
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 31 October 2022
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1018724
This article is part of the Research Topic Chlamydia Trachomatis Infection: Epidemiology, Prevention, Clinical, and Basic Science Research View all 13 articles
 Lingen Shi1,2†
Lingen Shi1,2† Jun Luo3†
Jun Luo3† Yuheng Chen1
Yuheng Chen1 Liping Chen1
Liping Chen1 Haiyang Hu1
Haiyang Hu1 Tao Qiu1
Tao Qiu1 Xiaoyan Liu1
Xiaoyan Liu1 Xiaoqin Xu1
Xiaoqin Xu1 Yunting Chen1
Yunting Chen1 Zhi Zhang1
Zhi Zhang1 Ying Zhou1
Ying Zhou1 Jing Lu1
Jing Lu1 Gengfeng Fu1*
Gengfeng Fu1*Background: Female sex workers (FSWs) are considered highly vulnerable to sexually transmitted infections (STIs), but available data on the prevalence of STIs among FSWs in China is limited at a provincial level. This study aimed to evaluate the prevalence of STIs and risk factors among FSWs in Jiangsu, China.
Methods: We conducted a multicenter cross-sectional study in seven cities of Jiangsu to investigate the prevalence and risk factors associated with HIV and other STIs. Blood and urine were collected to test for HIV, syphilis, Hepatitis C (HCV), Neisseria gonorrhoeae (NG) and Chlamydia trachomatis (CT) infections.
Results: We enrolled 3,580 FSWs. The overall prevalence of bacterial STIs was 6.2% (5.4%−7.0%). The prevalence of HIV, syphilis infection, HCV, NG and CT were 0.1% (95%CI, 0.0–0.2), 1.8% (95%CI, 1.4–2.3), 0.3% (95%CI, 0.1–0.5), 0.3% (95%CI, 0.2–0.5) and 4.3% (95%CI, 3.6–5.0), respectively. Most FSWs (85.6%) reported consistent condom use with clients in the past month. Only 10.6% of FSWs reported group sex, and 68.3% self–reported HIV testing in the previous year. According to the multivariable model, having group sex in the past year (aOR, 2.521, 95%CI: 1.366–4.651) and HIV infection (aOR, 26.260, 95%CI: 2.432–283.563) were associated with a higher risk of syphilis infection. Migrants (aOR, 1.669, 95%CI: 1.163–2.395), having a history of STIs in the past year (aOR, 4.601, 95%CI: 1.003–21.118), and NG infection (aOR, 38.549, 95%CI: 11.214–132.514) were associated with a higher risk of CT infection. On the contrary, FSWs aged older than 25 were associated with lower risk of syphilis infection (25–34: aOR, 0.339, 95%CI: 0.151–0.763) and CT infection (25–34: aOR, 0.503, 95%CI: 0.316–0.802; ≥35: aOR, 0.578, 95%CI: 0.362–0.925).
Conclusion: This study's prevalence rates of syphilis and CT infections show the need to promote comprehensive STIs control and prevention strategies, including behavioral intervention and STIs screening, especially in younger high–risk populations. With the increasing coverage of HIV testing, integrating other STIs screening with HIV testing may be a reasonable way to implement comprehensive STIs control and prevention.
According to the World Health Organization, 374 million new infections [including Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), Syphilis, and Trichomoniasis] were estimated nationwide in 2020. Nearly 35% of new infections were CT, one of the world's most commonly reported sexually transmitted infections (STIs) (1). The prevalence of CT and NG were high in key populations [CT: 16.3% and NG: 3.0% among men who have sex with men (MSM), CT: 17.0% and NG: 2.3% among female sex workers (FSWs)] (2, 3) than in the general population (CT: 10.2% and NG: 4.09% among women) (4). The case report of CT was under–estimated nationwide in China, considering the CT was previously not a notifiable reporting infectious diseases according to the Law of the People's Republic of China on the Prevention and Treatment of Infectious Diseases. STIs can cause serious outcomes without treatment in females, such as infertility, pelvic infection, pregnancy complications, and an increased risk of other STIs (especially HIV).
FSWs remain at high risk of HIV and other STIs worldwide. A global meta–analysis, covering 101 countries and 2,103,380 women, reported that the estimated HIV prevalence remained high and stable between 10.4 and 11.8% among FSWs from 2014 to 2018 (5). A cross–sectional study, conducted at Yunnan in 2008, reported prevalence rates of 36.8% for NG, 46.3% for CT, and 22.1% for trichomonas vaginalis among FSWs in China (6). Syphilis infection was estimated at 1.7% among FSWs in China, which was 6.8 times higher than among general population women in 2017 (7). FSWs contribute significantly to STIs transmission networks through their engagement in frequent unprotected sexual activities, multiple commercial sex partners (8–10), and limited asymptomatic STIs awareness (11). An Ecuador study reported that 25.5% of FSWs had unprotected sexual activities at least once in the previous 3 months (12). Another study in Australia observed an inconsistent condom use rate of 24% for vaginal sex with clients in 2021. About fellatio, the rate of inconsistent condom use reached 74% among clients in this population (13). In some instances, FSWs faced risks of reduced payment or intimate partner violence during negotiations for safe sex with routine clients or intimate sexual partners. Offers of higher monetary incentives for condomless sex sometimes derailed condom–use negotiations and further exposed FSWs to STIs (14, 15).
