- 1College of Economics, Xi'an University of Finance and Economics, Xi'an, China
- 2Center for Experimental Economics in Education, Shaanxi Normal University, Xi'an, China
- 3Zhongshan Ophthalmic Center, State Key Laboratory of Ophthalmology, Sun Yat-sen University, Guangzhou, China
Background: Cataracts are highly prevalent in rural China, but patient utilization of eye care services is low. Cataract knowledge is regarded as an important factor in eye care utilization. Few studies, however, have been conducted to measure the level of cataract knowledge and its relationship with eye care utilization among older adults in rural China. Hence, we described cataract knowledge and investigated the relationships between cataract knowledge and eye care utilization among adults (≥50 years) in rural Western China.
Methods: A large community-based cross-sectional study was conducted from October to December 2020 among adults aged 50 years and older in 73 rural villages in Qingcheng County, Western China. The participants underwent an eye examination at their village clinic to determine whether they had cataracts. Participants also answered a questionnaire about cataracts, eye care utilization status, and sociodemographic characteristics. The collected data underwent descriptive and multiple logistic regression analyses.
Results: The eye examinations revealed that 45.15% (675/1,495) of participants had cataracts in at least one eye, yet 90.67% (612/675) were left untreated. The average score achieved by participants about cataract knowledge was 4.91 points (total score was eight points). Correct knowledge about cataracts was positively associated with cataract screening and cataract surgery. Elders with better cataract knowledge were 2.21 times more likely to undergo cataract screening (OR, 2.21; 95% CI, 1.54–3.16) and 5.61 times more likely to undergo cataract surgery (OR, 5.61; 95% CI, 2.87–10.98). More than half had three fundamental misconceptions about how cataracts should be treated, how much they should cost, and when they should be treated. Participants who did not have these misconceptions were more likely to receive cataract screening by 1.21–2.02 times and cataract surgery by 1.76–3.48 times.
Conclusion: There are misunderstandings about cataract treatment methods, treatment costs and timing in the sample areas. A better understanding of cataracts was significantly positively associated with cataract screening and cataract surgery. Health education on cataracts and regular eye examinations are needed to improve eye care utilization in rural China.
Introduction
Cataract remains the leading cause of blindness in developing countries (1). The prevalence of cataracts is highly correlated with age and more prevalent in adults over 50 years old (2). If left untreated, cataracts worsen vision and reduce the quality of life by limiting the patient's productive activities and lowering personal and family economic levels (3, 4). People with cataracts are also more prone to depression and social isolation (5). Some studies have also found that cataracts pose other risks, such as increased falls, a common cause of death in older adults (6, 7).
China provides a representative case for cataract study. Cataracts caused 18.14 million Chinese people to have a moderate or severe visual impairment in 2019, and 2.95 million became blind (8). The disease burden caused by cataracts in China ranks second globally, only lower than in India (9). As the aging population grows in China (10), timely cataract treatment is necessary.
Surgery is the only effective way to treat cataracts and has been rated by the WHO as one of the most cost-effective medical procedures (2). In addition, with the development of surgical technology, surgical vision can be recovered quickly, and the visual effect is good (1). However, China's cataract surgical rate (CSR) is low, especially in rural areas. Cataract Surgical Rate, which refers to the number of Cataract surgery each year for every million people, is the most commonly used national standard. The National Health Commission reported in June 2020 that the CSR in China was close to 3,000 (11), which is far lower than the average rate of 6,000 CSR in developing countries, and 10,000 CSR in developed countries average rates (12). CSR saw a large urban-rural gap in China. An empirical study points out that in 2012, the CSR in Shanghai's urban area exceeded 6,000, while is only 500 in rural areas (13). In addition to the CSR indicator, cataract surgical coverage (CSC) provides a more accurate measure of how many patients who require cataract surgery have already had cataract surgery (4). A population-based sample representative of rural areas throughout China finds that CSC among those with VA worse than 20/200 in both eyes because of cataracts was 62.8% (14), which has not met the World Health Organization's minimum CSC standard (85%).
The main barrier to the cataract surgery rate may come from the demand side, especially patients' knowledge of cataracts (15, 16). In China, villagers can reduce at least 50% cost of cataract surgery through the New Rural Cooperative Medical System (17). On the other hand, many studies find that awareness and knowledge of cataracts is the main barrier to the low cataract surgery rate (15, 18, 19). A study in southern China found that only 10% of people know adequately about cataracts (20).
