
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 09 January 2023
Sec. Disaster and Emergency Medicine
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1016649
 Emanuela Parotto1*
Emanuela Parotto1* Alessandro Lamberti-Castronuovo2,3
Alessandro Lamberti-Castronuovo2,3 Veronica Censi4
Veronica Censi4 Martina Valente2,3
Martina Valente2,3 Andrea Atzori4
Andrea Atzori4 Luca Ragazzoni2,3
Luca Ragazzoni2,3The COVID-19 pandemic exerted an extraordinary pressure on the Italian healthcare system (Sistema Sanitario Nazionale, SSN), determining an unprecedented health crisis. In this context, a multidisciplinary non-governmental initiative called Italian Response to COVID-19 (IRC-19) was implemented from June 2020 to August 2021 to support the Italian health system through multiple activities aimed to mitigate the effects of the pandemic. The objective of this study was to shed light on the role of NGOs in supporting the SSN during the first pandemic wave by specifically exploring: (1) the main challenges experienced by Italian hospitals and out-of-hospital care facilities and (2) the nature and extent of the IRC-19 interventions specifically implemented to support healthcare facilities, to find out if and how such interventions met healthcare facilities' perceived needs at the beginning of the pandemic. We conducted a cross-sectional study using an interviewer administered 32-item questionnaire among 14 Italian healthcare facilities involved in the IRC-19 initiative. Health facilities' main challenges concerned three main areas: healthcare workers, patients, and facilities' structural changes. The IRC-19 initiative contributed to support both hospital and out-of-hospital healthcare facilities by implementing interventions for staff and patients' safety and flow management and interventions focused on the humanization of care. The support from the third sector emerged as an added value that strengthened the Italian response to the COVID-19 pandemic. This is in line with the Health—Emergency and Disaster Risk Management (H-EDRM) precepts, that call for a multisectoral and multidisciplinary collaboration for an effective disaster management.
The SARS-CoV-2 outbreak and the related COVID-19 pandemic have been the worst public health challenge in recent Italian history, placing extraordinary pressure on the country's healthcare and long-term care systems, and on the economy as a whole (1–5). COVID-19 emerged in Italy with major clusters located in northern Italy, mainly around the cities of Codogno, Bergamo and Cremona in the Lombardy region, and around the cities of Vo' and Padua in Veneto region (6) (Figure 1). Subsequently, cases spread across the country with a more sustained transmission in neighboring regions (1). Two months after the beginning of the first COVID-19 wave, the estimated excess deaths in Lombardy, the hardest hit region in the country, reached a peak of more than 23,000 deaths. This is equivalent to an excess mortality of +118% compared to the average mortality rate of the period 1st January-−30th April 2015–2019 (7). In the context of a rapidly evolving pandemic situation, the Italian Health System (Servizio Sanitario Nazionale, SSN) struggled to deal with the surge of COVID-19 patients. The most immediate challenge that the SSN faced during the first wave was the rapid saturation of hospital Intensive Care Units (ICU) capacity (8). The consequences of the spread of the virus were felt also in out-of-hospital facilities, such as nursing homes and community hospitals. Nursing homes represented particularly fragile environments in which protection strategies and training came at a later stage compared to hospitals. Personal Protective Equipment (PPE) and swab tests were in short supply for hospital staff and were even more scarce in long-term-care institutions (9). This resulted in a very rapid spread of the virus: between February, 1st and April, 14th, 2020, ~40% of deaths in the nursing homes were associated with COVID-19 (9).
Italy developed an array of strategies to contain and mitigate the epidemic. These strategies included case-detection and contact-tracing, isolation and quarantine, physical distancing and mobility restrictions and a massive expansion of health care infrastructure and equipment (8, 10–13). Unfortunately, due to the novel aspects of the COVID-19 pandemic and to the sudden surge of patients, the SSN was unable to mount a unified response to the health crisis. Many Non-Governmental Organizations (NGOs) were mobilized to strengthen Italian healthcare facilities (14–16) and to support vulnerable populations (17, 18). The Italian NGO CUAMM—Doctors with Africa (hereinafter referred to as CUAMM) launched the Italian Response to COVID-19 (IRC-19) initiative, thanks to the support of the United States Agency for International Development (USAID) and the Center for Research and Training in Disaster Medicine, Humanitarian Aid, and Global Health (CRIMEDIM) at the University of Eastern Piedmont (Università del Piemonte Orientale, UPO), Novara, Italy (19) (Figure 2). This initiative had a duration of 14 months (June 2020–August 2021) and aimed at supporting the Italian health system through multiple activities across the territory for the prevention and mitigation of the effects of the COVID-19 pandemic (Figure 2). Within the IRC-19 initiative, four main fields of activity were defined: (1) supporting both hospital and out-of-hospital care facilities that had previously contacted the NGO asking for specific interventions to face the first pandemic wave; (2) promoting training initiatives with a focus on Global Health and Disaster Medicine topics; (3) increasing communities' awareness on pandemic-related issues; (4) providing assistance to vulnerable communities, e.g., homeless individuals (Appendix A in Supplementary material).
The objective of this study was to shed light on the role of NGOs in supporting SSN during the first pandemic wave by specifically exploring: (1) the main challenges experienced by Italian hospitals and out-of-hospital care facilities and (2) the nature and extent of the IRC-19 interventions specifically implemented to support healthcare facilities, in order to find out if and how such interventions met the healthcare facilities' perceived needs at the beginning of the pandemic.
