- Eye Center, Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China
The cognitive attitudes and behaviors of medical post-graduates may be influenced by the coronavirus disease 2019 (COVID-19) pandemic. A cross-sectional study was used from a questionnaire survey in hospitals affiliated with the Zhejiang University School of Medicine. Questionnaire was distributed online including demographic information, cognitive attitudes, and personal protective behaviors. Moreover, personal protective behaviors such as wearing protective equipment were compared between different academic major and gender, respectively. A total of 176 valid questionnaires were obtained. Of the medical post-graduates in this study, (1) 89.67% believed that the COVID-19 pandemic had an impact on their clinical internships, and 40.34% expressed concerns about their infection on inadequate personal protection; (2) 91.48% took personal protection in hospital and 86.36% enhanced personal hygiene; (3) There were no statistically differences in the personal protection by academic major and gender (p > 0.05). This study suggests that the COVID-19 pandemic had an impact on the medical post-graduates' clinical practice, and affected their cognitive attitudes and behaviors. As such, universities and hospitals should increase pandemic prevention training and investment, provide more psychological counseling to their medical post-graduates to reduce their psychological burden, and take measures to reduce the influence of the COVID-19 pandemic on their medical post-graduates' clinical practice.
Introduction
Since the World Health Organization announced in January 2020 that the coronavirus disease 2019 (COVID-19) pandemic is a public health emergency of international concern (1), the Chinese medical staff have demonstrated outstanding skill and dedication in striving to save lives across the country. COVID-19 has caused unprecedented damage to the medical education system worldwide (2). It is difficult to continue teaching as usual, thus affecting the lecture and patient-based clinical practice (3). The COVID-19 pandemic puts people at risk, which poses a major challenge to medical education, because teachers must teach safely while at the same time ensuring the integrity and continuity of the medical education system. Due to the focus on patients with COVID-19, these challenges have resulted in limited patient care, which limits the opportunities for medical students to teach at the bedside (4). Clinical practice through rotation has been suspended for a long time (5). Other challenges include concerns that medical students may contract the virus during their clinical practice and need to wear personal protection (6). Passing on their skill and dedication to the future medical practitioners is the most important task of medical education. In consequence, COVID-19 may cause great impact on the medical students' attitude and behaviors during the clinical practice (7, 8).
As of this writing, as the COVID-19 pandemic is under control in China, clinical medical post-graduates have returned to the hospital to carry out their internships. However, due to the normalization of the pandemic prevention, the medical post-graduates who are preparing for medical practice are not only striving to learn what they should but are also enduring the long-term challenges posed by the COVID-19 pandemic. There is a growing literature on how medical educators and students adapted to the COVID-19 pandemic (9–13). However, the studies from China are limited. In this study, the cognitive attitudes and behaviors of medical post-graduates conducting internship during the COVID-19 pandemic in China were investigated through a questionnaire survey. Our research questions are:
1. What are the clinical medical post-graduates' cognitive attitudes toward the COVID-19 pandemic?
2. What are the personal protective measures taken by the clinical medical post-graduates in response to the COVID-19 pandemic?
3. What are the difference of prevention and control measures taken by clinical medical post-graduates with different majors?
4. What are the difference of prevention and control measures taken by clinical medical post-graduates with different genders?
Methods
Participants
The subjects of this study were clinical medical post-graduates of the Zhejiang University School of Medicine. We conducted a cross-sectional survey from March to April, 2021.
Data Collection From the Questionnaire Survey
The questionnaires had 3 parts. The first part asked about the basic demographic information of the respondents (such as gender, age, grade, academic major, and health status). The second part was the questionnaire addressed their experience with cognitive attitudes during the COVID-19 pandemic, including the impact of COVID-19 on clinical practice, reasons for anxiety and fear during clinical practice, worry in clinical practice during the COVID-19 pandemic, the most desirable COVID-19 prevention and training mode, most desired COVID-19-related training content, vaccination, and most gratified thing about the current pandemic prevention and control. The third part was the investigation of personal protective measures of the clinical medical post-graduates. They were asked about which kinds of personal protective measures to take, such as wearing protective articles in the hospital, strengthening one's personal hygiene, reducing access to patients, and exercising more to improve one's immunity.