Studies suggested that individual awareness and knowledge of eye diseases are important factors in screening, diagnosis, treatment compliance, and prevention (21). Furthermore, assessing cataract knowledge is a prerequisite for designing cataract health education interventions (22, 23). However, previous studies were conducted in cities or areas with better economic levels (16, 22, 24) and were small samples (19, 20, 25). Besides, studies targeting the population over 50 years of age are insufficient. Nevertheless, paying attention to the cataract knowledge level of this group of people is essential for the timely treatment of cataracts. More research was needed in this field. Therefore, this paper aims to describe the knowledge of cataracts among adults aged 50 and above in rural Western China and to analyze the relationships between knowledge of cataracts and eye care utilization using a large-scale community-based sample.
Methods
Setting
A community-based, cross-sectional study was conducted among adults aged 50 and above in rural areas of Qingchen county, Gansu Province, Northwestern China. This study was carried out from October to December 2020. Qingcheng County is located 60 km from the main Qingyang City. Two public hospitals provide different eye care services in Qingcheng, including cataract screening and cataract surgery. Five hospitals in Qingyang city also provide cataract treatment services.
Qingcheng County is in the eastern part of Gansu Province. Gansu province is relatively underdeveloped compared to other regions of China. Official statistics indicate that in 2020, villagers' per capita income in Gansu was 39.6% lower than the national level. The villagers' per capita income in Qingcheng County was 2.5% lower than in Gansu province. Our sample area is more representative of the situation in poorer rural areas.
Sampling
The study sample was collected using a random sampling procedure at the village level. First, a list of the population in each village was obtained through the county people's hospital, involving 153 villages. Ten villages were dropped due to the total population of the village being less than 800. Then, we randomly selected half of the 143 villages as sample villages. Hence, 73 villages were included in this study. Finally, all residents who were 50 years old and above in these villages participated in this study.
Eligibility criteria included being a registered resident of Qingcheng, aged 50 years or older, able to give oral informed consent and verbally answer questions on the researcher-administered questionnaire. A total of 1,554 participants were eligible for the study, among which 1,495 provided complete information required by the questionnaire. The response rate was 96.2%.
Data collection
Eye examinations
The survey included two parts: eye examinations and a questionnaire survey. The eye examinations were carried out by a team of five people, including an ophthalmologist and a nurse from the local public hospital, an experienced ophthalmologist from the Zhongshan Ophthalmic Center, and two questionnaires.
Three days before the eye examinations, the village clinic doctor informed the villagers aged over 50 to attend the eye examinations on the appointed day and informed them that the eye examinations were free. The eye examinations session lasted from 9 a.m. to 5 p.m. at the village clinic, during which the ophthalmic screening team offered free eye examinations to all villagers aged above 50. Eye examinations included two steps: vision screening and cataract diagnosis. First, the nurse measured participants' presenting visual acuity (PVA) by Early Treatment Diabetic Retinopathy Study (ETDRS) charts, a worldwide standard instrument for assessing visual acuity (26). If one's PVA was ≤0.3 in the better eye (a recommended criteria for cataract surgery) (27), he/she would proceed to the cataract screening. Secondly, the ophthalmologist conducted a full ocular examination of pupil dilation using a slit lamp microscope to diagnose the cataract. When there is a dispute about cataract diagnosis, the result is subject to the ophthalmologist from the Zhongshan Ophthalmic Center. Visual acuity and further cataract diagnosis results were recorded by the nurse and the ophthalmologist, respectively.
Questionnaire survey
The questionnaire survey was executed in the form of a face-to-face interview. The questionnaire survey consists of three parts: basic information, eye care utilization and knowledge of cataracts. Basic information included age, gender, education status and marital status. The facts, such as whether the interviewee lives with at least one child or not and the annual household income, were also included in the information.
Eye care utilization can be measured by asking participants to answer yes or no to (1) whether they had at least a vision screening in the past, (2) whether they ever had cataract screening in the past, and (3) whether they were ever had cataract surgery. According to these answers, eye care utilization was defined as three dummy variables (0 = No, 1 = Yes).
Participants' knowledge of cataracts was assessed using eight questions in our study. Participants' knowledge of cataracts was assessed using eight questions in our study. Following the literature (15, 20), these questions were developed by a group of health experts from Shaanxi Normal University and Zhongshan Ophthalmic Center (an authoritative ophthalmology institution in China). Each item was equally weighted. The eight dichotomous variables (knowledge of cataracts) were given a score of 0 (wrong answer) or 1 (right answer).
Hence, the total score for all knowledge questions ranged from 0 to 8 points. We also generate a dummy variable named cataract knowledge level, which takes the value of 1 if the total score is higher than the mean (good knowledge), and 0 (poor knowledge).
