- 1School of Public Health, Kunming Medical University, Kunming, China
- 2Department of Gastroenterology, Affiliated Hospital of Yunnan University, Kunming, China
Liver cancer is a major public health challenge. Few published studies reported temporal trend and geographical distribution of liver cancer mortality in China, especially in less developed southwest regions with higher liver cancer incidence. In the current study, we obtained liver cancer mortality data from population-based death surveillance system in Yunnan province in 2015–2019. The mortality of liver cancer was analyzed by using the joinpoint regression model. The space distribution of liver cancer mortality in 129 counties and districts in Yunnan province was illustrated by using the ArcGIS software. Moran's I method was used to estimate the global and local spatial autocorrelation of liver cancer mortality. Analytical results revealed that from 2015 to 2019, the average mortality rate of liver cancer in Yunnan province was 12.96/100,000, with an average annual growth rate of 6.26% (p < 0.05). Higher liver cancer mortality was found in rural areas and in males. Moreover, people aged 45–50 years experienced a steep increase in liver cancer mortality rate. High-high cluster was mainly consisted of areas with higher hepatitis virus infection rate or severe intravenous drug use problem. Our study results suggest a heavy burden of liver cancer in southwest China Yunnan province. Comprehensive intervention measures need to be developed and implemented.
Introduction
Cancer is a major health threat. New cancer cases and cancer related deaths had been estimated around 19.3 and 10 million in 2020 (1). Liver cancer is one of the most common carcinomas. In 2020, with over 0.9 million new cases and over 0.8 million deaths, liver cancer ranked 6th and 3rd by incidence and mortality among all cancers globally (2). East and southeast Asia, north and west Africa report higher incidence and mortality of liver cancer (3–5). Although China has made great efforts in the past decades, liver cancer remains one of the malignant tumors with the highest incidence and mortality today (6). In China, liver cancer accounted for 45.27 and 47.12% of new cancer cases and cancer related deaths in 2020 (1). Geographically, southwest regions of China report higher prevalence of liver cancer (7).
The majority of existing studies have identified risk factors of liver cancer at individual level, such as age, sex, socioeconomic status, overweight, hepatitis B virus (HBV) or hepatitis C virus (HCV) infection, excessive alcohol consumption and smoking (8–10). Although they are valuable in guiding primary intervention policies and measures of liver cancer, for effective regional prevention and control, an extra endeavor needs to be done to disclose spatial and temporal characteristics of liver cancer, to help determine high risk areas of intervention priority. At present, spatial epidemiology has gradually been used in describing geographical distribution of cancers in China. For instance, recently, a spatial and temporal study of gastric cancer indicated that the mortality of gastric cancer varied between different regions of China, and environmental management was probably behind this discrepancy (11). Another Chinese study explored spatial and temporal pattern of lung cancer in Shenzhen (12).
However, few studies had been published regarding to spatial and temporal patterns of liver cancer mortality in China (13–15). Moreover, these studies only briefly described time or space distribution of liver cancer mortality at the country level or in some developed coastal areas, no published study has ever elaborately discussed this issue in impoverished inland provinces, which reported much higher liver cancer incidence and disease burden. In the current study, aiming to address this deficiency, we investigated spatial and temporal distributions of liver cancer mortality in southwest China Yunnan province from 2015 to 2019.
Materials and methods
Data sources
Liver cancer cause specific deaths in Yunnan province at county level in 2015–2019 were obtained from the all-cause death registration system which incorporated into the China Disease Prevention and Control Information System. In this population-based death registration system, cause of death is coded according to the International Classification of Diseases (ICD-10). In this study we only extracted deaths caused by liver cancer (coded as C22.0-C22.9). Population data at county level of Yunnan province were obtained from the resident population information module which also incorporated into the China Disease Prevention and Control Information System, and the age standardized mortality rates were calculated by using the 2010 Chinese standard population: we divided age into 18 groups from 0 to 85 (5 years a group), and then used the direct standardization method to calculate the age standardized mortality rate (ASR) by using the formula (i: age group i; ai: observed mortality rate in age group i; wi: the standard population size in age group i). The digital maps of Yunnan (illustrating at county level) were freely obtained from the National Geomatics Center of China (https://www.webmap.cn/main.do?method=index, accessed on 16/3/2022) and the official Planning Cloud website (http://www.guihuayun.com/, accessed on 16/3/2022).
Statistical analysis
Joinpoint regression analysis
The joinpoint regression, also known as piecewise linear regression, is an ideal tool for analyzing time series data (16). In some previously published studies, this method had been successfully used to assess changing trends in cancer mortality (17, 18). Here in this study, we used joinpoint regression model to calculate the average annual percentage change (AAPC) of liver cancer mortality in Yunnan province in 2015–2019: when AAPC > 0, it indicates an increasing trend of liver cancer mortality; when AAPC < 0, it indicates a decreasing trend of liver cancer mortality; when AAPC = 0, it indicates no change (19).
Spatial distribution analysis
Liver cancer mortality rates in Yunnan province were linked to the digital map of Yunnan province by using a primary geographic key at county level (altogether 129 counties). In order to make the map uniform across years, all counties were divided into six groups based on their liver cancer mortality rates (in units of 7/100,000) and differentiated by colors.