We developed the questionnaire in Chinese. We tested its internal consistency in a pilot study comprising 50 students. All the questionnaires had high level of internal consistency among our study population, with a Cronbach's alpha over 0.9 (0.91, 0.94, 0.96, respectively). An electronic survey questionnaire was formulated and randomly sent out through the Questionnaire Star survey program (https://www.wjx.cn/) on WeChat. A total of 195 questionnaires were sent out. Nineteen of the retrieved questionnaires were invalid and were thus excluded from the study, and 176 were valid. The effective survey questionnaire retrieval rate was thus 90.26%.
Statistical Analysis
The data from the retrieved electronic survey questionnaires were gathered by Questionnaire Star. We described categorical variables as frequencies and percentages. The data were analyzed using chi-square tests (χ2) to compare the differences between groups and p-values were two-sided and considered significant at p < 0.05. All data were analyzed by SPSS version 22.0 software.
Ethical Approval
Ethical approval was obtained from the ethics committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University in China. All participants provided written informed consent prior to participating in the study, without identifiable data.
Results
Demographic Characteristics
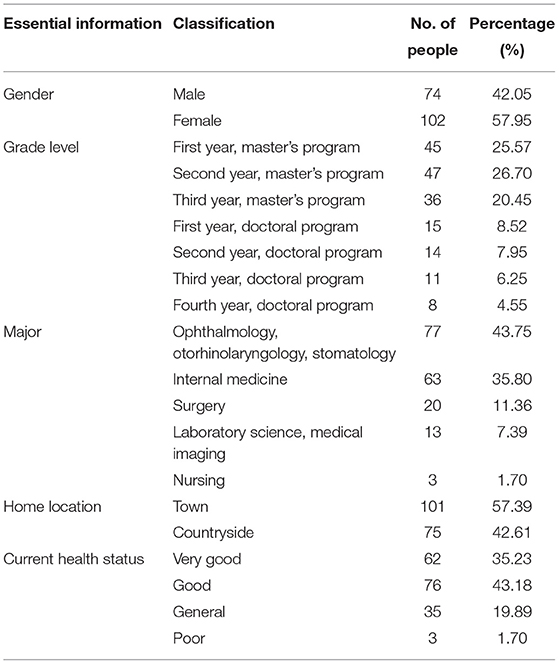
A total of 176 medical post-graduates completed the survey, and most of them (57.95%) were female. Table 1 shows the distribution of the study participants. Most of those who completed the survey were post-graduate students of ophthalmology, otorhinolaryngology, and stomatology (43.75%). The current health status of the students was basically good, and the proportion of students with a poor health status was only 1.7% based on self-assessment.
