- 1Department of Chronic Disease Control and Prevention, Tai'an Center for Disease Control and Prevention, Tai'an, China
- 2Tai'an Maternal and Child Health Care Hospital, Tai'an, China
- 3Department of Vascular Cardiology, Tai'an Central Hospital, Tai'an, China
- 4Department of Hematology, Second Affiliated Hospital of Shandong First Medical University, Tai'an, China
Objectives: To examine the association of protein intake from different sources with cognitive decline.
Methods: Our analysis included 3,083 participants aged 55–93 years from the China Health and Nutrition Survey. Cognition was assessed in 1997, 2000, 2004, 2006, and 2015. Diet intake was assessed using weighing methods in combination with 24-h dietary recalls for three consecutive days at each survey.
Results: Participants consumed 13.94% of energy intake from total protein, with 11.47 and 2.47% from plant and animal sources, respectively. During a follow-up of 9 years, participants in quintile 5 of plant protein intake (% energy) had a higher risk [odds ratio (95% CI): 3.03 (1.22–7.53)] of cognitive decline compared with those in quintile 1. Higher animal protein intake (% total protein) was associated with a lower risk of cognitive decline [odds ratio (95% CI) for quintile 5 vs. quintile 1: 0.22 (0.07–0.71)]. Grains (plant source) protein intake was inversely but fish/shrimp and poultry (animal source) protein intake were positively associated with change in cognitive Z-score.
Conclusion: Increasing animal protein consumption in a population with plant dominant diets may help to prevent cognitive decline.
Introduction
The global number of individuals with dementia increased from 20.2 million in 1990 to 43.8 million in 2016 (1). Notably, China accounted for approximately one-quarter of the worldwide dementia population in 2016 (2). While the age-standardized prevalence of dementia worldwide increased by 1.7% from 1990 to 2016, in China, it increased by 5.6% during this same period (2). The epidemic of dementia and its subsequent cost impose a tremendous burden on economics and health system in China (3). This will become a more important concern with the increased aging population in China, therefore, it is imperative to target intervention priorities for the prevention of dementia and cognitive decline.
Diabetes, smoking, physical inactivity, and unhealthy dietary patterns have been identified as important modifiable risk factors for dementia (4, 5). Increasing evidence has shown that healthy dietary patterns are associated with a lower risk of cognitive decline and dementia, but the association between the intake of individual foods or nutrients and cognitive decline is inconsistent across studies (6–8).
Prospective studies investigating dietary patterns have highlighted the importance of foods rich in protein including grains, nuts, beans, fish, and poultry on the prevention of dementia (9, 10). Furthermore, animal and plant protein intakes have been shown to have divergent associations with well-known dementia risk factors including diabetes, hypertension, obesity, and metabolic syndrome (11, 12). This suggests the protein intake from different food sources may have different associations with cognitive decline. Several studies from Western countries with animal dominant diets have investigated the association between protein intakes from different sources and cognitive function with inconsistent findings (13, 14). However, no such data are available from Asian countries with plant dominant diets.
In this paper, we aimed to examine whether the protein intake from animal and plant foods and main food groups were predictive of cognitive decline. We also aimed to test the association between the composition of animal and plant proteins and cognitive decline.
Materials and methods
Participant selection
The China Health and Nutrition Survey (CHNS) is an ongoing open-cohort study initiated in 1989 and followed up in 1991, 1993, 1997, 2000, 2004, 2006, 2009, 2011, and 2015. The design and sampling have been detailed elsewhere (15, 16). Briefly, a multistage, random cluster process was used to select participants in nine provinces from northeast to southwest in China. Two cities and four counties were randomly selected in each province based on their income levels as reported by the State Statistical Bureau in 1988. Four communities in each city or county and 20 households in each community were then randomly selected. The response rate, based on those who participated in 1989, in the 2006 survey was >60%. Overall response rates, based on those who participated in at least two surveys, were around 88% at the individual level and 90% at the household level (15). Cognitive assessment in a sub-cohort of participants aged ≥55 years was conducted in 1997, 2000, 2004, 2006, and 2015. Of the 38,536 individuals who participated in any of the ten surveys, the following were excluded from the present analysis: those aged <55 years (n = 32,083), those who did not have cognitive function assessed (n = 2,207), those who completed the cognitive assessment at only one survey (n = 908), or those who had stroke, heart disease, or cancer at baseline (n = 255). A total of 3,083 participants were included in the final analysis (Figure 1).
The survey was approved by the institutional review committees of the University of North Carolina at Chapel Hill and the National Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention. Written informed consent was obtained from all participants.
Dietary assessment
Dietary intake, at the household level and the individual level, was assessed using weighing methods in combination with 24-h dietary recalls for three consecutive days at each survey. All foods and condiments for the home food inventory at the beginning and end of the 3-day survey period were measured using scales and recorded by trained interviewers. Individual dietary data for the same three consecutive days were recorded for all household members and proportions of foods and condiments consumed at the household level were allocated to each individual (17). Food and nutrient intake at the individual level was then calculated.
Nutrients and energy intake was calculated based on the China Food Composition (18). We computed the protein intake from different sources separately by multiplying daily consumption by the protein content and summing this across foods/beverages. Foods were grouped as plant or animal sources and further broken down into grains, tubers, vegetables, fruits, beans, nuts (plant sources), red meat, poultry, fish/shrimp, dairy, and eggs (animal sources). The average annual protein intake from different sources of the surveys completed before the first cognitive assessment was also calculated.
The assessment of energy intake has been validated by using the doubly labeled water method with a correlation efficient of 0.56 for men and 0.60 for women (19).
