
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 10 January 2023
Sec. Health Economics
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1022344
This article is part of the Research Topic From Clinical Trials to Real-World Data Sciences for Value in Health: Access, Utilization, and Quality View all 8 articles
 Xiaoyan Liu1,2†
Xiaoyan Liu1,2† Huijun Zhou1*†
Huijun Zhou1*† Jie Wei3
Jie Wei3 Minghui Li4
Minghui Li4 Guofen Luo1
Guofen Luo1 Nasheen Naidoo5
Nasheen Naidoo5 Guang Zhang1
Guang Zhang1 Ye Bi6
Ye Bi6 Mengmeng Gao1
Mengmeng Gao1Background: The occupational health of university staff bears great social and economic value for which health utility is an indivisible aspect. Utility is also the primary data for the cost-utility analysis of occupational health programs. Health utility and occupational diseases have not been reported for the university staff in China. In the light of “Healthy China,” we conducted this study aiming to (1) estimate the health utility of university staff to inform cost-utility analysis and (2) screen and identify potential occupational diseases for this occupation and examine their impacts on health.
Methods: An occupational health survey was conducted in a sample of working-age university staff. Participants were interviewed face-to-face using the WHO Health and Work Performance Questionnaire and the European Quality of Life 5 Dimensions (EQ-5D) instrument to measure health conditions and health utility, respectively. The univariate analysis included the t-test, chi-square test, and correlation techniques. Multivariate generalized linear models were applied to evaluate the significance of each health condition when controlling for other factors.
Results: The sample (n = 154) had a mean age of 40.65 years and consisted of slightly more women (51.30%). Participants attained a mean (standard deviation) health utility of 0.945 (0.073). The most affected domain was anxiety/depression with 62 (40.26%) participants reporting problems, followed by pain/discomfort which captured 60 (37.66%) staff with problems. Thus, pain and psychologically related conditions were prevalent. Multivariate models identified two conditions that can significantly reduce the health utility. The psychological/emotional conditions were associated with a utility loss of −0.067 (95%CI: −0.089, −0.045). The pain in body parts other than the head, neck, and back reduced the utility by −0.034 (95%CI: −0.055, −0.014).
Conclusion: Working-age staff in Chinese universities may have a lower health utility than the general population. Psychological conditions and musculoskeletal pain appear like occupational diseases. With the health utility data available, economic evaluation of cost-utility should follow up to facilitate the implementation of cost-effective programs.
Occupational health is not only a public health issue but also an economic issue per se. Work-related health problems have caused tremendous loss to individuals, families, organizations, and society (1, 2). University staff constitute a unique occupational group in that they are highly skilled and highly educated, and their jobs demand intensive physical and mental efforts. Additionally, academics in the higher education sector are tasked with cultivating competent graduates and progressing science and culture to better society. Thus, the ill-health of this population has extensive social, economic, and cultural implications.
Although the occupational health of university staff bears great value, it has been largely ignored in China. This is most likely attributed to their work environment which is free of noise, dust, or heat. Occupational hazards are not easy to identify and occupational diseases are hard to define in a university setting. With that being said, studies have reported that mental disorders and musculoskeletal problems were common in this profession (3). In parallel with these reports, burnout, low job satisfaction, and occupational stress were frequently reported (4–6). Occupational factors such as work overload, sedentary work style, and long hours of lecturing have been blamed for the suboptimal health and health-related quality of life (HRQoL) (7–10). Therefore, university staff, just like workers in mining, construction, and manufacturing, maybe another health-disadvantaged population.
Occupational health and safety (OHS) programs have been proven effective in promoting the health of the workforce, reducing sickness absence, and improving the productivity of the organization and the sustainability of the business (11). The limited resources prohibit employers to invest in OHS fearing that it is not an economically wise investment. Economic evaluations in occupational health had the promise to address the issue (2). Nevertheless, the endeavors have been hampered by data deficiency, such as the health utility data of the employees for a cost-utility analysis (CUA) (2, 12).
CUA is a well-developed, full economic evaluation approach to inform the worthiness of health measures. CUA studies have been used to inform policies and programs in occupational health (13–15). Health utility derived from HRQoL is the primary input for a CUA. Moreover, HRQoL or health utility is in itself an important topic in occupational health research (16). Studies in China have suggested that HRQoL remains a concern in the population of university staff (4–7, 17). Unfortunately, none of these studies has reported health utility to support the CUA research in occupational health.
Recognizing this gap, we surveyed a school of a public university using the WHO Health and Work Performance Questionnaire (HPQ) and European Quality of Life 5 Dimensions 5 level (EQ-5D-5L) HRQoL instrument. The study set two objectives: (1) To estimate the health utility of university staff to inform occupational CUAs; and (2) to screen and identify potential occupational diseases for this occupation and examine their impacts on health utility. All in all, the study aspires to facilitate economic research in occupational health and inform the design and implementation of cost-effective OHS programs for university staff.
