- 1School of Psychology, Nanjing Normal University, Nanjing, China
- 2Faculty of Psychology, Beijing Normal University, Beijing, China
- 3Beijing Key Laboratory of Applied Experimental Psychology, National Demonstration Center for Experimental Psychology Education, Beijing, China
- 4Faculty of Arts, Shenzhen University, Shenzhen, China
Object: Repeated quarantine policies over the past 3 years have led to poor psychological consequences for the public. Previous studies have proved that the quarantine policy leaves individuals vulnerable to anxiety, depression, and insomnia, especially among college students. This study aims to explore whether psychological problems during isolation continue with the release of isolation.
Methods: Overall, 2,787 college students both answered a web-based survey during and after the closure management was lifted. The Patient Health Questionnaire, Generalized Anxiety Disorder Scale, and Youth Self-rating Insomnia Scale were measured. The cross-lagged path model was used to explore the influence of psychological impact during isolation on the individual after the release.
Results: We found that anxiety and sleep disturbance levels alleviated significantly after quarantine, except for depression. As expected, a bidirectional relationship exists between anxiety, depression, and sleep disturbance. Moreover, depression and sleep disturbance can predict post quarantine depression, sleep disturbance, and anxiety, yet anxiety cannot predict sleep disturbance afterward.
Conclusion: Timely and effective intervention for anxiety, depression, and insomnia during isolation is essential for individuals to repair themselves quickly after the release.
Introduction
At the end of 2019, Coronavirus disease was reported in China. COVID-19 spread quickly throughout the world to its highly contagious property, and the World Health Organization (WHO) declared it a global pandemic (1). Containment measures, including social distance, quarantine, or even city lockdown, are effective in disease containment, whereas stringent measures have introduced a greater risk of mental illness to the public (2). Evidence shows that the prevalence of mental illness during the pandemic was higher than in pre-pandemic (2–4). For college students, the impact of the pandemic on mental and physical health was worse (3, 5). Among mental health problems, depression and anxiety are the most prevalent in college students (6), negatively affecting mental health and daily performance (7). Meanwhile, data from several studies also suggest that sleep disturbance is prevalent in college students, impairing daytime function (5, 8). Previous research has established that anxiety, depression, and sleep disturbance are intertwined (8, 9). However, due to different measurements, no longitudinal studies, whether the relationship between anxiety, depression, and sleep disturbance alters with time is not yet clear (3, 10), as if the interpretation of this relationship will benefit the prevention and intervention of anxiety, depression, and sleep disturbance after the pandemic. Given this, our study aims to reveal the relationship between anxiety, depression, and sleep disturbance.
In terms of the relationship between anxiety and depression, previous studies established that depression and anxiety are two quotidian comorbidities (8, 11, 12). However, a much-debated question is whether the longitudinal relationship between anxiety and depression is bidirectional. Several studies demonstrate that anxiety precedes the advent of depression (12–14). Different from these studies, other studies suggest that depression precedes the advent of anxiety (15, 16). Apart from the statement that the relationship between anxiety and depression is unidirectional, a meta-analysis focusing on longitudinal studies demonstrates that the relationship between anxiety and depression is bidirectional (11). However, with a sample from western countries, we cannot establish a bidirectional relationship between anxiety and depression in Chinese samples (11). Considering the controversy of the relationship between anxiety and depression, further research about this will be needed, and we put forward the following hypothesis:
Hypothesis 1. There would be a bidirectional relationship between anxiety and depression during the pandemic.
