
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 24 November 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1036929
This article is part of the Research Topic Refractive Errors: Public Health Challenges and Interventions View all 29 articles
 Nan Jiang1†
Nan Jiang1† Jiayue Chen2*†
Jiayue Chen2*† He Cao1†
He Cao1† Yongyi Liu3
Yongyi Liu3 Yuxin Zhang1
Yuxin Zhang1 Quqin Wang1
Quqin Wang1 Ting Wang1
Ting Wang1 Huilan Zhao2
Huilan Zhao2 Hui Lu2
Hui Lu2 Lei Yang2
Lei Yang2 Jiwei Wang1*
Jiwei Wang1*Objective: This study aimed to develop an integrated model based on the health belief model (HBM) and the theory of planned behavior (TPB) to explore the influencing factors of parents' intentions toward preschool children's myopia preventive behaviors.
Methods: This cross-sectional study was conducted in Minhang District, Shanghai, China in January 2022. One thousand six hundred and twenty-eight parents of preschool children from seven preschools were recruited in the study. A four-part questionnaire was used to collect data on socio-demographic characteristics, HBM variables, TPB variables and parental intentions. This study used exploratory factor analysis to analyze HBM and TPB items. Hierarchical multiple regression analysis was performed to explore the relationship between independent variables and parents' intentions toward preschool children's myopia preventive behaviors.
Results: The final integrative model showed that perceived severity, perceived barriers, attitudes, subjective norms, and perceived behavioral control were associated with parents' intentions toward preschool children's myopia preventive behaviors. In model 1, Child's age was entered as a control variable and explained 0.6% of the variance (F = 7.241, p = 0.007). When the HBM variables were entered in model 2, the proportion of variance increased to 25.4% (F = 73.290, P < 0.001). In model 3, TPB variables were entered and explained 63.2% of the variance (F = 246.076, p < 0.001).
Conclusion: The integrated model of HBM and TPB constructed in this study significantly improved the degree of explanation of parents' intentions toward preschool children's myopia preventive behaviors. Parents' perceived severity, perceived barriers, attitudes, subjective norms, and perceived behavioral control can be prioritized intervention targets for myopia preventive practices in preschool children.
Myopia is a growing public health concern, especially in Asian countries due to its high prevalence (1). A recent study showed that the prevalence of myopia in 4-year-old, 5-year-old, and 6-year-old children in China was 5.7, 5.8, and 7.1%, respectively (2), higher than the finding from Australia (1.4%) (3) and Kosovo (3.4%) (4). Most importantly, previous studies have shown that the earlier the onset of myopia, the more likely it is to progress into more severe myopia and even lead to irreversible loss of vision (5, 6). For example, the increased risk of myopic complications such as myopic macular degeneration, retinal detachment, cataract, and open angle glaucoma, have become the leading cause of untreatable visual loss in East Asian countries (7, 8).
Although the cure for myopia has not yet been established, the risk of myopia progression is manageable. There is empirical evidence that both genetic and environmental factors contribute to the development of myopia (9, 10). As modifiable environmental risk factors, myopia preventive behaviors are receiving increasing attention. Myopia preventive behaviors were divided into two categories. The first is the risk behaviors for myopia, such as prolonged screen exposure, prolonged reading and writing, and prolonged near work (10). The second category is protective behaviors for myopia, such as plenty time for outdoor activities (11). Restricting individual risk behaviors and promoting protective behaviors will help prevent the development of myopia (1, 12). It has been well-documented that the period from birth to 3–5 years of age is critical for visual development (13, 14). However, because preschool children have poor self-control, they always tend to follow their parents' arrangements (15, 16). Thus, near work, screen and outdoors time among preschool children are significantly influenced by parental attitudes and intentions (16).
Complicated psychosocial factors influence parents' intentions toward preschool children's myopia preventive behaviors, such as self-efficacy, response efficacy, and susceptibility (17). Therefore, a single theoretical model has limitations in explaining behavioral intentions (18). Under this circumstance, many researchers begin to explore the possibilities of combining various theories to construct a more comprehensive theoretical system to explain behavior or behavioral intentions. For example, one study constructed an integrated model of the theory of planned behavior (TPB) and self-determination theory to explain myopia-preventive behaviors (19). In addition, some researchers have proposed the comprehensive application of TPB and health belief model (HBM) interpretation of parents' intentions to vaccinate their children (20).
TPB is one of the most widely used social cognitive models that attempts to predict behavioral intentions and health behaviors (21, 22), which is an extension of the theory of reasoned action (23). Specifically, TPB posits that intention is the immediate predictor of behavior, which is determined by attitude, subjective norm, and perceived behavioral control. This theory states that when individuals perceive a behavior as positive (attitude), know that important people want them to perform the behavior (subjective norms), and perceive that the behavior is under their own volitional control (perceived behavioral control), then the individual will perform the behavior (24). The TPB has been applied to many health behaviors including myopia preventive behavior and parents' intentions to vaccinate their children (19, 25).
The HBM is a theoretical guideline and general conceptual framework for health behaviors (26). HBM focuses on changes in health beliefs, which lead to changes in health behaviors (27). According to the HBM, individuals' involvement in health-related behaviors can be explained by perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and cues to action. The theory postulates that individuals are more likely to adopt healthy behaviors when they perceived risks and believe these behaviors can promote their health (28). HBM has been widely used in various health behaviors, including myopia preventive behavior intentions (29, 30).