Cognitive function test
A subset of the items from the Telephone Interview for Cognitive Status–modified was used to assess cognitive function (20). The tool has been adopted in other population studies in China (21, 22). The cognitive screening included the immediate and delayed recall of a 10-word list, counting backward from 20, and serial seven subtraction from 100 for five times. Each correctly recalled word was assigned a score of 1 and the total score for immediate and delayed recall ranged from 0 to 20. For counting backward, a score of 2 was given to those counted backward correctly in the first try and one to those only counted backward correctly in the second try. A score of 1 was assigned to each of the 5 serial subtractions and the total score for serial seven subtraction ranged from 0 to 5.
The composite cognitive Z-score was computed by summing the scores of all three tasks and ranged from 0 to 27. The composite cognitive Z-score was analyzed in Z-score and a higher score represented better cognitive function. The change in composite cognitive Z-score was computed by subtracting the score at baseline from that at follow-up. Cognitive decline was defined as change in composite cognitive Z-score below the mean minus two standard deviations (SDs). This was retested by change in the composite cognitive Z-score below the mean minus 1.5 SDs.
Physical examinations
Height was measured using a freestanding stadiometer and weight was measured using an electronic scale. Body mass index (BMI) was calculated based on weight and height, and overweight/obesity was defined as BMI ≥ 25 kg/m2 (23).
Blood pressure was measured using a standard mercury sphygmomanometer by trained nurses. Three measurements were taken to the nearest two mmHg and the average of the last two was used.
Confounders
All confounders at the time of the first cognitive measure were used in the analysis. Demographic socioeconomic factors included age, gender, region, education, smoking, and alcohol consumption were collected using a questionnaire. Physical activity was assessed based on hours per week spent in different occupational, household, transportation, and leisure-time activities, from which metabolic equivalent of task (MET) was calculated (24). History of diabetes was also self-reported.
Statistical analysis
Data were expressed as frequency (percentage) and means ± SDs. ANOVA for continuous variables and the Chi-square test for categorical variables was performed to compare the difference of baseline characteristics across the quintiles of protein intake.