There are mainly three different viewpoints regarding the relationship between depression, anxiety, and sleep disturbance. According to cognitive models, the first viewpoint is that depression and anxiety are predictors of sleep disturbance, for fear, worry, and anxiety can cause insomnia (17). However, Buysse et al. (18) asserted that sleep disturbance is the prefigure of depression through a longitudinal cohort study. Furthermore, several review articles show that sleep disturbance is a risk factor for both anxiety and depression (7, 19, 20). Inspired by two unidirectional viewpoints, recent evidence suggests that the relationship between depression, anxiety, and sleep disturbance is bidirectional instead. On the one hand, depression and anxiety will lead to sleep disturbance. And conversely, suffering from sleep disturbance will result in the occurrence or development of anxiety and depression. Cui et al. (3) has done a cross-sectional survey in China, suggesting that the relationship between anxiety, depression, and sleep disturbance is bidirectional. The result of this study is consistent with several other studies (21–23). However, to our knowledge, many studies that suggest bidirectional relationships are cross-sectional or meta-analysis studies. Little longitudinal studies determine the directionality and causality between anxiety, depression, and sleep disturbance (3, 8). Although debate continues, given the situation that the last viewpoint is the combination of the first two ideas, we pose the following hypothesis:
Hypothesis 2. There would be a bidirectional relationship between sleep disturbance and depression.
Hypothesis 3. There would be a bidirectional relationship between sleep disturbance and anxiety.
In addition, previous research established that gender may influence the relationship between anxiety, depression, and sleep disturbance. First of all, as for the prevalence of anxiety, depression, and sleep disturbance, evidence shows that there is a discrepancy between males and females. Using meta-analysis, a study collected and analyzed 98 previous studies, suggesting that female students had a higher prevalence of depression and anxiety than male students (2). In terms of the prevalence of sleep disturbance, large-scale research showed that females had higher total Pittsburgh Sleep Quality Index (PSQI) scores than males, indicating that females had more sleep problems (8). Consistent with this result, other studies demonstrated that females were prone to symptoms of anxiety, depression (24, 25), and sleep disturbance (26, 27). Conversely, some studies suggest that the incidence of anxiety, depression, and sleep disturbance is higher in males than females (28), even not significant (29). However, as for the question of whether gender affects the relationship between anxiety, depression, and sleep disturbance, few studies have investigated it (30, 31), and further study is worthy. Considering the controversy and paucity of this area, we put up the following hypothesis:
Hypothesis 4. There would be a gender difference in the relationship between anxiety, depression, and sleep disturbance.
The current longitudinal study collected data from Chinese college students, conducting cross-lagged analysis to examine the relationship between anxiety, depression, and sleep disturbance. Additionally, this study examined the gender difference in the relationship between anxiety, depression, and sleep disturbance through multiple-group analysis. The results of this study will provide further evidence of the relationship between anxiety, depression, and sleep disturbance. Moreover, given that COVID-19 worsens people's mental and physical health, the results of this study will also provide information on the prevention and intervention of anxiety, depression, and sleep disturbance.
Methods
Participants
The first wave of data was obtained from 6,710 college students during the COVID-19 pandemic lockdown in Harbin on September 26, 2021. The second wave of data was collected from 3,731 college students from the same school after the closure management was lifted on December 27, 2021. When the datasets from two waves were combined according to the students' school numbers, 2,787 participants (58.6% females, Meanage = 18.34, SDage = 0.92, range from 15 to 28) were finally recruited. Students and their parents had to provide signed informed consent before participating in the assessment. All participants answered the questionnaires through the Wenjuanxing online questionnaire platform (https://www.wjx.cn/). The research was examined and approved by the ethical committee of Beijing Normal University (Reference number: 202112220084).
Measures
Patient health questionnaire (PHQ-9)
The Patient Health Questionnaire (PHQ-9) is a widely used scale for screening depression symptoms (32). Participants were asked about the frequency [not at all (0), several days (1), more than half of the days (2), nearly every day (3)] of experiencing given symptoms in the last 2 weeks, and higher scores indicate more severe depression symptoms. The Chinese version of PHQ-9 was proved valid and reliable (33). In the current study, PHQ-9 has a high internal consistency with Cronbach α values of 0.89 and 0.92 in wave 1 and wave 2, respectively.
Generalized anxiety disorder scale (GAD-7)
The Generalized Anxiety Disorder Scale (GAD-2) is a valid and reliable assessment to screen for generalized anxiety symptoms (34). Participants answered seven questions about the frequency of anxiety symptoms that occurred over the last 2 weeks. Each item scored from 0 (not at all) to 3 (nearly every day), with a higher score indicating more severe anxiety symptoms. The Chinese version also has good psychometric properties for identifying anxiety (35). In the current study, GAD-7 has a high internal consistency with Cronbach α values of 0.93 and 0.95 in wave 1 and wave 2, respectively.
