- 1Clinical Educational Department, Gansu Provincial Hospital, Lanzhou, China
- 2School of Public Health, The University of Queensland, Herston, QLD, Australia
- 3School of Nursing, Gansu University of Chinese Medicine, Lanzhou, China
- 4Department of Human Resource, Gansu Provincial Hospital, Lanzhou, China
- 5Geriatrics Department, Gansu Provincial Hospital, Lanzhou, China
Background: With the spread of COVID-19 around the world, herd immunity through vaccination became a key measure to control the pandemic, but high uptake of vaccine is not guaranteed. Moreover, the actual acceptance of COVID-19 vaccination and associated factors remain uncertain among health care students in Northwest China.
Methods: A cross-sectional survey of a sample of 631 health care students was performed using a questionnaire developed through Wen Juan Xing survey platform to collect information regarding their attitudes, beliefs, and acceptance of COVID-19 vaccination. Binary logistic regression analyses were performed to identify the association between vaccination willingness and demographics, attitudes, and beliefs to determine the factors that actually effect acceptance and hesitancy of COVID-19 vaccine among health care students.
Results: Overall, 491 (77.81%) students actually received the COVID-19 vaccine, and of the 140 unvaccinated, 69 were hesitant and 71 rejected. Binary logistic regression analysis showed that the actually vaccinated individuals were those who mostly believed in the effectiveness of the COVID-19 vaccine (OR = 2.94, 95%CI: 1.37, 6.29), those who mostly felt it is their responsibility to receive the vaccine to protect others from infection (OR = 2.75, 95%CI: 1.45, 5.23), with less previous experience about other vaccines (OR = 1.70, 95%CI: 1.06, 2.72), students who mostly thought COVID-19 to be very severe (OR = 1.77, 95%CI: 1.07, 2.93), and students who mostly thought the COVID-19 vaccine was one of the best protection measures (OR = 1.68, 95%CI: 1.03, 2.76). Concerns about side effects of vaccines (OR = 0.30, 95%CI: 0.18, 0.51) and the use of personal protective behavior as an alternative to the COVID-19 vaccination (OR = 0.16, 95%CI: 0.06, 0.39) hindered the vaccine acceptance.
Conclusions: Our study showed higher COVID-19 vaccine acceptance among healthcare students. However, the individuals with vaccine hesitancy and rejection were still worrying. Vaccine safety and effectiveness issues continue to be a major factor affecting students' acceptance. To expand vaccine coverage in response to the COVID-19 pandemic, appropriate vaccination strategies and immunization programs are essential, especially for those with negative attitudes and beliefs.
Introduction
Coronavirus disease 2019 (COVID-19) is still spreading around the world. Up to August 2021, a total of 216.30 million COVID-19 patients were confirmed worldwide with 4.49 million deaths (1). To mitigate the spread of COVID-19 and its impact, tireless measures have been taken. Of them, universal vaccination against COVID-19 is expected to be the most efficient preventive measure for limiting the pandemic (2). At the end of 2020, COVID-19 vaccines were approved for use. It has been reported that there have been more than 160 candidate vaccines to date, with around 20 candidates in clinical evaluation (3). With the availability of effective COVID-19 vaccines, one critical step is to achieve herd immunity through mass use of the vaccines in the general population (3). Health care workers (HCWs) including health care students are at much greater risk of developing COVID-19 with a 11-fold increased positive rates as compared to the general community (4). They also played an important role in transmission of nosocomial infections to people through the hands, equipment, and enclosing surfaces in the clinical settings (5). Therefore, HCWs including health care students were targeted in the first phase for vaccination across different countries (6, 7).
Vaccine hesitancy is defined by the World Health Organization (WHO) Strategic Advisory Group of Experts on Immunization (SAGE) as a “delay in acceptance or refusal of vaccination despite the availability of vaccination services” (8) which is recognized as a serious public health threat (9). The public would assume that given the nature of the profession, HCWs should not have hesitancy to accept the COVID-19 vaccine (10). However, evidence shows that HCWs can themselves be vaccine hesitant, which may further impact hesitancy and aversion to receiving the vaccine among the public (11, 12). During the COVID-19 pandemic, students in health care professions helped serve on the front line, worked as volunteers with vaccination campaigns, and took on roles where there could be greater exposure to COVID-19 infection (13). Additionally, health care students are prone to an increased risk of contracting infectious diseases as part of their clinical training requirement (13). Therefore, they are obliged to receive certain vaccines especially in the clinical years of their undergraduate courses. Different studies have been produced to fully understand the drivers of vaccine hesitancy and its prevalence among medical students. However, a global assessment including students/trainees of health care professions from 39 countries, conducted between April 2020 and April 2021, indicated that the overall rate of COVID-19 vaccination hesitancy was 18.9% (10). In a study conducted in the United States in February 2021, only 45% of nursing students intended to be vaccinated (14). In an Egyptian study conducted in January 2021, only 35% of the medical students accepted the vaccination (6). This issue poses a significant problem for ongoing efforts to control the current COVID-19 pandemic.