Meanwhile, a 2010 China study found that 39.8% of FSWs experienced challenges in using a condom correctly, such as condom rupture, and only used condoms during ejaculation (16). Most studies have demonstrated that STIs infection facilitates HIV infection. Controlling STIs could contribute to the Aim of “Zero AIDS” not only among FSWs but also in other high–risk sub–populations and the general population (17, 18). So, identifying the prevalence of STIs and risk characteristics of FSWs could contribute to improving strategies for controlling STIs in this population and preventing STIs from their clients and the general population.
Jiangsu, located in eastern China, belongs to the Yangtze–river economic zone, one of the three most developed and richest areas in China. The commercial sex industry flourished alongside China's rapid economic growth since the policy of economic reforms and open policies was initiated in the 1980s (19). With the rapid economic development, residents increased disposable income. Most rural–urban immigrants migrate to this province for more job opportunities and higher salaries. By 2021, the migrant population in Jiangsu reached almost 24 million, accounting for 25% of the whole population in Jiangsu province (20). Compared to indigenous residents, migrants lacked sources of health care, had poorer awareness of STIs–related knowledge, and were more likely to engage in condomless sex and commercial sex, increasing the likelihood of HIV/STIs acquisition in FSWs (21–23). Overlapping these characteristics, FSWs contribute to the worsening epidemic of HIV/STIs in Jiangsu. However, limited data on STIs surveillance among the high–risk population, especially FSWs in Jiangsu, have been reported. One study conducted in 2009 reported a high rate of syphilis (4.9%), CT (14.6%), and NG (5.4%) prevalence among FSWs in two Jiangsu province cities (24). Another study in Changzhou demonstrated high rates of CT (17.0%) and NG (2.3%) among FSWs in 2011 (3). This study aimed to investigate the prevalence of STIs and associated factors to evaluate and improve the comprehensive policies to control STIs in a provincial level.
From April to June 2021, a cross–sectional study was conducted in seven cities, named Nanjing, Wuxi, Suzhou, Huai'an, Yancheng, Yangzhou, and Zhenjiang, in Jiangsu province. A convenient sampling approach was used to recruit eligible participants. Firstly, we mapped the sex work venues and stratified them into three subgroups, i.e., high, middle, and low titers by minimum charge (3). High–titer venues included hotels and karaoke bars, and low–titer venues included street or other public outdoor sites. Middle–titer venues included barber bars, hair salons, massage parlors, roadside shops, guesthouses, or roadside restaurants (25). Secondly, we selected the potential venues randomly according to titers. Then, we conducted an on–site survey. All eligible venue members were recruited sequentially. Based on previous studies, we restricted the proportion of participants from each titer was high (<50%), middle (>40%), and low (>10%) in each city respectively to recruit a representative sample (26, 27).
Eligible participants were biologically females aged ≥16 years and self–reported providing vaginal, oral, or anal sex for male clients within the previous 12 months.
This study was approved by Ethics Committee of Jiangsu Provincial Center for Disease Prevention and Control in Jiangsu, China. All participants provided written informed consent before this survey.
The Jiangsu Center for Disease Control and Prevention designed a structured questionnaire for data collection. The information included socio–economic data, such as age (<25/25–34/35 and above), level of education (Secondary education or below/ High school and above), marital status (Single/married), migratory status, and monthly income (<5000/5000–7999/8000 and above, RMB). Participants who did not have official household registration in Jiangsu were deemed immigrants. Behavioral information included sexual behavior, condom use history, way to find male clients, drug history, HIV testing history, and STIs.
Based on the survey map and stratified titer of venues, the center for disease control and prevention staff contacted the house keepers or stakeholders, or managers to conduct an on–site survey. If they supported this survey, three professional staff (one for enrolling, one for screening and questionnaire, one for collecting sample of blood and urine) would take an on–site survey. Eligible participants would register their cellphone number for this survey. There was unique code linked the registration information, informed consent, questionnaire, blood and urine samples for each participant. The interviews remained anonymous throughout the survey. Each enrolled participant finished a face–to–face structured questionnaire interview.
After completing a questionnaire, each FSW donated 5 ml of venous blood with the help of trained nurses for HIV, Hepatitis C (HCV), and syphilis testing. All participants also provided 5 ml first–void urine held for more than 2 h for CT and NG testing. Finally, each participant received 50 RMB (approximately 7.5 US dollars) as participation incentives.
The enzyme–linked immunosorbent assay (ELISA) kit screened for plasma HIV and HCV antibodies in blood samples (Zhuhai livzon Diagnostics Inc., Zhuhai, China). If the result of HIV or HCV antibodies were positive, the same blood samples were retested by another ELISA reagent (Wantai Bio–pharmacy Enterprise Co., Ltd., Beijing, China). For HCV, both tests with positive results were recorded as HCV positive. For HIV, participants need provide new blood specimens for confirmatory testing by Western Blot (MP Biomedical Asia Pacific Pte. Ltd., Singapore) if both tests with positive results. Tests with positive results from both ELISA and WB were recorded as HIV infection.
Test for treponema pallidum (TP) was conducted using ELISA (TP–ELISA, Wantai Bio–pharmacy Enterprise Co., Ltd., Beijing, China) and subsequently by toluidine red untreated serum test (TRUST, Wantai Bio–pharmacy Enterprise Co., Ltd., Beijing, China) when the antibody for TP was positive. Positive results for both TP-ELISA and TRUST were recorded as syphilis infection. If only TP–ELISA was positive, we defined as syphilis antibody positive.
Pathogens of NG and CT were tested via nucleic amplification tests (NAATs) using (RENDU Biotechnology Co., Ltd., Shanghai, China), followed the manufacturer's instructions. A positive NAATs result of CT or NG was defined as CT or NG infection.