HBM and TPB are two of the most common and accepted theories in the field of health behavior. Both of them are based on the expectancy value theory, but offer different perspectives on behavioral decision-making (28, 31). However, a number of studies have identified that existing single theories may have some shortcomings that potentially reduce their predictive power (19, 32). For example, TPB is considered not to identify the more global cognitive variables related to its constituent variables and the model does not account how general motivation serves as a source of information to guide social cognitive processes (32). One of the limitations of HBM is that it ignores the influence of external pressures such as subjective norms on one's acceptance of a healthy behavior (33). Therefore, the combination of the two models not only helps to improve the limitations of existing theories on health behavior and helps to explain health behaviors to a greater degree, but also provides more recommendations for healthy behavior management. For myopia preventive behaviors, applying an integrative model to design a health education program should not only take into account parents' confidence in helping children adopt healthy behaviors, the behaviors and expectations of their friends and family, but also consider that parents' low awareness and beliefs may also influence their decisions. The combination of HBM and TPB has many applications in explaining parents' intentions to vaccinate their children and parental beliefs related to children's behavioral problems (20, 34). However, there is still a lack of exploration of the combination of two theories in explaining parents' intentions toward preschool children's myopia preventive behaviors. Therefore, based on the integrated model of HBM and TPB, this study explores the influencing factors of parents' intentions toward preschool children's myopia preventive behaviors, with the goal of exploring effective intervention measures to improve myopia preventive behavior and reduce the occurrence of myopia in preschool children in China.
This cross-sectional study recruited parents of preschool children from seven preschools in Minhang District, Shanghai in January 2022. According to the calculation method of the sample size of the cross-sectional study, the average score of behavioral intention is 3.47, and the standard deviation is 0.94 (35). The significance level is 0.05 and allowable error was taken as 0.015 mean score, the sample size was required to be at least 1,253. With a possible invalid rate of 20%, no fewer than 1,566 participants should be recruited. There are 189 preschools in Minhang District with about 71,000 students. This study adopted the method of cluster sampling and recruitment invitations were sent to 189 preschools. Seven preschools were recruited on a first-come, first-served basis. Finally, a total of 1,628 parents of preschool children from seven preschools were included. The inclusion criteria for this study including (1) parents are guardians of children; (2) parents of children aged 3–6; (3) be able to complete the questionnaire independently. Exclusion criteria include (1) parents who have participated in other myopia intervention programs in the past 12 months; (2) parents of children with severe eye or head trauma. Parents of each preschooler were invited to complete an online questionnaire, the content of the questionnaire and the purpose of the study were explained to all parents prior to the start of the survey. Before participating in this study, all participants had only received the simplest school-based education on myopia knowledge required by the government, and had not received special training in myopia intervention. Informed consent was obtained from the parents.
In order to ensure the quality of the questionnaires filled in by parents, we set up two quality control questions. A questionnaire was considered valid only if all two quality control questions were answered correctly. In addition, the questionnaire was set to be submitted only after all questions have been answered, and each account could only submit the questionnaire once. In the end, a total of 1,537 questionnaires were collected, with a response rate of 94.41%, of which 1,300 were valid questionnaires, with a valid rate of 84.58%. The study was approved by the Medical Research Ethics Committee of the School of Public Health, Fudan University (The international registry nos. IRB00002408 and FWA00002399).
The questionnaires used in this study were developed by the research team after referencing to the questionnaire framework in the relevant literature. We mainly made some modifications to the behavioral content in the questionnaire to make it more in line with our research purposes, the question frames in different dimensions were retained, and none of the existing items were used. The 24 items of the HBM variables referred to two studies on parental intentions of children (20, 36). For example, perceived benefits and perceived barriers were measured using items like “It is good for my child to [target behavior],” “It is difficult for me keep my child [target behavior].” The content of the questionnaire for TPB variables was mainly based on a study about parents' decisions for limiting their young child's screen time (37). For example, items like “Most people who are important to me think that I should ensure that [target behavior]” were used to measure subjective norms. All items in the HBM and TPB models use a 5-point Likert scale and response scale from 1 “strongly disagree” to 5 “strongly agree.” Each dimension is expressed using the mean score, calculated by adding up the score for each item under each dimension and dividing by the corresponding number of items.
Data regarding child gender, child's age, preterm birth, single child, father's age, mother's age, father's educational level, mother's educational level, annual household income, father myopia and mother myopia were obtained from each participant.
The HBM variables include (Table 1): perceived susceptibility (2 items), perceived severity (6 items), perceived benefits (6 items), perceived barriers (5 items), and cues to action (5 items). For our study, Cronbach's alpha was 0.83, indicating acceptable internal consistency reliability.