Youth self-rating insomnia scale (YSIS-8)
The Youth Self-rating Insomnia Scale (YSIS-8) is a 5-point Likert questionnaire assessing sleep disturbance in the last month. Participants answered two questions about overall sleep quality and six about the frequency of specific sleep disturbance symptoms. Total scores range from 3 to 15, and higher scores indicate poorer sleep quality. Previous studies have shown that YSIS-8 in Chinese is valid and reliable (36). In the current study, YSIS-8 has a high internal consistency with Cronbach α values of 0.91 and 0.93 in wave 1 and wave 2, respectively.
Data analyses
Preliminary analyses were conducted in SPSS 22.0. The cross-lagged paths and multiple-group analysis were performed via Mplus 8.3. Because depression and anxiety symptoms in adolescents and young adults change over time (37), age was included as a covariate in the model. It should be mentioned that all variables were assumed to be related to all others; therefore, this model had zero degrees of freedom, and it did not make sense to assess model fit (38) except for multiple-group analysis.
Results
Preliminary analyses
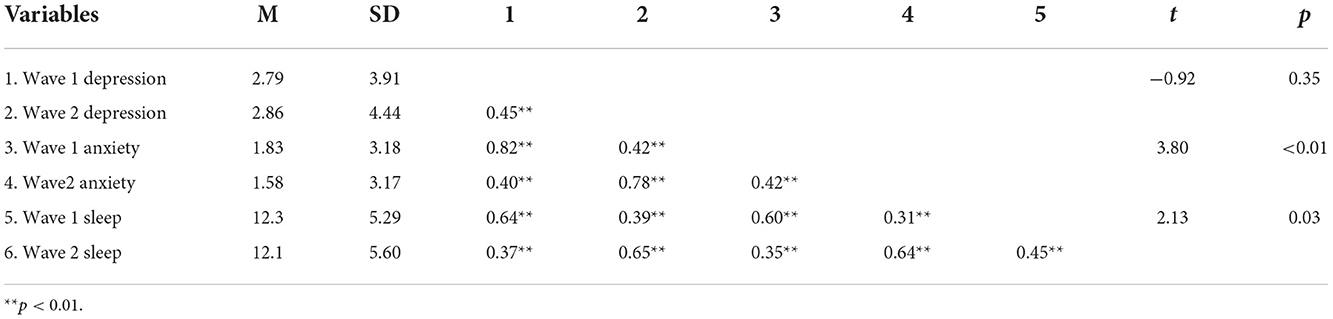
Means, standard deviations, correlations, and t-test results of major variables are shown in Table 1. The results demonstrated that anxiety, depression, and sleep disturbances were significantly and positively related to each other at each wave. Additionally, after 3 months when the lockdown ended, there was no significant change in the level of depression. At the same time, the level of anxiety and sleep disturbances have decreased significantly.
The cross-lagged path model
The cross-lagged regression model was performed to analyze the causal link between anxiety, depression, and sleep disturbances while controlling by age. As shown in Figure 1, all three constructs demonstrated strong stability over 3 months, with autoregression path coefficients ranging from 0.25 to 0.35. Moreover, after controlling the autoregression of anxiety, depression, and sleep disturbances, as well as the correlation of three constructs at the same wave, depression at wave 1 could significantly predict anxiety (β = 0.16, p < 0.001) and sleep disturbances (β = 0.10, p < 0.001) at wave 2. Anxiety at wave 1 could significantly predict depression (β = 0.12, p < 0.001) at wave 2. Sleep disturbances could significantly predict depression (β = 0.15, p < 0.001) and anxiety (β = 0.06, p < 0.01) at wave 2. However, anxiety at wave 1 could not significantly predict sleep disturbances (β = 0.05, p = 0.08). These results indicated that the relationship between anxiety and depression, sleep disturbances, and depression is bidirectional, while the relationship between anxiety and sleep disturbances is unidirectional.