Participants were divided into quintiles based on the % energy from protein from major food sources at baseline. General linear regression models were used to obtain coefficients for the change in composite cognitive Z-score for quintiles 2–5 vs. the quintile 1 and per 1% increment in energy intake from animal foods, plant foods, grains, tubers, vegetables, fruits, beans, nuts, red meat, poultry, fish, dairy, and eggs. The following models were tested: (1) age and gender; (2) model 1 plus education, urbanization, duration of follow-up, smoking, alcohol intake, physical activity, composite cognitive Z-score, diabetes, BMI, systolic, and diastolic blood pressure at baseline; (3) model 2 plus intake of energy, sodium, potassium, fat, and fiber. We also calculated the linear trend by assigning participants the median intake within each quintile of the percentage of energy from dietary protein for each food source. Logistic regression models were used to examine whether protein intakes from different food sources were associated with cognitive decline.
Whether the composition of animal and plant protein intake (% total protein) was predictive of the change in composite cognitive Z-score and cognitive decline was also examined where total protein intake was further adjusted for.
Moderation analysis was used to test whether the association between protein intake and cognitive decline depended on other important factors. Moderation analysis was conducted to examine whether the association of plant and animal protein intake with cognitive decline was modified by age, gender, education, urbanization, and follow-up duration.
Sensitivity analysis was conducted to examine whether the association of the average annual protein intake of surveys completed before the first cognitive assessment with changes in cognitive Z-scores.
Analyses were performed using SAS version 9.4 (SAS Institute Inc.) and all P-values were two-sided.
Results
Participant characteristics
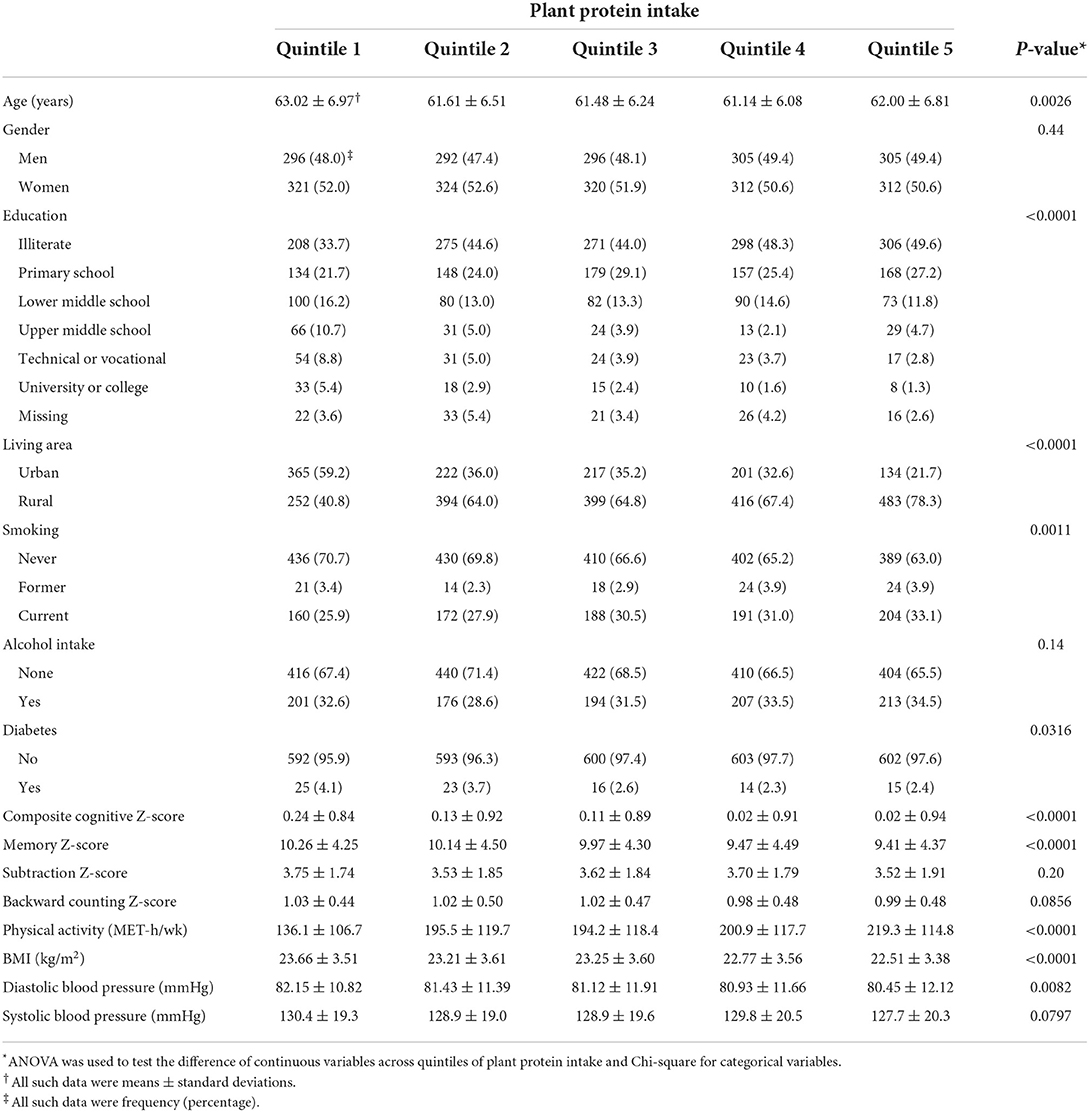
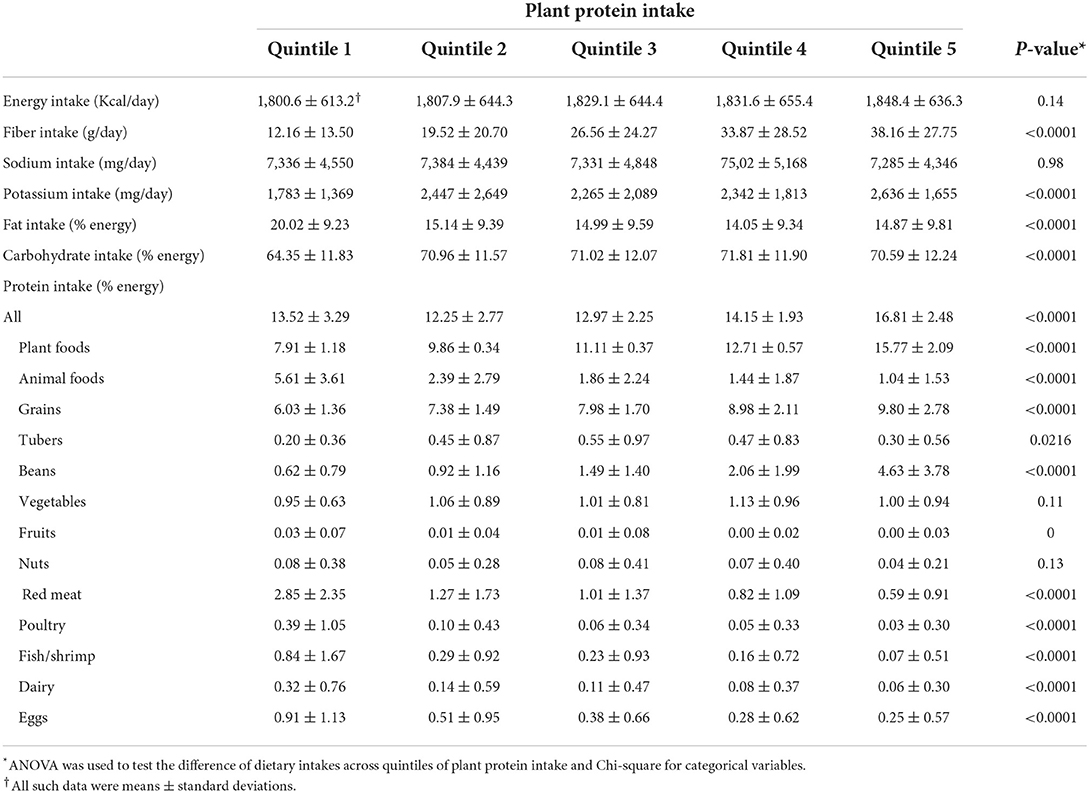
A total of 3,083 participants (51.5% women) aged 55–93 (mean ± SD: 61.9 ± 6.6) years at baseline with complete data on variables of interest were included in the analysis. Individuals with a higher plant protein intake were more likely to have lower education, live in rural areas, currently smoke, and have higher physical and occupation activity levels compared to those with a lower plant protein intake. An inverse association between plant protein intake and composite cognitive Z-scores at baseline was observed (Tables 1, 2). In contrast, higher animal protein intake was associated with lower energy intake, lower fiber intake, and higher sodium intake. There was a positive association between the animal protein intake and the composite cognitive Z-score at baseline (Supplementary Table 1).
