- Faculty of Pharmacy, University of Belgrade, Belgrade, Serbia
Background: Patients with chronic diseases, like diabetes need to continuously perform tasks associated with self-management especially with medications they use. It is shown that the patients with diabetes with limited HL and PTHL cannot read medication labels correctly, may misuse their medications, spend much more on therapy and generally have difficulties in understanding printed care instructions and perceiving health advice and warnings. There has been an increasing demand for valid and reliable instruments for HL and PTHL assessment in this population. This review aims to search and critically discuss instruments used to assess HL and PTHL in people with type 2 diabetes and propose their use in different settings.
Methods: Authors conducted a comprehensive, electronic search of original studies using a structured approach of the Scopus and PubMed databases, during November and the first 2 weeks of December 2020 to find relevant papers. The review was conducted in accordance with the Cochrane guidelines and the reporting was based on the PRISMA-ScR. The comparison of instruments was made by utilizing a comparison model related to their structure, measurement scope, range, psychometric properties, validation, strengths, and limitations.
Results: The final number of included studies was 24, extracting the following identified instruments: Korean Functional Test HL, NVS, FCCHL, HLS-EU-47, TOFLHA, S-TOFHLA, REALM-R, 3-brief SQ, REALM, HLQ and DNT-15. In all, FCCHL and 3-brief SQ are shown with the broadest measurement scopes. They are quick, easy, and inexpensive for administration. FCCHL can be considered the most useful and comprehensive instrument to screen for inadequate HL. The limitation is that the English version is not validated. Three-brief SQ has many advantages in comparison to other instruments, including that it is less likely to cause anxiety and shame. These instruments can be considered the best for measuring functional HL in patients with diabetes mellitus type 2 and other chronic diseases. PTHL instruments (REALM and DNT-15) did not find the best application in this population.
Conclusions: The future research should be directed in validation of the FCCHL in English and establishing of the structural validity of this questionnaire. Developing a specific PTHL questionnaire for this population will be of great help in management of their disease.
Introduction
The main goal of today's healthcare system is to promote and maintain good health and at the same time enable people to take care of their health. People are also expected to be more responsible for their health and participate more in decision-making related to their health (1–3). When we talk about responsibility for our health, we must consider different assumptions. Efforts should be focused on a person's ability to cope and take responsibility for their health (3). The Patients' Rights Act from 1999 states that the manner of participation in healthcare decisions should be adapted to each person's ability to give and receive health information. These abilities are related to health literacy (HL) (4).
To understand and use health information to make health decisions, adequate HL is needed (4). In a report by the World Health Organization (WHO), HL is one of the most important determinants of health. HL can be considered necessary to control and monitor one's health (5). Several studies have shown that most people have limited HL (6–12). Also, people with low HL are more likely to be with poorer health, more prone to complications, and have a higher mortality rate than people with high HL (5).
Healthcare professionals should consider that individuals possess different levels of HL. Therefore, knowledge about HL of people is necessary to adapt better health professionals' communication with different target groups, which would make the information more beneficial for the individual by enabling them to participate in health decisions and take responsibility for their health (13).
Optimizing health communication can prevent misunderstandings and other complications, thus the quality of care and patient safety would be improved (13). In order to meet expectations such as increased participation and responsibility for one's health, it is necessary to consider HL in individuals and the general population. The purpose of today's public health policy is to create conditions for educating people to be able to take control of their health and control it (3). Therefore, measuring HL in different populations would provide essential knowledge that would be used to improve health communication, and thus the ability of individuals to control their health. However, the validity and reliability of individual HL instruments have not been adequately established (14) and only a few HL instruments were validated using modern test theory, such as Rasch modeling (15, 16).
Health Literacy
Adequate health literacy is crucial for patients to make optimal choices for their health and medications management. Additionally, successful health communication presupposes certain levels of competence of both the healthcare professional and the patients and is adapted to the HL of the individuals (5).
“HL” as a recognized term came into use around 1974, but only became a [Medical Subject Headings (MeSH)] term in MEDLINE in 2006. A systematic review of Sørensen et al. (17) discovered 17 definitions and 12 conceptual models of HL. Based on all the offered, one overall definition was obtained, which reads: “HL is linked to literacy and entails people's knowledge, motivation and competencies to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course.” There is currently no consensus on defining HL, which means that different approaches to this term are used in various research environments (17–20). An additional concept of understanding becomes a problem when it comes to assessing and measuring HL and then comparing these results between different studies (16). The presence of different definitions is probably due to the fact that the concept has been developed in different parts of the world, with varying abilities and skills considered necessary to deal with health information in each specific context (21).
In the twentieth century, reading and writing were sufficient to use information obtained from health professionals. However, with increasing expectations of active participation in health decisions, increasing responsibility for one's health, and digital development in health information, additional skills are needed to handle health information. First, the need for reading has increased, and the skills to apply and critically evaluate health information from various sources are essential. HL combines a set of skills or abilities, while on the other hand it depends on the requirements to which the individual is exposed. The impact of technological development has also increased, which will affect the definition and understanding of HL in the future (22).
Pharmacotherapy Literacy (PTHL)
Patients with chronic diseases need to continuously perform tasks associated with self-care and self-management of their medications. When taking medicines, they constantly need abilities related to various domains of HL, so HL brings together many concepts that are associated with patient's pharmacotherapy. Whether they rely on information in printed materials or verbal instruction patients with chronic conditions need to have adequate HL related to medications as critical for managing their conditions. Due to the complexity of the various procedures required for the adequate use of medications, the concept of PTHL was introduced.
King and colleagues, in consultation with the academy and pharmacists, formulated PTHL as: “An individual's capacity to obtain, evaluate, calculate, and comprehend basic information about pharmacotherapy and pharmacy related services necessary to make appropriate medication-related decisions, regardless of the mode of content delivery (e.g., written, oral, visual images and symbols)” (23). This definition was updated by adding to reduce thereby the risk of poor pharmacotherapy outcomes (24).
HL and PTHL in Persons With Type 2 Diabetes Mellitus
Diabetes is one of the most common chronic non-communicable diseases and is a major public health problem. In 2019, the International Diabetes Federation estimated that 463 million adults worldwide have diabetes and that this number is expected to increase to 700 million by 2,045. The cause of this disease is multifactorial, but it is associated with unhealthy lifestyles such as physical inactivity and poor diet. It is assumed that between 30 and 80% of people with type 2 diabetes are still undiagnosed. Complications such as diabetic nephropathy and neuropathy may occur at a later diagnosis of disease (25). Despite advances in therapy and the availability of clinical practice guides, only 30% of patients manage to achieve the target values of glycemia, cholesterol and blood pressure. The fact is that patients perform 95% of diabetes care on their own (26).
Type 2 diabetes is more common than type 1, so 90% of all diabetes is type 2 diabetes. It most often occurs in middle age and in the elderly. It is closely related to lifestyle and health habits, with being overweight and obese being risk factors. Hereditary factors can also influence the risk of developing this disease. Therapy includes weight loss, diet and therapy with drugs that lower blood glucose levels. Affected people are advised to give up cigarettes and reduce alcohol intake to prevent the appearance of cardiovascular diseases. Living with this disease requires changes in health behavior, self-control, and a lot of care (27–29). Since living with type 2 diabetes requires a lot from people with the disease, these persons must be informed about therapy, diet and other health behaviours, which require adequate HL and PTHL. Several international studies have shown that reading and understanding the guidelines for modern diabetes medications, applying appropriate dietary restrictions, and gaining insight into the physiological processes involved in the disease can be a major challenge for an individual (30, 31). The performing of diabetes self-management tasks frequently involves abilities, such as taking medications at the right time, interpreting blood glucose levels and calculating insulin doses.
A recent review of HL and health outcomes in patients with type 2 diabetes concludes that there is strong evidence to suggest a positive correlation between HL and diabetes knowledge (32). It is also considered that there is sufficient evidence to support a link between HL and self-care (33). On the other hand, the evidence of a link between HL and clinical indicators was inconsistent (34).
Some primary studies that looked at the level of HL in patients with type 2 diabetes found that a small number of these patients had adequate levels of HL (35–39).
Patients with diabetes and limited HL and PTHL often cannot read drug medication labels correctly, may misuse their medication, do not understand the meaning of consent forms, and generally have difficulty understanding printed care instructions and reading health advice and warnings (40–43). For this reason, is very important to assess their PTHL and in case of needs perform adequate training in order to improve control of their disease and pharmacotherapy management.