If participants received any positive result of STIs, professional staff would contact with positive participants, and referred them to local infectious disease hospital for further diagnose or treatment and care.
Descriptive analysis of categorical variables was reported as percentages. A chi–square test was used to assess the difference between subgroups. Where the chi–square test was not applicable, a fisher exact test was conducted to assess the difference between subgroups. A stepwise backward selection method was used for a multivariable logistic regression. Only variables with P < 0.2 were entered into the multivariable regression model. Odds ratio (OR) and adjusted Odds ratio (aOR) with a 95% Confidence interval (CI) were used to present the results. All data analyses were performed using IBM SPSS STATISTISCS (version 19.0, SPSS Inc., Chicago, IL, USA).
In total, we enrolled 3,580 FSWs from seven cities of Jiangsu province, including 985 (27.5%) from low titer venues, 1,866 (52.1%) from middle titer venues, and 729 (20.4%) from high titer venues. The mean age of FSWs was 35.0 years old (range, 16.0–65.0 years). The majority of FSWs were older than 35 years old (47.1%), with secondary education or below (69.9%), and currently married (72.4%). Among FSW participants, 43.5% were migrants, and 51.6% earned < 5000 RMB monthly (Table 1).
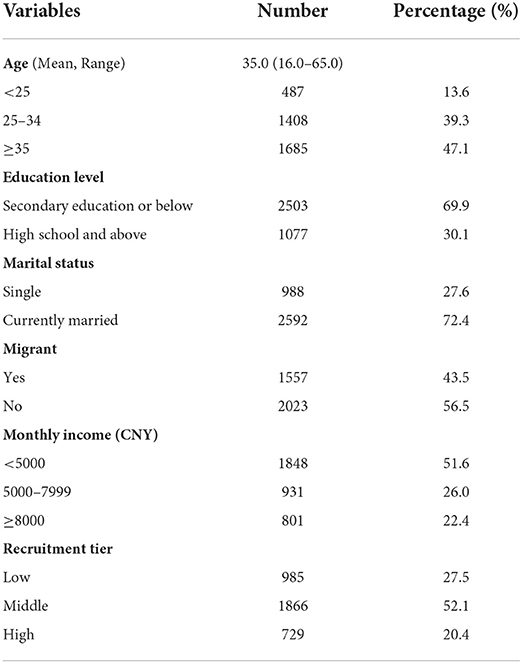
Table 1. Socio–demographic characteristics of 3,580 FSWs in a multi–center cross–sectional and venue–based study in Jiangsu, China.
Most FSWs (82.6%) reported staying in the enrolled cities for commercial sex work for more than 6 months, and 43.1% of FSWs stayed in the same city for their last venue for commercial sex work (Table 2).
Considering the way to find clients, 87.3% of FSWs reported ever in local fixed venues. 30.9% of FSWs found clients using the phone and providing door–to–door service, and 47.3% found clients using the internet. The main way to find clients was fixed venues (62.8%) and the internet (29.1%) (Table 2).
Most FSWs (85.6%) reported consistent condom use with clients in the past month. When they reached the last episode of commercial sex, 96.6% of them reported condom use. On the contrary, 14.4% of FSWs reported unprotected sex with clients in the past month, and 10.6% reported group sex in the previous year. Only 8 (0.2%) of FSWs used illicit drugs in the past year (Table 2).
Overall, 2,445 (68.3%) FSWs reported receiving HIV testing the previous year, 187 (5.2%) admitted having symptoms of STIs, and 13 (0.4%) reported STIs diagnosis in the previous year (Table 2).
In total 3,580 (100.0%) blood specimens and 3,307 (92.4%) urinary specimens were collected. Only 4 (0.1%, 95%CI, 0.0%−0.2%) case of HIV infection was found. The overall prevalence of bacterial STIs (syphilis, CT or NG) was 6.2% (95%CI, 5.4%−7.0%). The prevalence of syphilis antibody positive was 4.9% (95%CI, 4.2–5.5), and the prevalence of current syphilis infection was 1.8% (95%CI, 1.4–2.3). The prevalence of single CT and NG infections was 4.3% (95%CI, 3.6–5.0) and 0.3% (95%CI, 0.2–0.5), respectively. Only one FSW with current syphilis infection was co–infected with HIV. 4.3% (6/141) of FSWs with CT were co–infected with NG (Table 2), and 11 (0.3%, 95%CI, 0.1–0.5) cases of HCV infections were found (Table 3).
Chi–square or Fisher exact tests were used to compare syphilis and CT infection differences between subgroups of variables. Syphilis infection was significantly associated with age, migrant status, monthly income, group sex in the past year (all P < 0.05). CT infection was significantly associated age, marital status, migrant status, recruitment titer, and NG infection (all P < 0.05) (Table 4).
