- 1Department of Pharmacy, School of Health Sciences, University of Zambia, Lusaka, Zambia
- 2Department of Public Health, Michael Chilufya Sata School of Medicine, Copperbelt University, Ndola, Zambia
- 3Clinical Research Department, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 4Department of Pharmacology and Pharmacognosy, School of Pharmacy, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya
- 5Department of Pharmaceutical Sciences, School of Pharmacy, Sefako Makgatho Health Sciences University, Pretoria, South Africa
Background: The COVID-19 pandemic led to the disruption of physical classes for university students globally, as large gatherings fuelled the transmission of the virus. In the efforts to mitigate its transmission and return to normality, prevention measures, including vaccination, have been encouraged. Therefore, it is critical to understand the knowledge and practices of students regarding COVID-19. This study assessed the knowledge and practices toward COVID-19 among healthcare students at the University of Zambia.
Materials and methods: This questionnaire-based cross-sectional study was carried out from August 2021 to October 2021 among 478 healthcare students (pharmacy, physiotherapy, nursing, biomedical, medicine, and radiography). We used a previously validated questionnaire to measure knowledge and practice. The predictors of knowledge and practices were assessed using logistic regression with robust estimation of standard errors. Statistical analysis was conducted using Stata/BE version 17.0.
Results: Of the 478 respondents, 243 (50.8%) were females. A larger proportion, 175 (36.6%) were in Pharmacy training, and 156 (32.6%) were in their fifth year of study. The overall mean knowledge score of the participants was 87.9 (SD = 16.1), being higher at 89.6 (SD = 14.3) among medical students and the lowest at 86.7 (SD = 17.1) among Pharmacy students, although this was statistically non-significant (p = 0.488). The overall mean practice score was 60.0 (SD = 24.7), being significantly higher at 63.5 (23.4) among nursing, physiotherapy and environmental students compared to other students (p = 0.048). In multivariable analysis, the participant training program was non-significantly associated with knowledge and practice toward COVID-19. However, increased age (AOR = 1.09, 95% CI: 1.01–1.117) and residing in urban areas (AOR = 1.79, 95% CI: 1.07–3.01) than in rural areas were associated with higher odds of good practice toward COVID-19.
Conclusion: The healthcare students generally showed good knowledge levels and poor practices toward COVID-19. Further, there was no evidence of a difference in knowledge of COVID-19 among healthcare students. These findings suggest the need for implementation strategies to be centered on improving the practices of students toward COVID-19.
Introduction
Pandemics like the coronavirus disease 2019 (COVID-19) can potentially disrupt university education activities (1–3). This may eventually affect students' academic performance and social life (4–6). In addition, evidence has suggested that COVID-19 affected many people's mental health, including university students (7–10). This could be attributed to increased transmission and spread of the disease among students (11–14). Therefore, to curb disease transmission, face-to-face learning was suspended in many learning institutions globally (15–19).
The knowledge of individuals concerning COVID-19, its transmission, spread, and clinical features is significant in developing prevention strategies (20–22). Critical aspects of COVID-19-related knowledge required to illicit good practices have been postulated, including spread, symptoms, transmission, protective measures and vaccines (23). As future health care service providers and disease prevention specialists, students of health-related disciplines are expected to demonstrate appreciable knowledge in COVID-19 etiology, transmission, treatment, prevention and control (20). Variable findings have been reported, including high knowledge among students in India (24, 25) and Vietnam (26). Conversely, low knowledge levels were observed in Poland and China (27, 28). A study in sub-Saharan Africa reported good knowledge among students in selected institutions (29).
Evidence has demonstrated that individuals who adhere to preventive measures such as wearing face masks tend to have lower risks of contracting COVID-19 (30). In addition, practicing adequate hand hygiene has also been reported to reduce the transmission of the virus (31–33). Most people frequently touch their eyes, nose, and mouth when such acts may cause much harm. The practice of handwashing with running water and using alcohol-based handsanitisers can significantly reduce microbial contamination (32, 34). Moreover, studies have indicated that social distancing, avoiding crowded places, wearing masks, and hand hygiene reduce the probability of contracting COVID-19 and other respiratory diseases (35, 36). Thus, good practices toward COVID-19 prevention measures may help reduce the transmission of the virus and the spread of the disease (21, 22, 37, 38).
A milestone in the fight against COVID-19 has been developing, deploying and administering vaccines (39–42). Vaccines are critical in promoting the immune system to fight against infections (39). However, due to their accelerated development, there have been inconsistencies in the acceptance of the vaccine across populations (43–45). For instance, among the general population, vaccine acceptance was 83% in Denmark (46), 64.5% in Malaysia (47), 63.4% in Lebanon (48), 47% in France and Hungary (46), and 33.4% in Zambia (49). Similarly, inconsistencies in vaccine acceptance have been reported among healthcare workers (HCWs) including94.9% in Singapore (50), 89.2% in the United Arab Emirates (51), 74.5% in Ethiopia (52), 63.8% in Sudan (53), and 45.6% in Egypt (54). Acceptance of COVID-19 vaccine among students was 87.4% in China (55), 55.8% in Sudan (56), 54% in the United States, 27.1% in Ethiopia (57), and 24.5% in Zambia (58). These variations in vaccine acceptance have been due to concerns regarding the safety and effectiveness of vaccines (44, 59–61). Vaccine beliefs, myths and misinformation have also contributed to increased vaccine hesitancy (62, 63). Alongside this, vaccines' high cost and availability reduce their overall uptake (44). Therefore, targeted interventions must tackle vaccine hesitancy and improve acceptance and uptake across all populations (61–63).
In Zambia, COVID-19 led to increased morbidity and mortality with some deaths being reported as brought in dead (64–66). Alongside this, there has been low adherence to the COVID-19 prevention measures which could promote spread of the disease (20, 67). Additionally, many factors have been reported to affect the adherence to the COVID-19 prevention measure viz a viz limited information on COVID-19, travel patterns and social movements, negative attitudes toward COVID-19 guidelines, structural and socioeconomic factors (67). Therefore, addressing these factors is critical in reducing the spread of the disease.
The fight against COVID-19 requires a collaborative approach among all healthcare providers, including healthcare students, to provide optimum patient care (26). Furthermore, healthcare students are the future healthcare workers and will be responsible for providing disease prevention strategies to the public. Consequently, it is crucial to determine health-related students' level of knowledge about COVID-19 and associated prevention practices. Unfortunately, in many countries, including Zambia, there is a dearth of information regarding the knowledge and practices of university students concerning COVID-19. As such, this study assessed the knowledge and attitudes of healthcare students regarding COVID-19 at the University of Zambia in Lusaka, Zambia.
Materials and methods
Study design, setting and population
This cross-sectional study was conducted among healthcare students (biomedical sciences, medicine, nursing, pharmacy, physiotherapy, and radiography) from August 2021 to October 2021. The students were enrolled at the University of Zambia, Ridgeway medical campus in Lusaka. As the leading university in training healthcare professionals in Zambia; it was a good starting point to understand the knowledge and practices of students regarding COVID-19. To be part of the study, a student had to be enrolled in human healthcare programs at the University of Zambia and willing to respond to the questionnaire after giving consent.