Ethical consideration
The study was conducted following the Declaration of Helsinki and approved by the Stanford University Institutional Review Board (ID. 64279). Health education about cataracts was given after the survey for each study participant. We obtained the respondents' oral informed consent; All data were analyzed anonymously.
Statistical analysis
Frequencies and percentages were used to describe data. Multivariate logistic analyses were used to analyze the associations between cataract knowledge and eye care utilization. Covariables were included in the regression, including age, gender, education status, marital status, whether the interviewee lives with at least one child, household income and whether PVA ≤0.3 in either eye. This study's result was deemed statistically significant if the P-value was < 0.05. Odds ratios (OR), 95% confidence intervals (CI), and P-value are presented in Tables 4, 5. All analyses were conducted using Stata15.1 (Stata Corp).
Results
Sociodemographic characteristics of the sample
Among 1,554 adults aged ≥50 years, 1,495 of them completed the interview. The response rate was 96.20%. The mean age was 63 years (±9 years). Among the study participants, about 60% are female. In terms of education, 43.75% of respondents had no formal education. Three-quarters (1,124/1,495) of the study participants have a spouse, and more than half (877/1,495) do not live with a child. Forty-six percent (690/1,495) of the study participants' household income was <10,000 RMB (Criteria for low-income families in rural China). Most respondents (1,124/1,495) have PVA less than or equal to 0.3 in either eye (Table 1).
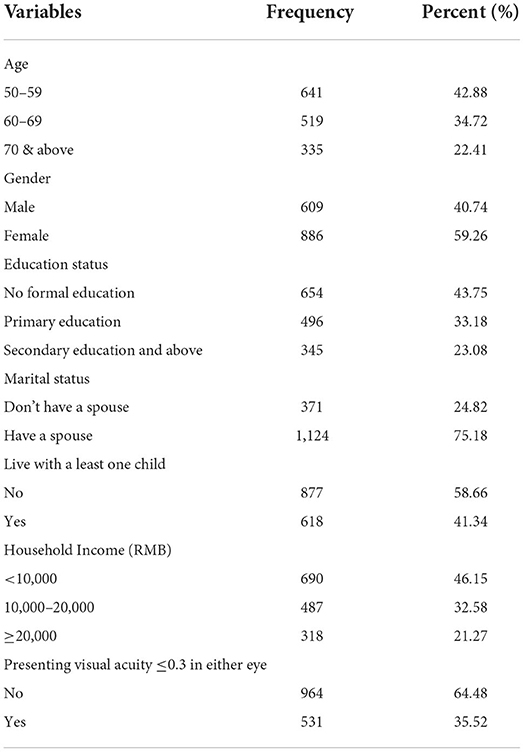
Table 1. Sociodemographic characteristics of adults aged 50 and above in rural Western China (n = 1,495).
History of eye care utilization and prevalence of cataract
Before this study, 35.52% of the 1,495 participants had received vision screening and 17.99% had undergone cataract screening. Our vision and cataract screening revealed that 45.15% of participants had cataracts in at least one eye (Table 2). Among those diagnosed with cataracts, the majority (90.67%) of them were left untreated, suggesting the cataract surgical coverage was <10% in our sample, lower than the World Health Organization's minimum cataract surgery coverage standard (85%).
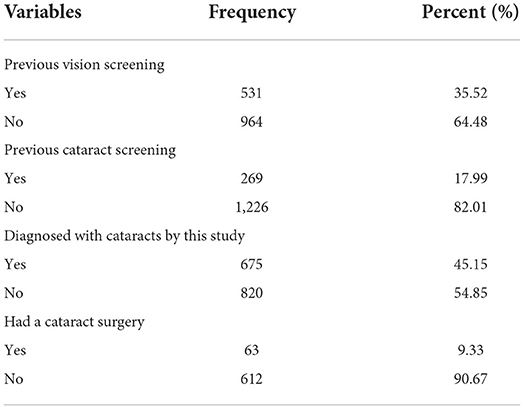
Table 2. Previous history of eye care utilization and prevalence of cataracts of adults aged 50 and above in rural Western China (n = 1,495).
Participants' knowledge of cataracts
Table 3 shows the knowledge of cataracts among the participants presented in the correct rate of questions from high to low. The participants' mean (±SD) knowledge score is 4.91 ± 1.91 points. Among the eight questions, the correct rate of five questions is more than 50%. As for the level of cataract knowledge, we find nearly two-thirds (62.88%) of the participants had good knowledge of cataracts.