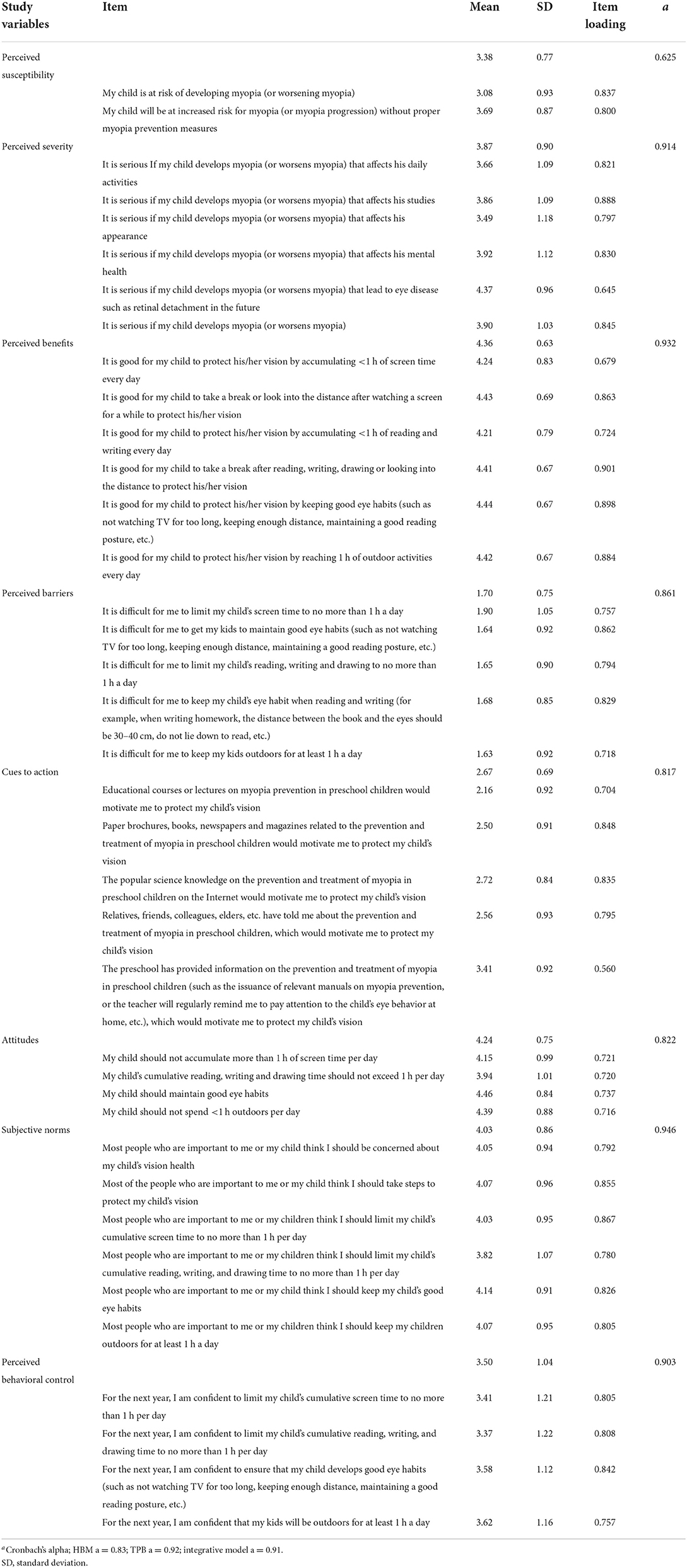
Table 1. Exploratory factor analysis, descriptive analysis and reliability of the HBM and TPB variables.
The TPB variables include (Table 1): attitude (4 items), subjective norms (6 items), perceived behavioral control (4 items). For our study, Cronbach's alpha was 0.92, implying good internal consistency reliability.
Parents' intentions toward preschool children's myopia preventive behavior were measured by 4 items, including: “I intend to take measures to protect my child's vision in the next 12 months,” “I intend to limit my child's screen time to no more than 1 a day in the next 12 months,” “I intend to limit the time my child spends reading, writing, and drawing to no more than 1 h a day in the next 12 months,” “I intend to keep my child's outdoor time at least 1 h a day in the next 12 months.” Questions were scored on a 5-point rating scale ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores reflected higher levels of parents' intentions.
Numbers and percentages were used to describe qualitative variables, while quantitative variables were presented as mean and standard deviation. Cronbach's alpha was calculated to test the internal consistency of each dimension in the HBM and TPB models. Use t-test or ANOVA to analyze differences in parental intention, where appropriate. Exploratory factor analysis was used to examine the construct validity and factors were extracted by applying principal component analysis with a varimax rotation. Items with factor loadings <0.40 or loadings >0.40 on multiple factors were eliminated (38). To explore the relationship between independent variables and parents' intentions toward preschool children's myopia preventive behaviors, a hierarchical multiple regression was performed. Model 1 consisted of significant socio-demographic variables found in the univariate analysis. Model 2 entered perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and cues to action; these were HBM variables. Model 3 entered TPB variables, which were attitude, subjective norms and perceived behavioral control. The order of variables inclusion in the model was based on two prior hypotheses. First, HBM variables can explain additional variance after accounting for individual socio-demographic factors. Second, after accounting for the variance of individual factors and HBM variables, the increased variance may be explained by the TPB variables. All statistical analysis were performed using IBM SPSS Statistics 20 software (IBM Corp.). Statistical significance was set at 0.05.