These patients also have poorer communication with doctors and participate less in making health decisions (4). Patients who are diagnosed have to make health decisions daily and must also perform complex self-care activities to keep the disease under control. Interventions in upgrading HL education and intensive diabetes-related education have shown good results in patients with limited HL to improve diabetes outcomes (44, 45). People with type 2 diabetes should undergo diabetes education programs at the time of diagnosis and then once a year. This education aims to enable individuals to participate in informed decision-making and disease control, all with the aim of better outcomes in treatment of this disease, improvement of glycemic control, prevention of complications and comorbidities, and improvement of quality of life (46). Education for diabetics should be evidence-based, have specific goals, and be tailored to the needs of individuals. However, the effectiveness of this education depends on individuals, i.e., characteristics such as age, gender, ethnicity, level of HL, ability to take care of themselves, all of which should be taken into account when planning and implementing this type of education (27, 47). In this way, they will be able to understand and use the information they receive to maintain health and control diabetes in everyday life (47).
Instrument Development
In the past 25 years, numerous instruments have been developed to measure HL and PTHL in various contexts (14, 24, 48). These instruments significantly differ in structure, measurement, range, and psychometric properties. The diversity of instruments has led to inconsistencies in measurement with the complexity of interpreting the results and choosing suitable instruments for new studies. Several studies have examined the variation through the range of the most used HL instruments (49, 50). Such variations can come from the fact that the instruments measure different conceptual dimensions of HL. However, it may be difficult for health professionals or researchers to choose the best instrument when they are unfamiliar with measurement properties. Another very important consideration in selecting a HL instrument is its mode of administration. In a subjective instrument, individuals self-report their perceived levels of literacy skills, such as using Likert scales. In contrast, an objective instrument is the interviewer-administrated instrument and assesses the ability to process information by asking respondents to answer specific questions, such as about the time to take the next medication. A subjective instrument requires less cognitive effort in responding to questions, whereas an objective instrument assesses health numeracy more accurately. A self-administrated instrument can be more practical in a very busy clinical settings, than interviewer-administered instrument. Sometimes, the interviewer-administrated instrument may result in discomfort or embarrassment for patients who have a low HL.
Although the instruments were used in several populations, due to the complexity of the tasks and skills that people with type 2 diabetes require, their usefulness and applicability for this population remain challenging. With the growing interest in this construct, there has been an increasing demand for valid and reliable instruments for estimating HL and PTHL.
A systematic review of measurement properties has been designed for providing a comprehensive overview of the available instruments and identifying the best currently available instrument for general population (51). In the previous reviews of HL instruments methodological limitations were identified, such as being descriptive rather than systematic reviews, or lacking quality assessment or data synthesis (14, 52, 53). To address these limitations, a scoping review was conducted to systematically collect the literacy instruments used in people with type 2 diabetes and meet needs for understanding the characteristics, scope of measurements, and their applicability in this population.
Methodological Study Design
Aim
This study aims to analyze instruments used in patients with type 2 diabetes mellites for measuring HL and PTHL, in relation to their characteristics (measurement scope, structure, domains, method of scoring), validation, strengths, limitations and accordingly to propose applicability of these instruments in clinical and research settings. This work can be useful as an inventory for researchers and practitioners who are seeking to identify validated measurement instruments in patients with type 2 diabetes mellitus and other chronic diseases that are fitting the best for their research and practice.
Materials and Methods
Authors built a search strategy by using the PICOS questionnaire. During November and the first 2 weeks of December 2020, a systematic search of the Scopus and PubMed databases was performed in search of peer-reviewed literature of patients with type 2 diabetes mellitus. The protocol of this systematic review (including the article identification strategy and data collection form, etc.) mainly referred to the Cochrane Handbook for Systematic Reviews of Interventions (54) and the reporting of this systematic review was based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (55).
Search Strategy
The keywords used were: “medication literacy,” “measurement tool,” “assessment,” “patient,” “chronic diseases” and “healthcare system.” A search of the terms above found that the number of articles specifically mentioning PTHL was limited, so the search was extended to articles mentioning “health literacy” combined with patients with type 2 diabetes.
In the articles obtained by this search, the references were manually checked to identify additional articles of importance for the work.
Study Screening and Selection
All original articles in English are taken into consideration, which meet the below criteria. Duplicates have been excluded. The evaluation of studies regarding the inclusion and exclusion criteria was performed by a pair of independent reviewers (ML and DK): (1) review of titles and abstracts of articles related to the topic (2) review of complete articles was done which examined the HL and PTHL of patients with type 2 diabetes and had the original results of the health and pharmacotherapeutic literacy of patients with type 2 diabetes mellitus conducted through appropriate questionnaires. After cross-checking, a third reviewer (NBS) resolved cases of disagreement.
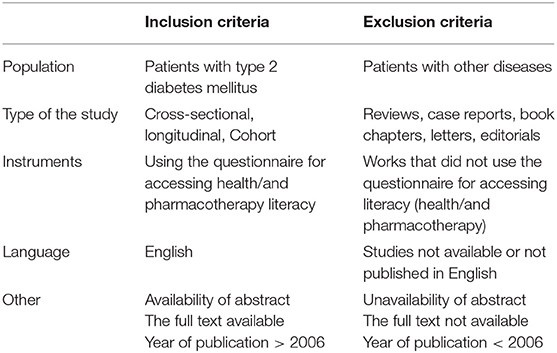
Inclusion and Exclusion Criteria
Peer-reviewed papers with cross-sectional studies, longitudinal studies and cohorts were included if they were: published between the period 2006–2021, written in English, involved patients with type 2 diabetes and papers in which HL and PTHL were examined in patients with type 2 diabetes.
The exclusion criteria were: reviews, case reports, book chapters, letters, editorials, studies that did not address HL and PTHL among patients with type 2 diabetes, studies that did not use the questionnaire for assessing literacy, studies not available or not published in English.
The inclusion and exclusion criteria are presented in Table 1.
Data Extraction and Synthesis of Results
Data extraction was performed independently by the authors. They extracted different characteristics from each publication, such as (i) publication information: author and year; (ii) study characteristics: country, setting, population, number of participants and results in terms of HL and PTHL (iii) HL and PTHL instruments: name, dimensions, number of items, purpose, target population, administration mode, validation process, scoring, cut-off points, strengths and limitations.
The studies were grouped according to instruments used for the measurement of literacy: HL and PTHL. A descriptive synthesis of the identified studies was performed, and variables described in the synthesis include number of participants, setting, country, population and results. Formal analysis of the results was a descriptive synthesis of the identified instruments from selected studies to determine instruments key characteristics including identifying domains, length of tool (number of questions/items/domains), time for completion, format, and psychometric properties.