Sample size and sampling technique
The sample size was estimated using Cochrane's formula;
With no previous study done in this setting based on the literature search, a conservative expected proportion of 50%, 95% confidence level, 5% margin of error, 10% non-response or incomplete response, and desired design effect of 1.2 was used to determine the sample size. A minimum of 423 sample size was determined to achieve a minimum power of 80% to detect the difference in knowledge by the program of study. The sampling procedure had three steps. Firstly, we grouped the students into blocks based on their program of study (biomedical sciences, medicine, nursing, pharmacy, physiotherapy, and radiography). Secondly, we stratified the students according to their year of study. All potential participants were identified using the class registered for all registered students. Finally, a simple random sampling technique (using computer-generated random numbers without replacement) was used to select a random sample of students from each program of study.
Data collection tool
Data collection was conducted using previously validated questionnaire from a similar study (68). The questionnaire was reviewed by two experts from the University of Zambia. The resultant questionnaire had three sections comprising seven questions on socio-demographics of participants, six questions on knowledge and four questions on practices toward COVID-19. Each correct knowledge question was assigned a score of one and a wrong response was assigned a zero. The questions on practice were assigned a score of one for good practices, otherwise, a zero was assigned. A Cronbach's alpha score of >0.7 was acceptable and used to determine the internal consistency of the questions. The self-administered questionnaire was piloted using 30 undergraduate healthcare students, but the pilot study findings were not part of the analyzed data in the main survey. The piloting of the data collection tool revealed that each participant would take between 10 and 20 min to respond to the questions. Data collection was conducted by three data collectors trained in the data collection process. To increase the chances of meeting the desired sample size and fears of non-response due to the COVID-19 spread, we distributed 600 questionnaires to the potential participants.
Study measures
The main outcome measures were knowledge and practice measured on a binary scale (coded as yes = 1, no = 0). For each scale (knowledge and attitude scales) the item scores were summed to create a percentage score. The continuous scores for knowledge and practice were categorized based on Bloom's cut-off value (60% or less as poor knowledge and practice, >60% as good knowledge and practice). The primary predictor was the student's training program (pharmacy, medicine, biomedical sciences, nursing, environmental health, radiography). Other variables measured were age (years), sex (male, female), residence (urban, rural), marital status (married, unmarried) year of study, and religion.
Statistical analysis
All analyses took into account the clustering of students within programs of study through the robust estimation of standard errors, which also accounted for the stratification by year of study. We used both descriptive and analytical statistical methods. The Q-Q plots were used to assess the normality of continuous data. The Analysis of Variance (ANOVA) test was used to evaluate the differences in the overall scores among the healthcare students. To assess pairwise comparison, ANOVA was followed by the Bonferroni post-hoc test where appropriate.
Separate logistic regression models with robust estimation of standard errors were fitted with knowledge and practice as outcome variables. The adjustment variables were chosen based on p-values from the univariable logistic regression models with knowledge and practice as outcomes, respectively, using a significance level of 20%. The main estimates were the training program's unadjusted odds ratios (UOR) and adjusted odds ratios (AOR). While adjusting for potential confounders, adjusted odds ratios and 95% confidence intervals were estimated to evaluate the type of training program with a report of good knowledge and practice toward COVID-19. Interactions between the training program and significant modifying variables were assessed, and none reached any statistical significance. We used Stata/BE version 17.0 (Stata Corp., College Station, Texas, USA) for analysis, and significance level was set at 5%.
Ethical considerations
This study was approved by the University of Zambia Health Sciences Research Ethics Committee (UNZAHSREC) with protocol ID of 202112030049. Participation was voluntarily and confidentiality was observed.
Results
Socio-demographic characteristics of the study participants
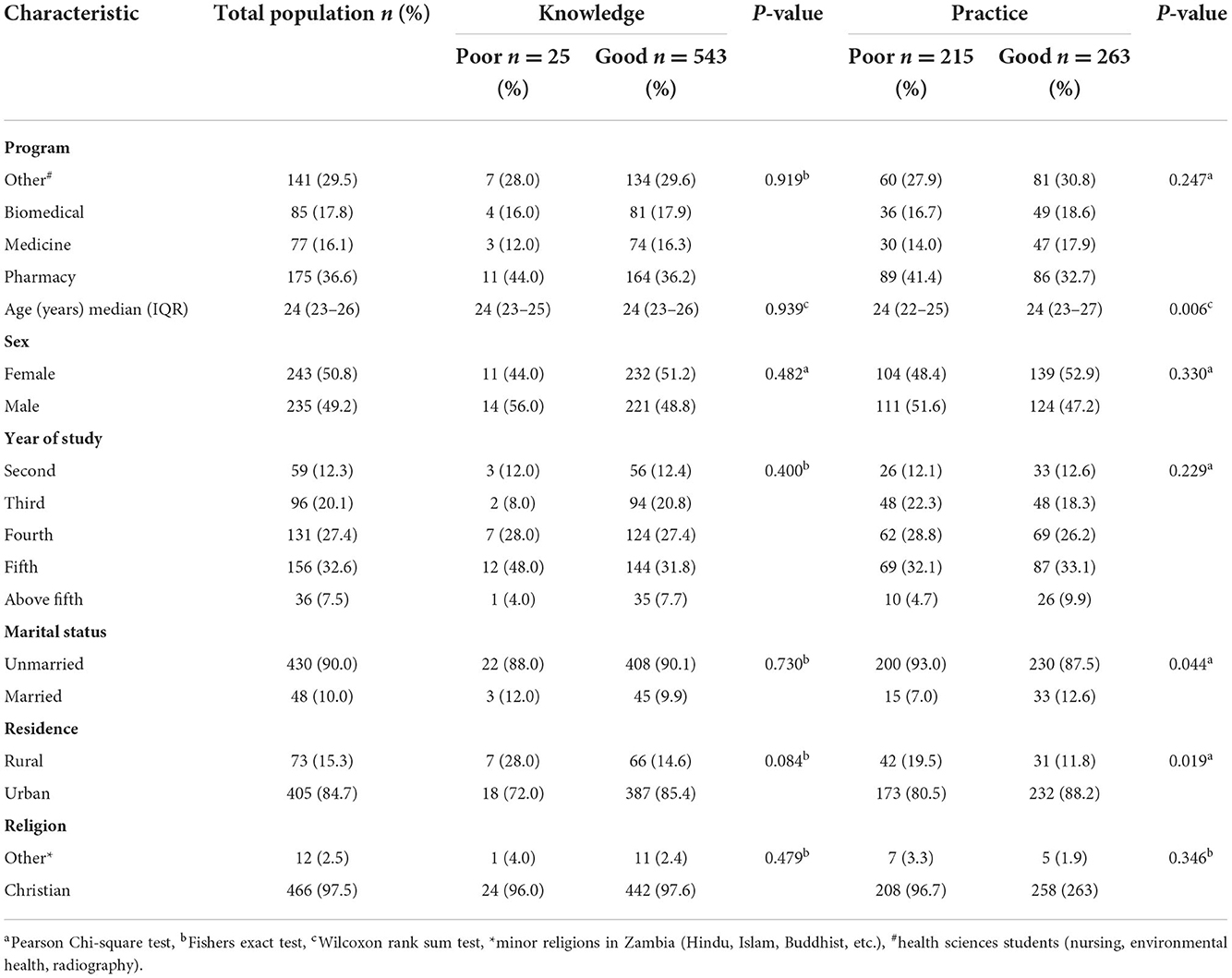
We enrolled 478 respondents with a median age of 24 years (IQR, 23–26), of whom 243(50.8%) were females. Approximately two-in-five 175(36.6%) of the respondents were in Pharmacy training and 156(32.6%) were in the fifth year of study. Nearly all 466(97.5%) were of Christian faith, and 430(90.0%) were not married. Furthermore, the majority, 405(84.7%), resided in the urban parts of Zambia. There was no evidence suggesting that knowledge (p = 0.919) and practice (0.247) toward COVID-19 differed among the students. However, there was a statistically significant difference in median age, residential area and marital status between those respondents who reported a good attitude toward COVID-19 and those who did not (Table 1).