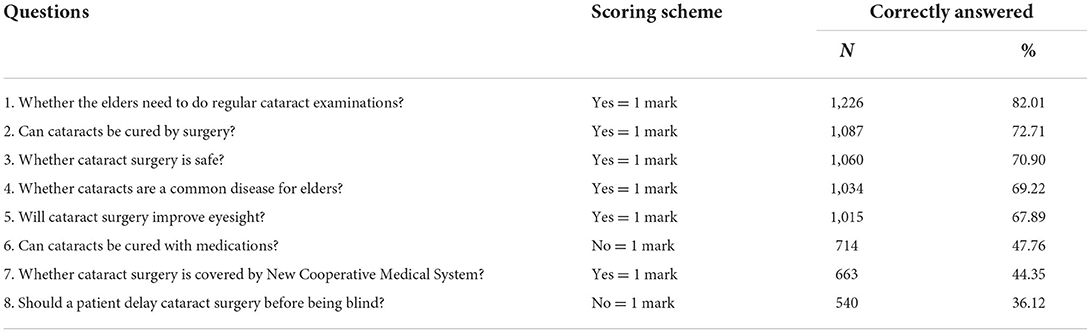
Table 3. Knowledge about cataracts among adults aged 50 and above in rural Western China (n = 1,495).
Specifically, the accuracy of each question is ranked in descending order as follows. The importance of regular cataract examinations was acknowledged by 1,226 (82.01%) participants. About 70% of the participants believed that cataracts could be treated with surgery and that the surgery was safe. It was understood by 1,034 participants (69.22%) that cataracts are a common disease for older. More than two-thirds (67,89%) believed that cataract surgery improves visual acuity. However, the accuracy of the three questions is < 50%. Over half of the participants had the wrong idea about how to treat cataracts, as evidenced by the 714 (47.76%) people who correctly answered that cataracts cannot be cured with medications. Less than half of those participants (44.35%) knew that the new cooperative health system covered cataract surgery. In addition, only 37 (2.47%) participants know the specific reimbursement rate of cataract surgery. As for the question with the lowest accuracy, only 540 (36.12%) participants realized that cataracts should be treated in time, which means that about two-thirds of the participants might delay cataract surgery before losing eye vision (Table 3).
Knowledge of cataracts and eye care utilization
Table 4 shows the associations of cataract knowledge level with eye care utilization (cataract screening and surgery) estimated by multiple logit models. We find that cataract knowledge level was significantly associated with cataract screening and cataract surgery. Participants with good cataract knowledge were 2.21 times more likely to undergo cataract screening (OR = 2.21; 95% CI = 1.54–3.16, P = 0.007). Moreover, cataract patients with good knowledge were 4.92 times more likely to undergo cataract surgery (OR = 4.92; 95% CI = 2.50–9.70, P = 0.001).
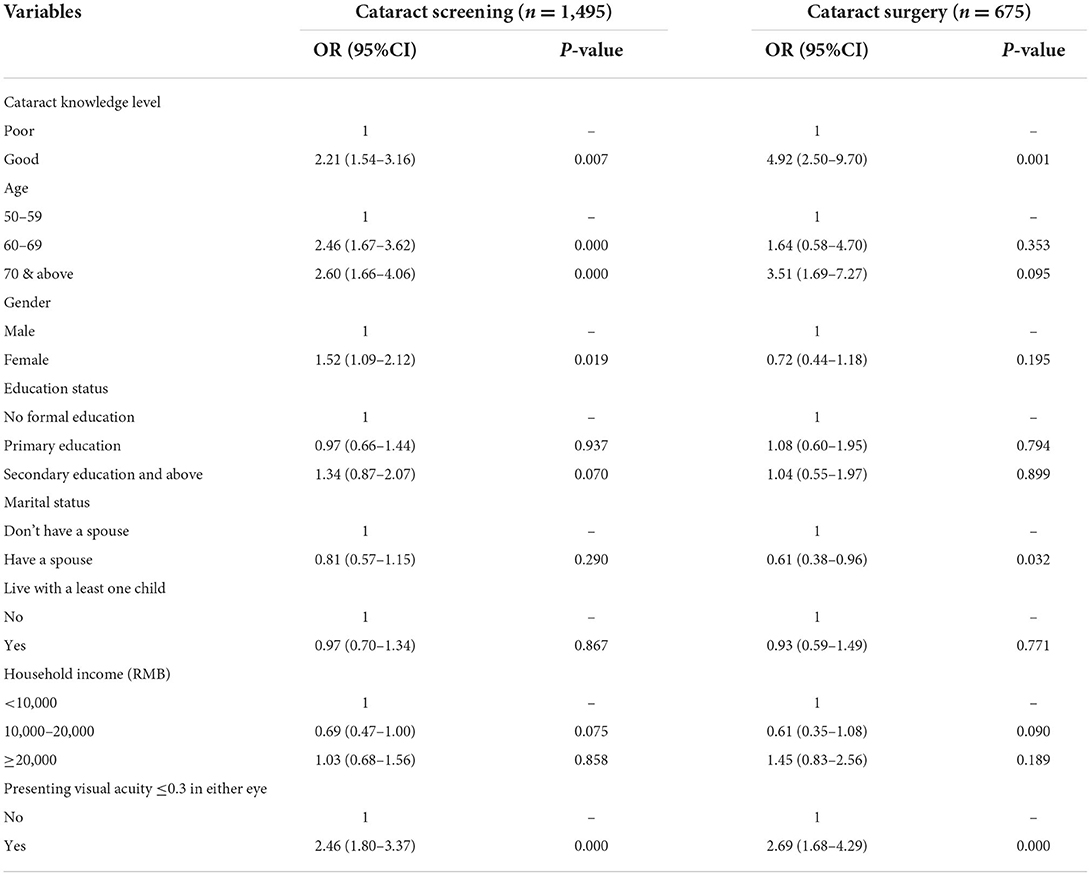
Table 4. Multivariate estimation of the association of knowledge level about cataracts with eye care utilization.