Spatial aggregation analysis
The global and local spatial autocorrelation analyses were further performed. At first, Moran's I was used as an indicator to reflect global spatial aggregation in the whole region and significance test was performed. When the Moran's I value > 0, it indicates a positive spatial autocorrelation; when the Moran's I value < 0, it indicates a negative spatial autocorrelation; when the Moran's I value = 0, it indicates a random distribution (20). The LISA plots were then used to measure local spatial autocorrelation of liver cancer mortality in Yunnan Province. When the local Moran's I was significant, the LISA plot can reflect four types of spatial aggregation: high-high, where high value regions are adjacent to regions with high values; high-low, where high value regions are adjacent to regions with low values; low-high, where low value regions are adjacent to regions with high values; and low-low, where low value regions are adjacent to regions with low values.
Softwares
Data merging and sorting were performed by using the Stata/SE software (Version: 16.0). Joinpoint regression analysis of liver cancer mortality was performed by the Joinpoint software (Version: 4.9.0.0). Regional distribution of liver cancer mortality was mapped by using the ArcGIS software (Version: 10.8.1). The GeoDa software (Version: 1.18.0) was used for global and spatial autocorrelation analysis. Significance level for all statistical tests or inferences was set as a two-tailed probability no higher than 0.05.
Results
General characteristics of liver cancer mortality in Yunnan
The total, sex-specific, and region-specific mortality of liver cancer in Yunnan province from 2015 to 2019 are reported in Table 1. During the study period, a total of 30,921 liver cancer deaths were reported, with an overall crude mortality rate of 12.96/100,000 (calculated as: ) and an age standardized rate (ASR) of 13.62/100,000. There were 22,813 deaths in males and 8,099 deaths in females, with a much higher ASR in males (20.29/100,000) than in females (6.93/100,000). Liver cancer deaths in rural and urban regions were 22,776 and 8,136, with a higher ASR in rural region (15.47/100,000) than in urban region (10.21/100,000).
Trends of liver cancer mortality
The joinpoint regression results indicated that there was no statistical significance in the time point segmentation, suggesting that the trend and degree of changes in liver cancer mortality rate by sex and region were in general similar from 2015 to 2019. Crude mortality rates of liver cancer in males, females, and rural region all showed an increasing trend from 2015 to 2019 (total AAPC: 6.26%, male AAPC: 6.43%, female AAPC: 5.34%, rural AAPC: 6.74%, all with p < 0.05). However, from 2015 to 2019, there were no significant trends for the ASRs of liver cancer mortality in Yunnan (Figure 1).
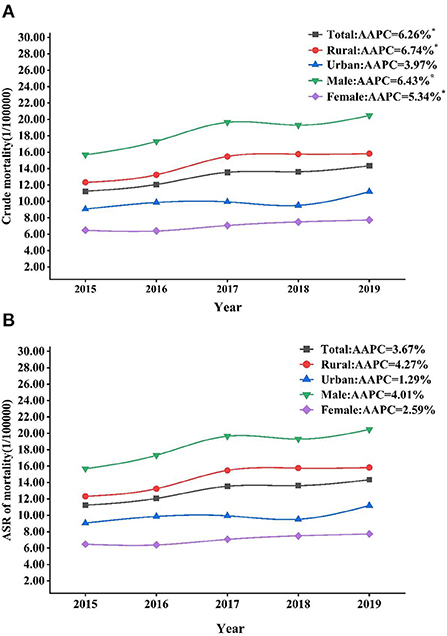
Figure 1. Trends of crude mortality rates (A) and ASRs (B) of liver cancer in Yunnan by sex and region, 2015–2019. ASR, age standardized rate. *p < 0.05.
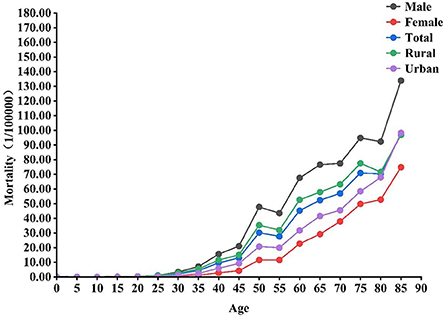
For all liver cancer deaths in Yunnan province in 2015–2019, the average age at death was higher for females (66.29 ± 13.83 years) than for males (60.15 ± 13.44 years), higher for urban residents (63.31 ± 13.86 years) than for rural residents (61.21 ± 13.75 years). The mortality rate of liver cancer gradually increased from the age of 30 years onwards, and the 80–85 and 45–50 age groups were seen the most prominent increase. The overall trends in age-specific mortality rates for liver cancer by sex and region were generally similar (Figure 2).
Spatial distribution of liver cancer mortality
According to the distribution maps, liver cancer mortality was generally at a higher level from 2015 to 2019 in Pingbian, Jingdong, Mengla, Shizong and Shiping counties, with Pingbian county in the south consistently led liver cancer death rate. Liver cancer mortality in most counties fluctuated between 2015 and 2019, whereas continuously increased in Yingjiang, Qubei, Dongchuan, Huize, and Jiangchuan counties, continuously decreased in Yongshan, Nyingchi, Yuanyang, Yanshan, Xichuan, and Menghai counties (Figure 3).
