
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 29 November 2022
Sec. Occupational Health and Safety
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.1004910
Objective: Military training-induced fatigue (MIF) often results into non-combat attrition. However, standard evaluation of MIF is unavailable. This study aimed to provide credible suggestions about MIF-evaluation.
Methods: A 3-round Delphi study was performed. The authority of the experts was assessed by the authority coefficient (Aa). In round 1, categories of indicators were collected via anonymous survey of experts, then potential indicators were selected via literature search. In round 2, experts should evaluate the clinical implication, practical value, and importance of each potential indicators, or recommend new indicators based on feedback of round 1. Indicators with recommendation proportions ≥ 70% and new recommended indicators would be included in round 3 to be rated on a 5-point Likert scale. “Consensus in” was achieved when coefficient of concordance (Kendall's W) of a round was between 0.2 and 0.5 and the coefficient of variation (CV) of each aspect for an indicator was < 0.5. If round 3 could not achieve “consensus in,” more rounds would be conducted iteratively based on round 3. Indicators included in the recommendation set were ultimately classified into grade I (highly recommended) or grade II (recommended) according to the mean score and CV of the aspects.
Results: Twenty-three experts participated with credible authority coefficient (mean Aa = 0.733). “Consensus in” was achieved in round 3 (Kendall's W = 0.435, p < 0.001; all CV < 0.5). Round 1 recommended 10 categories with 73 indicators identified from 2,971 articles. After 3-round consultation, consensus was reached on 28 indicators focusing on the cardiovascular system (n = 4), oxygen transport system (n = 5), energy metabolism/metabolite level (n = 6), muscle/tissue damage level (n = 3), neurological function (n = 2), neuropsychological/psychological function (n = 3), endocrine function (n = 3), and exercise capacity (n = 2). Among these, 11 indicators were recommended as grade I: basic heart rate, heart-rate recovery time, heart rate variability, hemoglobin, blood lactic acid, urine protein, creatine kinase, reaction time, Borg Rating of Perceived Exertion Scale, testosterone/cortisol, and vertical jump height.
Conclusion: This study developed a reliable foundation for the comprehensive evaluation of MIF among soldiers.
Exercise-induced fatigue (EIF) refers to a state in which the physiological function of the body cannot be kept at a certain level or the organism cannot maintain a predetermined exercise intensity (1). Military personnel, especially soldiers, regularly train or work with heavy loads in high intensity, often at risk of fatigue (2, 3). In China, the prevalence of fatigue among military personnel is significantly higher than the general population, especially the army and navy (4). Although fatigue among military personnel can be triggered by various factors, overtraining is the primary cause (5).
Military training-induced fatigue (MIF), a special type of EIF caused by military training, has become one of the obstructions affects the combat effectiveness of the army and led to the reduction of non-combat attrition (6). Therefore, management of MIF has strategic significance for maintaining combat capability.
However, the precise pathophysiological mechanism of MIF remains unclear. Some evidences show that the occurrence of MIF correlates with both physical and social-psychological factors (7, 8). Many researchers believe that MIF is brought out by complex mechanisms, which include central and peripheral nerve-muscle functional activities (9), cardiovascular and respiratory system functions (10), energy and substance metabolism (11), internal environment disorders (12), and fatigue control chain collapse (13). The uncertainty of the mechanism results in the uncertainty of MIF diagnosis and evaluation.
Many studies have researched EIF assessment among non-military personnel like athletes: they usually focus on one or two factors contributing to EIF, such as the type of exercise, location of muscle fatigue (14), immune and inflammatory alternation (15), physiological state (16) and other factors. Although there are various researches of EIF evaluation, up to now, the confirmed and widely-acknowledged tool of EIF assessment is only the Borg's Rating of Perceived Exertion Scale, a widely used psycho-physical tool to semi-quantitatively assess subjective perception of EIF (17), while objective specific indicator for the evaluation of EIF is still absent. Take blood lactic acid (LAC), one of the traditional discussed biomarkers of EIF, as an example. The “LAC hypothesis” for muscle fatigue, a kind of EIF, states that “accumulation of lactate or acidosis in working muscle causes inhibition of contractile processes, either directly or via metabolism, resulting in diminished exercise performance” (18). At present, LAC, as an indicator of energy metabolism, has been regarded as a biomarker of EIF in some intensive exercises such as swimming (19, 20) and cycling (21, 22). However, its cut-off value of swimming and cycling is still controversial. Besides, some studies also reported unchanged level of LAC among post-exercise persons who are evaluated as EIF by Borg's Rating of Perceived Exertion Scale (23). Therefore, though various indicators may be useful in evaluation EIF triggered by specific exercise type or among specific population, their efficacy in other exercise types like military training or special population like soldiers still remains unknown.
Military training or workload often covers a variety of modes of motion and various body parts. Thus, MIF of military personnel has difference between but also relationship with EIF among athletes of specific conventional sports, i.e., the measurement of EIF may be potential indicators of MIF but may also have its limitation and needs to be re-evaluated about its efficacy and applicability in MIF evaluation with specific factors considered. For example, hemoglobin (24), blood urea (25), and creatine kinase (26, 27) were reported as indicators of EIF among athletes. However, the study of Chen et al. (28) showed that among Chinese army special operation soldiers, levels of hemoglobin, blood urea, and creatine kinase had no significant difference between MIF and non-MIF soldiers, indicating the low-efficacy of hemoglobin, blood urea, and creatine kinase in the evaluation of MIF. Besides objective indicators, some psychological factors may also impact the degree of MIF. Previous study showed that physical inactivity has proven resistant to be trained and the decision to engage in exercise is based on psychological factors (29). For example, mood state, the main manifestation of psychological state is reported to have varied impact on person in and post exercise training (29). In America, the studies of Shannon et al. (30) observed depressive symptoms among soldiers with MIF. In China, though both positive and passive psychological state have been observed in new recruits during military training (31, 32). Our previous study manifested that basic combat training, a kind of common military training, could trigger MIF among soldiers with passive mood state while adding to the pleasure feeling among soldiers with positive mood state (33), indicating the potential efficacy of mood state in assessing MIF. What is more, social factors may also impact the psychological state of soldiers, which in turn, has influence on MIF (34).
In brief, though there are various studies explored the evaluation of EIF and MIF, at present, there is no research on the comprehensive evaluation of MIF based on physical and psychological indicators among military personnel such as soldiers.
Delphi methods or Delphi technique is a structured process used to anonymously collect opinions of individuals across diverse locations and areas of expertise to select indicators or develop healthcare framework, which could avoid domination of the consensus process by one or a few experts (35). Now, Delphi methods have been widely applicated for selecting healthcare quality indicators (36), involving sports medicine (37) and healthcare evaluation (38), among normal folks (39) and military population (40). A common Delphi consensus study is composed of four domains, i.e., questionnaire preparation, expert panel, progress of Delphi survey, and Delphi results assessment to achieve consensus (36). Generally, to suit for the questionnaire of different demands, the number of Delphi round and experts, and points-scoring principle of questionnaire items are varied among Delphi studies, therefore, modified Delphi methods (41) are widely applied.