Cognitive Attitudes of Medical Post-graduates in Clinical Practice During the COVID-19 Pandemic
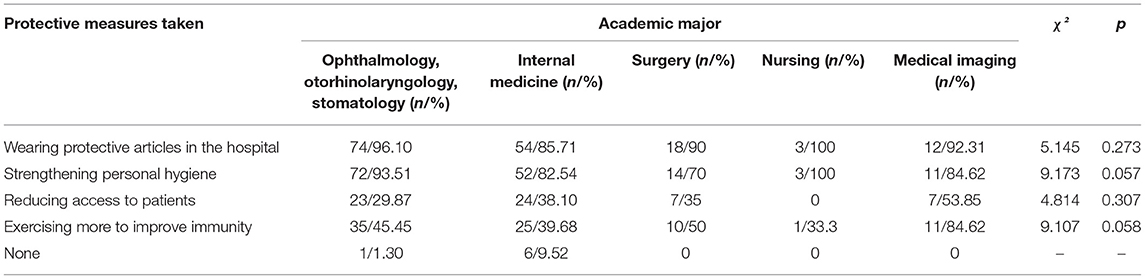
Of the medical post-graduates who participated in this study, 89.77% believed that the COVID-19 pandemic had affected their clinical practice in different ways (Table 2). Among these was the fact that they developed nervousness and fear due to their knowledge that the virus causing COVID-19 could be transmitted in various ways and was highly infectious. Their biggest worries in relation to their clinical practice were self-infection, cross-infection, and large-scale infection due to inadequate personal protection, the presence of too many patients in the hospital, and the patients' concealment of their illness. For pandemic prevention and training mode, most of the students hope to obtain is the unified arrangement of the medical school and the hospital. Most of the students (63.64%) thought that the COVID-19 vaccines were effective, and 66.5% thought that being vaccinated is the best way to gradually return to original clinical work.
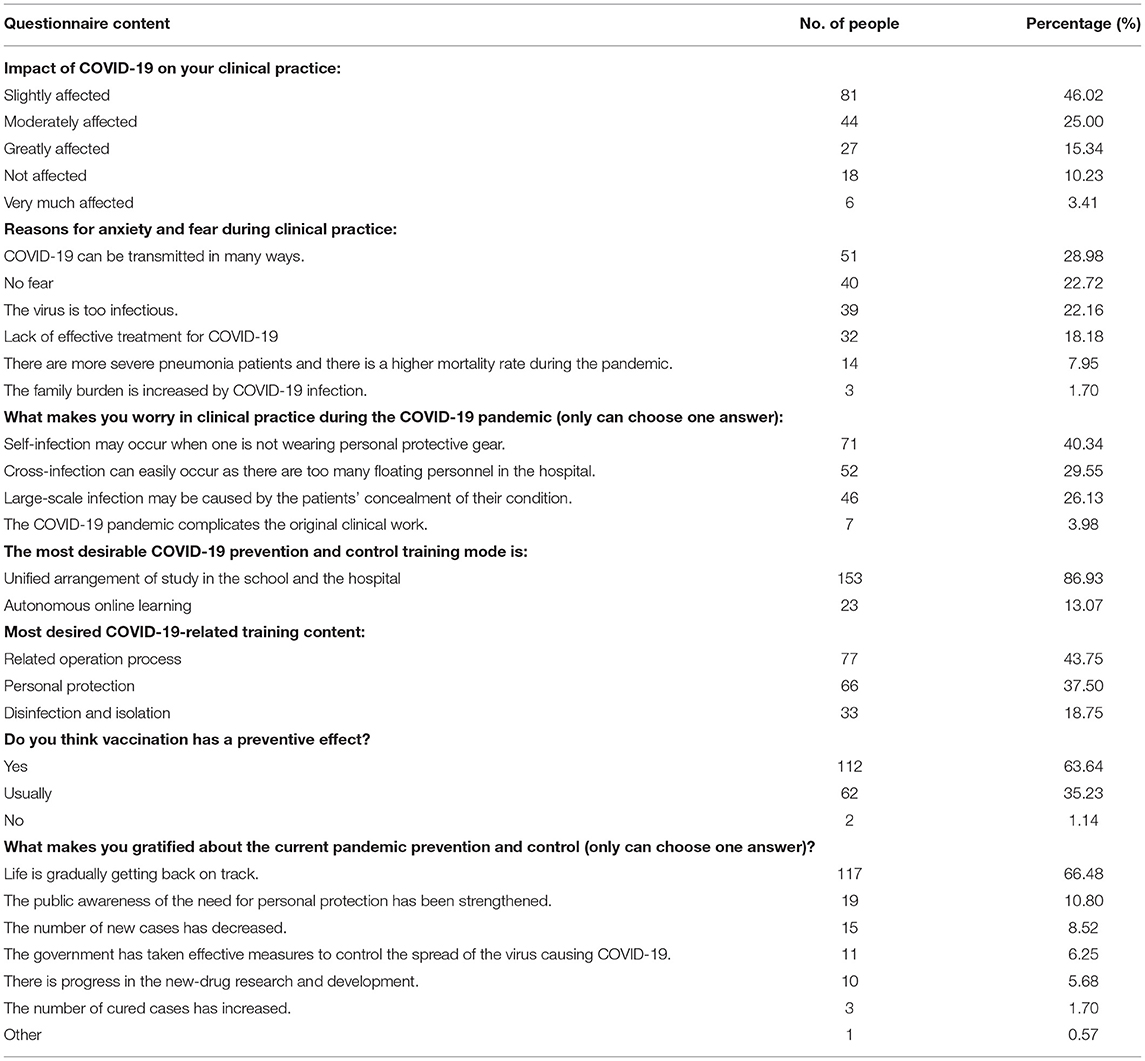
Table 2. Results of the questionnaire survey on the clinical medical post-graduates' cognitive attitudes toward the COVID-19 pandemic.
