- School of Economics and Management, Tiangong University, Tianjin, China
Since the outbreak of COVID-19, there has been a large body of literature focusing on the relationship between the COVID-19 pandemic and young people. The purpose of this study is to explore the current research status and the specific mechanism of COVID-19's effects on young people based on related literature. This paper mainly used VOS viewer and CiteSpace software to conduct a scientometric analysis of 5,077 publications retrieved from the Web of Science database. The results show that the main contributors to the field were mainly from North America and Europe, and the trend of research focus was from shallow to deep. The five main research areas in the field were summarized by keyword clustering analysis as follows: lifestyle changes due to lockdown; changes in stress and emotions; psychological illness and trauma; risk perception and practice toward the epidemic; interventions and social support. Finally, they were linked by four pathways to form a framework that integrates the relationships between the five domains and between elements within each of them, revealing the mechanism of COVID-19's effect on young people. In addition, less studied but promising elements are also presented in the framework, such as research on special groups (disadvantaged socioeconomic groups and sexual minority youth) and extreme suicidal tendencies that deserve our further attention.
Introduction
Since the emergence of the Corona Virus Disease 2019 (COVID-19), the virus has rapidly swept the world due to its high infectiousness. As of September 2022, there were more than 600 million cumulative confirmed cases and more than 6 million deaths worldwide (1). Countries around the world have responded with various measures to control the spread of the virus. And in many cases, people have to reduce their social activities and keep a social distance. For this group of young people, social isolation (such as the closure of schools and social venues) has kept them in a state of long-term online learning and weakened their connections with teachers, classmates, and other social networks. At the same time, emerging adults who are about to enter society and seek employment also feel confused and uneasy about their futures (2). With COVID-19 now in its third year, the prolongation of such a public crisis event generates fear, sleep disorders, anxiety, depression, and other risk factors that affect the mental health of young people (3–5) and can even lead to unhealthy lifestyles, reduced physical fitness, and other physical problems in the future as a result (6).
So far, a large amount of literature has been published in this field to investigate and analyze the effects of COVID-19 on young people, and it can be said that the relationship between the COVID-19 pandemic and young people deserves our attention. However, the scope of research involves different countries and regions, the content of research is abundant, and the focus of research is different. In the face of the vast literature, some meta-analyses or reviews have existed, but most of them are relatively one-sided, and there is a lack of more comprehensive and systematic studies. Scientometrics, as a quantitative research method, enables a systematic and objective analysis of a large number of publications to identify the current development status and research focus in a particular field (7, 8). In this paper, we will collect and organize the literature in this field in the Web of Science database through the corresponding search strategy and visualize the retrieved literature by using VOS viewer and CiteSpace. The goal of this paper is to provide this field with a new way to understand knowledge distribution through visual analysis and to summarize the research status, hotspots, and main research framework in this field.
Compared with previous review articles on this topic, there are three main contributions as follows: (1) The current state of research (number of publications and leading countries, institutions, subject categories, journals, and references), research focus, and research trends are visualized to provide a new approach to understanding the field from a scientometric perspective. (2) Through keyword clustering analysis, five main research domains within the field are identified, and based on this, they are linked by four pathways to form a framework showing the influence relationships between them and their respective internal elements, thus revealing how the COVID-19 pandemic has affected young people. (3) Studies that are difficult to be noticed due to less research but still have the prospect of development (e.g., suicidal extremism, special groups such as disadvantaged socioeconomic groups and sexual minority youth) are also captured and presented in the framework.
Materials and methods
Data sources and search strategies
The Web of Science Core Collection (WoSCC) was selected as the data source for this study, with a large number of publications covering the most comprehensive range of literature possible. The search date for this study was November 4, 2022, and the search date range was 2020-01-01 to 2022-09-30, with the search term “TS = (COVID-19 OR SARS-CoV-2 OR Coronavirus disease 2019 OR severe acute respiratory syndrome coronavirus 2) AND TS = (teenager OR adolescent OR juvenile OR young OR child OR children OR offspring OR descendant OR junior OR son OR daughter).” After the search, the document types were restricted to “review” and “article,” and the language was restricted to English. In order to ensure that the results are more accurate and effective, after discussion with experts from related disciplines, it was determined that the Web of Science Categories should be limited to Public Environmental Occupational Health, Health Care Sciences Services, Psychology Multidisciplinary, Psychology Developmental, Psychology Clinical, Education Educational Research, Health Policy Services, Social Sciences Interdisciplinary, Social Work, Psychology Social, Sport Sciences, and Psychology Social. Then, the two authors continued to conduct manual screening to eliminate publications that were not related to the research theme. Finally, after deleting duplicate records, a total of 5,077 records were obtained, including 4,851 original research articles and 226 reviews. In summary, authoritative database sources, comprehensive search terms, rigorous category screening, and ultimately manual screening can effectively ensure the accuracy of the study sample.
Scientometric tools and functions
Visualization software
VOS viewer is a free JAVA-based software that focuses on the visualization of scientific knowledge through the use of literature data (9), and the version used in this article is VOS viewer1.6.17. We used the citation, co-citation, and co-occurrence functional modules of the software to visualize and analyze institutions, journals, references, and keywords. Each node in the visualization map represents a different parameter, such as institution, journal, keyword, etc. The larger the node, the greater its weight. Nodes are connected by links. Total Link Strength (TLS) is an important metric for identifying this type of visual graph, and the TLS value of a node refers to the number of times that node appears together with all other nodes (10). CiteSpace is a JAVA application for presenting the structure, patterns, and distribution of scientific knowledge (11). The version used in this article is CiteSpace V6.1.R2. The program focuses on analyzing the research progress in a field by using information such as literature authors, titles, keywords, abstracts, citations, etc. In this study, we used CiteSpace to mine the data and produce the dual-map overlay of the journals and the network visualization map of subject categories.
Visualization process
In the process of visual analysis by VOS viewer software, the basic parameters were set as follows: The visualization scale was set at 1.0, and the weight of the node size was total link strength; the layout used the default value; the algorithm for the clustering process using this software was the association strength of the normalization method, as well as a clustering resolution of 1.00 and a minimum cluster size of 1. Based on the above parameter settings, we performed citation analysis of institutions, co-citation analysis of journals and references, and co-occurrence analysis of keywords. The number of clusters in each visualization map will be automatically generated by the software's association strength algorithm.
This article used CiteSpace software to make the dual-map overlay of the journals, set the source circle size to 120, set the target circle size to 15, and checked Z scores. In the process of creating the visualization map of subject categories, the following parameters were set: Time Slicing was 2020 to 2022; Node Type was chosen as categories; Pruning was checked as pathfinder and pruning sliced networks; the rest were the default settings.
Results and discussion
Knowledge structure of research status
Publications and geographic distribution
Figure 1A presents the trends in the number of publications from 2020 to 2022 on a half-yearly basis. Overall, there is a growing body of research exploring the relationship between COVID-19 and young people: from 2020 onwards, the number of publications starts to increase significantly; from the second half of 2021 to the present, the upward trend plateaus. A small increase in the number of publications in this area is expected in the second half of 2022. From the search results, a total of 156 countries/regions have published articles in this research area. The country/region with the highest number of publications and citations was the USA, and its number far exceeded that of other countries, followed by England and China.