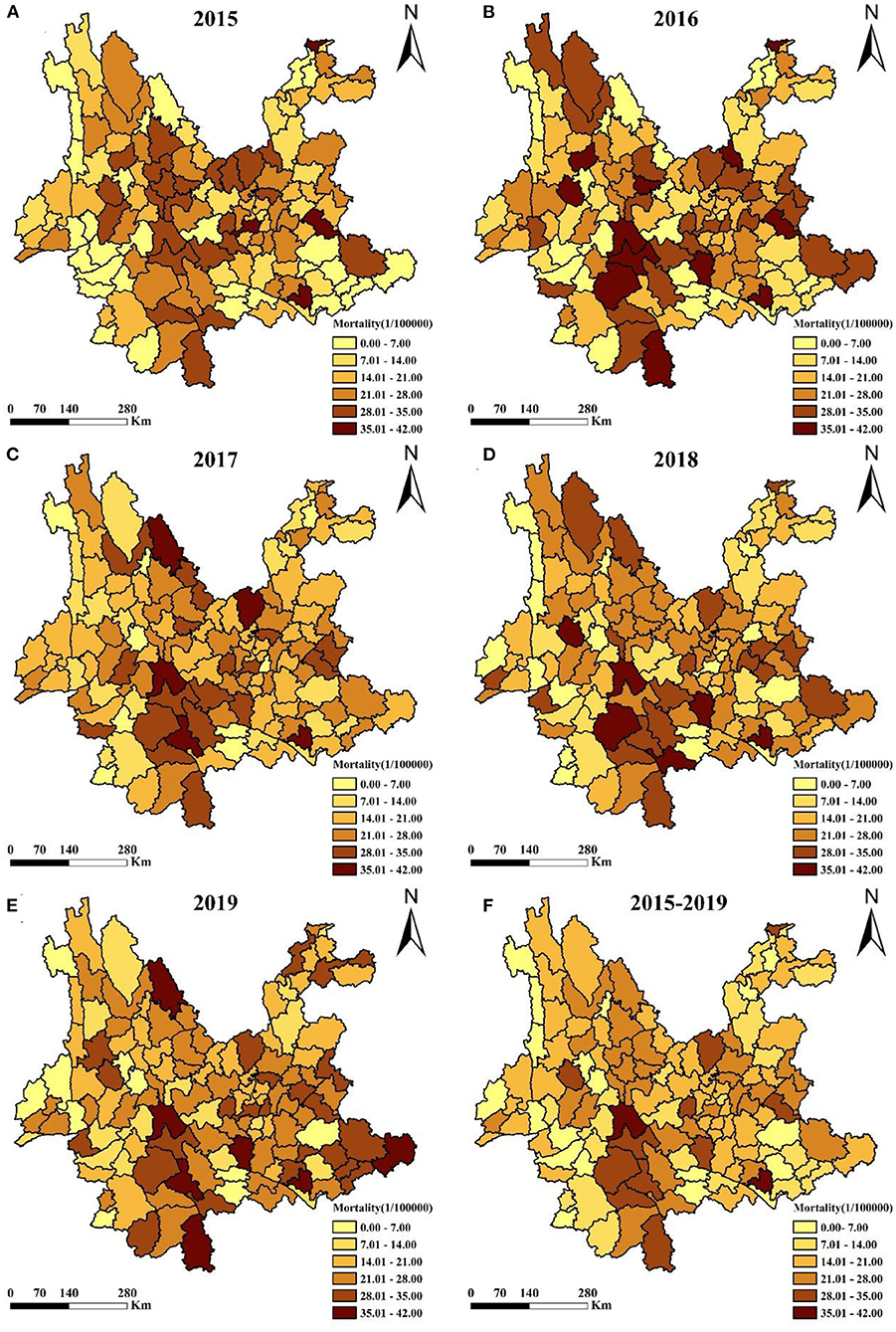
Figure 3. Geographic distribution of liver cancer mortality rates at county level in Yunnan, 2015–2019. (A–E) year 2015–2019, (F) year 2015–2019 on average.
Spatial aggregation of liver cancer mortality
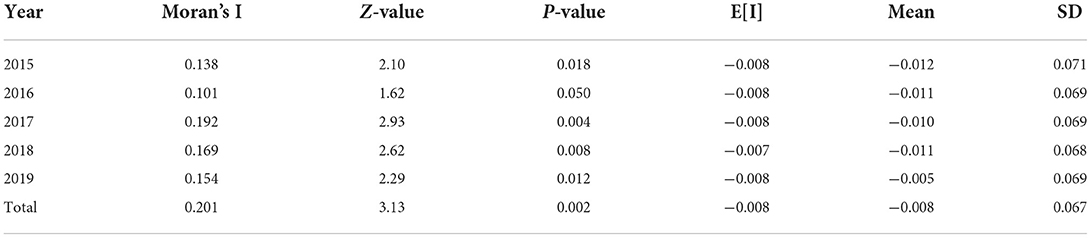
The global and local autocorrelation analyses of liver cancer mortality in Yunnan province in 2015–2019 were shown in Figure 4. The global autocorrelation results revealed that the Moran's I values for the year 2015 to 2019 were 0.138, 0.101, 0.191, 0.169, and 0.154, respectively, suggesting that liver cancer mortality in Yunnan province was spatially positively correlated across regions in 2015–2019 (Table 2). Further local autocorrelation analysis results were presented in Figure 5: LISA plots revealed high-high cluster in southwest regions of Yunnan, like Ninger, Jingdong and Zhenyuan counties, low-low cluster in western border areas. All clustering types in the graphs were statistically significant.