Personal Protective Measures and Behaviors of Clinical Medical Post-graduates During the COVID-19 Pandemic
Of the medical post-graduates who participated in this study, 161 (91.48%) took protective measures against COVID-19 infection in the hospital during their internship (Table 3). One hundred fifty-two medical post-graduates (86.36%) chose to strengthen their personal hygiene, and 61 (34.66%) chose to reduce their contact with the patients. The number of medical post-graduates who exercised more to improve their immunity was basically the same as the number of those who did not take such measure. Seven medical post-graduates (3.98%) did not take any measure to prevent themselves from acquiring COVID-19.
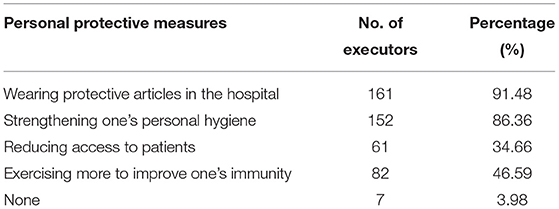
Table 3. Survey questionnaire items on the personal protective measures taken by the clinical medical post-graduates in this study during the COVID-19 pandemic.
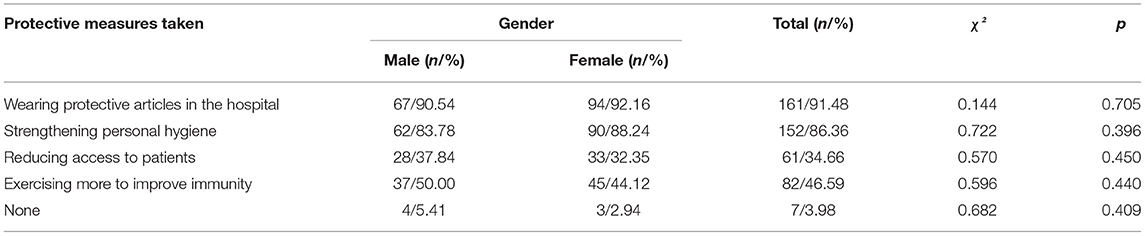
Prevention and Measures Taken by Clinical Medical Post-graduates With Different Majors and Genders
Table 4 shows that there was no statistically significant difference in taking various prevention and measures among the medical post-graduates in this study by academic major (p > 0.05). Table 5 shows that the proportion of male and female medical post-graduates who wear protective items in hospitals exceeds 90%. Interestingly, in terms of strengthening personal hygiene, the percentage of males who did so (83.78%) was slightly lower than the percentage of females who did the same (88.24%). There was no significant difference in the prevention and measures taken by gender (p > 0.05).
