulu Tiruneh1Background: Even though the total fertility rate (TFR) has decreased significantly over the past decades in many countries, it has remained stable in sub-Saharan African (SSA) countries. However, there is variation among the sub-regions and inhabitants of SSA. Therefore, this study aimed to conduct a meta-analysis of demographic and health surveys (DHS) to estimate the pooled level of TFR in SSA and to depict sub-regional and inhabitant differences.
Methods: The data source for this study was the standard Demographic and Health Survey datasets of 33 sub-Saharan African countries, accessed through www.meaasuredhs.com between 2010 and 2018. The point estimate of the total fertility rate with its corresponding standard error in each sub-Saharan African country was estimated using the DHS.rates R package. Using the point estimate of the TFR with the standard error of each country, the pooled estimate of the TFR was generated by the metan STATA command.
Results: The study comprised 1,324,466 live births in total. The pooled estimate of sub-Saharan Africa's overall fertility rate was five children per woman (95% CI: 4.63–5.37). Consequently, the pooled estimate of total fertility for people living in urban and rural areas was 3.90 (95% CI: 3.60–4.21) and 5.82 (95% CI: 5.43–6.21) children per woman, respectively. In sub-group analysis, the pooled estimates of the TFR for the East African, Central African, Southern African, and West African regions, respectively, were 4.74, 5.59, 3.18, and 5.38 children per woman. Total fertility rates were greater in low-income nations (5.45), lower-middle-income countries (4.70), and high-middle-income countries (3.80).
Conclusions: SSA has a relatively high total fertility rate. The regions of West and Central Africa have the highest overall fertility rate. The fertility rate is higher in countries with a large rural population and low income. Strategies should be developed to address this public health concern, especially in rural Central and Western Africa.
Many women want to have biological offspring (1, 2). The fertility rate is the total number of children a woman has during her reproductive period (1, 3). Fertility contributes to population growth in either a positive or negative way, depending on whether it is above and below the replacement level, respectively (3). According to early conventional demographic theory, high fertility results from a highly desired family size. People want their children to assist with the family. In addition, high child mortality can lead parents to have additional children to protect against loss or to replace lost children (4). The number of children desired by couples changes over time (5). In the last six decades since 1950, the total fertility rate (TFR) (the number of children each woman bears on average) has decreased worldwide, particularly in developed countries (6–8). The global fertility rate declined from 3.2 live births per woman in 1990 to 2.5 births in 2019. However, sub-Saharan Africa is the region with the highest fertility level (6), with no fertility reduction or only an incipient decline (9). In the industrialized world, fertility reached 2.8 births per woman in the late 1950s. It fell below the replacement level (1.7 per woman) in the late 1990s in Europe, North America, and Australia. Consequently, Japan reached below the replacement level in the late 1950s and has declined further (4, 10). However, in low-income countries, women have many babies (11–14). In low-resource countries, the demographic pattern is characterized by the coexistence of high infant and child mortality (15). Subsequently, in any region of the world, fertility in sub-Saharan African countries remained at the highest level (16). Studies indicated that, whenever fertility is high, maternal, infant, and child mortality are high (17). High fertility poses health risks for mothers and children, causes significantly slower economic growth, and exacerbates environmental degradation (18–21). As the fertility rate remains high, the youth dependency ratio also increases exponentially (22). Meanwhile, the proportion of reproductive-age women who were married or living in a union and used modern contraceptive methods was not >22% in SSA, compared with East Asia at 86% and Latin America and the Caribbean at 72% (22). Worldwide, in 2019, 50% of all women of reproductive age were using some form of contraception. However, in the same year, only 29% of women in sub-Saharan Africa were using some form of contraception (8). Due to the minimal utilization of contraceptives in Africa, particularly in SSA, women are exposed to unintended pregnancy. According to a recent report from the WHO, around 40% of pregnancies are unplanned (22, 23). Woman empowerment (increasing women's decision-making capacity) is identified as a key solution that can change the prevailing fertility and contraceptive utilization patterns in SSA (24–26). The level of fertility in SSA is projected to fall from 3.1 births per woman in 2010 to 2.1 births in 2050. Continued rapid population growth presents a challenge to achieving sustainable development, particularly in SSA (8). Although the DHS is a widely used source of estimates of fertility and mortality in low-income countries, estimates of the TFR and mortality can vary between different data sources. In a comparison study that compared DHS estimates of fertility with other estimates, the fertility rate computed from PMA2020 data showed a range of 5–22% difference compared to the result from DHS surveys (27).