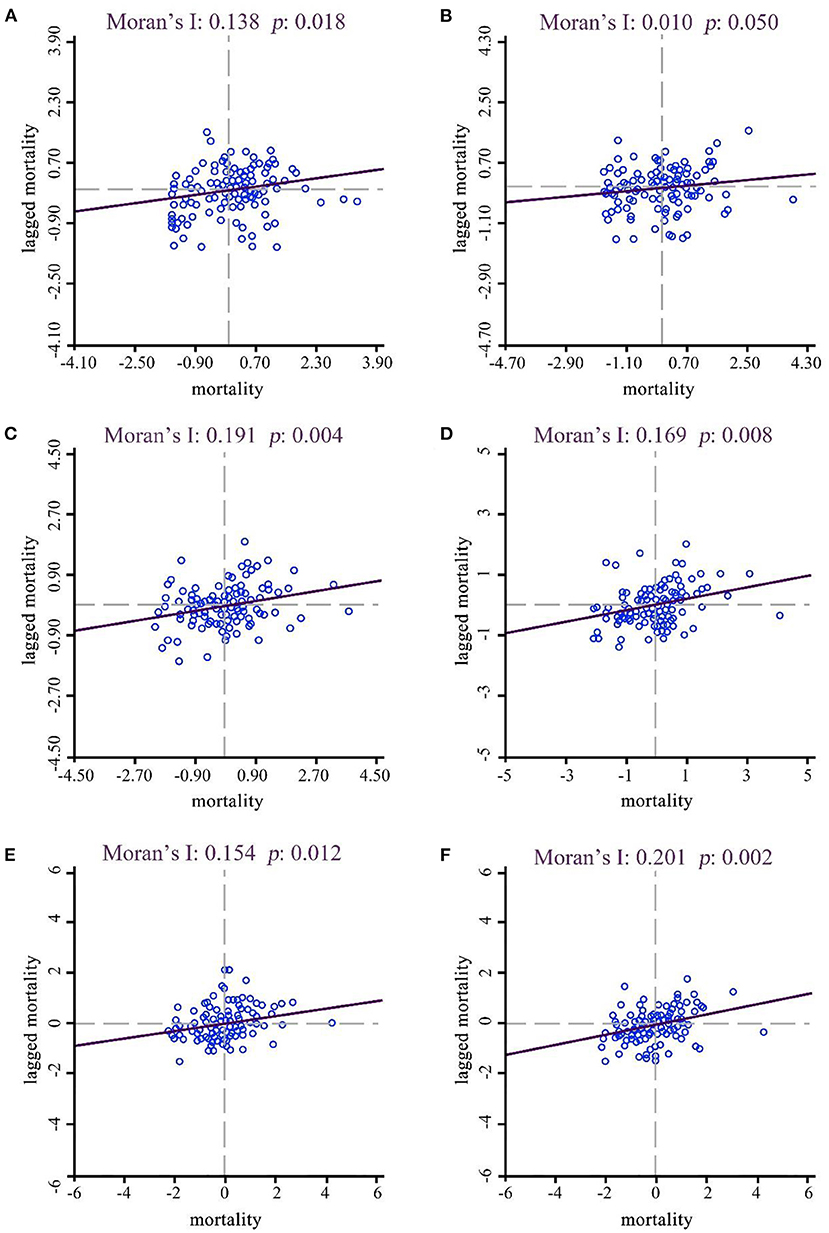
Figure 4. Moran's I scatter plots of liver cancer mortality in Yunnan, 2015–2019. (A–E) year 2015–2019, (F) year 2015–2019 on average.
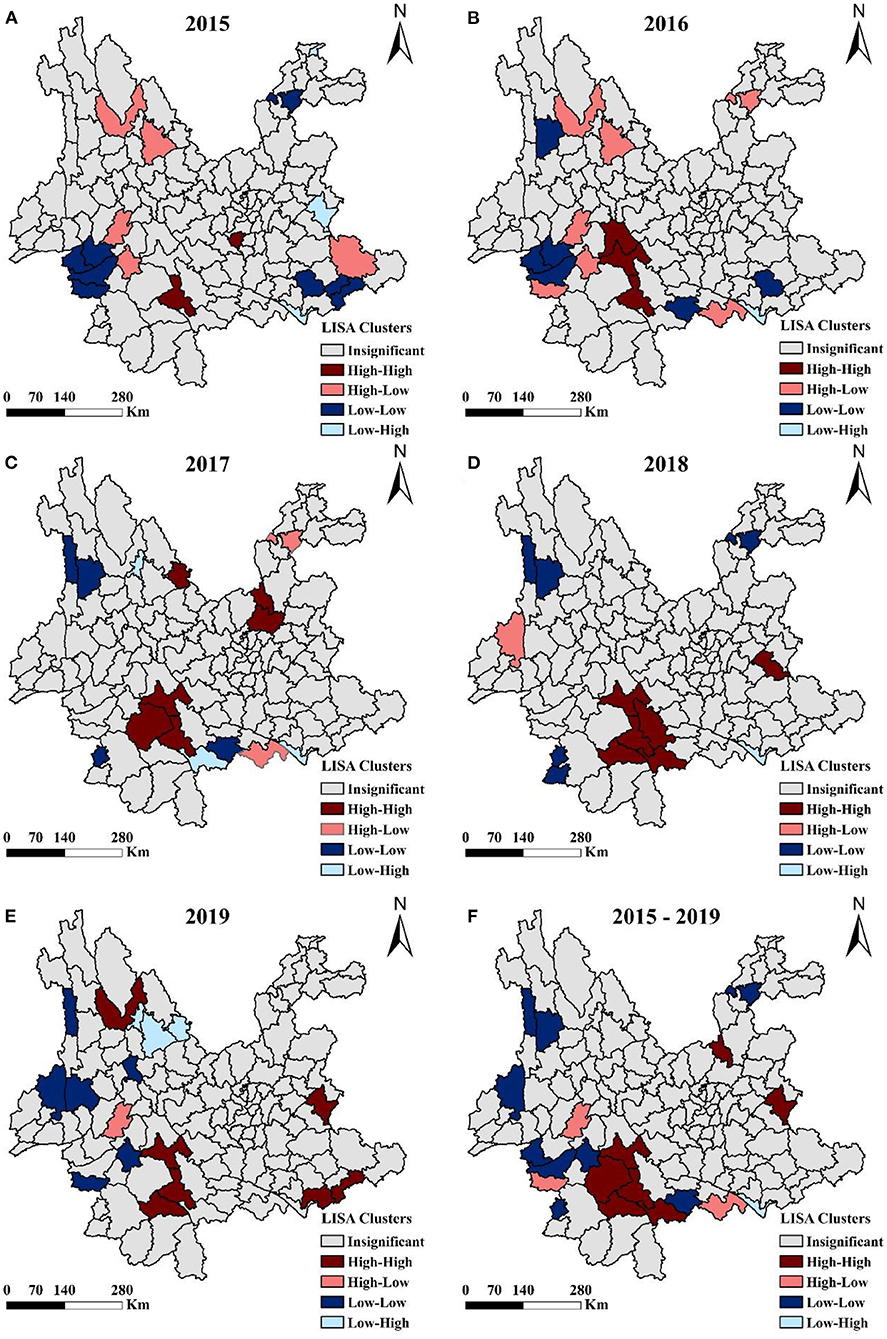
Figure 5. LISA maps of liver cancer mortality in Yunnan at county level, 2015–2019. (A–E) year 2015–2019, (F) year 2015–2019 on average.
Discussion
In this study, we performed spatial and temporal analysis for liver cancer mortality in Yunnan province in 2015–2019. Based on analytical results, we have the following major findings: first, the overall mortality of liver cancer in Yunnan province was at a high level and still presented a slow increase; second, the mortality of liver cancer varied considerably by different characteristics of the population, such as region, sex and age; third, spatial autocorrelation analysis identified some high-high areas in liver cancer mortality, which should be prioritized for liver cancer prevention and control.
The age standardized mortality rate of liver cancer in Yunnan province was 14.10/100,000 in the year 2019, much higher than the national average rate of 8.44/100,000 (21), reflecting a higher level of liver cancer burden in Yunnan. This high liver cancer mortality probably can be attributed to HBV/HCV infection, as HBV infection rate was much higher in Yunnan (49.92/100,000) when compared with other regions in China, like Jiangsu province (16.17/100,000) and Shanghai (35.07/100,000) (22). Besides, Yunnan province is also an important epidemic center for blood-borne viruses such as HCV (23, 24). Meanwhile, Yunnan province is an economically underdeveloped region locates in southwest border of China. It has been reported that the participation rate in cancer screening was only about 50% in Yunnan (25, 26), which may further contribute to increased liver cancer incidence and mortality due to inefficient primary and secondary prevention measures caused by socioeconomic predicaments. The slow increase in liver cancer mortality in Yunnan province between 2015 and 2019 that we observed in this study was consistent with the national trend (27). This increased liver cancer mortality probably was the consequence of elevated HBV prevalence from 36.17/100,000 in 2004 to 49.92/100,000 in 2015 in Yunnan province (22).