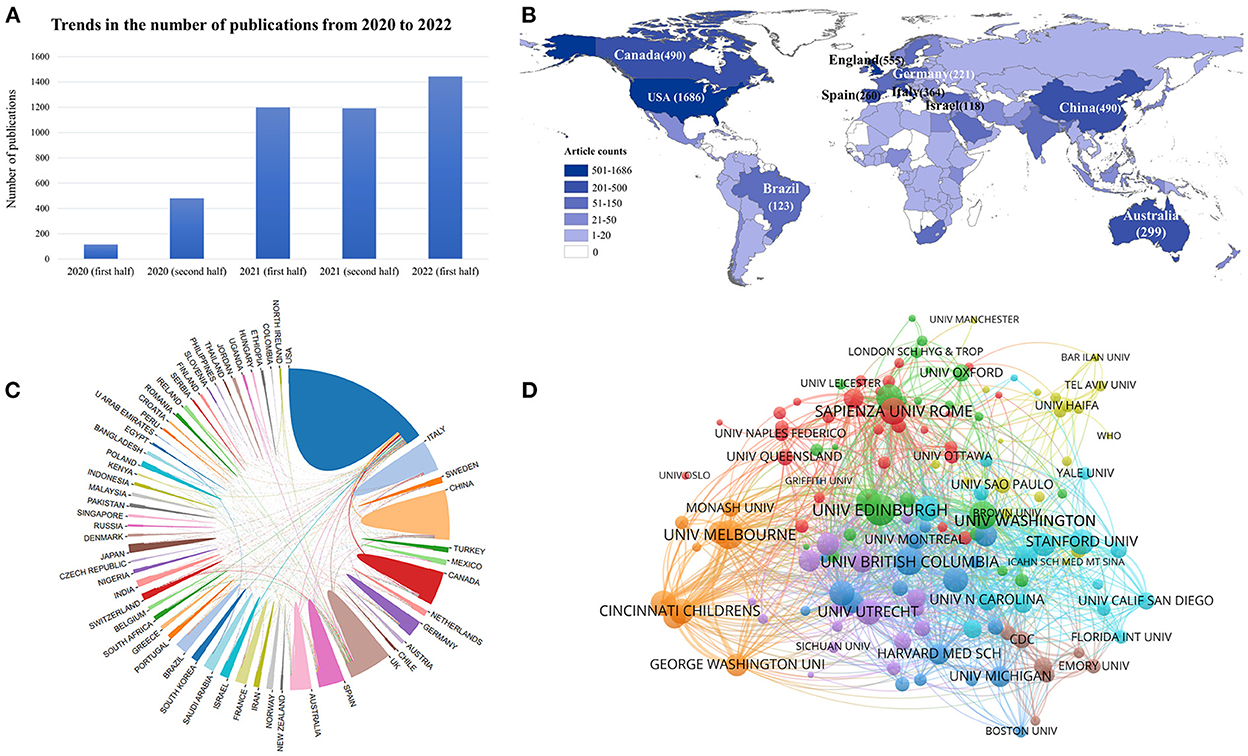
Figure 1. (A) Trends in the number of publications from 2020 to 2022. (B) Geographical distribution based on the number of articles issued by various countries/regions. (C) Inter-country/region cooperation relationship map. (D) Citation network visualization map of institutions.
Figure 1B shows a geographical distribution based on the number of articles issued by various countries or regions in the field of research on the relationship between COVID-19 and young people. This map allows us to visualize that the majority of articles came from North America, Western Europe, and East Asia. The inter-country/region cooperation relationship map (Figure 1C) shows the international partnerships between countries/regions with at least 20 publications by connecting the lines of different colors. We can clearly see that the USA and the UK were the countries that cooperated the most with other countries.
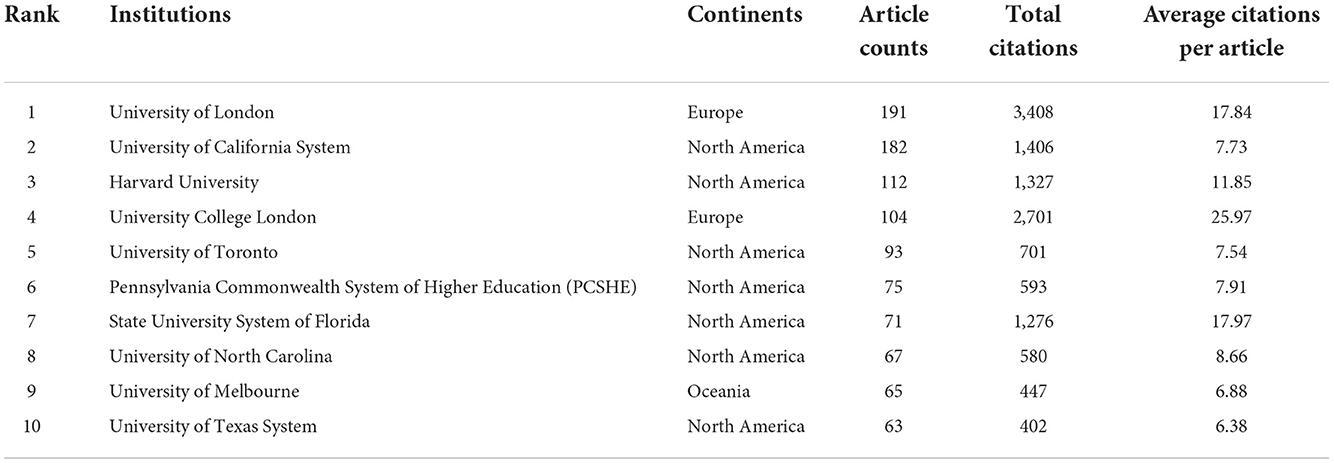
A total of 6,226 institutions have published articles related to this topic. Table 1 shows the top 10 most active institutions. Overall, these prolific institutions were mainly from Europe and North America. Figure 1D shows the citation network visualization map of institutions. By limiting the documents of the institutions to at least 15, this figure presents a total of 140 nodes representing institutions and 3,290 links. The institution with the highest TSL value was the University of Edinburgh from England (TLS = 324), which had a strong influence among the institutions. Followed by the University of Melbourne (TLS = 288) from Australia and the University of Washington (TLS = 270) from the USA.
Analysis of subject categories and interdisciplinary
In this paper, we analyzed the subject categories obtained from the search results using CiteSpace software and created a network visualization map consisting of several nodes representing the subject categories shown in Figure 2A. Nodes with a centrality value >0.1 are key nodes and carry a purple outer ring. The higher the centrality value of a node, the greater its influence. The top three disciplinary categories with the highest centrality values were PUBLIC, ENVIRONMENTAL and OCCUPATIONAL HEALTH (0.7), PSYCHOLOGY, MULTIDISCIPLINARY (0.29), and PSYCHIATRY (0.28).
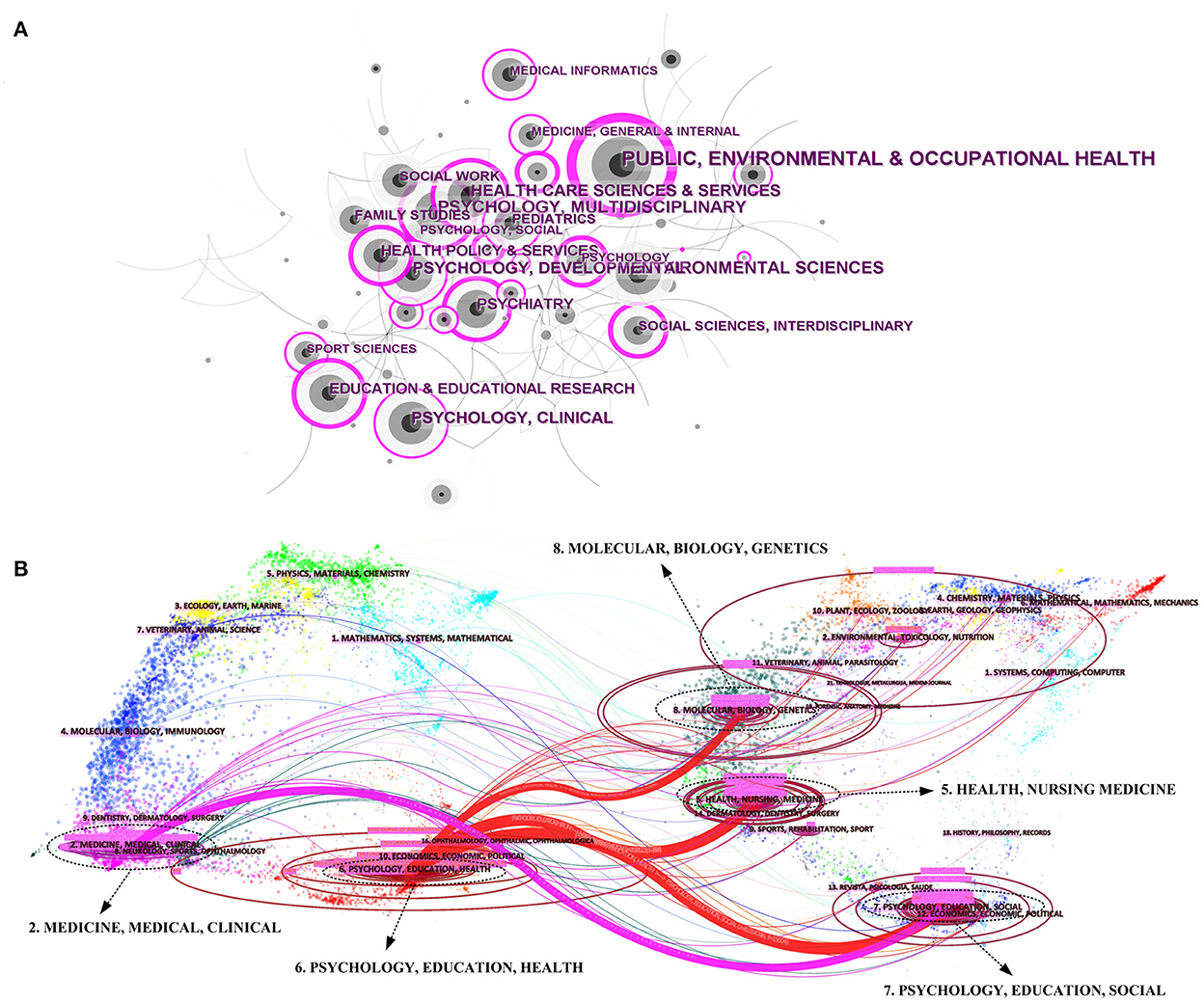
Figure 2. (A) The network visualization map of subject categories created with CiteSpace software. (B) The dual-map overlay of the journals.