Expanding access to contraceptives and reducing unmet needs for family planning can help decrease the TFR among reproductive-age group women in SSA (28). However, scarce data and inconsistent data sources create difficulties in monitoring progress in different regions of Africa for policy development and program planning. Although several data sources, including the DHS, have provided estimates of the TFR in SSA, no study has yet investigated the pooled fertility rate within the WHO sub-region (Eastern Africa, Southern Africa, Central Africa, and Western Africa) to allow for sub-regional comparison. Therefore, showing the pooled rate of TFR in sub-Saharan African countries among EDHS reports is critical for monitoring and evaluation.
The DHS Program has been working with developing countries around the world to collect data about significant health issues, including fertility. The data are nationally representative, of high quality, follow standardized data collection procedures across countries, and have consistent content over time. We obtained raw data from www.meaasuredhs.com on all completed population-based surveys conducted under the DHS projects (29). The survey targeted women aged 15–49 years and men aged 15–59 years in randomly selected households in each country using a multi-stage sampling method. Detailed information was collected on the background characteristics of the respondents, including maternal health and child health, as well as harmful traditional practices (30). The source population included all mothers aged 15–49 years in the 3 years preceding the survey, excluding the month of the interview (1–36 months before the survey), in 33 SSA countries. The study population consisted of all reproductive-age mothers in the 3 years preceding the survey period in the selected enumeration areas (EAs) in each country. The data for this study were extracted from the birth record (BR) file in the standard DHS dataset for sub-Saharan African countries between 2010 and 2018. A total of 1,324,466 live births were included from sub-Saharan countries (11 East African, 6 Central African, 13 West African, and 3 South African countries) (Table 1).
Reproductive-age women aged 15–49 years in the 3 years preceding the survey in the selected enumeration areas of each country were included in this study. However, countries (the Central African Republic, Eswatini, Sao Tome and Principe, Madagascar, and Sudan) that did not have a DHS survey report after the 2010/2011 survey year were excluded. Three sub-Saharan countries (Botswana, Mauritania, and Eritrea) were excluded because the dataset was not publicly available (Figure 1).
The outcome variable of this study was the total fertility rate. The TFR is a hypothetical measure of women's fertility. It could be defined as the number of children born per woman if she experienced current age-specific fertility rates throughout her childbearing years and did not die, according to a current schedule of age-specific fertility rates, and not be subject to mortality. In standard DHS surveys, ASFRa is calculated for a reference period of 3 years preceding the survey for seven five-year age groups. Thus, the TFR can be written as follows:
The data were extracted using Microsoft excel and R Software. The point estimate of TFR with the standard error for each country was extracted from the individual record file (IR file) using the DHS.rates R package. In each country, along with fertility, the “fert” function estimates standard error (SE), relative standard error (RSE), and confidence interval (CI) for each rate (31). The methods of calculating the standard errors in the DHS rates package were in line with the DHS approach detailed in the DHS Sampling and Household Listing Manual. After extracting the point estimate and standard error, the pooled estimate of TFR (Table 2) was pooled using the “metan” STATA command. The pooled estimation of the TFR was determined with the random-effects model using DerSimonian-Laird weight. A subgroup analysis was conducted based on the sub-regions of sub-Saharan Africa, residence, and country income status.
Overall, a total of 1,324,466 live births, with a minimum of 14,769 in Comoros and a maximum of 116,888 in Nigeria, were included in this study (Table 1). The pooled TFR estimate for sub-Saharan African countries was calculated. The pooled TFR estimate for 33 countries in sub-Saharan Africa was five children per woman (95% CI: 4.63–5.37). The pooled TFR estimates for East African countries were 4.74 (95% CI: 4.32–5.16) children per woman, 5.59 (95% CI: 4.83–6.35) children per woman in Central Africa, 3.18 (95% CI: 2.55–3.81) children per woman in Southern Africa, and 5.38 (95% CI: 4.49–5.85) children per woman in West Africa (Figure 2). The pooled TFR estimates for low-, middle-, and upper-middle-income countries were 5.45 (95% CI: 5.02–5.89), 4.70 (95% CI: 4.24–5.16), and 3.80 (95% CI: 2.80–4.80), respectively (Figure 3). Consequently, the pooled TFR estimate for urban and rural inhabitants was 3.90 (95% CI: 3.60–4.21) and 5.82 (95% CI: 5.43–6.21), respectively (Figures 4, 5).