Knowledge of COVID-19 among healthcare students
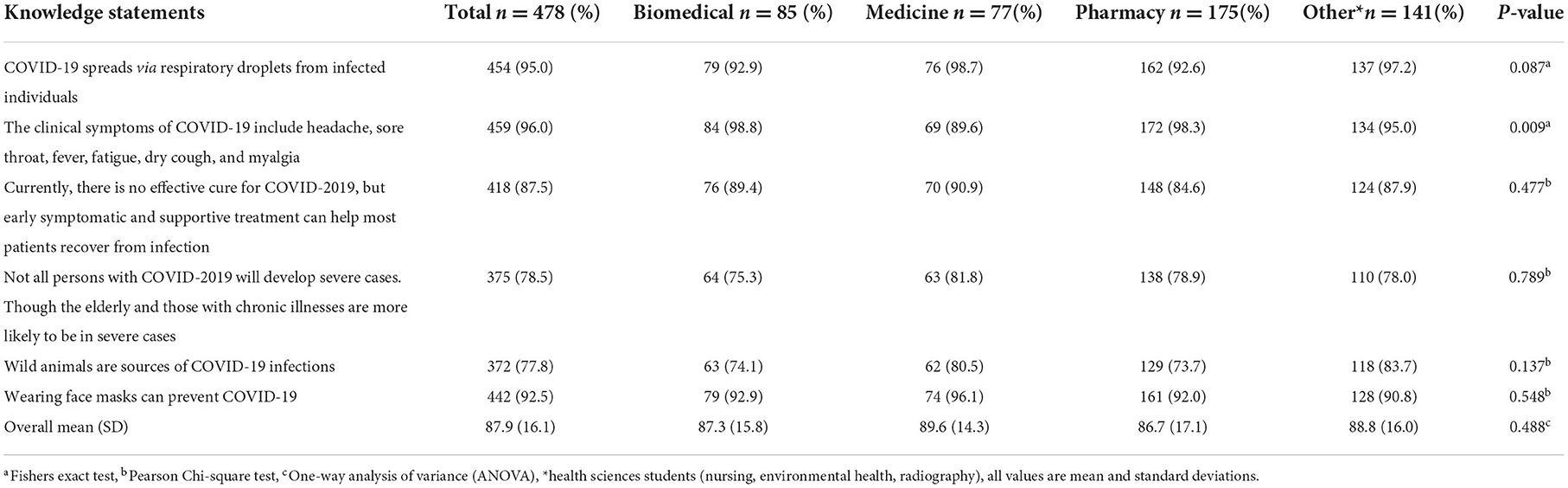
The knowledge statements and percentage of correct responses from the participating healthcare students are shown in Table 2. Overall, the mean knowledge score of the participants was 87.9 (SD = 16.1), the highest score 89.6 (SD = 14.3) arising from medical students and the lowest 86.7 (SD = 17.1) from Pharmacy students, although this was statistically non-significant (p = 0.488). The most correctly answered question among the participants was on the clinical symptoms of COVID-19 infection (96%), and the least was on whether eating or contacting wild animals would result in infection with COVID-19 (77.8%). When different questions on knowledge of COVID-19 were compared among the participating healthcare students, a significant difference was found with a question on the clinical symptoms of COVID-19 (p = 0.009).
Practice toward COVID-19 among healthcare students
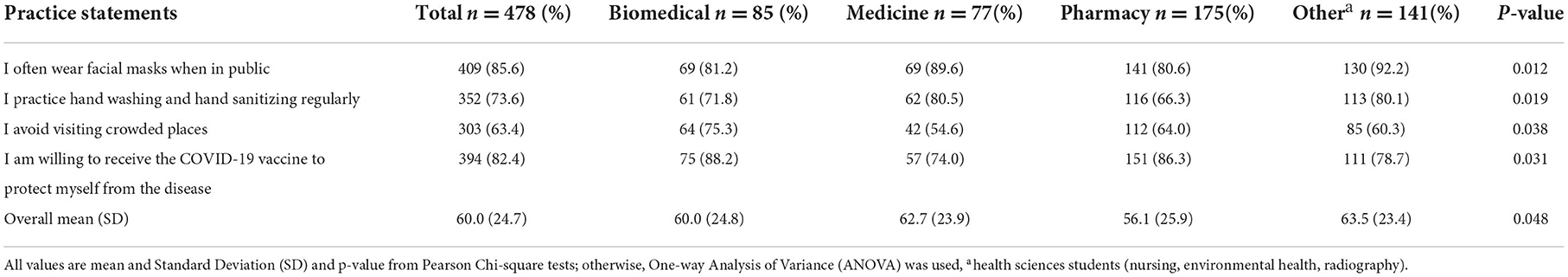
The practice statements and percentage of correct responses from the participating healthcare students are shown in Table 3. Overall, the mean practice score of the participants was 60.0 (SD = 24.7), being significantly higher at 63.5 (SD = 23.4) among other students (nursing, physiotherapy and environmental health students) compared to biomedical, medicine and pharmacy students (p = 0.048). Most 409 (85.6%) students reported wearing facial masks often when in public. On the other hand, the majority, 303 (63.4%) reported that they did not avoid visiting crowded places. When study programs were compared, a statistically significant difference was observed across all practice questions. When different questions on practice toward COVID-19 were compared among the participating healthcare students, a significant difference was found with all the questions.