Protein intake
Participants consumed 13.94% of the energy intake from total protein, with 11.47% from plant protein and 2.47% from animal protein. The main plant sources of protein were grains 8.03% of total energy intake), beans (1.94%), and vegetables (1.03%). The main animal sources of protein included red meat (1.31%), eggs (0.46%), and fish/shrimp (0.32%).
Cognitive decline
During a median follow-up of 9 (2–18) years, composite cognitive Z-score declined by 0.4 (−0.4 ± 1.1) SD. The prevalence of cognitive decline defined by the cognitive change below mean minus 1.5 SDs and below mean minus 2 SDs was 7.0 and 2.3%, respectively.
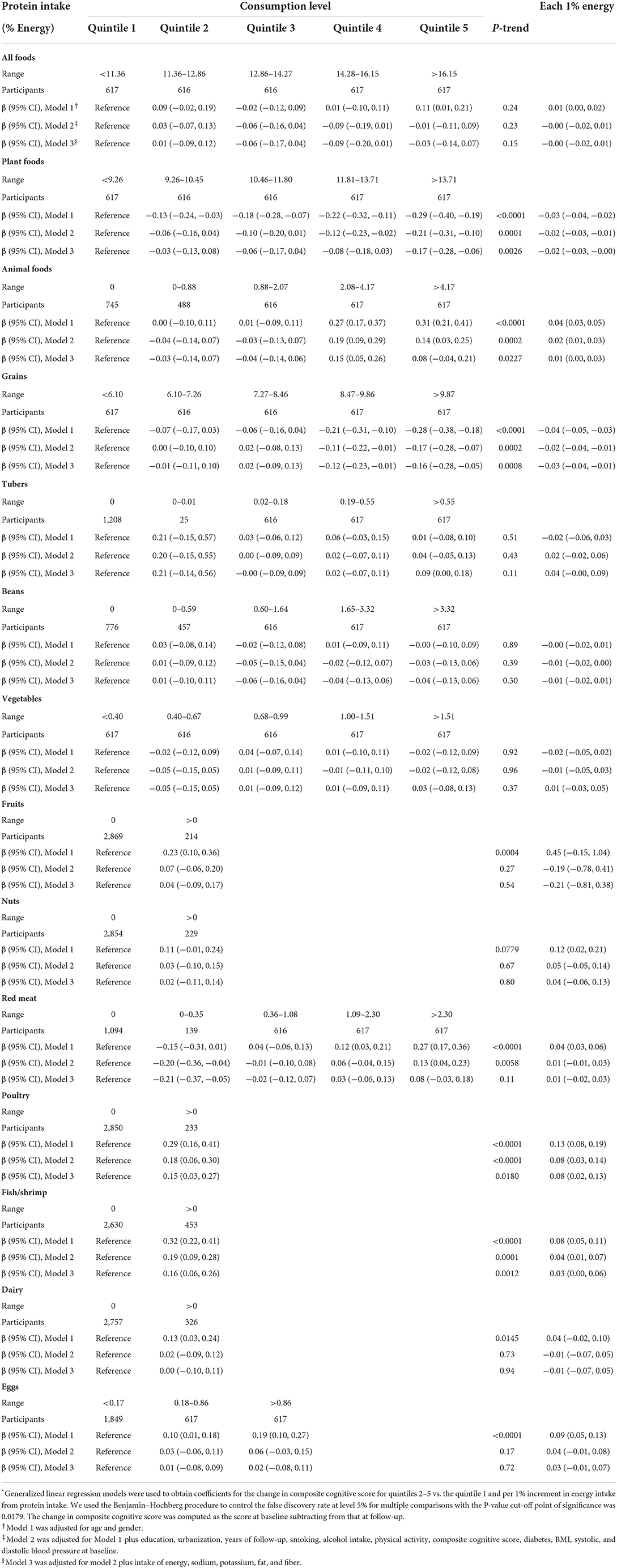
Protein intake and the change in composite cognitive Z-score
Individuals in quintile 5 of plant protein intake had a higher decrease in composite cognitive Z-score [β (95% confidence interval (CI)): −0.17 (−0.28, −0.06) SD] compared with those in quintile 1. Each 1% increment in energy intake from grain protein was found to represent a 0.03 SD decrease in composite cognitive Z-score. Protein intake from other plant foods was not significantly associated with change in composite cognitive Z-score.
Conversely, animal protein intake was positively associated with change in composite cognitive Z-score. Each 1% increment in energy intake from animal protein was found to represent a 0.01 SD increase in composite cognitive Z-score. The corresponding number for protein intake from poultry and fish was 0.08 SD and 0.03 SD, respectively. Protein intake from red meat, dairy, or eggs was positively associated with change in composite cognitive Z-score before but not after adjustment for the intake of energy, fiber, sodium, potassium, and fat (Table 3).
Protein intake and changes in Z-scores of memory, subtraction, and backward counting tests
Plant protein intake was inversely associated with change in memory Z-score [β (95% CI) for quintile 5 vs. quintile 1: −0.79 (−1.32, −0.26)] in the multivariable analysis. Animal protein intake was positively associated with change in memory Z-score before but not after adjustment for confounders (Supplementary Table 2). An inverse association between plant protein intake and change in subtraction Z-score was found before but not after adjustment for confounders. Animal protein intake was positively associated with change in subtraction Z-score [β (95% CI) for quintile 5 vs. quintile 1: 0.34 (0.09, 0.58)] (Supplementary Table 3). In the multivariable analysis, plant protein intake was inversely [β (95% CI) for quintile 5 vs. quintile 1: −0.08 (−0.15, −0.01)] but animal protein intake was positively [0.09 (0.01, 0.17)] associated with change in backward counting Z-score (Supplementary Table 4).