Since March 2020, China has reached a well-contained phase with work, study, and life of the general population returned to relatively normality (15). In addition, as the leading country in the development of COVID-19 vaccines, the China Health Authority approved its first COVID-19 inactivated vaccine on December 31, 2020, and the vaccines were firstly scheduled to use in groups with higher risk of infection aged 18–59 (e.g., workers in the cold-chain logistics sector, customs inspectors, health professionals, community workers) (16). A study conducted in May 2020 showed the COVID-19 vaccine hesitancy in Chinese general community was 20% (17), and meanwhile, HCWs showed more willingness to be vaccinated with 6.1% of hesitancy (18). In July 2021, the steady situation in China was dramatically overturned since the importation of the mutant delta viral strain from overseas. Due to management issues in Nanjing International Airport, workers within the airport were infected by the delta strain. Consequently, the imported delta strain has been transmitted rapidly to 27 provinces in China. Facing the possibility of outbreak resurgence, public enlightenment was of notable importance. For the global vaccination campaign to be effective, any reasons for hesitation about vaccination must be addressed. However, at present, few studies have investigated the prevalence of COVID-19 vaccine acceptance and hesitancy among health care students in Northwest China, which was less hit during the first COVID-19 wave compared to other Chinese regions; moreover, factors associated with vaccination motivation and hesitation are also unclear. Having this information could help educators identify students with hesitation and develop effective interventions to promote adherence to vaccination. In light of these gaps, our aim was to identify factors associated with the COVID-19 vaccine acceptance among health care students.
Methods
Ethics Statement
This study was approved by the Medical Ethics Committee at Gansu Provincial Hospital, Lanzhou, China. Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire.
Sample Size
According to a previous study, currently the average proportion of people who are vaccinated is 54.6% in China (17). Assume a proportion of vaccination acceptance of p = 50% and a precision level of 4% (50 ± 4%). The sample size was calculated as follows (19):
where confidence level Z (α/2) = 1.96, and δ is the allowable error (0.04). The resulting sample size of 600 was increased of 10–12% to account for questionnaires discard due to lack of information and filling errors.
Survey Design and Participants
We conducted a cross-sectional, web-based survey using an online questionnaire. The survey was administered from August 16–20, 2021, through the biggest online survey platform in China-Wen Juan Xing. Potential participants for the study were conveniently drawn from eight medical universities in Gansu, China, which were located in Northwest China, with total confirmed COVID-19 cases of 169. The eligible students were students enrolled, at any year level, in an undergraduate health care profession program majoring in a specialty area (nursing, clinical medicine, clinical laboratory, radiology, midwifery, traditional Chinese medicine, rehabilitation medicine, psychology, pharmaceutics). The director of students management of each included university was asked to randomly select 80 students. WeChat (the most popular social media platform in China) was used to distribute the survey link to the selected students via WeChat contact lists. The students were also asked to share the survey link with other health care students who were eligible and willing to take part in the study. Finally, the survey link was reached by 673 students from 13 schools or universities with all of them finishing the survey.
Instruments
In the first part of the survey page, we described the nature of the study and set informed consent that the respondents can choose to agree or disagree to continue or stop response to the questionnaire. Basically, the questionnaire was designed based on previous studies to evaluate the vaccine acceptance among students (6, 14). A preliminary pilot experiment was conducted on 30 health care students who interned in Gansu Provincial Hospital with Cronbach's alpha coefficients of the questionnaire internal consistency reliability as 0.86, which means that the questionnaire can accurately measure the degree of vaccination behavior among health care students. The final questionnaire included the following information: (1) Demographics and health status: age, gender, education level, attending volunteer activity, history of COVID-19 training, previous history of other vaccines, the way of acquiring knowledge about vaccine (Television or journals, internet, advice from others), health status. (2) Attitudes and beliefs of COVID-19 vaccination: Awareness of the severity of COVID-19, thinking COVID-19 vaccine is one of the best protection measures, having a responsibility to be vaccinated to protect others, expectation to return to normal outdoor travel and activities, trust in the effectiveness of COVID-19 vaccine, thinking vaccination is a way to ensure one's safety, complying with health ministry recommendations, concerns about side effects of vaccines, concern about the ineffectiveness of vaccines, considering the personal protection behaviors as a substitute of vaccination in the prevention of COVID-19, absence of confirmed cases locally, presence of contraindications for COVID-19 vaccination. Each subject answered all the questions. (3) Acceptance of COVID-19 vaccine: measured using a one-item question (Currently vaccine against COVID-19 is available without payment, have you taken it?) on a four-point scale (“definitely no” to “definitely yes”) which stands for the actual accept group (definitely yes), hesitancy group (“probably yes” or “probably no”), and refusal group (definitely no). In the analysis, “definitely no,” “probably yes,” and “probably no” were all referred to as unvaccinated.
Statistical Analysis
Statistical analysis was performed using SPSS 21.0, frequencies and proportions were used to describe the demographic characteristics, attitudes, beliefs, and behavior of COVID-19 vaccination. Chi-square test and Fisher's exact test were performed to preliminarily analyse various independent variables (i.e., demographics, vaccine history, vaccine knowledge, sources of information, attitudes and beliefs) related to each of the main outcomes (actual vaccination acceptance yes/no). The actual accept group and the non-vaccinated group including students who hesitated and refused were compared. Next, binary logistic analysis with the forward variable selection method was used to examine the independent factors related to COVID-19 vaccination behavior. The dependent variable was the vaccination acceptance (non-vaccinated = 0, actual vaccination = 1), with the significant factors in univariate analyses included as independent variables. In order to prevent over fitting of logistic regression model, we used Chi-square test and calculating the Phi correlation coefficient for each pair-wise correlation. Then we discarded from logistic regression model estimation those variables that have a correlation coefficient phi higher than 0.8. Significantly statistical difference was set at 0.05 (two-tailed). The odds ratio (OR), standard error (SE), 95% confidence interval (CI), and p-values were reported. As the students from each school out of the previously selected eight were <10, we did not further analyze the differences of geographic location of 13 medical schools with respect to the burden of COVID-19 experienced.