Regarding to regional distribution, we found that liver cancer mortality was significantly higher in rural areas than in urban areas, and this difference was consistent with findings in other Chinese provinces (14, 28). Urban-rural differences in risk factors (HBV infection, aflatoxin intake) exposure, socioeconomic development, hygiene status, and accessibility to health care (including treatment accessibility) may collectively contribute to this discrepancy in liver cancer mortality (29, 30). Based on gender, a higher liver cancer mortality had been found in males, also consistent with the findings of previously published Chinese studies (31, 32). Males reported higher levels of exposure to some identified behavioral risk factors of liver cancer, such as smoking and alcohol abuse (33, 34). Besides, sex related steroid hormones, immune responses, and epigenetic differences may also play a role (35, 36). For age distribution, an interesting finding to be noticed is that the 45–50 age group was seen a steep increase in liver cancer mortality. A study from Shanghai also reported a sharp increase in liver cancer mortality in residents aged above 40, and concluded that the high mortality in this age group probably can be attributed to HBV infection (37). One study showed that HBV infection rate in Chinese residents aged 40–59 was 181.62/100,000, significantly lower than which in the younger age groups (22). This phenomenon could be the consequence of the fact that HBV vaccine was not introduced into China until the 1980s (38, 39).
Spatial autocorrelation analysis revealed that liver cancer mortality in Yunnan was in general not randomly distributed: Dongchuan district and Xundian county in Kunming, Ning'er county, Jingdong county, Zhenyuan county, Jiangcheng county in Pu'er city, and Malipo county in Wenshan city, were all seen high liver cancer mortality rates. It is well-known that HBV/HCV infection is the most important risk factor of liver cancer in China (40). Reports indicated that Kunming city had the highest HCV infection rate (15.26/100,000) in Yunnan in 1990–2014, and Pu'er city had the highest HBV infection rate (66.19/100,000) in 2015 (41, 42). Therefore, areas reported high liver cancer mortality rates in this study were largely regions with high HBV/HCV infection, suggesting that liver cancer mortality is closely related to local hepatitis epidemic (41). Moreover, Yunnan province also reports a higher prevalence of HIV infection caused by injecting drugs, due to its geographical location (next to the Golden Triangle). Yingjiang county, where the liver cancer mortality rate was also high, is the same county that mostly affected by illicit drug use and AIDS epidemic in Yunnan (43). Previous studies have shown that HIV infection caused by injecting drugs was more likely to be co-infected with HBV or HCV (44, 45).