We conducted a cross-sectional study using an interviewer-administered 32-item questionnaire (Appendix B in Supplementary material) among 14 Italian healthcare facilities from 5 different Italian regions (Lombardia, Trentino Alto-Adige, Veneto, Emilia-Romagna, Marche) involved in the IRC-19 initiative. The questionnaire was administered online from April 1st to May 31st, 2021, via the video conferencing tool Zoom. Two researchers conducted the interviews to collect responses to the questionnaire: one researcher actively asked the questions, and the other took notes throughout the interviews. All interviews were conducted in Italian and targeted people in managerial positions within the healthcare facilities. The average interview time was 30 min. Scientific literature was consulted (20–22) to develop the questionnaire. Such questionnaire (Appendix B in Supplementary material) predominantly relied on the World Health Organization (WHO) Emergency and Disaster Risk Management framework (H-EDRM) (23) and the United States Centers for Disease Control and Prevention (CDC) comprehensive hospital preparedness checklist for COVID-19 (24). The recommendations provided by the H-EDRM and the items selected from the CDC checklist were integrated in order to develop a guide aimed to explore the challenges experienced by the healthcare facilities related to healthcare workers, patients and structural/logistic features. Four different sections were distinguished: (a) general information about the healthcare facility; (b) basic characteristics of the facility; (c) main challenges experienced by the facility at the beginning of the first COVID-19 pandemic wave; (d) interventions implemented through the IRC-19 initiative. Data was collected in each healthcare facility in the period from June 1st, 2020, to April 1st, 2021. Each section included multiple choice questions that were integrated with additional comments provided by participants. Count, frequency, percentage, and mean/median scores were used to report descriptive statistics. The limited sample size and heterogeneity among healthcare centers did not allow to assess any statistical inference. Qualitative thematic analysis was used to analyze the open-ended answers provided by participants to supplement multiple choice questions (25). The qualitative analysis was performed following the Consolidated Criteria for Reporting Qualitative Research (COREQ) (26). Both descriptive statistical and qualitative results were reported as integrated with each other.
Stakeholders were contacted via email and information on the study objective, methodology and ethical implications was reported in the email. Written informed consent was obtained by all participants. The study was conducted according to the Declaration of Helsinki guidelines and approved by the Ethics Committee of the A.O.U. “Maggiore della Carità” in Novara (Study Number 015.059).
The 14 healthcare facilities that took part in this study belonged to the following categories: nursing homes (N = 5); community hospital (N = 1); community for people with addiction problems (N = 1); tertiary hospital wards (N = 5); field hospital (N = 1). Community hospitals are intended as short-term hospitalization facilities aimed to support patients who require low clinical intensity health interventions and who need continuous nursing health care/surveillance that is not available at home. The number of beds for each healthcare facility ranged from 38 to 1,220. The number of hospital admissions per year, reported per hospital ward, ranged from 3,600 to 40,000 (Table 1). The interviewed people were nurses (N = 7) and medical doctors (N = 7). All of them had managerial roles.
The challenges that Italian healthcare facilities faced during the first COVID-19 wave can be categorized in three main areas: (1) maintaining and supporting healthcare workforce (safety, training, and wellbeing), (2) providing care to patients, and (3) improving the infrastructure of the healthcare facilities (digitization and structural changes) (Table 2; Figure 3).
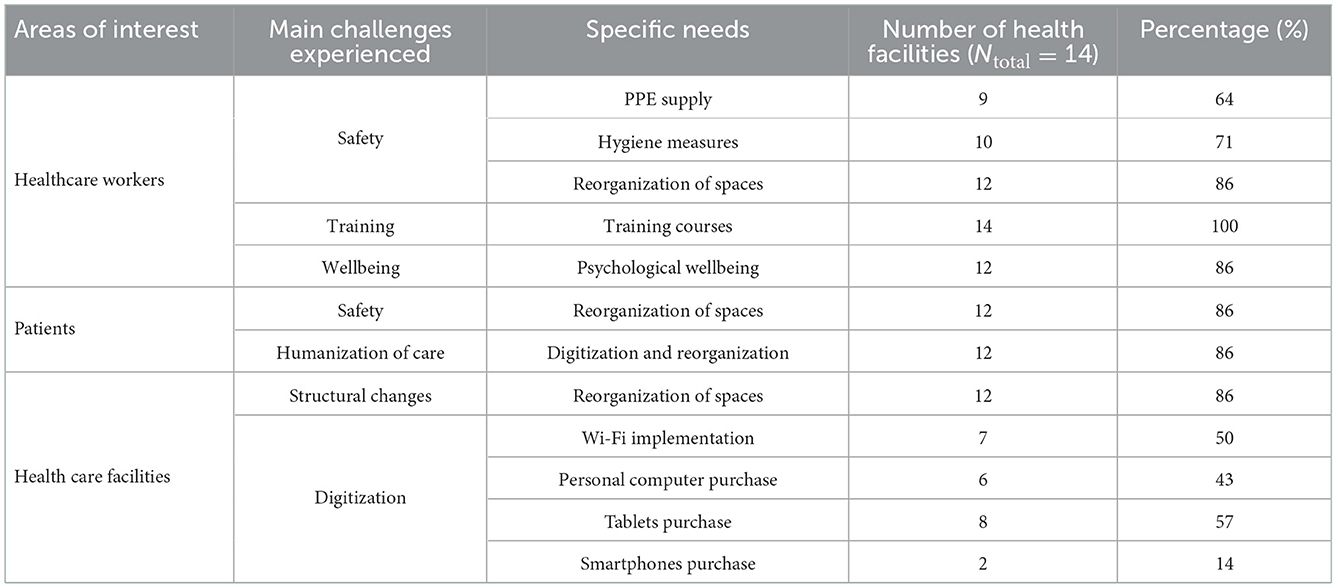
Table 2. Main challenges reported from different Italian healthcare facilities during the first COVID-19 pandemic wave (PPE, Personal Protective Equipment).