Results
Students' Characteristics
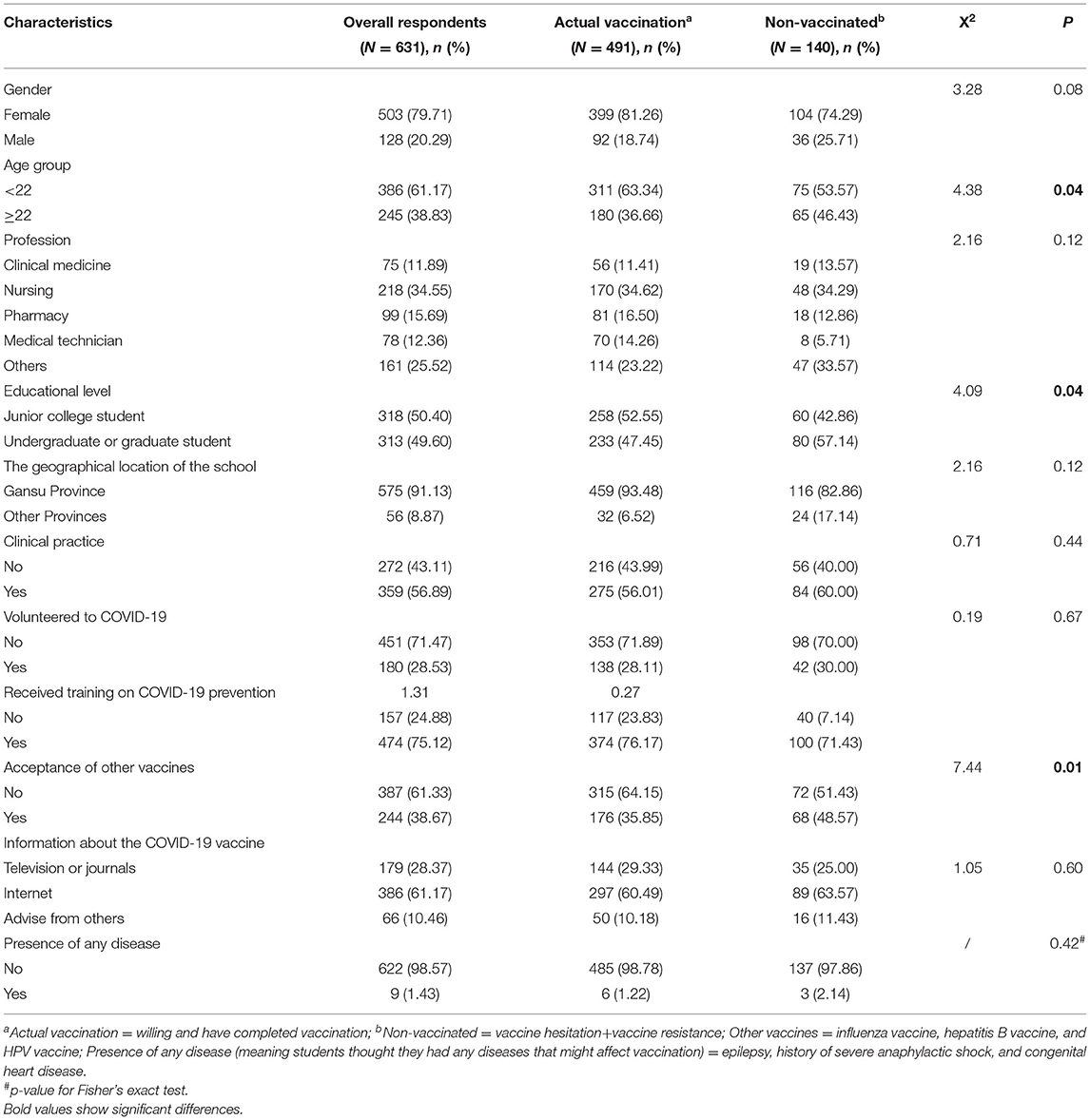
After sorting out the 673 collected questionnaires, we excluded 42 invalid questionnaires (lack of information, filling errors) and finally 631 valid questionnaires were included with a rate of 93.76%. Among 631 respondents, 79.71% were female, the mean age was 20.08 ± 1.7 years with 61.17% aged below 22, and 91.13% were students from universities in Gansu Province. More than half of the students (56.89%) have attended clinical practice, 34.55% were students majoring in nursing, and the majority (75.12%) of the students have received training on COVID-19. In total, 61.33% of students had no prior experience with other vaccines, and 1.43% thought they had presence of any disease that might affect vaccination, including epilepsy, history of severe anaphylactic shock, and congenital heart disease (Table 1).