Factors associated with knowledge and practice toward COVID-19
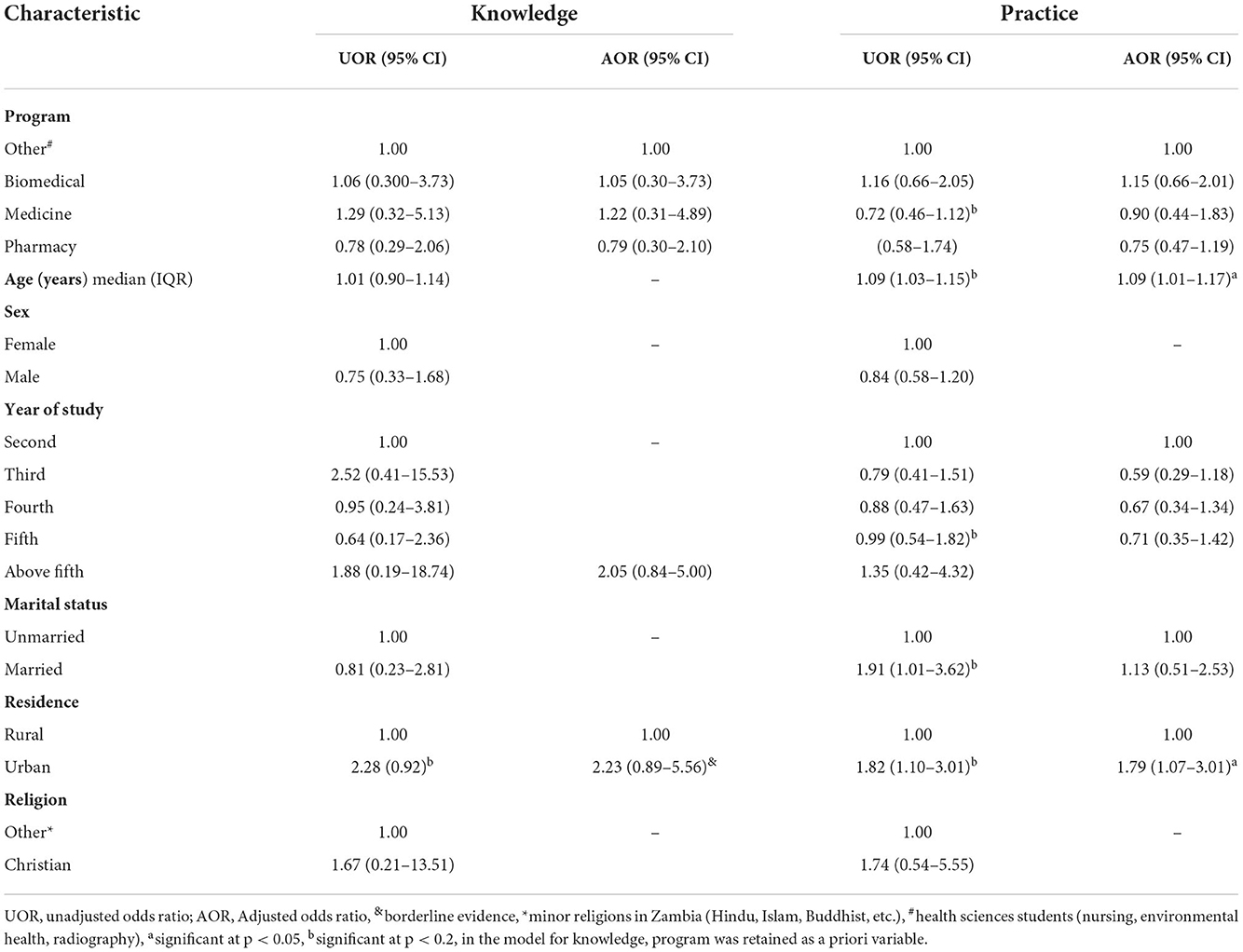
The univariable and multivariable results from a logistic regression analysis are depicted in Table 4. The univariable analysis showed no association between participants' training program, practice, and knowledge of COVID-19. Multivariable analysis was further used to evaluate participants' training program while adjusting for potential confounders. In multivariable analysis, the participant training program remained non-significantly associated with knowledge and practice toward COVID-19. However, age and residence (Urban compared to Rural) were positively associated with practice toward COVID-19. A unit increase in the participant's age was associated with higher odds of good practice toward COVID-19 (AOR = 1.09, 95% CI: 1.01–1.117). In addition, participants who resided in urban areas were more likely to have good practices toward COVID-19 (AOR = 1.79, 95% CI: 1.07–3.01) than those who resided in rural areas.
Discussion
We believe this is the first comprehensive study on knowledge and practices among healthcare students in Zambia to provide baseline data regarding COVID-19 in tertiary learning institutions. In addition, provide key areas to inform future quality improvement efforts and capacity development of COVID-19 response and preventive measures in Zambia. The latter is important as there have been concerns with knowledge and practices regarding COVID-19 among healthcare students in Zambia (20). In the present, overall, we found an average knowledge and attitude score of 89.6 and 60% among healthcare students. Medical students were more knowledgeable about COVID-19 causes, spread, and prevention than other students, while nursing, physiotherapy, and environmental health students reported good practices toward COVID-19 prevention measures than other students. Even though the students' training program was not independently associated with knowledge and practice toward COVID-19, increased age and residing in urban areas (compared to rural) predicted higher odds of good practice toward COVID-19.
The overall healthcare students' knowledge of COVID-19 is consistent with the extant literature (69, 70). For instance, a study in Vietnam found that most students had good knowledge (86.6%) about COVID-19 and the prevention measures (26), similar to findings from Ethiopia (70). However, our findings suggest that the level of knowledge of COVID-19 was not independently associated with students' programs of study, which is contrary to findings from a study done in Poland where significant differences were observed between students of different training programs (27). Although no significant difference was reported regarding knowledge of COVID-19 across study programs in our study, medical students scored higher compared to other study programs. This is similar to what was found in Poland in which medical students had better knowledge of COVID-19 compared to other students from other programs (27). These findings could be attributed to the fact that medical students are exposed to clinical practice early and attend several hospital meetings. Nevertheless, the findings are encouraging as they indicate that future healthcare workers have sufficient knowledge of COVID-19 which is key in developing preventive measures for this pandemic.
The participants in this study were knowledgeable about the spread of the disease, clinical features, treatment, predisposed individuals to severe disease, and wearing face masks. These findings corroborate reports from Iran in which students had good knowledge regarding COVID-19 transmission and spread, symptoms, and wearing face masks (71). This knowledge, however, should be enhanced by providing students with information regarding the proper use and different types of facemasks.
The current study highlighted the poor practices of students regarding COVID-19, similar to findings reported in studies conducted among university students (13, 69, 70, 72). For instance, a study in Indonesia reported an overall practice of 51.5% among university students (69), in line with findings from Ethiopia (70). Most participants reported wearing facemasks in public, which corroborate findings from other studies (69, 73). However, the current findings are higher than those reported by Kateule and others in an observational study where 24% of the participants wore masks in Lusaka district and 27% wore masks in Mansa district of Zambia (74). These differences could be attributed to differences in study designs and socio-demographic characteristics of study participants. Therefore, wearing face masks during outbreaks of respiratory infections should be promoted as a public health disease prevention and control strategy.
Overall, most participants in this study reported handwashing and sanitizing regularly. However, the percentage of compliance was lower than those reported in 10 countries in Africa through a multinational survey (75). While avoiding crowded places is a key COVID-19 intervention strategy, it was observed in our study that there was less inclination to avoid crowded places than what was reported in a similar study done in the Netherlands (76). The majority (82.5%) of participants in this study were willing to receive the COVID-19 vaccine, which was identical to observations reported in Lebanon (77), Bangladesh (78), China (55), and the Philippines (79). It is envisaged that increased vaccine acceptance may help increase vaccinations across the globe (80). An earlier study conducted immediately after vaccine deployment in Zambia reported a very low vaccine acceptance (24.5%) among pharmacy students (58). This could have been due to inadequate and negative information about the vaccines. Other studies have reported low vaccine acceptance among students with low vaccine acceptance attributed to misinformation, myths, and concerns about the adverse effects and effectiveness of vaccines (56, 57, 81–83).