This was an occupational health survey conducted at the Business School, the University of Shanghai for Science and Technology, which is a public university in China. The eligibility criteria included: (1) official employee of the school; (2) not hospitalized or immediately after hospital discharge; (3) not handicapped or disabled; (4) able to carry out day-to-day work normally; and (5) able to give personal consent. The study was approved by the IRB committee of the Air Force Medical Center in Beijing.
The sampling frame consisted of 216 employees including both academic and administrative staff. The staff were personally invited through email, WeChat, or face-to-face contact. The recruitment advertisement was also announced at school-level meetings and internal WeChat workgroups. During the study period from 1 November 2020 to 15 January 2021, 155 people participated in the study, giving rise to a response rate of 78%. Seventeen persons were unavailable for reasons such as studying overseas, long-term sick or parental leave, hospitalization, resignation, or near-retirement. Another 35 staff were out of contact. Only nine personnel officially rejected the invitation. All participants were briefed about the study and then signed the informed consent form.
Data were collected through face-to-face interviews. Participants completed the questionnaires in the presence of the interviewer. The interviewer team consisted of one postgraduate and four undergraduate students who had attended three training sections each lasting 2 h. This pre-interview training aimed to ensure equivalent task understanding, procedures, and interactions with subjects. Interviewers were trained to give briefings and answer questions only, and not to promote a “right” or “wrong” answer as a measure to minimize the social desirability effect.
We used the Chinese version of the EQ-5D-5L instrument to measure health utility (18). The EQ-5D is a preference-based HRQoL instrument asking participants to rate their present-day health. Compared to the old version of the EQ-5D-3L instrument, the EQ-5D-5L instrument is more favorable for HRQoL measurement due to its greater discriminatory power and lower ceiling effect (19, 20). Its validity and reliability have been validated in various Chinese populations (19, 21, 22).
The EQ-5D instrument has two parts. The first part is the descriptive system which classifies 3,125 health states into five health domains, that is, mobility (MO), self-care (SC), usual activities (UA), pain/discomfort (PD), and anxiety/depression (AD), each with five ordinal severity levels (no problems, slight problems, moderate problems, severe problems, and extreme problems/unable to). A respondent rated his/her health subjectively against the most appropriate statement in each of the five dimensions based on their health on the day of the interview. The scores of the five dimensions were used to calculate health utility according to the Chinese-specific value set (23). Health utility by definition has a range of 0 (death) to 1 (full health). The second part is called the visual analog scale (VAS), a 10-cm vertical bar anchored at 0 (worst imaginable health) and 100 (best imaginable health). The VAS indicated the overall health status rated by the respondents themselves.
Occupation-related health conditions were investigated using the WHO HPQ (24). In completing the HPQ, subjects need to report a wide range of health conditions of diseases and symptoms. HPQ is a self-report instrument designed to estimate the workplace costs of health problems. Its validity in studying chronic diseases relating to the workplace has been proven satisfactory (25). The questionnaire also collected information about other health determinants such as demographic (age, gender, height, and weight), lifestyle or behavioral (smoking and drinking), and socioeconomic (education, marital status, and number of children) factors (26).
One participant was removed due to missing data. The final sample size for analyses was 154 participants. Categorical variables were described as counts and proportions. The prevalence of health conditions was estimated as the proportion of the sample presenting with certain health conditions. Continuous variables were presented as the mean and standard deviation (S.D.). The skewness and kurtosis of continuous variables were also explored to choose the appropriate models for multivariate analysis.
BMI was categorized into three groups—underweight/normal weight, overweight, and obese using a gender-specific standard for Chinese populations (27, 28), that is, 22.5 and 25.9 kg/m2 as cutoff points to define overweight and obesity in men, and 22.8 and 26.6 kg/m2 in women. Marital status was dichotomized into alone (single, divorced, or widowed) and married. A total of 40 health conditions were reported. This was too many to be treated as independent variables in the multivariate analysis for the sake of statistical power given the sample size. To carry out valid multivariate analyses, the six most prevalent conditions (≥20%) were treated as independent variables. These conditions were back/neck pain, pain in other areas, fatigue, high blood cholesterol, headache, and sleeping problems. The remaining 34 conditions were combined into seven groups by anatomical and/or physiological system (allergy, high blood pressure/cardiovascular, digestive system, respiratory system, musculoskeletal, psychological/emotional conditions, and others).