On consideration the objectivity and authority of Delphi methods, and the fact that there is still no standard criterion for evaluating MIF. This study aimed to explore credible suggestions for evaluating MIF based on the current evidence and expert consensus via Delphi methods, so as to establish qualified criteria or a standard framework for the comprehensive evaluation of MIF. The results of this study could be a strong support for MIF prevention and cure among soldiers, contributing to the maintenance and improvement of combat effectiveness.
This study was designed according to the reported Delphi method with modification (17), a method for achieving consensus among a panel of experts. In total, 3 rounds of the Delphi survey were conducted during January 2018 and January 2019 via letter. The study process is shown in Figure 1.
This study was approved by the Shanghai Changhai Hospital Ethnics Committee (No: 2018-048).
A purposive sample of Chinese experts engaged in military medicine, sports and exercise medicine, rehabilitation medicine, kinesiology and exercise science, and medical laboratory science was selected for this Delphi study. The eligible experts had experience in their related profession more than 10 years, had a title of deputy equal to or higher than associate professor/associate chief physician/chief coach/associate researcher, and were available to complete all 3 rounds of surveys in Chinese before the required deadline.
All the experts included in this study were willing to participate and signed a written informed consent.
The related research of Delphi's expert consultation method (42) suggested that the preferable number of experts is 15–30: too few participants will limit the representation, and too many participants will result in low response and agreement rates and add to the complexity and cost. Therefore, the number of experts in this study is limited to this range.
The first Delphi round aimed to underpin the categories of indicators and to search for potential evaluation indicators of MIF for further rounds.
In this round, first, experts who participated were asked to propose relative categories of indicators openly. Next, the researchers summarized the proposals into several categories and calculated the recommendation proportion of each category. Potential indicators were then searched via literature review. Database searches were performed in PubMed, Web of science, and four Chinese databases, including the China Biomedical Literature Database, the China National Knowledge Infrastructure, the Chongqing VIP Chinese Science and Technology Periodical Database, and the Wanfang databases. The search terms covered exercise-induced fatigue, fatigue, military training, soldier, and their synonyms (Supplementary material-Appendix 1). Studies published before January 31, 2018, were selected. Indicators used to evaluate the fatigue degrees of soldiers, athletes, and other participants after physical exercise were identified as potential.
Before this round, potential indicators classified into certain categories were introduced to participants as reference book A, which was written and edited by researchers according to the opinion of experts in round 1 and literature review. In this round, participants were asked to generally evaluate the clinical implication, practical value, and importance of each potential indicator, then vote for it. In this round, participants can recommend new indicators that were not involved in the reference book mentioned above and propose advice for revision of indicators, such as one indicator can be substituted by others. The recommendation proportion was calculated. Indicators with recommendation proportions ≥ 70% and new indicators recommended by participants would be included in round 3.
Before this round, the results of round 2 were reported to each participant as reference book B, which included the list of deleted indicators with reasons, the recommendation proportions of each indicator, and a literature summary of new indicators brought out in round 2. In this round, participants rated each indicator on five aspects based on a 5-point Likert scale (43). The five aspects are (1) the indicator is evidence-based (aspect 1), (2) the indicator is effective to evaluate MIF (aspect 2), (3) the indicator can prevent adverse events (aspect 3), (4) it is feasible to determine this indicator in the military (aspect 4), and (5) the indicator could be involved when measuring EIF among soldiers (aspect 5). Scores of 1 to 5 indicated disagree, slightly agree, agree, strongly agree, and completely agree, respectively.
Each Delphi round was conducted under the fully respect of subject anonymity as follows.
Before each Delphi round, researcher A sent our survey questionnaire and reference book to each expert via letter. Then within required time, experts should anonymously write their opinions, comments, and feedback in the survey questionnaire, and then send it back to researcher A. When researcher A collected back all experts' response, the anonymous paper version of response was sent to researcher B and C for data analysis.
Therefore, during this study, only researcher A knew the identity of experts, while all the opinions, comments, and feedback of experts were analyzed anonymously, and each expert get back other experts' viewpoint anonymously.
According to the modified Delphi method (43), the consistency of participant opinions in this study was measured by the coefficient of concordance (Kendall's W) and coefficient of variation (CV). Kendall's W Test was conducted to calculate the value of Kendall's W, which is a number between 0 and 1, with higher values indicating better consistency of agreement (43). The CV of each aspect for each indicator was calculated as a standard deviation/mean of scores, with lower values indicating better consistency of agreement. “Consensus in” was achieved when Kendall's W of a round was between 0.2 and 0.5 and the CV of each aspect for an indicator was < 0.5 (44). If round 3 could not achieve “consensus in,” then more rounds would be conducted iteratively according to the process of round 3 (43), i.e., a round 4 or more should be conducted until whose Kendall's W is between 0.2 and 0.5 and CV < 0.5.
The indicators included in the recommendation set, namely, the recommended indicators, met the following criteria: the mean scores of aspects 1, 2, 3 and 5 are ≥ 3.0, and that of aspect 4 is ≥ 3.5. Additionally, we classified the recommend indicators into grade I (highly recommended) or grade II (recommended). The recommended indicators included in grade I met the following criteria: (1) the mean scores of aspects 1–5 are ≥ 3.5, and (2) the CV of aspect 5 is ≤ 0.25. The recommend indicators not included in grade I were classified into grade II.
The credibility of a Delphi study, which depends on the authority of the expert panel, is important to further research based on it. Thus, according to the Delphi method (43, 44), the quality of this study was assessed by the authority coefficient (Aa), which is the arithmetic mean value of the familiarity coefficient (As) and the coefficient of judgement basis (Ai). In this study, the value of As was calculated as the sum of familiarity scores of related disciplines (military medicine, sports and exercise medicine, rehabilitation medicine, kinesiology and exercise science, and medical laboratory science). Familiarity scores were reported by participants from 1.0 to 0 corresponding to the degree of familiarity as follows: very familiar (1.0 or 0.9), familiar (0.8 or 0.7), generally familiar (0.6, 0.5, or 0.4), unfamiliar (0.3 or 0.2) or very unfamiliar (0.1 or 0). The value of Ai was calculated as the sum of the judgement basis score, which was assigned based on theoretical analysis (0.30, 0.20, and 0.10), practical experience (0.50, 0.40, and 0.30), domestic and international references (0.10, 0.08, and 0.05) and intuitive judgement (0.10, 0.07, and 0.05) sequentially for large, medium, and small levels. The authority coefficient is positively correlated with the credibility. According to previous study, Aa > 0.7 indicates good credibility (43).
The levels of agreement between participants in the first, second, and third rounds were assessed with the intraclass correlation coefficient (ICC) as another evaluation of study reliability (45). The strength of reliability was defined as: very good (0.80 ≤ ICC < 1.00), good (0.60 ≤ ICC < 0.80), moderate (0.41 ≤ ICC < 0.60), fair (0.20 ≤ ICC < 0.40), and poor ( ≤ 0.20), with p < 0.05 (46).