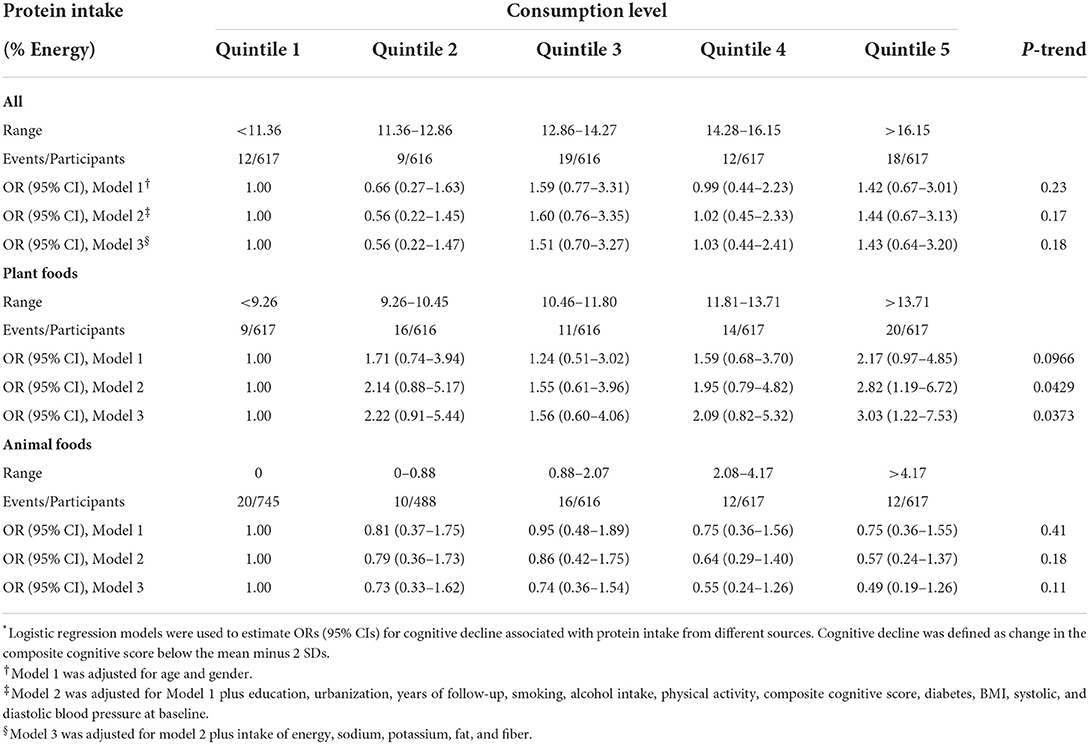
Protein intake and cognitive decline
Participants in quintile 5 of plant protein intake had a higher risk [odds ratio (OR) (95% CI): 3.03 (1.22–7.53)] of cognitive decline as defined by cognitive change below mean minus 2 SDs compared with those in quintile 1 (Table 4). This was consistent with cognitive decline as defined by cognitive change below mean minus 1.5 SDs [OR (95% CI) for quintile 5 vs. quintile 1 of plant protein intake: 1.62 (0.99–2.67)]. Animal protein intake was not significantly associated with cognitive decline (Supplementary Table 5).
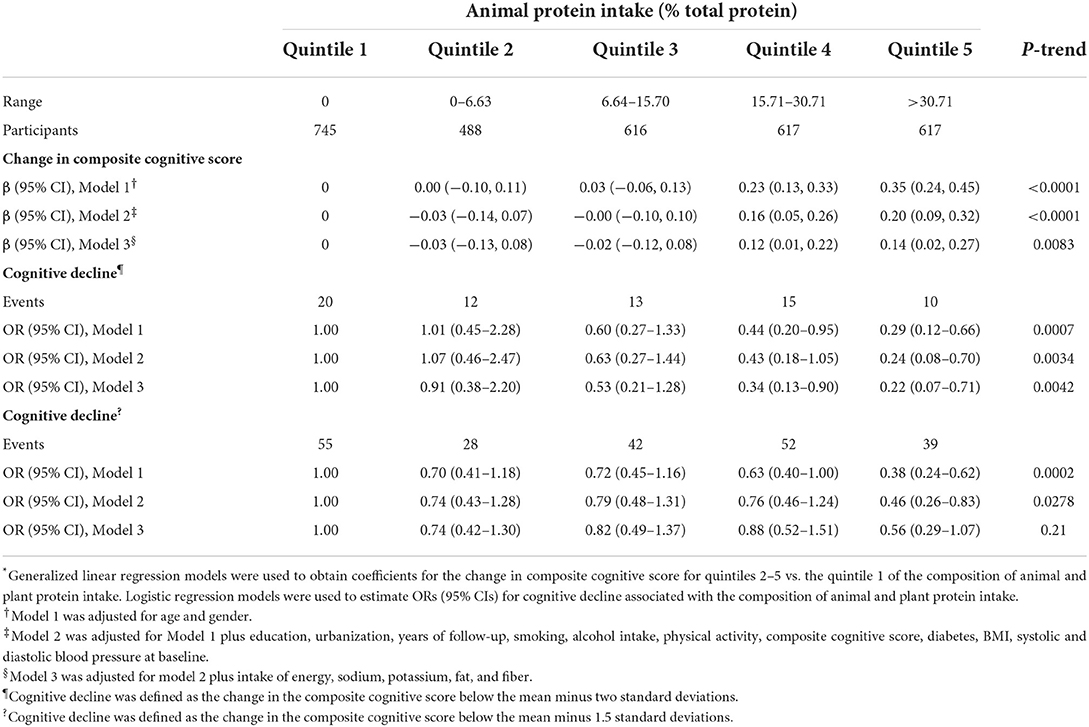
Composition of protein sources and the change in composite cognitive Z-score
Compared with participants in quintile 1 of animal protein (% total protein), those in the highest quintile had a higher increase in composite cognitive Z-score [0.14 (95% CI: 0.02, 0.27) SD)]. High animal protein intake was associated with a lower risk of cognitive decline defined by cognitive change below mean minus 2 SDs [OR (95% CI) for quintile 5 vs. quintile 1: 0.22 (0.07–0.71)] (Table 5).