Several sociodemographic characteristics were also associated with cataract screening and cataract surgery (Table 4). Older age (P < 0.001); female (P < 0.05), and PVA ≤0.3 in either eye (P < 0.001) were associated with cataract screening, while education status, marital status, living status and household income were not; As for the cataract surgery, the following characteristics were associated with cataract surgery: don't have a spouse (P < 0.05) and PVA ≤0.3 in either eye (P < 0.001).
Furthermore, we investigated the association between these eight categories of knowledge and eye care utilization respectively to investigate which category of knowledge influences the participants' eye care utilization. The results are shown in Table 5. In general, participants with adequate knowledge of cataract surgery were more likely to undergo cataract screening and surgery.
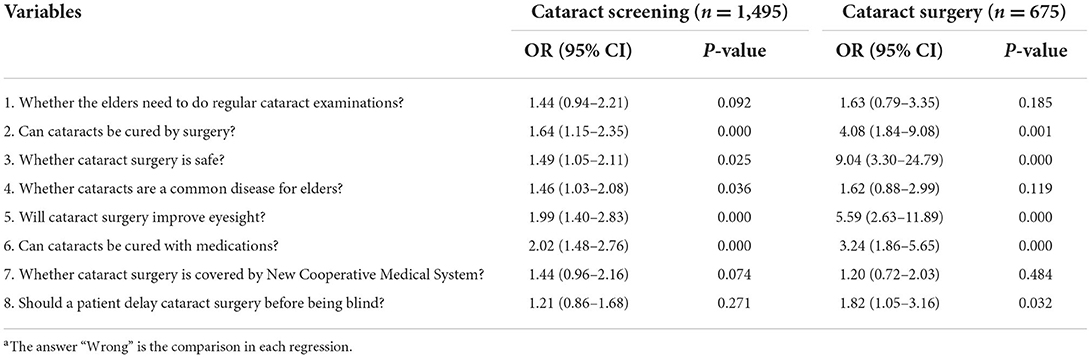
Table 5. Multivariate estimation of the association of knowledge about cataracts with eye care utilizationa.
For cataract screening, participants who correctly answered the question “cataracts cannot be cured with medications” were two times more likely to undergo cataract screening (OR = 2.02; 95% CI =1.48–2.76), which has the strongest influence on the screening among eight questions. Participants who realized that “cataracts can be cured by surgery,” “cataracts surgery is safe,” “cataracts are a common disease,” and “cataract surgery can improve eyesight” were more likely to undergo cataract screening than their counterparts. However, the knowledge of “Should a patient delay cataract surgery before being blind?” was insignificantly associated with cataract screening (P = 0.271). It is understandable, considering that this knowledge seems to be indirectly related to accepting cataract screening.
For cataract surgery, patients who realize that “cataracts can be cured by surgery,” “cataracts surgery is safe,” “cataracts cannot be cured with medication,” “cataract surgery can improve eyesight” and “a patient should not delay cataract surgery before being blind” were more likely to undergo cataract surgery than their counterparts.
Discussion
Like in other countries or areas, cataracts in rural Western China remain a devastating condition. Cataracts were diagnosed in 45.15% of the participants aged 50 and above, which is consistent with earlier research (8, 28). However, our study found that the rate of eye care utilization in rural areas was much lower than in urban or developed areas. According to the American Academy of Ophthalmology's (AAO) guidelines, people aged 65 years and older should have a vision test every 1–2 years (29). Whereas, only one-third of the subjects (35.52%) in this study reported they had sought vision screening in the past, and even fewer (17.99%) indicated they had undergone cataract screening. Among the patients diagnosed with cataracts, only 9.33% underwent cataract surgery. This proportion was only half of that in urban areas (17.81%) (25). This finding implies that improving cataract surgical coverage in rural areas of China continues to be challenging.