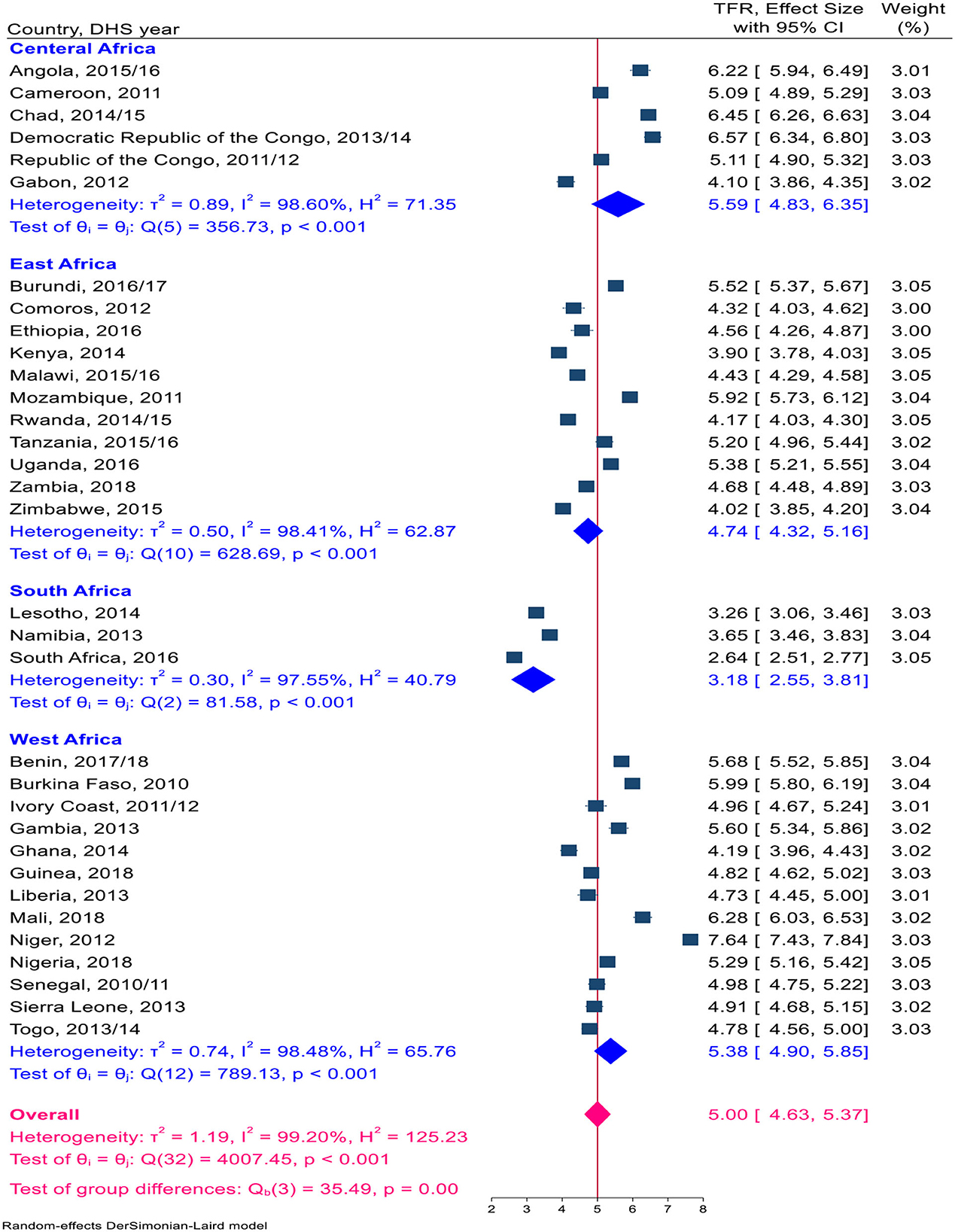
Figure 2. A Forest plot of the pooled estimate of TFR in SSA countries using the recent DHS 2010–2018, 2020.

Figure 3. A Forest plot of the pooled estimate of TFR by country income across sub-Sharan African countries using the recent DHS between 2010–2018, 2020.