The Bartlett test of sphericity (χ2 = 36208.14, p < 0.001) and Kaiser–Meyer–Olkin measure (0.91) verified interpretability of the exploratory factor analysis. Eight factors with eigenvalues >1 were retained, explaining 69.24% of the total variance. Two questionnaire items were eliminated: “It is serious If my child develops myopia (or worsens myopia) that increases expenses” (perceived severity) and “The ophthalmologist once told me to protect my child's vision” (cues to action). Besides, the factor loadings for the remaining items ranged from 0.560 to 0.901, which is acceptable (Table 1). The Cronbach's alpha coefficient of perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, attitude, subjective norms and perceived behavioral control were 0.625, 0.914, 0.932, 0.861, 0.817, 0.822, 0.946, and 0.903, respectively, indicating good internal consistency reliability. The mean scores and standard deviation for the HBM and TPB variables are detailed in Table 1.
A total of 1,300 parents of preschool children aged 3–6 years were recruited for this study. Table 2 presents the socio-demographic characteristics of the children and parents. The average age of the fathers was 35.79 (SD = 4.40) years, and the average age of the mothers was 34.16 (SD = 4.01) years. About half are single-child families (53.0%). Most of the parents have a bachelor's degree or above. The self-reported prevalence of myopia was 49.9% for fathers and 54.5% for mothers. Among these socio-demographic variables, univariate analysis found there were significant differences in parental intention scores in child's age (F = 2.75, p = 0.042).
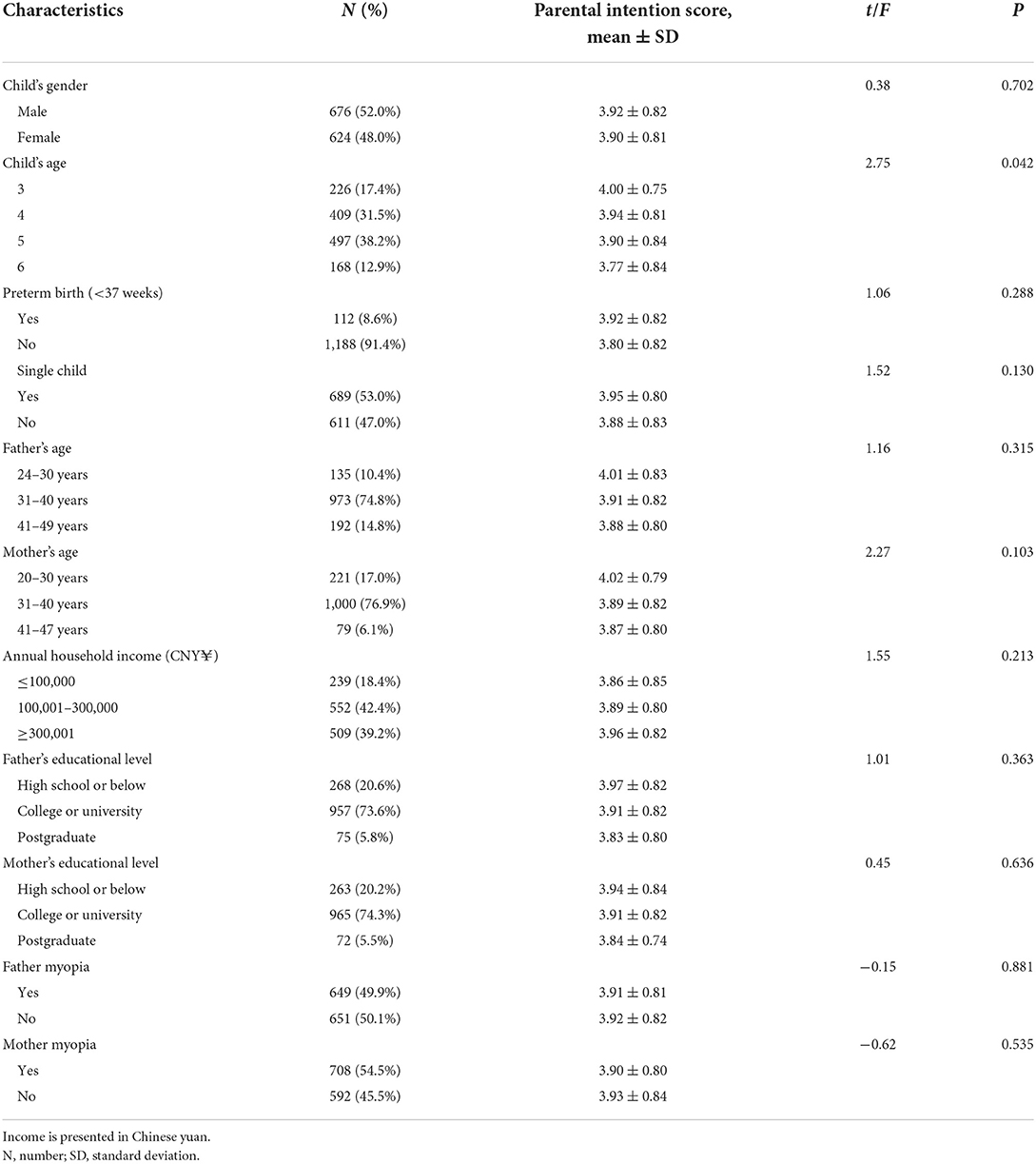
Table 2. Relationships between the parents' intentions scores and socio-demographic characteristics for children and parents (n = 1,300).