The dual-map overlay of the journals (Figure 2B) reflects the topic distribution of journals, which are clustered and named by the LLR algorithm. In the final result presentation, the citing graph of journals is on the left, the cited graph of journals is on the right, and the curves are the citation links (12, 13). On the left side, the focus was on the topics “6. PSYCHOLOGY, EDUCATION, HEALTH” and “2. MEDICINE, MEDICAL, CLINICAL,” which were connected to “5. HEALTH, NURSING, MEDICINE,” “7. PSYCHOLOGY, EDUCATION, SOCIAL,” and “8. MOLECULAR, BIOLOGY, GENETICS” on the right side by four connecting lines. These four lines were the most dominant citation paths among journals in this field. And on the right side of the graph, it can be seen that the topic distribution of cited journals was more dispersed.
Authoritative journals and highly cited references
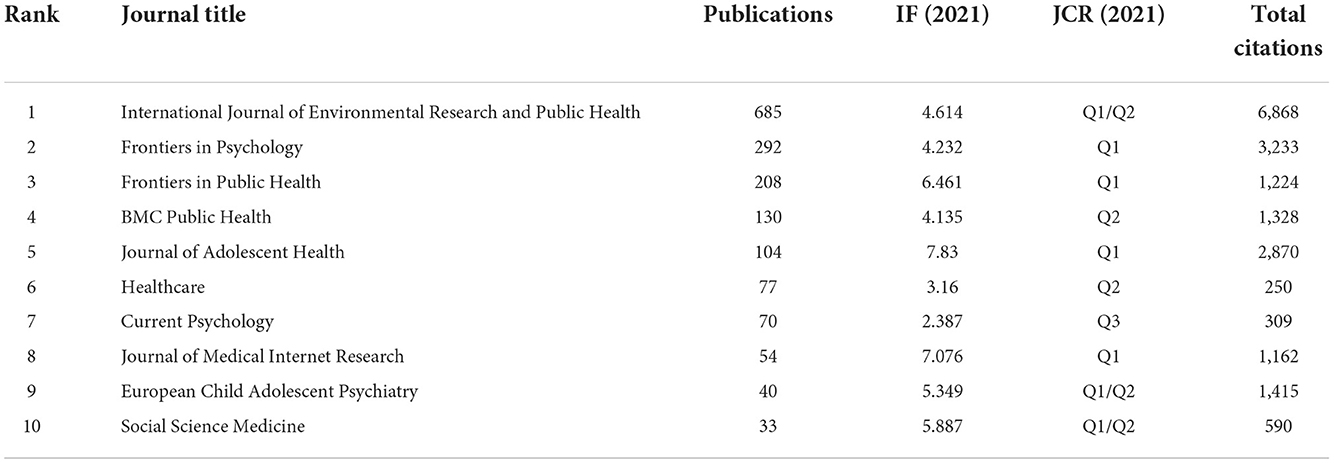
The journals with the most contributions are listed in Table 2. Figure 3A shows a visualization of the co-citation network of journals, which presents the journals with at least 180 citations in the field, forming a total of 170 nodes with 14,188 links in the graph. The top three journals with the largest TSL values were INTERNATIONAL JOURNAL OF ENVIRONMENTAL RESEARCH AND PUBLIC HEALTH (TSL = 96,741), PLOS ONE (TSL = 68,082), and PSYCHIATRY RESEARCH (TSL = 61,294). These three journals had the strongest correlation with other journals in the field.

Figure 3. (A) Co-citation network visualization map of journals by VOS viewer. (B) Co-citation network visualization map of references by VOS viewer.
Figure 3B shows the co-citation network visualization map of references. One hundred fifty-eight references with at least 40 citations were filtered out to form this visualization map. Among them, the reference with the largest TLS value was The psychological impact of quarantine and how to reduce it: rapid review of the evidence (14) published in 2020 by Brooks SK et al. in the Lancet, which shows that this article had the most associations with other articles.
Research focus and trends
Changes in co-occurrence keywords
The analysis of high frequency co-occurrence keywords not only identifies the research focus but also reveals the changing themes and trends. We filtered keywords that occurred 30 or more times as high-frequency keywords and excluded keywords that were duplicated with the search terms to finally generate the co-occurrence overlay visualization map (Figure 4A).
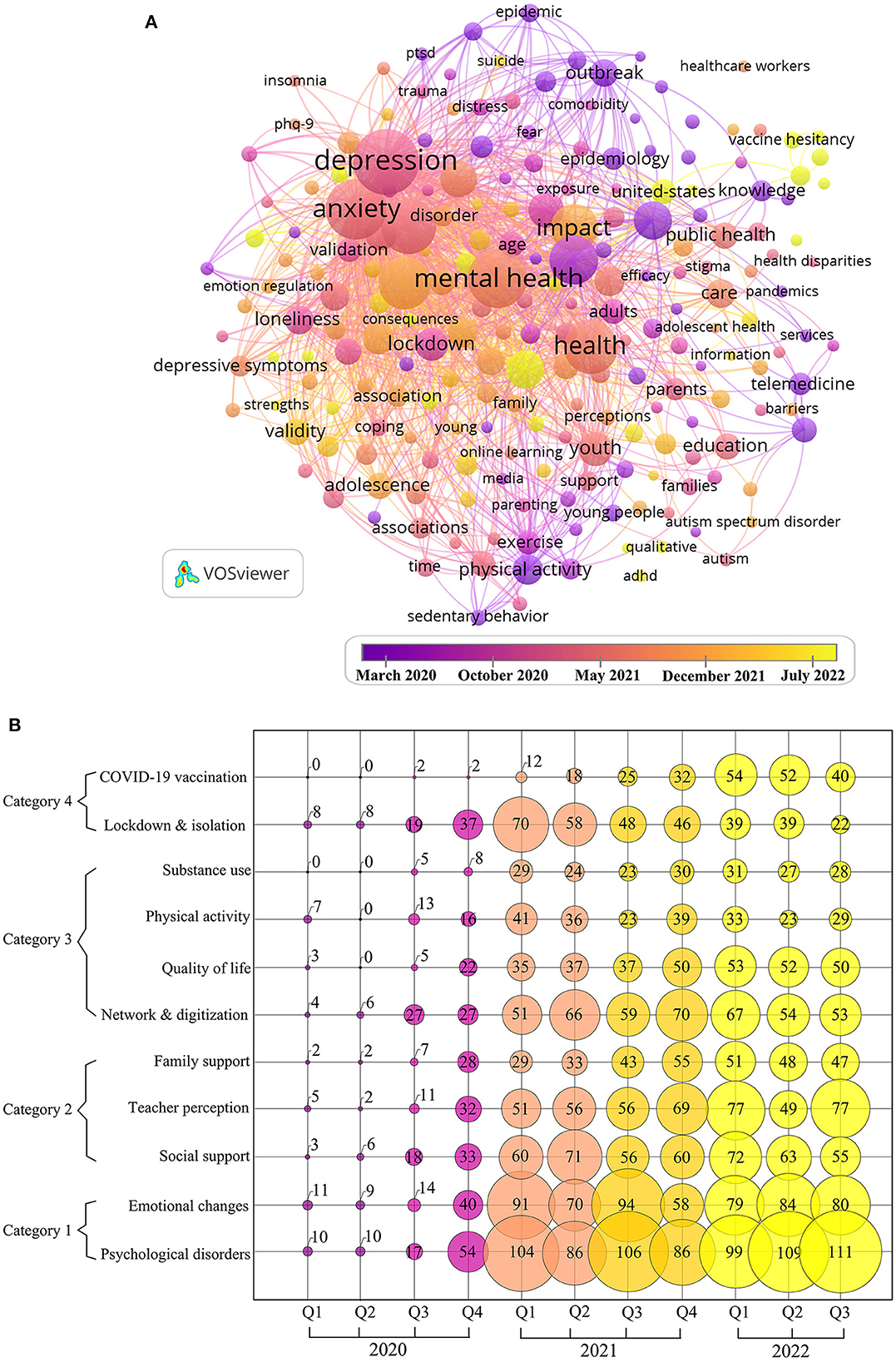
Figure 4. (A) Co-occurrence overlay visualization map of high-frequency keywords. (B) Bubble charts of research topics.