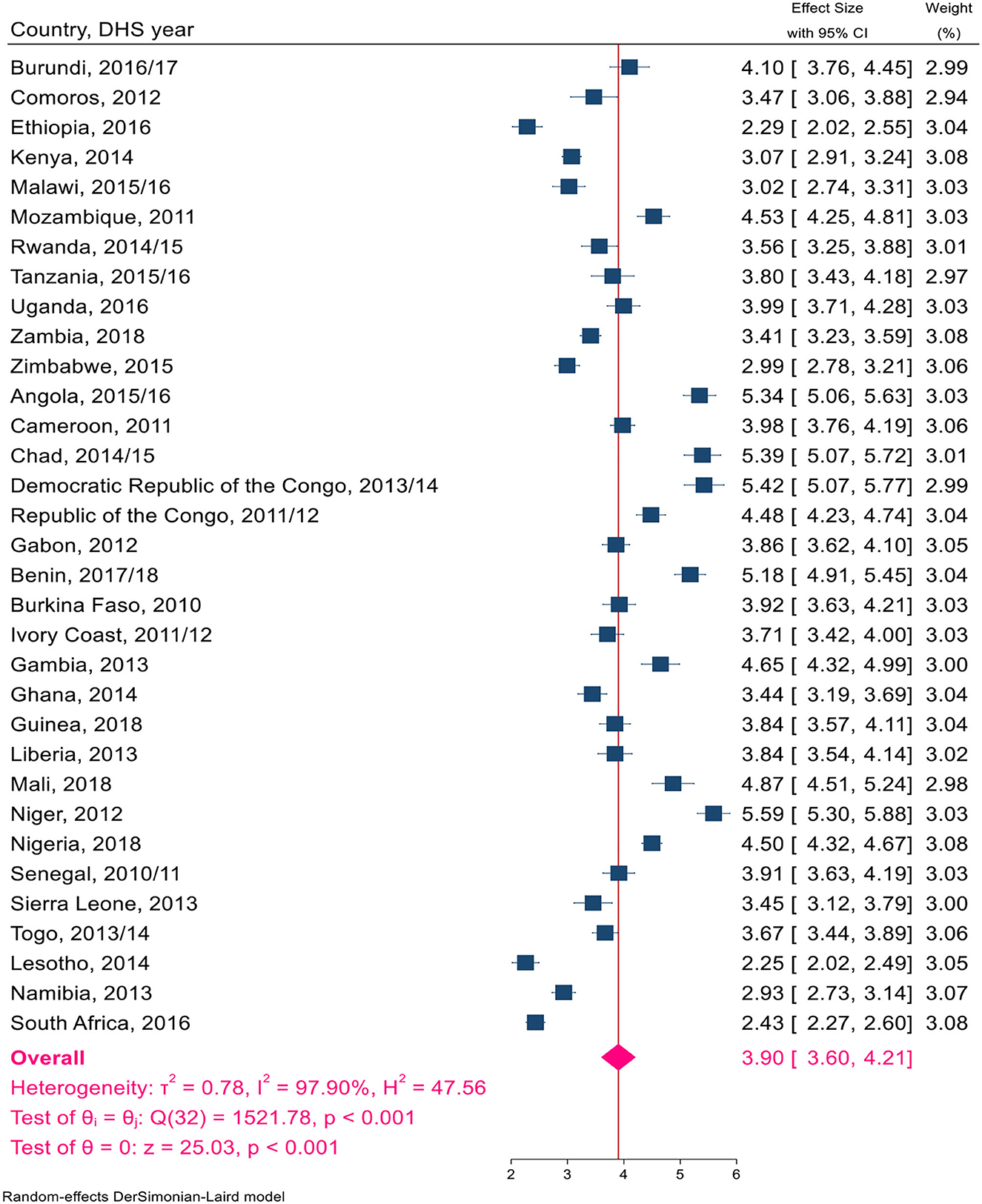
Figure 4. A Forest plot of the pooled estimate of TFR by urban residents in sub-Sharan African countries using the recent DHS between 2010–2018, 2020.