Discussion
The COVID-19 pandemic has swept the world, and the pandemic prevention and control work has become a norm (14). As they serve as the backup force of clinicians, medical post-graduates consider clinical practice the main content of their study. However, due to the large number of patients in hospitals and the high work intensity, their occupational exposure risk from the doctor–patient ratio imbalance is much higher than that of students in other academic majors (15). The changeable clinical situation will create tremendous pressure on clinical medical students who are still in the growth stage, and this is likely to affect their clinical study and practice (16). During the COVID-19 pandemic, especially in the stage of normalization of the pandemic prevention and control work, medical post-graduates in clinical practice are faced with clinical risks and thus belong to the high-risk groups. This study focused on the cognitive attitudes and prevention and control behaviors of clinical medical students during the COVID-19 pandemic. According to the survey, the pandemic has had an impact on the medical post-graduates' clinical practice, but the students have a relatively positive attitude toward the pandemic situation. They are also doing a good job of protecting themselves in their clinical practice. For hospitals and schools, they should strengthen their personal protection training, encourage active participation in vaccination, and strengthen the teaching of infectious-disease prevention and control. At the same time, they should actively cultivate the professional quality and identity of medical post-graduates.
The survey showed that 89.77% of the medical post-graduates thought that the COVID-19 pandemic has had an impact on them. Among these, 15.34% thought that the pandemic has had a great influence and 3.41% thought that the pandemic has had a major influence on their clinical practice. The reasons for these can be roughly divided into two points. First, in early 2020, when the domestic pandemic situation was relatively severe, almost all the medical students in clinical practice were required to stop their practice for their own protection (17). They resumed their clinical practice after several months, and no measures were put in place to make up for their lack of practice time. Second, some clinical frontline doctors were transferred to pandemic prevention and control teams, leading to a decrease in the number of clinical teachers (18). As each of the remaining clinical teachers was then put in charge of more students to make up for the shortage of clinical teachers, the teaching effect was bound to be affected (19). With the emergence of COVID-19 vaccines and vaccination, 66.5% of the medical students were glad to see that life was getting back to the old normal, which showed that most of the students were eager to return to normal life after experiencing the pandemic. Schools need to encourage their students to take part in the pandemic prevention and control training and work and to strive to cut off the COVID-19 transmission routes and to get back to the old normal as soon as possible.
A previous study found that the COVID-19 pandemic has had a negative psychological impact on post-graduate trainees (20). Among Chinese college students, 0.9% suffer from severe anxiety, and 2.7% have moderate anxiety symptoms during the outbreak of COVID-19 pandemic (21). We found that in spite of the pandemic, the post-graduates in all the academic departments and grades in our University are basically in good health. A high 78.41% of the students said that they were in good health, which shows that the pandemic prevention and control work in our University has yielded relatively satisfactory outcomes. COVID-19 has had little influence on the health status of the University's medical clinical post-graduates. This study also investigated the infection prevention measures that could be taken by clinical post-graduates. It was found that medical students are more conscious of their personal protection in the face of the pandemic. Only 3.98% of the students said that they had not taken any preventive measure during the pandemic, and the remaining students said that they had taken different protective measures against COVID-19 infection. Moreover, there were no significant differences in the prevention and control measures taken by the medical post-graduates by gender and academic major. The results showed that 91.48% of the medical post-graduates chose to strengthen their personal protection against COVID-19 and 86.34% chose to strengthen their personal hygiene. Previous studies have demonstrated that the hands are an important medium for virus transmission, and hand hygiene is thus the simplest and most cost-effective measure for reducing the occurrence of hospital infection (22). Hand hygiene is also listed in the guidelines issued by China to protect the public against COVID-19 as one of the important measures that can be taken to prevent COVID-19 infection (23). However, only 46.59% of the students chose to exercise more to improve their immunity and to reduce their risk of infection. Zhu et al. found that it is safe to exercise during the COVID-19 outbreak (24). Proper physical exercise is also a scientific protective measure to strengthen one's resistance. Our study results also showed that most of the students had a positive attitude toward the COVID-19 vaccine, and only 1.14% of them thought that the vaccine had no effect on the prevention of COVID-19 infection. The existing literature also confirmed that the vaccine used in China has good immunogenicity (25). In the follow-up pandemic prevention and control work, accelerating the maturity and popularization of the existing vaccines and increasing the COVID-19 vaccination will play a relatively positive role in combatting the COVID-19 pandemic. Thus, medical schools and hospitals can also strengthen their training programs on and investments in personal protection and personal hygiene for the medical post-graduates, encourage the medical post-graduates to actively engage in physical exercise, provide safe exercise spaces for them, and actively promote COVID-19 vaccination among them to reduce the impact of the pandemic on their clinical practice and to better protect them against COVID-19 infection.