A hierarchical multiple regression analysis was conducted to investigate the association between child's age, HBM variables, TPB variables and the parents' intentions toward preschool children's myopia preventive behaviors (Table 3). Multicollinearity analysis was performed on all independent variables, and all variance inflation factor were <1.34. In model 1, Child's age was entered as a control variable and explained 0.6% of the variance (F = 7.241, p = 0.007). When the HBM variables were entered in model 2, the proportion of variance increased to 25.4% (F = 73.290, P < 0.001). In model 3, TPB variables were entered and explained 63.2% of the variance (F = 246.076, p < 0.001). It was found that perceived severity (β = 0.049, p = 0.008), perceived barrier (β = −0.083, p < 0.001), attitude (β = 0.145, p < 0.001), subjective norms (β = 0.230, p < 0.001) and perceived behavioral control (β = 0.507, p < 0.001) were significantly associated with parents' intentions toward preschool children's myopia preventive behaviors.
This study comprehensively used HBM and TPB theories to explore the influencing factors of parents' intentions toward preschool children's myopia preventive behaviors. The final integrative model showed that perceived severity, perceived barriers, attitudes, subjective norms, and perceived behavioral control were associated with parents' intentions. The present study found that the combination of the two theories significantly improved the degree of explanation of parents' intentions toward preschool children's myopia preventive behaviors.
Child's age was the only significant sociodemographic variable in the univariate analysis. Increasing children's age was associated with a decline in parents' intentions toward preschool children's myopia preventive behaviors. An intervention study of preschool children have found that parents report increasing difficulty controlling their children's time spent outdoors and screen use as children get older (39). This decline in parental control as children age might contribute to the decrease in parents' intentions, suggesting that parents should supervise their children to form good myopia preventive behaviors in their early years.
Consistent with other research findings, there was a significant positive association between perceived severity and parents' intentions toward preschool children's myopia preventive behaviors (17). As such, the higher level of perceived severity of myopia, the greater intention parents would exhibit to help their children take myopia preventive behaviors. A previous study further supported this result, where parents with higher levels of severity perception were more likely to supervise children to reduce screen time (40). Besides, this study found perceived severity to be a less influential factor, possibly because the public tends to view myopia as a non-life-threatening condition, distinct from infectious and degenerative diseases such as measles and cancer (17). However, the importance of perceived severity cannot be overlooked, since the intention to act against the threat is not activated if parents perceive myopia as not a threat (26, 41).
Perceived barrier is another variable significantly correlated with parents' intentions toward preschool children's myopia preventive behaviors in HBM theory, which is consistent with other research findings (17). When parents realize there are barriers to helping their children maintain good myopia preventive behaviors, their intentions decrease. Importantly, time cost has been reported as a major barrier in other studies (39). Most families are dual-employed parents who are too busy with their jobs to supervise their children's screen viewing or spend time with their children in outdoor activities (39). However, the average level of parents' perceived barriers was not high in this study. This may indicate that for most preschool children, it is not difficult for parents to control them to adopt various types of myopia preventive behaviors. Nonetheless, perceived barrier shows a significant effect in the final integrative model, possibly due to the strong correlation between perceived barrier and health protective behaviors (42). Although the effect size of perceived barrier on parents' intentions may be weaker than other variables in the integrative model, it still suggests that intervention on parents' perceived barrier can play a role. Therefore, we still recommend that appropriate educational training should be conducted to improve parental intervention techniques and strategies for children, while advocating for parents to spend more time helping children adopt myopia preventive behaviors.
Our study demonstrated a significant positive relationship between parental intentions and attitudes toward preschool children's myopia preventive behaviors. Given the crucial influence of parents on children's lifestyles, parental attitudes are considered to be a key agent in controlling the development of children's myopia (43). Therefore, improving parents' awareness of myopia and changing their attitudes will help motivate parents to take active measures to prevent children's myopia.
The relationship between subjective norms and intentions was often considered to be weak (44). However, our findings suggested that subjective norms not only have a significant positive correlation with parents' intentions toward preschool children's myopia preventive behaviors, but also explain intentions in a large degree. This is consistent with a study finding that subjective norm is a strong predictor of parents' intentions to limit their child's screen time behavior (37). This may be explained by the fact that parents are perceived to have parenting responsibilities and are responsible for their children's healthy behaviors, thereby reinforcing parents' perceived social norms (45, 46). In practical terms, this study provides evidence that subjective norms play an important role in involving parents' intentions toward preschool children's myopia preventive behaviors. Based on the apparent influence of subjective norms, it can be hypothesized that directing social change in a positive direction will be effective, especially emphasizing the advocacy of myopia preventive behaviors by influential people (e.g., teachers). This suggested that it is necessary to provide teachers and parents with appropriate training in children's vision health. Similarly, emphasizing to parents that more and more people are paying attention to maintaining myopia preventive behaviors in their children can have a positive effect.
In this study, the perceived behavioral control component showed the strongest effect on parents' intentions toward preschool children's myopia preventive behaviors. This was supported by a previous study revealing that perceived behavioral control was the main predictor of behavioral intentions (31). The more resources individuals have and the fewer obstacles they anticipate, the greater control they perceived over their behaviors, and the stronger confidence they have to perform behaviors (22). Therefore, when parents have a more comprehensive understanding of children's vision health and myopia preventive behaviors, their confidence in controlling children's related behaviors will increase, and they will be more willing to take action. Accordingly, parents' perceived behavioral control should be strengthened through enhanced advocacy and practice.