The univariate analysis involved correlation analysis between health utility and individual continuous variables, and t-test and ANOVA comparing the utility of different risk levels of categorical variables. A generalized linear model (GLM) was chosen to perform multivariate analyses as the dependent variable, EQ-5D utility, followed by a negatively skewed distribution (skewness = −1.89) to which GLMs were immune. The multivariate analysis evaluated the associations of health utility with sample characteristics. To remove the effect of collinearity and to produce consistent coefficients, the GLMs were set to use robust methods for parameter estimation and profile likelihood methods for confidence intervals. Unlike ordinary linear regression which models the raw data of the dependent variable, GLMs model the means of the dependent variable. Thus, in our study, the parameter coefficients of the GLMs represented the mean utility change associated with the specific variables.
All health conditions, except the category of other conditions, were evaluated simultaneously in one model together with demographic and socioeconomic variables. Doing so was to minimize collinearity because all the participants with other health conditions already had one or more classified diseases/symptoms. The analysis took p < 0.05 as being statistically significant. SPSS version 19 (SPSS Inc) was used for the analysis.
The characteristics of the sample are presented in Table 1. Our sample belongs to the working-age population and therefore had a mean age of 40.65 years with an upper age limit of the retirement age of 60 years. The mean BMI was 23.49 kg/m2 indicating that the enrolled staff were generally overweight for men and women alike (27). Only seven (4.55%) respondents had a Bachelor's degree. The majority (83.77%) were married and living with their families. For those raising children, the majority had one child only which was consistent with the One-Child policy in China. Up to 74% of the sample never smoked whereas half had the experience of drinking alcoholic beverages.
The overall prevalence of health conditions was 81.17% covering 40 diseases or symptoms. Half participants had back and/or neck pain reflecting a sedentary work style. The conditions inflicting eight (5%) or more subjects were summarized in Table 2. There were six conditions with a minimum prevalence of 20% (in descending order: chronic back and/or neck pain, pain in other body parts, chronic fatigue or low energy, high blood cholesterol, headache, and sleeping problems).
Despite the symptoms and diseases reported, the overall mean (SD) utility was 0.945 (0.073), with only 0.055 (5.5%) utility loss compared to the full health of 1 (Figure 1). The mean VAS score was 83.00 (11.32), which was 17% lower than 100, the score indicating the best imaginable health. Both health indices followed negative distribution and were highly correlated (r = 0.595, p < 0.001).
The health profile of the sample was reflected by the five EQ-5D domains in Figure 2. There were 74 (48.1%) participants who did not report any problems in the five domains, that is, they rated themselves in full health. This proportion also indicated the ceiling effect of the EQ-5D-5L instrument from the measurement perspective. The most affected domain was AD. Overall, 40.26% of participants reported anxiety or depression problems, one subject had a severe problem, seven subjects had moderate problems, and 54 subjects had slight problems. The second most affected domain was PD, in which 37.66% of the sample reported problems including seven subjects with moderate severity. On the other hand, very few participants reported problems in the MO, SC, and UA domains. None of these domains captured a case with problems more severe than slight problems.
As shown in Table 3, age and number of health conditions were negatively correlated with utility. Univariate analysis did not find significant comparisons of health utility for demographic and socioeconomic factors. For health conditions, all conditions except respiratory system conditions were associated with significant utility loss. Those subjects living with any condition reported lower utility than those without. The largest utility loss was related to psychological/emotional conditions. The subjects presenting with psychological/emotional conditions had a mean utility of 0.88, which was 0.09 lower than those without.
In the GLMs evaluating multiple health conditions (Table 4), psychological/emotional conditions were associated with the biggest mean utility loss of −0.063, followed by the education level of a Master's degree or higher and pain in other body parts, which were associated with a utility loss of −0.048 and −0.036, respectively. Notably male gender, marriage, smoking, or having children were associated with utility gain. However, these factors did not achieve statistical significance in predicting health utility.
