- 1Department of Public Health and Laboratory Services, Teaching Hospital, University of Campania “Luigi Vanvitelli”, Naples, Italy
- 2Department of Experimental Medicine, University of Campania “Luigi Vanvitelli”, Naples, Italy
Background: The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is evolving,the newly emerged Omicron variant being the dominant strain worldwide, and this has raised concerns about vaccine efficacy. The purposes of this survey were to examine the extent to which healthcare workers (HCWs) intend to receive a second booster dose of the COVID-19 vaccine and the factors that influence their willingness to accept it.
Methods: The study was conducted among HCWs who were randomly selected from four public hospitals in the Campania region, Southern Italy.
Results: A total of 496 HCWs answered the questionnaire (a response rate of 61.2%). Among the respondents, 20.8% indicated a score of 10, using a 10-point Likert-type scale, regarding the usefulness of a second COVID-19 vaccine booster dose. Physicians, HCWs who believed that COVID-19 was a severe disease, and those who have acquired information about the second booster dose from scientific journals were more likely to have this positive attitude. Slightly more than half of HCWs self-reported willingness to receive a second booster dose. Respondents who believe that HCWs are at higher risk of being infected by SARS-CoV-2, those who have a higher belief that COVID-19 is a severe disease, and those who have a higher belief that a second booster dose is useful were more willing to receive a second booster dose. The main reasons for those who had a positive intention were to protect their family members and patients, whereas, the main reasons for not getting vaccinated or for uncertainty were that the dose does not offer protection against the emerging variants and the fear of its side effects. HCWs of younger age, physicians, those who have a higher belief that a second booster dose is useful, and those who were willing to receive a second booster dose were more likely to recommend the booster dose to their patients.
Conclusion: This study's findings highlight the necessity for designing and implementing educational interventions for improving second booster dose uptake and beliefs among HCWs and their capacity to recommend the vaccine to the patients.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has generated more than half a billion confirmed cases and almost 6.5 million deaths around the world (1), including over 23.5 million and 179,000 people in Italy by 31 October 2022 (2). Several measures have been implemented to contain and prevent the spread of the disease, such as hand hygiene, social distancing, wearing a mask, and vaccination. However, SARS-CoV-2 is continuously evolving with the newly emerged Omicron variant being the dominant strain worldwide (3, 4), and this has raised concerns about vaccine efficacy. In Italy, on 11 July 2022, the Ministry of Health for this evolving scenario recommended an additional second booster dose or “fourth dose” of the currently available mRNA COVID-19 anti-Omicron variant vaccines, at least 4 months (120 days) after the first booster dose or the last post-booster infection (date of the positive test), to adults aged 60 years and above and individuals aged 12 years and above with concomitant/preexisting conditions (5). As of 19 September 2022, less than one-fourth of those eligible had received this second booster dose (6). Healthcare workers (HCWs), one of the most affected groups (7–9), have not been included, although, from 27 November 2021, the Italian government made vaccination with three doses mandatory for this group but this does not include the second booster dose (10). Moreover, HCWs also play an important role in transmitting the virus to their patients while providing care.
From this point of view, it is, therefore, extremely important and crucial to understand and assess HCWs' willingness to have the second booster dose of the COVID-19 vaccine; no literature is available on this topic. Therefore, the purposes of this present survey were to examine the extent to which a large sample of HCWs in Italy intends to receive a second booster dose of the COVID-19 vaccine and the factors that influence their willingness for accepting it.
Materials and methods
Setting and study population
The study was carried out from 12 July to 9 September 2022. The source population included all 4,000 HCWs who worked in different wards in four randomly selected public hospitals, one teaching and three nonteaching, located in the Campania region, Southern Italy. The sample for the present study included 496 HCWs who had been selected by a simple random sampling technique. A sample size of 384 HCWs was estimated assuming that 50% of the study population would intend to receive a second booster of the COVID-19 vaccine, 95% confidence interval, and a margin of error of 5%.
Data collection
Initially, the research team asked for permission from the health director of each hospital to conduct the study. After the approval, the team identified in each ward an HCW to distribute the questionnaire to the HCWs who were randomly selected from the list of those present at that moment in each ward and to collect the filled questionnaires within an envelope to maintain anonymity and to return the envelope. The questionnaire contained a brief introduction about the objectives, procedure, confidentiality, and anonymity of the survey, that the participation was voluntary, that the information provided will be used only for research purposes, and that the participant was able to withdraw at any moment. HCWs gave their informed consent to participate by handing in the questionnaire. The participants received no incentive to complete the questionnaire.
Survey development
All data were collected through a self-administered questionnaire adopted and modified from previously published studies of the research group (11–20). The questionnaire required 5–10 min to complete and capture the following information: a) sociodemographic, general, and professional characteristics (14 questions), including gender, age, relationship status, degree of education, professional role, duration of employment in the healthcare profession, area of working activity, self-rated health status, and previous COVID-19 infection; b) source(s) from which they receive information related to the second booster dose and whether they would like to get additional information (2 questions); and c) attitudes and behaviors (7 questions). The first comprised 5 items concerning attitudes toward COVID-19 and the second booster dose, using a 10-point Likert-type scale with a response format ranging from 1 = not at all to 10 = a great deal and a 5-point Liker-type scale ranging from 1 = strongly disagree to 5 = strongly agree, assessing whether the responder had been/had not been vaccinated with a second booster dose and the related reason(s). Those unvaccinated were asked to indicate whether they were willing or unwilling to receive a second booster dose and the underlying reasons in favor of or against receiving this vaccination. The survey was first piloted and tested by the research team to assess the feasibility and acceptability of the questions.