The high-high cluster of liver cancer mortality in Yunnan province, as disclosed by autocorrelation analysis, mainly includes areas with high hepatitis virus infection rate or widespread intravenous drug abuse, and these areas are undoubtedly of the highest priority for liver cancer prevention and control. A comprehensive intervention strategy which incorporates multiple effective measures from different aspects should be considered. For instance, more health care resources need to be allocated to these areas, to help increase HBV/HCV vaccination rate and improve treatment quality of hepatitis patients. Moreover, for drug users, local health departments should provide effective counseling and referral services, promote methadone maintenance treatment clinic initiatives (46–48). However, some high-high clustering areas, like Malipo, Yuanjiang and Luoping, are neither hepatitis epidemic nor drug abuse areas, the primary risk factors that are driving up local liver cancer mortality should be further investigated, preferably by using case-control studies.
Our study has several limitations. First, restricted by data availability, we only analyzed liver cancer mortality in 5 years, therefore the long-term liver cancer mortality trend in Yunnan province needs to be continuously updated, to help build an ideal prediction model. Besides, the spatial and temporal distributions of liver cancer incidence are also of considerable study interest, which should be further investigated in the future. Second, the accuracy of study results could be influenced by the quality of surveillance data. Finally, we only preliminarily analyzed spatial and temporal trends of liver cancer mortality, in subsequent studies, some important influencing factors, especially environmental factors, could be further included.
Conclusion
In this study, by using spatial and temporal analysis, we found a high liver cancer mortality rate with increasing trend in southwest China Yunnan province from 2015 to 2019, especially in rural areas and in males. Moreover, a sharp increase has been identified for residents aged 45–50. The high-high cluster in liver cancer mortality largely includes areas with high local HBV/HCV infection rate or severe intravenous drug abuse problem. Comprehensive intervention measures should be adopted in reducing liver cancer burden in Yunnan. Future studies with updated surveillance data and include important environmental covariates are warranted.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
YX and WC designed the study and critically revised the manuscript. CF, JL, HR, LW, XL, and HS carried out the data collection. CF and HR performed data analysis. CF and JL prepared the draft manuscript. All authors critically revised the manuscript for important intellectual content, contributed to the article, and approved the submitted version.
Funding
The study was supported by Joint Special Project of Yunnan Provincial Department of Science and Technology, Kunming Medical University for Applied Basic Research [No. 2019fe001(-178)], and Top Young Talents of Yunnan Ten Thousand Talents Plan [No. YNWR-QNBJ-2018-286].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J. (2021) 134:783–91. doi: 10.1097/CM9.0000000000001474
3. Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, McGlynn KA, et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. (2020) 159:335–49.e15. doi: 10.1053/j.gastro.2020.02.068
4. Florio AA, Ferlay J, Znaor A, Ruggieri D, Alvarez CS, Laversanne M, et al. Global trends in intrahepatic and extrahepatic cholangiocarcinoma incidence from 1993 to 2012. Cancer. (2020) 126:2666–78. doi: 10.1002/cncr.32803
5. Sharma R. Descriptive epidemiology of incidence and mortality of primary liver cancer in 185 countries: evidence from globocan 2018. Jpn J Clin Oncol. (2020) 50:1370–9. doi: 10.1093/jjco/hyaa130
6. Shi JF, Cao M, Wang Y, Bai FZ, Lei L, Peng J, et al. Is it possible to halve the incidence of liver cancer in China by 2050? Int J Cancer. (2021) 148:1051–65. doi: 10.1002/ijc.33313
7. An L, Zeng HM, Zheng RS, Zhang SW, Sun KX, Zou XN, et al. Liver cancer epidemiology in China, 2015. Chin J Oncol. (2019) 41:721–7. doi: 10.3760/cma.j.issn.0253-3766.2019.10.001
8. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. Adults. N Engl J Med. (2003) 348:1625–38. doi: 10.1056/NEJMoa021423
9. Choo SP, Tan WL, Goh BKP, Tai WM, Zhu AX. Comparison of hepatocellular carcinoma in eastern versus western populations. Cancer. (2016) 122:3430–46. doi: 10.1002/cncr.30237
10. Marengo A, Rosso C, Bugianesi E. Liver cancer: connections with obesity, fatty liver, and cirrhosis. Ann Rev Med. (2016) 67:103–17. doi: 10.1146/annurev-med-090514-013832