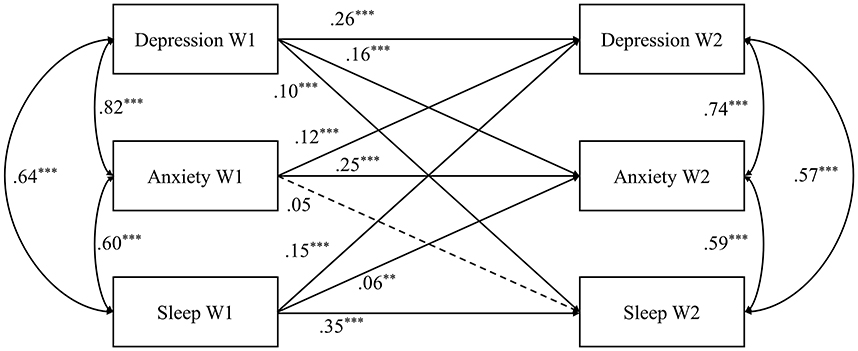
Figure 1. The standardized cross-lagged model between depression, anxiety, and sleep disturbances. The residuals were not shown; **p < 0.01, ***p < 0.001.
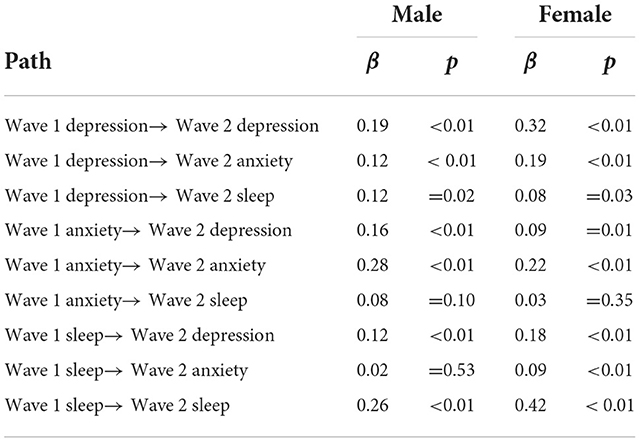
A multi-group analysis grouped by gender was conducted to examine gender differences in the cross-lagged model. We constructed a structural weights equivalent model, supposing that regression coefficients were equal between genders. Fitting results were excellent referencing to Hu and Bentler's criteria (39): χ2 = 15.99, df = 9, CFI = 0.99, TLI = 0.99, RMSEA = 0.02 (90% CI = [0.00, 0.04]). We compared the structural weights equivalent model to the unconstrained model to test whether there is a gender difference. The results showed that Δχ2 = 15.99, Δdf = 9, p > 0.05) indicated no significant gender difference in the cross-lagged model of depression, anxiety, and sleep disturbances among Chinese college students (see Table 2).
Discussion
Studies on sleep disturbance, depression, and anxiety have lasted for over 40 years (40). However, with the foreground of the pandemic of COVID-19, depression, anxiety, and sleep disturbance have become more prevalent, especially among college students. Lack of longitudinal studies, our results portrayed several findings as follows. Some points are worth discussing.
Inconsistent with the result of Wang et al. (41), which indicated that anxiety levels of high school students in Wuhan raised with the new semester after being quarantined for several months in the first wave of the pandemic. Our result provides sequential proof that after home quarantine, anxiety alleviated significantly in the situation that the pandemic has already lasted for over 1 year. Our results also may support the hypothesis that increased physical activities can mitigate the anxiety level of college students (42), for the anxiety level is reduced after quarantine which means more space and opportunities for physical activities can buffer anxiety. Even if no previous studies revealed the fluctuation of sleep disturbance, after quarantine, sleep quality also resurrects to some degree. Combined with previous studies, besides physical activities, augmentation, improvement, or a stable diet may contribute to sleep disturbance resurrection (43).
In contrast, as if levels of depression seemed to increase with time, the comparison is not significant on a statistical level. To deduce why college students did not get rid of the shackle of depression after home quarantine, clues from Xiang et al. (42) implied that only when physical activities reach a moderate level can depression be mitigated. Therefore, in the situation that college students did not do enough physical activities, depression was not meliorated at an effective level.