Our study found that older participants observed COVID-19 prevention practices much better than younger participants, despite both groups displaying comparable levels of knowledge. These findings contrasts those from a study that was conducted among healthcare students in Vietnam whereby the pattern and extent of COVID-19 practices could not be distinguished along the age of the study participants (26). While it is unclear why age might have contributed to the discrepancy in the students' COVID-19-related safe practices, we posit that older age is generally associated with more responsible health behaviors. Moreover, those students who resided in urban areas tended to uphold safe hygiene and other preventive practices toward controlling possible COVID-19 transmission, compared to those who identified themselves as living in rural areas. Similar observations were reported in a survey among students in Japan where students who lived in the capital city scored highly compared to others, in following national and international measures recommended to mitigate against the spread of COVID-19 (68). It is conceivable that public health outreach programs that rely heavily on social media and other digital communication platforms are central to the observed differences. There is generally better penetration and access to information among the urban dwelling residents than rural residents. Also, in most cases, initial and severe cases of COVID-19 were reported in urban areas. This could have made the urban residents much more aware and conscious of the public health implications of the uncontrolled spread of the disease. Interestingly, rural-dwelling students in another African set-up in Ethiopia were twice as likely to comply with recommended public health measures to avert COVID-19 transmission, compared to their urban counterparts (84). Potential socioeconomic differences, the impact of the public health campaign strategies, and outreach that the two countries may have mounted, could be contributing factors to this observation.
Surprisingly, the reported good knowledge regarding COVID-19 across all students in our survey was at variance with the practices. Similar findings were reported from Ethiopia in which good knowledge did not translate into good practices toward COVID-19 (70). These findings may require multiple strategies to be implemented when disseminating COVID-19 information to college and university students. Conversely, a study in the Kingdom of Bhutan among college students found good knowledge that translated into good practices toward COVID-19 (85). Similarly, a recent study in Ethiopia reported good knowledge and good practices regarding COVID-19 (86). The good knowledge and practices reported in other studies could be due to the increased dissemination of educational information regarding COVID-19 by the governments and related stakeholders. Our findings and those from similar surveys may be used to develop strategies that limit disease spread.
This study had some limitations. First, it was conducted at one institution of higher learning, therefore, the findings may not be generalized to all the universities across the country. Secondly, the study focused on healthcare students, hence, the findings may not be generalized to non-healthcare students.
Conclusion
The study found good knowledge of COVID-19 among university students. However, the overall poor practices are of much concern and require urgent attention from authorities. Despite the students having good knowledge, the poor practices in some infection prevention measures call for improved dissemination of COVID-19 information in universities and across the youth population. The findings from the study are hypothesis-generating and can guide implementation strategies aimed at improving the practices toward COVID-19.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
The study was conceptualized by SM and NN. Data collection was done by SM, NN, and CNH. Data analysis was done by SM and MM. Intellectual content of the manuscript was done by SM, MM, CNH, SKM, VD, MB, RLM, and BAW. Writing of the first draft was done by SM. All authors participated in the writing of the final manuscript, reviewed, and approved the final version of the manuscript.
Acknowledgments
The authors would like to acknowledge the students who took part in the study. In addition, they are grateful to the University of Zambia Ridgeway Campus (UNZARWC) administration for allowing them to collect data, indicating their full support and promotion of research activities in the various schools. They are also grateful to the University of Zambia e-library for providing access to most of the articles used in this publication. MM would like to acknowledge that some of his time was supported by the UNC-UNZA-Wits Partnership for HIV and Women's Reproductive Health which was funded by the U.S. National Institute's Health (Grant Number: D43 TW010558). The authors would also like to acknowledge the support of APC from Sefako Makgatho Health Sciences University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1028312/full#supplementary-material
References
1. d'Orville H. COVID-19 causes unprecedented educational disruption: is there a road towards a new normal? Prospects. (2020) 49:11–15. doi: 10.1007/s11125-020-09475-0
2. Harmey S, Moss G. Learning disruption or learning loss: using evidence from unplanned closures to inform returning to school after COVID-19. Educ Rev. (2021) 1–20. doi: 10.1080/00131911.2021.1966389
3. Debbarma I, Durai T. Educational disruption: impact of COVID-19 on students from the Northeast states of India. Child Youth Serv Rev. (2021) 120:105769. doi: 10.1016/j.childyouth.2020.105769
4. Ivanec TP. The Lack of academic social interactions and students' learning difficulties during COVID-19 faculty lockdowns in croatia: the mediating role of the perceived sense of life disruption caused by the pandemic and the adjustment to online studying. Soc Sci. (2022) 11:42. doi: 10.3390/socsci11020042
5. Al-Maskari A, Al-Riyami T, Kunjumuhammed SK. Students academic and social concerns during COVID-19 pandemic. Educ Inf Technol. (2022) 27:1–21. doi: 10.1007/s10639-021-10592-2
6. Elmer T, Mepham K, Stadtfeld C. Students under lockdown: comparisons of students' social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE. (2020) 15:e0236337. doi: 10.1371/journal.pone.0236337