11. Cui C, Wang B, Ren H, Wang Z. Spatiotemporal variations in gastric cancer mortality and their relations to influencing factors in S County, China. Int J Environ Res Public Health. (2019) 16:784. doi: 10.3390/ijerph16050784
12. Lei L, Huang A, Cai W, Liang L, Wang Y, Liu F, et al. Spatial and temporal analysis of lung cancer in Shenzhen, 2008-2018. Int J Environ Res Public Health. (2020) 18:26. doi: 10.3390/ijerph18010026
13. Fang JY, Wu KS, Zeng Y, Tang WR, Du PL, Xu ZX, et al. Liver cancer mortality characteristics and trends in China from 1991 to 2012. Asian Pacific J Cancer Prev. (2015) 16:1959–64. doi: 10.7314/APJCP.2015.16.5.1959
14. Fu ZT, Wang HT, Lu ZL, Chen XX, Sun JD, Zhang JY, et al. Spatial clustering analysis and trend of liver cancer death rate in Shandong Province, 1970-2013. Chin J Epidemiol. (2020) 41:1865–70. doi: 10.3760/cma.j.cn112338-20200604-00807
15. Wang L, Hu Y, Huang C, Huang Q, Hua Y, Lu Y. Spatial epidemiological and tend analysis of liver cancer in Suzhou, 2006-−2015. China Cancer. (2020) 29:481–5. doi: 10.11735/j.issn.1004-0242.2020.07.A001
16. Goovaerts P, Xiao H. Geographical, temporal and racial disparities in late-stage prostate cancer incidence across florida: a multiscale joinpoint regression analysis. Int J Health Geogr. (2011) 10:63. doi: 10.1186/1476-072X-10-63
17. Wilson L, Bhatnagar P, Townsend N. Comparing trends in mortality from cardiovascular disease and cancer in the United Kingdom, 1983-2013: joinpoint regression analysis. Popul Health Metr. (2017) 15:23. doi: 10.1186/s12963-017-0141-5
18. Crispo A, Barba M, Malvezzi M, Arpino G, Grimaldi M, Rosso T, et al. Cancer mortality trends between 1988 and 2009 in the metropolitan area of Naples and Caserta, Southern Italy: results from a joinpoint regression analysis. Cancer Biol Ther. (2013) 14:1113–22. doi: 10.4161/cbt.26425
19. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. (2000) 19:335–51. doi: 10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z
20. Rodrigues M, Bonfim C, Portugal JL, de Frias PG, Gurgel IG, Costa TR, et al. Spatial analysis of infant mortality and the adequacy of vital information: a proposal for defining priority areas. Ciencia Saude Coletiva. (2014) 19:2047–54. doi: 10.1590/1413-81232014197.18012013
21. Fan Y, Mao C, Li H, Yan X, Sun D, Siyi H, et al. Analysis and prediction of the epidemiological trend of liver cancer in the Chinese population from 1990 to 2019. Chin J Digest Surg. (2022) 21:106–13. doi: 10.3760/cma.j.cn115610-20211203-00616
22. Jiang W, MAO X, LIU Z, Zhang T, Yu S, Jin L, et al. Changing trend in reported hepatitis B incidence among residents of Mainland China, 2004 – 2017. Chin J Public Health. (2022) 38:257–61. doi: 10.11847/zgggws1132715
23. Zhang AM, Yang M, Gao L, Zhang M, Jiao L, Feng Y, et al. The distinct epidemic characteristics of Hcv co-infection among Hiv-1-infected population caused by drug injection and sexual transmission in Yunnan, China. Epidemiol Infect. (2019) 147:e261. doi: 10.1017/S0950268819001365
24. Peng H, Zhang L, Feng Y, Tang H, Luo Z, Qi Z, et al. A cross-sectional serum investigation of a clustering hepatitis C virus infection in Southwest China. J Med Virol. (2019) 91:508–13. doi: 10.1002/jmv.25315
25. Zhang Q, Huang Y, Shen L, Zhao Y, Jiang G, Zhou H, et al. Analysis of cancer risk assessment and screening results among urban residents in Kunming City. China Cancer. (2018) 27:641–6. doi: 10.11735/j.issn.1004-0242.2018.09.A001
26. Zhang L, Dong Y, Zhang X. Coupling and coordination analysis of the medical service and economic development level in china based on the national and provincial panel data from 2009 to 2019. Chin Health Serv Manag. (2022) 39:133874. doi: 10.1016/j.jclepro.2022.133874
27. Wang F, Mubarik S, Zhang Y, Wang L, Wang Y, Yu C, et al. Long-term trends of liver cancer incidence and mortality in China 1990-2017: a joinpoint and age-period-cohort analysis. Int J Environ Res Public Health. (2019) 16:2878. doi: 10.3390/ijerph16162878
28. Fei FR, Hu RY, Gong WW, Pan J, Wang M. Analysis of mortality and survival rate of liver cancer in Zhejiang Province in China: a general population-based study. Can J Gastroenterol Hepatol. (2019) 2019:1074286. doi: 10.1155/2019/1074286
29. Akinyemiju TF, Soliman AS, Johnson NJ, Altekruse SF, Welch K, Banerjee M, et al. Individual and neighborhood socioeconomic status and healthcare resources in relation to black-white breast cancer survival disparities. J Cancer Epidemiol. (2013) 2013:490472. doi: 10.1155/2013/490472
30. Chen JG, Zhang SW. Liver cancer epidemic in China: past, present and future. Semin Cancer Biol. (2011) 21:59–69. doi: 10.1016/j.semcancer.2010.11.002