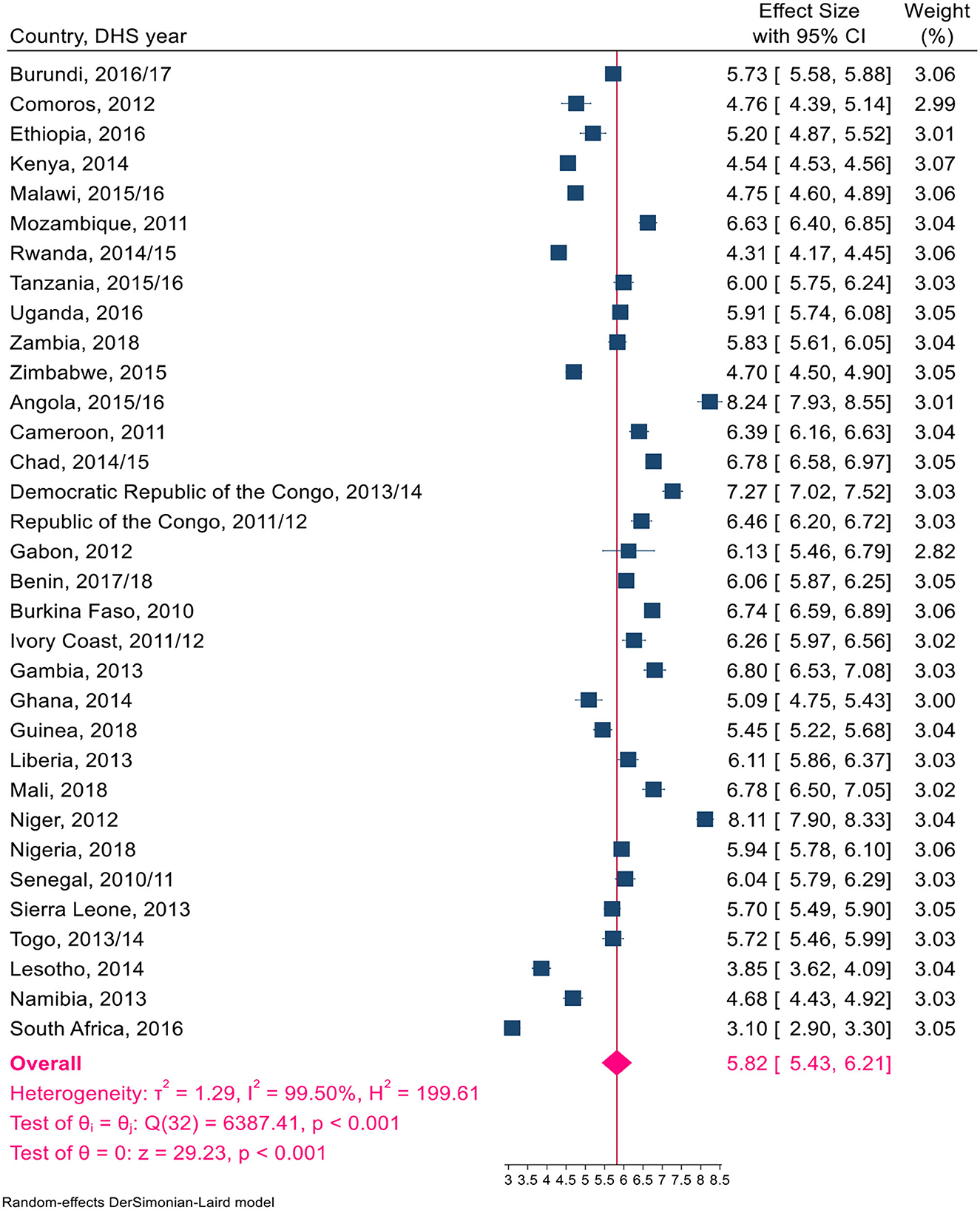
Figure 5. A Forest plot of the pooled estimate of TFR by rural inhabitants in SSA countries using the recent DHS between 2010–2018, 2020.
The fertility decline in SSA countries has been relatively steady and occurred later compared to other regions in the world. Its age-specific fertility rate also showed substantial variation among countries (3, 32, 33). The pace of decline varies considerably across countries; as a result, the median pace change in SSA countries (0.03 per year) is less than one-third the pace in other regions (0.13 per year) (34). Throughout resource-constrained countries, a considerable proportion of women who did not want to become pregnant were not using contraception. There could be multiple barriers to using contraception that contribute to this “unmet need” for contraception. Similarly, there are noticeable differences among some regions in Africa. The demand for and “met need” for family planning is higher in eastern and southern African countries than in central and western African countries, which is a major factor in the increase in fertility.
In this study, the overall pooled estimate of the TFR from DHS data in SSA was five per woman. Even though the TFR has fallen significantly in the past decades in many countries, it has remained stable (or “stable population”) at around 6,400 children per 1,000 women in 1990 (3) in SSA countries. According to a report from the World Health Organization 1 year ago (2019), the TFR in SSA was 4,600 per 1,000 women (8, 32). In the same time period, the average number of children a woman would have by the end of her childbearing years also declined in Latin America and the Caribbean (from 3.3 to 2.4), in Central and Southern Asia (from 4.3 to 2.4), in Eastern Asia (from 2.5 to 1.8), and in Northern Africa (from 4.4 to 2.9). There is a discrepancy between the TFR of SSA countries reported by the WHO in 2019 and the current (2020) pooled DHS reports.