The overall cataract knowledge level found in the current study was 62.88%, which is close to a study done in northwest Ethiopia (61.7%) (19) but lower than studies done in Chengdu, China (70.8%) (24) and Nepal (70.4%) (30). The target population for the last two studies was age ≥40. Hence, these subtle differences may be due to the difference in the target population and study setting.
Specifically, in our sample, adults over 50 years old are unable to understand cataract knowledge mainly in 3 aspects. The first and biggest misconception is that many people believe that cataracts need to be treated until they are blind, which means villagers do not know the right time to treat cataracts. On the second, more than half of the participants were unaware that new rural cooperative medical care reimburses the cost of cataract surgery, and even fewer were aware of specific reimbursement ratios. As a result, these individuals may choose not to seek eye care services because of miscalculating treatment costs for their cataracts. While on the third, 52.24% of the participants thought that taking medicine could cure cataracts, which illustrated that the correct treatment modality for these individuals was unclear. People with this misconception may choose not to have cataract surgery because they think medications (e.g., eye drops) can replace surgery. This result was also demonstrated by the multiple regression results in Table 5 (Row 6, columns 3), in which individuals who believed that cataracts could not be treated with medication were 3.24 times more likely to have surgery than those with these misconceptions. These results show that the correction of misunderstandings above must be covered in the health education on cataracts. Of course, other cataract-related knowledge in health education is also needed.
Furthermore, we found that those with better knowledge of cataracts were more likely to participate in cataract screening and surgery. Whether cataract knowledge is analyzed as a whole or divided into eight questions, the results are robust. The results have also been found in other related studies (15, 31, 32). This study enlightens that education on cataract knowledge in rural areas may help improve eye care utilization. In addition to cataract knowledge, we also found that age and vision status may be major factors affecting eye health services.
Our study still has several limitations. Firstly, our results may be skewed because villagers with an existing vision impairment or cataract would be more likely to participate than those with no such problem. However, the prevalence of cataracts in this study is generally consistent with previous studies suggesting that any bias would be small. Further studies are needed to evaluate the causal relationship between knowledge of cataracts and eye care utilization. Second, the utilization of eye care services are self-reported variables, and self-report bias may influence our results. Additionally, this study describes a population from a single region in rural Western China. Thus, extending our results to other settings must be done only with caution.
Despite its limitations, based on a large sample, our study provides new data on the villagers' knowledge of cataracts and its relationship with eye care utilization in rural areas. Moreover, the study has described the key misunderstanding in cataract cognition in rural areas and generated a useful prerequisite for eye health education interventions in the future. Therefore, the results of this study will provide researchers, policymakers, and resource distributors with basic information to plan health education and promotion programs that enable early cataract prevention and treatment options.
Conclusions
Cataract patients in Western China's rural areas have low utilization of eye care and misconceptions about cataract treatment methods, timing, and cost. Better knowledge of cataracts was significantly and positively associated with cataract screening and surgery. With the aging population in the future, the scale of cataract patients and the number of blindness caused by cataracts will continue to expand. Hence, it is recommended for the national and regional ministry of health offices to organize different health education programs focusing on regular eye examinations in rural areas.
Data availability statement
The raw data supporting the conclusions of this study is available from the corresponding author upon reasonable request.
Ethics statement
The study was conducted following the Declaration of Helsinki and was reviewed and approved by the Stanford University Institutional Review Board (ID. 64279). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
HG conceptualized and supervised the study. KD developed the proposal, did the data collection, analyzed the data, and wrote the manuscript. YZ, YD, and DW contributed to the study design, made substantial contributions to the acquisition, and quality assurance of the data. All authors read and approved the final manuscript.