COVID-19 is a new infectious respiratory disease. Due to its multiple transmission routes and strong contagion effect (25), the biggest worry of the medical post-graduates in this study was their COVID-19 infection due to their inadequate personal protection and the possibility of cross-infection in the hospital. The survey also found that 86.93% of the students hope that unified arrangement of pandemic prevention and control training mode can be achieved. There have been three major disease outbreaks in the 21st century: China's severe acute respiratory syndrome outbreak (26) in 2003, the Middle East respiratory syndrome (MERS) outbreak in 2012 (27), and the West African Ebola epidemic in 2014 (28). Thus, it is possible that every medical post-graduate student in clinical practice will face a new infectious-disease outbreak. Therefore, knowledge regarding pandemic prevention and control and the related training are necessary in hospitals and medical schools. It is also one of the most recognized forms of training for medical post-graduates. In recent years, with the advances in the field of medicine, the spectrum of infectious diseases has changed significantly; for instance, the incidence rates of plague, cholera, and encephalitis B have dropped significantly (29). The COVID-19 pandemic has shown the need to teach infectious-disease outbreak control as new infectious diseases may emerge at any time. Every clinical worker should thus be alert to the emergence of new infectious diseases. For the teaching of infectious-disease treatment and control for medical post-graduates, what is most important is to update the information in real time and to add the concept, types, characteristics, causes, and influencing factors of new infectious diseases to the medical syllabus on infectious diseases. Second, it is necessary to increase the exercises in coping with the outbreak of infectious diseases in the teaching of the said matter so that the students will be able to understand all the aspects of the prevention and control of infectious diseases through actual participation. Combined with the existing resident standardized training, hospitals can also increase the training contents related to infectious diseases and pandemic response.
In early 2020, the COVID-19 pandemic raged around the world (30, 31). Tens of thousands of Chinese medical staff rushed to Wuhan, China, to help treat the patients there, bravely facing the risk of infection and demonstrating the resolve to “respect life, save the dead, and heal the wounded” (32). As the reserve army of clinicians, medical students have the mission not only to safeguard human health but also to inherit the spirit of medical practice. Therefore, besides medical skills, moral education should be placed at the core of medical education (32). Before medical students start their clinical practice, teachers should make them feel the suffering of patients at close range, experience the race against death, and actively cultivate their professionalism and professional identity. The results of this survey showed that most of the medical post-graduates in this study were not willing to reduce their risk of contracting COVID-19 by reducing their contact with patients. The medical education curriculum can regard pandemics as a teaching material and can mandate the discussion of these in class, along with medical skills and medical ethics education (33).