In Figure 4A, the keywords with the largest nodes, i.e., the most co-occurrences, are “depression,” “anxiety,” “mental health,” “stress,” “impact,” “prevalence,” etc., indicating that most of the research in this area has focused on mental health. The color of each node in the figure is determined by the average appearing year (AAY), and the color of the nodes with earlier appearing years is purple, while the color of the nodes with later appearing years is yellow. The number of keywords obtained for 2020, 2021, and the first half of 2022 were 2,140, 6,580, and 4,481, respectively, indicating that the scope study is expanding rapidly and showing a further growth trend.
At the beginning of the epidemic in 2020, research was focused on: “outbreak,” “social isolation,” “quarantine,” “outcomes,” “fear,” “worry,” “mortality,” etc., which reflects the harm caused by the spread of the epidemic itself and the intuitive feelings it brought to young people. In 2021, the co-occurrence keywords were mainly focused on words like “mental health,” “anxiety,” “depression,” “disorders,” “prevalence,” and “symptoms,” etc. This indicates that medium term concerns were more serious psychological affects. Since entering 2022, keywords such as “therapy,” “vaccine,” “sex,” “ADHD,” “suicide,” “predictors,” and “adjustment” have emerged. People's attention has shifted from the initial outbreak itself to the treatment of the harm caused by the outbreak and more in-depth and detailed research, such as the investigation of the hesitancy of young people regarding vaccines (15, 16), the study of the sexuality of adolescents and young adults (17, 18), and the study of the impact of the epidemic on children and adolescents with ADHD (19).
Cumulatively, studies of the impact of COVID-19 on young people show a trend from superficial to deeper, evolving from focusing on the initial stage of the outbreak to exploring more subtle changes.
Evolution of research topics
After sorting the keywords by frequency and focusing on the top 100 most frequently occurring keywords, a bubble chart of this study area by quarterly changes between January 2020 and September 2022 is shown in Figure 4B with 11 topics and 4 main categories, which can visually display the change in the heat of the main research hotspots in the field through the evolution of time.
The content of Category 1 “mental health” (“emotional changes” and “psychological disorders”) is the most researched, indicating that the mental health of young people has been receiving great academic attention from 2020 to 2022, and its content mainly focuses on issues such as depression, anxiety, stress, and loneliness in young people. Although interest declined at the end of 2021, it rebounded rapidly afterward.
Category 2 focuses on “support from various groups.” Except for the topic “teacher perceptions,” the popularity of other topics in this category has decreased in 2022.
Category 3 mainly discusses “impact on lifestyle.” The main components of the topics “physical activity” and “network & digitization” are the investigation and confirmation of the decrease in physical activity and the increase in internet use among young people during the epidemic (20). The year 2021 is the culmination phase of these topics, followed by a decline, suggesting that academic interest in these topics is declining. However, the topics “substance use” and “quality of life” in category 3 have not fluctuated much in the past 2 years and will continue to receive attention in the future.
Category 4, “epidemic control,” includes topics such as “lockdown and isolation” and “COVID-19 vaccination.” “Lockdown and isolation,” which focuses on the outbreak itself and the immediate impact of lockdown and isolation on young people, has received considerable attention but is now less and less studied. Meanwhile, the popularity of the COVID-19 vaccination has increased in 2022. This is because, since the emergence of the COVID-19 vaccine as one of the major measures for people to deal with COVID-19, its safety and efficacy, as well as young people's attitudes toward the vaccine, have been the subject of research.
Main research domain and framework
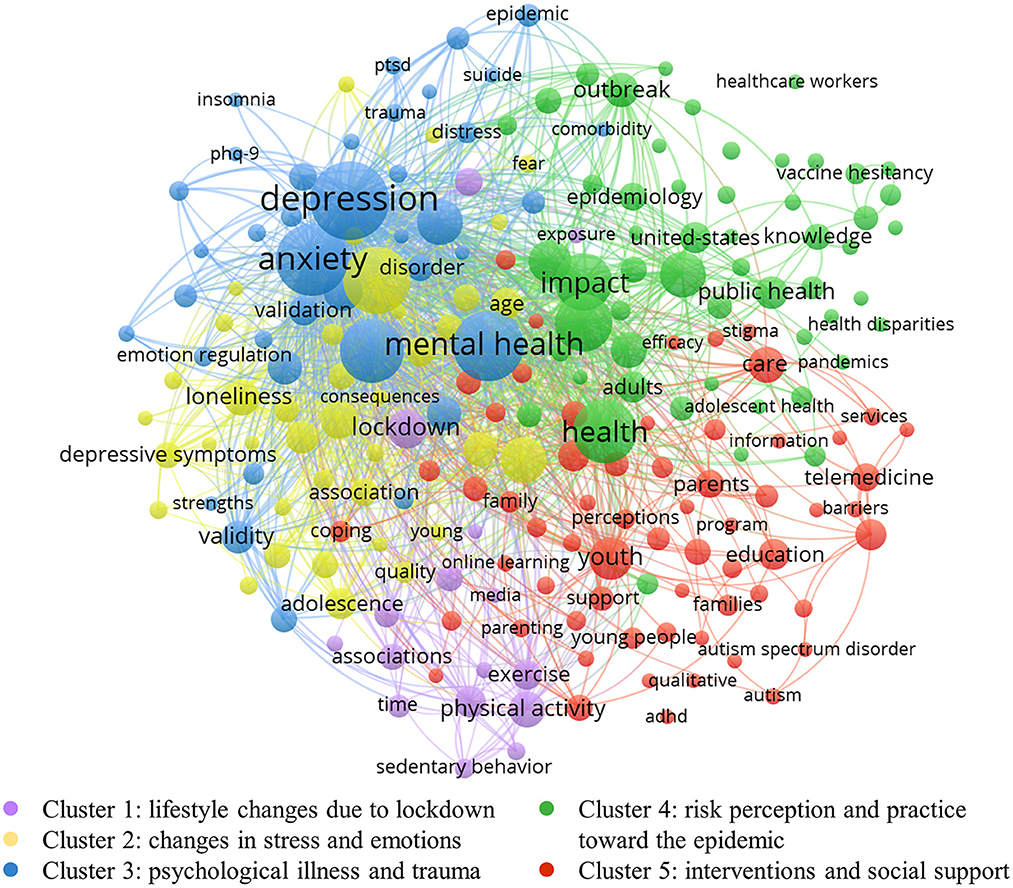
Cluster analysis of keywords
Cluster analysis of frequently occurring keywords facilitates a precise grasp of the main knowledge distribution in the field, which is essential for understanding hotspots and anticipating trends. In this study, the keywords were visualized and clustered by VOS viewer. The number of keyword occurrences was limited to 30 or more, and duplicate or unreasonable keywords were manually removed, thus forming the keyword network visualization map (Figure 5). Based on the association strength algorithm, the software divided the high-frequency keywords into five clusters. However, over-reliance on the content of high-frequency keywords for the analysis may result in the five clusters obtained from the results being difficult to achieve comprehensive coverage of all information or having partial overlap between the clusters. Therefore, after understanding and analyzing the five clusters, we imported the data into CiteSpace for keyword clustering analysis. Then, after verifying the Silhouette score several times, we confirmed that the five clusters here are all reasonable. Finally, by inviting three experts in adolescent mental health and two experts in youth sports to study and discuss the keywords in each cluster, we named each of these five clusters, which are shown below:
Cluster 1 (lifestyle changes due to lockdown, purple nodes): The main keywords included in this cluster are: “lockdown,” “physical activity,” “screen time,” “substance use,” “wellbeing,” etc. Lockdown is one of the essential preventive and control measures during the COVID-19 pandemic to prevent the transmission and spread of the epidemic. However, because of the social isolation and school closures, the living conditions of young people are very different compared to those of the past. From several of the most significant nodes in the cluster, it can be summarized that the research in this cluster focused on the changes in physical activity, internet use, and substance use among young people as a result of the lockdown under COVID-19.