Attitudes and Beliefs of COVID-19 Vaccination
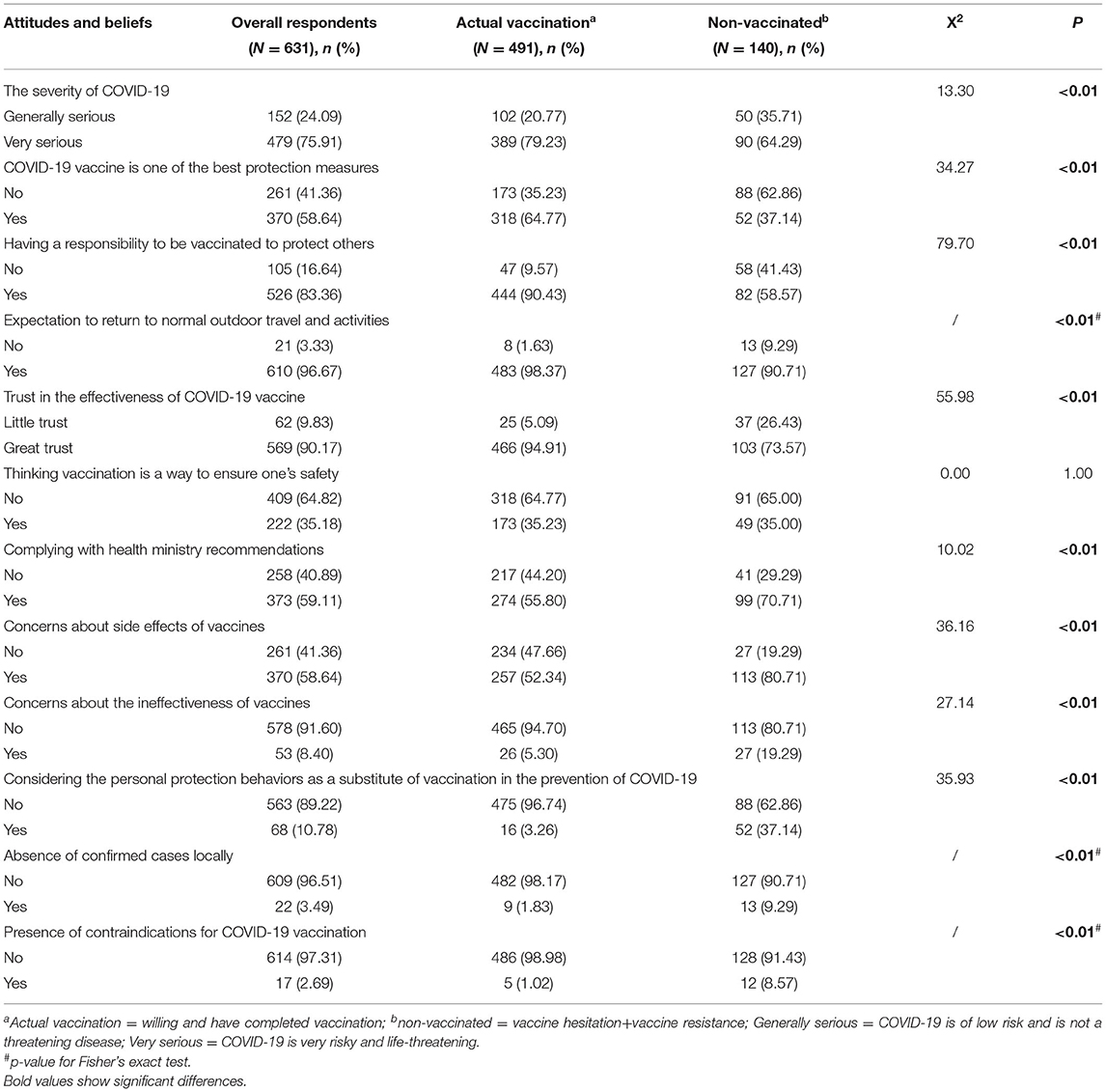
Of the 631 students included, most (75.91%) thought that COVID-19 was very serious, and 58.64% believed that vaccine was one of the best protection measures against COVID-19. In total, 88.36% of them thought they had responsibility to receive the vaccine to protect others, 96.67% wanted to resume normal outdoor travel and activities, and most (90.17%) believed the effectiveness of the COVID-19 vaccine. In addition, 59.11% wanted to comply with health ministry recommendations, while 58.64% of students were concerned about the side effects of vaccines, and 10.78% considered personal protective behavior as an alternative to vaccination against COVID-19 (Table 2).
Factors Associated With COVID-19 Vaccination Behavior
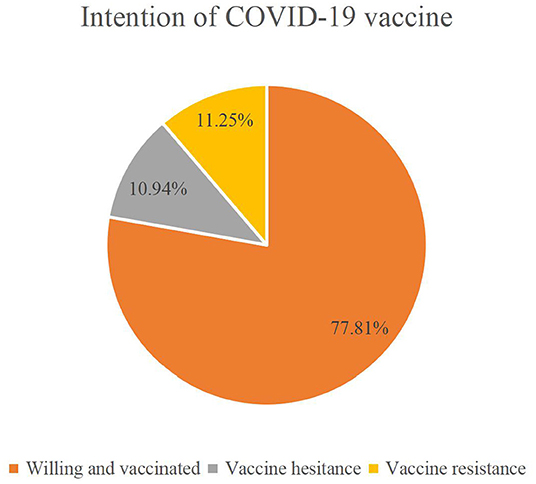
Overall, 491 (77.81%) students actually received the COVID-19 vaccine, and of the 140 unvaccinated, 69 were hesitant and 71 rejected (Figure 1).