Ethical approval of the study protocol and questionnaire was received from the Ethics Committee of the Teaching Hospital of the University of Campania “Luigi Vanvitelli.”
Statistical analysis
All statistical analyses were conducted using the software STATA version 15.1. Descriptive statistics were used with frequency, mean, and standard deviation to describe the principal characteristics of the participants, as well as behavior and attitude toward having a second COVID-19 booster dose. Multiple logistic regression models were built using the strategy suggested by Hosmer et al. (21). Each variable was examined by univariate analysis, using the chi-square test and Student's t-test, to evaluate predictors of the different outcomes of interest. Only those variables with a p < 0.25 in the univariate analysis were entered into three multivariate logistic regression models to assess associations between the main dependent variables and the several independent variables. Then, multivariate logistic regression analysis with backward elimination of any variable that did not contribute to the model on the grounds of the Likelihood Ratio test (cut-off at p = 0.05) was performed. Variables whose exclusion altered the coefficient of the remaining variables were kept in the model. Backward stepwise selection has been used with a threshold of p = 0.2 and p = 0.4, respectively, for the entry or removal of the variables from the final models. Odds ratios (OR) and their corresponding 95% confidence intervals (CI) were calculated in the models. Three outcomes of interest have been identified: a) belief that a second booster dose of the COVID-19 vaccine was useful (1–9 = 0; 10 = 1) (Model 1); b) willingness to receive a second booster dose of the COVID-19 vaccine (no/do not know = 0; yes = 1) (Model 2); c) recommendation of a second booster dose of the COVID-19 vaccine to the patients (no = 0; yes = 1) (Model 3). The following potential determinants were included in all models: gender (female = 0; male = 1); age, in years (continuous); marital status (unmarried/separated/divorced/widowed = 0; married/cohabitant = 1); physicians (no = 0; yes = 1); length of practice, in years (less than three = 0; at least three = 1); having worked in a COVID-19 ward (no = 0; yes = 1); having underlying at least one chronic medical condition (no = 0; yes = 1); having been tested positive for COVID-19 (no = 0; yes = 1); at least one family member/colleague/friend who had been tested positive for COVID-19 (no = 0; yes = 1); perceived risk of getting infected with SARS-CoV-2 during the working activity (1–9 = 0; 10 = 1); belief that COVID-19 is a serious disease (1–9 = 0; 10 = 1); belief that HCWs are at a higher risk of being infected by SARS-CoV-2 (strongly disagree/disagree/undecided = 0; agree/strongly agree = 1); scientific journals as source of information about the second booster dose of the COVID-19 vaccine (no = 0; yes = 1); and needing additional information regarding the second booster dose of the COVID-19 vaccine (no = 0; yes = 1). Moreover, the variables belief that the second booster dose of the COVID-19 vaccine was useful (1–9 = 0; 10 = 1) and belief that the second booster dose of the COVID-19 vaccine was effective (1–9 = 0; 10 = 1) were included in Models 2 and 3; and the variable willingness to receive the second booster dose of the COVID-19 vaccine (no/undecided = 0; yes = 1) was included in Model 3. For all analyses, two-tailed tests were used and statistical significance was determined with a p-value equal to or less than 0.05.