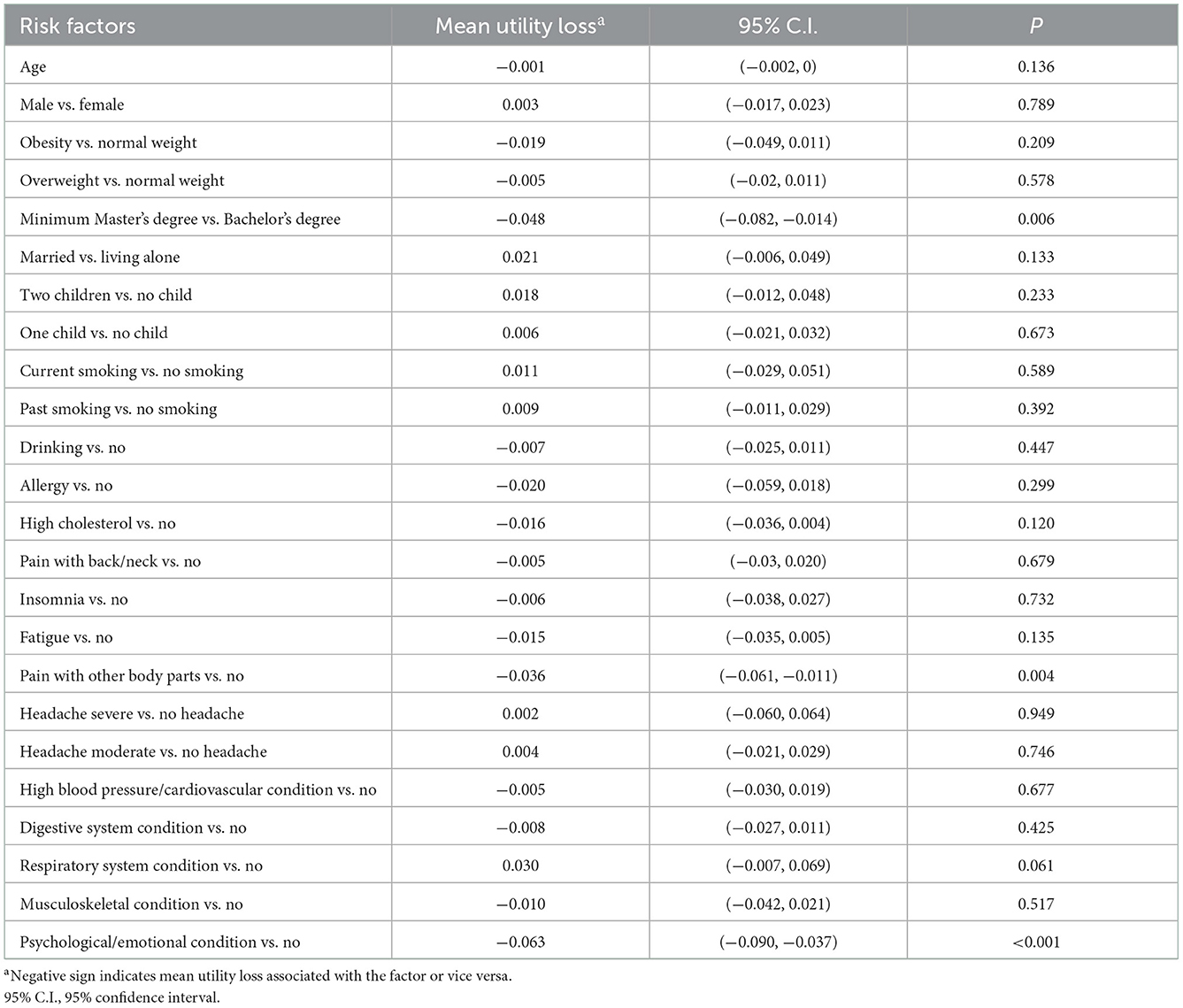
Table 4. Multivariate GLM simultaneously evaluating associations of individual factors with health utility.
Focusing on the HRQoL aspect of occupational health, our study estimated that the mean health utility was 0.945 for the university staff, while the subjective HRQoL was conservative with a mean VAS score of 83. The utility was closely linked to the AD and PD domains in which 40.26 and 37.66% of participants reported problems, respectively. The most prevalent diseases or symptoms in this occupation seemed to be broadly related to pain (back, neck, head, and other body parts) and mental problems (sleep problems, fatigue, and anxiety disorder). Psychological/emotional conditions, Master's degree, and pain in body parts were significant factors contributing mean utility loss of −0.067, −0.048, and −0.034, respectively. To the best of our knowledge, this is the first study specifically dedicated to the health utility of university staff in China.
Economic and social benefits are important considerations of employers in providing OHS services to their employees. Anyway, resources are limited and deserve cost-effective use. Following that, economic evaluations on OHS policies are common research practices in advanced countries (2, 12, 13, 29). Data availability always emerged as a barrier for such studies, which can only be worse in developing countries such as China. To conduct CUA in an occupational health setting, the utility data is harder to obtain than the cost data, as the latter is more direct for collection. Although health utility has been measured nationally with the EQ-5D-3L in China (National Health Services Survey, NHSS) once every 5 years since 2003 (30), the data are supposedly limited to inform the HRQoL of a specific occupational group. Additionally, the EQ-5D-3L tends to overestimate health utility for a generally healthy population (31). Compared to the EQ-5D-5L, EQ-5D-3L is less powered to discriminate between different health statuses and more affected by the ceiling effect (19, 20). Therefore, the health utility estimated by this study makes valid evidence for a CUA targeting at occupational health of university staff.