A possible justification for this discrepancy might be the data source that the two studies used. As mentioned previously, there is a considerable decrease in the TFR from time to time in different regions of the world. However, the decrement is steady in SSA. There are several reasons why SSA lacks a marked decline in total fertility, including political instability, poverty, a lack of government commitment to female education, a weak healthcare system, and cultural beliefs that view children as sources of income; in almost all African countries, early marriage is taboo (35, 36). In contrast, when women delay childbearing and the mean age of childbirth increases, the TFR decreases because of the reduced number of births over a woman's reproductive years (10). Compared to our study, in India, the TFR was 2.2 per woman among sampled registration systems in 22 states in 2017, which was close to the replacement level; this decrease was attributed to factors such as higher education, increased mobility, late marriage, and financial independence for women (37).
In this study, the distributions of total fertility in the sub-region of SSA countries are not similar. Consequently, the pooled estimates of TFR in Eastern Africa, Southern Africa, Central Africa, and Western African countries were 4.74, 3.18, 5.59, and 5.38, respectively. Countries within each sub-region have experienced sociodemographic, socio-political, economic, and cultural events that could influence total fertility variations. In Central Africa and Western African countries, the TFR is higher than the pooled level. This rise could be because >50% of women in these regions experience their first marriage, sexual initiation, and the birth of their first child by the age of 20 (33). In contrast, in China, only 2% of children are born to teenage mothers (38, 39).
Besides, West and Central African countries have low rates of modern contraceptive use, with some of the lowest contraceptive prevalence rates in the world in two sub-regions of Africa (40); this could be because family planning is not accepted by certain religious and social doctrines and because these regions tend to have a preference for large families (33). Countries such as almost all of central Africa except Gabon, Mozambique in East Africa, and Niger in West African countries reported the highest TFR within each sub-region. Meanwhile, in this study, among 33 SSA countries, Niger reported the highest total fertility rate. However, South Africa's TFR is significantly lower than in other sub-regions of sub-Saharan Africa. In the meantime, countries in southern Africa reported the highest level of contraceptive use, followed by countries in East Africa. Modernization, urbanization, school-based education, and male involvement were higher in Southern Africa than in other sub-regions of SSA countries (40).
Ascertaining fertility levels by residence is crucial for a better understanding of contemporary demographic changes in developing countries. The pooled fertility level was significantly higher in rural inhabitants than in urban inhabitants, at 3.90 and 5.82 per woman, respectively. These findings were also consistent with some studies (41, 42). Because there are known variations in social, economic, demographic, and health characteristics across urban and rural settlements (43–45). Another sub-group in which we saw the variation in total fertility was income. This study showed a significant variation in total fertility in upper-middle-income countries and low-income countries. Because in upper-middle-income countries, the age at which women first give birth is delayed, which influences the number of children a woman will conceive in her lifetime, and the proportion of women progressing from parity to the next parity was high (15-9). In high-income agricultural societies, parents tend to need relatively fewer children (using modern contraceptives). In contrast, in lower-income societies, women want many children, and adolescents are more likely to experience unwanted and poorly timed pregnancies (4, 46, 47).
This pooled estimate revealed that the TFR in sub-Saharan countries is high, with the highest TFR being reported in central and west African countries. The fertility rate of rural dwellers was higher compared to those living in urban areas. Decreasing total fertility can indirectly lead to a decrease in maternal and child mortality. However, the decrease was steady in SSA countries. Therefore, appropriate efforts should be made to reduce the TFR in sub-Saharan countries, particularly in the Central and Western African sub-regions and among rural inhabitants. The government and health professionals should work toward meeting the reproductive and maternal health needs of the population.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
DT and ST were involved in this study from its inception through the design, acquisition, analysis, interpretation of data, and manuscript drafting. All authors contributed to the conception and design, analysis, and interpretation of the data and reviewed and revised the manuscript for important intellectual content, and also gave final approval for the version to be published and are accountable for all aspects of the study.
The authors extend their deepest thanks to the Demographic and Health Survey (DHS) data archivist, which allowed us to access the dataset.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
DHS, Demographic and Health Survey; TFR, Total Fertility Rate; SSA, Sub-Saharan Africa; WHO, World Health Organization.
1. Bongaarts J, Sinding S. Population Policy in Transition in the Developing World. Science, vol. 333. (2011). p. 574–6.
2. Bongaarts J. Population policy options in the developing world. Science. (1994) 263:2–7. doi: 10.31899/pgy1994.1008
3. World Population Prospects. United Nations Department of Economic and Social Affairs, Population Division. (2019). World Population Prospects 2019.