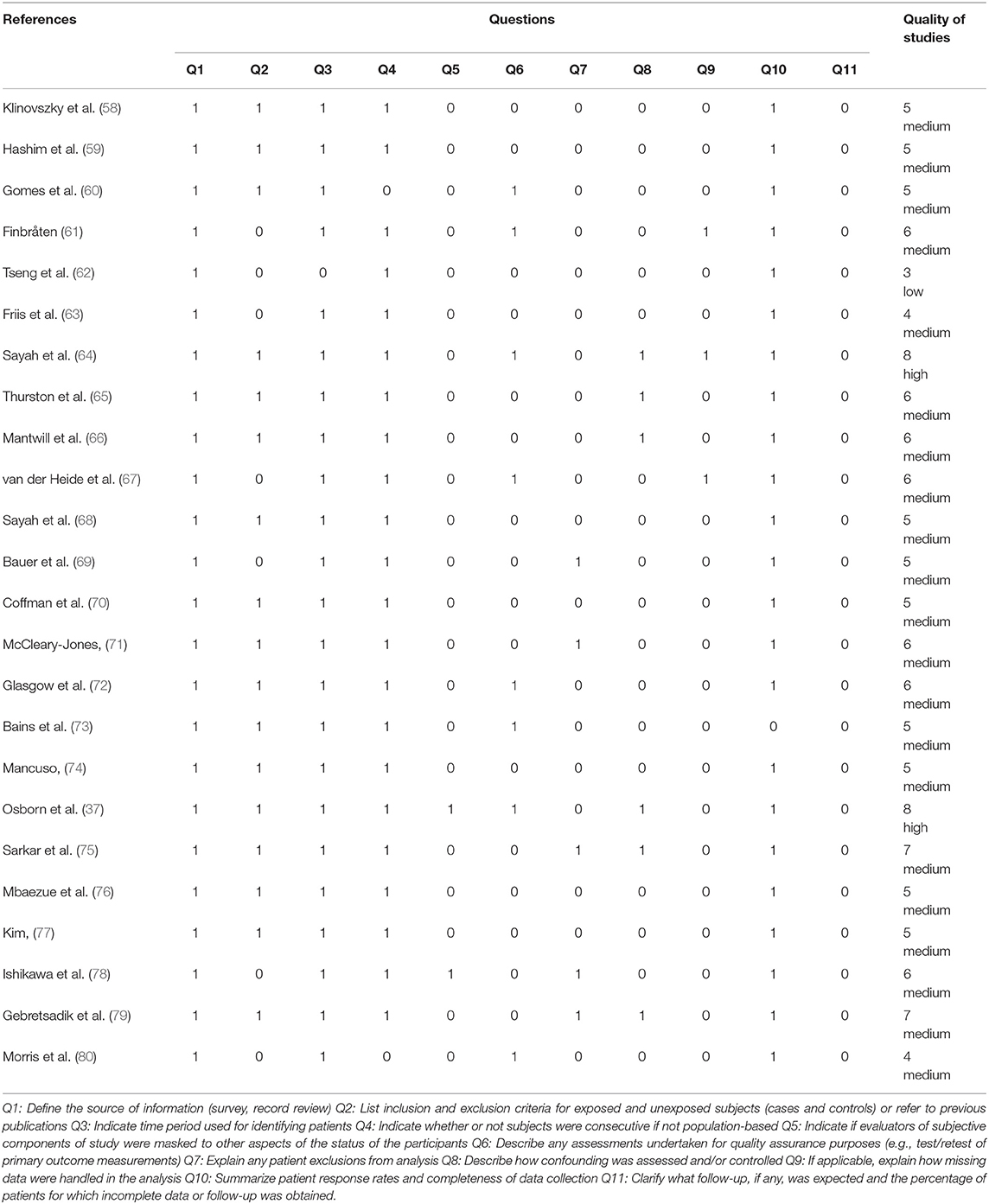
Critical Appraisal
At the time of our research, there were no accepted quality assessment instruments for cross-sectional studies (56), authors decided to choose a relatively widely used scale, the Agency for Healthcare Research and Quality scale (AHRQ scale) with 11 items, each of which was answered with “yes,” “no” and “unclear.” Two researchers (DK and ML) independently evaluated the quality of the included articles using the AHRQ scale. Any disagreements after cross-checking were resolved by discussions between the two researchers with the final decisions of the third researcher (NBS). If the answer was “no,” “unclear” or “not applicable,” the item was given a score of “0”; if the answer was “yes,” the item was scored as “1.” The quality assessments of the articles were classified as follows: low quality = 0–3, medium quality = 4–7, high quality = 8–11 (57).
The quality assessment of the identified studies is presented in Table 2. The majority of them were classified with medium quality and one fulfilled the criteria for high.
Results
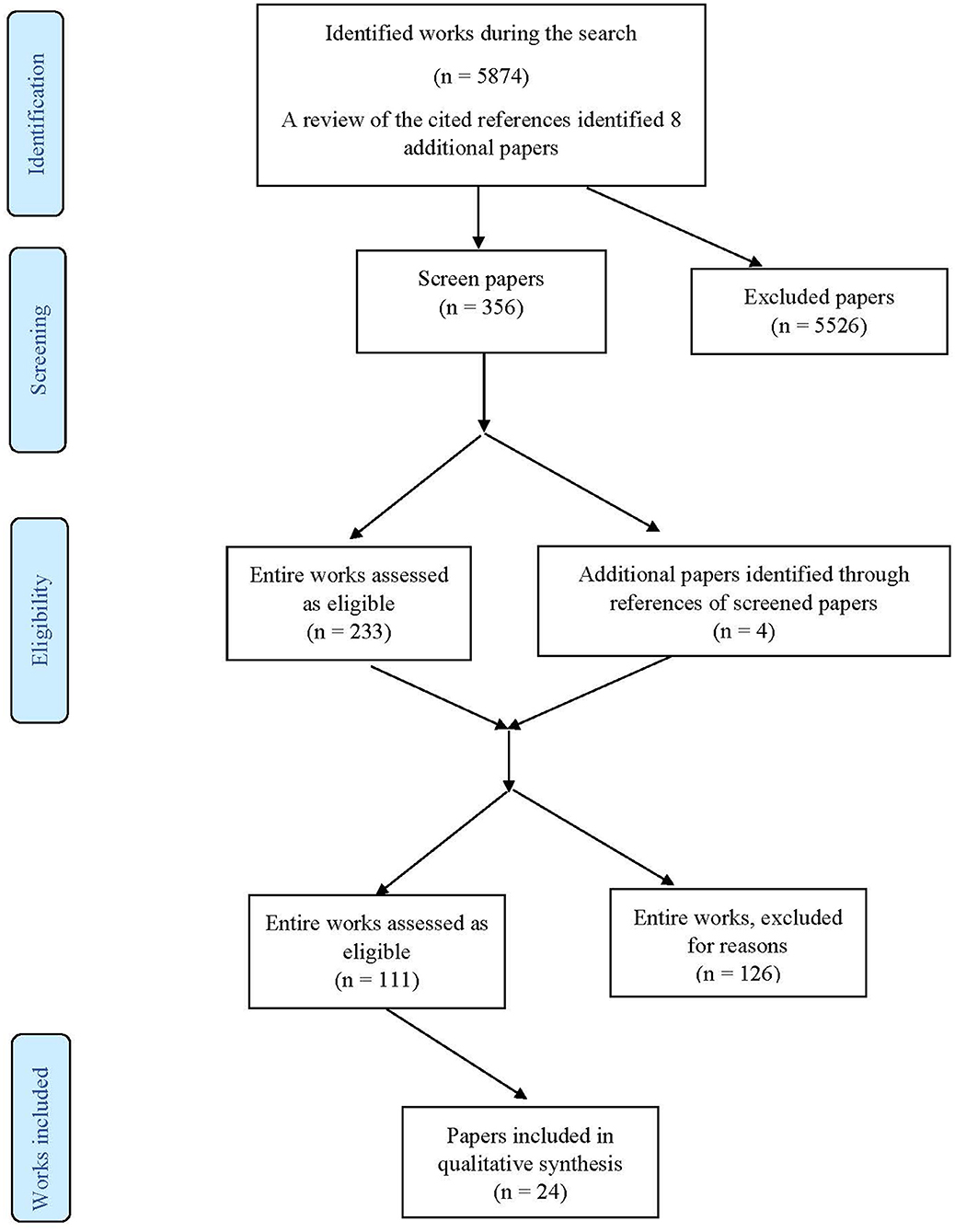
Study Screening and Selection
The PRISMA flow chart in Figure 1 summarises the results of the search process. 1. A search obtained 5,874 potentially relevant studies, while 8 were found by reference review. A cursory review of the content of the papers left 356 papers for further evaluation. Further exclusion (after reading the abstracts and methodology) was based on the principle of excluding papers that mentioned the instrument for assessing HL and PTHL, but without analyzing its structure, and excluding papers that are duplicates (same author, same instrument) left 111 articles for full reading, of which the final number of included studies was 24.
The comparison method was used to compare the instrument in terms of their structure (number and type of questions), the way of reporting, version, purpose, place where they were developed, target population, the person who developed it, year of publication, scoring, heath literacy domains, time and way for administration, measurement scope, validation, strengths, and limitations.