31. Zheng W, Zhang H, Wang D, Wang C, Zhang S, Shen C, et al. Urban-rural disparity in cancer mortality and changing trend in Tianjin, China, during 1999 and 2016. BMC Cancer. (2021) 21:1208. doi: 10.1186/s12885-021-08907-0
32. Jiang F, Fu ZT, Lu ZL, Chu J, Guo XL, Xu A. Cancer survival during 2012-2018 in cancer registries of Shandong Province. Chin J Prev Med. (2022) 56:806–14. doi: 10.3760/cma.j.cn112150-20210910-00882
33. Makarova-Rusher OV, Altekruse SF, McNeel TS, Ulahannan S, Duffy AG, Graubard BI, et al. Population attributable fractions of risk factors for hepatocellular carcinoma in the United States. Cancer. (2016) 122:1757–65. doi: 10.1002/cncr.29971
34. Im PK, Millwood IY, Guo Y, Du H, Chen Y, Bian Z, et al. Patterns and trends of alcohol consumption in rural and urban areas of China: findings from the China kadoorie biobank. BMC Public Health. (2019) 19:217. doi: 10.1186/s12889-019-6502-1
35. Dorak MT, Karpuzoglu E. Gender differences in cancer susceptibility: an inadequately addressed issue. Front Genet. (2012) 3:268. doi: 10.3389/fgene.2012.00268
36. Petrick JL, Braunlin M, Laversanne M, Valery PC, Bray F, McGlynn KA. International trends in liver cancer incidence, overall and by histologic subtype, 1978-2007. Int J Cancer. (2016) 139:1534–45. doi: 10.1002/ijc.30211
37. Luo Z, Zou Y, Xie J, Cao H, Chen Y, Ding Y, et al. Influence of demographic factors on long-term trends of premature mortality and burden due to liver cancer: findings from a population-based study in Shanghai, China, 1973-2019. Front Public Health. (2022) 10:808917. doi: 10.3389/fpubh.2022.808917
38. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
39. Cui F, Shen L, Li L, Wang H, Wang F, Bi S, et al. Prevention of chronic hepatitis b after 3 decades of escalating vaccination policy, China. Emerg Infect Dis. (2017) 23:765–72. doi: 10.3201/eid2305.161477
40. Wang M, Wang Y, Feng X, Wang R, Wang Y, Zeng H, et al. Contribution of hepatitis b virus and hepatitis c virus to liver cancer in China north areas: experience of the Chinese National Cancer Center. Int J Infect Dis. (2017) 65:15–21. doi: 10.1016/j.ijid.2017.09.003
41. Wu W, Kang W, Kong Y, Xu L, Hu X, Li Q. Epidemiology of hepatitis b in Yunnan Province, 2005 - 2015. Dis Surveill. (2016) 31:1028–32. doi: 10.3784/j.issn.1003-9961.2016.12.012
42. Kong Y, Xu L, Kan W, li Q. Epidemiological characteristics of viral hepatitis in Yunnan Province, 1959–2014. Chin J Health Stat. (2016) 33:657–9.
43. Jia Y, Sun J, Fan L, Song D, Tian S, Yang Y, et al. Estimates of Hiv prevalence in a highly endemic area of China: Dehong Prefecture, Yunnan Province. Int J Epidemiol. (2008) 37:1287–96. doi: 10.1093/ije/dyn196
44. Ju W, Yang S, Feng S, Wang Q, Liu S, Xing H, et al. Hepatitis C virus genotype and subtype distribution in Chinese chronic hepatitis c patients: nationwide spread of Hcv genotypes 3 and 6. Virol J. (2015) 12:109. doi: 10.1186/s12985-015-0341-1
45. Quan VM, Go VF, Nam le V, Bergenstrom A, Thuoc NP, Zenilman J, et al. Risks for Hiv, Hbv, and Hcv infections among male injection drug users in Northern Vietnam: a case-control study. AIDS Care. (2009) 21:7–16. doi: 10.1080/09540120802017610
46. Marienfeld C, Liu P, Wang X, Schottenfeld R, Zhou W, Chawarski MC. Evaluation of an implementation of methadone maintenance treatment in China. Drug Alcohol Depend. (2015) 157:60–7. doi: 10.1016/j.drugalcdep.2015.10.001
47. Li J, Wang C, McGoogan JM, Rou K, Bulterys M, Wu Z. Human resource development and capacity-building during China's rapid scale-up of methadone maintenance treatment services. Bull World Health Organ. (2013) 91:130–5. doi: 10.2471/BLT.12.108951
Keywords: liver cancer, mortality, spatial autocorrelation, temporal trend, time-series data
Citation: Feng C, Liu J, Ran H, Wu L, Liang X, Sun H, Xiao Y and Chang W (2022) Spatial and temporal analysis of liver cancer mortality in Yunnan province, China, 2015–2019. Front. Public Health 10:1010752. doi: 10.3389/fpubh.2022.1010752
Received: 03 August 2022; Accepted: 05 September 2022;
Published: 27 September 2022.
Edited by:
Sumaira Mubarik, Wuhan University, ChinaReviewed by:
Muhammad Fawad, Zhengzhou University, ChinaNawsherwan, Wuhan University, China
Kamal Hezam, Nankai University, China
Copyright © 2022 Feng, Liu, Ran, Wu, Liang, Sun, Xiao and Chang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuanyuan Xiao, MzMyMjU2NDdAcXEuY29t; Wei Chang, MTM5Nzk3ODQ2NkBxcS5jb20=
†These authors have contributed equally to this work
 Chengcheng Feng
Chengcheng Feng Jinghua Liu2†
Jinghua Liu2† Hailiang Ran
Hailiang Ran Hao Sun
Hao Sun Yuanyuan Xiao
Yuanyuan Xiao