Response data from each round were transferred into electronic data by one researcher and checked by another researcher, then saved as Excel files (Microsoft office 2016). Data analysis was conducted using SPSS 21.0 (SPSS, Chicago, IL).
Demographic characteristics of the Delphi panel are shown in Table 1. In total, 23 of the 40 invited experts agreed to participate in all the Delphi rounds. The mean age of the participants was 46.1 years (standard deviation [SD] = 5.4). The professional experience of the participants was 23.7 years on average (SD = 5.3). All 23 participants finished the Delphi survey in rounds 1, 2 and 3. The response rate of each round was 100.0%.
A total of 10 categories were put forward in this round. The recommendation proportions of categories varied from 34.8% to 100.0% (Table 2). Indicators of exercise capacity were recommended by all participants, followed by indicators of the cardiovascular system (91.3%), neuropsychological/psychological function (78.3%), and muscle/tissue damage (73.9%). The function of the respiratory, oxygen transport, neurological function, and energy metabolism/metabolite level were recommended by the majority to be important indicators of MIF degree (recommendation proportion > 60%, respectively). Although indicators showing endocrine and immune function were also recommended, the proportions were low.
According to the categories recommended by experts, potential indicators were searched according to the database search strategy in Methods (section 2.3.1. Delphi round 1). The initial search retrieved 26,527 articles. After removing 4,531 duplications, screen via title and abstract (15602 removed), and assessed for eligibility via full text (3,423 removed), finally, 2,971 qualified articles were selected out. Among these 2,971 articles, a total of 73 indicators were identified according to the recommended 10 categories (Figure 2). Indicators evaluating the function of the nervous system and the energy metabolism/metabolite level constituted the majority, with a total proportion of 50.7% (n = 19 and 18, respectively). The number of indicators for each category is shown in Table 2. The number of articles per indicator is shown in Supplementary material-Appendix 2.
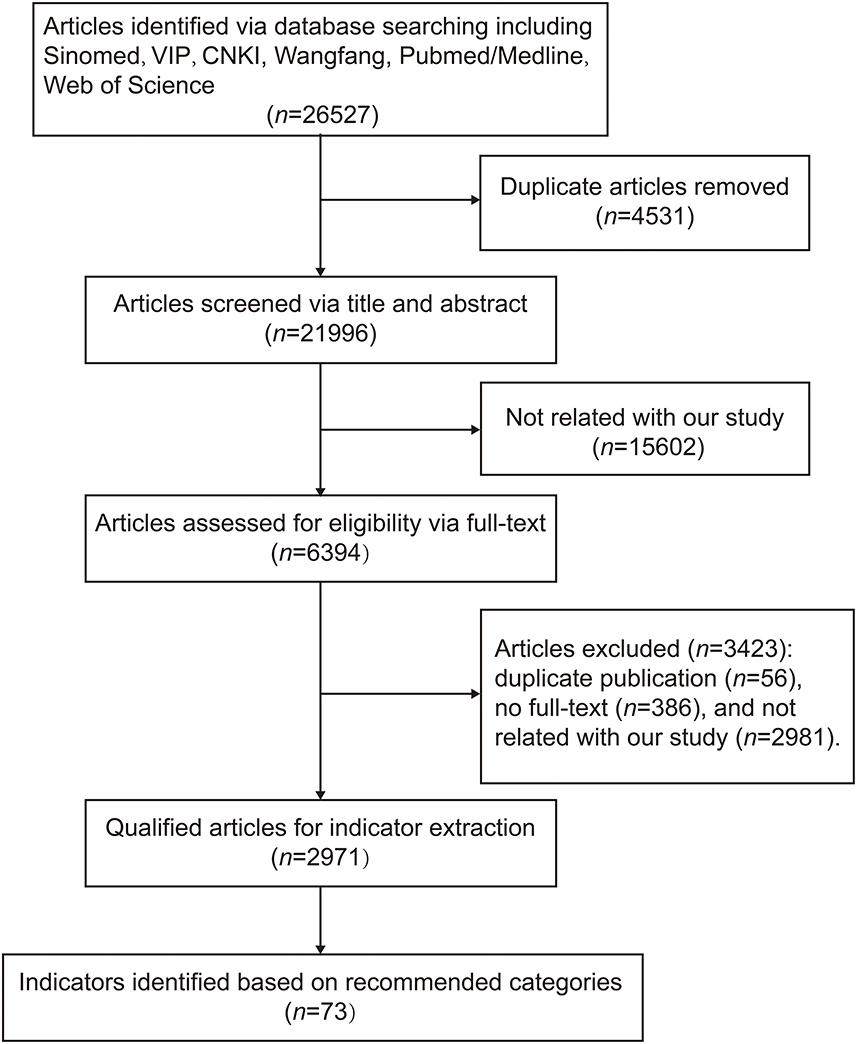
Figure 2. Process of literature review for potential indicators. CNKI, China National Knowledge Infrastructure; Sinomed, China Biomedical Literature Database; VIP, Chongqing VIP Chinese Science and Technology Periodical Database.
All 73 indicators identified in round 1 were voted by the participants. The Kendall's W of this round was 0.174 (χ2: 287.835, P < 0.001). As shown in Table 3, the recommendation proportions varied from 30.4% to 100.0%. A total of 28 indicators had recommendation proportion ≥ 70% (Table 3), among which, the indicators Wingate test was recommended to be substituted by fatigue index and mean power, and muscle strength substituted by maximum voluntary contraction and twitch force (the experts' reasons were shown in Table 4). In addition, 14 new indicators were put forward by participants including 4 for oxygen transport system, 2 for neurological function, 3 for muscle/tissue oxidative damage and neuropsychological/psychological function respectively, and 1 for immune function and exercise capacity respectively (the indicators list and experts' reasons were shown in Table 5). Therefore, a total of 44 indicators were forwarded to round 3.
The Kendall's W of round 3 is 0.435 (χ2: 430.607, P < 0.001). The mean score and CV of each aspect of the individual indicators fluctuated between 2.00 and 4.83 (Figure 3A) and between 0.080 and 0.484, respectively (Figure 3B). The value of Kendall's W (> 0.2) and CV (all < 0.5) indicated this round achieved “consensus in.” As shown in Figure 3A, 28 indicators meet the inclusion criteria of the mean score for the recommendation set, among which 14 meet the criteria for grade I (highly recommended). As shown in Figure 3B, only 13 indicators meet the inclusion criteria of the CV for grade I (highly recommended), among which 2 indicators (serum myoglobin and delayed-onset muscle soreness) did not meet the mean score criterion. Thus, a total of 28 indicators were included, with 11 classified as grade I and 17 as grade II (Figure 3 and Table 6). As shown in Table 6, the categories covered cardiovascular system (n = 4), oxygen transport system (n = 5), energy metabolism/metabolite level (n = 6), muscle/tissue damage (n = 3), neurological function (n = 2), neuropsychological/psychological function (n = 3), endocrine function (n = 3), and exercise capacity (n = 2).
