
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 10 November 2022
Sec. Public Mental Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1049069
This article is part of the Research Topic Emerging Technologies for Employee Mental Health and Work Performance under Industry 4.0/5.0 View all 9 articles
Comparing a family structure to a company, one can often think of parents as leaders and adolescents as employees. Stressful family environments and anxiety levels, depression levels, personality disorders, emotional regulation difficulties, and childhood trauma may all contribute to non-suicidal self-injury (NSSI) behaviors. We presented a support vector machine (SVM) based method for discovering the key factors among mazy candidates that affected NSSI in adolescents. Using SVM as the base learner, and the binary dragonfly algorithm was used to find the feature combination that minimized the objective function, which took into account both the prediction error and the number of selected variables. Unlike univariate model analysis, we used a multivariate model to explore the risk factors, which better revealed the interactions between factors. Our research showed that adolescent education level, anxiety and depression level, borderline and avoidant personality traits, as well as emotional abuse and physical neglect in childhood, were associated with mood disorders in adolescents. Furthermore, gender, adolescent education level, physical abuse in childhood, non-acceptance of emotional responses, as well as paranoid, borderline, and histrionic personality traits, were associated with an increased risk of NSSI. These findings can help us make better use of artificial intelligence technology to extract potential factors leading to NSSI in adolescents from massive data, and provide theoretical support for the prevention and intervention of NSSI in adolescents.
Non-suicidal self-injury (NSSI) is a common psychiatric behavioral problem that threatens adolescents' health. NSSI refers to behaviors that do not aim at suicide, intentionally and directly harm their body tissues and are not recognized by society and culture (1). Common types of NSSI include cutting, scratching, hitting, knocking, and burning themselves (1). In 2013, the Diagnostic and Statistical Manual of Mental Disorders (5th edition) (DSM-5) classified NSSI as a separate disorder and established strict diagnostic criteria. Currently, suicide has become the third leading cause of death among adolescents (10–19 years old) worldwide, and NSSI is an important prerequisite for adolescent suicide and one of the strongest predictors of future suicide (2), adding a huge medical and economic burden to society. Furthermore, NSSI is associated with other adverse outcomes, such as cognitive impairment, poor interpersonal relationships, and violent crimes (3). NSSI has become an important global adolescent mental health problem. Currently, there are still many clinical challenges in the identification and intervention of NSSI (4). However, understanding the factors associated with NSSI is essential for conducting clinical risk assessment and therapeutic interventions.
The incidence of NSSI is higher in adolescents than in any other age group (5). Lim et al. (6) conducted a systematic review of 66 studies and showed that the lifetime and 12-month incidence of NSSI were 22.1 and 19.5%, respectively. In addition, there were differences in the incidence of NSSI among different regions and ethnic groups. Studies have shown that Caucasians have the highest incidence of NSSI (7). Zubrick et al. (8) surveyed 2,967 adolescents in Australia in 2013–2014 and found that the 12-month incidence of NSSI in adolescents was about 8%. Brunner et al. (9) investigated 12,068 adolescents from 11 countries in Europe in 2014 and found that the lifetime incidence of self-injury was 27.6%, ranging from 17.1 to 38.6% in each country. A recent meta-analysis study showed that the 12-month incidence of NSSI among adolescents was higher in low- and middle-income countries than in high-income countries (6). In recent years, the incidence of NSSI among adolescents in China has been on the rise, and surveys in different cities and regions have shown that the prevalence of NSSI among adolescent ranges from 5.4 to 33.8% (10). Moreover, the onset age of adolescent NSSI behavior is mainly concentrated in early adolescence (12–14 years old). The incidence of NSSI peaks in mid-adolescence (15–16 years old), and then decreases in late adolescence (18 years old) (11). Notably, the early onset of NSSI creates greater disease vulnerability. Studies have shown that individuals with NSSI onset younger than 12 years old tend to develop severe NSSI behaviors (12). Moreover, NSSI in early adolescence may predict the onset of mental disorders in late adolescence. Therefore, identifying risk factors for NSSI in adolescents is important for the early identification and prevention of NSSI behaviors.
Earlier studies have shown that NSSI behavior is the end product of interactions between genetic, biological, psychiatric, psychological, social and cultural factors (13). The potential causes of NSSI include individual and environmental factors (14). Individual factors include mental illness, personality traits, and emotional regulation abilities. Depressive disorder and borderline personality disorder are the most common co-morbidities in the adolescent with NSSI. Depressive symptoms are important predictors of NSSI behavior in adolescents (15). In addition, NSSI is considered to be a precursor of borderline personality disorder in a socio-biological developmental model (16). NSSI behaviors are associated with adolescents' personality traits. Studies have shown that adolescents with NSSI show higher levels of impulsivity than those without NSSI (17) and have higher scores on all subscales of the Barratt Impulsivity Scale (18). Furthermore, emotional regulation plays an important role in adolescents' NSSI behavior (19). On the other hand, the family environment is the most important growth environment for adolescents and plays an important role in the development of adolescents' characters and behaviors. Family systems theory pointed out that family functions affected the physical and mental health of family members (20), and had an important impact on individual emotional and behavioral problems (21). Research indicated that poor family function mediated the link between childhood adversity and NSSI in adolescents (22). In addition, adolescents with pathological family relationships and disharmonious relationships with their parents have a higher risk of self-harm (23). Furthermore, experiencing adverse life events (parental abuse or neglect) in childhood (24), parental divorce (25), family death (26), and witnessing parental violence (27) have all been associated with NSSI behaviors in adolescents. Notably, improving family relationships may reduce NSSI in later childhood who experience adverse life events in childhood. Therefore, understanding the family environment of Chinese adolescents with NSSI is beneficial to explore the influence of family factors on adolescents with NSSI, thereby improving family relationships and functions.
Feature selection is a key preprocessing mechanism in data mining tasks, which avoids the interference of irrelevant variables by finding the optimal feature subset from the given dataset (28). With the development and enrichment of artificial intelligence technology, researchers have developed a large number of feature selection methods (29), including three categories of filter (30), wrapper (31), and embedding (32). The ensemble algorithm based on the decision tree model, such as random forest (33), evaluates the importance of features according to the improvement of purity. Principal component analysis (34, 35) and its improvements (36) are also commonly used methods of dimensionality reduction. The feature is transformed into a set of line-independent variables through orthogonal transformation, so that a large number of variables can be represented by a few principal components. The least absolute shrinkage and selection operator (LASSO) (37, 38) and ridge regression methods (39) take the features' weight as a regularization term while considering the accuracy of multiple linear regression to reduce the number of selected features. In this paper, inspired by the LASSO method, we proposed a support vector machine (SVM) based feature selection method to find the key indicators of NSSI. We used a binary state vector to represent the selected indicator, took the average error rate of the SVM classifier 10-fold cross-validation as the objective function, and the other part of the objective function was the number of selected indicators. The binary dragonfly algorithm was used to optimize the state vector to minimize the objective function.