Moderation analysis
No significant interaction (all P-values for interaction >0.05) between animal/plant protein intake and important factors examined with the change in composite cognitive Z-score was observed (data not shown).
Sensitivity analysis
Sensitivity analysis showed the average annual plant protein intake reported in surveys completed before the first cognitive assessment was inversely associated with change in composite cognitive Z-score during follow-up (Supplementary Table 6).
Discussion
This longitudinal study of community-dwelling older Chinese adults demonstrated that lower plant protein but higher animal protein intake was associated with a lower risk of cognitive decline. Lower protein intake from grains and higher protein intake from poultry and fish/shrimp, were associated with a lower rate of cognitive decline.
We found higher plant protein intake was associated with greater cognitive decline. Our findings are supported by some studies from Europe demonstrating a positive association between plant protein intake and diabetes (25). The harmful effect of high plant protein intake may be attributed to the deficiency of micronutrients in plant-based diets including vitamin B12 and iron, which are associated with a higher risk of cognitive impairment (26–28). Furthermore, plant-based proteins have relatively low essential amino acids and leucine contents or even lack one or more of the essential amino acids when compared with animal-based proteins, such that, a higher plant protein intake is less likely to increase lean and skeletal muscle mass (29). This may explain the inverse association between plant protein intake was associated and change in cognition. Higher protein intake from grains was independently associated with accelerated cognitive decline. This may be due to the fact that grains contain relatively low quantities of essential amino acid lysine, of which lower intake may increase the risk of hypertension, diabetes and obesity (30, 31) resulting in cognitive decline.
We found an inverse association between animal protein intake and cognitive decline. A meta-analysis showing that higher animal protein intake was associated with a lower risk of stroke [RR (95% CI): 0.71 (0.50–0.99)] is consistent with our findings (32). Our findings are also consistent with some studies of Japanese and Chinese populations demonstrating that animal protein intake was inversely associated with blood pressure (33, 34). Animal proteins usually contain all essential amino acids, and therefore may consist of optimal amino acid composition resulting in better metabolic health (29). A recent longitudinal study demonstrates that an adequate methionine (mainly from animal foods) status may decrease the risk of dementia and brain atrophy (35). We observed higher fish protein intake was independently associated with a lower risk of cognitive decline, which is consistent with a study showing that ≥1 servings/week of fish intake was associated with a reduced cognitive decline rate in adults aged ≥ 65 years (36). We also found an inverse association between poultry protein intake and the risk of cognitive decline. Our findings are supported by a prospective study demonstrating that higher poultry intake was associated with less cognitive decline over 6 years in older Swedish adults (7). Protein intake from red meat, dairy, or eggs was not independently associated with cognitive decline suggesting potential beneficial effects of higher animal protein intake were driven by fish/shrimp and poultry.
An optimal amino acid composition of dietary protein intake may help optimize amino acid metabolism and protect against dementia risks including obesity, diabetes, hypertension, and stroke (37). A cross-sectional study of 661 Chinese adults found that a higher total protein intake was associated with a higher likelihood of mild cognitive impairment (38). Likely, we found higher total protein intake was associated with accelerated cognitive decline. Notably, animal sources accounted for only 16.3% of total protein intake in our study, which was much lower than that reported in individuals from the USA, Europe, and Australia (64–75%) as well as in Japan (54%) (25, 39–42). Meanwhile, plant protein intake was inversely but animal protein intake was positively associated with change in composite cognitive Z-score suggesting the inverse association between total protein intake and cognition was driven by plant protein in our study. This indicates that increasing the proportion of animal protein in populations with plant dominant diets may help protect against cognitive decline. A recent study of US women and men demonstrated that higher plant protein intake and lower animal protein intake was associated with lower likelihood of cognitive decline (13), but other studies showed that specific protein food sources were not significantly associated with cognitive function (14).
The conflicting findings between our study and Yeh et al. may be due to the fact that the plant foods are dominant in our population, but animal foods are dominant in the US population.
To our knowledge, this is the first longitudinal study to examine the association between protein intakes from different food sources with cognitive decline. Our study has several limitations. First, cognitive assessment was conducted in a subgroup of the CHNS cohort, which limits the generalization of our findings to the whole population in China. Second, our study was conducted in a population with plant food dominant diets, therefore, more longitudinal studies in populations with animal food dominant diets are needed to warrant our findings. Finally, the wide range of follow-up in our study might influence associations between protein intake and cognition. However, the results did not substantially change after adjusting for follow-up and the follow-up did not mediate the association, suggesting our findings are independent of the follow-up duration.
In conclusion, the intake of protein from plant foods especially grains were positively associated but the intake of protein from animal foods, especially fish/shrimp and poultry, were inversely associated with accelerated cognitive decline. A relatively high proportion of animal protein in population with plant dominant diets may be protective of cognitive decline.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
RG, ZY, and WY conceived and designed the study. RG, WD, and YZ conducted data analysis and drafted the initial manuscript. ZY, WY, and FZ made critical revision of the manuscript for important intellectual content. All authors read the manuscript and approved the final draft.