Based on the survey results, most parents are aware of their children's possible risk of myopia and the benefits of myopia preventive behaviors, and feel a general level of health cues. But this did not increase their intentions to adopt myopia preventive behaviors for their children. Previous studies based either on TPB or HBM to explain parents' intentions to vaccinate their children found that not all TPB and HBM constructs had significant effects, with some variables showing significant effects in one study and others in another study showing a significant impact (20, 25, 47–49). Just as the findings of this study that perceived susceptibility, perceived benefits and cues to action were not significant variables are inconsistent with other findings on parents' intentions toward preschool children's myopia preventive behaviors (17, 30, 40). It is not surprising that these results are different from those of other populations. Given that few studies have explored factors related to parents' intentions toward preschool children's myopia preventive behaviors using TPB and HBM constructs simultaneously, interventions should be designed based on both models to further verify the effects of each construct. Overall, the integrated model of HBM and TPB can better explain the effects of variables on parents' intentions toward preschool children's myopia preventive behaviors compared to using each of the two behavior models separately.
There are several limitations for this study to consider. First, the participants were recruited from Minhang District, Shanghai, which is a city with a high level of economic and urbanization. This might limit the generalization of the findings to populations in other regions, particularly rural areas. Second, the data of this study were collected through an online survey, which means that there may be some situations that affect the quality of the data, such as comprehension bias in the content of the questionnaire and fill out the questionnaire without reading it. However, we avoid these problems by answering questions from participants in real time online, and setting quality control questions. In addition, to ensure the smooth conduct of research, the use of online surveys during a pandemic is reasonable. Third, this study did not collect data on the refractive errors/ prevalence of myopia of the children recruited as this may have influenced parental knowledge of myopia. Future research may consider incorporating these factors. Finally, although the integrated model of HBM and TPB used in this study can explain parents' intentions toward preschool children's myopia preventive behaviors well. However, other theoretical models of behavior change such as Self-Determination Theory and Integrated Behavioral Models were not included in the study. Future research can incorporate more theoretical models to explore.
The integrated model of HBM and TPB constructed in this study could be well used to explain parents' intentions toward preschool children's myopia preventive behaviors. Parents' perceived severity, perceived barriers, attitudes, subjective norms, and perceived behavioral control can be prioritized intervention targets for myopia preventive practices in preschool children. In particular, there should be more advocacy and practical training for the public and parents of preschool children. Not only to promote myopia preventive behaviors and expectations of the public, but also to improve parents' awareness and attitude, thereby increasing the parents' intentions.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Medical Research Ethics Committee of the School of Public Health, Fudan University (The international registry nos. IRB00002408 and FWA00002399). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
NJ, JC, and HC were responsible for the acquisition, analysis and interpretation of data, and the drafting of the manuscript. YL and YZ contributed to the acquisition, interpretation of data, and critically reviewed the manuscript for important intellectual content. QW, TW, HZ, and HL provided advice regarding study design and developed the questionnaire. JW and JC were the project coordinator and contributed to the review and revision of the manuscript. All authors read and approved the final manuscript.
This study was supported by the Minhang District Natural Science Research Project of Shanghai (Grant No. 2021MHZ047), the Shanghai Eye Starlight Children and Adolescent Myopia Prevention and Control Personnel Training Program (Grant No. 2022HYXG-SQ01), and the Fudan-Minhang Health Consortium Cooperation Project (Grant No. 2021FM10).
We are very grateful to all preschools for their support of this research, and to every parent who willingly and generously granted us their time.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Chua SYL, Ikram MK, Tan CS, Lee YS, Ni Y, Shirong C, et al. Relative contribution of risk factors for early-onset myopia in young Asian children. Invest Ophthalmol Vis Sci. (2015) 56:8101–7. doi: 10.1167/iovs.15-16577
2. Li T, Zhou X, Chen X, Qi H, Gao Q. Refractive error in Chinese preschool children: the Shanghai study. Eye Contact Lens. (2019) 45:182. doi: 10.1097/ICL.0000000000000555
3. Ojaimi E, Rose KA, Morgan IG, Smith W, Martin FJ, Kifley A, et al. Distribution of ocular biometric parameters in a population-based study of Australian children. Invest Ophthalmol Vis Sci. (2005) 46:2748–54. doi: 10.1167/iovs.04-1324
4. Flaka S, Mire H-S, Fitore S, Fjolla S, Avdyl S. Prevalence of myopia in preschool and school children in the municipality of Prishtina in Kosovo. Open J Ophthalmol. (2020) 10:33. doi: 10.4236/ojoph.2020.101005
5. Chua SYL, Sabanayagam C, Cheung Y-B, Chia A, Valenzuela RK, Tan D, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthal Physiol Optics. (2016) 36:388–94. doi: 10.1111/opo.12305
6. Wu P-C, Huang H-M, Yu H-J, Fang P-C, Chen C-T. Epidemiology of myopia. Asia Pac J Ophthalmol. (2016) 5:386–93. doi: 10.1097/APO.0000000000000236
7. Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu H, Kitazawa Y, et al. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology. (2006) 113:1354–62.e1. doi: 10.1016/j.ophtha.2006.04.022
8. Xu L, Wang Y, Li Y, Wang Y, Cui T, Li J, Jonas JB. Causes of blindness and visual impairment in urban and rural areas in Beijing: the Beijing Eye Study. Ophthalmology. (2006) 113:1134.e1–11. doi: 10.1016/j.ophtha.2006.01.035
9. Mutti DO, Zadnik K, Adams AJ. Myopia - the nature versus nurture debate goes on. Invest Ophthalmol Vis Sci. (1996) 37:952–7.