Cluster 2 (changes in stress and emotions, yellow nodes): The prominent keywords in this cluster are: “stress,” “loneliness,” “emotion,” “fear,” etc. Children and adolescents are still immature in their physical and psychological development and have a limited ability to cope with external stress and stabilize their emotions, while young people entering society are also facing a volatile situation pattern. Therefore, the changes in stress and emotions among young people during the epidemic have received much attention and have led to a series of related studies, which is another major research area in this field.
Cluster 3 (psychological illness and trauma, blue nodes): This cluster reflects the increased stress and emotional distress associated with the COVID-19 pandemic, leading to the onset of some psychological illness and trauma in young people. The majority of the literature in this area highlights the impact of COVID-19 as a health crisis on the development of psychological illness in young people, which is one of the most important and typical topics in these clusters. The main keywords included in this cluster are: “mental health,” “depression,” “anxiety,” “disorders,” “PTSD,” etc.
Cluster 4 (risk perception and practice toward the epidemic, green nodes): the main keywords included in this cluster are: “risk,” “health,” “attitude,” “knowledge,” “vaccination,” etc. The high risk of COVID-19 puts people at constant risk of infection, but subjective risk perceptions of the epidemic often vary from person to person. Young people's risk perceptions of outbreaks influence their outbreak prevention behaviors and mental health status, and this area has received attention in academic circles.
Cluster 5 (interventions and social support, red nodes): COVID-19 and its attendant controls have a significant impact on young people, so another major area of research on how to provide appropriate early interventions and strong social support for young people is presented in this cluster. The main keywords included in this cluster are: “intervention,” “support,” “service,” “education,” “parents,” etc.
The mechanism of COVID-19's effect on young people
By reading and sorting out the representative literature involved in each cluster, we identified the relationships among the clusters and produced the framework of the effect of COVID-19 on young people (Figure 6). The colored boxes in the figure coincide with the colors to which the clusters belong in Figure 5. The text in the dashed box indicates that it is not represented in the co-occurring keyword clusters due to the small number of existing studies, but it still deserves our further attention.

Figure 6. The framework of the effect of COVID-19 on young people, based on high-frequency keywords and cluster analysis.
Mechanism between the five clusters
In Figure 6, there are four pathways expressing the relationship between these five clusters in the effect mechanism. Firstly, pathway 1 shows that the global outbreak of COVID-19 has caused countries and regions to adopt lockdown measures to deal with this highly infectious virus, which has changed the lifestyles of young people (Cluster 1). The disruption of the formerly standard and healthy lifestyle of young people has had a consequent impact on their mental health status. Secondly, pathway 2 is a shift from Cluster 2 to Cluster 3. That is, increased stress and fluctuating emotions (e.g., the emergence of adverse feelings such as fear, loneliness, etc.) in young people during COVID-19 further intensify into serious psychological disorders and severe trauma (e.g., anxiety, depression, PTSD, etc.). Pathway 2 reflects this exacerbation process. In addition, from pathway 3, the perceived risk profile and action performance of young people in the context of the COVID-19 pandemic are also a major research component (Cluster 4). The level of risk perceived by young people facing such a major public health hazard and the uncertainty and uncontrollability of that risk will increase the psychological stress and negative emotions of individuals and have an impact on their mental health. Finally, pathway 4 flows to the other four clusters centered on intervention and social support for young people (Cluster 5). Given that the aforementioned COVID-19 has led to lifestyle changes, severe risk perceptions of the epidemic, increased stress, mood swings, and psychological disorders among young people, interventions and strong social support are needed to address the current unpromising situation of young people.
We focus on the specific mechanisms of effect within each cluster as follows.
Effect mechanisms within each cluster
Effect mechanism in cluster 1: Lifestyle changes due to lockdown
The impact of the lockdown measures on young people's lifestyles is reflected in the purple box in Figure 6. First, there has been a general increase in screen time use by young people who are confined to their homes due to the need for online learning and contact with family and friends via the Internet (20, 21). However, with the increase in screen time, game addiction and compulsive internet use have been exacerbated, especially among adolescents and young adults (22, 23). This may be a risk factor for worsening sleep quality, increased stress, and the development of depression and anxiety symptoms (24–26). Second, it is reflected in the reduction of physical activity among young people as a result of the lockdown, which has now been confirmed by numerous studies (27–29). More exercise can be effective in protecting one's mental health, such as preventing the emergence and development of anxiety and depression (30, 31), but the current situation of young people today is deviating from this. Third, in the context of COVID-19, substance use among young people has changed (32, 33). Since the beginning of social distance, studies have found increased alcohol and marijuana use among adolescents (34, 35), and there are also studies linking the emergence of the COVID-19 pandemic to increased nicotine use and prescription drug abuse (36). For young people in the early exploratory stages of substance use, uncontrolled substance use during COVID-19 has the potential to lead to the emergence of substance use disorders, increased dependence, and poorer mental health (37, 38).
Effect mechanism in cluster 2: Changes in stress and emotions
Children and adolescents are one of the most vulnerable groups in this pandemic in terms of the development of psychological abnormalities (39, 40). It was found that their stress during this epidemic mainly stemmed from the inability to participate in social activities/normal daily activities and important plans/events being canceled or postponed (41). Children and adolescents who did not originally have mental health disorders experienced a significant deterioration in mood during the pandemic (42), and feelings of anxiety and sadness were prevalent among them (43). It can be argued that the increased stress and unstable emotions caused by COVID-19 may reduce young people's quality of life and life satisfaction, affecting their daily wellbeing. Also, young adults exhibit strong concerns and feelings of loneliness during the COVID-19 pandemic (44, 45), which would predict the emergence of certain mental health symptoms. Compared with older adults, young adults are more susceptible to stress-induced mood swings and respond to stressful situations with fewer resources and experience. Their greatest stress stemmed mainly from uncertainty, such as not knowing when the COVID-19 pandemic will end (41). Young adults who have just reached adulthood are likely to be confused and worried about their future in the face of a difficult college life and a worsening economic environment, which could have a serious impact on their self-efficacy and undoubtedly reduce their sense of wellbeing.