Funding
This research uses data from China Health and Nutrition Survey (CHNS). We thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Carolina Population Center (P2C HD050924 and T32 HD007168), the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700) and the NIH Fogarty International Center (D43 TW009077 and D43 TW007709) for financial support for the CHNS data collection and analysis files from 1989 to 2015 and future surveys, and the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Center at Shanghai since 2009, and Beijing Municipal Center for Disease Prevention and Control since 2011.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1016016/full#supplementary-material
Abbreviations
BMI, body mass index; CHNS, china health and nutrition survey; CI, confidence interval; MET, metabolic equivalent of task; OR, odds ratio; SD, standard deviation.
References
1. Nichols E, Szoeke CEI, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, et al. Global, regional, and national burden of Alzheimer's disease and other dementias, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2019) 18:88–106. doi: 10.1016/S1474-4422(18)30403-4
2. Jia J, Wang F, Wei C, Zhou A, Jia X, Li F, et al. The prevalence of dementia in urban and rural areas of China. Alzheimers Dement. (2014) 10:1–9. doi: 10.1016/j.jalz.2013.01.012
3. Jia L, Quan M, Fu Y, Zhao T, Li Y, Wei C, et al. Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurol. (2020) 19:81–92. doi: 10.1016/S1474-4422(19)30290-X
4. Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, et al. Dementia prevention, intervention, and care. Lancet. (2017) 390:2673–734. doi: 10.1016/S0140-6736(17)31363-6
5. Baumgart M, Snyder HM, Carrillo MC, Fazio S, Kim H, Johns H. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: a population-based perspective. Alzheimers Dement. (2015) 11:718–26. doi: 10.1016/j.jalz.2015.05.016
6. Wang Z, Pang Y, Liu J, Wang J, Xie Z, Huang T. Association of healthy lifestyle with cognitive function among Chinese older adults. Eur J Clin Nutr. (2020) 75:325–34. doi: 10.1038/s41430-020-00785-2
7. Shakersain B, Rizzuto D, Larsson SC, Faxén-Irving G, Fratiglioni L, Xu WL. The Nordic prudent diet reduces risk of cognitive decline in the swedish older adults: a population-based cohort study. Nutrients. (2018) 10:229. doi: 10.3390/nu10020229
8. Mi W, van Wijk N, Cansev M, Sijben JW, Kamphuis PJ. Nutritional approaches in the risk reduction and management of Alzheimer's disease. Nutrition. (2013) 29:1080–9. doi: 10.1016/j.nut.2013.01.024
9. Morris MC, Tangney CC, Wang Y, Sacks FM, Bennett DA, Aggarwal NT. MIND diet associated with reduced incidence of Alzheimer's disease. Alzheimers Dement. (2015) 11:1007–14. doi: 10.1016/j.jalz.2014.11.009
10. Hosking DE, Eramudugolla R, Cherbuin N, Anstey KJ. MIND not Mediterranean diet related to 12-year incidence of cognitive impairment in an Australian longitudinal cohort study. Alzheimers Dement. (2019) 15:581–9. doi: 10.1016/j.jalz.2018.12.011
11. Richter CK, Skulas-Ray AC, Champagne CM, Kris-Etherton PM. Plant protein and animal proteins: do they differentially affect cardiovascular disease risk? Adv Nutr. (2015) 6:712–28. doi: 10.3945/an.115.009654
12. Shang X, Scott D, Hodge A, English DR, Giles GG, Ebeling PR, et al. Dietary protein from different food sources, incident metabolic syndrome and changes in its components: an 11-year longitudinal study in healthy community-dwelling adults. Clin Nutr. (2017) 36:1540–8. doi: 10.1016/j.clnu.2016.09.024
13. Yeh TS, Yuan C, Ascherio A, Rosner BA, Blacker D, Willett WC. Long-term dietary protein intake and subjective cognitive decline in US men and women. Am J Clin Nutr. (2022) 115:199–210. doi: 10.1093/ajcn/nqab236
14. Koh F, Charlton K, Walton K, McMahon AT. Role of dietary protein and thiamine intakes on cognitive function in healthy older people: a systematic review. Nutrients. (2015) 7:2415–39. doi: 10.3390/nu7042415
15. Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the China health and nutrition survey–monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol. (2010) 39:1435–40. doi: 10.1093/ije/dyp322
16. Zhang B, Zhai FY, Du SF, Popkin BM. The China health and nutrition survey, 1989-2011. Obes Rev. (2014) 15 (Suppl. 1):2–7. doi: 10.1111/obr.12119
17. Du S, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. (2014) 99:334–43. doi: 10.3945/ajcn.113.059121
19. Yao M, McCrory MA, Ma G, Tucker KL, Gao S, Fuss P, et al. Relative influence of diet and physical activity on body composition in urban Chinese adults. Am J Clin Nutr. (2003) 77:1409–16. doi: 10.1093/ajcn/77.6.1409
20. Plassman BL, Welsh KA, Helms M, Brandt J, Page WF, Breitner JC. Intelligence and education as predictors of cognitive state in late life: a 50-year follow-up. Neurology. (1995) 45:1446–50. doi: 10.1212/WNL.45.8.1446