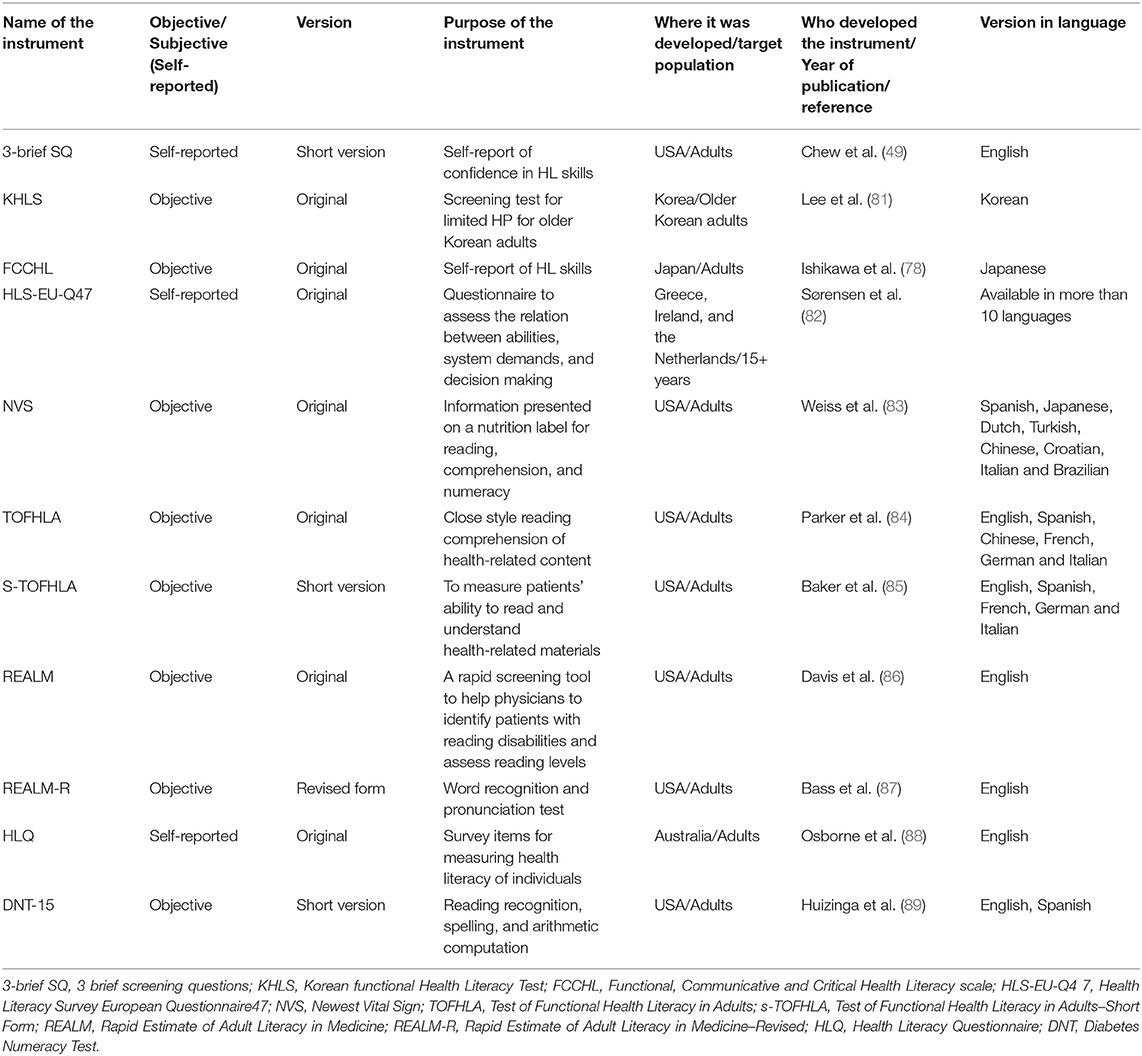
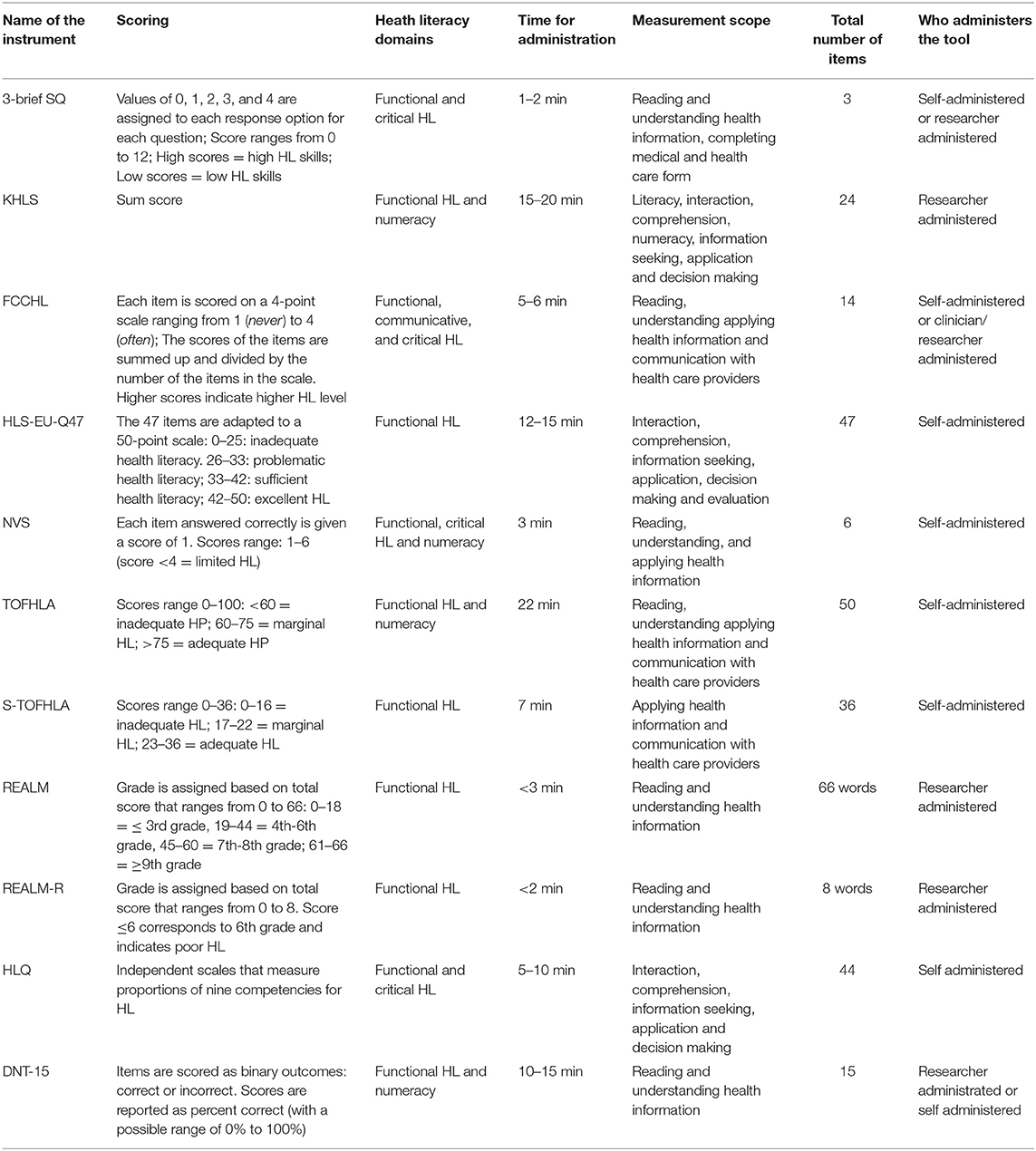
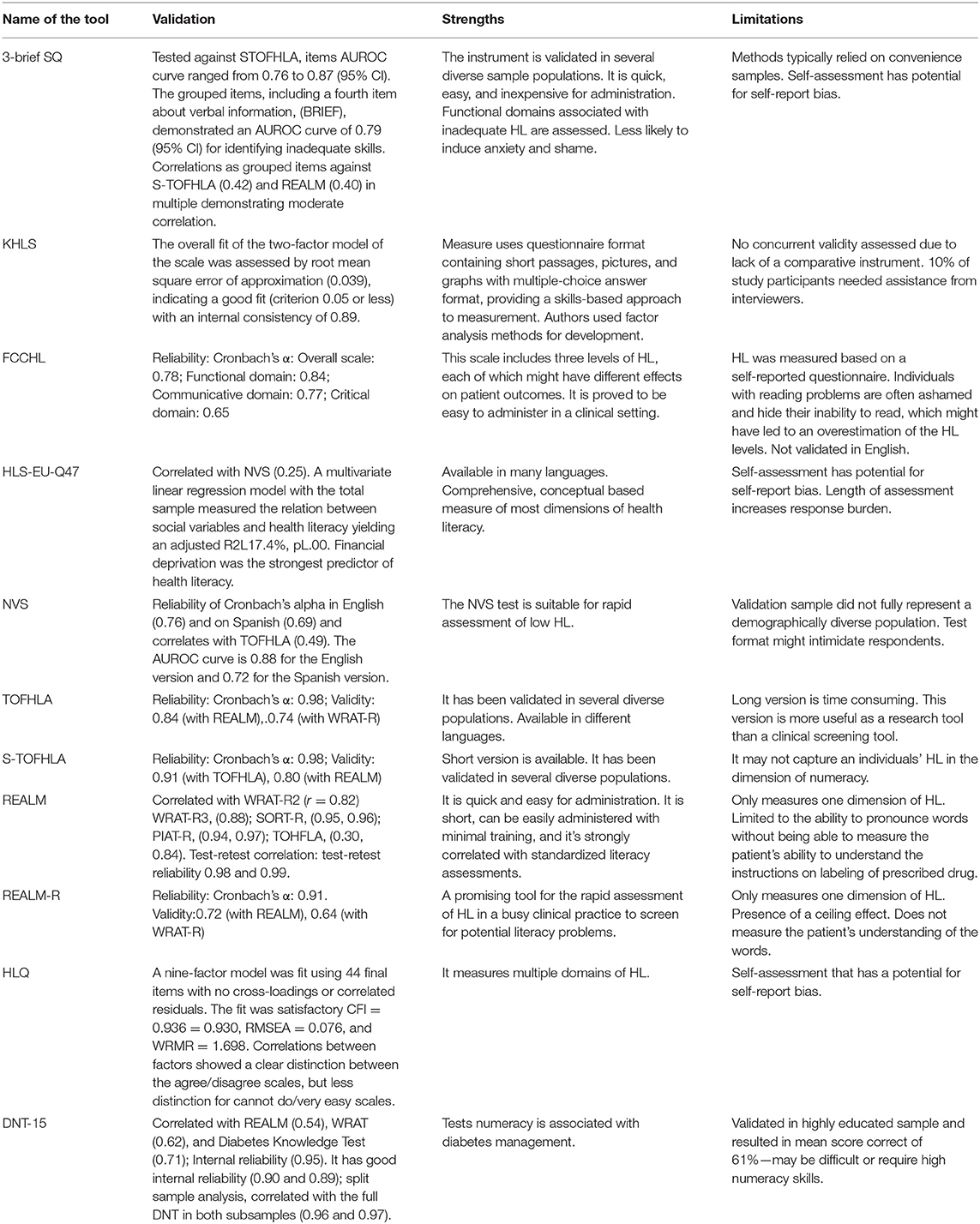
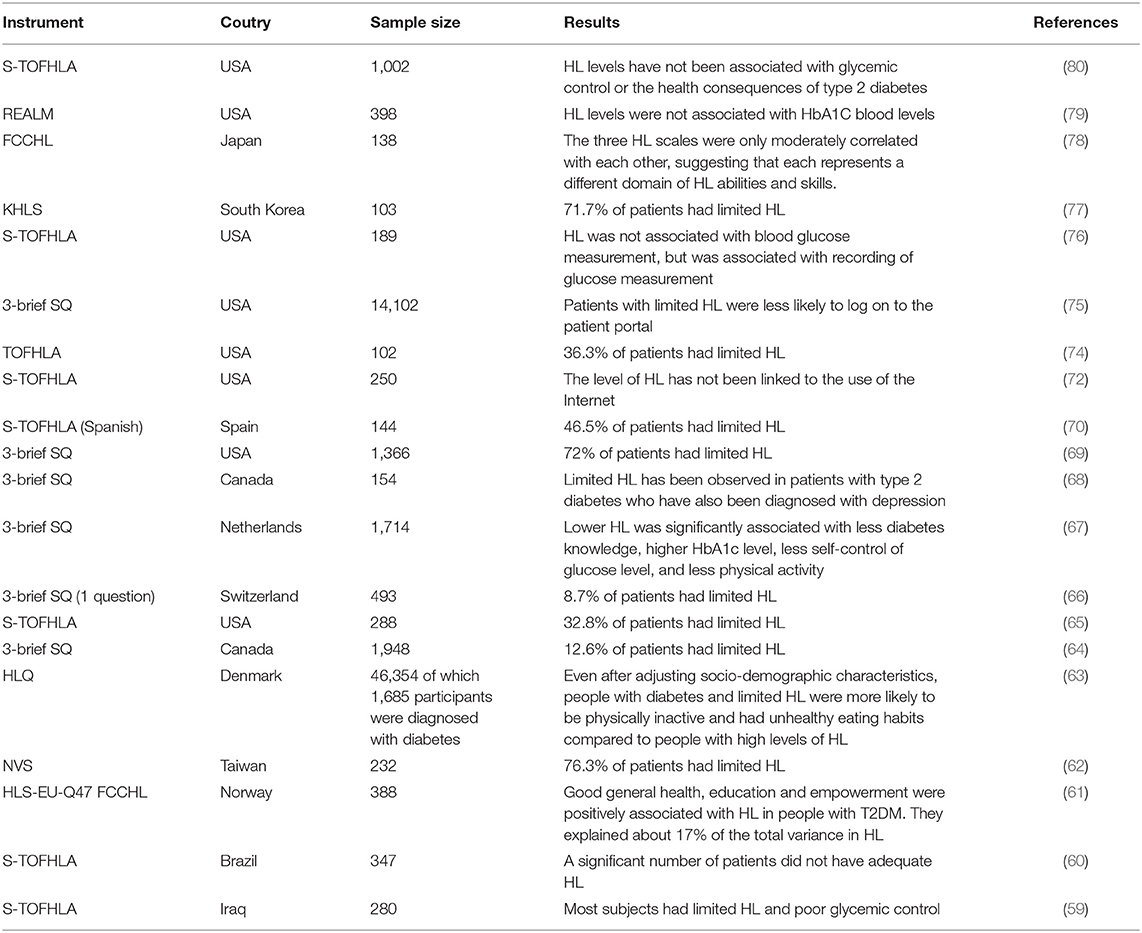
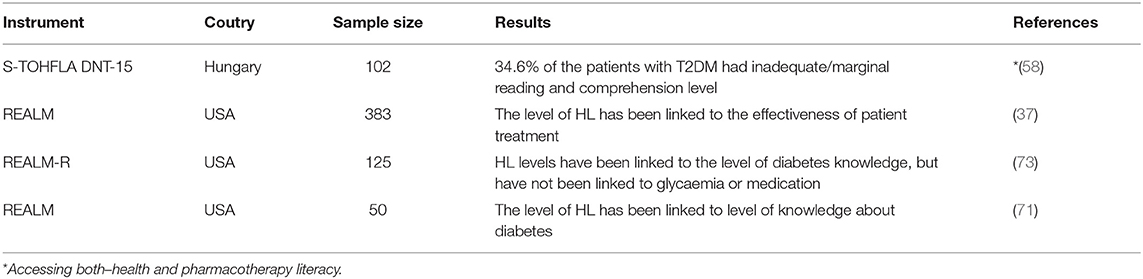
A thorough analysis has been presented in the Tables 3–5. Tables 3, 4 present the instruments used in the studies to assess HL and PHTL, their basic characteristics: domains, methods of assignment, structure and method of scoring. Table 5 shows the psychometric characteristics of the instruments, strengths and limitations.
Instrument Characteristics
The identified instruments used for assessing the level of HL and PTHL in extracted works are the following: Korean Functional Test HL (1 study), Newest Vital Sign, NVS (1 study), Functional, Communicative and Critical Health Literacy scale, FCCHL (1 study), Health Literacy Survey European Questionnaire 47, HLS-EU-47 (1 study), Test of Functional Health Literacy in Adults, TOFLHA (1 study), Test of Functional Health Literacy in Adults–Short Form, S-TOFHLA (8 studies), Rapid Estimate of Adult Literacy in Medicine–Revised, REALM-R (1 study), 3 brief screening questions, 3-brief SQ (6 studies), Rapid Estimate of Adult Literacy in Medicine, REALM (3 studies), Health Literacy Questionnaire, HLQ (1 study) and Diabetes Numeracy Test 15, DNT-15 (1 study) (37, 58–80). There are considerable differences found in their structure, number of items, administration time, available languages, type of administration, scoring system, measurement scope and properties, implicating their use in different settings.