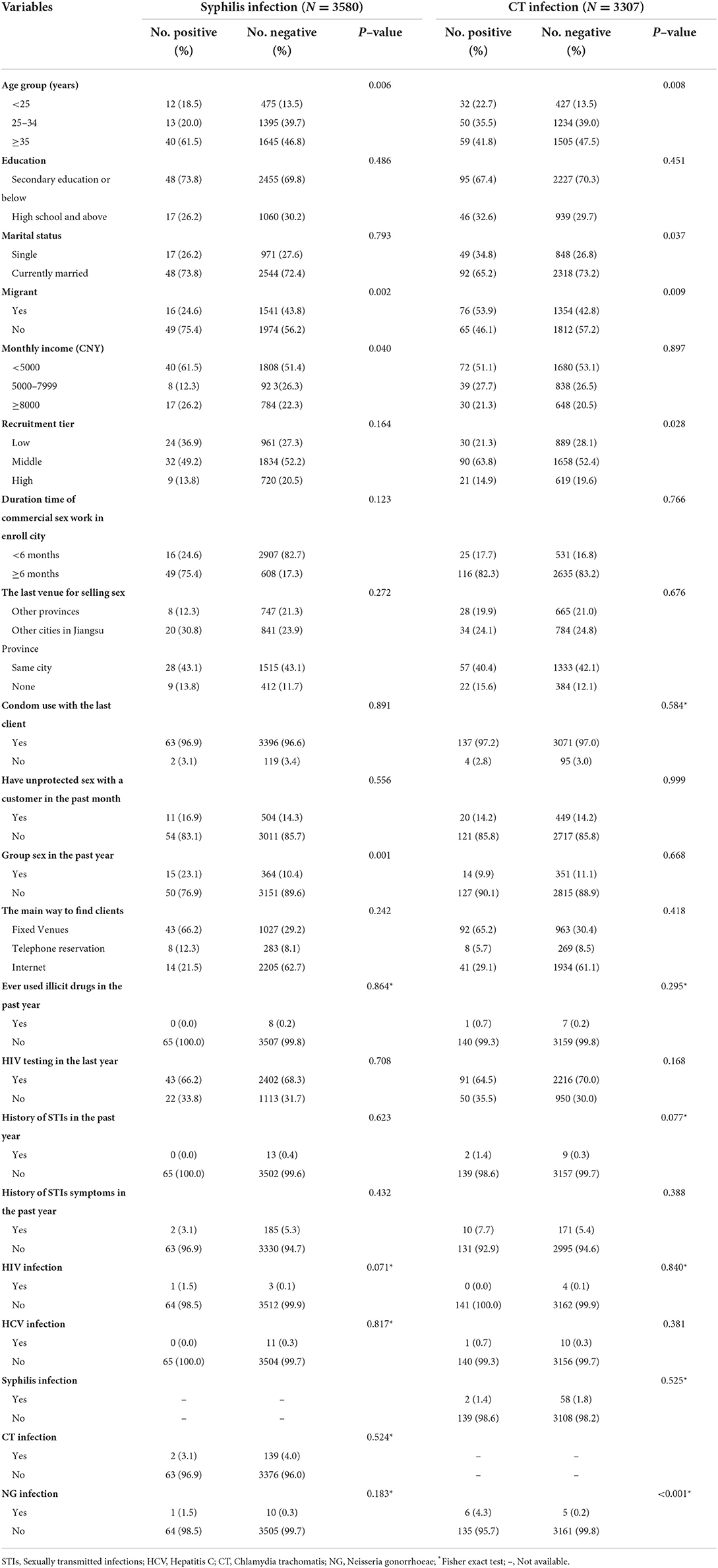
Table 4. Differences in syphilis and CT infection between subgroups of variables among FSWs in Jiangsu, China.
In the multivariable model, FSWs who were aged among 25–34 (aOR, 0.339, 95%CI: 0.151–0.763), migrants (aOR, 0.466, 95%CI: 0.257–0.845), and monthly income of 5000–7999 (aOR, 0.450, 95%CI: 0.205–0.991) were less likely to have syphilis infection. On the contrary, having group sex in the past year (aOR, 2.521, 95%CI: 1.366–4.651) and HIV infection (aOR, 26.260, 95%CI: 2.432–283.563) were associated with a higher risk of syphilis infection. FSWs who were migrants (aOR, 1.669, 95%CI: 1.163–2.395), having a history of STIs in the past year (aOR, 4.601, 95%CI: 1.003–21.118), and NG infection (aOR, 38.549, 95%CI: 11.214–132.514) were more likely to have CT infection (Table 5).
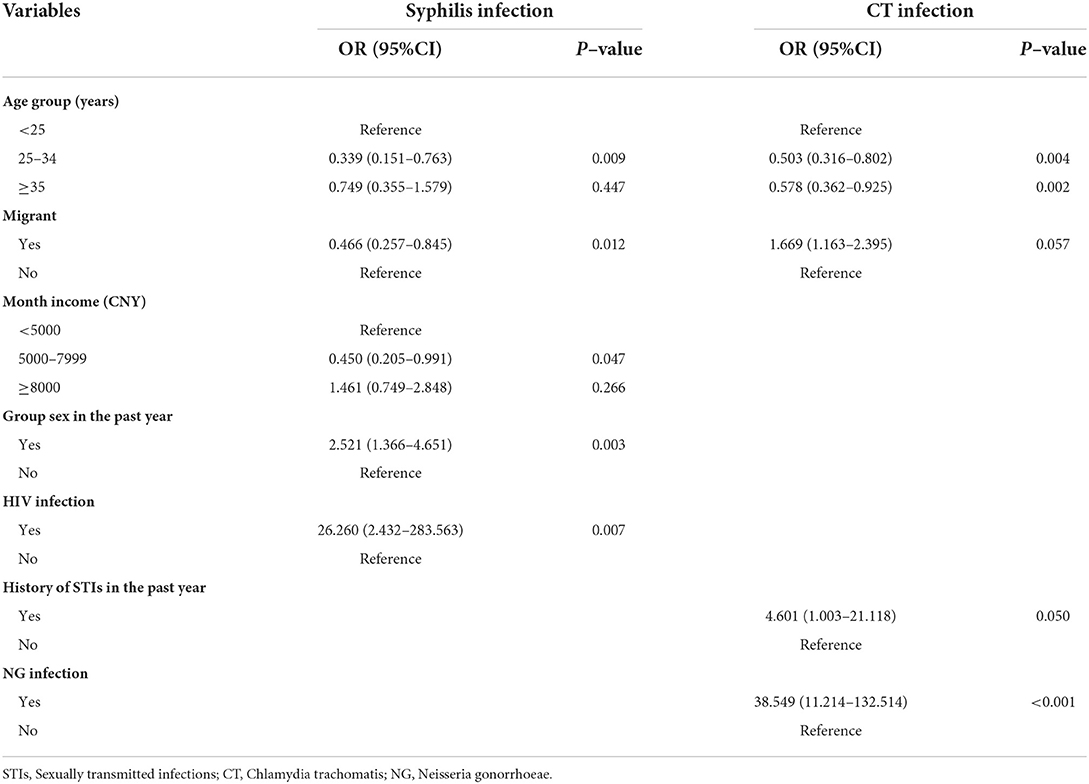
Table 5. Factors independently associated with syphilis and CT infection among FSWs in Jiangsu, China.