Results
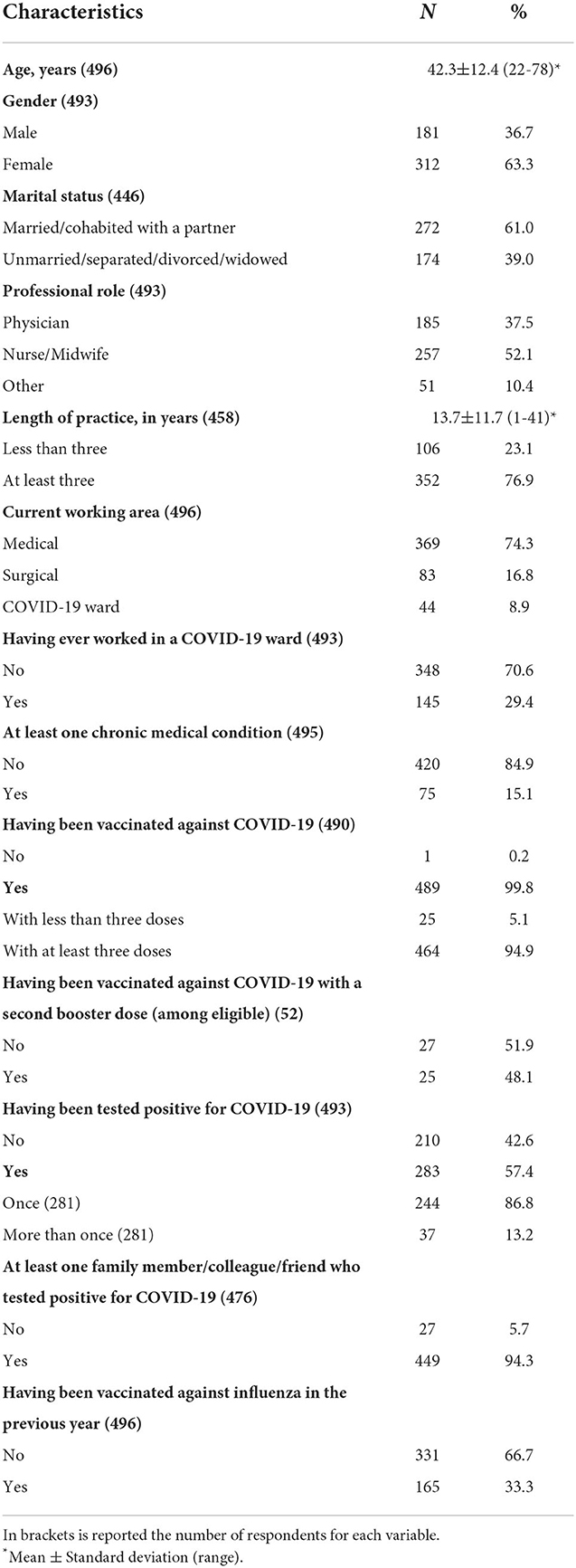
A total of 496 HCWs, out of the 810 selected, answered the questionnaire with a response rate of 61.2%. The main sociodemographic, general, and professional characteristics of the respondents are summarized in Table 1. The average age was 42.3 years, almost two-thirds were female participants, more than half were nurses/midwives, two-thirds worked in medical wards, almost one-third have had working experience in a COVID-19 ward, the mean length of working activity was 13.7 years, only 15.1% self-identified as having a chronic medical condition, more than half have had COVID-19, almost all had a family member/colleague/friend who tested positive for COVID-19, and only 25 of the 52 eligible has been vaccinated with a second booster dose.
The results regarding the attitudes, measured on a 10-point Likert-type scale, showed that the mean scores of the respondent's belief that COVID-19 was a severe disease and whether they feel at risk of being infected by SARS-CoV-2 during the working activity were 7.4 and 6.8, respectively, with 19.6% believing themselves to be at an elevated risk (as by indicated a value of 10). The mean scores regarding the usefulness and efficacy of a second booster dose of the COVID-19 vaccine were 6.7 and 6, respectively, with only 20.8% and 16.4% of participants who had indicated a score of 10. Table 2 presents the results from the three multivariate logistic regression models examining the relationship between several variables and the different outcomes of interest. The first model showed that a score of 10 regarding the usefulness of a second booster dose of the COVID-19 vaccine was more likely to be observed in physicians (OR: 1.99, 95% CI: 1.14–3.46), in those who have a higher belief that COVID-19 was a severe disease (OR: 4.47, 95% CI: 2.39–8.37), and in those who have acquired information about the second booster dose of the COVID-19 vaccine from scientific journals (OR: 2.24, 95% CI: 1.31–3.85).
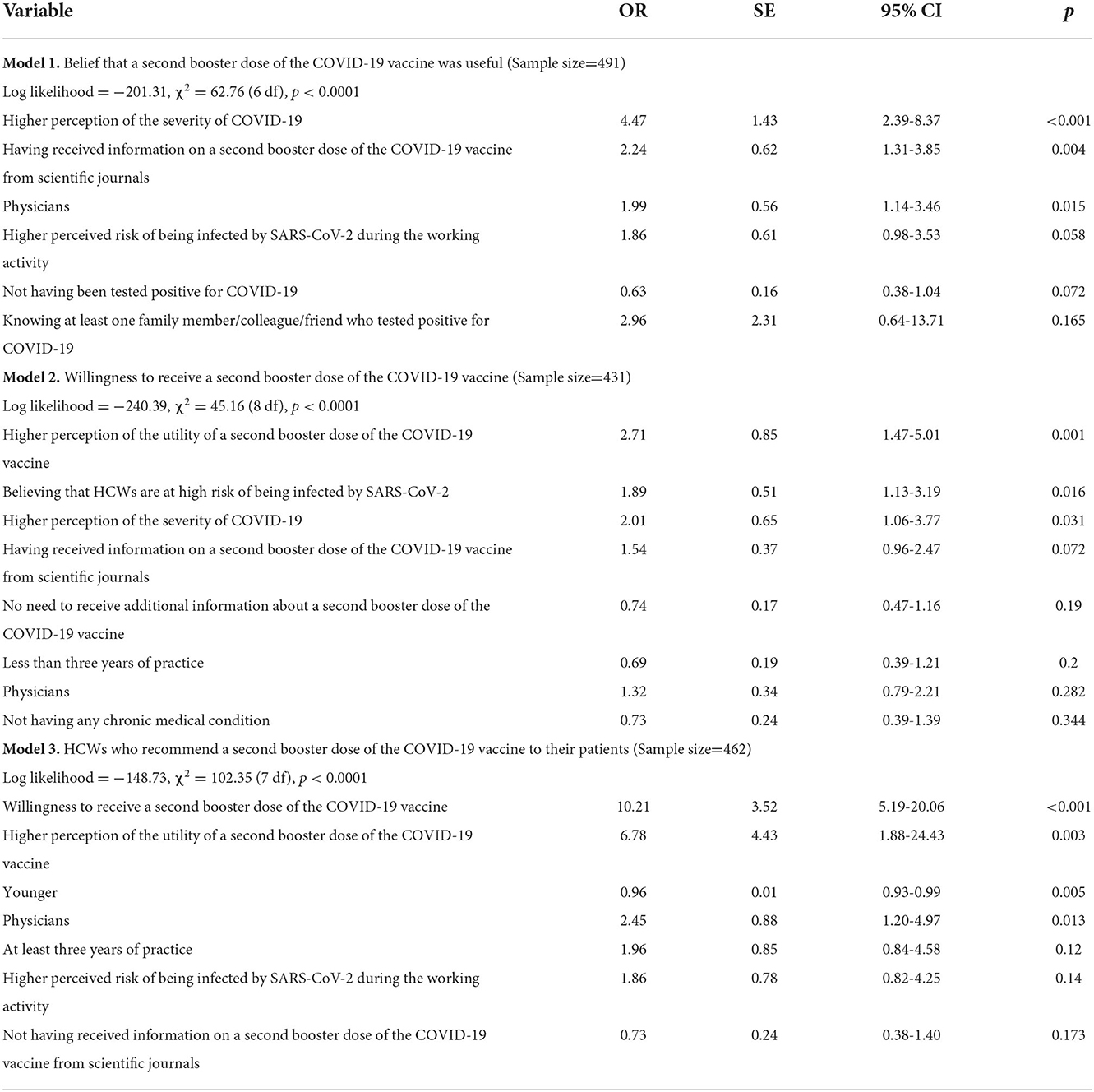
Table 2. Results of the multivariate logistic regression analysis showing determinants of the different outcomes of interest.
Among those respondents who had not had the second booster dose of the COVID-19 vaccine, 52.6% self-reported a willingness to receive it, and 25.1% and 22.3% indicated that they had “no intention” or showed “uncertainty.” The main self-reported reasons for those who had a positive intention were to protect their family members (49.6%) and their patients (42.9%) and the fear of acquiring the infection (37.6%). The main reasons for not getting vaccinated or for uncertainty, however, were that the dose does not offer protection against the emerging variants (54.6%) and the fear of its side effects (27%). Three variables were found to be associated with the HCWs' willingness to receive a second booster dose in the multivariate logistic regression analysis. Respondents who believed that HCWs are at higher risk of being infected by SARS-CoV-2 (OR: 1.89, 95% CI: 1.13–3.19), those who have a higher belief that COVID-19 was a severe disease (OR: 2.01, 95% CI: 1.06–3.77), and those who have a higher belief that a second booster dose is useful (OR: 2.71, 95% CI: 1.47–5.01) were more willing to receive a second booster dose of the COVID-19 vaccine (Model 2 in Table 2). A total of 