7. Allen R, Kannangara C, Vyas M, Carson J. European university students' mental health during COVID-19: exploring attitudes towards COVID-19 and governmental response. Curr Psychol. (2022) 1:1–14. doi: 10.1007/s12144-022-02854-0
8. Chen T, Lucock M. The mental health of university students during the COVID-19 pandemic: an online survey in the UK. PLoS One. (2022) 17:e0262562. doi: 10.1371/journal.pone.0262562
9. Irfan M, Shahudin F, Hooper VJ, Akram W, Abdul Ghani RB. The psychological impact of coronavirus on university students and its socio-economic determinants in Malaysia. Inquiry. (2021) 58:1–7. doi: 10.1177/00469580211056217
10. Mudenda S, Mukosha M, Mwila C, Saleem Z, Kalungia AC, Munkombwe D, et al. Impact of the coronavirus disease on the mental health and physical activity of pharmacy students at the University of Zambia: a cross-sectional study. Int J Basic Clin Pharmacol. (2021) 10:324. doi: 10.18203/2319-2003.ijbcp20211010
11. Llupià A, Borràs-Santos A, Guinovart C, Utzet M, Moriña D, Puig J. SARS-CoV-2 transmission in students of public schools of Catalonia (Spain) after a month of reopening. PLoS ONE. (2021) 16:e0251593. doi: 10.1371/journal.pone.0251593
12. Bani Hani A, Alaridah N, Abu Abeeleh M, Shatarat A, Rayyan R, Kamal A, et al. Medical students and risk of COVID-19 infection: a descriptive cross-sectional study from the University of Jordan. Ann Med Surg. (2021) 70:102775. doi: 10.1016/j.amsu.2021.102775
13. Yesuf M, Abdu M. Knowledge, attitude, prevention practice, and associated factors toward COVID-19 among preparatory school students in Southwest Ethiopia, 2021. PLoS ONE. (2022) 17:e0262907. doi: 10.1371/journal.pone.0262907
14. Brooks-Pollock E, Christensen H, Trickey A, Hemani G, Nixon E, Thomas AC, et al. High COVID-19 transmission potential associated with re-opening universities can be mitigated with layered interventions. Nat Commun. (2021) 12:1–10. doi: 10.1038/s41467-021-25169-3
15. Sahu P. Closure of universities due to Coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. (2020) 12:4. doi: 10.7759/cureus.7541
16. Mudenda S, Zulu A, Phiri MN, Ngazimbi M, Mufwambi W, Kasanga M, et al. Impact of Coronavirus disease 2019 (COVID-19) on college and university students: a global health and education problem. Aquademia. (2020) 4:ep20026. doi: 10.29333/aquademia/8494
17. Walke HT, Honein MA, Redfield RR. Preventing and responding to COVID-19 on college campuses. J Am Med Assoc. (2020) 324:1727–8. doi: 10.1001/jama.2020.20027
18. Akhter S, Robbins M, Curtis P, Hinshaw B, Wells EM. Online survey of university students' perception, awareness and adherence to COVID-19 prevention measures. BMC Public Health. (2022) 22:1–9. doi: 10.1186/s12889-022-13356-w
19. Alonso S, Català M, López D, Álvarez-Lacalle E, Jordan I, García-García JJ, et al. Individual prevention and containment measures in schools in Catalonia, Spain, and community transmission of SARS-CoV-2 after school re-opening. PLoS ONE. (2022) 17:e0263741. doi: 10.1371/journal.pone.0263741
20. Mudenda S, Botha M, Mukosha M, Daka V, Chileshe M, Mwila K, et al. Knowledge and attitudes towards COVID-19 prevention measures among residents of Lusaka district in Zambia. Aquademia. (2022) 6:ep22005. doi: 10.21601/aquademia/12210
21. Kundu S, Al Banna MH, Sayeed A, Begum MR, Brazendale K, Hasan MT, et al. Knowledge, attitudes, and preventive practices toward the COVID-19 pandemic: an online survey among Bangladeshi residents. J Public Heal. (2021) 1–15. doi: 10.1007/s10389-021-01636-5
22. Ngwewondo A, Nkengazong L, Ambe LA, Ebogo JT, Mba FM, Goni HO, et al. Knowledge, attitudes, practices of/towards COVID 19 preventive measures and symptoms: a cross-sectional study during the exponential rise of the outbreak in Cameroon. PLoS Negl Trop Dis. (2020) 14:e0008700. doi: 10.1371/journal.pntd.0008700
23. Chawe A, Mfune RL, Syapiila PM, Zimba SD, Vlahakis PA, Mwale S, et al. Knowledge, attitude and practices of COVID-19 among medical laboratory professionals in Zambia. Afr J Lab Med. (2021) 10:2225–2002. doi: 10.4102/ajlm.v10i1.1403
24. Modi PD, Nair G, Uppe A, Modi J, Tuppekar B, Gharpure AS, et al. COVID-19 awareness among healthcare students and professionals in Mumbai metropolitan region: a questionnaire-based survey. Cureus. (2020) 12:e7514. doi: 10.7759/cureus.7514
25. Prathibha KM, Harsha SS, Sundararajan P. Knowledge, Preventive behaviour and risk perception about COVID-19 in health care professional students. Biomed Pharmacol J. (2022) 15:1069–78. doi: 10.13005/bpj/2442
26. Le An P, Huynh G, Nguyen H, Pham B, Nguyen T, Tran T, et al. Knowledge, attitude, and practice towards COVID-19 among healthcare students in Vietnam. Infect Drug Resist. (2021) 14:3405–13. doi: 10.2147/IDR.S328677
27. Sarzyńska K, Czwojdziński E, Kuzniarski A, Rayad S, Piwowar A, Jankowska-Polańska B. Medical students' knowledge about COVID-19 and evaluation of the effectiveness of the applied preventive strategies. Arch Public Heal. (2022) 80:1–13. doi: 10.1186/s13690-022-00873-8
28. Zhang J, Yin Y, Dean J, Zhang X, Zhang Y, Wang J, et al. Knowledge, attitude, and practice survey of COVID-19 among healthcare students during the COVID-19 outbreak in China: an online cross-sectional survey. Front Public Heal. (2021) 9:742314. doi: 10.3389/fpubh.2021.742314
29. Adejumo PO, Nawagi F, Kolawole IO, Ismail MR, Mukalay AW, Nabirye RC, et al. Knowledge, preparedness, and attitude towards COVID-19 among health profession students in Sub-Saharan Africa: a cross-sectional survey. IJID Reg. (2021) 1:150–8. doi: 10.1016/j.ijregi.2021.10.010
30. Ayn Umaisara Mohamad N, Mohamed NA, Hasan ZIA, Umar NS, Sanip S, Rani MDM. Knowledge, attitude and practice (KAP) towards COVID-19 prevention among Malaysian adults during the period of movement control order (MCO): An online cross-sectional survey. Int J Res Pharm Sci. (2020) 11:1458–68. doi: 10.26452/ijrps.v11iSPL1.3693
31. Szczuka Z, Abraham C, Baban A, Brooks S, Cipolletta S, Danso E, et al. The trajectory of COVID-19 pandemic and handwashing adherence: findings from 14 countries. BMC Public Health. (2021) 21:1–13. doi: 10.1186/s12889-021-11822-5
32. Hirose R, Ikegaya H, Naito Y, Watanabe N, Yoshida T, Bandou R, et al. Survival of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and influenza virus on human skin: importance of hand hygiene in coronavirus disease 2019 (COVID-19). Clin Infect Dis. (2021) 73:e4329–35. doi: 10.1093/cid/ciaa1517
33. Alzyood M, Jackson D, Aveyard H, Brooke J. COVID-19 reinforces the importance of handwashing. J Clin Nurs. (2020) 29:2760–1. doi: 10.1111/jocn.15313