To our knowledge, this study was a large sample size and recruited from various categories of sex venues among FSWs in Jiangsu, China. In this multicenter cross–sectional study, the total prevalence of bacterial STIs was 6.2% for FSWs. The STIs prevalence among FSWs were 0.1% for HIV, 1.8% for syphilis infection, 0.3% for HCV, 4.3% for CT, and 0.3% for NG, respectively. Nearly half of FSWs were migrants from other provinces, and almost 100% of FSWs reported condom use with their last client. However, almost one–sixth of FSWs reported unprotective sex with clients in the past month. One in ten FSWs reported group sex in the past year, and 68.3% of FSWs got HIV testing in the past year. In the multiple logistic regression model, having group sex and HIV infection were risk factors for syphilis infection; being a migrant, having a history of STIs, and previous NG infection increased the risks of CT infection.
In our study, the CT and NG prevalence was 4.3 and 0.3%, respectively, lower than previous CT and NG prevalence rates reported among FSWs in Jiangsu by other studies. For instance, one study reported a CT prevalence of 14.61% and an NG prevalence of 5.42% in 2009 (24). Another study found a CT prevalence of 17.0% and an NG prevalence of 2.3% among FSWs in 2011 (3). It is possible that different specimens contribute to variations in sensitivity for CT/NG testing may explain the difference between our findings and other study findings (28). Guo and Tang collected cervical specimens to test CT and NG infection using NAATs in their studies. Our study collected first–void urine specimens to test CT and NG using NAATs. Also, compared with 40.7% of FSWs who reported consistent condom use with clients in the last month in Guo's study, 85.6% of participants reported consistent condom use in our study, which might imply a higher rate of STIs prevention among our sample. Nonetheless, the difference in reported prevalence rates implies that multiple specimens could be collected from different anatomical sites to evaluate the actual prevalence of CT/NG among FSWs in future studies.
Our result called for increased attention to stop STIs transmission among youth who sell sex. We found a high prevalence of CT among FSWs, particularly in <25 years old participants. Young–aged FSWs accounted for nearly one to five FSWs, suggesting a significant burden of bacterial STIs (syphilis and CT infection) compared with other age groups in our study. This finding corroborated with results from previous studies (11, 25, 29). Meanwhile, the high rate of CT infections indicated continuing high levels of risky behaviors among FSWs in Jiangsu. In China, there was still no national surveillance plan for CT and NG among the high–risk population. Our study's observed high rate of bacterial STIs infection also underlines the impendence and necessity of implementing bacterial STIs interventions (especially CT and NG) among FSWs.
Condom use can reduce HIV or other STIs transmission at a community level (30, 31). Since 2004, Jiangsu has promoted 100% condom use among FSWs to prevent HIV and other STIs. In our study, nearly 100% of FSWs reported condom use during their last sexual episode, which was higher than the country–level rate of condom use (77%) among FSWs (32). Nine to ten FSWs reported consistent condom use with their clients in the past month, which was higher than the rate (50.5%) in Zhejiang, another province in the Yangtze–river economic zone (33). Since 2010, the HIV prevalence consistently remained below 0.5%, and the syphilis infection prevalence also decreased from 5.32 to 1.72% from 2011 to 2020 among FSWs (unpublish data). The sentinel surveillance showed that condom promotion could effectively prevent HIV and syphilis transmission among the FSWs sub–population.
In this study, we found that 68.3% of FSWs received HIV testing last year, which was higher than the result from a meta–analysis conducted using data from China (34). China adopted regular HIV testing every three to six months among the high–risk population as part of its national programming (35). With this national guidance, 76.7% of FSWs reported taking at least one HIV test in the last year, from 2018 to 2019, in nine cities in China (36). This study's higher rate of HIV testing may be due to comprehensive prevention measures, such as condom promotion, educational campaigns, and HIV testing and counseling implemented over the years (37, 38). However, there were no recommended CT/NG screening strategies in China, even though a high prevalence of CT/NG was observed in multiple studies among the high–risk population in China (39–41). The increasing trend of HIV testing implies that integrating CT/NG testing with HIV testing was a reasonable way to screen for STIs, considering nearly 50% of NG and 75% of CT remain asymptomatic among FSWs (11, 42).