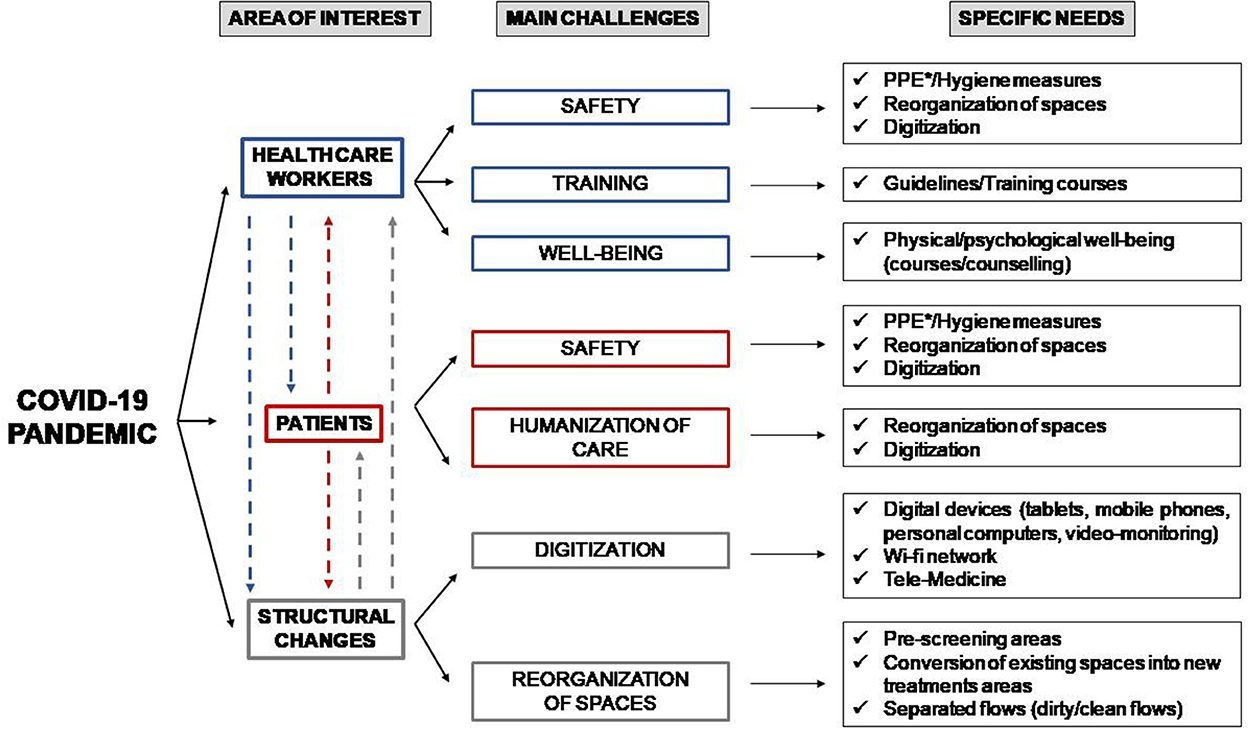
Figure 3. Main challenges experienced by both hospitals and out-of-hospital care facilities during the first pandemic wave. The three main areas of interest (healthcare workers, patients and structural changes) showed interdependence among each other. The interdependence is illustrated in the figure with dashed lines. *PPE, Personal Protective Equipment.
The challenges that the sudden surge of COVID-19 patients determined in each of the above mentioned sectors (healthcare workforce, patients, and healthcare facilities' infrastructure) are interdependent among each other. As an example, the surge in COVID-19 patients created challenges with HCWs' safety, training, and wellbeing (Figure 3). It also led to specific structural changes in the health facilities to expand existing treatment areas. The subsequent reorganization of spaces within healthcare facilities allowed to implement infection prevention and control measures and a safe management of patients, consequently leading to a redistribution of HCWs themselves within the healthcare facilities.
Most of the respondents (93%) considered safety of HCWs a primary concern. Issues in PPE availability and the lack of hand wash points were reported by 64% and 71% of the facilities, respectively: “At the beginning of the first pandemic wave we didn't have facial masks, not even surgical ones” (Nursing home, Trentino Alto-Adige); “At the beginning of the first pandemic wave we experienced a shortage of PPE. When we had the first positive patient in our facility, we didn't have adequate PPE to protect ourselves and other patients. Subsequently, the situation improved, but at first the supply was sufficient only for COVID-19 wards and not for all health professionals and patients” (Community hospital, Marche). Adequate training of HCWs concerning the proper use of PPE and the managing of COVID-19 patients was considered a priority by all respondents in order to ensure safety of the health professionals: “After receiving the proper training about the virus, we were able to overcome our fears” (Nursing home, Veneto). Moreover, 86% of the participants underlined the importance of ensuring the separation between dirty and clean areas. Alongside physical safety, a vast majority of respondents (86%) reported the need to manage severe psychological stress and to protect health workers' wellbeing as a major priority. The psychological stress was due to the spread of an unknown and severe disease with a high number of victims and to the need of working in unfamiliar environments with new protocols: “We were worn out and devastated. We have had a lot of deaths among our patients” (Nursing home, Trentino Alto –Adige); “The beginning of the pandemic felt almost like being swept away by an avalanche...At the beginning of the pandemic our pediatric unit was transformed into an adult COVID-19 unit. This change was extremely stressful for our healthcare workers, not used to managing adult patients” (Pediatric Hospital ward, Lombardia); “We were overwhelmed by the emergency and the massive influx of patients…We cried in the wards, in the offices…but we didn't have the time to organize psychological support for our workers” (Hospital, Lombardia). Protection of patients' safety emerged as a critical challenge in 86% of the health facilities considered. Many participants considered the reorganization of pre-existing spaces through the purchase of specific furnishings (62%) and the installation of automated doors (38%) as fundamental. This was done in order to ensure the separation between dirty and clean areas: “It was very difficult to guarantee the different dirty/clean paths due to the structural characteristics of our building” (Nursing home, Trentino Alto –Adige); “In our facility we had tight spaces … it was difficult to guarantee community life in safe conditions to our guests” (Nursing home, Veneto). In addition, many respondents (69%) underlined the need to develop new structures aimed to guarantee an adequate treatment area both for COVID-19 and non-COVID-19 patients. In order to ensure the best possible treatment to patients, many respondents (86%) considered providing humanized care despite the strict isolation measures imposed by the emergency as necessary (“our structure is built to foster community life”, Nursing home, Trentino Alto–Adige). The quick implementation of digital services was considered a major need at the beginning of the first pandemic wave. Many participants regarded the implementation of the Wi-Fi system (50%) and the purchase of digital devices (personal computers, 43%; tablets, 57% and mobile phones, 14%) as fundamental. These initiatives served to improve working conditions and the humanization of care.