34. Hayward AC, Beale S, Johnson AM, Zambon M, Fragaszy EB. Hand hygiene practices and the risk of human Coronavirus infections in a UK community cohort. Wellcome Open Res. (2021) 5:98. doi: 10.12688/wellcomeopenres.15796.2
35. Dwipayanti NMU, Lubis DS, Harjana NPA. Public perception and hand hygiene behavior during COVID-19 pandemic in Indonesia. Front Public Heal. (2021) 9:621800. doi: 10.3389/fpubh.2021.621800
36. Chiu NC, Chi H, Tai YL, Peng CC, Tseng CY, Chen CC, et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: retrospective national epidemiological surveillance study. J Med Internet Res. (2020) 22:e21257. doi: 10.2196/21257
37. Al-Hanawi MK, Angawi K, Alshareef N, Qattan AMN, Helmy HZ, Abudawood Y, et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Front Public Heal. (2020) 8:217. doi: 10.3389/fpubh.2020.00217
38. Lee M, Kang BA, You M. Knowledge, attitudes, and practices (KAP) toward COVID-19: a cross-sectional study in South Korea. BMC Public Health. (2021) 21:1–10. doi: 10.1186/s12889-021-10285-y
39. Graham BS. Rapid COVID-19 vaccine development. Science. (2020) 368:945–6. doi: 10.1126/science.abb8923
40. Li M, Wang H, Tian L, Pang Z, Yang Q, Huang T, et al. COVID-19 vaccine development: milestones, lessons and prospects. Signal Transduct Target Ther. (2022) 7:1–32. doi: 10.1038/s41392-022-00996-y
41. Carneiro DC, Sousa JD, Monteiro-Cunha JP. The COVID-19 vaccine development: a pandemic paradigm. Virus Res. (2021) 301:198454. doi: 10.1016/j.virusres.2021.198454
42. Li Y-D, Chi W-Y, Su J-H, Ferrall L, Hung C-F, Wu T-C. Coronavirus vaccine development: from SARS and MERS to COVID-19. J Biomed Sci. (2020) 27:1–23. doi: 10.1186/s12929-020-00695-2
43. Kashte S, Gulbake A, El-Amin SF, Gupta A. COVID-19 vaccines: rapid development, implications, challenges and future prospects. Hum Cell. (2021) 34:711–33. doi: 10.1007/s13577-021-00512-4
44. Cascini F, Pantovic A, Al-Ajlouni Y, Failla G, Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: a systematic review. EClinicalMedicine. (2021) 40:101113. doi: 10.1016/j.eclinm.2021.101113
45. Ogunleye OO, Godman B, Fadare JO, Mudenda S, Adeoti AO, Yinka-Ogunleye AF, et al. Coronavirus disease 2019 (COVID-19) pandemic across africa: current status of vaccinations and implications for the future. Vaccines. (2022) 10:1553. doi: 10.3390/vaccines10091553
46. Lindholt MF, Jørgensen F, Bor A, Petersen MB. Public acceptance of COVID-19 vaccines: cross-national evidence on levels and individual-level predictors using observational data. BMJ Open. (2021) 11:e048172. doi: 10.1136/bmjopen-2020-048172
47. Mohamed NA, Solehan HM, Mohd Rani MD, Ithnin M, Isahak CIC. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: a web-based survey. PLoS ONE. (2021) 16:e0256110. doi: 10.1371/journal.pone.0256110
48. Hanna P, Issa A, Noujeim Z, Hleyhel M, Saleh N. Assessment of COVID-19 vaccines acceptance in the Lebanese population: a national cross-sectional study. J Pharm Policy Pract. (2022) 15:1–9. doi: 10.1186/s40545-021-00403-x
49. Mudenda S, Hikaambo CN, Daka V, Chileshe M, Mfune RL, Kampamba M, et al. Prevalence and factors associated with COVID-19 vaccine acceptance in Zambia: a web-based cross-sectional study. PAMJ. (2022) 41:112. doi: 10.11604/pamj.2022.41.112.31219
50. Koh SWC, Liow Y, Loh VWK, Liew SJ, Chan YH, Young D. COVID-19 vaccine acceptance and hesitancy among primary healthcare workers in Singapore. BMC Prim Care. (2022) 23:1–9. doi: 10.1186/s12875-022-01693-z
51. AlKetbi LMB, Elharake JA, Memari S, Al Mazrouei SAl, Shehhi BAl, Malik AA, et al. COVID-19 vaccine acceptance among healthcare workers in the United Arab Emirates. IJID Reg. (2021) 1:20–6. doi: 10.1016/j.ijregi.2021.08.003
52. Yilma D, Mohammed R, Abdela SG, Enbiale W, Seifu F, Pareyn M, et al. COVID-19 vaccine acceptability among healthcare workers in Ethiopia: do we practice what we preach? Trop Med Int Heal. (2022) 27:418–25. doi: 10.1111/tmi.13742
53. Yassin EOM, Faroug HAA, Ishaq ZBY, Mustafa MMA, Idris MMA, Widatallah SEK, et al. COVID-19 vaccination acceptance among healthcare staff in Sudan, 2021. J Immunol Res. (2022) 2022:3392667. doi: 10.1155/2022/3392667
54. Sharaf M, Taqa O, Mousa H, Badran A. COVID-19 vaccine acceptance and perceptions among dental teaching staff of a governmental university in Egypt. J Egypt Public Health Assoc. (2022) 97:1–10. doi: 10.1186/s42506-022-00104-6
55. Li S, Gao Z, Zhong M, Yu Z, Li J, Bi H. Chinese university students' awareness and acceptance of the COVID-19 vaccine: a cross-sectional study. Risk Manag Healthc Policy. (2022) 15:845–64. doi: 10.2147/RMHP.S360274
56. Raja SM, Osman ME, Musa AO, Hussien AA, Yusuf K. COVID-19 vaccine acceptance, hesitancy, and associated factors among medical students in Sudan. PLoS ONE. (2022) 17:e0266670. doi: 10.1371/journal.pone.0266670
57. Asres F, Umeta B. COVID-19 vaccines: awareness, attitude and acceptance among undergraduate University students. J Pharm Policy Pract. (2022) 15:32. doi: 10.1186/s40545-021-00397-6
58. Mudenda S, Mukosha M, Hikaambo C, Catharina JC, Fadare J, Kampamba M, et al. Awareness and acceptance of COVID-19 vaccines and associated factors among pharmacy students in Zambia. Malawi Medical J. (2022) 34:1–8. doi: 10.4314/mmj.v34i3
59. Demeke CA, Kifle ZD, Atsbeha BW, Wondmsigegn D, Yimenu DK, Woldeyohanins AE, et al. COVID-19 vaccine hesitancy among health professionals in a tertiary care center at the university of gondar specialized hospital, Ethiopia: a cross-sectional study. SAGE Open Med. (2022) 10:205031212210769. doi: 10.1177/20503121221076991
60. Mudenda S. COVID-19 vaccine acceptability and hesitancy in Africa: implications for addressing vaccine hesitancy. J Biomed Res Environ Sci. (2021) 2:999–1004. doi: 10.37871/jbres1342
61. Mudenda S, Chileshe M, Mukosha M, Hikaambo CN, Banda M, Kampamba M, et al. Zambia's response to the COVID-19 pandemic: exploring lessons, challenges and implications for future policies and strategies. Pharmacol Pharm. (2022) 13:11–33. doi: 10.4236/pp.2022.131002
62. Matenga TFL, Zulu JM, Moonzwe Davis L, Chavula MP. Motivating factors for and barriers to the COVID-19 vaccine uptake: a review of social media data in Zambia. Cogent Public Heal. (2022) 9:2059201. doi: 10.1080/27707571.2022.2059201
63. Steffens MS, Bullivant B, Bolsewicz K, King C, Beard F. Factors influencing COVID-19 vaccine acceptance in high income countries prior to vaccine approval and rollout: a narrative review. Int J Public Health. (2022) 67:9. doi: 10.3389/ijph.2022.1604221