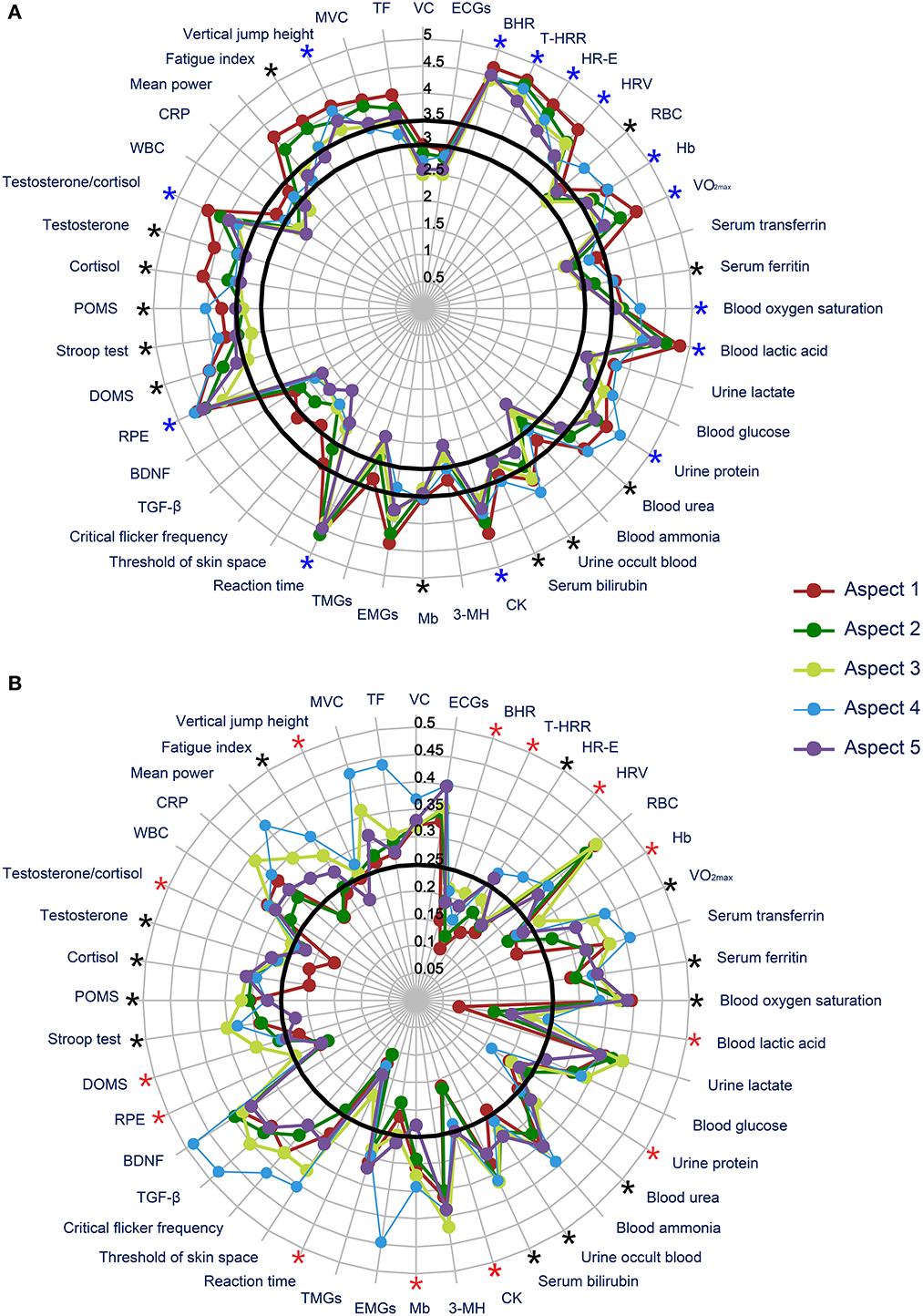
Figure 3. Results of round 3. (A) Mean score of each indicator in round 3; (B) coefficient of variation of each indicator in round 3. *in black color: indicators with mean scores of aspects 1, 2, 3 and 5 of ≥ 3.0 and that of aspect 4 of ≥ 3.5; *in blue color: indicators with mean scores of aspects 1–5 of ≥ 3.5; *in red color: indicators with CVs of aspect 5 of ≤ 0.25. VC, vital capacity; ECGs, electrocardiogram parameters; BHR, basic heart rate; T-HRR, heart-rate recovery time; HR-E, heart rate during exercise; HRV, heart rate variability; RBC, red blood cell count; Hb, hemoglobin; VO2max, maximum oxygen intake; CK, creatine kinase; 3-MH, urea 3-methylhistidine; Mb, serum myoglobin; EMGs, electromyogram parameters; TMGs, tensiomyography parameters; TGF-β, transform growth factor-β; BDNF, brain-derived neurotrophic factor; RPE, Borg's Rating of Perceived Exertion Scale; DOMS, delayed onset muscle soreness; POMS, Profile of Mood State Questionnaire; WBC, white blood cell count; CRP, C-reactive protein; MVC, maximum voluntary contraction; TF, twitch force.
The mean familiarity coefficient and judgement coefficient were 0.64 and 0.83, respectively; thus, the mean authority coefficient was 0.733 (> 0.7). The authority of experts was good, and the results of the 3-round consultation were credible.
The ICC for the first, second, and third round were 0.821 (95% confidential interval [CI]: 0.607–0.947, p < 0.001), 0.787 (95% CI: 0.710–0.852, p < 0.001), and 0.932 (95% CI: 0.899–0.958, p < 0.001), which all meet the “very good (0.80 ≤ ICC < 1.00) or good (0.60 ≤ ICC < 0.80)” criteria of reliability, further illustrating the good reliability of this Delphi study.
The Delphi method is a way to solicit expert opinions to gain consensus by iterative stages of anonymous responses (66). The goal of this method is to reduce the range of responses to gain expert consensus quantitatively and qualitatively, which is often seen as more credible than conjecture or individual opinion (42).
A total of 23 experts participated all Delphi rounds, whose average professional experience year was 23.7 years. The mean authority coefficient of experts was 0.733, indicating good authority of participants. The majority of experts are male (19/23, 82.6%) and aged between 40 and 50 years. As previous comparison study exploring the potential confounding factor of Delphi consensus reported (67), no significant difference was observed between men and women experts when giving their opinion, but the authority of experts impacts their opinion significantly. In our study, to achieve a high authority of experts, we set the qualification criteria of experts as “has experience in their related profession more than 10 years, had a title of deputy equal to or higher than associate professor/associate chief physician/chief coach/associate researcher,” which results to the experts aged between 40 and 50 years.