Effect mechanism in cluster 3: Psychological illness and trauma
Overall, the prevalence of anxiety and depression was much higher than before the COVID-19 pandemic (41, 46, 47), and more pronounced in females (41). The COVID-19 pandemic is sufficient as a life-threatening infection to cause post-traumatic stress disorder (PTSD), which may have more severe consequences for children and adolescents (48, 49). Young people's unattended and unimproved psychological problems may lead to extreme tendencies if they continue to grow. A portion of the research has addressed the impact of the COVID-19 pandemic on suicidal ideation and behavior among young people, but because it has not been adequately studied, this portion is shown in the blue dashed box. According to related studies, pediatric mental health-related ED visits among adolescents aged 12–17 years increased by 31% in the USA beginning in April 2020, compared with 2019 data (50). In May 2020, there was also an increase in the number of ED visits for suspected suicide attempts among young people aged 12–25 years (51). In Australia, an increase in the number of contacts regarding suicide/self-harm was also found through helplines used by children and adolescents (52). Of particular interest to us is the fact that an increase in suicide rates among young people was not found in some areas early in the outbreak (53, 54), suggesting that suicidal ideation and behavior among young people may also increase cumulatively over time during the epidemic (55, 56). Further research is still necessary to determine whether COVID-19 caused the rise in the suicide rate among young people.
Effect mechanism in cluster 4: Risk perception and practice toward the epidemic
It was found that young adults perceived a higher risk than older adults during the epidemic (57) and exhibited higher anxiety values (58). This higher risk perception may be related to the high exposure to COVID-19 information on social media and the emotions of anger and fear (59). Adolescents, on the other hand, showed a lower perception of risk, which could lead to their worse practice performance (60). Adolescence is a stage of life that experiences excitement and adventure, and as such, some adolescents may feel invulnerable and fail to comply with preventive measures. Also, there is a strong correlation between COVID-19 risk perception and vaccination status: individuals with a higher COVID-19 risk perception are more likely to be vaccinated. In addition, there are specific groups that differ in their risk perception. Some studies have shown that young people from disadvantaged socioeconomic groups still have a lower level of awareness and acceptance of COVID-19 (61, 62). Unfortunately, this gap is also reflected in studies of health disparities among young people facing COVID-19. Young people may differ in their vulnerability and susceptibility to COVID-19 depending on family conditions, race, etc. For example, children from low-income families (63) and black or Spanish children (64, 65) have significantly higher rates of COVID-19 infection and mortality. Research has found that youth who identify as sexual minorities experienced higher levels of disruption and adversity during the pandemic (66). And sexual minority youth are more vulnerable and affected than other cisgender and heterosexual peers (67, 68). There is a lack of research on such groups, which is shown in the green dashed box.
Effect mechanism in cluster 5: Interventions and social support
Social support could help young people face challenges. Positive teacher-student relationships can help young people in the student phase to effectively improve their mental health (69, 70). A survey found that more than two-thirds of teens said communication with teachers decreased during the pandemic (71). Enhancing students' school connectedness has been shown to have substantial protective effects on health and wellbeing during adolescence and adulthood (66). Therefore, those working in education should pay attention to this issue and increase student-teacher interaction to meet the social and emotional needs of students during COVID-19. Next, family relationships act as a double-edged sword that has a dual impact on young people who are closed to home. On the one hand, it is seen that many adolescents have experienced significant negative changes in their relationships with their parents, such as having more anger, arguments, and resentment, compared to the pre-pandemic period (72). And these poor parent-child relationships are risk factors for the development of anxiety and depressive symptoms (73). On the other hand, positive and stable family relationships help to alleviate mental health problems in young people (74). It was found that families with high levels of education were effective in alleviating adolescents' stress and emotional fluctuations during the COVID-19 pandemic, while adolescents from low/moderately educated families experienced more dramatic and negative changes in their emotional health (75). In addition, the emergence of telemedicine in a lockdown setting offers a new intervention to help young people respond to the COVID-19 pandemic and has proven to be effective (76, 77). Telemedicine and specific practices for dealing with various conditions deserve to be further explored in the future to support and help young people with adverse mental health conditions.
Limitations
First, although this study tried to collect data as accurately and comprehensively as possible, the database selected for this paper was the Web of Science. There are also databases such as PubMed, Google Scholar, and Scopus that were not covered, which may lead to the omission of a small number of relevant articles. Second, this paper obtained the main research domains in this field by clustering keywords, which is not comprehensive. This is because it relies too much on keyword content analysis, but does not provide enough in-depth knowledge of specific reviews, which is the result of the shortcomings of bibliometrics. Therefore, future studies need to be combined to further elucidate how the COVID-19 pandemic has affected young people from multiple perspectives (including country, discipline, study design, etc.).
Conclusion
Since the beginning of 2020, the number of publications exploring the relationship between COVID-19 and young people has increased, the scope of studies has expanded, and the content of studies has been refined. The current research in this area is mainly from North America and Europe, and systematic and comprehensive studies across regions still need to be explored. The effect of the COVID-19 pandemic on young people has been focused on mental health, as evidenced by a large body of literature. The research hotspots have gradually evolved from focusing on the superficial description in the early stages of the outbreak and the intuitive impact on young people to exploring more in-depth and detailed psychological problems and countermeasures.
In this study, the literature in this field was classified into five main research domains through keyword clustering analysis. Linking these five domains by four pathways helps us to reveal the mechanism of COVID-19's effect on young people and to identify research content that has not yet received much attention but has some promise for the future. The development of specific groups (young people from disadvantaged socioeconomic groups, sexual minority adolescents) and extreme tendencies (suicide) among young people during the COVID-19 period deserve further attention.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XL proposed the topic and designed the overall article. JY analyzed the data and wrote the article. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Social Science Fund of China (Grant Number 22BGL223).
Acknowledgments
The authors thank all the experts who provided guidance and suggestions for this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1052727/full#supplementary-material
References
1. WHO. Coronavirus Disease (COVID-19) Dashboard. (2022). Available online at: https://covid19.who.int/ (accessed September 12, 2022).
2. Gittings L, Toska E, Medley S, Cluver L, Logie CH, Ralayo N, et al. 'Now my life is stuck!': experiences of adolescents and young people during COVID-19 lockdown in South Africa. Glob Public Health. (2021) 16:947–63. doi: 10.1080/17441692.2021.1899262
3. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
4. Chtourou H, Trabelsi K, H'Mida C, Boukhris O, Glenn JM, Brach M, et al. Staying physically active during the quarantine and self-isolation period for controlling and mitigating the COVID-19 pandemic: a systematic overview of the literature. Front Psychol. (2020) 11:1708. doi: 10.3389/fpsyg.2020.01708