This study is the first–time urine samples have been collected for CT and NG testing in a community in Jiangsu. Based on clinical study protocols, previous studies usually collected cervical specimens to test CT and NG. However, according to a study on model sampling for HPV–based cervical cancer screening in 2019, 79% of participants had positive feelings about urine–based testing rather than cervical–vaginal sampling (18%) (43). According to findings from two studies conducted in Jiangsu, the rate of providing a cervical specimen for CT and NG tests was 28.57% (24) and 71.59% (3), respectively. However, 92.37% of participants in our study provided a urine sample for the CT/NG test, which showed high acceptability and feasibility of using urine samples. Furthermore, Cervical–based sampling needs a professional clinician and appropriate space for the sampling. In a community–based survey, we could not provide enough room for cervical samples, or participants refused to provide cervical swabs. Therefore, using first–void urine samples was more convenient for both researchers and participants. Further study on the sensitivity of CT/NG from different anatomical sites should be undertaken.
Several limitations of this study should be considered for interpreting the results. First, as a hidden and marginalized group, we could not reach this population without the cooperation of stakeholders or venue owners, or managers in potential venues. Participants were not randomly recruited based on a convenient sample in this study. Sample representativeness might be jeopardized by the venue–based sampling method, which overlapped with the increasing proportion of non–venue–based venue–seeking sex activities. Second, we only used the urine samples to test NG and CT among FSWs, not rectal or pharyngeal samples. Even though the rate of urogenital chlamydia was higher than that of anorectal chlamydia, the prevalence of CT might be underestimated without a multiple anatomical site specimens (44). Nearly 10% of participants refused to collect a urine sample for the NG and CT testing. That also might have contributed to an underestimation of the prevalence of NG and CT. Third, recall bias could not be ignored since all data associated with risk behaviors are based on self–report. Finally, we could not ignore the impact of COVID−19 pandemic on the prevalence of STIs among FSW. Regardless, our study has provided representative data to show the current rates of STIs prevalence and associated factors related to STIs infection among FSWs in Jiangsu, which may be used to modify future prevention strategies.
The observed percentages of syphilis and CT infections show the need to promote more comprehensive STIs control and prevention strategies, including behavioral intervention and STIs screening, especially among younger high–risk populations. The increasing coverage of HIV testing implies that integrating other STIs screening with HIV testing may be a reasonable way to implement comprehensive STIs control and prevention.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of Jiangsu Provincial Center for Disease Prevention and Control. The patients/participants provided their written informed consent to participate in this study.
LS, JuL, and GF had the original idea. LC, HH, XX, ZZ, YZ, and JiL conducted the testing for STIs. YuhC, TQ, XL, and YunC collected the data. LS and JuL analyzed the data. LS wrote the main manuscript text. All authors contributed to manuscript revision and approved the submitted version.
The authors acknowledge Center for Disease Control and Prevention staff in Jiangsu. Thanks Gifty Marley for language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CT, Chlamydia trachomatis; NG, Neisseria gonorrhoeae; STIs, Sexually transmitted infections; FSWs, Female sex workers; ELISA, Enzyme-linked immunosorbent assay; TP, Treponema pallidum; TRUST, Toluidine red untreated serum test; NAATs, Nucleic amplification tests; OR, Odds ratio; aOR, adjust Odds ratio; CI, Confidence interval.
1. World health Organization. Sexually Transmitted Infections. (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-STIS (accessed July 24, 2022).
2. Lin XX, Meng SY, Ke WJ, Zhang XH, Wang LY, Liao YY, et al. Community engagement on-site rapid test for chlamydia and gonorrhea among men who have sex with men: a pioneering study in Guangzhou, China. BMC Public Health. (2022) 22:1036. doi: 10.1186/s12889-022-13460-x
3. Guo Y, Xu X, Fu G, Huan X, Jiang N, Yin Y, et al. Risk behaviours and prevalences of HIV and sexually transmitted infections among female sex workers in various venues in Changzhou, China. Int J STD AIDS. (2017) 28:1135–42. doi: 10.1177/0956462416689763
4. Cai S, Pan J, Duan D, Yu C, Yang Z, Zou J, et al. Prevalence of ureaplasma urealyticum, chlamydia trachomatis, and neisseria gonorrhoeae in gynecological outpatients, Taizhou, China. J Clin Lab Anal. (2020) 34:e23072. doi: 10.1002/jcla.23072
5. Shannon K, Crago AL, Baral SD, Bekker LG, Kerrigan D, Decker MR, et al. The global response and unmet actions for HIV and sex workers. Lancet. (2018) 392:698–710. doi: 10.1016/S0140-6736(18)31439-9
6. Xu JJ, Wang N, Lu L, Pu Y, Zhang GL, Wong M, et al. HIV and STIS in clients and female sex workers in mining regions of Gejiu City, China. Sex Transm Dis. (2008) 35:558–65. doi: 10.1097/OLQ.0b013e318165926b
7. Korenromp EL, Zhang W, Zhang X, Ma Y, Jia M, Luo H, et al. The Spectrum-STIS Groups model: syphilis prevalence trends across high-risk and lower-risk populations in Yunnan, China. Sci Rep. (2020) 10:5472. doi: 10.1038/s41598-020-62208-3
8. Jiang T, Pan X, Ma Q, Jiang J, Chen L, Wang H, et al. Characteristics of low-tier female sex workers who engage in commercial sex with old male clients in Zhejiang province, China: a cross-sectional study. BMJ Open. (2021) 11:e049410. doi: 10.1136/bmjopen-2021-049410
9. Zappulla A, Fairley CK, Donovan B, Guy R, Bradshaw CS, Chen MY, et al. Sexual practices of female sex workers in Melbourne, Australia: an anonymous cross-sectional questionnaire study in 2017-18. Sex Health. (2020) 17:53–60. doi: 10.1071/SH19037
10. Khezri M, Tavakoli F, Bazrafshan A, Sharifi H, Shokoohi M. Condomless sex with partners and clients among female sex workers in Iran: a systematic review and meta-analysis. J Assoc Nurses AIDS Care. (2022) 33:63–77. doi: 10.1097/JNC.0000000000000305
11. Foschi C, Zagarrigo M, Belletti M, Marangoni A, Re MC, Gaspari V, et al. Genital and extra-genital chlamydia trachomatis and neisseria gonorrhoeae infections in young women attending a Sexually Transmitted Infections (STIs) clinic. New Microbiol. (2020) 43:115–20.