In round 2, 14 new indicators were put forward by participants to evaluate MIF via oxygen transport function (4/14, 28.57%), muscle/tissue oxidative damage levels (3/14, 21.43%), neurological and psycho-behavioral functions (5/14, 35.71%), immune system function (1/14, 7.14%), and exercise capacity (1/14, 7.14%). The results showed that, on the one hand, in the previous literature research (Figure 2), the research group still had some shortcomings and failed to comprehensively identify potential indicators of MIF; on the other hand, the factors involved in MIF may be much larger than we surmised: both the physical and psychological status of soldiers should be considered when evaluating MIF. As previous study on the influence of the literature searches reported (68), the amount of information available (i.e., keywords, bibliographics, abstracts) and the cognitive characteristics of the searcher could both lead to different search outcomes. In our study, literature search aimed to identify potential indicators of MIF. The initial search retrieved 26,527 articles. When removing duplications (n = 4,531), there are still a huge number of articles should be screened for checking their eligibility. Therefore, careless omission or exclusion of literature could not be avoidable, which partially leads to the gap between literature search and experts' recommendation. While, for physical and psychological status, our research strategy did not pinpoint on keywords “physical” or “psychological,” which may also partially lead to leak detection. The above results acknowledged the value of extensive expert consultation and multidisciplinary knowledge exchange in the exploration of MIF indicators and comprehensive evaluation.
After 3 rounds of consultation, a total of 28 recommended indicators (grades I and II) were screened out. Most of these indicators were involved in evaluating MIF via cardiopulmonary and oxygen transport system function (9/28, 32.14%) and energy metabolism/metabolite level (6/28, 21.43%). These results were consistent with the current “wear-out doctrine” and “blockage doctrine” of the mechanism of MIF: that is, the consumption of a large amount of energy substances and accumulation of metabolites during physical exercise/training leads to a decline in the function capacity of tissues, muscles, and organs, ultimately resulting in fatigue (17). The function of the cardiopulmonary and oxygen transport systems is the basis of substance metabolism of energy supply during the exercise process, and the level of material energy metabolism can further regulate the function of the cardiopulmonary and oxygen transport systems (17). Therefore, these two systems have an important role in maintaining the movement of the human body, and thus, should be considered in the evaluation of MIF. Besides cardiopulmonary and oxygen transport system function, and energy metabolism/metabolite level, this Delphi consultation also recommended indicators about muscle/tissue damage, neurological function, neuropsychological/psychological function, endocrine function, and exercise capacity. These results were consistent with previous study about the relationship between exercise and fatigue: physical exercise affects the equilibrium of the internal environment of various physical systems which in turn create sensations of fatigue and exhaustion in the mind of the exercising subject (69). Muscle/tissue damage indicators like creatine kinase are related to the injury of muscle cell triggered by forced myotasis during exercise/training (26, 27), and the injured muscle cells will decrease the exercise capacity of a person, therefore, leading to fatigue. The change of neurological function is one manifestation of fatigue originating from central nervous system. Some invasive indicators such as motor-evoked potentials of transcranial magnetic stimulation (70) were reported before. However, invasive examination has difficulty in the application among soldiers. In our study, reaction time (71) and Stroop test (61) recommended after three-round consensus could avoid the defects of application, further acknowledged the value of extensive expert consultation among indicator selection. For indicators on endocrine function, testosterone (72) and cortisol (73) were reported to be related to the degree of EIF among male athletes. Although their application in female athletes remained unknown, for military populations, gender limitation (the majority are men) on the contrary adds to their feasibility in assessing MIF. Finally, though decreasing of exercise capacity is the most direct symptom of MIF, how to conduct exercise capacity test without adding to the degree of fatigue is an important issue. The grade I indicator recommended by our study is vertical jump height, a simple test that will almost not deteriorate exercise capacity (65), could be a good choice for MIF evaluation.
The results of response rate, quality assessment, Kendall's W and CV showed satisfied attendance of experts (100%), good credibility of this study (authority coefficient > 0.7), and consistency of experts' opinions (Kendall's W = 0.435, all CV < 0.5 in round 3), indicating this Delphi-consensus study made a reliable recommendation about the indicators that may be potentially useful in the comprehensive evaluation of MIF among soldiers. In China, this is the first MIF-evaluation study focusing on military personnel; thus, it may benefit further research on the management of MIF among soldiers.
This study initially clarified the value of comprehensive evaluation in the diagnosis and assessment of MIF. This study better followed the principle of Delphi consensus, and therefore, is a good reference for the management of MIF. But anyway, there do be some limitations. Firstly, this consensus study based on the previous literature of fatigue evaluation and the experience of expertise, therefore, the efficacy of recommended indicators in evaluation MIF needs further study to confirm. Secondly, this consensus study recommends to evaluate MIF comprehensively based on eight aspects of physical systems/capacity, but further comprehensive frame of these aspects and specific combination of indicators needs more sectional and cohort studies to support.
In China, this is the first MIF-evaluation study focusing on military personnel; thus, it could benefit further research on the management of MIF among soldiers. This consensus study indicates the necessary to evaluate MIF in a comprehensive way. Further researches of MIF will focus on constructing a comprehensive evaluation framework for MIF diagnosis and management.
This 3-round Delphi consensus study developed a reliable foundation about the comprehensive evaluation of MIF among soldiers. Although more clinical studies should be performed to confirm the diagnostic efficacy of each potential indicator among soldiers with MIF, the recommendation of indicators in grades I and II provided a more detailed and operable reference for evaluating MIF in the Chinese military. Also, since the military population includes female soldiers, gender is an important factor that must be considered when evaluate MIF with potential indicators like neurophysiological/psychological function, endocrine function, etc.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
WG and C-qL put forward the conception and design of the study. YR, S-jS, MW, and NH collected the original data. S-jS, Z-fY, and YR analyzed and interpreted the data. Z-fY, WG, and C-qL revised it critically. All authors drafted the article and approved the final version to be submitted.
This study was supported by National Science and Technology Major Project (No: 2018ZX09J18110-003-002), Military Special Program to Cultivate and Improve TCM Service Capability (2021ZY002), and Military Health Care Special Scientific Research Project (22BJZ16) but not in data analysis and preparation of the article, writing of the report; and in the decision to submit the article for publication.
We thank all the experts who participated all the 3 rounds of this Delphi consensus study or give us valuable guidance during the process of this study. All the experts were involved in selecting and reviewing/rating the evidence, and formulating the final recommendations.