Unlike workers employed in hazardous occupations, university staff were unlikely to be considered a health-disadvantaged population. Our findings seemed to suggest otherwise. Compared to a survey attempting to create health utility norm in urban residents with EQ-5D-5L (32), their subjects (n = 965) of the same age as our sample achieved a mean utility of 0.961, which was higher than 0.945 for our sample. The difference does not reach statistical significance reflecting that the two study populations are generally considered healthy. Our participants reported more problems in all EQ-5D domains than the age-matched participants of the norm study. The differences in AD and PD were statistically significant (P = 0.001 and P = 0.016). Of our sample, 40.26 and 37.66% of subjects reported AD and PD problems, respectively, compared to 27.56 and 28.7% of age-matched subjects in that study (32). The health disadvantage of university staff was further supported by comparing our study with the 2013 NHSS enrolling 188,720 Chinese across mainland China (33). Our sample again had a significantly lower utility than the national sample (0.945 vs. 0.985, P = 0.011). Given that the national sample was heterogeneous with respect to health determinants, our sample was further compared to the subpopulation holding university degrees or higher, in that the education level is the distinctive characteristic of university staff and is closely relevant to other factors such as residence, employment, and health insurance. Compared to the education-matched cohort, the larger gaps in utility and VAS were revealed seeing that, for our sample of university staff, the utility shortage was 0.05 and the VAS shortage was 2.44 on average. Both differences were statistically significant (P < 0.001, P = 0.007).
Occupational diseases for university staff have not been defined in the National List of Occupational Diseases in China. According to our findings, pain and mental problems are popular medical complaints. Different types of pain all had relatively high prevalence (Table 2). Psychological and emotionally relevant problems such as fatigue or low energy, sleep problems, anxiety disorder, other emotional problems, and depression were also common or had a higher prevalence than the national figures (34). As for HRQoL, our participants were 7.68 times more likely to report PD problems and 16.10 times more likely to report AD problems than the education-matched NHSS sample (33). Even compared to other NHSS cohorts with similar socioeconomic characteristics of working age, employment status, or residence, the likelihood of PD and AD in our sample was three and eight times higher (33). Consistent with our findings, previous Chinese studies also reported poor mental health in university lecturers (3, 6, 35). Neck or back pain is popular among university employees in China and other countries and has caused considerable productivity loss due to sickness (8, 36–38). Our results are also in line with international studies showing that problems with mental health and the musculoskeletal system are the two major work-related medical conditions causing high costs to employers (39–41). Putting all evidence together, pain and mental disorders seem to be qualified as occupational diseases for the profession of university staff and are officially listed as so. A CUA study taking full account of cost and utility would produce convincing evidence for this purpose.
There were 63.64% of participants reporting physiological pain while only 37.68% reporting problems in the PD domain. Conversely, 24.68% of participants reporting psychological or mental conditions while 40.26% reporting problems in the AD domain. The health profile from a clinical perspective appears quite different from an HRQoL perspective. This disparity is most likely culture-related (42). The Chinese are not willing to admit their mental problems for fear of discrimination. The social stigma surrounding mental disease is stronger in China than in the West (43, 44). However, it is the opposite with respect to pain. Being traditionally viewed as diligent or industrious, the Chinese have a high tolerance for pain for fear of appearing lazy or irresponsible (45). This finding has highlighted the need to include the HRQoL in the basket of occupational health indicators to have a better understanding of the relationship between personnel's health and the organization's productivity (5, 7, 16).
There were several advantages to our study. The ceiling effect of the EQ-5D-5L in measuring our sample was 48% only, much lower than the 84.2% in the NHSS and similar studies in Asia, the USA, and Europe (46–50). The ceiling effect limits an HRQoL instrument to measure suboptimal health when subjects are generally healthy resulting in overestimated utility. A modest ceiling effect secures the reliability and validity of our findings of health utility. Another advantage is that we employed a GLM for multivariate analysis, which is superior to more commonly used linear regression models and produces more stable estimates for the study population.
Some limitations to our study are notable. The sample size is small which may affect its representativeness of the population of university staff in China. However, university staff are homogenous in terms of age, education level, job duty, and socioeconomic characteristics. This means that, statistically, a small sample may have good representativeness of the study population (51). The idea based on our findings that university staff have worse health status than the general population might be related to the choice of HRQoL instrument or measurement bias. Our study used the EQ-5D-5L instrument to measure HRQoL, whereas the NHSS studies used the EQ-5D-3L instrument (30, 33), which, due to its lower discretionary power, systematically generated higher health utility than the EQ-5D-5L instrument (19). This implies that the lower health utility in our sample might be spurious and introduced by the EQ-5D-5L. On the reverse side, compared with the more recent study that used the EQ-5D-5L (32), university staff again had lower health utility and significantly more problems in AD and PD. If the measurement bias ever existed, it would be less likely to bias our findings to a worrying extent. Finally, this study did not evaluate occupational factors, for example, working hours or workload, in terms of their impacts on the HRQoL. This might weaken the power of study findings as an occupational survey.