Currently, most studies on adolescent NSSI in China have explored the effect of a single factor on NSSI behavior or explored the correlation between two factors, and no studies have yet analyzed the effect of individual and family factors on adolescent NSSI behavior. Thus, we present a support vector machine (SVM) based method to discover the key factors among individual and family factors influencing adolescent NSSI, providing a theoretical basis for the prevention and intervention of adolescent NSSI.
We conducted this cross-sectional research from June 2020 to April 2021 in China. Adolescents aged 10–24 years were recruited. Rather than age 10–19 years, the definition of 10–24 years corresponds more closely to adolescent growth and the general understanding of this life stage, facilitating expanding research (40). What's more, an expanded and broader definition of the adolescent is critical to the development of social policies and service systems (40). Adolescents diagnosed with mood disorders (i.e., depressive disorder, depressive episode of bipolar disorder, and unspecified behavioral and mood disorders originating in childhood and adolescence) according to the International Classification of Diseases-10 (ICD-10) were recruited from the psychological ward and outpatient clinic of a tertiary hospital in Changsha, China. After eliminating participants with suicidal ideation and attempts within the past 12 months, participants with mood disorders were divided into two groups based on the DSM-5 criteria of NSSI: with and without NSSI groups. Typical developmental (TD) adolescents studying in primary school, middle school, or university were recruited. All participants or parents signed an informed consent form. Adolescents were excluded if they: (1) suffered from severe somatic disorders; (2) had cognitive impairment, audiovisual impairment, etc.; (3) suffered from other severe mental illnesses. The research was approved by the medical ethics committee of the Second Xiangya Hospital of Central South University (MD20200309).
The surveys included self-reported information on sociodemographic characteristics including adolescents' characteristics (i.e., gender, age, ethnicity, education level, grade) and parental characteristics (i.e., education level, age).
The generalized anxiety disorder-7 (GAD-7), developed by Spitzer et al. (41), is used to assess subjects' anxiety symptoms and severity during the last 2 weeks. The scale contains seven items and uses a four-point Likert scale scored from 0 (not at all) to 3 (almost every day). The higher the score, the more severe the anxiety symptoms. A total score of 0–4 indicates no anxiety; 5–9 indicates mild anxiety; 10–13 indicates moderate anxiety; 14–18 indicates moderate to severe anxiety; and 19–21 indicates severe anxiety. The Cronbach's alpha co-efficient for this scale in this study was 0.924.
The patient health questionnaire-9 (PHQ-9), developed by Kroenke et al. (42), is used to assess subjects' depressive symptoms during the last 2 weeks. The scale contains 9 items, each of which consists of four options and is scored on a four-point scale (0 = not at all, 3 = almost every day). The higher the score, the more severe the depression. A total score of <5 means no depression, 5–9 mild depression, 10–14 moderate depression, 15–19 moderate to severe depression, and ≥20 severe depression. The Cronbach's alpha co-efficient of internal consistency was 0.927.
The personality diagnostic questionnaire-4+ (PDQ-4+), developed by Hyler et al. (43), is a self-administered questionnaire for screening personality disorders, which was consistent with the DSM-IV criteria for the 10 officially recognized and two proposed Axis II personality disorders. Yang, a Chinese scholar (44), translated the PDQ-4 into Chinese. Moreover, another Chinese scholar translated the PDQ-4+ into Chinese and revised it for the Chinese cultural context, resulting in a Chinese version of the PDQ-4+ with good reliability and validity (45). In this study, we used the Chinese version of the PDQ-4+ (45). The higher the score, the more consistent the personal characteristic description. The Cronbach's alpha co-efficient of this scale in the present study was 0.921.
The difficulties in emotion regulation scale (DERS), developed by Gratz and Roemer in 2004 (46), is a self-report questionnaire used to assess subjects' difficulties in emotion regulation. The scale contains 36 items and six subscales (non-acceptance of emotional responses, difficulties in engaging in goal-oriented behaviors, difficulties in controlling impulses, lack of emotional awareness, restricted access to emotional regulation strategies, and lack of emotional clarity). The scale uses a five-point Likert scale scored from 1 (almost never) to 5 (almost always). The higher the score, the more difficult to regulate emotion. The Cronbach's alpha co-efficient for this scale in this study was 0.941.
Subjects' trauma experience in childhood was assessed by childhood trauma questionnaire-short form (CTQ-SF), which was developed by Bernstein et al. (47) and translated into Chinese by Fu et al. (48). The scale represents a 28-item retrospective self-report questionnaire which contains five subscales: emotional (EN) and physical neglect (PN), emotional (EA), sexual (SA) and physical abuse (PA) (49). Each item is scored on a five-point Likert scale from 1 (never true) to 5 (very often true). The Cronbach's alpha co-efficient of this scale in the present study was 0.793.
Multiple groups were compared using Chi-square tests. Meanwhile, non-parametric Kruskal-Wallis tests and pairwise comparisons were used. α < 0.05.
Data mining and data analysis through information technology to obtain potential value can better guide people's production and life. In order to reduce the noise contained in the data and improve the reliability of data mining, lots of feature selection algorithms have been proposed and adopted for diagnosis, classification, and categorization in recent years. The tree model computes variable importance by finding the optimal partitioning features that vary purity, information gain, or gain rate, and leads to different decision tree generation schemes, such as iterative dichotomy 3 (ID3) (50), C4.5 (51, 52) and Classification and Regression Trees (CART) (53). Our previous work proposed the mixed correlation co-efficient to measure the linear or non-linear correlation between two variables and used it to study the user participation mechanism in virtual tourism communities (54). As a common tool for big data mining, machine learning algorithms have been more and more widely used in the clinical and medical fields, such as COVID-19 (55–57), Crohn's disease (58), and schizophrenia diagnosis (59–61).
Support vector machine (SVM) was proposed by Cortex and Vapnik (62) in the 1990s, and quickly became the mainstream technology in machine learning methods due to its excellent performance in text classification. SVM can avoid the curse of dimensionality and overfitting in solving pattern recognition tasks with a small number of samples, non-linearity, and high dimensionality. The principle of support vector classification (SVC) is to find an optimal classification hyperplane, that is, it can tolerate the local disturbance of training samples while distinguishing samples of different categories. As shown in Figure 1A, although multiple hyperplanes can distinguish samples, only the red hyperplane located in the middle of the two classes has the best robustness and is considered the optimal division hyperplane. For the training set {xi, yi} record the positive sample as yi = 1 and the negative sample as yi = −1, then the hyperplanes (ω, b) is required to hold the following equations:
and the optimal division hyperplanes in Figure 1B can be written as . The optimization goal is to maximize the distance between the support samples and the hyperplane larger, that is:
In fact, it is difficult to find a hyperplane that can accurately divide the two classes into practical problems. In Figure 2, a slack variable can be introduced to allow SVC to make misclassification of a few samples, and the corresponding optimization function is given by:
Where is the l2 norm, and C is the penalty co-efficient, The larger C is, the fewer training samples do not satisfy the constraints. Equation (3) is equivalent to Equation (2) when C → ∞.