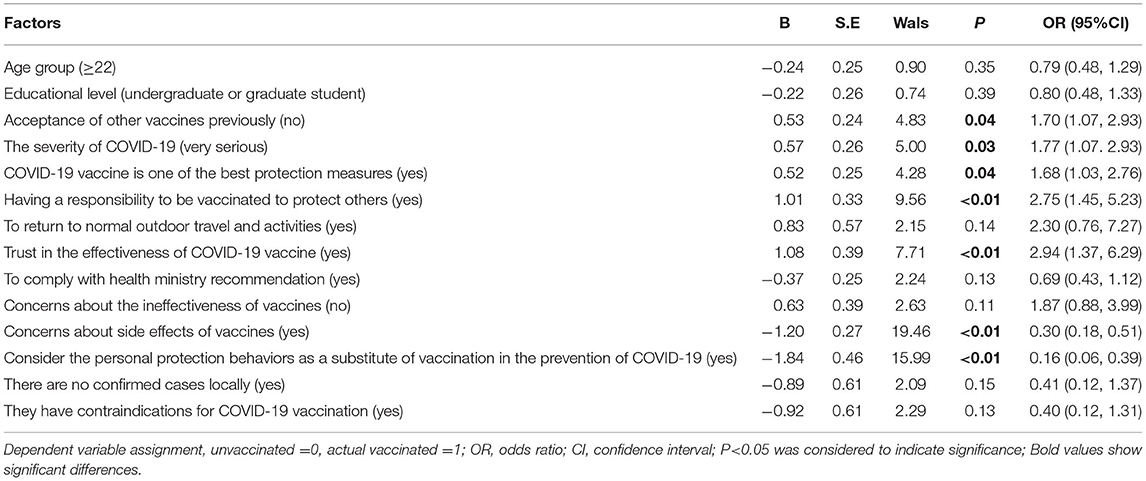
In order to eliminate the influence of confounding factors on motivations of COVID-19 vaccination, 14 statistically significant factors from the univariate analysis in Tables 1, 2 were entered into a binary regression model. Multivariate analysis results in Table 3 showed that the greatest factor affecting vaccine acceptance was trust in the effectiveness of COVID-19 vaccine (OR = 2.94, 95%CI: 1.37, 6.29) and feeling the COVID-19 vaccine as a responsibility to protect others (OR = 2.75, 95% CI: 1.45, 5.23). The actually vaccinated individuals were also more likely to be students who had not received other vaccines (OR = 1.70, 95%CI: 1.06, 2.72), students who thought COVID-19 to be very severe (OR = 1.77, 95%CI: 1.07, 2.93), students who thought COVID-19 vaccine was one of the best protection measures (OR = 1.68, 95%CI: 1.03, 2.76), and students who felt it was their responsibility to receive the vaccine to protect others from infection (OR = 2.75, 95%CI: 1.45, 5.23).
Concerns about side effects of vaccines (OR = 0.30, 95%CI: 0.18, 0.51) and the use of personal protective behavior as an alternative to COVID-19 vaccination (OR = 0.16, 95%CI: 0.06, 0.39) hindered the vaccine acceptance.
Discussion
In this study, we surveyed the acceptance of COVID-19 vaccine and related factors among health care students. Previous surveys among students majoring in nursing, dental, and medical showed the vaccine willingness rates varying from 56 to 91.9% in different countries or regions (6, 10, 13, 20–23). In the present study, the number of students willing to be vaccinated reached 88.75% with 77.81% of them actually vaccinated. Similar results were also found in Chinese nursing students (84.4%) during February–April 2021 (24), as well as Chinese HCWs with 86.2% acceptance during January 2021 (18). These high acceptance rates of COVID-19 vaccination may be associated with higher literacy on health-related issues, as well as the Chinese government's policy to complete the COVID-19 vaccination in all HCWs (25).
Importantly, multivariable analysis found that the factor that explained the greatest proportion of the variance in vaccination acceptance was trust in the effectiveness of the COVID-19 vaccine, and feeling the COVID-19 vaccine as a responsibility to protect others, similar results were also found in medical students (26, 27) and the general population (28). In our study, the majority of students (90.17%) believed the efficacy of vaccines, yet a few students were skeptical. Previous studies found that health care workers who believe in vaccines were more likely to recommend vaccines to friends, families, and their patients (18, 29). This suggested that people's general positive sense is driving vaccination intention at this point, and interventions targeted at modifying such health beliefs about COVID-19 may lead to improved vaccination rates. Thus, it is necessary for school and hospital leaders to promote widespread trust in vaccines among students through active role models and the mobilization of influencers within institutions. Students who felt they had a responsibility to get vaccinated to protect others from infection were more likely to get vaccinated. The more people have doubts about COVID-19 vaccination, the more courage and responsibility should be taken to break the doubts in society (18). Health care students were actively taking the lead in vaccination and making contributions to the country's fight against the epidemic, which reflected not only support for the epidemic prevention and value for the achievements of the fight against the epidemic but also a high level of personal ethics and trust in the health system (17, 25). The COVID-19 pandemic and its associated social isolation have worsened the mental state of people (26), and positive social outcomes such as an end to social isolation or attending in-person classes may be an important driver for increased uptake of vaccine in this population (30). Therefore, schools should actively carry out educational lectures to establish students' good sense of responsibility so that more health care students can take the initiative to shoulder the responsibility, play the vanguard role of youth, and take the lead in voluntary vaccination.