75.3% of HCWs recommend the booster dose to their patients, whereas among those who did not recommend it, 83.6% were unwilling to make the recommendation. HCWs were more likely to recommend the booster dose to the patients if they were younger (OR: 0.96, 95% CI: 0.93–0.99), physicians (OR: 2.45, 95% CI: 1.20–4.97), have a higher belief that a second booster dose is useful (OR: 6.78, 95% CI: 1.88–24.43), and if they were more willing to receive a second booster dose (OR: 10.21, 95% CI: 5.19–20.06) (Model 3 in Table 2).
Almost all HCWs had received information about the second COVID-19 booster dose (96.6%). The internet (51.8%), mass media (48.6%), scientific meetings (48.2%), and scientific journals (41.5%) were indicated as primary sources for this information, followed by social networks (26.7%). More than one-third of the respondents expressed an interest in acquiring additional information about the second booster dose (36.3%).
Discussion
To our knowledge, this is the largest survey of HCWs' willingness to have a second booster dose of the COVID-19 vaccine and the factors associated with this decision conducted in Italy. The major findings can be summarized in the following five points. First, slightly more than 50% of the sample would accept a second booster dose of the COVID-19 vaccine. Second, the main reasons behind the willingness to have a second booster dose were to protect family members and patients. Third, the main reasons for the intention to not receive or uncertainty toward the second booster dose were the belief that it does not offer protection against the emerging variants and the fear of side effects. Fourth, scientific meetings and journals were among the primary sources of information on the second booster dose. Fifth, several determinants have been observed to be significantly associated with the different outcomes of interest.
Overall, the present survey revealed that only 52.6% of respondents self-reported a willingness to receive a second booster dose. Though it is only mandatory for HCWs to have the first COVID-19 booster dose, it was nonetheless a striking and unexpected finding that very few (48.1%) eligible HCWs had received a second booster dose. The prevalence of this willingness was lower than the values observed among HCWs in Saudi Arabia (55.3%) (22), Czechia (71.3%) (23), and China (87%) (24). A surprising finding was that this value was also considerably lower than those in the general population in India (59.1%) (25), the Middle East and North Africa Region (60.2%) (26), China (91.1%) (27), Japan (97.8%) (28), university students and staff in Italy (85.7%) (15), and the United States (96.2%) (29). The finding of the present study is of great concern because HCWs have a higher risk of infection with SARS-CoV-2 than the general population; in Italy, since the beginning of the pandemic as of September 2021, there have been 3,970 deaths among HCWs out of a total of 124,000 (30). This alarming picture has had an important impact on the healthcare delivery system, with the difficulty in maintaining levels of care and in responding to the population's needs. Therefore, it is important to increase willingness and uptake of a second COVID-19 booster dose since it has been reported in the literature that vaccinated HCWs, as other groups of individuals, have a considerable influence on their patient's intention to get vaccinated or more likely to deliver the vaccinations (31–34).