Figure 1. Hyperplanes in sample space: (A) There are multiple hyperplanes in the sample space that can accurately classify samples; (B) The optimal division hyperplanes.
The Dragonfly Algorithm (DA) (63) is an intelligent optimization algorithm that finds the optimal solution of the objective function by imitating the group behavior of dragonflies to find food and avoid natural enemies. The binary Dragonfly Algorithm (BDA) is the discrete form of DA that represents the position of the dragonfly as a vector with elements 0 or 1 (64). The behavior of a dragonfly colony includes five main behaviors: namely separation, alignment, cohesion, attraction, and distraction, which are used to update the position of each dragonfly. The mathematical model of these behaviors can be described as follows:
Separation. The purpose of separation is to prevent adjacent dragonflies from colliding, that is, two dragonflies are not allowed to exist in the same position at the same time. Thus, we have:
where X is the position of a dragonfly in feature space, and there are M dragonflies nearby, and their coordinates are marked as Xj.
Alignment. Alignment requires that the velocity of each dragonfly match its swarm or sub-swarm, preventing falling behind or leaving the swarm. That is, velocity V should equal the average speed of the nearby dragonflies:
Cohesion. Cohesion prevents the group from being dissolved, it allows dragonflies to move toward the center of the group, that is:
Attraction. Dragonflies need to eat in order to survive, so they are attracted to food. At the same time, the dragonfly in the swarm flew toward the leading dragonfly Xpb closest to the food Xf. This process can be defined as:
Distraction. In order to avoid predation, dragonflies need a distraction to stay away from natural enemies. Similar to the attraction process, Xpw means the position of the dragonfly closest to the enemy Xe is also considered. Distraction can be expressed mathematically as:
We use the iterative algorithm defined in Equation 9 to update the coordinate vector of the dragonfly to guide the dragonfly to find the food, and ΔXi represents the stepping direction.
where represents the d-th position of the i-th dragonfly, rand is a random number uniformly distributed in the interval [0, 1]. αi, i = 1, 2, 3, 4, 5 are the weights of five behaviors, which are set as 0.2 as default.
In order to select key features from given data sets, a novel SVM-based selector is designed in this section, and its brief flowchart is given in Figure 3. The most important thing is to define “good” as the selected combination of features. A set of “good” features needs to have the following three characteristics. First, it can minimize the error of the model on the validation set. Second, the model obtained from this set of features has better robustness to the data set, that is, it is not easy to be attacked by individual outlier samples. Finally, choose as few metrics as possible. Combining the above requirements, we define the following objective function:
where datai is a sub-dataset obtained by resampling the original dataset data by K-fold cross-validation method. The SVM is used as the base classifier and training with the training data, Err(S, datai) is the prediction error on the corresponding validation set. S is the selected feature and |S| represents the number of S. |O| means the number of all candidate features. Then, the feature selection task is transformed into finding a combination of features that minimizes the objective function. This optimization problem can be implemented by BDA, that is, expand S with one-hot encoding as Ŝ, which is an |O|-dimensional vector, each element in Ŝ is 0 or 1, where Ŝi = 0 means that S does not select the feature xi, otherwise Ŝi = 1 means S contains a feature xi. Considering Ŝ as the position of the dragonfly, BDA updates Ŝ by imitating the movement trajectory of the dragonfly. We gave the pseudo-code of this feature selection algorithm in Algorithm 1.
In addition, the experiments are independently repeated on multiple sub-datasets through the bootstrapping sampling technique, making the selected features more robust. Denote the variable combination that minimizes the objective function on the sub-dataset datai as Si, and the average classification accuracy on K-fold cross-validation is Acci. A voting algorithm is used to add up the features selected on each sub-data set. In fact, these votes are not equal. The weight of each vote is determined by Acci, which means that the combination of selected variables that makes the classification accuracy higher will be more favored. Finally, our SVM-based selector can obtain the M metrics with the most votes, and default M = mean(|Si|), which is the average number of selected features in sub-datasets, to avoid adding more hyperparameters.
Ultimately, we included 186 adolescents with mood disorders, 137 of whom had NSSI behaviors and 49 of whom did not. We also enrolled 96 typically developing adolescents. A total of 77 males and 205 females were included in this study, with a male-to-female ratio of ~1:3, which was close to the male-to-female incidence ratio of NSSI (65). Comparisons between groups revealed that the differences between the three groups were statistically significant in terms of adolescent age, education level, and parental age, while differences in parental education levels were not significant. Sociodemographic characteristics were shown in Table 1.
Our result showed that with NSSI group scored highest on all psychological/behavioral problems except for the sexual abuse score, followed by without NSSI and TD groups. The non-parametric Kruskal-Wallis tests revealed significant differences between the three groups for psychological and behavioral variables, including anxiety, depression, personality traits, emotion regulation ability, and childhood trauma (Table 2). Specifically, the average anxiety and depression levels were moderate to severe (>14) and severe (>19) in the mood disorder with NSSI group, moderate (>10) and moderate to severe (>15) in the mood disorder without NSSI group, and mild in the TD group. Furthermore, the PDQ-4+ scores indicated that adolescents in the mood disorder with NSSI group may have paranoid (4.175 ± 1.499 >4), borderline (7.700 ± 1.858), avoidant (6.401 ± 1.572), and obsessive-compulsive (6.182 ± 2.381) personality traits, whereas adolescents in the mood disorder without NSSI group may have borderline (6.041 ± 2.267), avoidant (5.918 ± 1.923), and obsessive-compulsive (5.592 ± 2.571) personality traits, while the TD group did not indicate any personality traits. Post-hoc pairwise tests showed that compared with the mood disorder with NSSI group, the mood disorder without NSSI group scored significantly lower on PHQ-9, borderline, physical abuse, awareness, clarity, and impulse scores; the TD group scored significantly lower on all study variables except for sexual abuse score. Moreover, compared with the mood disorder without NSSI group, the TD group scored significantly lower on all study variables except for physical abuse and neglect, sexual abuse, and awareness. Furthermore, when the mood disorder (both with and without NSSI) and TD groups were compared, there were significant differences between the two groups on all indicators except sexual abuse (Table 2).