4. Bongaarts J, Casterline J. Fertility transition: is sub-Saharan Africa different? NIH public access. Popul Dev Rev. (2013) 38:153–168. doi: 10.1111/j.1728-4457.2013.00557.x
5. Zabin LS, Huggins GR, Emerson MR, Cullins VE. Partner effects on woman's intention to conceive: 'not with this parbrer.' Family Plann Perspect. (2000) 32:39–4. doi: 10.2307/2648147
6. Payne J. The impact of a reduced fertility rate on women's health. BMC Women's Health. (2004) 4:S11. doi: 10.1186/1472-6874-4-S1-S11
7. World Bank. Determinants and Consequences of High Fertility: A Synopsis of the Evidence Portfolio Review. (2010). Washington, D.C.: World Bank
8. Unitied Nation Department Department of Economics. World Fertility and Family Planning 2020, Highlights. New York, NY: Unitied Nation, Department of Economics
9. Conséquences de la croissance démographique dans les Pays les Moins Développés (PMD)? Keynote address presented at the Forty-second session of the United Nations Commission on Population and Development. New York 30 March-3 April 2009. Available from http://www.un.org/esa/population/cpd/cpd2009/comm2009.htm (accessed on November 18, 2009).
10. Bongaarts J, Feeney G. On the quantum and tempo of fertility. Pop and Devel Rev. (1998) 24:271–91. doi: 10.2307/2807974
11. Wesley, Y, Smeltzer S, Redeker, N, Walkeq, S, Palumbo, P. Repioductive Decision Making among Mothers with HIV-I. Health Care—Natl. (2000) 31:291–30. doi: 10.1080/073993300245159
12. Moyo W, Mbizvo MT. Desire for a future pregnancy among women from Zimbabwe in relation to their self-perceived risk of HIV infectiorU child mortality spontaneous abortion. AIDS Behav. (2004) 8:9-1. doi: 10.1023/B:AIBE.0000017521.26426.9d
13. Abbasi-Shavaz MJ. Low Fertility in Asia: Pathways, Consequences and Policy Implication. In: UN Expert Group Meeting on Fertility, Changing Population Trends and Development: Challenges and Opportunities New York. p. 21–2 (accessed on October 21–22, 2013).
14. Rammohan A. Fertility transition in South and Southeast Asia. ASEAN Econ Bull. (2004) 21:183–97. doi: 10.1355/AE21-2C
15. Saksena D, Srivastava J, Lehler E. Impact of child mortality and socio demographics attributes on family size: some data from Urban India. J Biosoc Sci. (1984) 16:119–26. doi: 10.1017/S0021932000014851
16. Kirk D, Pillet B. Fertility levels, a trend and differential in sub-Saharan Africa in the 1980's and 1990's. Stud Family Plann. (1988) 26:1–25.
17. John Hopkins University. Saving Women's lives. Population Reports 1999; 25. Baltimore, MD: John Hopkins University. p. 3-4.
18. Bulatao RA, Lee RD. Determinants of Fertility in Developing Countries. (1983). New York: Academic Press. p. 1–2.
20. Easterlin R. An economic framework for fertility analysis. Stud Family Plann. (1975) 6: 54–63. doi: 10.2307/1964934
21. Notestein FW. Economic problems of population change. In: Proceedings of the Eighth International Conference of Agricultural Economics. (1953). London: Oxford University Press. p. 13–31.
22. Canning D, Raja S, Yazbeck AS. Africa's demographic transition: dividend or disaster?. (2015) Available online at: https://openknowledge.worldbank.org/handle/10986/22036 (accessed on December 05, 2018).
23. Chola L, Pillay Y, Barron P, Tugendhaft A, Kerber K, Hofman K. Cost and impact of scaling up interventions to save the lives of mothers and children: taking South Africa closer to MDGs 4 and 5. Glob Health Action. (2015) 8:27265-15. doi: 10.3402/gha.v8.27265
24. Mbacké C. The persistence of high fertility in sub-Saharan Africa: a comment. Popul Dev Rev. (2017) 43:330–7. doi: 10.1111/padr.12052
25. Mokomane Z. Work-family Interface in sub-Saharan Africa: Challenges and Responses. (2013). Berlin, Germnay: Springer.
26. Upadhyay UD, Karasek D. Women's empowerment and ideal family size: an examination of DHS empowerment measures in sub-Saharan Africa. Int Perspect Sex R H.. (2012) 38:78–89. doi: 10.1363/3807812
27. Pullum T, Assaf S, Staveteig S. USAIDS, Comparisons of DHS Estimates of Fertility and Mortality with Other Estimates, Rockville, Maryland, USA. (2017).