Funding
This study was funded by Sany Foundation (Beijing, China). The authors are also supported by Higher Education Discipline Innovation Project, Grant Number B16031. The study's funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Acknowledgments
We would like to acknowledge Matthew Boswell, Juerong Huang, Min Li, Rong Dai, Baoping Cao, Wenting Liu, and the great effort of enumerators from the Center for Experimental Economics in Education of Shaanxi Normal University. We give special thanks to the staff from Zhongshan Ophthalmic Center at Sun Yat-sen University for their invaluable guidance and advice. We wish to thank all the adults who participated in this study and the research assistants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Liu Y-C, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts. Lancet. (2017) 390:600–12. doi: 10.1016/S0140-6736(17)30544-5
2. Asbell PA, Dualan I, Mindel J, Brocks D, Ahmad M, Epstein S. Age-related cataract. Lancet. (2005) 365:599–609. doi: 10.1016/S0140-6736(05)70803-5
3. Polack S, Kuper H, Eusebio C, Mathenge W, Wadud Z, Foster A. The impact of cataract on time-use: results from a population based case-control study in Kenya, the Philippines and Bangladesh. Ophthalmic Epidemiol. (2008) 15:372–82. doi: 10.1080/09286580802478716
4. Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology. (2015) 122:1706–10. doi: 10.1016/j.ophtha.2015.04.014
5. Chen PW, Liu PS, Lin SM, Wang JH, Loh CH. Cataract and the increased risk of depression in general population: a 16-year nationwide population-based longitudinal study. Sci Rep. (2020) 10:13421. doi: 10.1038/s41598-020-70285-7
6. Menezes C, KHC Vilaça, Menezes R. Falls and quality of life of people with cataracts. Rev Bras Oftalmol. (2016) 75:40–44. doi: 10.5935/0034-7280.20160009
7. Lu B, Yang M, Cumming RG, Stanaway FF. Falls and impact on disability and healthy life expectancy in China: evidence from the China Health and Retirement Longitudinal Survey (CHARLS). China Econ Rev. (2020) 61:101426. doi: 10.1016/j.chieco.2020.101426
8. Song P, Wang H, Theodoratou E, Chan KY, Rudan I. The national and subnational prevalence of cataract and cataract blindness in China: a systematic review and meta-analysis. J Glob Health. (2018) 8:010804. doi: 10.7189/jogh.08.010804
9. Xu T, Wang B, Liu H, Wang H, Yin P, Dong W, et al. Prevalence and causes of vision loss in China from 1990 to 2019: findings from the Global Burden of Disease Study 2019. Lancet Public Health. (2020) 5:e682–91. doi: 10.1016/S2468-2667(20)30254-1
10. Mai Y, Peng X, Chen W. How fast is the population ageing in China? Asian Popul Stud. (2013) 9:216–39. doi: 10.1080/17441730.2013.797295
11. National Health Commission of China. Available online at: http://www.gov.cn/xinwen/2020-06/06/content_5517657.htm (accessed July 21, 2021).
12. Wang W, Yan W, Fotis K, Prasad NM, Lansingh VC, Taylor HR, et al. Cataract surgical rate and socioeconomics: a global study. Invest Ophthalmol Vis Sci. (2016) 57:5872–81. doi: 10.1167/iovs.16-19894
13. Zhu M, Zhu J, Zou H, He X, Zhao R, Lu L. Analysis of cataract surgical rate and its influencing factors in Shanghai, China. Natl Med J China. (2013) 93:3737. doi: 10.3760/cma.j.issn.0376-2491.2013.47.000
14. Zhao J, Xu X, Ellwein LB, Guan H, He M, Liu P, et al. Cataract surgical coverage and visual acuity outcomes in rural China in 2014 and comparisons with the 2006 China Nine-Province Survey. Am J Ophthalmol. (2018) 193:62–70. doi: 10.1016/j.ajo.2018.06.004
15. Chen T, Jin L, Zhu W, Wang C, Zhang G, Wang X, et al. Knowledge, attitudes and eye health-seeking behaviours in a population-based sample of people with diabetes in rural China. Br J Ophthalmol. (2020) 105:806–11. doi: 10.1136/bjophthalmol-2020-316105
16. Li L-S, Ge Z-Y, Lohfeld L, Zhou K, Zhou W-H, Cui L-L, et al. Knowledge, attitudes and practices related to seeking medical eyecare services by adults with moderate-to-severe visual impairment in rural Yueqing, Wenzhou, China: a cross-sectional survey. Int J Ophthalmol. (2020) 13:1115–23. doi: 10.18240/ijo.2020.07.16
17. Yan X, Congdon N, He M. Prevention of cataract blindness in rural China. Asia Pac J Ophthalmol. (2012) 1:69–71. doi: 10.1097/APO.0b013e31824a4383