Conclusions
In conclusion, our study found that the COVID-19 pandemic had an impact on the medical post-graduates' clinical practice, and affected their cognitive attitudes and behaviors. There were no statistically differences in the personal protection by academic major and gender. Medical schools and hospitals should therefore increase their targeted measures against the medical post-graduates' COVID-19 infection, offer psychological counseling to them to lighten their psychological burden, and strive to reduce the impact of outbreaks on their clinical practice.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University, and conducted in accordance with the Declaration of Helsinki principles. Informed consent from all participants was included at the start of the questionnaire, and all participants voluntarily participated or withdrew from the questionnaire. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
LF and JS: conceptualization and formal analysis, funding acquisition, and writing—review and editing. ZX: data curation. LF, ZX, and JS: methodology. LF and ZX: writing—original draft. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Natural Science Foundation of China (Nos. 81870648, 82070949, and 82000886) and Natural Science Foundation of Zhejiang Province (No. LQ20H120011).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are greatly indebted to all subjects who were enrolled in our study.
References
1. World Health Organization. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV) [EB/OL]. (2020). Available online at: https://www.scirp.org/reference/referencespapers.aspx?referenceid=2794385 (accessed March, 08, 2021).
2. Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, et al. Impact of the COVID-19 pandemic on medical education: medical students' knowledge, attitudes, and practices regarding electronic learning. PLoS ONE. (2020) 15:e0242905. doi: 10.1371/journal.pone.0242905
3. Sklar DP. COVID-19: lessons from the disaster that can improve health professions education. Acad Med. (2020) 95:1631–3. doi: 10.1097/ACM.0000000000003547
4. Calhoun KE, Yale LA, Whipple ME, Allen SM, Wood DE, Tatum RP. The impact of COVID-19 on medi- cal student surgical education: implementing extreme pandemic response measures in a widely distrib- uted surgical clerkship experience. Am J Surg. (2020) 220:44–7. doi: 10.1016/j.amjsurg.2020.04.024
5. Akers A, Blough C, Iyer MS. COVID-19 implications on clinical clerkships and the residency applica- tion process for medical students. Cureus. (2020) 12:e7800. doi: 10.7759/cureus.7800
6. Khasawneh AI, Humeidan AA, Alsulaiman JW, Bloukh S, Ramadan M, Al-Shatanawi TN, et al. Medical students and COVID-19: knowledge, attitudes, and precautionary measures. A descriptive study from Jordan. Front Public Health. (2020) 8:253. doi: 10.3389/fpubh.2020.00253
7. Chang J, Yuan Y, Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao. (2020) 40:171–6. doi: 10.12122/j.issn.1673-4254.2020.02.06
8. Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect. (2020) 148:e98. doi: 10.1017/S0950268820001107
9. Hall AK, Nousiainen MT, Campisi P, Dagnone JD, Frank JR, Kroeker KI, et al. Training disrupted: practical tips for supporting competency-based medical education during the COVID-19 pandemic. Med Teach. (2020) 42:756–761. doi: 10.1080/0142159X.2020.1766669
10. Orsini C, Rodrigues V. Supporting motivation in teams working remotely: the role of basic psychological needs. Med Teach. (2020) 42:828–9. doi: 10.1080/0142159X.2020.1758305
11. Jervis CG, Brown LR. The prospects of sitting 'end of year' open book exams in the light of COVID-19: a medical student's perspec- tive. Med Teach. (2020) 42:830–1. doi: 10.1080/0142159X.2020.1766668
12. Kapadia SJ. Perspectives of a 2nd-year medical student on ‘Students as Partners’ in higher education – what are the benefits, and how can we manage the power dynamics? Med Teach. (2021) 43:478–9. doi: 10.1080/0142159X.2020.1779922