We also found that students who think COVID-19 is very serious and those think COVID-19 vaccine is one of the best protection measures were more likely to get vaccinated, which was similar to other studies (12, 18). Most of the health care students had high perceptions of the severity of COVID-19 and perceived benefits in obtaining the vaccine. However, zero confirmed delta strain cases reported in Gansu during the study period lead to insufficient awareness and risk of COVID-19 among some health care students. There is also evidence that as the number of confirmed cases continues to increase, people may be more aware of the severity of COVID-19, which further increase COVID-19 vaccine acceptance (31). Bai et al.'s research showed that students who attend health-related courses have a higher awareness of the risk of COVID-19 and thus higher vaccination rates (32). Our study did not find a significant effect of this factor on vaccination behavior, but it is worth noting that a quarter of the students in our study had still not been trained on COVID-19, which also reflects the importance that the government and schools attached to the prevention and controlling of COVID-19. Wong et al.'s study found that dissemination of knowledge about the severity of COVID-19 is needed as it has been found to be useful in influencing vaccine-related behavior (33).
In our sample there were 22% of hesitant students or students who rejected the COVID-19 vaccination. Similar results were found in India (13) and Poland (27). Even higher vaccine hesitancy was reported by medical students in Uganda (62.7%) (20), USA (44.5%) (22), and Egypt (19.4%) (6). The occurrence of COVID-19 vaccination hesitancy and refusal in students of health care professions is concerning. Without COVID-19 vaccination, health care students themselves can pose a risk of infection in high burden situations. Given that individuals are more likely to accept COVID-19 vaccination with the health care providers' recommendation, if acceptance of COVID-19 vaccines remains lower in health care professionals, how will they be able to make recommendations to others (10)?
Our results found that the most reported barrier for the vaccination among unvaccinated individuals was fear of adverse effects. Lack of vaccine confidence, in particular mistrust in the safety of a COVID-19 vaccine, represents a significant barrier to vaccine acceptance not only in our study but also indicated in dental students (34), medical students (6), as well as among HCWs (35, 36) and community population (26), which could significantly reduce an individual's confidence in the vaccine or select to delay vaccination (37–43). Thus, more information about vaccine safety, efficacy, and side effects should be addressed in a transparent way by health education campaigns. In particular, health care professionals and school leaders should be encouraged to share their COVID-19 vaccination experiences with friends or relatives to build vaccine confidence and trust (44). In addition, in our sample, the students who had not received other vaccines previously were more likely to engage in COVID-19 vaccination behavior, which was not surprising as the adverse reactions to other vaccinations in young people has been repeatedly exaggerated in the news, stoking public doubts about the vaccine's safety, which are an important reason for an individual's hesitation about vaccines (43). Universal vaccination is an important measure to control the epidemic, especially as high vaccination coverage among younger adults could be key to reaching adequate herd immunity. Strategies are required to reach individuals who distrust information from their government and health officials with accurate information concerning risks and beliefs about vaccine immunity. Future studies may benefit from qualitative methods to identify the factors that contribute to the perceived fears of vaccines, which likely include perceptions of the risk of side effect and the effectiveness against illness and associated benefits.
Similarly, our results also showed that students who consider personal protection behaviors as a substitute of vaccination in the prevention of COVID-19 were more likely to hesitate and reject vaccination, which reflected the lack of medical knowledge about COVID-19 vaccine among health care students. Some studies showed that this might be because of the misinformation dissemination within some media (36, 45). This requires the government to crack down disinformation and misinformation, and provide the public with the most authoritative information in a timely manner (45). Thus, developing an educational framework for governments and health care providers to inform the public about the risks of delaying or refusing vaccination is critical to mitigate the harmful effects of the COVID-19 pandemic (46). Meanwhile, to improve COVID-19 vaccination behavior among health care students, schools need to conduct more educational and social campaigns describing the importance of vaccination.
Strength and Limitation
To our knowledge, there was limited research regarding health care students' actual acceptance of COVID-19 vaccination. This study provides information on the impact of the COVID-19 pandemic on acceptance of vaccination among this young group, and identify factors associated with acceptance of COVID-19 vaccination.
There are limitations to this study. First, due to the selection method, the sample cannot be considered as representative of areas other than Gansu province. Moreover, the voluntary effect, i.e., participants' self-selection, does not allow us to consider the prevalence of vaccine acceptance generalizable to the health care student population. Despite these limitations, these findings are not inconsistent with the findings from previous studies about health care students' vaccine hesitancy. In the future, we need to select a large sample data to analyze whether there are differences in students' willingness to vaccinate in different areas. Second, despite our study recruiting an adequate number of students, the study focused on the working setting, and thus years of participants studying in university were not collected. In addition, this paper did not compare the intention of vaccination during or after the pandemic, and future study should compare this difference in detail.
Conclusions
In the present survey, the majority of students already received the COVID-19 vaccine. However, those who hesitated or rejected the vaccine were still worrying. Vaccine safety and effectiveness issues continue to be a major factor affecting students' acceptance. The negative attitudes and beliefs about vaccinations toward COVID-19 were highly correlated with vaccination hesitancy or rejection. It is important to design an evidence-based strategy to promote the uptake of vaccination for health care students. Additionally, effectiveness and the safety of the vaccine will be important when rolling out the COVID-19 vaccine. Future studies are needed to explore reasons of COVID-19 vaccination acceptance, and to examine the effectiveness of promotion strategies.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee at Gansu Provincial Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JZ, JD, YS, and JW: conception and design of the study. JZ and DW: acquisition of data. YY, JD, and JW: analysis and interpretation of data. JZ and YY: drafting the article. ZZ, JD, YY, JZ, and JW: revising the article. JW and JZ: funding acquisition. All authors contributed to the final approval of the version to be submitted.