28. Alkema L, Kantorova V, Menozzi C, Biddlecom A. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. Lancet, (2012) 381:1642–52. doi: 10.1016/S0140-6736(12)62204-1
30. The DHS Program. Available online at: http://dhsprogram.com/data/data-collection.cfm
31. Elkasabi M. Calculating fertility and childhood mortality rates from survey data using the DHS. rates R package. PLoS ONE. (2019) 14:1–22. doi: 10.1371/journal.pone.0216403
32. World Health Organization. South-East Asia: Health Situation and Trend Assessment: Total Fertility Rate (per Woman). (2020). Available online at http://origin.searo.who.int/entity/health_situation_trends/data/chi/TFR/en/
33. Shekar M, Yazbeck A, Hasan R, Bakilana A. Population Development in the Sahel : Policy Choices to Catalyze a Demographic Dividend. (2016). Available online at: https://openknowledge.worldbank.org/handle/10986/25293
34. Machiyama K. DHS Working Papers No 68. A reexamination of recent fertility declines in sub-Saharan Africa. (2010). Calverton, MD: ICF Macro.
35. Kirigia J, Barry S. Health challenges in Africa and the way forward. Int Arch Med. (2008) 1:27. doi: 10.1186/1755-7682-1-27
36. Prata N Passano P Rowen T Bell S Walsh J and Potts M. Where there are (few) skilled birth attendants. J Health Population Nutr. (2011) 29:81. doi: 10.3329/jhpn.v29i2.7812
37. Drishti. India's Falling Fertility Rate. Available online at: https://www.drishtiias.com/pdf/1596148669-indias-falling-fertility-rate.pdf
38. Temin M, Levine R. Start With A Girl: A New Agenda for Global Health. Washington, D.C.: The Center for Global Development (2009).
39. Levine R, Lloyd C, Greene M, Grown C. Girls Count: A Global Investment & Action Agenda. (2009). Washington DC: The Center for Global Development.
40. Sharan M, Ahmed S, May J, Soucat A. Family planning trends in sub-Saharan Africa: progress, prospects, and lessons learned. Yes Africa Can. (2011) 445:258643–1271798 012256.
41. Daniels K, Martinez GM, Nugent CN. Urban and Rural Variation in Fertility-related Behavior Among U.S. Women, 2011–2015. NCHS Data Brief . (2017) 297:1–8.
42. Kulu H. Why Fertility Levels Vary between Urban and Rural Areas?. Regional Studies. (2011). London, UK: Taylor & Francis (Routledge).
43. U.S. Census Bureau. Measuring America: Our Changing Landscape. (2016). Available from: https://www.census.gov/library/visualizations/2016/comm/acs-rural-urban.html?CID=acs-ruralurban (accessed May 15, 2014).
44. Meit M, Knudson A, Gilbert T, Yu AT, Tanenbaum E, Ormson E, et al. The 2014 Update of the Rural-Urban Chartbook. Bethesda, MD: Rural Health Reform Policy Research Center (2014).
45. CDC. Rural Health. Available from: https://www.cdc.gov/ruralhealth/ (accessed August 2, 2017).
46. Silverman R, Glassman A. Adolescent Fertility in Low- and Middle-Income Countries: Effects and Solutions, Kate McQueston Program Coordinator Center for Global Development. (2012). Washington, D.C.: Center for Global Development.
Keywords: pooled, total fertility rate, sub-Saharan Africa, demographic, health survey
Citation: Tesfa D, Tiruneh SA, Gebremariam AD, Azanaw MM, Engidaw MT, Kefale B, Abebe B, Dessalegn T and Tiruneh M (2023) The pooled estimate of the total fertility rate in sub-Saharan Africa using recent (2010–2018) Demographic and Health Survey data. Front. Public Health 10:1053302. doi: 10.3389/fpubh.2022.1053302
Received: 25 September 2022; Accepted: 27 December 2022;
Published: 26 January 2023.
Edited by:
Aristide Romaric Bado, Research Institute for Health Sciences (IRSS), Burkina FasoReviewed by:
Piyush Rai, AKS University, IndiaCopyright © 2023 Tesfa, Tiruneh, Gebremariam, Azanaw, Engidaw, Kefale, Abebe, Dessalegn and Tiruneh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Desalegn Tesfa,  ZGVzYWxlZ250ZXNmYTUwQGdtYWlsLmNvbQ==
ZGVzYWxlZ250ZXNmYTUwQGdtYWlsLmNvbQ==
†Present address: Belayneh Kefale, Department of Pharmacy, College of Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.