Referring to associations between anxiety, depression, and sleep disturbance, only could anxiety just predict depression and anxiety afterward, while depression and sleep disturbance can simultaneously predict anxiety, sleep disturbance, and depression. However, previous studies portrayed a bidirectional relationship between anxiety and sleep disturbance, which indicated that anxiety and sleep disturbance could predict mutually (44, 45). However, from our results, the situation varies with the foreground of COVID-19, a pandemic. Tao et al. (46) researched symptoms of sleep disturbance, anxiety, and depression, a change in sleep disturbance can change the anxiety and depression structure. Hence, it is proper to speculate that before anxiety is alleviated after quarantine, sleep quality improves in advance. Therefore, from this point of view, anxiety cannot predict sleep disturbance.
Besides disease association, though no studies contain a comparison between pre-pandemic, during the pandemic, and post-pandemic, we can draw some clues from previous studies to raise surmises and supply information to patch a holistic view. From the perspective of cross-sectional data, correlations exist between anxiety, depression, and sleep disturbance which is coherent with the results of Becker et al. (8). From data of wave 1 and wave 2, there is a significant bidirectional relationship between anxiety, depression, and sleep disturbance. When we make the comparison between wave 1 and wave 2, the relationship between anxiety, depression, and sleep disturbance becomes less close. Though no studies were done during the pandemic and post the pandemic, research done by Deng et al. (2) showed that levels of anxiety, depression, and sleep disturbance reached the peak level during the pandemic. Our results provide information from another facet after quarantine, the relationship between anxiety, depression, and sleep disturbance becomes sparser. In the domain of hopelessness, a factor related to anxiety and depression, Tao et al. (47) drew the same trend in college students, which implied that after quarantine, hopelessness was reduced. Combining previous studies' results, we estimate that less time spent on mobile phones and more physical activities can reduce anxiety, depression, and sleep disturbance and further dilute the bidirectional relationship (42, 48).
Limitation
First, as discussed above, the severity of depression, anxiety, and sleep disturbance can be affected by many externals, such as school schedule and containment measurement. Some other information, such as time of sleep and frequency of physical activities can be confounding factors influencing degrees of anxiety, depression, and sleep disturbance. Second, anxiety, depression, and sleep disturbance can alter with quarantine duration and time after quarantine duration. Hence, in future studies, more time points, time duration, and other pandemic containment measures can be pinned for investigation.
Conclusion
In our current study, three main findings were (1) levels of anxiety and sleep disturbance alleviated significantly after quarantine except for depression; (2) a bidirectional relationship exists between anxiety, depression, and sleep disturbance; (3) depression and sleep disturbance can predict post quarantine depression, sleep disturbance and anxiety, yet anxiety cannot predict sleep disturbance afterward. Our current study clearly shows that quarantine adds great pressure and stress on college students while, after quarantine, college students' mental status resumes great resilience.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Beijing Normal University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
CS took the lead in writing the manuscript. YL conceived the study design and supervised the data collection. SW performed the data analysis. QT, XL, and YL provided critical feedback and helped shape the research, analysis, and manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. Rolling updates on coronavirus disease (COVID-19). (2022). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
2. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. (2021) 301:113863. doi: 10.1016/j.psychres.2021.113863
3. Cui X, He Y, Gong J, Luo X, Liu J. Epidemiology of sleep disturbances and their effect on psychological distress during the COVID-19 outbreak: a large national study in China. Front Psychol. (2021) 12:615867. doi: 10.3389/fpsyg.2021.615867
4. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. (2020) 3:e2019686–e2019686. doi: 10.1001/jamanetworkopen.2020.19686
5. Okun M, Walden A, Feliciano L. 706 sleep and mental health in college students before and during the initial COVID-19 shutdown. Sleep. (2021) 44(Supplement_2):A275–6. doi: 10.1093/sleep/zsab072.704
6. Chang J, Ji Y, Li Y, Pan H, Su P. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: a meta-analysis. J Affect Disord. (2021) 292:242–54. doi: 10.1016/j.jad.2021.05.109
7. Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. (2019) 43:96–105. doi: 10.1016/j.smrv.2018.10.006
8. Becker SP, Jarrett MA, Luebbe AM, Garner AA, Burns GL, Kofler MJ. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health. (2018) 4:174–81. doi: 10.1016/j.sleh.2018.01.001
9. Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
10. Frances A, Manning D, Marin D, Kocsis J, Mckinney K, Hall W, et al. Relationship of anxiety and depression. Psychopharmacologia. (1992) 106:S82–6. doi: 10.1007/BF02246243
11. Jacobson NC, Newman MG. Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychol Bull. (2017) 143:1155–200. doi: 10.1037/bul0000111
12. Ned H, Kalin MD. The Critical Relationship Between Anxiety and depression. Am J Psych. (2020) 177:365–7. doi: 10.1176/appi.ajp.2020.20030305
13. Jacobson NC, Newman MG. Avoidance mediates the relationship between anxiety and depression over a decade later. J Anxiety Disord. (2014) 28:437–45. doi: 10.1016/j.janxdis.2014.03.007
14. Belzer K, Schneier FR. Comorbidity of anxiety and depressive disorders: issues in conceptualization, assessment, and treatment. J Psych Pract. (2004) 10:296–306. doi: 10.1097/00131746-200409000-00003
15. Fichter MM, Quadflieg N, Fischer UC, Kohlboeck G. Twenty-five-year course and outcome in anxiety and depression in the upper Bavarian longitudinal community study. Acta Psychiatr Scand. (2010) 122:75–85. doi: 10.1111/j.1600-0447.2009.01512.x
16. Goodwin RD. Anxiety disorders and the onset of depression among adults in the community. Psychol Med. (2002) 32:1121–4. doi: 10.1017/S0033291702005482
17. Harvey AG, A. cognitive model of insomnia. Behav Res Ther. (2002) 40:869–93. doi: 10.1016/S0005-7967(01)00061-4
18. Buysse DJ, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. (2008) 31:473–80. doi: 10.1093/sleep/31.4.473
19. Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. (2003) 160:1147–56. doi: 10.1176/appi.ajp.160.6.1147
20. Riemann D. Primary insomnia: a risk factor to develop depression? J Affect Disord. (2003) 76:255–9. doi: 10.1016/s0165-0327(02)00072-1
21. Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. (2019) 23:2324–32. doi: 10.1111/jcmm.14170
22. Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. (2022) 10:473–81. doi: 10.31887/DCNS.2008.10.4/plfranzen
23. Jansson-Frojmark M, Lindblom K, A. bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. (2008) 64:443–9. doi: 10.1016/j.jpsychores.2007.10.016
24. Gonzalez-Sanguino C, Ausin B, Castellanos MA, Saiz J, Lopez-Gomez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. (2020) 87:172–6. doi: 10.1016/j.bbi.2020.05.040
25. Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, et al. A nationwide survey of psychological distress among italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. (2020) 17:3165. doi: 10.3390/ijerph17093165
26. Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. (2020) 11:306. doi: 10.3389/fpsyt.2020.00306
27. Suh S, Cho N, Zhang J. Sex Differences in insomnia: from epidemiology and etiology to intervention. Curr Psychiatry Rep. (2018) 20:69. doi: 10.1007/s11920-018-0940-9
28. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
29. Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr. (2020) 51:102092. doi: 10.1016/j.ajp.2020.102092