These experts were listed as follows in alphabetical order by name: Bing Cai (Chief Physician, Department of Rehabilitation Medicine, Shanghai Ninth People's Hospital, Shanghai, China); Bo Gou (Professor, Department of Sports Medicine, Xi'an Physical Education University, Xi'an, China); Chun Liang (Professor, Department of Cardiology, Changzheng Hospital, Shanghai, China); Fan-fu Fang (Physician, Department of Rehabilitation Medicine, Changhai Hospital, Shanghai, China); Hai-dong Huang (Associate Chief Physician, Department of Respiratory Medicine, Changhai Hospital, Shanghai, China); Hao-jie Li (Professor, School of Sports and Health Technology, Jilin Institute Of Physical Education, Jilin, China); Hua Yuan (Associate Professor, Department of Rehabilitation Medicine, Xijing Hospital, Xi'an, China); Jia-si Li (Associate Chief Physician, Department of Neurology, Changhai Hospital, Shanghai, China); Jia-zhen Wang (Department head of Health Services Branch, Wuxi lianqin Security Center, Wuxi, China); Jun-feng Mao (cProfessor, Military Physical and Psychological Training Center, Navy Academy of Commanding, Nanjing, China); Li Guo (Associate Professor, School of Sports Science, Shanghai University of Sport, Shanghai, China); Li Zhang (Associate Professor, Clinical Trial Center of Changhai Hospital, Shanghai, China); Liang-hua Wang (Professor, School of Basic Medicine, Navy Medical University, Shanghai, China); Lin Liu (Associate Researcher, Institute of Aeronautical Medicine, Beijing, China); Lin Shao (Associate Professor, Department of Military Sports, Navy Medical University, Dalian, China); Lin Wang (Associate Professor, School of Sports Science, Shanghai University of Sport, Shanghai, China); Min Li (Professor, Department of Military Hygiene, Navy Medical University, Shanghai, China); Ming Yang (Professor, Key Laboratory of Endurance Project, General Administration of Sport of China, Jilin, China); Qin Qin (Associate Professor, Laboratory Department, Changhai Hospital, Shanghai, China); Reng-fei Shi (Associate Professor, Department of Exercise Physiology, Shanghai University of Sport, Shanghai, China); Shen Zhang (Associate Chief Physician, Department of Rehabilitation Medicine, Changzheng Hospital, Shanghai, China); Sheng Hu (Professor/vice-president, Wuhan Sports University, Wuhan, China); Shi-bo Wang (Chief physician/president, The 101 Hospital, Wuxi, China); Wei-jie Fu (Associate Professor, School of Sports Science, Shanghai University of Sport, Shanghai, China); Wen Huang (Professor, Department of Field Battle Internal Medicine, Changhai Hospital, Shanghai, China); Xiao-dong Zhang (Professor, Logistic Support Department of China Military); Xiao-qiang Yue (Associate Chief Physician, Department of Traditional Chinese Medicine, Changzheng Hospital, China); Xue-qiang Wang (Associate Professor, School of Sports Science, Shanghai University of Sport, Shanghai, China); Yan-jie Cao (Chief physician, Department of Cardiology, Air Force General Hospital, Beijing, China); Yi-zhi Yu (Professor, Immunology Department, Navy Medical University); Yong Liu (Chief Coach, Bayi Rugby Team of Army, Nanjing, China); Yong-jun Xu (Associate Professor, Department of Military Sports, Aeronautical Mechanics School of Air Force Engineering University); You Yin (Associate Professor, Department of Neurology, Changzheng Hospital, Shanghai, China); Yu Li (Professor, Department of Military Sports, PLA Navy's Dalian Ship College, Dalian, China); Yun-xia Li (Professor, Department of Sports Medicine, Huashan Hospital, Shanghai, China); Zhao-quan Shi (Professor, Department of Respiratory Medicine, Changzheng Hospital, Shanghai, China); Zhi-fu Guo (Associate Chief Physician, Department of Cardiology, Changhai Hospital, Shanghai, China).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1004910/full#supplementary-material
1. Hou L, Su X, Bian Y, Ji W, Zhang Y, Liu X, et al. Evaluation of exercise-induced fatigue model in rats with HR using treadmill exercise with progressively increasing load. J Am Coll Cardiol. (2017) 70(16 Supplement):C64. doi: 10.1016/j.jacc.2017.07.218
2. Taylor NAS, Peoples GE, Petersen SR. Load carriage, human performance, and employment standards. Appl Physiol Nutr Metab. (2016) 41(6 Suppl 2):S131–47. doi: 10.1139/apnm-2015-0486
3. Gan Z, Yang GL, Fan YF, Chen HY, Gu W, Ling CQ. China's growing contribution to military Chinese medicine (2005–2014): a ten-year literature survey. J Integr Med. (2016) 14:480–4. doi: 10.1016/S2095-4964(16)60283-2
4. Zhang S, Cai W, Dong W, Wei C, Deng G. Effect of cognitive emotion regulation on fatigue status of soldiers. Hosp Admin J Chin PLA. (2017) 24:305–28. doi: 10.16770/j.cnki.1008-9985.2017.04.002
5. Tong CL. Causes and preventive measures for military training injury in recruits. World Latest Med Inform. (2019) 19:34–5. doi: 10.19613/j.cnki.1671-3141.2019.60.015
6. Lu Y, Lin C, Huang J, Yan H, Weng F. Management on psychoreaction of military personnel to modern war: a literature review. J Prev Med Chin PLA. (2004) 22:455–6. doi: 10.3969/j.issn.1001-5248.2004.06.019
7. Ahn S, Nguyen T, Jang H, Kim JG, Jun SC. Exploring neuro-physiological correlates of drivers' mental fatigue caused by sleep deprivation using simultaneous EEG, ECG, and fNIRS data. Front Hum Neurosci. (2016) 10:219. doi: 10.3389/fnhum.2016.00219
8. Smith CA, Miner AS, Barbee RW, Ratz PH. Metabolic stress-induced activation of AMPK and inhibition of constitutive phosphoproteins controlling smooth muscle contraction: evidence for smooth muscle fatigue? Front Physiol. (2017) 8:681. doi: 10.3389/fphys.2017.00681
9. Gandevia SC. Spinal and supraspinal factors in human muscle fatigue. Physiol Rev. (2001) 81:1725–89. doi: 10.1152/physrev.2001.81.4.1725
10. Wan JJ, Qin Z, Wang PY, Sun Y, Liu X. Muscle fatigue: general understanding and treatment. Exp Mol Med. (2017) 49:e384. doi: 10.1038/emm.2017.194
11. Kent-Braun JA, Fitts RH, Christie A. Skeletal muscle fatigue. Comprehen Physiol. (2012) 2:997–1044. doi: 10.1002/cphy.c110029
12. Hwang HJ, Kwak YS, Yoon GA, Kang MH, Park JH, Lee BK, et al. Combined effects of swim training and ginseng supplementation on exercise performance time, ROS, lymphocyte proliferation, and DNA damage following exhaustive exercise stress. Int J Vitam Nutr Res. (2007) 77:289–96. doi: 10.1024/0300-9831.77.4.289
14. Matthews MJ, Green D, Matthews H, Swanwick E. The effects of swimming fatigue on shoulder strength, range of motion, joint control, and performance in swimmers. Phys Ther Sport. (2017) 23:118–22. doi: 10.1016/j.ptsp.2016.08.011
15. Bouic PJ, Clark A, Lamprecht J, Freestone M, Pool EJ, Liebenberg RW, et al. The effects of B-sitosterol (BSS) and B-sitosterol glucoside (BSSG) mixture on selected immune parameters of marathon runners: inhibition of post marathon immune suppression and inflammation. Int J Sports Med. (1999) 20:258–62. doi: 10.1055/s-2007-971127
16. Djaoui L, Haddad M, Chamari K, Dellal A. Monitoring training load and fatigue in soccer players with physiological markers. Physiol Behav. (2017) 181:86–94. doi: 10.1016/j.physbeh.2017.09.004