The interventions implemented within the IRC-19 initiative can be grouped in three main sectors: (1) interventions for patients and staff safety; (2) for the positive/negative flow management of patients/HCWs; (3) for the humanization of care (Table 3).
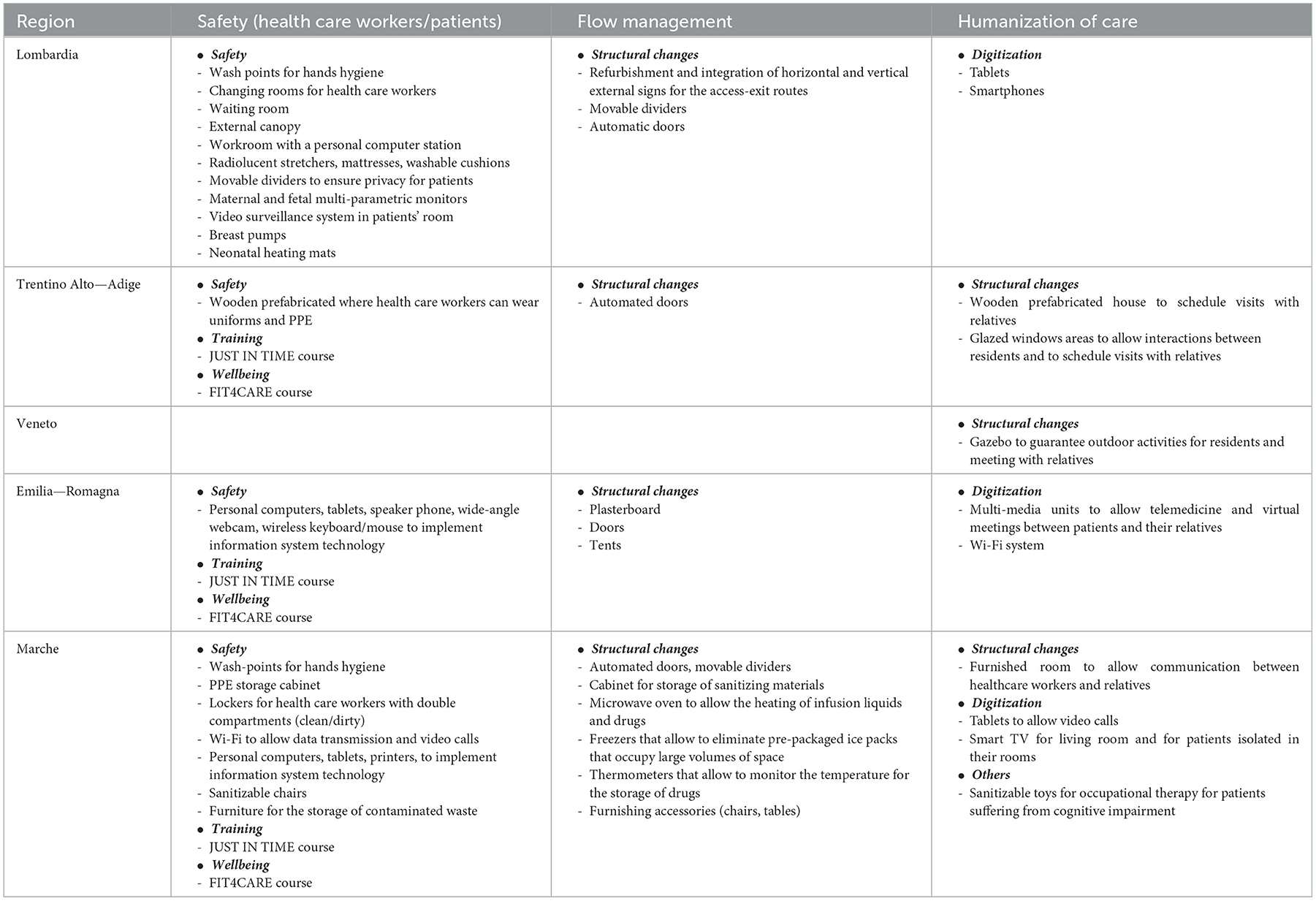
Table 3. IRC-19 interventions group according to five Italian regions involved in the study (PPE, Personal Protective Equipment).