30. Goldstein-Piekarski AN, Greer SM, Saletin JM, Harvey AG, Williams LM, Walker MP. Sex, sleep deprivation, and the anxious brain. J Cogn Neurosci. (2018) 30:565–78. doi: 10.1162/jocn_a_01225
31. Matud MP, Garcia MC. Psychological distress and social functioning in elderly spanish people: a gender analysis. Int J Environ Res Public Health. (2019) 16:341. doi: 10.3390/ijerph16030341
32. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
33. Zhang YL, Liang W, Chen ZM, Zhang HM, Zhang JH, Weng XQ, et al. Validity and reliability of patient health questionnaire-9 and patient health questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. (2013) 5:268–75. doi: 10.1111/appy.12103
34. Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
35. Luo Z, Li Y, Hou Y, Zhang H, Liu X, Qian X, et al. Adaptation of the two-item generalized anxiety disorder scale (GAD-2) to Chinese rural population: a validation study and meta-analysis. Gen Hosp Psychiatry. (2019) 60:50–6. doi: 10.1016/j.genhosppsych.2019.07.008
36. Liu X, Yang Y, Liu Z, Luo Y, Fan F, Jia C. Psychometric properties of youth self-rating insomnia scale (YSIS) in Chinese adolescents. Sleep Biol Rhythms. (2019) 17:339–48. doi: 10.1007/s41105-019-00222-3
37. Axelson DA, Birmaher B. Relation between anxiety and depressive disorders in childhood and adolescence. Depress Anxiety. (2001) 14:67–78. doi: 10.1002/da.1048
38. Schönberger M, Ponsford J, Gould KR, Johnston L. the temporal relationship between depression, anxiety, and functional status after traumatic brain injury: a cross-lagged analysis. J Int Neuropsychol Soc. (2011) 17:781–7. doi: 10.1017/S1355617711000701
39. Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling. Multidisc J. (1999) 6:1–55. doi: 10.1080/10705519909540118
40. Boehm MA, Lei QM, Lloyd RM, Prichard JR. Depression, anxiety, and tobacco use: overlapping impediments to sleep in a national sample of college students. J Am Coll Health. (2016) 64:565–74. doi: 10.1080/07448481.2016.1205073
41. Wang C, Zhao H, Zhang H. Chinese college students have higher anxiety in new semester of online learning during COVID-19: a machine learning approach. Front Psychol. (2020) 11:7413. doi: 10.3389/fpsyg.2020.587413
42. Xiang M, Tan X, Sun J, Yang H, Zhao X, Liu L, et al. Relationship of physical activity with anxiety and depression symptoms in chinese college students during the COVID-19 outbreak. Front Psychol. (2020) 11:2436. doi: 10.3389/fpsyg.2020.582436
43. Rotvold A, Parker K, Honrath K, Rhee Y. Sleep and diet patterns of college students during the COVID-19 pandemic lockdowns. J Am College Health. (2022) 3:1–4. doi: 10.1080/07448481.2022.2089850
44. Cox RC, Olatunji BO. A systematic review of sleep disturbance in anxiety and related disorders. J Anxiety Disord. (2016) 37:104–29. doi: 10.1016/j.janxdis.2015.12.001
45. O'Kearney R, Pech M. General and sleep-specific worry in insomnia. Sleep Biol Rhythms. (2014) 12:212–5. doi: 10.1111/sbr.12054
46. Tao Y, Hou W, Niu H, Ma Z, Zhang S, Zhang L, et al. Centrality and bridge symptoms of anxiety, depression, and sleep disturbance among college students during the COVID-19 pandemic—a network analysis. Curr Psychol. (2022). doi: 10.1007/s12144-022-03443-x
47. Tao Y, Niu H, Hou W, Zhang L, Ying R. Hopelessness during and after the COVID-19 pandemic lockdown among Chinese college students: A longitudinal network analysis. J Clin Psychol. (2022) 1–14. doi: 10.1002/jclp.23439
Keywords: anxiety, depression, sleep disturbance, cross-lagged panel model, college students
Citation: Shi C, Wang S, Tang Q, Liu X and Li Y (2022) Cross-lagged relationship between anxiety, depression, and sleep disturbance among college students during and after collective isolation. Front. Public Health 10:1038862. doi: 10.3389/fpubh.2022.1038862
Received: 07 September 2022; Accepted: 14 November 2022;
Published: 06 December 2022.
Edited by:
Wulf Rössler, Charité Universitätsmedizin Berlin, GermanyCopyright © 2022 Shi, Wang, Tang, Liu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Li, bGVlQHN6dS5lZHUuY24=
 Congying Shi
Congying Shi Shujian Wang
Shujian Wang Qihui Tang
Qihui Tang Xiangping Liu2,3
Xiangping Liu2,3 Yue Li
Yue Li