17. Feng L, Feng M, Feng W. Evaluation of Physical Function of Elite Athletes. Beijing: People's Sports Press. (2003).
18. Cairns SP. Lactic acid and exercise performance: culprit or friend? Sports Med. (2006) 36:279–91. doi: 10.2165/00007256-200636040-00001
19. Nikolaidis S, Karpouzi C, Tsalis G, Kabasakalis A, Papaioannou K, Mougios V. Reliability of urine lactate as a novel biomarker of lactate production capacity in maximal swimming. Biomarkers. (2016) 21:328–34. doi: 10.3109/1354750X.2016.1138323
20. Mota MR, Dantas RAE, Oliveira-Silva I, Sales MM, Sotero RDC, Venancio PEM, et al. Effect of self-paced active recovery and passive recovery on blood lactate removal following a 200 m freestyle swimming trial. J Sports Sci. (2017) 8:155–60. doi: 10.2147/OAJSM.S127948
21. Faude O, Hecksteden A, Hammes D, Schumacher F, Besenius E, Sperlich B, et al. Reliability of time-to-exhaustion and selected psycho-physiological variables during constant-load cycling at the maximal lactate steady-state. Appl Physiol Nutr Metab. (2017) 42:142–7. doi: 10.1139/apnm-2016-0375
22. Boning D, Klarholz C, Himmelsbach B, Hutler M, Maassen N. Causes of differences in exercise-induced changes of base excess and blood lactate. Eur J Appl Physiol. (2007) 99:163–71. doi: 10.1007/s00421-006-0328-0
23. Ruan Y, Yu X, Wang H, Zou B, Song WJ, Gu W, et al. Sleep quality and military training injury during basic combat training: a prospective cohort study of Chinese male recruits. Occup Environ Med. (2021) 78:433–7. doi: 10.1136/oemed-2020-106950
25. Lin WT. Biochemical analysis of exercise training. Taiwan: China Culture University Press;. (2000).
26. da Silva DK, Jacinto JL, de Andrade WB, Roveratti MC, Estoche JM, Balvedi MCW, et al. Citrulline malate does not improve muscle recovery after resistance exercise in untrained young adult men. Nutrients. (2017) 9:e9101132. doi: 10.3390/nu9101132
27. Romagnoli M, Sanchis-Gomar F, Alis R, Risso-Ballester J, Bosio A, Graziani RL, et al. Changes in muscle damage, inflammation, and fatigue-related parameters in young elite soccer players after a match. J Sports Med Phys Fitness. (2016) 56:1198−205.
28. Chen Q. Characteristic of biomarkers of exercise-induced fatigue among army special operation soldiers. J Third Military Med University. (2019) 41:11. doi: 10.16016/j.1000-5404.201901026
29. Ekkekakis P, Parfitt G, Petruzzello SJ. The pleasure and displeasure people feel when they exercise at different intensities: decennial update and progress towards a tripartite rationale for exercise intensity prescription. Sports Med. (2011) 41:641–71. doi: 10.2165/11590680-000000000-00000
30. Crowley SK, Wilkinson LL, Wigfall LT, Reynolds AM, Muraca ST, Glover SH, et al. Physical fitness and depressive symptoms during army basic combat training. Med Sci Sports Exerc. (2015) 47:151–8. doi: 10.1249/MSS.0000000000000396
31. Wu DC, Li JY, Bai F. The mental health and its influencing factors in cadets pre and after freshman training. China J Health Psychol. (2015) 23:426–9. doi: 10.13342/j.cnki.cjhp.2015.03.030
32. Wang W. The research on the mental health of armed policemen recruits during military training. China J Health Psychol. (2007) 15:648–50. doi: 10.13342/j.cnki.cjhp.2007.07.037
33. Ruan Y, Song S-j, Yin Z-f, Wang X, Zou B, Wang H, et al. Opposite effect of basic combat training on mood state of recruits with different physical fitness: a study from perspective of fatigue. Front Psychol. (2022) 13:961351. doi: 10.3389/fpsyg.2022.961351
34. Zhou YL, Cao L, Lu S, Qi YP, Tian T, Hou LP, et al. Fatigue status of Chinese armed police force and its influence factors. Contemp Med. (2015) 21:7–10. doi: 10.3969/j.issn.1009-4393.2015.13.003
35. Jairath N, Weinstein J. The Delphi methodology (Part one): A useful administrative approach. Can J Nurs Adm. (1994) 7:29–42.
36. Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS ONE. (2011) 6:e20476. doi: 10.1371/journal.pone.0020476
37. Delahunt E, Bleakley CM, Bossard DS, Caulfield BM, Docherty CL, Doherty C, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST):2019 consensus statement and recommendations of the International Ankle Consortium. Br J Sports Med. (2018) 52:1304–10. doi: 10.1136/bjsports-2017-098885
38. Smith MD, Vicenzino B, Bahr R, Bandholm T, Cooke R, Mendonça LM, et al. Return to sport decisions after an acute lateral ankle sprain injury: introducing the PAASS framework-an international multidisciplinary consensus. Br J Sports Med. (2021) 55:1270–6. doi: 10.1136/bjsports-2021-104087
39. Carsons SE, Vivino FB, Parke A, Carteron N, Sankar V, Brasington R, et al. Treatment guidelines for rheumatologic manifestations of Sjogren's syndrome: Use of biologic agents, management of fatigue, and inflammatory musculoskeletal pain. Arthritis Care Res (Hoboken). (2017) 69:517–27. doi: 10.1002/acr.22968
40. Vining RD, Shannon ZK, Salsbury SA, Corber L, Minkalis AL, Goertz CM. Development of a clinical decision aid for chiropractic management of common conditions causing low back pain in veterans: results of a consensus process. J Manipulative Physiol Ther. (2019) 42:677–93. doi: 10.1016/j.jmpt.2019.03.009
41. Jandhyala R. Delphi, non-RAND modified Delphi, RAND/UCLA appropriateness method and a novel group awareness and consensus methodology for consensus measurement: a systematic literature review. Curr Med Res Opin. (2020) 36:1873–87. doi: 10.1080/03007995.2020.1816946
42. Taylor E. We agree, don't we? The Delphi method for health environments research. Herd. (2020) 13:11–23. doi: 10.1177/1937586719887709
43. Sun Z, Wang L. Comprehensive Evaluation Method and Its Application in Medicine. Beijing: People's Medical Publishing House. (2014).