Funding
This research was funded by Natural Science Foundation of Gansu Province (Grant number 21JR7RA613), Lanzhou Chengguan District Science and Technology plan project (Grant number 2019RCCX0011), Horizontal project of Lanzhou Hand-foot Surgery Hospital (Grant number 071100278), and Natural Science Foundation of Gansu Province (Grant number 21JR7RA607).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are grateful to eight student managers from medical universities for recruiting participants in this study.
References
1. WHO. Coronavirus Disease (?COVID-19)?: Weekly Epidemiological Update on COVID-19 (2021). Available online at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19 (accessed 24 August, 2021)
2. Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. (2020) 26:100495. doi: 10.1016/j.eclinm.2020.100495
3. Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 vaccines at pandemic speed. N Engl J Med. (2020) 382:1969–73. doi: 10.1056/NEJMp2005630
4. Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. (2020) 5:e475–83. doi: 10.1016/S2468-2667(20)30164-X
5. Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin Med. (2020) 20:124–7. doi: 10.7861/clinmed.2019-coron
6. Saied SM, Saied EM, Kabbash IA, Abdo SAE. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol. (2021) 93:4280–91. doi: 10.1002/jmv.26910
7. Eibensteiner F, Ritschl V, Nawaz FA, Fazel SS, Tsagkaris C, Kulnik ST, et al. People's willingness to vaccinate against COVID-19 despite their safety concerns: twitter poll analysis. J Med Internet Res. (2021) 23:e28973. doi: 10.2196/28973
8. MacDonald NE. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
9. Ebrahimi OV, Johnson MS, Ebling S, Amundsen OM, Halsøy Ø, Hoffart A, et al. Risk, trust, and flawed assumptions: vaccine hesitancy during the COVID-19 pandemic. Front Public Health. (2021) 9:700213. doi: 10.3389/fpubh.2021.700213
10. Mustapha T, Khubchandani J, Biswas N. COVID-19 vaccination hesitancy in students and trainees of healthcare professions: a global assessment and call for action. Brain Behav Immun Health. (2021) 16:100289. doi: 10.1016/j.bbih.2021.100289
11. Qattan AMN, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. (2021) 8:644300. doi: 10.3389/fmed.2021.644300
12. Li M, Luo Y, Watson R, Zheng Y, Ren J, Tang J, et al. Healthcare workers' (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J. (2021) 30:postgradmedj-2021-140195. doi: 10.1136/postgradmedj-2021-140195
13. Jain J, Saurabh S, Kumar P, Verma MK, Goel AD, Gupta MK, et al. COVID-19 vaccine hesitancy among medical students in India. Epidemiol Infect. (2021) 149:e132. doi: 10.1017/S0950268821001205
14. Kregar Velikonja N, Dobrowolska B, Stanisavljević S, Erjavec K, Globevnik Velikonja V, Verdenik I. Attitudes of nursing students towards vaccination and other preventive measures for limitation of COVID-19 pandemic: cross- sectional study in three European Countries. Healthcare. (2021) 9:781. doi: 10.3390/healthcare9070781
15. Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. (2020) 8:482. doi: 10.3390/vaccines8030482
16. Press Conference of the Joint Prevention and Control Mechanism of the State Council (2021). Available online at: http://www.gov.cn/xinwen/gwylflkjz145/index.htm. (accessed January 14, 2021)
17. Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. (2020) 14:e0008961. doi: 10.1371/journal.pntd.0008961
18. Wang MW, Wen W, Wang N, Zhou MY, Wang CY Ni J, et al. COVID-19 vaccination acceptance among healthcare workers and non-healthcare workers in China: a survey. Front Public Health. (2021) 9:709056. doi: 10.3389/fpubh.2021.709056
19. Schmidt SAJ, Lo S, Hollestein LM. Research techniques made simple: sample size estimation and power calculation. J Invest Dermatol. (2018) 138:1678–82. doi: 10.1016/j.jid.2018.06.165
20. Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Trop Med Health. (2021) 49:37. doi: 10.1186/s41182-021-00331-1
21. Szmyd B, Bartoszek A, Karuga FF, Staniecka K, Błaszczyk M, Radek M. Medical students and SARS-CoV-2 vaccination: attitude and behaviors. Vaccines. (2021) 9:128. doi: 10.3390/vaccines9020128
22. Mascarenhas AK, Lucia VC, Kelekar A, Afonso NM. Dental students' attitudes and hesitancy toward COVID-19 vaccine. J Dent Educ. (2021) 85:1504–10. doi: 10.1002/jdd.12632
23. Kelekar AK, Lucia VC, Afonso NM, Mascarenhas AK. COVID-19 vaccine acceptance and hesitancy among dental and medical students. J Am Dent Assoc. (2021)152:596–603. doi: 10.1016/j.adaj.2021.03.006
24. Jiang N, Wei B, Lin H, Wang Y, Chai S, Liu W. Nursing students' attitudes, knowledge and willingness of to receive the coronavirus disease vaccine: a cross-sectional study. Nurse Educ Pract. (2021) 55:103148. doi: 10.1016/j.nepr.2021.103148
25. Xu B, Gao X, Zhang X, Hu Y, Yang H, Zhou YH. Real-world acceptance of COVID-19 vaccines among healthcare workers in perinatal medicine in China. Vaccines. (2021) 9:704. doi: 10.3390/vaccines9070704