64. Chileshe M, Mulenga D, Mfune RL, Nyirenda TH, Mwanza J, Mukanga B, et al. Increased number of brought-in-dead cases with COVID-19: is it due to poor health-seeking behaviour among the Zambian population? Pan Afr Med J. (2020) 37:136. doi: 10.11604/pamj.2020.37.136.25967
65. Sudden Unexpected Community D. Africa - a medico-legal whole-body autopsy case series. Int J Infect Dis. (2021) 109:160–7. doi: 10.1016/j.ijid.2021.07.001
66. Mwananyanda L, Gill CJ, Macleod W, Kwenda G, Pieciak R, Mupila Z, et al. COVID-19 deaths in Africa: prospective systematic postmortem surveillance study. BMJ. (2021) 372:n334. doi: 10.1136/bmj.n334
67. Sialubanje C, Sitali DC, Mukumbuta N, Liyali L, Sumbwa PI, Kamboyi HK, et al. Perspectives on factors influencing transmission of COVID-19 in Zambia: a qualitative study of health workers and community members. BMJ Open. (2022) 12:e057589. doi: 10.1136/bmjopen-2021-057589
68. Hatabu A, Mao X, Zhou Y, Kawashita N, Wen Z, Ueda M, et al. Knowledge, attitudes, and practices toward COVID-19 among university students in Japan and associated factors: an online cross-sectional survey. PLoS ONE. (2021) 15:e0244350. doi: 10.1371/journal.pone.0244350
69. Adli I, Widyahening IS, Lazarus G, Phowira J, Baihaqi LA, Ariffandi B, et al. Knowledge, attitude, and practice related to the COVID-19 pandemic among undergraduate medical students in Indonesia: a nationwide cross-sectional study. PLoS ONE. (2022) 17:e0262827. doi: 10.1371/journal.pone.0262827
70. Berihun G, Walle Z, Teshome D, Berhanu L, Abebe M, Ademas A, et al. Knowledge, attitude, and preventive practices towards COVID-19 among students of Ethiopian higher education institutions. J Multidiscip Healthc. (2021) 14:2123–36. doi: 10.2147/JMDH.S322495
71. Hatami H, Abbasi-Kangevari M, Malekpour MR, Kolahi AA. Knowledge, attitudes, and safety practices about COVID-19 among high school students in iran during the first wave of the pandemic. Front Public Heal. (2021) 9:680514. doi: 10.3389/fpubh.2021.680514
72. Kumar B, Pinky SD, Nurudden AM. Knowledge, attitudes and practices towards COVID-19 guidelines among students in Bangladesh. Soc Sci Humanit Open. (2021) 4:100194. doi: 10.1016/j.ssaho.2021.100194
73. Wang S, Li LZ, van Antwerpen N, Suparman S, Gayatri M, Sari NP, et al. Hand hygiene and mask-wearing practices during COVID-19 among healthcare workers: Misinformation as a predictor. Am J Trop Med Hyg. (2021) 105:1483–9. doi: 10.4269/ajtmh.21-0463
74. Kateule E, Banda I, Chika M, Tembo E, Akufuna K, Keembe K, et al. Cross-sectional study of face mask use during the COVID-19 pandemic-Lusaka and Mansa Districts, Zambia, December 2020. Pan Afr Med J. (2022) 41:306. doi: 10.11604/pamj.2022.41.306.29854
75. Olapeju B, Hendrickson ZM, Rosen JG, Shattuck D, Storey JD, Krenn S, et al. Trends in handwashing behaviours for COVID-19 prevention: Longitudinal evidence from online surveys in 10 sub-Saharan African countries. PLOS Glob Public Heal. (2021) 1:e0000049. doi: 10.1371/journal.pgph.0000049
76. Stroom M, Eichholtz P, Kok N. Avoiding crowded places during COVID-19: common sense or a complex strategic decision? Front Psychol. (2021) 12:700640. doi: 10.3389/fpsyg.2021.700640
77. Bou Hamdan M, Singh S, Polavarapu M, Jordan TR, Melhem NM. COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiol Infect. (2021) 149:e242. doi: 10.1017/S0950268821002314
78. Kamal AHM, Sarkar T, Khan MM, Roy SK, Khan SH, Hasan SMM, et al. Factors affecting willingness to receive COVID-19 vaccine among adults: a cross-sectional study in Bangladesh. J Health Manag. (2021). doi: 10.1177/09735984211050691
79. Pagador P, Pacleb A, Ormita MJ, Valencia FE, Velasco DH, Josue-Dominguez R. Acceptance of COVID-19 vaccine among unvaccinated filipinos. Int J Med Students. (2022) 10:264–276. doi: 10.5195/ijms.2022.1192
80. Patwary MM, Alam MA, Bardhan M, Disha AS, Haque MZ, Billah SM, et al. COVID-19 vaccine acceptance among low-and lower-middle-income countries: a rapid systematic review and meta-analysis. Vaccines. (2022) 10:427. doi: 10.3390/vaccines10030427
81. Jain L, Vij J, Satapathy P, Chakrapani V, Patro B, Kar SS, et al. Factors influencing COVID-19 vaccination intentions among college students: a cross-sectional study in India. Front Public Heal. (2021) 9:735902. doi: 10.3389/fpubh.2021.735902
82. Ackah BBB, Woo M, Fazal ZA, Stallwood L, Okpani A, Adu PA. COVID-19 vaccine hesitancy in Africa: a scoping review. Glob Heal Res Policy. (2022) 7:21. doi: 10.1186/s41256-022-00255-1
83. Taye BT, Amogne FK, Demisse TL, Zerihun MS, Kitaw TM, Tiguh AE, et al. Coronavirus disease 2019 vaccine acceptance and perceived barriers among university students in northeast Ethiopia: a cross-sectional study. Clin Epidemiol Glob Heal. (2021) 12:2213–3984. doi: 10.1016/j.cegh.2021.100848
84. Angelo AT, Alemayehu DS, Dacho AM. Knowledge, attitudes, and practices toward covid-19 and associated factors among university students in Mizan Tepi University, 2020. Infect Drug Resist. (2021) 14:349–60. doi: 10.2147/IDR.S299576
85. Dorji T, Wangmo K, Yezer, Wangchuk T, Tshokey, Wangdi K. Knowledge, attitude, and practice toward COVID-19 among sherubtse college students in Bhutan: a web-based cross-sectional study. Front Public Heal. (2021) 9:721493. doi: 10.3389/fpubh.2021.721493
Keywords: COVID-19, healthcare students, knowledge, practices, Zambia
Citation: Mudenda S, Ngalande N, Mukosha M, Hikaambo CN, Daka V, Matafwali SK, Banda M, Mfune RL, Mayoka G and Witika BA (2022) Knowledge and practices toward COVID-19 among healthcare students: A cross-sectional study at the University of Zambia. Front. Public Health 10:1028312. doi: 10.3389/fpubh.2022.1028312
Received: 25 August 2022; Accepted: 11 November 2022;
Published: 30 November 2022.
Edited by:
Zhongwei Huang, Lanzhou University, ChinaReviewed by:
Zhiguo Liu, Chinese Center for Disease Control and Prevention, ChinaElisabetta Pupillo, Mario Negri Institute for Pharmacological Research (IRCCS), Italy
Copyright © 2022 Mudenda, Ngalande, Mukosha, Hikaambo, Daka, Matafwali, Banda, Mfune, Mayoka and Witika. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Steward Mudenda, ZnJlc2hzdGV3YXJkQGdtYWlsLmNvbQ==; Bwalya Angel Witika, YndhbHlhLndpdGlrYUBzbXUuYWMuemE=
 Steward Mudenda
Steward Mudenda Nelly Ngalande1
Nelly Ngalande1 Moses Mukosha
Moses Mukosha Victor Daka
Victor Daka Scott Kaba Matafwali
Scott Kaba Matafwali Michelo Banda
Michelo Banda Ruth Lindizyani Mfune
Ruth Lindizyani Mfune Bwalya Angel Witika
Bwalya Angel Witika