10. Yang G-Y, Huang L-H, Schmid KL, Li C-G, Chen J-Y, He G-H, et al. Associations between screen exposure in early life and myopia amongst chinese preschoolers. Int J Environ Res Public Health. (2020) 17:1056. doi: 10.3390/ijerph17031056
11. French AN, Ashby RS, Morgan IG, Rose KA. Time outdoors and the prevention of myopia. Exp Eye Res. (2013) 114:58–68. doi: 10.1016/j.exer.2013.04.018
12. Morgan IG, Ohno-Matsui K, Saw S-M. Myopia. Lancet. (2012) 379:1739–48. doi: 10.1016/S0140-6736(12)60272-4
13. Daw NW. Critical periods and amblyopia. Arch Ophthalmol. (1998) 116:502–5. doi: 10.1001/archopht.116.4.502
14. Bremond-Gignac D, Copin H, Lapillonne A, Milazzo S, European Network of S, Research in Eye D. Visual development in infants: physiological and pathological mechanisms. Curr Opin Ophthalmol. (2011) 22(Suppl.):S1–8. doi: 10.1097/01.icu.0000397180.37316.5d
15. Tao T, Wang L, Fan C, Gao W. Development of self-control in children aged 3 to 9 years: perspective from a dual-systems model. Sci Rep. (2014) 4:7272. doi: 10.1038/srep07272
16. Zhou S, Yang L, Lu B, Wang H, Xu T, Du D, et al. Association between parents' attitudes and behaviors toward children's visual care and myopia risk in school-aged children. Medicine. (2017) 96:e9270. doi: 10.1097/MD.0000000000009270
17. Lwin MO, Saw S-M. Protecting children from myopia: a PMT perspective for improving health marketing communications. J Health Commun. (2007) 12:251–68. doi: 10.1080/10810730701266299
18. Guo X. Construction and validation of the integration model of planned behavior theory and health belief model. In: 9th International Conference on Management Science and Engineering Management (ICMSEM). Karlsruhe, Germany: Karlsruhe Inst Technol. (2015). p. 151–60. doi: 10.1007/978-3-662-47241-5_11
19. Chan DK-C, Fung Y-K, Xing S, Hagger MS. Myopia prevention, near work, and visual acuity of college students: integrating the theory of planned behavior and self-determination theory. J Behav Med. (2014) 37:369–80. doi: 10.1007/s10865-013-9494-9
20. Li J-B, Lau EYH, Chan DKC. Why do Hong Kong parents have low intention to vaccinate their children against COVID-19? testing health belief model and theory of planned behavior in a large-scale survey. Vaccine. (2022) 40:2772–80. doi: 10.1016/j.vaccine.2022.03.040
21. Ajzen I. From Intentions to Actions: A Theory of Planned Behavior. In: Kuhl J, Beckmann J, editors. Action Control: From Cognition to Behavior. Berlin; Heidelberg: Springer (1985). p. 11–39. doi: 10.1007/978-3-642-69746-3_2
22. Ajzen I. The theory of planned behavior. Organizational behavior and human decision processes. (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
23. Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Philos Rhetoric. (1977) 10:578.
24. Zeidi IM, Hajiaghaye AP, Zeidi BM. Investigating the effect of education based on the theory of planned behavior on employee safety behaviors. Knowl Health. (2013) 8:105–1. doi: 10.1234/2Fknh.v8i3.24
25. Caso D, Capasso M, Fabbricatore R, Conner M. Understanding the psychosocial determinants of Italian parents' intentions not to vaccinate their children: an extended theory of planned behaviour model. Psychol Health. (2022) 37:1111–31. doi: 10.1080/08870446.2021.1936522
26. Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Quart. (1988) 15:175–83. doi: 10.1177/109019818801500203
27. Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: John Wiley & Sons (2008).