5. Orgiles M, Morales A, Delvecchio E, Mazzeschi C, Espada JP. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front Psychol. (2020) 11:579038. doi: 10.3389/fpsyg.2020.579038
6. Chaddha A, Robinson EA, Kline-Rogers E, Alexandris-Souphis T, Rubenfire M. Mental health and cardiovascular disease. Am J Med. (2016) 129:1145–8. doi: 10.1016/j.amjmed.2016.05.018
7. Fang Y, Yin J, Wu BH. Climate change and tourism: a scientometric analysis using CiteSpace. J Sustain Tour. (2018) 26:108–26. doi: 10.1080/09669582.2017.1329310
8. Wu HY, Zhou Y, Xu LX, Tong LJ, Wang YL, Liu BL, et al. Mapping knowledge structure and research frontiers of ultrasound-induced blood-brain barrier opening: a scientometric study. Front Neurosci. (2021) 15:706105. doi: 10.3389/fnins.2021.706105
9. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. (2010) 84:523–38. doi: 10.1007/s11192-009-0146-3
10. Lv W, Zhao X, Wu P, Lv J, He H. A Scientometric analysis of worldwide intercropping research based on web of science database between 1992 and 2020. Sustainability. (2021) 13:2430. doi: 10.3390/su13052430
11. Chen C. CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inform Sci Technol. (2006) 57:359–77. doi: 10.1002/asi.20317
12. Chen C, Dubin R, Kim MC. Emerging trends and new developments in regenerative medicine: a scientometric update (2000–2014). Expert Opin Biol Ther. (2014) 14:1295–317. doi: 10.1517/14712598.2014.920813
13. Chen C, Leydesdorff L. Patterns of connections and movements in dual-map overlays: a new method of publication portfolio analysis. J Assoc Inform Sci Technol. (2014) 65:334–51. doi: 10.1002/asi.22968
14. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
15. Dai HY, Barrington-Trimis JL, Unger JB, Baezconde-Garbanati L, Leventhal AM. Patterns and mediators of racial and ethnic disparities in COVID-19 vaccine hesitancy among young adults. Prev Med. (2022) 159:107077. doi: 10.1016/j.ypmed.2022.107077
16. Liu Y, Ma Q, Liu H, Guo Z. Public attitudes and influencing factors toward COVID-19 vaccination for adolescents/children: a scoping review. Public Health. (2022) 205:169–81. doi: 10.1016/j.puhe.2022.02.002
17. Gomez-Castro J, Cerecero-Garcia D, Vermandere H, Bautista-Arredondo S. Changes in sexual behavior, PrEP use, and COVID-19 experience among men who have sex with men in Mexico. AIDS Behav. (2022) 26:3451–8. doi: 10.1007/s10461-022-03688-4
18. Zulaika G, Bulbarelli M, Nyothach E, van Eijk A, Mason L, Fwaya E, et al. Impact of COVID-19 lockdowns on adolescent pregnancy and school dropout among secondary schoolgirls in Kenya. BMJ Global Health. (2022) 7:e007666. doi: 10.1136/bmjgh-2021-007666
19. Ogundele MO, Ayyash HF, Ani C. The impact of COVID-19 pandemic on services for children and adolescents with ADHD: results from a survey of paediatricians in the United Kingdom. Aims Public Health. (2022) 9:542–51. doi: 10.3934/publichealth.2022037
20. Kharel M, Sakamoto JL, Carandang RR, Ulambayar S, Shibanuma A, Yarotskaya E, et al. Impact of COVID-19 pandemic lockdown on movement behaviours of children and adolescents: a systematic review. BMJ Global Health. (2022) 7:e007190. doi: 10.1136/bmjgh-2021-007190
21. Trott M, Driscoll R, Irlado E, Pardhan S. Changes and correlates of screen time in adults and children during the COVID-19 pandemic: a systematic review and meta-analysis. EClinicalMedicine. (2022) 48:101452. doi: 10.1016/j.eclinm.2022.101452
22. Singh S, Datta M, Gupta P, Batra S. Predictors of 'problematic internet use' among adolescents and adults amid the pandemic in India. Clin Epidemiol Global Health. (2022) 15:101036. doi: 10.1016/j.cegh.2022.101036
23. Teng Z, Pontes HM, Nie Q, Griffiths MD, Guo C. Depression and anxiety symptoms associated with internet gaming disorder before and during the COVID-19 pandemic: a longitudinal study. J Behav Addict. (2021) 10:169–80. doi: 10.1556/2006.2021.00016
24. Fernandes B, Biswas UN, Tan-Mansukhani R, Vallejo A, Essau CA. The impact of COVID-19 lockdown on internet use and escapism in adolescents. Revista De Psicologia Clinica Con Ninos Y Adolescentes. (2020) 7:59–65. doi: 10.21134/rpcna.2020.mon.2056
25. Dong H, Yang F, Lu X, Hao W. Internet addiction and related psychological factors among children and adolescents in China during the Coronavirus disease 2019 (COVID-19) epidemic. Front Psychiatry. (2020) 11:00751. doi: 10.3389/fpsyt.2020.00751
26. Wang JM, Li W, Ding L, Chen SL. The relationship between duration of smartphone uses and anxiety in university students during the COVID-19 Outbreak. Int J Environ Res Public Health. (2022) 19:6620. doi: 10.3390/ijerph19116620
27. Knight RL, McNarry MA, Runacres AW, Shelley J, Sheeran L, Mackintosh KA. Moving forward: understanding correlates of physical activity and sedentary behaviour during COVID-19 in children and adolescents-an integrative review and socioecological approach. Int J Environ Res Public Health. (2022) 19:1044. doi: 10.3390/ijerph19031044
28. Rossi L, Behme N, Breuer C. Physical activity of children and adolescents during the COVID-19 pandemic-a scoping review. Int J Environ Res Public Health. (2021) 18:11440. doi: 10.3390/ijerph182111440
29. Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. (2021) 7:e000960. doi: 10.1136/bmjsem-2020-000960
30. Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. (2018) 175:631–48. doi: 10.1176/appi.ajp.2018.17111194
31. Schuch FB, Stubbs B, Meyer J, Heissel A, Zech P, Vancampfort D, et al. Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress Anxiety. (2019) 36:846–58. doi: 10.1002/da.22915
32. Horigian VE, Schmidt RD, Feaster DJ. Loneliness, mental health, and substance use among US young adults during COVID-19. J Psychoactive Drugs. (2021) 53:1–9. doi: 10.1080/02791072.2020.1836435
33. Masonbrink AR, Middlebrooks L, Gooding HC, Abella M, Hall M, Burger RK, et al. Substance use disorder visits among adolescents at children's hospitals during COVID-19. J Adolesc Health. (2022) 70:673–6. doi: 10.1016/j.jadohealth.2021.12.024
34. Jacob L, Smith L, Armstrong NC, Yakkundi A, Barnett Y, Butler L, et al. Alcohol use and mental health during COVID-19 lockdown: a cross-sectional study in a sample of UK adults. Drug Alcohol Depend. (2021) 219:108488. doi: 10.1016/j.drugalcdep.2020.108488
35. Papp LM, Kouros CD. Effect of COVID-19 disruptions on young adults' affect and substance use in daily life. Psychol Addict Behav. (2021) 35:391–401. doi: 10.1037/adb0000748
36. Pelham WE, Tapert SF, Gonzalez MR, McCabe CJ, Lisdahl KM, Alzueta E, et al. Early adolescent substance use before and during the COVID-19 pandemic: a longitudinal survey in the ABCD study cohort. J Adolesc Health. (2021) 69:390–7. doi: 10.1016/j.jadohealth.2021.06.015
37. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. (2020) 67:354–61. doi: 10.1016/j.jadohealth.2020.06.018
38. Hingson R, White A. New research findings since the 2007 surgeon general's call to action to prevent and reduce underage drinking: a review. J Stud Alcohol Drugs. (2014) 75:158–69. doi: 10.15288/jsad.2014.75.158
39. Djurdjevic S, Ghigliazza IC, Dukanac V, Djurdjevic A. Anxiety and depressive symptomatology among children and adolescents exposed to the COVID-19 pandemic - a systematic review. Vojnosanitetski Pregled. (2022) 79:389–99. doi: 10.2298/VSP210521092D
40. Imran N, Zeshan M, Pervaiz Z. Mental health considerations for children and adolescents in COVID-19 pandemic. Pak J Med Sci. (2020) 36:S67–72. doi: 10.12669/pjms.36.COVID19-S4.2759
41. Mohler-Kuo M, Dzemaili S, Foster S, Werlen L, Walitza S. Stress and mental health among children/adolescents, their parents, and young adults during the first COVID-19 lockdown in Switzerland. Int J Environ Res Public Health. (2021) 18:4668. doi: 10.3390/ijerph18094668
42. Rothe J, Buse J, Uhlmann A, Bluschke A, Roessner V. Changes in emotions and worries during the COVID-19 pandemic: an online-survey with children and adults with and without mental health conditions. Child Adolesc Psychiatry Ment Health. (2021) 15:1–9. doi: 10.1186/s13034-021-00363-9
43. Morelli M, Graziano F, Chirumbolo A, Baiocco R, Longobardi E, Trumello C, et al. Parental mediation of COVID-19 news and children's emotion regulation during lockdown. J Child Fam Stud. (2022) 31:1522–34. doi: 10.1007/s10826-022-02266-5
44. Conrad RC, Hahm H, Koire A, Pinder-Amaker S, Liu CH. College student mental health risks during the COVID-19 pandemic: implications of campus relocation. J Psychiatr Res. (2021) 136:117–26. doi: 10.1016/j.jpsychires.2021.01.054
45. Mayorga NA, Smit T, Garey L, Gold AK, Otto MW, Zvolensky MJ. Evaluating the interactive effect of COVID-19 worry and loneliness on mental health among young adults. Cognit Ther Res. (2022) 46:11–9. doi: 10.1007/s10608-021-10252-2
46. Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. (2020) 29:749–58. doi: 10.1007/s00787-020-01541-4
47. Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. (2021). doi: 10.1017/S0033291720005358. [Epub ahead of print].