This study highlighted that the protection of their family members and patients and the fear of acquiring the infection were the most frequent reasons for the willingness to receive a second booster dose of the COVID-19 vaccine. These findings are consistent with other recent similar research studies (35–38). A possible explanation for the protection of the family is that household transmission has been observed as one of the most common primary routes of SARS-CoV-2 transmission (39–43). Therefore, vaccines and boosters are the best primary interventions for preventing SARS-CoV-2 transmission since, in the household, it is not easy to maintain social distancing, avoid close contacts, and wear masks. Moreover, among those HCWs who did not intend to receive the second booster dose or were uncertain, concerns about the safety and effectiveness of the vaccine against the emerging variants were the most common reasons. Previous studies among different samples and geographic areas have linked these reasons with hesitancy or unwillingness to get vaccinated against COVID-19 (44–48). Addressing these concerns is of crucial importance to improve the uptake of a second booster dose also at the population level through evidence-based messages considering the pivotal role of the HCWs in community health.
The results of the multivariate logistic regression analysis showed that several factors were significant predictors of attitude, vaccine willingness, and vaccine recommendation. Of the several sociodemographic and professional characteristics, only age and professional role were associated with the outcomes of interest. Indeed, physicians indicated a higher score regarding the usefulness of a second booster dose of the COVID-19 vaccine, and as, those younger, they were more likely to recommend this booster dose to the patients and more willing to receive it. Moreover, three variables related to the respondents' attitudes have had a significant impact. HCWs who believed that COVID-19 was a serious disease and who believed that they are at higher risk of being infected by SARS-CoV-2 were more likely to believe that the second booster dose is useful and more willing to receive the booster dose, and HCWs who believed that the second booster dose is useful and who were willing to receive it were more likely to recommend the booster dose to the patients. Therefore, it is extremely important that the HCWs should be aware of the vaccine's effectiveness in preventing SARS-CoV-2 infection and to improve their attitudes as an effective way to enhance HCWs' willingness to be vaccinated with a second booster dose of the COVID-19 vaccine or to recommend it. Some of these associations have been observed in a previous investigation (49).
This present survey showed that almost all HCWs had received information related to a second booster dose of the COVID-19 vaccine, with scientific meetings and journals being two of the most trusted sources. It is important to highlight that scientific journals have a significant effect on the higher belief regarding the usefulness of a second booster dose. This finding confirms that these sources are an important factor in the vaccination process and decision. Indeed, this association is in accordance with previous studies that showed that scientific journals played a significant role in determining a higher level of knowledge, a more positive attitude, an increase in the willingness to receive a vaccine, and a higher vaccination coverage among those who have acquired information from these sources (17, 18). Moreover, it should also be noted that mass media, social media, and the internet were also accepted by many HCWs. However, these sources need to be carefully used because evidence indicated that there is the possibility of the spread of untrue and negative information, resulting in worry about the COVID-19 vaccination, lower coverage, and higher hesitancy (50, 51). It is interesting to observe that a systematic review of the reviews regarding infodemics and health misinformation indicated that social media has been increasingly propagating poor quality health-related information during pandemics and health emergencies (52).
The results from the present survey should also be considered with some potential methodological limitations. First, as in all cross-sectional studies, no causal relationships between the independent variables and the different outcomes of interest can be established. Second, the survey was administered to HCWs in a single geographic area, and therefore, the findings may not necessarily apply to other areas of Italy. Third, a self-reporting questionnaire may have introduced social desirability bias and the surveyed HCWs may tend to have more positive attitudes that lead to an overestimation of their intention to have a second booster dose of the COVID-19 vaccine. However, an anonymous questionnaire has been used to reduce this bias. Despite these limitations, this study was the first to assess the willingness to have a second booster dose among HCWs in Italy, and it thus provides an important picture with important implications for health policymakers.
In conclusion, this survey reveals a low willingness to receive a second booster dose, the facilitators and barriers influencing this willingness, and the factors associated with this choice. The findings have important implications and highlight the necessity for designing and implementing targeted education interventions for improving the second booster dose of the COVID-19 vaccine uptake among HCWs and their capacity to recommend the vaccine to the patients. In the future, investigations are expected to quantify the coverage level in HCWs and to evaluate whether they can promote this vaccination with special attention toward more vulnerable people.
The collaborative working group
Walter Longanella (Health Direction, San Giovanni di Dio Ruggi D'Aragona Hospital, Largo Città Ippocrate, 84131 Salerno, Italy), Mario Massimo Mensorio (Health Direction, Sant'Anna e San Sebastiano Hospital, Via Ferdinando Palasciano, 81100 Caserta, Italy), Federica Cantore (Health Direction, San Giuseppe Moscati Hospital, Contrada Amoretta, 03100 Avellino, Italy).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Teaching Hospital of the University of Campania Luigi Vanvitelli. The patients/participants provided their written informed consent to participate in this study.