Since adolescents with NSSI are often accompanied by mood disorders, identifying indicators that distinguish mood disorders from TD adolescents lays the foundation for further prediction of NSSI behavior. Hyperparameters in the SVM-based selector were set to default, with penalty co-efficient C = 1. The 10 dragonfly positions were randomly initialized in BDA, the personal learning rate was set as 0.4, and the group learning rate was 0.7. The objective function gradually decreased with the training process and converged after 150 iterations, and the shaded area represented the variance of 100 independent replicates (Figure 4A). The average number of selected features was 7.17, and the votes for each feature were plotted in Figure 4C.

Figure 4. (A) Objective function of the training process for identifying mood disorders; (B) The distribution of classification accuracy for identifying mood disorders; (C) Feature voting for identifying mood disorders; *selected feature.
It could be seen that adolescent education level, anxiety, and depression level, borderline and avoidant personality disorder, emotional abuse, and physical neglect were the seven characteristics that received the most votes on the 100 sub-datasets, and were thought to be highly correlated with identifying mood disorders (Figure 4C). To further illustrate the effectiveness of the selector, we verified the classification performance on the resampling sub-dataset using all features and filtered features, respectively. The distribution of classification accuracy was depicted in Figure 4B, which showed that only seven features were selected, but the prediction accuracy was even slightly improved, indicating that using only these selected features was sufficient to distinguish the mood disorder group from the TD group while avoiding the interference of irrelevant variables. We also compared different classification algorithms (Table 3), which demonstrated that SVM performed better in classification tasks. Most machine learning models could accurately distinguish between the mood disorder and TD groups, whereas LASSO got disoriented by failing to describe non-linear associations. Random forests implied feature selection and achieved better results than KNN and SVM when all original features were used.
The second part was to discover key factors in identifying NSSI. Similar to the mood disorders above, an SVM-based feature selector was optimized with BDA for 150 steps, and the decay of the objective function was plotted in Figure 5A. We also calculated the voting in 100 independent replicates (Figure 5C), where gender, adolescent education level, paranoid, borderline, and histrionic personality disorders, physical abuse, and non-acceptance of emotional responses were highlighted in red. Females were more likely to have NSSI than males, and the occurrence of NSSI behaviors was negatively correlated with their educational level. Special personality traits (e.g., paranoid, borderline, and histrionic) can help distinguish between NSSI behavior in patients with mood disorders. We demonstrated that using the selected seven key indicators to predict the occurrence of NSSI behavior was more accurate than using all indicators, proving the rationality of feature selection (Figure 5B).
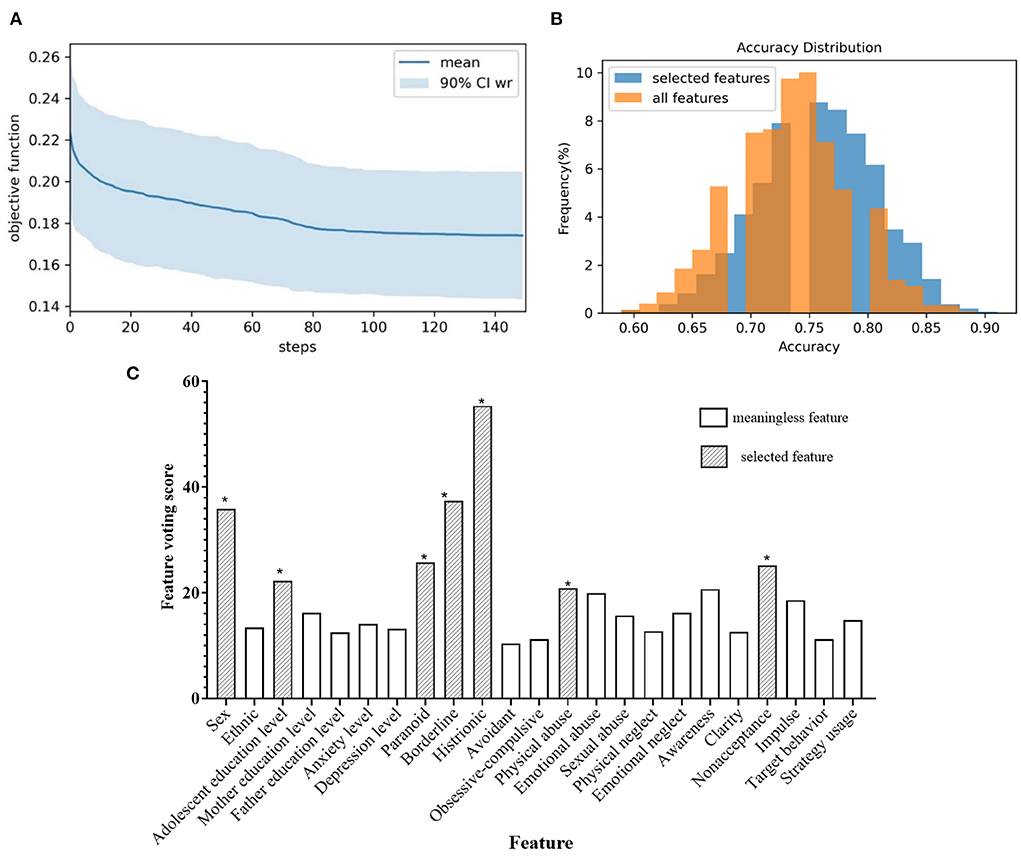
Figure 5. (A) Objective function of the training process for identifying NSSI; (B) The distribution of classification accuracy for identifying NSSI; (C) Feature voting for identifying NSSI; *selected feature.
We also compared other machine learning approaches to distinguishing NSSI from mood disorders (Table 4). Distinguishing mood disorders in adolescents with and without NSSI was a more difficult task, and the accuracy of all machine learning algorithms we considered was about 66–76%, although feature selection still improved prediction precision. In 1,000 independent repeated experiments, the average accuracy of SVM on the original features was 73.45%, with the highest accuracy of 87.39%, which was higher than KNN and Logistic regression, indicating that SVM retained some advantages in high-dimensional non-linear classification tasks. Our experiments also showed that the decision tree model was prone to overfitting, resulting in poor classification accuracy. The random forest model avoided this problem by constructing multiple decision trees. In addition, the random forest used important features instead of all features for prediction by limiting the number of nodes, and the regularization term in LASSO also played a role in feature selection, which had a better performance than the SVM method using all features. Our SVM-based method combined the above two advantages, which not only retained the high classification accuracy of SVM, but also avoided the attack of unimportant or harmful variables on the prediction model. Compared with other machine learning methods, the average accuracy was improved by 1%, and the highest accuracy could exceed 90%.