48. Herringa RJ. Trauma, PTSD, and the developing brain. Curr Psychiatry Rep. (2017) 19:69. doi: 10.1007/s11920-017-0825-3
49. Sun R, Zhou X. Differences in posttraumatic stress disorder networks between young adults and adolescents during the COVID-19 pandemic. Psychol Trauma. (2022). doi: 10.1037/tra0001252. [Epub ahead of print].
50. Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health-related emergency department visits among children aged < 18 years during the COVID-19 pandemic - United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1675–80. doi: 10.15585/mmwr.mm6945a3
51. Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z, et al. Emergency department visits for suspected suicide attempts among persons aged 12-25 years before and during the COVID-19 pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. (2021) 70:888–94. doi: 10.15585/mmwr.mm7024e1
52. Batchelor S, Stoyanov S, Pirkis J, Kolves K. Use of kids helpline by children and young people in Australia during the COVID-19 pandemic. J Adolesc Health. (2021) 68:1067–74. doi: 10.1016/j.jadohealth.2021.03.015
53. Isumi A, Doi S, Yamaoka Y, Takahashi K, Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. (2020) 110:104680. doi: 10.1016/j.chiabu.2020.104680
54. Mourouvaye M, Bottemanne H, Bonny G, Fourcade L, Angoulvant F, Cohen JF, et al. Association between suicide behaviours in children and adolescents and the COVID-19 lockdown in Paris, France: a retrospective observational study. Arch Dis Child. (2021) 106:918–9. doi: 10.1136/archdischild-2020-320628
55. Kiric B, Novak LL, Lusicky P, Radobuljac MD. Suicidal behavior in emergency child and adolescent psychiatric service users before and during the 16 months of the COVID-19 pandemic. Front Psychiatry. (2022) 13:893040. doi: 10.3389/fpsyt.2022.893040
56. Bera L, Souchon M, Ladsous A, Colin V, Lopez-Castroman J. Emotional and behavioral impact of the COVID-19 epidemic in adolescents. Curr Psychiatry Rep. (2022) 24:37–46. doi: 10.1007/s11920-022-01313-8
57. Gerhold L. COVID-19: risk perception and coping strategies. PsyArXiv [Preprint]. (2020). doi: 10.31234/osf.io/xmpk4
58. Lin YL, Hu ZJ, Alias H, Wong LP. Knowledge, attitudes, impact, and anxiety regarding COVID-19 infection among the public in China. Front Public Health. (2020) 8:236. doi: 10.3389/fpubh.2020.00236
59. Rivas DRZ, Jaldin MLL, Canaviri BN, Escalante LFP, Fernandez A, Ticona JPA. Social media exposure, risk perception, preventive behaviors and attitudes during the COVID-19 epidemic in La Paz, Bolivia: a cross sectional study. PLos ONE. (2021) 16:e0245859. doi: 10.1371/journal.pone.0245859
60. Yang XY, Gong RN, Sassine S, Morsa M, Tchogna AS, Drouin O, et al. Risk perception of COVID-19 infection and adherence to preventive measures among adolescents and young adults. Children. (2020) 7:311. doi: 10.3390/children7120311
61. Aguilar-Latorre A, Asensio-Martinez A, Garcia-Sanz O, Olivan-Blazquez B. Knowledge, attitudes, risk perceptions, and practices of Spanish adolescents toward the COVID-19 pandemic: validation and results of the Spanish version of the questionnaire. Front Psychol. (2022) 12:804531. doi: 10.3389/fpsyg.2021.804531
62. Kusuma D, Pradeepa R, Khawaja KI, Hasan M, Siddiqui S, Mahmood S, et al. Low uptake of COVID-19 prevention behaviours and high socioeconomic impact of lockdown measures in South Asia: evidence from a large-scale multi-country surveillance programme. SSM Popul Health. (2021) 13:100751. doi: 10.1016/j.ssmph.2021.100751
63. Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. (2020) 59:137–9. doi: 10.1016/j.amepre.2020.04.003
64. Adler AC, Shah AS, Blumberg TJ, Fazal FZ, Chandrakantan A, Ellingsen K, et al. Symptomatology and racial disparities among children undergoing universal preoperative COVID-19 screening at three US children's hospitals: early pandemic through resurgence. Pediatric Anesthesia. (2021) 31:368–71. doi: 10.1111/pan.14074
65. Smitherman LC, Golden WC, Walton JR. Health disparities and their effects on children and their caregivers during the Coronavirus disease 2019 pandemic. Pediatr Clin North Am. (2021) 68:1133–45. doi: 10.1016/j.pcl.2021.05.013
66. Krause KH, Mpofu JJ, Underwood M, Ethier KA. The CDC's adolescent behaviors and experiences survey - using intersectionality and school connectedness to understand health disparities during the COVID-19 pandemic. J Adolesc Health. (2022) 70:703–5. doi: 10.1016/j.jadohealth.2022.02.001
67. Kamal K, Li JJ, Hahm HC, Liu CH. Psychiatric impacts of the COVID-19 global pandemic on US sexual and gender minority young adults. Psychiatry Res. (2021) 299:113855. doi: 10.1016/j.psychres.2021.113855
68. DeMulder J, Kraus-Perrotta C, Zaidi H. Sexual and gender minority adolescents must be prioritised during the global COVID-19 public health response. Sex Reprod Health Matters. (2020) 28:1804717. doi: 10.1080/26410397.2020.1804717
69. Ye Y, Wang C, Zhu Q, He M, Havawala M, Bai X, et al. Parenting and teacher-student relationship as protective factors for Chinese adolescent adjustment during COVID-19. School Psych Rev. (2022) 51:187–205. doi: 10.1080/2372966X.2021.1897478
70. Zhu Q, Cheong Y, Wang C, Sun C. The roles of resilience, peer relationship, teacher-student relationship on student mental health difficulties during COVID-19. School Psychol. (2022) 37:62–74. doi: 10.1037/spq0000492
71. Lessard LM, Puhl RM. Adolescent academic worries amid COVID-19 and perspectives on pandemic-related changes in teacher and peer relations. Sch Psychol. (2021) 36:285–92. doi: 10.1037/spq0000443
72. Jiang Y, Tan Y, Wu D, Yin J, Lin X. The double-edged impact of the COVID-19 pandemic on Chinese family relationships. J Fam Issues. (2022) 1–21. doi: 10.1177/0192513X211041990
73. Qu M, Yang K, Cao YJ, Xiu MH, Zhang XY. Mental health status of adolescents after family confinement during the COVID-19 outbreak in the general population: a longitudinal survey. Eur Arch Psychiatry Clin Neurosci. (2022). doi: 10.1007/s00406-022-01459-9. [Epub ahead of print].
74. Zhuo R, Yu YH, Shi XX. Family resilience and adolescent mental health during COVID-19: a moderated mediation model. Int J Environ Res Public Health. (2022) 19:4801. doi: 10.3390/ijerph19084801
75. Finkelstein DM, Kubzansky LD, Capitman J, Goodman E. Socioeconomic differences in adolescent stress: the role of psychological resources. J Adolesc Health. (2007) 40:127–34. doi: 10.1016/j.jadohealth.2006.10.006
76. Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health. (2020) 67:164–71. doi: 10.1016/j.jadohealth.2020.05.006
Keywords: COVID-19, teenager, adolescent, children, mental health, lifestyle, VOS viewer, CiteSpace
Citation: Li X and Yu J (2022) How has the COVID-19 pandemic affected young people?—Mapping knowledge structure and research framework by scientometric analysis. Front. Public Health 10:1052727. doi: 10.3389/fpubh.2022.1052727
Received: 24 September 2022; Accepted: 17 November 2022;
Published: 02 December 2022.
Edited by:
Haibo Yang, Tianjin Normal University, ChinaReviewed by:
Constantin-Cristian Topriceanu, University College London, United KingdomJoshua Macdonald, Tel Aviv University, Israel
Copyright © 2022 Li and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiahui Yu, eWpoMTc2OTU3OTYzMzNAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Xiangfei Li
Xiangfei Li Jiahui Yu
Jiahui Yu