The most used measures of HL in patients with type 2 diabetes mellitus were S-TOFHLA, then 3-brief SQ, REALM and HLS-EU-47. The S-TOFHLA, TOFHLA and REALM have been validated in different populations and are used in validation studies for 3-brief SQ and NVS. They are considered as a gold standard in validation studies. However, 3-brief SQ and NVS have a broader measurement scope and better properties, which put them in a better position for use in future validation studies. S-TOFHLA, REALM and HLS-EU-47 are not practical in busy clinical settings and REALM requires researcher participation. While the most used instruments, S-TOFHLA and REALM, measure only the functional domain of HL, the others 3-brief SQ, and HLQ address functional and critical HL, and DNT-15, KHLS and TOFHLA functional HL and numeracy. The only one for examination of all three levels of HL individually, their mutual correlation and different effects on patient is FCCHL.
Validation, Strengths, and Limitations
NVS - Good reliability and convergent validity with well-validated and commonly used measures of HL such as the TOFHLA. Strengths are related to its suitability for rapid assessment of low HL. Test format might intimidate respondents.
FCCHL - Strong positive evidence for its content and structural validity and moderate positive evidence for internal consistency. This scale includes three levels of HL, each of which might have different effects on patient outcomes. It is proved to be easy to administer in a clinical setting. The scale is not validated in English.