21. Lei X, Hu Y, McArdle JJ, Smith JP, Zhao Y. Gender differences in cognition among older adults in China. J Hum Resour. (2012) 47:951–71. doi: 10.1353/jhr.2012.0033
22. Strauss J, Lei X, Park A, Shen Y, Smith JP, Yang Z, et al. Health outcomes and socio-economic status among the elderly in Gansu and Zhejiang provinces, China: evidence from the CHARLS pilot. J Popul Ageing. (2010) 3:111–42. doi: 10.1007/s12062-011-9033-9
23. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/S0140-6736(03)15268-3
24. Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. (2000) 32 (9 Suppl):S498–504. doi: 10.1097/00005768-200009001-00009
25. Shang X, Scott D, Hodge AM, English DR, Giles GG, Ebeling PR, et al. Dietary protein intake and risk of type 2 diabetes: results from the Melbourne collaborative cohort study and a meta-analysis of prospective studies. Am J Clin Nutr. (2016) 104:1352–65. doi: 10.3945/ajcn.116.140954
26. Moore E, Mander A, Ames D, Carne R, Sanders K, Watters D. Cognitive impairment and vitamin B12: a review. Int Psychogeriatr. (2012) 24:541–56. doi: 10.1017/S1041610211002511
27. Jauregui-Lobera I. Iron deficiency and cognitive functions. Neuropsychiatr Dis Treat. (2014) 10:2087–95. doi: 10.2147/NDT.S72491
28. Smith AD, Warren MJ, Refsum H. Vitamin B(12). Adv Food Nutr Res. (2018) 83:215–79. doi: 10.1016/bs.afnr.2017.11.005
29. Gorissen SHM, Crombag JJR, Senden JMG, Waterval WAH, Bierau J, Verdijk LB, et al. Protein content and amino acid composition of commercially available plant-based protein isolates. Amino Acids. (2018) 50:1685–95. doi: 10.1007/s00726-018-2640-5
30. Altorf-van der Kuil W, Engberink MF, De Neve M, van Rooij FJ, Hofman A, van't Veer P, et al. Dietary amino acids and the risk of hypertension in a Dutch older population: the Rotterdam study. Am J Clin Nutr. (2013) 97:403–10. doi: 10.3945/ajcn.112.038737
31. Iyer A, Fairlie DP, Brown L. Lysine acetylation in obesity, diabetes and metabolic disease. Immunol Cell Biol. (2012) 90:39–46. doi: 10.1038/icb.2011.99
32. Zhang Z, Xu G, Yang F, Zhu W, Liu X. Quantitative analysis of dietary protein intake and stroke risk. Neurology. (2014) 83:19–25. doi: 10.1212/WNL.0000000000000551
33. Kihara M, Fujikawa J, Ohtaka M, Mano M, Nara Y, Horie R, et al. Interrelationships between blood pressure, sodium, potassium, serum cholesterol, and protein intake in Japanese. Hypertension. (1984) 6:736–42. doi: 10.1161/01.HYP.6.5.736
34. Zhou B, Zhang X, Zhu A, Zhao L, Zhu S, Ruan L, et al. The relationship of dietary animal protein and electrolytes to blood pressure: a study on three Chinese populations. Int J Epidemiol. (1994) 23:716–22. doi: 10.1093/ije/23.4.716
35. Hooshmand B, Refsum H, Smith AD, Kalpouzos G, Mangialasche F, von Arnim CAF, et al. Association of methionine to homocysteine status with brain magnetic resonance imaging measures and risk of dementia. JAMA Psychiatry. (2019) 76:1198–205. doi: 10.1001/jamapsychiatry.2019.1694
36. Qin B, Plassman BL, Edwards LJ, Popkin BM, Adair LS, Mendez MA. Fish intake is associated with slower cognitive decline in Chinese older adults. J Nutr. (2014) 144:1579–85. doi: 10.3945/jn.114.193854
37. Wu G. Amino acids: metabolism, functions, and nutrition. Amino Acids. (2009) 37:1–17. doi: 10.1007/s00726-009-0269-0
38. Ding B, Xiao R, Ma W, Zhao L, Bi Y, Zhang Y. The association between macronutrient intake and cognition in individuals aged under 65 in China: a cross-sectional study. BMJ Open. (2018) 8:e018573. doi: 10.1136/bmjopen-2017-018573
39. Nanri A, Mizoue T, Kurotani K, Goto A, Oba S, Noda M, et al. Low-carbohydrate diet and type 2 diabetes risk in Japanese men and women: the Japan public health center-based prospective study. PLoS ONE. (2015) 10:e0118377. doi: 10.1371/journal.pone.0118377
40. Sluijs I, Beulens JW, van der AD, Spijkerman AM, Grobbee DE, van der Schouw YT. Dietary intake of total, animal, and vegetable protein and risk of type 2 diabetes in the European prospective investigation into cancer and nutrition (EPIC)-NL study. Diabetes Care. (2010) 33:43–8. doi: 10.2337/dc09-1321
41. Malik VS, Li Y, Tobias DK, Pan A, Hu FB. Dietary protein intake and risk of type 2 diabetes in US men and women. Am J Epidemiol. (2016) 183:715–28. doi: 10.1093/aje/kwv268
Keywords: dietary protein, animal protein, plant protein, cognitive decline, protein intake
Citation: Gao R, Yang Z, Yan W, Du W, Zhou Y and Zhu F (2022) Protein intake from different sources and cognitive decline over 9 years in community-dwelling older adults. Front. Public Health 10:1016016. doi: 10.3389/fpubh.2022.1016016
Received: 10 August 2022; Accepted: 29 September 2022;
Published: 14 October 2022.
Edited by:
Xianwen Shang, The University of Melbourne, AustraliaCopyright © 2022 Gao, Yang, Yan, Du, Zhou and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Zhu, emZ0c21jQDE2My5jb20=
†These authors share first authorship
 Rongtao Gao
Rongtao Gao Zhan Yang2†
Zhan Yang2†