26. Shih SF, Wagner AL, Masters NB, Prosser LA, Lu Y, Zikmund-Fisher BJ. Vaccine hesitancy and rejection of a vaccine for the novel coronavirus in the United States. Front Immunol. (2021) 12:558270. doi: 10.3389/fimmu.2021.558270
27. Grochowska M, Ratajczak A, Zdunek G, Adamiec A, Waszkiewicz P, Feleszko W, et al. Comparison of the level of acceptance and hesitancy towards the influenza vaccine and the forthcoming COVID-19 vaccine in the medical community. Vaccines. (2021) 9:475. doi: 10.3390/vaccines9050475
28. Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 Vaccination hesitancy in the United States: a rapid national assessment. J Community Health. (2021) 46:270–7. doi: 10.1007/s10900-020-00958-x
29. Wang K, Wong ELY, Ho KF, Cheung AWL, Chan EYY, Yeoh EK, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. (2020) 38:7049–56. doi: 10.1016/j.vaccine.2020.09.021
30. Kecojevic A, Basch CH, Sullivan M, Chen YT, Davi NK. COVID-19 Vaccination and intention to vaccinate among a sample of college students in New Jersey. J Community Health. (2021) 27:1–10. doi: 10.1007/s10900-021-00992-3
31. McCord M. Coronavirus Vaccine: How Soon Will We Have One? (2020) Available online at: https://www.weforum.org/agenda/2020/03/vaccine-covid-19-coronavirus-pandemic-healthcare/ (accessed March 26, 2020)
32. Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, et al. Attitudes toward COVID-19 vaccines in Chinese college students. Int J Biol Sci. (2021) 17:1469–75. doi: 10.7150/ijbs.58835
33. Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. (2020) 16:2204–14. doi: 10.1080/21645515.2020.1790279
34. Riad A, Abdulqader H, Morgado M, Domnori S, Koščík M, Mendes JJ, et al. Global prevalence and drivers of dental students' COVID-19 vaccine hesitancy. Vaccines. (2021) 9:566. doi: 10.3390/vaccines9060566
35. Wang J, Feng Y, Hou Z, Lu Y, Chen H, Ouyang L, et al. Willingness to receive SARS-CoV-2 vaccine among healthcare workers in public institutions of Zhejiang Province, China. Hum Vaccin Immunother. (2021) 17:2926–33. doi: 10.1080/21645515.2021.1909328
36. Karafillakis E, Dinca I, Apfel F, Cecconi S, Wurz A, Takacs J, et al. Vaccine hesitancy among healthcare workers in Europe: a qualitative study. Vaccine. (2016) 34:5013–20. doi: 10.1016/j.vaccine.2016.08.029
37. Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. (2020) 9:16. doi: 10.3390/vaccines9010016
38. Peretti-Watel P, Verger P, Raude J, Constant A, Gautier A, Jestin C, et al. Dramatic change in public attitudes towards vaccination during the 2009 influenza A(H1N1) pandemic in France. Euro Surveill. (2013) 18:20623. doi: 10.2807/1560-7917.es2013.18.44.20623
39. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H. Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine : a survey of US adults. Ann Intern Med. (2020) 173:964–73. doi: 10.7326/M20-3569
40. Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. (2020) 35:785–8. doi: 10.1007/s10654- 020-00675-8
41. Laurence D, Görlich Y, Simmenroth A. How do applicants, students and physicians think about the feminisation of medicine?- a questionnaire-survey. BMC Med Educ. (2020) 20:48. doi: 10.1186/s12909-020-1959-2
42. Shaw J, Stewart T, Anderson KB, Hanley S, Thomas SJ, Salmon DA, et al. Assessment of U.S. health care personnel (HCP) attitudes towards COVID-19 vaccination in a large university health care system. Clin Infect Dis. (2021) 25:ciab054. doi: 10.1093/cid/ciab054
43. Yoda T, Katsuyama H. Willingness to receive COVID-19 vaccination in Japan. Vaccines. (2021) 9:48. doi: 10.3390/vaccines9010048
44. Schaffer DeRoo S, Pudalov NJ, Fu LY. Planning for a COVID-19 vaccination program. JAMA. (2020) 323:2458–9. doi: 10.1001/jama.2020.8711
45. Wake AD. The willingness to receive COVID-19 vaccine and its associated factors: “vaccination refusal could prolong the war of this pandemic” - A systematic review. Risk Manag Healthc Policy. (2021) 14:2609–23. doi: 10.2147/RMHP.S311074
Keywords: COVID-19 vaccine, healthcare students, vaccine hesitant, vaccine acceptance, China
Citation: Zhang J, Dean J, Yin Y, Wang D, Sun Y, Zhao Z and Wang J (2022) Determinants of COVID-19 Vaccine Acceptance and Hesitancy: A Health Care Student-Based Online Survey in Northwest China. Front. Public Health 9:777565. doi: 10.3389/fpubh.2021.777565
Received: 16 September 2021; Accepted: 02 December 2021;
Published: 06 January 2022.
Edited by:
Bijaya Kumar Padhi, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
Mohamed Helmy, Agency for Science, Technology and Research (A*STAR), SingaporeNeeti Rustagi, All India Institute of Medical Sciences Jodhpur, India
Maria Pia Fantini, University of Bologna, Italy
Copyright © 2022 Zhang, Dean, Yin, Wang, Sun, Zhao and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenhua Zhao, NjQ4OTUwMjJAcXEuY29t; Jiancheng Wang, MzY0OTU0NjcyQHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Juxia Zhang
Juxia Zhang Judith Dean
Judith Dean Yuhuan Yin
Yuhuan Yin Dongping Wang
Dongping Wang Yanqing Sun1
Yanqing Sun1 Zhenhua Zhao
Zhenhua Zhao Jiancheng Wang
Jiancheng Wang