Three-brief SQ - Positive evidence for the criterion validity of the 3-SQ with the S-TOFHLA (36 items) and limited negative evidence for its hypothesis testing validity and internal consistency. Instrument is validated in several diverse sample populations. It is quick, easy, and inexpensive for administration. Limitation is related to self-assessment and potential for self-report bias.
HLS-EU-47 - High levels of internal consistency reliability. It is available in many languages, length of assessment increases response burden.
S-TOFHLA - Demonstrated evidence for the internal consistency due to there being no evidence of structural validity. It has been validated in several diverse populations. Lack of this instrument is that it may not capture an individuals' HL in the dimension of numeracy.
REALM - Found to have a high test-retest reliability of 0.99. It is assessed by healthcare professionals and was found to have good face validity; however, it lacks in construct validity. It is quick and easy for administration, limited to the ability to pronounce words without being able to measure the patient's ability to understand the instructions on labelling of prescribed drug.
HLQ - Positive moderate evidence for its content validity and internal consistency and unknown evidence for structural validity. Strength is that measures multiple domains of HL, but due to self-assessment has a potential for self-report bias.
DNT - Moderate evidence for its content validity and internal consistency and limited positive evidence for structural validity. This is test numeracy that is associated with diabetes management. Limitation is that can be difficult or require high numeracy skills (49, 78, 81–89).
Health Literacy and Pharmacotherapy Literacy
Preliminary data in relation to HL and PTHL were extracted from the studies included in the qualitative synthesis and summarized in Table 6 (for HL) and Table 7 (for PTHL).
In the research period most of the studies were published in the period from 2006 to 2021 (37, 58–80). The largest number of studies was conducted in the United States (11 studies) and Canada (2 studies). In contrast, in South Korea, Japan, Switzerland, Taiwan, Spain, Norway, Brazil, Denmark, Iraq, Netherlands and Hungary, one study was performed. Cross-sectional studies make up the majority (20 studies), while three are longitudinal and one is a cohort study. The sample size ranged from at least 50 to 46,354 subjects and are adults over the age of (37, 58–80).
In six studies, limited HL was observed in <50% of subjects, and in five studies, more than 50% of subjects had limited HL. HL levels have been linked to diabetes knowledge and treatment efficacy, while HbA1C concentrations, Internet use, glycemic control, and health consequences have not been linked to HL levels (37, 58–80). One study found an increased prevalence of people with limited HL who were diagnosed with depression (67), while another study found that people with limited HL were more likely to eat unhealthily and had reduced physical activity compared to people with high HL (62).
Discussion
This work presents the most comprehensive inventory of HL and PTHL measures in patients with type 2 diabetes mellites to date. There are limited number of works assessed the instruments that measure HL in patients with type 2 diabetes and they were focused only on available self-administered instruments in regards of validation aspects (90), however this work presents the broader perspective including the more comprehensive report on their structure, measurement scope, scoring etc. allowing possibilities for clinicians, health professionals and researchers to evaluate available HL and PTHL instruments and match them with the goals of their work.
HL has been presented as a measurable and important concept in considering education for patients with chronic diseases such as diabetes. It has been shown that in comparation to the other scales that focus exclusively on functional HL, FCCHL covers all three levels of HL, each of which can have different effects on patient outcomes. Also, the scale is easy to apply in clinical conditions (61).
The identified instruments have inherent strengths and weaknesses as a result of their structure, properties and measurement scope. The REALM, NVS, TOFHLA/ s-TOFHLA, DNT, KHLS, FCCHL and NVS are designed to directly measure specific skills and have some limitations in administration, especially in clinical settings where they are more likely to cause anxiety and shame among patients with inadequate HL and PTHL skills. Self-administrated instruments such as 3-brief SQ, HLS-EU-47 and HLQ non-directly measure certain skills and they are less likely to cause the anxiety and shame which makes them more suitable to be used in clinical settings and research applications. Many self-reported measures are designed as screening tests that may be differentially sensitive and specific than measures developed to more fully describe HL for research or clinical purposes. This is also seen in other articles (21, 91, 92).
The NVS had good sensitivity and may be more sensitive than the TOFHLA for marginal HL (83). Using the test can alert physicians and pharmacists to focus on the patients who require more attention and help them communicate with those patients by using recommended techniques.
The REALM and the TOFLHA focus primarily on reading-related skills and therefore do not present comprehensive measures for the skills needed by individuals in the healthcare system (21).
Time of administration plays a significant role in clinical settings. In this regard 3-brief SQ, NVS, FCCHL, REALM, REALM-R, S-TOFHLA and HLQ are relatively quick and easy for an administration and can be considered in different clinical settings and survey researches.
The type of administration must also be considered for practicality in clinical settings. REALM, REALM-R, KHLS and DNT-15 require involvement of the researcher and could cause shame and discomfort. Since self-administered instruments TOFHLA, S-TOFHLA, NVS, HLS-EU-47 and HLQ are very unlikely to cause discomfort, they require good visual abilities, full concentration, and good writing skills. Three-brief SQ and FCCHL can be administered in both ways and are more flexible and convenient for use.
A lack of researches with PTHL questionnaires in patients with type 2 diabetes mellitus is a very limiting factor for this population since the use of multiple drugs/insulins is very common. REALM only measures one dimension of HL and does not assess the patient's understanding of the words. DNT-15 is the test for numeracy.
The findings of this review can be used for other chronic conditions with similar HL and PTHL demands on individuals. This review did not only address the usefulness and applicability of the instruments in individuals with diabetes but also provided an evaluation of these instruments and their strengths and weaknesses, which are transferable for evaluating their applicability in other health conditions and situations.
Practice Implications
As instruments for measuring HL and PTHL continue to be published, authors advise clinicians, health professionals and researchers to evaluate available HL and PTHL measurements for a conceptual and practical match with the goals of their work.
When choosing a practical match, style of administration, purpose for measurement, their basic characteristics: domains, methods of assignment, structure, method of scoring, validation, strengths and limitations should be considered. It is important to align with the topic or task under consideration and choose the one that has been validated in a similar target population in order to have an accurate measure of the domain being assessed. Predictive qualities and appropriateness for assessment of changes in HL and outcomes over time have to be taken under consideration.
FCCHL was evaluated as the most appropriate instrument to apply to people with diabetes since a diabetes-specific type of instrument and the contents of its items may be more sensitive in a diabetes clinical setting targeted at diabetes, it is a model-based and comprehensive measure which covers all 3 levels of HL and the evidence for the measurement properties are better than those for the other instruments. However, his structural validity needs to be further established, and therefore adding DNT-15 questionnaire can be one of the options for considering application of FCCHL in this population (90).
Based on the previous considerations FCCHL and 3-brief SQ have the broadest measurement scopes. They are quick, easy, and inexpensive for administration. Three-level HL can be considered as the most useful and comprehensive instrument to screen for inadequate HL. The limitation is that the English version is not validated. Three-brief SQ has many advantages in comparison to other instruments, including that it is less likely to cause anxiety and shame. This instrument can be considered the best for measuring functional HL in patients with diabetes mellitus type 2 and other chronic diseases.
Limitations
This review was subject to some limitations. The use of non-interventional studies, the heterogeneity of studies in terms of samples represent important limitations for this scoping review. Only works written in English have been considered. Assessments of the instruments' dimensions, strengths, and limitations were made on the basis of our own experience and judgment; and as such, this was a subjective review. In order to minimize the effect of the issue of subjectivity, each measure was analyzed by multiple authors, and any discrepancy was addressed by all the authors and resolved through fruitful discussion.
Conclusion
The ongoing development of instruments suggests that there is still a need for comprehensive measurement across diverse populations. Three-brief SQ has been found convenient for use in populations with diabetes mellitus type 2 taking into consideration the broadest measurement scope, demonstrated good measurement properties, that has many advantages over other instruments, and could be considered the best available instrument to measure functional HL. FCCHL scale measures the broader concept of HL, including the ability to retrieve, understand, and use health-related information and could be one of the most appropriate and comprehensive instrument for measuring HL in people with diabetes. However, it has not been validated in English and the future research must be directed in this way, as well as establishing of the structural validity of the questionnaire.
The results of the studies show that HL may be directly related to the clinical outcome in patients with diabetes and that each individual level of HL could act differently. The ways in which each level of HL influences patient behaviour about care and health outcomes should be further explored.
So far, PTHL questionnaires (REALM/R and DNT-15) have not found their best application in people with type 2 diabetes mellitus and further research should certainly be aimed at developing a specific PTHL questionnaire for people with type 2 diabetes mellitus, due to the nature of the disease itself and the frequent use of multiple drugs in its therapy.