Staff working in Chinese universities may have lower HRQoL and health utility than the general population. This indicates that occupational health in the higher education sector remains an indispensable health issue. Psychological conditions and musculoskeletal pain appear like occupational diseases specifically in the population of working-age university staff. The utility loss was mainly manifested with impairment in the AD and PD domains. With the health utility data available, economic evaluations such as CUA should follow-up on time to facilitate the implementation of cost-effective OHS measures.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the IRB Committee of the Air Force Medical Center in Beijing. The patients/participants provided their written informed consent to participate in this study.
XL conceptualized and designed the study. HZ conceptualized the study, analyzed the data, and wrote the original draft. JW and ML managed the project and interpreted the results. GL and NN interpreted the results and offered important ideas for discussion. GZ did the preliminary statistical and advised on methodology. MG and YB collected and compiled the data. All authors made major revisions to the draft and approved the manuscript for final submission.
This work was funded by Shanghai Municipal Education Commission through the Program for Professor of Special Appointment (Eastern Scholar) at Shanghai Institutions of Higher Learning awarded to HZ (grant number: 10-20-303-601;10-19-303-602). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ning H, Zhou Y, Zhou Z, Cheng S, Huang R, Ning H, et al. Challenges to improving occupational health in China. Occup Environ Med. (2017) 74:924–5. doi: 10.1136/oemed-2017-104656
2. Grimani A, Bergstrom G, Casallas MIR, Aboagye E, Jensen I, Lohela-Karlsson M. Economic evaluation of occupational safety and health interventions from the employer perspective: a systematic review. J Occup Environ Med. (2018) 60:147–66. doi: 10.1097/JOM.0000000000001224
3. Chen N, Li X, Liu Q, Liu Y. Systematic review of university teachers' mental health based on SCL-90. Wei Sheng Yan Jiu. (2014) 43:990–7.
4. Yao SM, Yu HM, Ai YM, Song PP, Meng SY, Li W. Job-related burnout and the relationship to quality of life among Chinese medical college staff. Arch Environ Occup Health. (2015) 70:27–34. doi: 10.1080/19338244.2013.859120
5. Alves PC, Oliveira AF, Paro H. Quality of life and burnout among faculty members: how much does the field of knowledge matter? PLoS ONE. (2019) 14:e0214217. doi: 10.1371/journal.pone.0214217
6. Li MY, Wang ZY, Wu H, Wang JN, Wang L. Occupational mental health and job satisfaction in university teachers in Shenyang, China. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. (2017) 35:137–40. doi: 10.3760/cma.j.issn.1001-9391.2017.02.014
7. Liu C, Wang S, Shen X, Li MY, Wang L. The association between organizational behavior factors and health-related quality of life among college teachers: a cross-sectional study. Health Qual Life Outcomes. (2015) 13:1–12. doi: 10.1186/s12955-015-0287-4
8. López-Bueno R, Smith L, Andersen LL, López-Sánchez GF, Casajús JA. Association between physical activity and sickness absenteeism in university workers. Occup Med. (2020) 70:24–30. doi: 10.1093/occmed/kqz158
9. Karnes S, Niemeier B, Ksobiech K, Fischer E. A profile of stress, health, and work performance among university employees. Am J Health Stud. (2018) 33:9. doi: 10.47779/ajhs.2018.68
10. Gallinari C, Garsi JP, Vercambre-Jacquot MN. Voice disorders in French teachers: prevalence, risk factors and impact on well-being at work and quality of life. Arch Mal Prof Environ. (2016) 77:650–64. doi: 10.1016/j.admp.2015.12.008
11. Fu C, Zhu M, Yu TS, He Y. Effectiveness of participatory training on improving occupational health in small and medium enterprises in China. Int J Occup Environ Health. (2013) 19:85–90. doi: 10.1179/2049396713Y.0000000021
12. Miller P, Whynes D, Reid A. An economic evaluation of occupational health. Occup Med Oxford. (2000) 50:159–63. doi: 10.1093/occmed/50.3.159
13. Kankaanpaa E, van Tulder M, Aaltonen M, De Greef M. Economics for occupational safety and health. Scand J Work Environ Health. (2008) 34:9–13.