12. Llangarí-Arizo LM, Sadiq ST, Márquez C, Cooper P, Furegato M, Zhou L, et al. Sexually transmitted infections and factors associated with risky sexual practices among female sex workers: a cross-sectional study in a large Andean city. PLoS One. (2021) 16:e0250117. doi: 10.1371/journal.pone.0250117
13. Lee C, McManus H, Foster R, Davies SC. A survey of condom use among female sex workers in Northern Sydney; declining condom use for fellatio. Int J STD AIDS. (2021) 32:1326–37. doi: 10.1177/09564624211040951
14. Quaife M, Vickerman P, Manian S, Eakle R, Cabrera-Escobar MA, Delany-Moretlwe S, et al. The effect of HIV prevention products on incentives to supply condomless commercial sex among female sex workers in South Africa. Health Econ. (2018) 27:1550–66. doi: 10.1002/hec.3784
15. Roberts DA, Hawes SE, Bousso Bao MD, Ndiaye AJ, Gueye D, Raugi DN, et al. Trends in reported sexual behavior and Y-chromosomal DNA detection among female sex workers in the senegal preexposure prophylaxis demonstration project. Sex Transm Dis. (2020) 47:314–20. doi: 10.1097/OLQ.0000000000001175
16. Li Y, Detels R, Lin P, Fu X, Deng Z. Liu Y, et al. Prevalence of HIV and STIS and associated risk factors among female sex workers in Guangdong Province, China. J Acquir Immune Defic Syndr. (2010) 53 (Suppl. 1), S48–S53. doi: 10.1097/QAI.0b013e3181c7d72f
17. Jose JED, Sakboonyarat B, Mungthin M, Nelson KE, Rangsin R. Rising prevalence of HIV infection and associated risk factors among young Thai Men in 2018. Sci Rep. (2021) 11:7796. doi: 10.1038/s41598-021-87474-7
18. Tuot S, Teo AKJ, Chhoun P, Mun P, Prem K, Yi S, et al. Risk factors of HIV infection among female entertainment workers in Cambodia: Findings of a national survey. PLoS ONE. (2020) 15:e0244357. doi: 10.1371/journal.pone.0244357
19. Zhang L, Wilson DP. Trends in notifiable infectious diseases in China: implications for surveillance and population health policy. PLoS ONE. (2012) 7:e31076. 0031076. doi: 10.1371/journal.pone.0031076
20. Jiangsu Provincial Bureau of Statistics. Jiangsu Statistical yearbook. (2022). Available online at: http://tj.jiangsu.gov.cn/2021/nj02/nj0203.htm (accessed April 5, 2022).).
21. Liu H, Wang H, Feldman M. The risk of HIV/STDs infection and transmission among never-married male migrants in China: is risk attributable to bachelorhood or migration?. Arch Sex Behav. (2021) 50:3115–124. doi: 10.1007/s10508-021-02015-7
22. Zhu Z, Guo M, Petrovsky DV, Dong T, Hu Y, Wu B, et al. Age and regional disparity in HIV education among migrants in China: migrants population dynamic monitoring survey, 2014-2015. Int J Equity Health. (2019) 18:104. doi: 10.1186/s12939-019-0999-x
23. Xiao Q, Liu H, Wu B. How bachelorhood and migration increase the HIV transmission risk through commercial sex in China? AIDS Behav. (2020) 24:791–801. doi: 10.1007/s10461-019-02640-3
24. Tang W, Pan J, Jiang N, Hu HY, Mahapatra T, Yin YP, et al. Correlates of chlamydia and gonorrhea infection among female sex workers: the untold story of Jiangsu, China. PLoS ONE. (2014) 9:e85985. doi: 10.1371/journal.pone.0085985
25. Chen XS, Yin YP, Liang GJ, Wang QQ, Jiang N, Liu Q, et al. The prevalences of Neisseria gonorrhoeae and Chlamydia trachomatis infections among female sex workers in China. BMC Public Health. (2013) 13:121. doi: 10.1186/1471-2458-13-121
26. Wang L, Tang W, Wang L, Qian S, Li YG, Xing J, et al. The HIV, syphilis, and HCV epidemics among female sex workers in china: results from a serial cross-sectional study between 2008 and 2012. Clin Infect Dis. (2014) 59:e1–9. doi: 10.1093/cid/ciu245
27. Chen XS, Liang GJ, Wang QQ, Yin YP, Jiang N, Zhou YJ, et al. HIV prevalence varies between female sex workers from different types of venues in southern China. Sex Transm Dis. (2012) 39:868–70. doi: 10.1097/OLQ.0b013e318264c3ba
28. Coorevits L, Traen A, Bingé L, Van Dorpe J, Praet M, Boelens J, et al. Identifying a consensus sample type to test for Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium, Trichomonas vaginalis and human papillomavirus. Clin Microbiol Infect. (2018) 24:1328–32. doi: 10.1016/j.cmi.03,013
29. Connolly S, Wall KM, Parker R, Kilembe W, Inambao M, Visoiu AM, et al. Socio-demographic factors and STIS associated with chlamydia trachomatis and neisseria gonorrhoeae infections in Zambian female sex workers and single mothers. Int J STD AIDS. (2020) 31:364–74. doi: 10.1177/0956462419894453
30. Koff A, Goldberg C, Ogbuagu O. Condomless sex and HIV transmission among serodifferent couples: current evidence and recommendations. Ann Med. (2017) 49:534–44. doi: 10.1080/07853890.2017.1320423
31. Malekinejad M, Parriott A, Blodgett JC, Horvath H, Shrestha RK, Hutchinson AB, et al. Effectiveness of community-based condom distribution interventions to prevent HIV in the United States: a systematic review and meta-analysis. PloS ONE. (2017) 12:e0180718. doi: 10.1371/journal.pone.0180718
32. National Center for AIDS/STD Control and Prevention China CDC. China National HIV/Syphilis/HCV Surveillance Report in 2015. Beijing: National Center for AIDS/STD Control and Prevention, China CDC (2015).