13. Tabari P, Amini M, Moosavi M. Lessons learned from COVID-19 epidemic in Iran: the role of medical education. Med Teach. (2020) 42:833. doi: 10.1080/0142159X.2020.1754376
14. Tsang HF, Chan LWC, Cho WCS, Yu ACS, Yim AKY, Chan AKC, et al. An update on COVID-19 pandemic: the epidemiology, pathogenesis, prevention and treatment strategies. Expert Rev Anti Infect Ther. (2021) 19:877–88. doi: 10.1080/14787210.2021.1863146
15. Lee YM, Park KD, Seo JH. New paradigm of pediatric clinical clerkship during the epidemic of COVID-19. J Korean Med Sci. (2020) 35:e344. doi: 10.3346/jkms.2020.35.e344
16. Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. (2020) 369:m1642. doi: 10.1136/bmj.m1642
17. Rose S. Medical student education in the time of COVID-19. JAMA. (2020) 323:2131–2. doi: 10.1001/jama.2020.5227
18. Tariq EF, Sah PK, Malik A. The plight of COVID-19 pandemic on medical students and residency applicants. Ann Med Surg. (2020) 60:1–4. doi: 10.1016/j.amsu.2020.10.010
19. Ferrel MN, Ryan JJ. The impact of COVID-19 on medical education. Cureus. (2020) 12:e7492. doi: 10.7759/cureus.7492
20. Imran N, Masood HMU, Ayub M, Gondal KM. Psychological impact of COVID-19 pandemic on postgraduate trainees: a cross-sectional survey. Postgrad Med J. (2020) 97:632–7. doi: 10.1136/postgradmedj-2020-138364
21. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epi- demic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
22. De Angelis G, Lohmeyer FM, Grossi A, Posteraro B, Sanguinetti M. Hand hygiene and facemask use to prevent droplet-transmitted viral diseases during air travel: a systematic literature review. BMC Public Health. (2021) 21:760. doi: 10.1186/s12889-021-10814-9
23. Chinese Center for Disease Control and Prevention. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2020) 41:145–51. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003
24. Zhu WM. Should, and how can, exercise be done during a coronavirus outbreak? An interview with Dr. Jeffrey A. Woods. J Sport Health Sci. (2020) 9:105–7. doi: 10.1016/j.jshs.2020.01.005
25. Gao Q, Bao L, Mao H, Wang L, Xu K, Yang M, et al. Development of an inactivated vaccine candidate for SARS-CoV-2. Science. (2020) 369:77–81. doi: 10.1126/science.abc1932
26. Chowell G, Abdirizak F, Lee S, Lee J, Jung E, Nishiura H, et al. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. (2015) 13:210–22. doi: 10.1186/s12916-015-0450-0
27. Kucharski AJ, Althaus CL. The role of superspreading in Middle East respiratory syndrome coronavirus (MERS-CoV) transmission. Euro Surveill. (2015) 20:14–8. doi: 10.2807/1560-7917.ES2015.20.25.21167
28. Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. (2013) 382:694–9. doi: 10.1016/S0140-6736(13)61492-0
29. Liu Q, Xu W, Lu S, Jiang J, Zhou J, Shao Z, et al. Landscape of emerging and re-emerging infectious diseases in China: impact of ecology, climate, and behavior. Front Med. (2018) 12:3–22. doi: 10.1007/s11684-017-0605-9
30. Lancet T. COVID-19: too little, too late? Lancet. (2020) 395:755. doi: 10.1016/S0140-6736(20)30522-5
31. Day M. Covid-19: surge in cases in Italy and South Korea makes pandemic look more likely. BMJ. (2020) 368:m751. doi: 10.1136/bmj.m751
32. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–1720. doi: 10.1056/NEJMc2005203
Keywords: COVID-19 pandemic, medical post-graduates, clinical practice, attitudes and behaviors, investigation
Citation: Feng L, Xie Z and Shen J (2021) Investigation of the Cognitive Attitudes and Behaviors of Medical Post-graduates in Clinical Practice During the COVID-19 Pandemic in China. Front. Public Health 9:755163. doi: 10.3389/fpubh.2021.755163
Received: 08 August 2021; Accepted: 12 October 2021;
Published: 03 November 2021.
Edited by:
William Ka Fai Tse, Kyushu University, JapanCopyright © 2021 Feng, Xie and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junhui Shen, MTM0NDk0QHpqdS5lZHUuY24=
 Lei Feng
Lei Feng Zefeng Xie
Zefeng Xie Junhui Shen
Junhui Shen