In this paper, we proposed an SVM-based feature selection method for identifying influencing factors on adolescents with NSSI. An objective function was designed to describe how “good” the feature combinations, which required both higher accuracy and fewer features. Bootstrapping sampling made the features obtained by the selector more robust and might not be disturbed by abnormal samples. In addition, our findings proved that using only a few selected features can achieve higher accuracy than using all features, indicating that these selected features were critical for accurate classification, and that the unselected features interfered with the model. Furthermore, as a powerful machine learning technique, SVM exhibited better performance than other statistical methods. Our study showed that adolescent's anxiety and depression levels, borderline and avoidant personality traits, experiencing emotional abuse and physical neglect in childhood, and education level were associated with mood disorders in adolescents; adolescent's gender, paranoid and histrionic personality traits, suffering physical abuse in childhood, emotion non-acceptance, and their education level were associated with an increased risk of NSSI.
We found that adolescents in the mood disorder with NSSI group scored higher on psychological symptoms and childhood trauma than the without NSSI and TD groups, while the mood disorder group scored significantly higher on almost variables than the TD group. These findings supported the point that there were significant differences in psychological behavior between adolescents with and without NSSI. Not only that, adolescents with and without NSSI with mood disorders shared similar psychological and behavioral characteristics, but these characteristics were more prominent in adolescents with NSSI. Overall, adolescents with NSSI and mood disorders have similar but independent risk factors. However, in the overall sample of this study, univariate analyzes found no statistically significant differences in most variables between the mood disorder groups with and without NSSI.
In this study, the reporting rate of NSSI in female adolescents was higher than that in male adolescents, and multivariate analysis also showed that male was a protective factor for NSSI behavior in adolescents, which was consistent with the results of a recent meta-analysis (3). Previous studies have shown that the gender difference in clinical samples was larger than that in community samples, and the difference gradually decreases with age. In addition, there were differences in the patterns and motivations of NSSI among adolescents of different genders (66). Females were more likely to engage in cutting, scratching, and biting as means of NSSI, while males were more likely to burn, hit and bang. Moreover, female adolescents engaged in NSSI mainly for emotional regulation and self-control, while male adolescents were more eager to generate impulsive pleasure. The reasons for gender differences in adolescent NSSI may include (3): (a) biological factors: hormonal (e.g., androgens and estradiol) differences between males and females may influence gender involvement in NSSI; (b) differences in male and female emotion regulation strategies: research has shown that females were more likely than males to engage in emotion regulation strategies, and NSSI was considered an emotion regulation strategy.
The results of both univariate and multivariate analyzes showed that anxiety and depression levels were associated with NSSI in adolescents, which was consistent with previous research. Foreign studies have reported that there was a bidirectional correlation between anxiety, depression and NSSI. The higher the score of the anxiety and depression scale, the greater the likelihood of NSSI. Conversely, NSSI will increase anxiety and depression (67). Using a latent growth curve modeling, scholars suggested that lifetime depression predicted the longitudinal course of NSSI from grade 10 to 12, with depressed adolescents showing greater and more stable NSSI engagement over time than non-depressed adolescents (68). In addition, studies have shown the mediating role of depression on other factors (i.e., peer acceptance and frequent nightmares) and NSSI behavior in adolescents (69, 70). Furthermore, post-traumatic stress disorder, dissociative disorders, obsessive-compulsive disorders, eating disorders, sleep disorders, and substance use disorders were also common co-occurring disorders in adolescents with NSSI (1, 71).
Adolescent NSSI is associated with specific personality traits. Personality is a stable and lasting characteristic of a person's mental activity, especially in emotional activity and volitional behavior. Individuals with personality disorders were frequently diagnosed as being at risk for suicide, which suggested that personality pathology may reflect important individual differences in predicting suicide attempts (72). Previous studies showed that several personality disorder dimensions (i.e., paranoid, antisocial, borderline, histrionic, and dependent) emerged as risk factors for suicidal attempts based on univariate models (72). However, Jenkins et al. (72) found borderline personality disorder severity uniquely predicted suicidal attempts over other personality disorder severity based on multivariate models, which was similar to our findings. Specifically, borderline personality disorder is one of the most common co-morbidities of adolescent NSSI (71). Studies have shown that ~61% of adolescents with borderline personality disorder engaged in at least one NSSI behavior (73). More than that, NSSI was considered a precursor to the development of borderline personality disorder under the sociobiological developmental model (16). A review based on seven longitudinal studies showed a longitudinal association between NSSI and borderline personality disorder symptoms in adolescents (16).
Furthermore, emotion regulation was one of the motivations for NSSI (74), which was consistent with our findings. The previous study has demonstrated that emotion regulation ability is negatively associated with NSSI behavior (75). In adolescence, adaptive internal emotion regulation has limited efficacy; therefore, adolescents lack effective coping strategies in dealing with negative emotions and are more likely to adopt NSSI behaviors to alleviate negative emotions, which results in impaired social relationships and increased negative emotions, forming a vicious cycle. Emotional regulation ability is developed during the emotional interactions with caregivers in the early stage of children's growth. Parents' denigration or contempt behaviors and frequent negative emotions against children will weaken children's emotional regulation ability and disrupt the development of normal emotional regulation ability (76). Therefore, effective emotion regulation strategies should be carried out based on adolescents and their parents in order to achieve a virtuous cycle of emotion regulation.
Another important finding was that physical abuse in childhood significantly increased the risk of NSSI in adolescents. Studies have demonstrated that childhood abuse and neglect (both physical and emotional) were positively associated with self-injurious behavior and that the incidence of NSSI increased with greater levels of abuse and neglect (77, 78). The American scholar demonstrated that childhood physical and sexual abuse was strongly associated with adolescent NSSI and that the frequency of NSSI increased with the frequency of abuse (79). Moreover, the incidence of NSSI was higher in females than in males when exposed to high levels of sexual abuse, emotional neglect, and physical abuse (80). However, sexual abuse did not show significance in our study. Furthermore, we speculated that since China has fully implemented 9-year compulsory education, educational attainment to some extent implies the age of adolescents. Due to NSSI, they may interrupt their studies, resulting in lower educational attainment. Therefore, parents and health managers should pay attention to the healthy growth of children and reduce the occurrence of childhood abuse and trauma.