IRC-19 interventions for patients and staff safety aimed at creating a safer environment for both HCWs and patients, reducing the risk of COVID-19 infection while ensuring the performance of the services and activities (“Feeling taken into consideration made us stronger and more confident in dealing with the pandemic”, Nursing home, Trentino Alto-Adige). The interventions performed included assembling temporary infrastructures (29%), purchasing new furniture (43%) and new lockers for HCWs (21%), renovating existing structures with the creation of new spaces (57%), installing new automated doors (21%) and hand wash-points (43%), creating warehouses for the storage of PPE (7%). The IRC-19 initiative contributed to ensuring occupational health and safety strengthening HCWs' training with the realization of two free modular training packages called JUST IN TIME and FIT4CARE, performed in 64% of the health facilities enrolled in this study: “FIT4CARE course was much appreciated…concerning the issue of health professional well-being we didn't receive support from our hospital” (Pediatric ward, Emilia—Romagna).
The IRC-19 interventions for the positive/negative flow management of patients/HCWs aimed at managing the flows of patients, residents, visitors and HCWs entering and leaving the facilities and preventing the spread and contamination of the virus. This was possible thanks to the improvement and re-organization of the entry-exit routes of the facilities (21%), and the purchase of specific furnishings such as movable dividers to guarantee patients' privacy or to perform medical visits in safety (36%).
Many IRC-19 interventions were aimed at ensuring humanized care despite the isolation measures. The interventions performed ranged from the implementation of the Wi-Fi network (50%) to the purchase of mobile phones and tablets (64%): “Thanks to the IRC-19 initiative we implemented a tele-surveillance system for COVID-19 patients during labor and after delivery” (Obstetric ward, Lombardia); “We received tablets that allowed our COVID-19 patients to communicate with their relatives and to see their newborns in case they were admitted to Neonatal Intensive Care Unit after the delivery” (Obstetric ward, Lombardia). Moreover, prefabricated buildings (36%) were constructed, where family visits were allowed: “The family house given by this project represents an important additional value for our institute and our community. It has gathered admiration and positive comments among public opinion and in the media. It gave us the opportunity to react and to leave no one behind” (Nursing home, Trentino Alto-Adige); “Thanks to this project we had the possibility to re-organize our spaces for meetings and social interaction for our residents...Thanks to this project we will be able to open our institute to the community” (Nursing home, Veneto).
Notably, these interventions promoted the use of telemedicine both for patients and HCWs: “Thanks to these interventions we have managed to maintain the psychological well-being of our guests. We have managed to carry out the activities that are essential for our community. During the pandemic period we have not observed an increase in dropout rates among our guests” (Community for people with addiction problems, Emilia Romagna).
The main needs experienced by different Italian healthcare facilities concerned three main areas: HCWs (safety, training, and wellbeing), patients (safety and humanization of care) and structural changes (reorganization of spaces and digitization). Specific strategies were implemented to meet such needs. Despite the different specificities, it should be noticed that the three main groups mutually interacted (Figure 3), suggesting that they have to be considered all together in planning successful pandemic responses. With regard to the IRC-19 interventions, it is possible to identify three main target areas: interventions targeting staff and patients' safety, interventions targeting patients/health professionals flow management and interventions aimed to ensure humanization of care (Table 3). The entirety of the IRC-19 interventions supported the healthcare facilities involved in this study by promptly addressing the main needs experienced by the healthcare facilities during the first pandemic wave.
The shortage and improper use of PPE, that was mainly seen in out-of-hospital facilities, represented one of the major challenges encountered. This confirms the results of previous studies targeting nursing homes that highlighted not only the shortage of PPE during the first pandemic wave but also the late implementation of response strategies at this level compared to hospitals (27). The need to reshape health services delivery by improving primary and community care provision was already suggested in recent publications as a fundamental strategy to face health pandemic challenges and render communities more resilient (28). Strengthening primary and community care services might contribute to reducing the surge of avoidable hospitalizations for Ambulatory Care Sensitive conditions (ACSCs) that persist in the long term after disasters, as it was shown in a recent literature review (29). Furthermore, the respondents considered adequate training of HCWs as fundamental to guarantee safety and protection and to face the impact of the pandemic, reflecting findings reported in previous studies (30). Concerning HCWs' wellbeing, a relevant challenge identified in this study was the significant psychological stress to which the staff was exposed during the first pandemic wave. Scientific literature has previously documented the negative impact on HCWs' psychological health during the pandemic (24, 25). This is mainly attributable to the increased workload together with the shortage of adequate PPE and the absence of an evidence-based treatment (24, 25). The lack of adequate training (30, 31), the fear of contagion (32) and the management of quickly deteriorating patients (32–34) are additional factors mentioned in the literature.
The COVID-19 pandemic has altered the way patients and families endure illness and death and has emphasized the importance of being culturally prepared to face suffering and death to such a large extent (35–38). In this study, the lack of a “humanized care” was mainly felt in nursing homes and community hospitals, where patients' relational aspects with the community and the outside world are of paramount importance. Similarly, obstetric and pediatric units underlined the need to protect relationships between mothers and children despite the restriction measures.
With regard to the health facilities' structural changes described in this study, several measures were reported as fundamental to guarantee adequate infection prevention and control: (1) the ability for hospitals to retrofit or reallocate parts of their facilities in order to ensure separate emergency entrances for contagious patients, (2) having patients' pre-screening and treatment areas; (3) having separation between patients, visitors, and staff, based on their level of contagion. These are all measures that need to be considered when defining health facilities' preparedness strategies (39).
In addition to structural changes, the implementation of digitization was reported as a relevant measure both to facilitate relationships between HCWs/patients/caregivers and to allow remote medical consultations. The adoption of telemedicine emerged as a global theme during the COVID-19 pandemic (35–37). In this regard, the Italian Ministry of Health, together with the Ministry for Technology Innovation and Digitization and the WHO, launched an open call to implement telemedicine and monitoring system technologies (40) in the health facilities. However, many Italian hospitals lack adequate infrastructure for effective telemedicine platforms, due to supply-chain breakdown and insufficient internet capabilities (41). The IRC-19 initiative contributed to address these needs providing support with the implementation of digital technologies.