28. Ataei P, Gholamrezai S, Movahedi R, Aliabadi V. An analysis of farmers' intention to use green pesticides: the application of the extended theory of planned behavior and health belief model. J Rural Stud. (2021) 81:374–84. doi: 10.1016/j.jrurstud.2020.11.003
29. Tseng GL, Chen CY. Evaluation of high myopia complications prevention program in university freshmen. Medicine. (2016) 95:e5093. doi: 10.1097/MD.0000000000005093
30. Al Ghailani NAS, Noushad B, Khurshid F, Ismail GM. Parents'awareness and perception of children's refractive error. a qualitative study. Malaysian J Public Health Med. (2020) 20:85–91. doi: 10.37268/mjphm/vol.20/no.3/art.656
31. Wang X, Chen D, Xie T, Zhang W. Predicting women's intentions to screen for breast cancer based on the health belief model and the theory of planned behavior. J Obstetr Gynaecol Res. (2019) 45:2440–51. doi: 10.1111/jog.14109
32. Hagger MS, Chatzisarantis NL. Integrating the theory of planned behaviour and self-determination theory in health behaviour: a meta-analysis. Br J Health Psychol. (2009) 14:275–302. doi: 10.1348/135910708X373959
33. Li Y, Zhang S, Song J, Tuo M, Sun C, Yang F. Effects of self-management intervention programs based on the health belief model and planned behavior theory on self-management behavior and quality of life in middle-aged stroke patients. Evid Based Compl Altern Med. (2021) 2021:8911143. doi: 10.1155/2021/8911143
34. Javier JR, Deavenport-Saman A, Florendo E, Bantol KEA, Palinkas LA. Health equity and enrollment in preventive parenting programs: a qualitative study of Filipino parents. Evid Based Pract Child Adolesc Mental Health. (2022) 7:245–59. doi: 10.1080/23794925.2021.2013141
35. Cheng L, Kim HK. Eye screenings among Singaporeans aged 40–60 years: formative research based on the theory of planned behaviour. Singapore Med J. (2021) 1:9. doi: 10.11622/smedj.2021099
36. Natan MB, Kabha S, Yehia M, Hamza O. Factors that influence israeli muslim Arab parents' intention to vaccinate their children against influenza. J Pediatr Nurs. (2016) 31:293–8. doi: 10.1016/j.pedn.2015.12.014
37. Hamilton K, Spinks T, White KM, Kavanagh DJ, Walsh AM. A psychosocial analysis of parents' decisions for limiting their young child's screen time: an examination of attitudes, social norms and roles, and control perceptions. Br J Health Psychol. (2016) 21:285–301. doi: 10.1111/bjhp.12168
38. Costello AB, Osborne J. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. (2005) 10:7. doi: 10.7275/jyj1-4868
39. Liu S-M, Chang F-C, Chen C-Y, Shih S-F, Meng B, Ng E, et al. Effects of parental involvement in a preschool-based eye health intervention regarding children's screen use in china. Int J Environ Res Public Health. (2021) 18:11330. doi: 10.3390/ijerph182111330
40. Chang F-C, Chiu C-H, Chen P-H, Miao N-F, Chiang J-T, Chuang H-Y. Computer/mobile device screen time of children and their eye care behavior: the roles of risk perception and parenting. Cyberpsychol Behav Soc Netw. (2018) 21:179–86. doi: 10.1089/cyber.2017.0324
41. Rogers R, Prentice-Dunn S, Gochman D. Handbook of Health Behavior Research 1: Personal and Social Determinants. New York, NY: Plenum Press. (1997). Vol. 28. p. 113–32.
42. Carpenter CJ. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. (2010) 25:661–9. doi: 10.1080/10410236.2010.521906
43. McCrann S, Flitcroft I, Lalor K, Butler J, Bush A, Loughman J. Parental attitudes to myopia: a key agent of change for myopia control? Ophthal Physiol Opt. (2018) 38:298–308. doi: 10.1111/opo.12455
44. Ham M, Jeger M, Frajman Ivković A. The role of subjective norms in forming the intention to purchase green food. Econ Res. (2015) 28:738–48. doi: 10.1080/1331677X.2015.1083875
45. Andrews KR, Silk KS, Eneli IU. Parents as health promoters: a theory of planned behavior perspective on the prevention of childhood obesity. J Health Commun. (2010) 15:95–107. doi: 10.1080/10810730903460567
46. Hamilton K, Thomson CE, White KM. Promoting active lifestyles in young children: investigating mothers' decisions about their child's physical activity and screen time behaviours. Matern Child Health J. (2013) 17:968–76. doi: 10.1007/s10995-012-1081-0
47. Ellithorpe ME, Aladé F, Adams RB, Nowak GJ. Looking ahead: caregivers' COVID-19 vaccination intention for children 5 years old and younger using the health belief model. Vaccine. (2022) 40:1404–12. doi: 10.1016/j.vaccine.2022.01.052
48. Wan AW, Hagger MS, Zhang C-Q, Chung JS, Lee K, Bautista A, et al. Protecting children from COVID-19: examining US parents motivation and behaviour using an integrated model of self-determination theory and the theory of planned behaviour. Psychol Health. (2022):1–21. doi: 10.1080/08870446.2022.2111681. [Epub ahead of print].
Keywords: health belief model, theory of planned behavior, myopia, preschool children, parental intention
Citation: Jiang N, Chen J, Cao H, Liu Y, Zhang Y, Wang Q, Wang T, Zhao H, Lu H, Yang L and Wang J (2022) Parents' intentions toward preschool children's myopia preventive behaviors: Combining the health belief model and the theory of planned behavior. Front. Public Health 10:1036929. doi: 10.3389/fpubh.2022.1036929
Received: 05 September 2022; Accepted: 10 November 2022;
Published: 24 November 2022.
Edited by:
Carla Lanca, Escola Superior de Tecnologia da Saúde de Lisboa (ESTeSL), PortugalReviewed by:
Stephanie Kearney, Glasgow Caledonian University, United KingdomCopyright © 2022 Jiang, Chen, Cao, Liu, Zhang, Wang, Wang, Zhao, Lu, Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiayue Chen, Y2p5X21vb25AMTI2LmNvbQ==; Jiwei Wang, aml3ZWl3YW5nQGZ1ZGFuLmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.