18. Zhang XJ, Jhanji V, Leung CK-S, Li EY, Liu Y, Zheng C, et al. Barriers for poor cataract surgery uptake among patients with operable cataract in a program of outreach screening and low-cost surgery in rural China. Ophthalmic Epidemiol. (2014) 21:153–60. doi: 10.3109/09286586.2014.903981
19. Alimaw Y, Seid M, Tefera T, Yibekal B. Knowledge about cataract and associated factors among adults in Gondar town, northwest Ethiopia. PLoS ONE. (2019) 14:e0215809. doi: 10.1371/journal.pone.0215809
20. Ye G, Qu B, Shi W, Chen X, Ma P, Zhong Y, et al. Knowledge about benefits and risks of undergoing cataract surgery among cataract patients in Southern China. Int Ophthalmol. (2020) 40:2889–99. doi: 10.1007/s10792-020-01473-7
21. Farooqui JH, Acharya M, Dave A, Chaku D, Das A, Mathur U. Awareness and knowledge about eye donation and the impact of counselors: a North Indian perspective. J Curr Ophthalmol. (2019) 31:218–9. doi: 10.1016/j.joco.2018.11.001
22. Lau JTF, Lee V, Fan D, Lau M, Michon J. Knowledge about cataract, glaucoma, and age related macular degeneration in the Hong Kong Chinese population. Br J Ophthalmol. (2002) 86:1080–4. doi: 10.1136/bjo.86.10.1080
23. Lan C, Chen Y-H, Chen Y-J, Lee J-J, Kuo H-K, Wu P-C. Outcomes and eye care knowledge in rhegmatogenous retinal detachment patients with a history of laser refractive surgery for myopia. Front Public Health. (2022) 10:895024. doi: 10.3389/fpubh.2022.895024
24. Bing Zhang J-G, Gao, Cheng Pan, Mei Luan, Chen X-M. Awareness and knowledge about cataract, glaucoma, and age-related macular degeneration in Chengdu, China. Guoji Yanke Zazhi. (2016) 16:397–402. doi: 10.3980/j.issn.1672-5123.2016.3.01
25. Xu Y, He J, Lin S, Zhang B, Zhu J, Resnikoff S, et al. General analysis of factors influencing cataract surgery practice in Shanghai residents. BMC Ophthalmol. (2018) 18:102. doi: 10.1186/s12886-018-0767-5
26. Camparini M, Cassinari P, Ferrigno L, Macaluso C. ETDRS-fast: implementing psychophysical adaptive methods to standardized visual acuity measurement with ETDRS charts. Invest Ophthalmol Vis Sci. (2001) 42:1226–31. Available online at: https://iovs.arvojournals.org/article.aspx?articleid=2162384
27. Kuoppala J, Falck A, Winblad I, Tuulonen A. The Pyhäjärvi cataract study II. Criteria for cataract surgery. Acta Ophthalmol. (2012) 90:327–33. doi: 10.1111/j.1755-3768.2010.01935.x
28. Vashist P, Talwar B, Gogoi M, Maraini G, Camparini M, Ravilla R, et al. Prevalence of cataract in an older population in India the India study of age-related eye disease. Ophthalmology. (2011) 118:272–8.e1. doi: 10.1016/j.ophtha.2010.05.020
29. Feder RS, Olsen TW, Prum BE, Summers CG, Olson RJ, Williams RD, et al. Comprehensive adult medical eye evaluation preferred practice pattern guidelines. Ophthalmology. (2016) 123:P209–36. doi: 10.1016/j.ophtha.2015.10.047
30. Suman S, Thapa, Rosa V D, Berg, Shankar Khanal, Indira Paudyal, Ger H M B V Rens. Prevalence of visual impairment, cataract surgery and awareness of cataract and glaucoma in Bhaktapur district of Nepal: the Bhaktapur Glaucoma Study. BMC Ophthalmol. (2011) 11:1–9. doi: 10.1186/1471-2415-11-2
31. Livingston PM, McCarty CA, Taylor HR. Knowledge, attitudes, and self care practices associated with age related eye disease in Australia. Br J Ophthalmol. (1998) 82:780–5. doi: 10.1136/bjo.82.7.780
Keywords: cataract, cataract knowledge, eye care utilization, rural China, elder
Citation: Du K, Guan H, Zhang Y, Ding Y and Wang D (2022) Knowledge of cataracts and eye care utilization among adults aged 50 and above in rural Western China. Front. Public Health 10:1034314. doi: 10.3389/fpubh.2022.1034314
Received: 01 September 2022; Accepted: 03 October 2022;
Published: 15 November 2022.
Edited by:
Madhan Balasubramanian, Flinders University, AustraliaReviewed by:
Zicheng Cao, Shantou University, ChinaWinfried Amoaku, University of Nottingham, United Kingdom
Copyright © 2022 Du, Guan, Zhang, Ding and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongyu Guan, aG9uZ3l1Z3VhbjA2MjFAZ21haWwuY29t
 Kang Du
Kang Du Hongyu Guan
Hongyu Guan Yunyun Zhang
Yunyun Zhang Yuxiu Ding
Yuxiu Ding Decai Wang
Decai Wang