Our research focused on improving people's mental health based on artificial intelligence technology and discovered key indicators that affect NSSI in adolescents. Unlike univariate model analysis, we used a multivariate model to explore the risk factors, which better revealed the interactions between factors. However, sampling methods may limit the generalizability of study results. The majority of participants were outpatients, and the results may differ from inpatients or non-treatment seeking populations. Moreover, this study was cross-sectional, which could not infer the causal relationships between factors and NSSI behaviors in adolescents with mood disorders. Data from this survey were obtained from questionnaires and recall bias was unavoidable. Future studies could use a longitudinal study design to follow up on risk factors for adolescent NSSI behavior. It is worth noting that from family promotion to collective or company, our proposed SVM-based selector can also be used as a data-driven technique to improve the mental health of members and employees, find the key causes of employee mental health problems, and help companies reduce possible employee mental health problems.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of the Second Xiangya Hospital of Central South University (MD20200309). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
JY and YL conceived and designed the research. YC, GY, and ZW analyzed the data. XF and YT collected the data. JY and YC reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by the Clinical Nursing Research Foundation of the Second Xiangya Hospital of Central South University (grant number 2021-HLKY-05), Major Scientific and Technological Projects in Hunan Province (grant number 2020SK208), the National Natural Science Foundation of China (grant numbers 81974217 and 81901388), the Natural Science Foundation of Hunan Province, China (grant numbers 2020JJ5825 and 2020JJ5830), and the Major Scientific and Technological Projects for Collaborative Prevention and Control of Birth Defects in Hunan Province (grant number 2019SK1015).
We sincerely thank the adolescents who participated in our research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Fan YY, Liu J, Zeng YY, Conrad R, Tang YL. Factors associated with non-suicidal self-injury in Chinese adolescents: a meta-analysis. Front Psychiatry. (2021) 12:747031. doi: 10.3389/fpsyt.2021.747031
2. McManus S, Gunnell D, Cooper C, Bebbington PE, Howard LM, Brugha T, et al. Prevalence of non-suicidal self-harm and service contact in England, 2000–14: repeated cross-sectional surveys of the general population. Lancet Psychiatry. (2019) 6:573–81. doi: 10.1016/S2215-0366(19)30188-9
3. Wang YJ, Li X, Ng CH, Xu DW, Hu S, Yuan TF. Risk factors for non-suicidal self-injury (NSSI) in adolescents: a meta-analysis. EClinicalMedicine. (2022) 46:101350. doi: 10.1016/j.eclinm.2022.101350
4. Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR. Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. (2015) 54:97–107.e2. doi: 10.1016/j.jaac.2014.10.009
5. Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. (2008) 30:133–54. doi: 10.1093/epirev/mxn002
6. Lim KS, Wong CH, McIntyre RS, Wang J, Zhang Z, Tran BX, et al. Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int J Environ Res Public Health. (2019) 16:4581. doi: 10.3390/ijerph16224581
7. Klonsky ED, Muehlenkamp JJ. Self-injury: a research review for the practitioner. J Clin Psychol. (2007) 63:1045–56. doi: 10.1002/jclp.20412
8. Zubrick SR, Hafekost J, Johnson SE, Lawrence D, Saw S, Sawyer M, et al. Self-harm: prevalence estimates from the second Australian child and adolescent survey of mental health and wellbeing. Aust N Z J Psychiatry. (2016) 50:911–21. doi: 10.1177/0004867415617837
9. Brunner R, Kaess M, Parzer P, Fischer G, Carli V, Hoven CW, et al. Life-time prevalence and psychosocial correlates of adolescent direct self-injurious behavior: a comparative study of findings in 11 European countries. J Child Psychol Psychiatry. (2014) 55:337–48. doi: 10.1111/jcpp.12166
10. Yu G, Zhang Y, Tang L, Xu F. Progress in health management of adolescent non-suicidal self-injury behavior. Chin J Health Manage. (2022) 16:43–6. doi: 10.3760/cma.j.cn115624-20210902-00511
11. Moran P, Coffey C, Romaniuk H, Olsson C, Borschmann R, Carlin JB, et al. The natural history of self-harm from adolescence to young adulthood: a population-based cohort study. Lancet. (2012) 379:236–43. doi: 10.1016/S0140-6736(11)61141-0
12. Novak MA, Meyer JS. A rhesus monkey model of non-suicidal self-injury. Front Behav Neurosci. (2021) 15:674127. doi: 10.3389/fnbeh.2021.674127
13. Fox KR, Ribeiro JD, Kleiman EM, Hooley JM, Nock MK, Franklin JC. Affect toward the self and self-injury stimuli as potential risk factors for non-suicidal self-injury. Psychiatry Res. (2018) 260:279–85. doi: 10.1016/j.psychres.2017.11.083
14. Annarosa C, Stefania C, Paolo C. Non-suicidal self-injury: a systematic review. Front Psychol. (2017) 8:1946. doi: 10.3389/fpsyg.2017.01946
15. Plener PL, Schumacher TS, Munz LM, Groschwitz RC. The longitudinal course of non-suicidal self-injury and deliberate self-harm: a systematic review of the literature. Borderline Personal Disord Emot Dysregul. (2015) 2:2. doi: 10.1186/s40479-014-0024-3
16. Stead VE, Boylan K, Schmidt LA. Longitudinal associations between non-suicidal self-injury and borderline personality disorder in adolescents: a literature review. Borderline Personal Disord Emot Dysregul. (2019) 6:3. doi: 10.1186/s40479-019-0100-9
17. Claes L, Muehlenkamp J. The relationship between the UPPS-P impulsivity dimensions and non-suicidal self-injury characteristics in male and female high-school students. Psychiatry J. (2013) 2013:654847. doi: 10.1155/2013/654847
18. Tschan T, Peter-Ruf C, Schmid M, In-Albon T. Temperament and character traits in female adolescents with non-suicidal self-injury disorder with and without comorbid borderline personality disorder. Child Adolesc Psychiatry Ment Health. (2017) 11:4. doi: 10.1186/s13034-016-0142-3
19. Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. J Consult Clin Psychol. (2004) 72:885–90. doi: 10.1037/0022-006X.72.5.885
20. Beavers R, Hampson RB. The beavers systems model of family functioning. J Fam Ther. (2002) 22:128–43. doi: 10.1111/1467-6427.00143