The first IRC-19 intervention area was aimed to guarantee staff and patients safety through structural changes and training strategies. Structural changes included the creation of specific prefabricated buildings, the purchase of specific furniture and devices (automated doors, lockers, wash points for hand hygiene, warehouse for PPE storage) and the renovation of existing structures with the creation of new spaces and the installation of temporary infrastructures. The measures taken were considered as essential by most of the participants in order to establish an adequate Infection Prevention and Control (IPC) system within the healthcare facilities affected by the pandemic crisis.
Training strategies were developed as online teaching learning sessions (OTL) and included the JUST IN TIME and the FIT4CARE courses. The JUST IN TIME course focused on disasters and COVID-19 management principles and offered take-home messages to support healthcare workers struggling with the lack of knowledge and the absence of evidence-based treatments. The FIT4CARE course was aimed to improve healthcare professionals' wellbeing offering feasible and easy-to-apply tools provided by experts in Nutrition, Fitness training and Psychology. It facilitated healthcare workforce in facing the intense physical and mental fatigue experienced during the first pandemic wave.
The second IRC-19 intervention area focused on the appropriate flow-management within the healthcare facilities. It included the purchase of specific furniture (movable dividers and automated doors), the installation of new buildings (gazebos and tents) and the delineation of different clean/dirty pathways. Reorganizing spaces efficiently was considered as a fundamental intervention in most of the healthcare facilities involved in this project due to the fact that it helped to create a safer environment reducing the risk of the contagion and the spread of the virus.
The third IRC-19 intervention concerned the need to ensure humanized care with a patient-centered approach despite social distancing and restrictive safety measures. The possibility to guarantee an appropriate relationship between patients and HCWs and between patients and their families was an important need experienced both in hospital wards and in community hospitals/nursing homes. In hospitals, interventions to guarantee the humanization of care were mainly requested in maternal and obstetric units. The installation of a Wi-Fi monitoring and of a video/audio system for maternal and fetal surveillance in each patient room allowed health professionals to constantly interact with patients during labor and after delivery, reducing movement across different areas. The purchase of tablets ensured the communication in the post-partum period between mothers and their newborns or relatives in case of women with prolonged hospital stay or newborns admitted in Neonatal Intensive Care Unit. The purchase of breast pumps and heating mats were aimed at protecting and maintaining the relationship between mothers and newborns in the COVID-19 maternal unit. In nursing homes maintaining human relations was considered fundamental for the protection of patients' health. The installation of new buildings (e.g., wooden houses and a gazebo with lighting and heating systems) allowed to schedule visits of family members in accordance with safety procedures. Moreover, the implementation of digitization systems (Wi-Fi, personal computers, webcam) helped guests to maintain some contact with their relatives and allowed telemedicine consultations.
The digitization measures adopted thanks to the support of the IRC-19 initiative played an important role in assisting healthcare facilities to face multiple pandemic challenges. The implementation of digital technologies was perceived as fundamental to ensure the continuity of care through remote medical consultations and to support the relationships between patients and family members in spite of the containment measures. Moreover, the possibility to provide medical consultations remotely reduced the risk of contagion both for healthcare professionals and patients contributing to creating a safer environment and to reducing the fear of contagion.
In conclusion, the IRC-19 initiative supported Italian health care facilities in facing the main challenges encountered during the first pandemic wave, stepping in to fill some unmet needs when the SSN was overwhelmed. Recent studies showed that NGOs globally played a significant role when national governments alone couldn't manage to fulfill the needs of the population (42–44), but scientific publications concerning this topic were missing at the time of writing this manuscript. The findings of this study confirmed the results of previous publications that have emphasized the importance of NGOs' role in supporting countries when emergencies and disasters occur (45, 46). The solid working experience with vulnerable and marginalized people in low resource settings, the closer connection with the communities and the adoption of more flexible bureaucratic processes were identified among the main factors that allow these organizations to respond more quickly to crises (43).
These reflections are closely related to the main foundations reported by the H-EDRM framework (23). The effective management of the challenges that the COVID-19 pandemic posed to the Italian health system required multisectoral and multidisciplinary collaboration to be solved. Recent findings shown that the interconnection of different sectors (e.g., PHC, hospital and third sector) with a decentralized distribution of services to primary and community care was key for overcoming challenges posed by the COVID-19 pandemic (30). Within the context of multisectoral collaboration, strong relationships between healthcare facilities and the third sector represented an irreplaceable strategy to face the pandemic disaster during the first wave.
The main limitations concerned the small sample size and the heterogeneity of the healthcare facilities involved. The small sample size didn't allow to assess any statistical inference concerning quantitative data. Nevertheless, the number of participants interviewed followed the principle of qualitative data saturation in accordance to the Consolidated Criteria for Reporting Qualitative Research (COREQ) (26). The heterogeneity of the sample encompassed both the different patients' admission capacity and the different typology of healthcare facilities involved. Although the absence of an homogeneous population entailed some important limitations, it offered a broader set of perspectives to evaluate the impact of COVID-19 pandemic on the Italian health system.
In addition, we considered health care facilities supported by the same non-governmental project. Hence, other strategies in support of the SSN (i.e., other non-governmental organizations, private sector, and private-public partnerships) were not considered. Further studies are needed to expand the sample and to prove the involvement of the third sector in the health management of disasters.