Author contributions
GDP, GMdG, LF, and AN participated in the conception and design of the study and contributed to the data collection, data analysis, and interpretation. IFA the principal investigator, designed the study, was responsible for the statistical analysis and interpretation, drafted and wrote the article. All authors have read and approved the final version of the article and agree to be accountable for all aspects of the work.
Funding
This work was supported by a grant of the Regione Campania (Executive decree n.75/2017 Strategic and nationally relevance objectives indicated in the National Health Plan. FSN 2014, 2015, and 2016).
Acknowledgments
The authors are extremely grateful to all healthcare workers who completed the questionnaire. The authors would also like to thank each hospital for its collaboration during data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. WHO Coronavirus (COVID-19) Dashboard (2022). Available online at: https://covid19.who.int/ (accessed September 19, 2022).
2. Italian Ministry of Health. COVID-19 Situazione Italia (2022). Available online at: https://opendatadpc.maps.arcgis.com/apps/dashboards/b0c68bce2cce478eaac82fe38d4138b1 (accessed October 31, 2022).
3. Tian D, Sun Y, Xu H, Ye Q. The emergence and epidemic characteristics of the highly mutated SARS-CoV-2 Omicron variant. J Med Virol. (2022) 94:2376–83. doi: 10.1002/jmv.27643
4. Karim SSA, Karim QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. (2021) 398:2126–8. doi: 10.1016/S0140-6736(21)02758-6
5. Italian Ministry of Health. Circolare Ministeriale n. 0032264. Estensione della platea vaccinale destinataria della seconda dose di richiamo (second booster) nell'ambito della campagna di vaccinazione anti-SARS-CoV-2/COVID-19 (2022). Available online at: https://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2022&codLeg=88043&parte=1%20&serie=nulll (accessed September 19, 2022).
6. Italian Ministry of Health. Report Vaccini anti-COVID-19. Available online at: https://www.governo.it/it/cscovid19/report-vaccini/ (accessed September 19, 2022).
7. Iversen K, Bundgaard H, Hasselbalch RB, Kristensen JH, Nielsen PB, Pries-Heje M, et al. Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet Infect Dis. (2020) 20:1401–8. doi: 10.1016/S1473-3099(20)30589-2
8. Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. (2020) 5:e475–e83. doi: 10.1016/S2468-2667(20)30164-X
9. van der Plaat DA, Madan I, Coggon D, van Tongeren M, Edge R, Muiry R, et al. Risks of COVID-19 by occupation in NHS workers in England. Occup Environ Med. (2022) 79:176–83. doi: 10.1136/oemed-2021-107628
10. President of the Italian Republic. Disposizioni urgenti in materia di prevenzione del contagio da SARS-CoV-2 mediante previsione di obblighi vaccinali per gli esercenti le professioni sanitarie e gli operatori di interesse sanitario (2022). Available online at: https://www.gazzettaufficiale.it/eli/id/2021/04/01/21G00056/sg (accessed September 19, 2022).
11. Miraglia del Giudice G Folcarelli L Napoli A Corea F Angelillo IF The The Collaborative Working Group. COVID-19 vaccination hesitancy and willingness among pregnant women in Italy. Front Public Health. (2022) 10:995382. doi: 10.3389/fpubh.2022.995382
12. Napoli A, Miraglia del Giudice G, Corea F, Folcarelli L, Angelillo IF. Parents' reasons to vaccinate their children aged 5-11 years against COVID-19 in Italy. Front Med. (2022) 9:949693. doi: 10.3389/fmed.2022.949693
13. Corea F, Folcarelli L, Napoli A, Miraglia del Giudice G, Angelillo IF. The impact of COVID-19 vaccination in changing the adherence to preventive measures: evidence from Italy. Vaccines. (2022) 10:777. doi: 10.3390/vaccines10050777
14. Miraglia del Giudice G, Napoli A, Corea F, Folcarelli L, Angelillo IF. Evaluating COVID-19 vaccine willingness and hesitancy among parents of children aged 5-11 years with chronic conditions in Italy. Vaccines. (2022) 10:396. doi: 10.3390/vaccines10030396
15. Folcarelli L, Miraglia del Giudice G, Corea F, Angelillo IF. Intention to receive the COVID-19 vaccine booster dose in a university community in Italy. Vaccines. (2022) 10:146. doi: 10.3390/vaccines10020146
16. Bianco A, Della Polla G, Angelillo S, Pelullo CP, Licata F, Angelillo IF. Parental COVID-19 vaccine hesitancy: a cross-sectional survey in Italy. Expert Rev Vaccines. (2022) 21:541–7. doi: 10.1080/14760584.2022.2023013
17. Di Giuseppe G, Pelullo CP, Della Polla G, Montemurro MV, Napolitano F, Pavia M, et al. Surveying willingness toward SARS-CoV-2 vaccination of healthcare workers in Italy. Expert Rev Vaccines. (2021) 20:881–9. doi: 10.1080/14760584.2021.1922081
18. Della Polla G, Pelullo CP, Di Giuseppe G, Angelillo IF. Changes in behaviors and attitudes in response to COVID-19 pandemic and vaccination in healthcare workers and university students in Italy. Vaccines. (2021) 9:1276. doi: 10.3390/vaccines9111276
19. Della Polla G, Licata F, Angelillo S, Pelullo CP, Bianco A, Angelillo IF. Characteristics of healthcare workers vaccinated against influenza in the era of COVID-19. Vaccines. (2021) 9:695. doi: 10.3390/vaccines9070695
20. Di Giuseppe G, Pelullo CP, Della Polla G, Pavia M, Angelillo IF. Exploring the willingness to accept SARS-CoV-2 vaccine in a university population in Southern Italy, September to November 2020. Vaccines. (2021) 9:275. doi: 10.3390/vaccines9030275