21. Baetens I, Andrews T, Claes L, Martin G. The association between family functioning and NSSI in adolescence: the mediating role of depressive symptoms. Fam Sci. (2015) 6:330–7. doi: 10.1080/19424620.2015.1056917
22. Cassels M, van Harmelen AL, Neufeld S, Goodyer I, Jones PB, Wilkinson P. Poor family functioning mediates the link between childhood adversity and adolescent non-suicidal self-injury. J Child Psychol Psychiatry. (2018) 59:881–7. doi: 10.1111/jcpp.12866
23. Gratz KL. Risk factors for deliberate self-harm among female college students: the role and interaction of childhood maltreatment, emotional inexpressivity, and affect intensity/reactivity. Am J Orthopsychiatry. (2010) 76:238–50. doi: 10.1037/0002-9432.76.2.238
24. Muehlenkamp JJ, Kerr PL, Bradley AR, Larsen MA. Abuse subtypes and non-suicidal self-injury preliminary evidence of complex emotion regulation patterns. J Nerv Ment Dis. (2010) 198:258–63. doi: 10.1097/NMD.0b013e3181d612ab
25. Wang F, Lu J, Lin L, Cai J, Xu J, Zhou X. Impact of parental divorce versus separation due to migration on mental health and self-injury of Chinese children: A cross sectional survey. Child Adolesc Psychiatry Ment Health. (2021) 15:71. doi: 10.1186/s13034-021-00424-z
26. Cerutti R, Manca M, Presaghi F, Gratz KL. Prevalence and clinical correlates of deliberate self-harm among a community sample of Italian adolescents. J Adolesc. (2011) 34:337–47. doi: 10.1016/j.adolescence.2010.04.004
27. Asgeirsdottir BB, Sigfusdottir ID, Gudjonsson GH, Sigurdsson JF. Associations between sexual abuse and family conflict/violence, self-injurious behavior, and substance use: the mediating role of depressed mood and anger. Child Abuse Negl. (2011) 35:210–9. doi: 10.1016/j.chiabu.2010.12.003
28. Pal M, Foody GM. Feature selection for classification of hyperspectral data by SVM. IEEE Trans Geosci Remote Sens. (2010) 48:2297–307. doi: 10.1109/TGRS.2009.2039484
29. Jovic A, Brkic K, Bogunovic N. A review of feature selection methods with applications. In: 2015 8th International Convention on Information and Communication Technology, Electronics and Microelectronics (Mipro). Opatija (2015). p. 1200–5. doi: 10.1109/MIPRO.2015.7160458
30. Peng HC, Long FH, Ding C. Feature selection based on mutual information: criteria of max-dependency, max-relevance, and min-redundancy. IEEE Trans Pattern Anal Mach Intell. (2005) 27:1226–38. doi: 10.1109/TPAMI.2005.159
31. Sebban M, Nock R. A hybrid filter/wrapper approach of feature selection using information theory. Pattern Recognit. (2002) 35:835–46. doi: 10.1016/S0031-3203(01)00084-X
32. Afshar M, Usefi H. Optimizing feature selection methods by removing irrelevant features using sparse least squares. Expert Syst Appl. (2022) 200:116928. doi: 10.1016/j.eswa.2022.116928
34. Lu ZQJ. The elements of statistical learning: data mining, inference, and prediction, 2nd edition. J R Stat Soc Ser A Stat Soc. (2010) 173:693–4. doi: 10.1111/j.1467-985X.2010.00646_6.x
35. Pearson K. LIII. On lines and planes of closest fit to systems of points in space. Lond Edinb Dublin Philos Mag J Sci. (1901) 2:559–72. doi: 10.1080/14786440109462720
36. Huang DS, Jiang FW, Li KP, Tong GS, Zhou GF. Scaled PCA: a new approach to dimension reduction. Manage Sci. (2022) 68:1678–95. doi: 10.1287/mnsc.2021.4020
37. Kukreja SL, Löfberg J, Brenner MJ. A least absolute shrinkage and selection operator (LASSO) for non-linear system identification. IFAC Proc Vol. (2006) 39:814–9. doi: 10.3182/20060329-3-AU-2901.00128
38. Tibshirani R. Regression shrinkage and selection via the lasso: a retrospective. J R Stat Soc B. (2011) 73:273–82. doi: 10.1111/j.1467-9868.2011.00771.x
39. Hoerl AE, Kennard RW. Ridge regression: biased estimation for non-orthogonal problems. Technometrics. (2000) 42:80–6. doi: 10.1080/00401706.2000.10485983
40. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. (2018) 2:223–8. doi: 10.1016/S2352-4642(18)30022-1
41. Spitzer RL, Kroenke K, Williams J, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
42. Kroenke K, Spitzer RL, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
43. Hyler SE, Rieder RO, Williams JBW, Spitzer RL, Hendler J, Lyons M. The personality diagnostic questionnaire: development and preliminary results. J Pers Disord. (1988) 2:229–37. doi: 10.1521/pedi.1988.2.3.229
44. Yang J, McCrae RR, Costa P, Yao S, Dai X, Cai T, et al. The cross-cultural generalizability of axis-II constructs: an evaluation of two personality disorder assessment instruments in the People's Republic of China. J Pers Disord. (2000) 14:249–63. doi: 10.1521/pedi.2000.14.3.249
45. Yang Y, Shen D, Wang J, Yang J. The reliability and validity of PDQ-4+ in China. Chin J Clin Psychol. (2002) 10:165–8. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD2002&filename=ZLCY200203002&uniplatform=NZKPT&v=xa0KUSkuqedV56XTWCuB0MblhzpD4qZHrfVkB4nxnUPgvYvoNhb_B1aoutpJWnJ3
46. Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. (2004) 26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
47. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. (1997) 36:340–8. doi: 10.1097/00004583-199703000-00012
48. Fu W, Yao S, Yu H, Zhao X. Initial reliability and validity of childhood trauma questionnaire (CTQ-SF) applied in Chinese college students. Chin J Clin Psychol. (2005) 13:40–2. doi: 10.16128/j.cnki.1005-3611.2005.01.012
49. Zhang JJ, Liu YD, Zhang H, Huang ZH, Wang F, Yang JJ, et al. Correlates of non-suicidal self-injury in adolescent psychiatric patients in China. Front Psychiatry. (2022) 13:864150. doi: 10.3389/fpsyt.2022.864150
50. Tsamardinos I, Brown LE, Aliferis CF. The max-min hill-climbing Bayesian network structure learning algorithm. Mach Learn. (2006) 65:31–78. doi: 10.1007/s10994-006-6889-7
51. Volinsky CT, Raftery AE. Bayesian information criterion for censored survival models. Biometrics. (2000) 56:256–62. doi: 10.1111/j.0006-341X.2000.00256.x
52. Wang HF, Wang DW, Yang SX. A memetic algorithm with adaptive hill climbing strategy for dynamic optimization problems. Soft Computing. (2009) 13:763–80. doi: 10.1007/s00500-008-0347-3
53. Posada D, Buckley TR. Model selection and model averaging in phylogenetics: advantages of akaike information criterion and Bayesian approaches over likelihood ratio tests. Syst Biol. (2004) 53:793–808. doi: 10.1080/10635150490522304