The COVID-19 pandemic has exerted extraordinary pressure on the entire SSN, both on hospitals and out-of-hospital healthcare facilities. The crisis of the first pandemic wave made it difficult for the SSN to homogeneously guarantee an immediate and effective support to all the challenges experienced by the different Italian health care facilities. In this complex context, the IRC-19 initiative represented an instrument to fill this gap, allowing to support and strengthen both hospitals in the frontline against the virus as well as out-of-hospital healthcare facilities that were nevertheless severely hit. The support from the third sector emerged as an added value that strengthened the Italian response to the COVID-19 pandemic disaster.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
EP designed the study and drafted the manuscript. EP and VC conducted the data collection. AL-C, MV, VC, AA, and LR completed and revised the drafted manuscript. All authors have approved the final version of the manuscript for submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1016649/full#supplementary-material
1. Riccardo F, Ajelli M, Andrianou XD, Bella A, Del Manso M, Fabiani M, et al. Epidemiological characteristics of COVID-19 cases and estimates of the reproductive numbers 1 month into the epidemic, Italy, 28 January to 31 March 2020. Euro Surveill. (2020) 25:2000790. doi: 10.2807/1560-7917.ES.2020.25.49.2000790
2. Harapan H, Itoh N, Yufika A, Winardi W, Keam S, Te H, et al. Coronavirus disease 2019 (COVID-19): a literature review. J Infect Public Health. (2020) 13:667–73. doi: 10.1016/j.jiph.2020.03.019
3. Liu YC, Kuo RL, Shih SR. COVID-19: The first documented coronavirus pandemic in history. Biomed J. (2020) 43:328–33. doi: 10.1016/j.bj.2020.04.007
4. Bandera A, Aliberti S, Gualtierotti R, Baldini M, Blasi F, Cesari M, et al. COVID-19 Network: the response of an Italian Reference Institute to research challenges about a new pandemia. Clin Microbiol Infect. (2020) 26:1576–8. doi: 10.1016/j.cmi.2020.06.028
5. Armocida B, Formenti B, Ussai S, Palestra F, Missoni E. The Italian health system and the COVID-19 challenge. Lancet Public Health. (2020) 5:e253. doi: 10.1016/S2468-2667(20)30074-8
6. EpiCentro. Sorveglianza Integrata COVID-19: i principali dati nazionali. Available online at: https://www.epicentro.iss.it/coronavirus/sars-cov-2-sorveglianza-dati (accessed August 6, 2021).
7. Wei PF. Diagnosis and treatment protocol for novel coronavirus pneumonia (Trial Version 7). Chin Med J (Engl). (2020) 133:1087–95. doi: 10.1097/CM9.0000000000000819
8. Carenzo L, Costantini E, Greco M, Barra FL, Rendiniello V, Mainetti M, et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. (2020) 75:928–34. doi: 10.1111/anae.15072
9. EpiCentro. Survey sul contagio da COVID-19 nelle RSA. Available online at: https://www.epicentro.iss.it/coronavirus/sars-cov-2-survey-rsa (accessed August 7, 2021).
10. Villa S, Lombardi A, Mangioni D, Bozzi G, Bandera A, Gori A, et al. The COVID-19 pandemic preparedness or lack thereof: from China to Italy. Glob Health Med. (2020) 2:73–7. doi: 10.35772/ghm.2020.01016
11. Aliberti S, Amati F, Pappalettera M, Di Pasquale M, D'Adda A, Mantero M, et al. COVID-19 multidisciplinary high dependency unit: the Milan model. Respir Res. (2020) 21:260. doi: 10.1186/s12931-020-01516-8
12. Goh KJ, Wong J, Tien JCC, Ng SY, Duu Wen S, Phua GC, et al. Preparing your intensive care unit for the COVID-19 pandemic: practical considerations and strategies. Crit Care. (2020) 24:215. doi: 10.1186/s13054-020-02916-4
13. Gazzetta Ufficiale. Available online at: https://www.gazzettaufficiale.it/eli/id/2020/03/09/20G00030/sg (accessed January 12, 2022).
14. Sanfelici M. The Italian response to the COVID-19 crisis: lessons learned and future direction in social development. Int J Commun Soc Dev. (2020) 2:191–210. doi: 10.1177/2516602620936037
15. UNICEF Supplies Arrive in Italy to Support COVID-19 Response. Available online at: https://www.unicef.org/press-releases/unicef-supplies-arrive-italy-support-covid-19-response (accessed January 23, 2022).
16. Platform EL. Coronavirus: NGOs and Philanthropists Stepping Up During the Pandemic. Liberties.eu. Available online at: https://www.liberties.eu/en/stories/coronavirus-ngos-philanthropists-step-up-pandemic/18707 (accessed January 23, 2022).
17. Editoriale-Barbieri_ENG_Web.pdf. Available online at: https://mediciperidirittiumani.org/medu/wp-content/uploads/2020/05/33300_Editoriale-Barbieri_ENG_Web.pdf (accessed January 23, 2022).
18. Italian NGO Calls for Migrant Protection Amid Coronavirus. InfoMigrants. (2020). Available online at: https://www.infomigrants.net/en/post/23694/italian-ngo-calls-for-migrant-protection-amid-coronavirus (accessed January 23, 2022).
19. casagrande. IRC19 | A Commitment Year in Italy. Doctors with Africa CUAMM. (2021). Available online at: https://doctorswithafrica.org/en/whats-new/news/irc19-a-commitment-year-in-italy/ (accessed May 30, 2022).
20. Boynton PM. Administering, analysing, and reporting your questionnaire. BMJ. (2004) 328:1372–5. doi: 10.1136/bmj.328.7452.1372
21. Rattray J, Jones MC. Essential elements of questionnaire design and development. J Clin Nurs. (2007) 16:234–43. doi: 10.1111/j.1365-2702.2006.01573.x
22. Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ. (2004) 328:1312–5. doi: 10.1136/bmj.328.7451.1312
23. World Health Organization. Health Emergency and Disaster Risk Management Framework. World Health Organization (2019). xi, p. 31. Available online at: https://apps.who.int/iris/handle/10665/326106 (accessed April 19, 2022).