21. Hosmer Jr DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. New York, NY: John Wiley & Sons (2013).
22. Alhasan K, Aljamaan F, Temsah MH, Alshahrani F, Bassrawi R, Alhaboob A, et al. COVID-19 delta variant: perceptions, worries, and vaccine-booster acceptability among healthcare workers. Healthcare. (2021) 9:1566. doi: 10.3390/healthcare9111566
23. Klugar M, Riad A, Mohanan L, Pokorná A. COVID-19 vaccine booster hesitancy (vbh) of healthcare workers in Czechia: national cross-sectional study. Vaccines. (2021) 9:1437. doi: 10.3390/vaccines9121437
24. Luo C, Chen HX, Tung TH. COVID-19 vaccination in China: adverse effects and its impact on health care working decisions on booster dose. Vaccines. (2022) 10:1229. doi: 10.3390/vaccines10081229
25. Achrekar GC, Batra K, Urankar Y, Batra R, Iqbal N, Choudhury SA, et al. Assessing COVID-19 booster hesitancy and its correlates: early evidence from India. Vaccines. (2022) 10:1048. doi: 10.3390/vaccines10071048
26. Abouzid M, Ahmed AA, El-Sherif DM, Alonazi WB, Eatmann AI, Alshehri MM, et al. Attitudes toward receiving COVID-19 booster dose in the Middle East and North Africa (MENA) region: a cross-sectional study of 3041 fully vaccinated participants. Vaccines. (2022) 10:1270. doi: 10.3390/vaccines10081270
27. Tung TH, Lin XQ, Chen Y, Zhang MX, Zhu JS. Willingness to receive a booster dose of inactivated coronavirus disease 2019 vaccine in Taizhou, China. Expert Rev Vaccines. (2022) 21:261–7. doi: 10.1080/14760584.2022.2016401
28. Yoshida M, Kobashi Y, Kawamura T, Shimazu Y, Nishikawa Y, Omata F, et al. Factors associated with COVID-19 vaccine booster hesitancy: a retrospective cohort study, Fukushima vaccination community survey. Vaccines. (2022) 10:515. doi: 10.3390/vaccines10040515
29. Lee RC, Hu H, Kawaguchi ES, Kim AE, Soto DW, Shanker K, et al. COVID-19 booster vaccine attitudes and behaviors among university students and staff in the United States: The USC trojan pandemic research initiative. Prev Med Rep. (2022) 28:101866. doi: 10.1016/j.pmedr.2022.101866
30. World Health Organization. The Impact of COVID-19 on Health and Care Workers: a Closer Look at Deaths (2022). Available online at: https://apps.who.int/iris/bitstream/handle/10665/345300/WHO-HWF-WorkingPaper-2021.1-eng.pdf?sequence=1&isAllowed=y (accessed September 19, 2022).
31. Wiysonge CS, Alobwede SM, de Marie C Katoto P, Kidzeru EB, Lumngwena EN, Cooper S, et al. COVID-19 vaccine acceptance and hesitancy among healthcare workers in South Africa. Expert Rev Vaccines. (2022) 21:549–59. doi: 10.1080/14760584.2022.2023355
32. Guidry JPD, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. (2021) 49:137–42. doi: 10.1016/j.ajic.2020.11.018
33. Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. (2021) 21:804. doi: 10.1186/s12889-021-10816-7
34. Le An P, Nguyen HTN, Nguyen DD, Vo LY, Huynh G. The intention to get a COVID-19 vaccine among the students of health science in Vietnam. Hum Vaccin Immunother. (2021) 17:4823–8. doi: 10.1080/21645515.2021.1981726
35. Gogoi M, Wobi F, Qureshi I, Al-Oraibi A, Hassan O, Chaloner J, et al. “The vaccination is positive; I don't think it's the panacea'': a qualitative study on COVID-19 vaccine attitudes among ethnically diverse healthcare workers in the United Kingdom. PLoS ONE. (2022) 17:e0273687. doi: 10.1371/journal.pone.0273687
36. Jiang F, Zhao Y, Bai J, Yang X, Zhang J, Lin D, et al. Perceived health literacy and COVID-19 vaccine acceptance among Chinese college students: a mediation analysis. PLoS ONE. (2022) 17:e0273285. doi: 10.1371/journal.pone.0273285
37. Ng JWJ, Vaithilingam S, Nair M, Hwang LA, Musa KI. Key predictors of COVID-19 vaccine hesitancy in Malaysia: an integrated framework. PLoS ONE. (2022) 17:e0268926. doi: 10.1371/journal.pone.0268926
38. Basta NE, Sohel N, Sulis G, Wolfson C, Maimon G, Griffith LE, et al. Factors associated with willingness to receive a COVID-19 vaccine among 23,819 adults aged 50 years or older: an analysis of the Canadian longitudinal study on aging. Am J Epidemiol. (2022) 191:987–98. doi: 10.1093/aje/kwac029
39. Matsumura Y, Yamamoto M, Shinohara K, Tsuchido Y, Yukawa S, Noguchi T, et al. High mortality and morbidity among vaccinated residents infected with the SARS-CoV-2 Omicron variant during an outbreak in a nursing home in Kyoto City, Japan. Am J Infect Control. (2022) 2022:S0196-6553(22)00675-7. doi: 10.1016/j.ajic.2022.09.007