33. Ma Q, Jiang J, Pan X, Cai G, Wang H, Zhou X, et al. Consistent condom use and its correlates among female sex workers at hair salons: a cross-sectional study in Zhejiang province, China. BMC Public Health. (2017) 17:910. doi: 10.1186/s12889-017-4891-6
34. Chow EP, Tung K, Tucker JD, Muessig KE, Su S, Zhang X, et al. Behavioral interventions improve condom use and hiv testing uptake among female sex workers in China: a systematic review and meta-analysis. AIDS Patient Care STDS. (2015) 29:454–60. doi: 10.1089/apc.2015.0043
35. Shi L, Liu G, Fu G, Zaller N, Wei C, Yang C, et al. Psychosocial and behavioral correlates with HIV testing among men who have sex with men during the COVID-19 pandemic in China. PLoS One. (2022) 17:e0262472. doi: 10.1371/journal.pone.0262472
36. Jiao K, Wei R, Li H, Chow EPF, Piqueiras E, Lewis T, et al. HIV testing frequency and associated factors among five key populations in ten cities of China: a cross-sectional study. BMC Infect Dis. (2022) 22:195. doi: 10.1186/s12879-022-07189-6
37. Wu ZY, Scott SR. Human immunodeficiency virus prevention strategies in China. Chin Med J (Engl). (2020) 133:318–25. doi: 10.1097/CM9.0000000000000647
38. Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China's response to HIV/AIDS. Lancet. (2007) 369:679–90. doi: 10.1016/S0140-6736(07)60315-8
39. Zhou Y, Cai YM, Li SL, Cao NX, Zhu XF, Wang F, et al. Anatomical site prevalence and genotypes of Chlamydia trachomatis infections among men who have sex with men: a multi-site study in China. BMC Infect Dis. (2019) 19:1041. doi: 10.1186/s12879-019-4664-1
40. Liang YY, Zhai HY, Li ZJ, Jin X, Chen Y, Chen SP, et al. Prevalence of Ureaplasma urealyticum, Chlamydia trachomatis, Neisseria gonorrhoeaeand herpes simplex virus in Beijing, China. Epidemiol Infect. (2018)14: e59. doi: 10.1017/S0950268818003163
41. Xue Y, Zheng H, Tang W, Mai Z, Huang J, Huang S, et al. Prevalence and genotype distribution of chlamydia trachomatis in urine among men attending sexually transmitted disease clinics in Guangdong Province, China, in 2016. Jpn J Infect Dis. (2018) 71:104–8. doi: 10.7883/yoken.JJID.2017.358
42. van Rooijen MS, van der Loeff MF, Morré SA, van Dam AP, Speksnijder AG, Vries de HJ, et al. Spontaneous pharyngeal Chlamydia trachomatis RNA clearance. a cross-sectional study followed by a cohort study of untreated STIS clinic patients in Amsterdam, The Netherlands. Sex Transm Infect. (2015) 91:157–64. doi: 10.1136/sextrans-2014-051633
43. Rohner E, McGuire FH, Liu Y, Li Q, Miele K, Desai SA, et al. Racial and Ethnic differences in acceptability of urine and cervico-vaginal sample self-collection for HPV-based cervical cancer screening. J Womens Health (Larchmt). (2020) 29:971–9. doi: 10.1089/jwh.2019.8132
44. Verougstraete N, Verbeke V, De Cannière AS, Simons C, Padalko E, Coorevits L, et al. To pool or not to pool? Screening of Chlamydia trachomatis and Neisseria gonorrhoeae in female sex workers: pooled versus single-site testing. Sex Transm Infect. (2020) 96:417–21. doi: 10.1136/sextrans-2019-054357
Keywords: sexually transmitted infections, prevalence, female sex worker, HIV, China
Citation: Shi L, Luo J, Chen Y, Chen L, Hu H, Qiu T, Liu X, Xu X, Chen Y, Zhang Z, Zhou Y, Lu J and Fu G (2022) Prevalence of syphilis and chlamydia trachomatis infection among female sex workers in Jiangsu, China: Results from a multicenter cross-sectional and venue-based study. Front. Public Health 10:1018724. doi: 10.3389/fpubh.2022.1018724
Received: 13 August 2022; Accepted: 14 October 2022;
Published: 31 October 2022.
Edited by:
Weiming Tang, University of North Carolina at Chapel Hill, United StatesReviewed by:
Chuanyi Ning, Guangxi Medical University, ChinaCopyright © 2022 Shi, Luo, Chen, Chen, Hu, Qiu, Liu, Xu, Chen, Zhang, Zhou, Lu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gengfeng Fu, ZnVnZkBqc2NkYy5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.