24. CDC. Healthcare Workers. Centers for Disease Control and Prevention (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/hcp-personnel-checklist.html (accessed January 12, 2022).
25. Braun_2006_Using.pdf. Available online at: https://jnoll.nfshost.com/7COM1085-spring-21/readings/Braun_2006_Using.pdf (accessed January 7, 2022).
26. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
27. sars-cov-2-survey-rsa-rapporto.pdf. Available online at: https://www.epicentro.iss.it/coronavirus/pdf/sars-cov-2-survey-rsa-rapporto.pdf (accessed August 7, 2021).
28. Lamberti-Castronuovo A, Valente M, Cretu A, Dal Molin A. Decentralization of healthcare during crises: riding the wave of post-pandemic health system reforms to rethink health workforce. Int J Disaster Risk Reduct. (2022) 76:103040. doi: 10.1016/j.ijdrr.2022.103040
29. Lamberti-Castronuovo A, Valente M, Aleni C, Hubloue I, Ragazzoni L, Barone-Adesi F. Using ambulatory care sensitive conditions to assess primary health care performance during disasters: a systematic review. Int J Environ Res Public Health. (2022) 19:9193. doi: 10.3390/ijerph19159193
30. Lamberti-Castronuovo A, Parotto E, Della Corte F, Hubloue I, Ragazzoni L, Valente M. The COVID-19 pandemic response and its impact on post-corona health emergency and disaster risk management in Italy. Front Public Health. (2022) 10:1034196. doi: 10.3389/fpubh.2022.1034196
31. Wu D, Wu T, Liu Q, Yang Z. The SARS-CoV-2 outbreak: what we know. Int J Infect Dis. (2020) 94:44–8. doi: 10.1016/j.ijid.2020.03.004
32. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
33. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. (2020) 9:241–7. doi: 10.1177/2048872620922795
34. Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. (2003) 168:1245–51.
35. Peek N, Sujan M, Scott P. Digital health and care in pandemic times: impact of COVID-19. BMJ Health Care Inform. (2020) 27:e100166. doi: 10.1136/bmjhci-2020-100166
36. Temesgen ZM, DeSimone DC, Mahmood M, Libertin CR, Varatharaj Palraj BR, Berbari EF. Health care after the COVID-19 pandemic and the influence of telemedicine. Mayo Clin Proc. (2020) 95:S66–8. doi: 10.1016/j.mayocp.2020.06.052
37. Bhaskar S, Bradley S, Chattu VK, Adisesh A, Nurtazina A, Kyrykbayeva S, et al. Telemedicine across the globe-position paper from the COVID-19 pandemic health system resilience PROGRAM (REPROGRAM) international consortium (Part 1). Front Public Health. (2020) 8:556720. doi: 10.3389/fpubh.2020.556720
38. Rivi V, Melegari G, Blom JMC. How to humanise the COVID-19 intensive care units. BMJ Evid Based Med. (2021). 26:bmjebm-2020-111513. doi: 10.1136/bmjebm-2020-111513
39. Pandemic Preparedness: How Hospitals Can Adapt Buildings to Address Worst-Case Scenarios. Available online at: https://www.stantec.comcovid-19/pandemic-preparedness-how-hospitals-can-adapt-buildings-to-address-worst-case-scenarios (accessed August 2, 2021).
40. Innova per l'Italia. Available online at: https://innovaperlitalia.agid.gov.it/call2action/index.html (accessed August 2, 2021).
41. Webster P. Virtual health care in the era of COVID-19. Lancet. (2020) 395:1180–1. doi: 10.1016/S0140-6736(20)30818-7
42. Shin YA, Yeo J, Jung K. The effectiveness of international non-governmental organizations' response operations during public health emergency: lessons learned from the 2014. Ebola outbreak in Sierra Leone. Int J Environ Res Public Health. (2018) 15:E650. doi: 10.3390/ijerph15040650
43. Jaysawal N. Role of non-governmental organization (NGO) in social capital: a review. Asian J Res Soc Sci Human. (2017) 7:341. doi: 10.5958/2249-7315.2017.00354.9
44. Hu M, Sidel M. Civil society and COVID in China: responses in an authoritarian society. Nonprofit Vol Sector Quart. (2020) 49:1173–81. doi: 10.1177/0899764020964596
45. Cancedda C, Davis SM, Dierberg KL, Lascher J, Kelly JD, Barrie MB, et al. Strengthening health systems while responding to a health crisis: lessons learned by a nongovernmental organization during the Ebola virus disease epidemic in Sierra Leone. J Infect Dis. (2016) 214:S153–63. doi: 10.1093/infdis/jiw345
Keywords: COVID-19 pandemic, Italian's healthcare system, health crisis, response, lessons learned, third sector, H-EDRM
Citation: Parotto E, Lamberti-Castronuovo A, Censi V, Valente M, Atzori A and Ragazzoni L (2023) Exploring Italian healthcare facilities response to COVID-19 pandemic: Lessons learned from the Italian Response to COVID-19 initiative. Front. Public Health 10:1016649. doi: 10.3389/fpubh.2022.1016649
Received: 11 August 2022; Accepted: 20 December 2022;
Published: 09 January 2023.
Edited by:
Shusen Sun, Western New England University, United StatesReviewed by:
Raffaele Campisi, Azienda Ospedaliera Universitaria Policlinico G. Rodolico-San Marco, ItalyCopyright © 2023 Parotto, Lamberti-Castronuovo, Censi, Valente, Atzori and Ragazzoni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emanuela Parotto,  ZW1hbnVlbGEucGFyb3R0b0BnbWFpbC5jb20=
ZW1hbnVlbGEucGFyb3R0b0BnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.