14. Geraedts AS, van Dongen JM, Kleiboer AM, Wiezer NM, van Mechelen W, Cuijpers P, et al. Economic evaluation of a web-based guided self-help intervention for employees with depressive symptoms: results of a randomized controlled trial. J Occup Environ Med. (2015) 57:666–75. doi: 10.1097/JOM.0000000000000423
15. Watson H, Godfrey C, McFadyen A, McArthur K, Stevenson M, Holloway A. Screening and brief intervention delivery in the workplace to reduce alcohol-related harm: a pilot randomized controlled trial. Int J Nurs Stud. (2015) 52:39–48. doi: 10.1016/j.ijnurstu.2014.06.013
16. Blanc PD. Why quality of life should matter to occupational health researchers. Occup Environ Med. (2004) 61:571. doi: 10.1136/oem.2004.013888
17. Ge C, Yang X, Fan Y, Kamara AH, Zhang X, Fu J, et al. Quality of life among Chinese college teachers: a cross-sectional survey. Public Health. (2011) 125:308–10. doi: 10.1016/j.puhe.2011.02.010
18. Luo N, Li M, Liu GG, Lloyd A, de Charro F, Herdman M. Developing the Chinese version of the new 5-level EQ-5D descriptive system: the response scaling approach. Qual Life Res. (2013) 22:885–90. doi: 10.1007/s11136-012-0200-0
19. Pan CW, Sun HP, Wang X, Ma Q, Xu Y, Luo N, et al. The EQ-5D-5L index score is more discriminative than the EQ-5D-3L index score in diabetes patients. Qual Life Res. (2015) 24:1767–74. doi: 10.1007/s11136-014-0902-6
20. Jia YX, Cui FQ, Li L, Zhang DL, Zhang GM, Wang FZ, et al. Comparison between the EQ-5D-5L and the EQ-5D-3L in patients with hepatitis B. Qual Life Res. (2014) 23:2355–63. doi: 10.1007/s11136-014-0670-3
21. Wang HM, Patrick DL, Edwards TC, Skalicky AM, Zeng HY, Gu WW. Validation of the EQ-5D in a general population sample in urban China. Qual Life Res. (2012) 21:155–60. doi: 10.1007/s11136-011-9915-6
22. Luo N, Li M, Chevalier J, Lloyd A, Herdman M. A comparison of the scaling properties of the English, Spanish, French, and Chinese EQ-5D descriptive systems. Qual Life Res. (2013) 22:2237–43. doi: 10.1007/s11136-012-0342-0
23. Luo N, Liu G, Li M, Guan H, Jin X, Rand-Hendriksen K. Estimating an EQ-5D-5L value set for China. Value Health. (2017) 20:662–9. doi: 10.1016/j.jval.2016.11.016
24. Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, et al. The World Health Organization health and work performance questionnaire (HPQ). J Occup Environ Med. (2003) 45:156–74. doi: 10.1097/01.jom.0000052967.43131.51
25. Kessler RC, Ames M, Hymel PA, Loeppke R, McKenas DK, Richling DE, et al. Using the World Health Organization health and work performance questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occup Environ Med. (2004) 46:S23–37. doi: 10.1097/01.jom.0000126683.75201.c5
26. Marmot M. Social determinants of health inequalities. Lancet. (2005) 365:1099–104. doi: 10.1016/S0140-6736(05)71146-6
27. He W, Li Q, Yang M, Jiao J, Ma X, Zhou Y, et al. Lower BMI cutoffs to define overweight and obesity in China. Obesity. (2015) 23:684–91. doi: 10.1002/oby.20995
28. Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/S0140-6736(03)15268-3
29. Mofidi A, Tompa E, Mortazavi SB, Esfahanipour A, Demers PA. A probabilistic approach for economic evaluation of occupational health and safety interventions: a case study of silica exposure reduction interventions in the construction sector. BMC Public Health. (2020) 20:1–12. doi: 10.1186/s12889-020-8307-7
30. Sun S, Chen J, Johannesson M, Kind P, Xu L, Zhang Y, et al. Population health status in China: EQ-5D results, by age, sex and socio-economic status, from the National Health Services Survey 2008. Qual Life Res. (2011) 20:309–20. doi: 10.1007/s11136-010-9762-x
31. Petrou S, Hockley C. An investigation into the empirical validity of the EQ-5D and SF-6D based on hypothetical preferences in a general population. Health Econ. (2005) 14:1169–89. doi: 10.1002/hec.1006
32. Yang Z, Busschbach J, Liu G, Luo N. EQ-5D-5L norms for the urban Chinese population in China. Health Qual Life Outcomes. (2018) 16:210. doi: 10.1186/s12955-018-1036-2
33. Yao Q, Liu C, Zhang Y, Xu L. Population norms for the EQ-5D-3L in China derived from the 2013 National Health Services Survey. J Glob Health. (2021) 11:08001. doi: 10.7189/jogh.11.08001
34. Ren X, Yu S, Dong W, Yin P, Xu X, Zhou M. Burden of depression in China, 1990–2017: findings from the global burden of disease study 2017. J Affect Disord. (2020) 268:95–101. doi: 10.1016/j.jad.2020.03.011