44. Ying-fei Bi J-yM. Application of Delphi method in traditional Chinese medicine clinical research. Zhong Xi Yi Jie He Xue Bao. (2012) 10:264–70. doi: 10.3736/jcim20120304
45. Robinson N, Lorenc A, Ding W, Jia J, Bovey M, Wang XM. Exploring practice characteristics and research priorities of practitioners of traditional acupuncture in China and the EU-A survey. J Ethnopharmacol. (2012) 140:604–13. doi: 10.1016/j.jep.2012.01.052
46. Hu X, Robinson N, Yu H, Liu J. Key elements required to publish a good article: consensus among executive editors of Traditional Chinese Medicine and integrative medicine journals - a Delphi study. J Tradit Chin Med. (2015) 35:335–42. doi: 10.1016/S0254-6272(15)30107-2
47. Naharudin MN, Yusof A. Fatigue index and fatigue rate during an anaerobic performance under hypohydrations. PLoS ONE. (2013) 8:e77290. doi: 10.1371/journal.pone.0077290
48. Buchwald-Werner S, Naka I, Wilhelm M, Schutz E, Schoen C, Reule C. Effects of lemon verbena extract (Recoverben(R)) supplementation on muscle strength and recovery after exhaustive exercise: a randomized, placebo-controlled trial. J Int Soc Sports Nutr. (2018) 15:5. doi: 10.1186/s12970-018-0208-0
49. Shephard RJ. Tests of maximum oxygen intake. A critical review. Sports Med. (1984) 1:99–124. doi: 10.2165/00007256-198401020-00002
50. Bandyopadhyay A. Validity of Cooper's 12-minute run test for estimation of maximum oxygen uptake in male university students. Biol Sport. (2015) 32:59–63. doi: 10.5604/20831862.1127283
51. Di Santolo M, Stel G, Banfi G, Gonano F, Cauci S. Anemia and iron status in young fertile non-professional female athletes. Eur J Appl Physiol. (2008) 102:703–9. doi: 10.1007/s00421-007-0647-9
52. Pedlar CR, Brugnara C, Bruinvels G, Burden R. Iron balance and iron supplementation for the female athlete: A practical approach. Eur J Sport Sci. (2018) 18:295–305. doi: 10.1080/17461391.2017.1416178
53. Dominelli PB, Molgat-Seon Y, Griesdale DEG, Peters CM, Blouin J-S, Sekhon M, et al. Exercise-induced quadriceps muscle fatigue in men and women: effects of arterial oxygen content and respiratory muscle work. J Physiol. (2017) 595:5227–44. doi: 10.1113/JP274068
54. Del Coso J, Gonzalez-Millan C, Salinero JJ, Abian-Vicen J, Soriano L, Garde S, et al. Muscle damage and its relationship with muscle fatigue during a half-iron triathlon. PLoS ONE. (2012) 7:e43280. doi: 10.1371/journal.pone.0043280
55. Nagasawa T, Yoshizawa F, Nishizawa N. Plasma N tau-methylhistidine concentration is a sensitive index of myofibrillar protein degradation during starvation in rats. Biosci Biotechnol Biochem. (1996) 60:501–2. doi: 10.1271/bbb.60.501
56. Jastrzebski Z, Zychowska M, Jastrzebska M, Prusik K, Prusik K, Kortas J, et al. Changes in blood morphology and chosen biochemical parameters in ultra-marathon runners during a 100-km run in relation to the age and speed of runners. Int J Occup Med Environ Health. (2016) 29:801–14. doi: 10.13075/ijomeh.1896.00610
57. Blundell S, Ray KK, Buckland M, White PD. Chronic fatigue syndrome and circulating cytokines: A systematic review. Brain Behav Immun. (2015) 50:186–95. doi: 10.1016/j.bbi.2015.07.004
58. Verbickas V, Baranauskiene N, Eimantas N, Kamandulis S, Rutkauskas S, Satkunskiene D, et al. Effect of sprint cycling and stretch-shortening cycle exercises on the neuromuscular, immune and stress indicators in young men. J Physiol Pharmacol. (2017) 68:125–32.
59. Skurvydas A, Verbickas V, Eimantas N, Baranauskiene N, Cernych M, Skrodeniene E, et al. Psychological and physiological biomarkers of neuromuscular fatigue after two bouts of sprint interval exercise. Clin Auton Res. (2017) 8:2282. doi: 10.3389/fpsyg.2017.02282
60. Larsen LH, Hirata RP, Graven-Nielsen T. Pain-evoked trunk muscle activity changes during fatigue and DOMS. Eur J Pain. (2017) 21:907–17. doi: 10.1002/ejp.993
61. Furst T, Massaro A, Miller C, Williams BT, LaMacchia ZM, Horvath PJ. β-Alanine supplementation increased physical performance and improved executive function following endurance exercise in middle aged individuals. J Int Soc Sports Nutr. (2018) 15:32. doi: 10.1186/s12970-018-0238-7
62. Zhu BL. Brief introduction of POMS scale and its model for China. J Tianjin Institute Phys Educ. (1995) 10:35–7.
63. Cho HJ, Kivimaki M, Bower JE, Irwin MR. Association of C-reactive protein and interleukin-6 with new-onset fatigue in the Whitehall II prospective cohort study. Psychol Med. (2013) 43:1773–83. doi: 10.1017/S0033291712002437
64. Nakajima T, Kurano M, Hasegawa T, Takano H, Iida H, Yasuda T, et al. Pentraxin3 and high-sensitive C-reactive protein are independent inflammatory markers released during high-intensity exercise. Eur J Appl Physiol. (2010) 110:905–13. doi: 10.1007/s00421-010-1572-x
65. General Administration of Sport of China. Handbook of National Physical Fitness Determination Standards. Beijing: People's Sports Press (2003).
66. Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. (2000) 32:1008–15. doi: 10.1046/j.1365-2648.2000.t01-1-01567.x
67. Vidal L-A, Marle F, Bocquet J-C. Building up a project complexity framework using an international Delphi study. Int J Technol Manage. (2013) 62:251–83. doi: 10.1504/IJTM.2013.055158
68. Cooper H, Ribble R. Influences on the Outcome of Literature Searches for Integrative Research Reviews. Washington, DC.: National Inst. of Education (ED) (1985).
69. Ament W, Verkerke GJ. Exercise and fatigue. Sports Med. (2009) 39:389–422. doi: 10.2165/00007256-200939050-00005
70. Spring JN, Place N, Borrani F, Kayser B, Barral J. Movement-related cortical potential amplitude reduction after cycling exercise relates to the extent of neuromuscular fatigue. Front Hum Neurosci. (2016) 10:257. doi: 10.3389/fnhum.2016.00257
72. Taylor MK, Padilla GA, Hernandez LM. Anabolic hormone profiles in elite military men: Robust associations with age, stress, and fatigue. Steroids. (2017) 124:18–22. doi: 10.1016/j.steroids.2017.05.010
Keywords: evaluation, military training, fatigue, soldier, Delphi study
Citation: Ruan Y, Song S-j, Yin Z-f, Wang M, Huang N, Gu W and Ling C-q (2022) Comprehensive evaluation of military training-induced fatigue among soldiers in China: A Delphi consensus study. Front. Public Health 10:1004910. doi: 10.3389/fpubh.2022.1004910
Received: 27 July 2022; Accepted: 02 November 2022;
Published: 29 November 2022.
Edited by:
Ibrahim Ouergui, University of Jendouba, TunisiaReviewed by:
Luca Paolo Ardigò, NLA University College, NorwayCopyright © 2022 Ruan, Song, Yin, Wang, Huang, Gu and Ling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Gu, Z3V3ZWlzbW11QDE2My5jb20=; c2FtNjExNkAxNjMuY29t; Chang-quan Ling, Y2hhbmdxdWFubGluZ0BzbW11LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.