40. Cerami C, Popkin-Hall ZR, Rapp T, Tompkins K, Zhang H, Muller MS, et al. Household transmission of severe acute respiratory syndrome coronavirus 2 in the United States: living density, viral load, and disproportionate impact on communities of color. Clin Infect Dis. (2022) 74:1776–85. doi: 10.1093/cid/ciab701
41. Dub T, Solastie A, Hagberg L, Liedes O, Nohynek H, Haveri A, et al. High secondary attack rate and persistence of SARS-CoV-2 antibodies in household transmission study participants, Finland 2020-2021. Front Med. (2022) 9:876532. doi: 10.3389/fmed.2022.876532
42. Madewell ZJ, Yang Y, Longini IM Jr, Halloran ME, Dean NE. Household secondary attack rates of SARS-CoV-2 by variant and vaccination status: an updated systematic review and meta-analysis. JAMA Netw Open. (2022) 5:e229317. doi: 10.1001/jamanetworkopen.2022.9317
43. Donnelly MAP, Chuey MR, Soto R, Schwartz NG, Chu VT, Konkle SL, et al. Household transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Alpha Variant-United States, 2021. Clin Infect Dis. (2022) 75:e122–32. doi: 10.1093/cid/ciac125
44. Sánchez-González L, Major CG, Rodriguez DM, Balajee A, Ryff KR, Lorenzi O, et al. COVID-19 vaccination intention in a community cohort in Ponce, Puerto Rico. Am J Trop Med Hyg. (2022) 107:268–77. doi: 10.4269/ajtmh.22-0132
45. Galanis P, Vraka I, Katsiroumpa A, Siskou O, Konstantakopoulou O, Katsoulas T, et al. Predictors of willingness of the general public to receive a second COVID-19 booster dose or a new COVID-19 vaccine: a cross-sectional study in Greece. Vaccines. (2022) 10:1061. doi: 10.3390/vaccines10071061
46. Huang Q, Gilkey MB, Thompson P, Grabert BK, Dailey SA, Brewer NT. Explaining higher COVID-19 vaccination among some US primary care professionals. Soc Sci Med. (2022) 301:114935. doi: 10.1016/j.socscimed.2022.114935
47. Vellappally S, Naik S, Alsadon O, Al-Kheraif AA, Alayadi H, Alsiwat AJ, et al. Perception of COVID-19 booster dose vaccine among healthcare workers in India and Saudi Arabia. Int J Environ Res Public Health. (2022) 19:8942. doi: 10.3390/ijerph19158942
48. Bianchi FP, Stefanizzi P, Brescia N, Lattanzio S, Martinelli A, Tafuri S. COVID-19 vaccination hesitancy in Italian healthcare workers: a systematic review and meta-analysis. Expert Rev Vaccines. (2022) 21:1289–300. doi: 10.1080/14760584.2022.2093723
49. Tylec A, Janiszewska M, Siejko K, Kucharska K. Determinants of the decision to be vaccinated against COVID-19 as exemplified by employees of a long-term health care centre. J Public Health. (2021) 2021:fdab395. doi: 10.1093/pubmed/fdab395
50. Viswanath K, Bekalu M, Dhawan D, Pinnamaneni R, Lang J, McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. (2021) 21:818. doi: 10.1186/s12889-021-10862-1
51. Zhang J, Featherstone JD, Calabrese C, Wojcieszak M. Effects of fact-checking social media vaccine misinformation on attitudes toward vaccines. Prev Med. (2021) 145:106408. doi: 10.1016/j.ypmed.2020.106408
Keywords: COVID-19, HCWs, Italy, second booster dose, vaccination, willingness
Citation: Della Polla G, Miraglia del Giudice G, Folcarelli L, Napoli A, Angelillo IF and The Collaborative Working Group (2022) Willingness to accept a second COVID-19 vaccination booster dose among healthcare workers in Italy. Front. Public Health 10:1051035. doi: 10.3389/fpubh.2022.1051035
Received: 22 September 2022; Accepted: 10 November 2022;
Published: 09 December 2022.
Edited by:
Silvio Tafuri, University of Bari Aldo Moro, ItalyReviewed by:
Pasquale Stefanizzi, University of Bari Aldo Moro, ItalyChiara de Waure, University of Perugia, Italy
Copyright © 2022 Della Polla, Miraglia del Giudice, Folcarelli, Napoli, Angelillo and The Collaborative Working Group. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Italo Francesco Angelillo, aXRhbG9mLmFuZ2VsaWxsbyYjeDAwMDQwO3VuaWNhbXBhbmlhLml0
 Giorgia Della Polla1
Giorgia Della Polla1 Grazia Miraglia del Giudice
Grazia Miraglia del Giudice Lucio Folcarelli
Lucio Folcarelli Annalisa Napoli
Annalisa Napoli Italo Francesco Angelillo
Italo Francesco Angelillo The Collaborative Working Group
The Collaborative Working Group