35. Li WJ, Kou CG. Prevalence and correlates of psychological stress among teachers at a national key comprehensive university in China. Int J Occup Environ Health. (2018) 24:7–16. doi: 10.1080/10773525.2018.1500803
36. Chaiklieng S, Suggaravetsiri P, Stewart J. Incidence and risk factors associated with lower back pain among university office workers. Int J Occup Saf Ergo. (2021) 27:1215–21. doi: 10.1080/10803548.2019.1706827
37. Tong F, Lv Q, Li A, Fang L, Luo Z, Feng J, et al. An epidemiological study of the prevalence rate of inflammatory back pain and axial spondyloarthritis in a university in the south of China. Clin Rheumatol. (2018) 37:3087–91. doi: 10.1007/s10067-018-4175-2
38. Mohseni Saravi B, Kabirzadeh A, Rezazadeh E, Khariki MF, Asgari Z, Bagherian Farahabadi E, et al. Prevalence and causes of medical absenteeism among staff (case study at mazandaran university of medical sciences: 2009–2010). Mater Sociomed. (2013) 25:233–7. doi: 10.5455/msm.2013.25.233-237
39. Odeen M, Magnussen LH, Maeland S, Larun L, Eriksen HR, Tveito TH. Systematic review of active workplace interventions to reduce sickness absence. Occup Med. (2013) 63:7–16. doi: 10.1093/occmed/kqs198
40. Pohling R, Buruck G, Jungbauer KL, Leiter MP. Work-related factors of presenteeism: the mediating role of mental and physical health. J Occup Health Psychol. (2016) 21:220–34. doi: 10.1037/a0039670
41. Stansfeld S, Candy B. Psychosocial work environment and mental health: a meta-analytic review. Scand J Work Environ Health. (2006) 32:443–62. doi: 10.5271/sjweh.1050
42. Li M, Bao Z, Lv G, Zhou J, Chen P, Luo N. Culture-related health disparities in quality of life: assessment of instrument dimensions among Chinese. Front Public Health. (2021) 9:663904. doi: 10.3389/fpubh.2021.663904
43. Phillips MR, Pearson V, Li FF, Xu MJ, Yang L. Stigma and expressed emotion: a study of people with schizophrenia and their family members in China. Br J Psychiat. (2002) 181:488–93. doi: 10.1192/bjp.181.6.488
44. Stuart H. Reducing the stigma of mental illness. Glob Ment Health. (2016) 3:87. doi: 10.1017/gmh.2016.11
45. Tung WC, Li ZZ. Pain beliefs and behaviors among Chinese. Home Health Care Manag Pract. (2015) 27:95–7. doi: 10.1177/1084822314547962
46. Huang WD, Yu HJ, Liu CJ, Liu GX, Wu QH, Zhou J, et al. Assessing health-related quality of life of Chinese adults in heilongjiang using EQ-5D-3L. Int J Environ Res Pub Health. (2017) 14:224. doi: 10.3390/ijerph14030224
47. Abdin E, Subramaniam M, Vaingankar JA, Luo N, Chong SA. Population norms for the EQ-5D index scores using Singapore preference weights. Qual Life Res. (2015) 24:1545–53. doi: 10.1007/s11136-014-0859-5
48. Shiroiwa T, Fukuda T, Ikeda S, Igarashi A, Noto S, Saito S, et al. Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res. (2016) 25:707–19. doi: 10.1007/s11136-015-1108-2
49. Janssen MF, Szende A, Cabases J, Ramos-Goni JM, Vilagut G, Konig HH. Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. Eur J Health Econ. (2019) 20:205–16. doi: 10.1007/s10198-018-0955-5
50. Garcia-Gordillo MA, Adsuar JC, Olivares PR. Normative values of EQ-5D-5L: in a Spanish representative population sample from Spanish Health Survey, 2011. Qual Life Res. (2016) 25:1313–21. doi: 10.1007/s11136-015-1164-7
51. Desai R. Optimum Sample: Definition Factors | Social Research, (2021). Available online at: https://www.yourarticlelibrary.com/social-research/optimum-sample-definition-and-factors-social-research/92926 (accessed April 16, 2022).
Keywords: health utility, health related quality of life, EQ-5D-5L = EuroQol 5-dimensions 5-level, real-world evidence (RWE), university staff, occupational health
Citation: Liu X, Zhou H, Wei J, Li M, Luo G, Naidoo N, Zhang G, Bi Y and Gao M (2023) An occupational health survey on health utility and occupational diseases in Chinese university staff to inform cost-utility analysis. Front. Public Health 10:1022344. doi: 10.3389/fpubh.2022.1022344
Received: 18 August 2022; Accepted: 19 December 2022;
Published: 10 January 2023.
Edited by:
Kevin Lu, University of South Carolina, United StatesReviewed by:
Fanwen Meng, National Healthcare Group, SingaporeCopyright © 2023 Liu, Zhou, Wei, Li, Luo, Naidoo, Zhang, Bi and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huijun Zhou,  bG9ja2dvMmx1Y2tAMTI2LmNvbQ==
bG9ja2dvMmx1Y2tAMTI2LmNvbQ==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.