54. Chen YH, Chen R, Hou JD, Hou MZ, Xie XL. Research on users' participation mechanisms in virtual tourism communities by Bayesian network. Knowl Based Syst. (2021) 226:1–13. doi: 10.1016/j.knosys.2021.107161
55. Appasami G, Nickolas S. A deep learning-based COVID-19 classification from chest X-ray image: case study. Eur Phys J-Spec Top. (2022) 18:1–11. doi: 10.1140/epjs/s11734-022-00647-x
56. Chamberlin JH, Aquino G, Schoepf UJ, Nance S, Godoy F, Carson L, et al. An interpretable chest CT deep learning algorithm for quantification of COVID-19 lung disease and prediction of inpatient morbidity and mortality. Acad Radiol. (2022) 29:1178–88. doi: 10.1016/j.acra.2022.03.023
57. Gupta V, Jain N, Sachdeva J, Gupta M, Mohan S, Bajuri MY, et al. Improved COVID-19 detection with chest x-ray images using deep learning. Multimed Tools Appl. (2022) 81:37657–80. doi: 10.1007/s11042-022-13509-4
58. Chen Y, Li Y, Wu M, Lu F, Hou M, Yin Y. Differentiating Crohn's disease from intestinal tuberculosis using a fusion correlation neural network. Knowl Based Syst. (2022) 244:108570. doi: 10.1016/j.knosys.2022.108570
59. Organisciak D, Shum HPH, Nwoye E, Woo WL. RobIn: a robust interpretable deep network for schizophrenia diagnosis. Expert Syst Appl. (2022) 201:1–12. doi: 10.1016/j.eswa.2022.117158
60. Palaniyappan L, Deshpande G, Lanka P, Rangaprakash D, Iwabuchi S, Francis S, et al. Effective connectivity within a triple network brain system discriminates schizophrenia spectrum disorders from psychotic bipolar disorder at the single-subject level. Schizophr Res. (2019) 214:24–33. doi: 10.1016/j.schres.2018.01.006
61. Oh J, Oh BL, Lee KU, Chae JH, Yun K. Identifying schizophrenia using structural MRI with a deep learning algorithm. Front Psychiatry. (2020) 11:1–11. doi: 10.3389/fpsyt.2020.00016
62. Cortes C, Vapnik V. Support-vector networks. Mach Learn. (1995) 20:273–97. doi: 10.1007/BF00994018
63. Mirjalili S. Dragonfly algorithm: a new meta-heuristic optimization technique for solving single-objective, discrete, and multi-objective problems. Neural Comput Appl. (2015) 27:1053–73. doi: 10.1007/s00521-015-1920-1
64. Sayed GI, Tharwat A, Hassanien AE. Chaotic dragonfly algorithm: an improved metaheuristic algorithm for feature selection. Appl Intell. (2018) 49:188–205. doi: 10.1007/s10489-018-1261-8
65. Wilkinson PO, Qiu T, Neufeld S, Jones PB, Goodyer IM. Sporadic and recurrent non-suicidal self-injury before age 14 and incident onset of psychiatric disorders by 17 years: prospective cohort study. Br J Psychiatry. (2018) 212:1–5. doi: 10.1192/bjp.2017.45
66. Bresin K, Schoenleber M. Gender differences in the prevalence of non-suicidal self-injury: a meta-analysis. Clin Psychol Rev. (2015) 38:55–64. doi: 10.1016/j.cpr.2015.02.009
67. Marshall SK, Tilton-Weaver LC, Stattin H. Non-suicidal self-injury and depressive symptoms during middle adolescence: a longitudinal analysis. J Youth Adolesc. (2013) 42:1234–42. doi: 10.1007/s10964-013-9919-3
68. Barrocas AL, Giletta M, Hankin BL, Prinstein MJ, Abela JR. Non-suicidal self-injury in adolescence: longitudinal course, trajectories, and intrapersonal predictors. J Abnorm Child Psychol. (2015) 43:369–80. doi: 10.1007/s10802-014-9895-4
69. Liu ZZ, Tein JY, Jia CX, Liu X. Depression as a mediator between frequent nightmares and non-suicidal self-injury among adolescents: a 3-wave longitudinal model. Sleep Med. (2021) 77:29–34. doi: 10.1016/j.sleep.2020.11.015
70. Wu N, Hou Y, Chen P, You J. Peer acceptance and non-suicidal self-injury among Chinese adolescents: a longitudinal moderated mediation model. J Youth Adolesc. (2019) 48:1806–17. doi: 10.1007/s10964-019-01093-0
71. Chen H, Zhou J. Research progress on the addictive characteristics of non-suicidal self-injury. Chin J Psychiatry. (2022) 55:64–8. doi: 10.3760/cma.j.cn113661-20210921-00130
72. Jenkins AL, McCloskey MS, Kulper D, Berman ME, Coccaro EF. Self-harm behavior among individuals with intermittent explosive disorder and personality disorders. J Psychiatr Res. (2015) 60:125–31. doi: 10.1016/j.jpsychires.2014.08.013
73. Buelens T, Costantini G, Luyckx K, Claes L. Comorbidity between non-suicidal self-injury disorder and borderline personality disorder in adolescents: a graphical network approach. Front Psychiatry. (2020) 11:580922. doi: 10.3389/fpsyt.2020.580922
74. Zhang F, Cloutier PF, Yang H, Liu W, Cheng W, Xiao Z. Non-suicidal self-injury in Shanghai inner bound middle school students. Nephron Clin Pract. (2019) 32:206–13. doi: 10.1136/gpsych-2019-100083
75. Wang Y, Yuan Y, Zhang J. Negative emotion and self-injury in left-behind adolescents: moderating effect of family functioning and emotion expression. Chin J Clin Psychol. (2017) 25:75–81. doi: 10.16128/j.cnki.1005-3611.2017.01.017
76. Zhong Y, Yang Y, Zhang YHL. Childhood trauma experiences and their impact on non-suicidal self-injury in adolescents with first episode depressive disorder. Chin J Psychiatry. (2020) 53:520–6. doi: 10.3760/cma.j.cn113661-20200107-00004
77. Su J, Chen J, Wan Y, Zhong C, Hu X, Tao F, et al. Relations between childhood abuse and non-suicidal self-injury in middle school students. Chin J School Health. (2015) 36:1326–9. doi: 10.16835/j.cnki.1000-9817.2015.09.017
78. Moore SE, Scott JG, Ferrari AJ, Mills R, Dunne MP, Erskine HE, et al. Burden attributable to child maltreatment in Australia. Child Abuse Neglect. (2015) 48:208–20. doi: 10.1016/j.chiabu.2015.05.006
79. Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. (2010) 125:e778–86. doi: 10.1542/peds.2009-0597
Keywords: non-suicidal self-injury, mood disorders, artificial intelligence, support vector machine, adolescents
Citation: Yang J, Chen Y, Yao G, Wang Z, Fu X, Tian Y and Li Y (2022) Key factors selection on adolescents with non-suicidal self-injury: A support vector machine based approach. Front. Public Health 10:1049069. doi: 10.3389/fpubh.2022.1049069
Received: 20 September 2022; Accepted: 24 October 2022;
Published: 10 November 2022.
Edited by:
Hanliang Fu, Xi'an University of Architecture and Technology, ChinaReviewed by:
Jin Wen, Northwest Normal University, ChinaCopyright © 2022 Yang, Chen, Yao, Wang, Fu, Tian and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yamin Li, YW1pbm55QGNzdS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.