This works provides information to enable practitioners, health professionals and researches to select the most appropriate instrument available for measuring HL and PTHL in patients with type 2 diabetes mellitus.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
DK and ML contributed substantially to the conception, design of the study, screening, and selection of the studies. ML produced the first draft of the paper, which was extensively redrafted by DK, with significant input from NB-S. All authors contributed to the interpretation of data and read and approved the final manuscript.
Funding
The research of DK and NB-S was partially funded by the Ministry of Education, Science and Technological Development, Republic of Serbia through Grant Agreement with University of Belgrade-Faculty of Pharmacy No: 451-03-9/2021-14/200161.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
DK and NB-S are also co-authors of one paper reviewed in this study. However, the authors believe that the systematic inquiry undertaken in this paper is transparent, reproducible, and sufficiently neutral.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the professor Oliver Feeney from the Institute of Ethics and History of Medicine, University of Tübingen in Germany who made language corrections to the work.
References
1. Ministry of Education and Research. Rammeplan for Sykepleierutdanning [National Curriculum for Nursing Education]. (2008). Available online at: https://www.regjeringen.no/globalassets/upload/kd/vedlegg/uh/rammeplaner/helse/rammeplan_sykepleierutdanning_08.pdf (accessed July 30, 2021).
2. Ministry of Health and Care Services. Samhandlingsreformen. (Meld. St. 47 2008-2009). [The coordination Reform. Report to the Storting no. 47(Norwegian Parliament)]. (2009). Available online at: https://www.regjeringen.no/contentassets/d4f0e16ad32e4bbd8d8ab5c21445a5dc/no/pdfs/stm200820090047000dddpdfs.pdf (accessed July 30, 2021).
3. Ministry of Health and Care Services. Nasjonal Helse- Og Omsorgsplan (2011-2015). (Meld. St.10 2010-2011). [National Health and Care Service Plan. Report to the Storting no. 10(Norwegian Parliament)]. (2011). Available online at: https://www.regjeringen.no/contentassets/f17befe0cb4c48d68c744bce3673413d/no/pdfs/stm201020110016000dddpdfs.pdf (accessed July 30, 2021).
4. Nutbeam D. Discussion Paper on Promoting, Measuring and Implementing Health Literacy - Implications for Policy and Practice in Non-Communicable Disease Prevention and Control (WHO GCM/NCD Working group 3.3 2017). (2017). Available online at: https://www.researchgate.net/publication/315091628_World_Health_Organisation_Discussion_Paper_Promoting_measuring_and_implementing_health_literacy__Implications_for_policy_and_practice_in_noncommunicable_disease_prevention_and_control_httpwwwwhointg (accessed July 30, 2021).
5. Kickbusch I., Pelikan JM., Apfel F, Tsouros AD. Health Literacy. The Solid Facts. Copenhagen: WHO (2013).
6. Berkman ND, Sheridan SL, Donahue KE., Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Int Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
7. Nakayama K., Osaka W., Togari T., Ishikawa H., Yonekura Y., Sekido A., et al. Comprehensive health literacy in Japan is lower than in Europe: a validated Japanese-language assessment of health literacy. BMC Public Health. (2015) 15:505. doi: 10.1186/s12889-015-1835-x
8. Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Int Med. (2005) 20:175–84. doi: 10.1111/j.1525-1497.2005.40245.x
9. Parker RM., Williams MV, Weiss BD, Baker DW, Davis TC, Doak CC, et al. Health literacy-report of the council on Scientific affairs. JAMA. (1999) 281:552–7. doi: 10.1001/jama.281.6.552
10. Sørensen K., Pelikan JM, Rothlin F, Ganahl K., Slonska Z., Doyle G., et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health. (2015) 25:1053–8. doi: 10.1093/eurpub/ckv043
11. von Wagner C, Knight K, Steptoe A, Wardle J. Functional health Literacy and health-promoting behaviour in a national sample of British Adults. J Epidemiol Community Health. (2007) 61:1086–90. doi: 10.1136/jech.2006.053967
12. Williams MV, Davis T, Parker RM., Weiss BD. The role of health literacy in patient-physician communication. Family Med. (2002) 34:383–9.
13. Dickens C, Lambert BL, Cromwell T, Piano MR. Nurse overestimation of patients' health literacy. J Health Comm. (2013) 18(Suppl. 1):62–9. doi: 10.1080/10810730.2013.825670
14. Altin SV, Finke I, Kautz-Freimuth S, Stock S. The evolution of health literacy assessment tools: a systematic review. BMC Public Health. (2014) 14:1207. doi: 10.1186/1471-2458-14-1207
15. Nguyen TH, Paasche-Orlow MK, Kim MT, Han HR, Chan KS. Modern measurement approaches to health literacy scale development and refinement: overview, current uses, and next steps. J Health Commun. (2015) 20(Suppl. 2):112–15. doi: 10.1080/10810730.2015.1073408
16. Nguyen TH, Paasche-Orlow MK, McCormack LA. The state of the science of health literacy measurement. Inform Serv Use. (2017) 37:189–203. doi: 10.3233/ISU-170827
17. Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:1–13. doi: 10.1186/1471-2458-12-80
18. Simonds S. K. Health education as social policy. Health Educ Monog. (1974) 2(1_Suppl):1–10. doi: 10.1177/10901981740020S102
19. Ishikawa H, Kiuchi T. Health literacy and health communication. Bio Psycho Soc Med. (2010) 4:18. doi: 10.1186/1751-0759-4-18
20. Rudd RE, Rosenfeld L, Simonds VW. Health literacy: a new area of research with links to communication. Atlan J Commun. (2012) 20:16–30. doi: 10.1080/15456870.2012.637025
21. Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. (2010) 15(Suppl. 2):9–19. doi: 10.1080/10810730.2010.499985
22. Parker RM. Measuring Health Literacy: What? So What? Now What. Paper Presented at the Measures of Health Literacy: Workshop Summary. (2009). Available online at: http://www.nationalacademies.org/hmd/~/media/Files/Activity%20Files/PublicHealth/HealthLiteracy/Parker.pdf (accessed July 30, 2021).
23. King SR, McCaffrey DJ, Bouldin AS. Health literacy in the pharmacy setting: defining pharmacotherapy literacy. Pharm Pract. (2011) 9:213–20. doi: 10.4321/S1886-36552011000400006
24. Krajnovic D, Ubavic S, Bogavac-Stanojević N. Pharmacotherapy literacy and parental practice in use of over-the-counter pediatric medicines. Medicina. (2019) 55:80. doi: 10.3390/medicina55030080
25. Williams R, Colagiuri S, Chan J, Gregg EW, Ke C. IDF Atlas. 9th ed. Brussels: International Diabetes Federation (2019).
26. Bailey SC, Brega AG, Crutchfield TM, Elasy T, Herr H, Kaphingst K. Update on health literacy and diabetes. Diabetes Educ. (2014) 40:581–604. doi: 10.1177/0145721714540220
27. International Diabetes Federation. IDF Diabetes Atlas. (2017). Available online at: https://www.idf.org/our-activities/advocacy-awareness/resources-andtools/134:idf-diabetes-atlas-8th-edition.html (accessed July 30, 2021).
28. Norwegian Institute of Public Health. Folkehelserapporten (nettutgaven) - Helsetilstanden i norge [Public health report (web version)]. (2017). Availabke online at: https://www.fhi.no/nettpub/hin/ (accessed July 30, 2021).
29. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Hess Fischl A, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabet Care. (2015) 38:1372–82. doi: 10.2337/dc15-0730
30. Bohanny W, Wu SF, Liu CY, Yeh SH, Tsay SL, Wang, et al. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J Am Assoc Nurse Pract. (2013) 25:495–502. doi: 10.1111/1745-7599.12017
31. Kim S, Love F, Quistberg DA, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care. (2004) 27:2980–2. doi: 10.2337/diacare.27.12.2980
32. Fransen MP, Von Wagner C, Essink-Bot M-L. Diabetes self-management in patients with low health literacy: ordering findings from literature in a health literacy framework. Patient Educ Couns. (2012) 88:44–53. doi: 10.1016/j.pec.2011.11.015
33. Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. (2007) 33:144–51. doi: 10.1177/0145721706297452
34. Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. (2011) 16:268–78. doi: 10.1080/10810730.2011.604388
35. Baur C, Harris L, Squire E. The U.S. National action plan to improve health literacy: a model for positive organizational change. Stud Health Technol Inform. (2017) 240:186–202.
36. Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. (2004) 19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x
37. Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care. (2009) 32:1614–9. doi: 10.2337/dc09-0425
38. Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. (2003) 51:267–75. doi: 10.1016/S0738-3991(02)00239-2
39. Heijmans M, Waverijn G, Rademakers J, van der Vaart R, Rijken M. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ Couns. (2015) 98:41–8. doi: 10.1016/j.pec.2014.10.006
40. Caruso R, Magon A, Baroni I, Dellafiore F, Arrigoni C, Pittella F, et al. Health literacy in type 2 diabetes patients: a systematic review of systematic reviews. Acta Diabetol. (2018) 55:1–12. doi: 10.1007/s00592-017-1071-1
41. Mantwill S, Monestel-Umaña S, Schulz PJ. The relationship between health literacy and health disparities: a systematic review. PLoS ONE. (2015) 10:1–22. doi: 10.1371/journal.pone.0145455
42. Barton JL, Trupin L, Tonner C, Imboden J, Katz P, Schillinger D, et al. English language proficiency, health literacy, and trust in physician are associated with shared decision making in rheumatoid arthritis. J Rheumatol. (2014) 41:1290–7. doi: 10.3899/jrheum.131350
43. Cavanaugh K, Wallston K, Gebretsadik T, Shintani A, Huizing MM. Addressing literacy and numeracy to improve diabetes care. Diabetes Care. (2009) 32:2149–55. doi: 10.2337/dc09-0563
44. Pleasant A, Cabe J, Patel K, Cosenza J, Carmona R. Health literacy research and practice: a needed paradigm shift. Health Commun. (2015) 30:1176–80. doi: 10.1080/10410236.2015.1037426
45. European Commission. Together for health: a strategic approach for the EU 2008-2013. Brussels: European Commission (2007).
46. Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes selfmanagement education. Diabetes Care. (2009) 32(Suppl. 1):S87–S94. doi: 10.2337/dc09-S087
47. Boren SA. A review of health literacy and diabetes: opportunities for technology. J Diabetes Sci Technol. (2009) 3:202–9. doi: 10.1177/193229680900300124
48. Loueng JL, Fitz AL, Maack BJ, Miller DR. Evaluation of health literacy tools for correct prescription understanding. J Am Pharm Assoc Japha. (2015) 55:273–7. doi: 10.1331/JAPhA.2015.14110
49. Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. (2008) 23:561–6. doi: 10.1007/s11606-008-0520-5
50. Haun JN, Valerio MA, McCormack LA, Sørensen K, Paasche-Orlow MK. Health literacy measurement: an inventory and descriptive summary of 51 instruments. J Health Commun. (2014) 19(Suppl. 2):302–33. doi: 10.1080/10810730.2014.936571
51. de Vet HCW, Terwee CB, Mokkink LB, Knol DL. Measurement in Medicine - A Practical Guide. New York, NY: U.S.A., Cambridge University Press. (2011).
52. Al Sayah F, Williams B, Johnson JA. Measuring health literacy in individuals with diabetes: a systematic review and evaluation of available measures. Health Educ Behav. (2013) 40:42–55. doi: 10.1177/1090198111436341
53. Guzys D, Kenny A, Dickson-Swift V, Threlkeld G. A critical review of population health literacy assessment. BMC Public Health. (2015) 4; 15:215. doi: 10.1186/s12889-015-1551-6
54. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester: John Wiley & Sons (2019).
55. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews meta-analyses of studies that evaluate health care interventions: explanation elaboration. J Clin Epidemiol. (2009) 62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006
56. Sanderson S, Tatt ID, Higgins JP. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. (2007) 36:666–76. doi: 10.1093/ije/dym018
57. Ni XF, Yang CS, Bai YM, Hu ZX, Zhang LL. Drug-Related problems of patients in primary health care institutions: a systematic review. Front Pharmacol. (2021) 12:698907. doi: 10.3389/fphar.2021.698907
58. Klinovszky A, Papp-Zipernovszky O, Buzás N. Building a house of skills-a study of functional health literacy and numeracy among patients with type 2 diabetes in hungary. Int J Environ Res Public Health. (2021) 18:1547. doi: 10.3390/ijerph18041547
59. Hashim SA, Barakatun-Nisak MY, Abu Saad H, Ismail S, Hamdy O, Mansour AA. Association of health literacy and nutritional status assessment with glycemic control in adults with type 2 diabetes mellitus. Nutrients. (2020) 12:3152. doi: 10.3390/nu12103152
60. Gomes MB, Muniz LH, Melo L, Pizzaro MH. Health literacy and glycemic control in patients with diabetes: a tertiary care center study in Brazil. Diabetol Metab Synd Feb. (2020) 12:11. doi: 10.1186/s13098-020-0519-6
61. Finbraten HS. Measuring health literacy-evaluating psychometric properties of the HLS-EU-Q47 and the FCCHL, suggesting instrument refinements and exploring health literacy in people with type 2 diabetes and in the general Norwegian population. Psychology. (2018) 2018:15. urn:nbn:se:kau:diva-66928.
62. Tseng HM, Liao SF, Wen YP, Chuang YJ. Stages of change concept of the transtheoretical model for healthy eating links health literacy and diabetes knowledge to glycemic control in people with type 2 diabetes. Prim Care Diabetes. (2017) 11:29–36. doi: 10.1016/j.pcd.2016.08.005
63. Friis K, Vind BD, Simmons RK, Maindal HT. The relationship between health literacy and health behaviour in people with diabetes: a danish population-based study. J Diabetes Res. (2016) 2016:7823130. doi: 10.1155/2016/7823130
64. Sayah FA, Qiu W, Johnson JA. Health literacy and health-related quality of life in adults with type 2 diabetes: a longitudinal study. Qual Life Res. (2016) 25:1487–94. doi: 10.1007/s11136-015-1184-3
65. Thurston MM, Bourg CA, Phillips BB, Huston SA. Impact of health literacy level on aspects of medication nonadherence reported by underserved patients with type 2 diabetes. Diabetes Technol Ther. (2015) 17:187–93. doi: 10.1089/dia.2014.0220
66. Mantwill S, Schulz PJ. Low health literacy associated with higher medication costs in patients with type 2 diabetes mellitus: evidence from matched survey and health insurance data. Patient Educ Couns. (2015) 98:1625–30. doi: 10.1016/j.pec.2015.07.006
67. van der Heide I, Uiters E, Rademakers J, Struijs JN, Schuit AJ, Baan CA. Associations among health literacy, diabetes knowledge, and self-management behavior in adults with diabetes: results of a dutch cross-sectional study. J Health Commun. (2014) 19(Suppl. 2):115–31. doi: 10.1080/10810730.2014.936989
68. Al Sayah F, Williams B, Pederson JL, Majumdar SR, Johnson JA. Health literacy and nurses' communication with type 2 diabetes patients in primary care settings. Nurs Res. (2014) 63:408–17. doi: 10.1097/NNR.0000000000000055
69. Bauer AM, Schillinger D, Parker MM, Katon W, Adler N, Adams AS, et al. Health literacy and antidepressant medication adherence among adults with diabetes: the diabetes study of northern california (DISTANCE). J Gen Intern Med. (2013) 28:1181–7. doi: 10.1007/s11606-013-2402-8
70. Coffman MJ, Norton CK, Beene L. Diabetes symptoms, health literacy, and health care use in adult latinos with diabetes risk factors. J Cult Divers. (2012) 19:4–9.
71. McCleary-Jones V. Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF J. (2011) 22:25–32.
72. Osborn CY, Bains SS, Egede LE. Health literacy, diabetes self-care, and glycemic control in adults with type 2 diabetes. Diabetes Technol Ther. (2010) 12:913–9. doi: 10.1089/dia.2010.0058
73. Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. (2011) 13:335–41. doi: 10.1089/dia.2010.0160
74. Mancuso JM. Impact of health literacy and patient trust on glycemic control in an urban USA population. Nurs Heal Sci. (2010) 12:94–104. doi: 10.1111/j.1442-2018.2009.00506.x
75. Sarkar U, Karter AJ, Liu JY, Moffet HH, Adler NE, Schillinger D. Hypoglycemia is more common among type 2 diabetes patients with limited health literacy: the diabetes study of northern California (DISTANCE). J Gen Intern Med. (2010) 25:962–8. doi: 10.1007/s11606-010-1389-7
76. Mbaezue N, Mayberry R, Gazmararian J, Quarshie A, Ivonye C, Heisler M. The impact of health literacy on self-monitoring of blood glucose in patients with diabetes receiving care in an Inner-City Hospital. J Natl Med Assoc. (2010) 102:5–9. doi: 10.1016/S0027-9684(15)30469-7
77. Kim SH. Health literacy and functional health status in Korean older adults. J Clin Nurs. (2009) 18:2337–43. doi: 10.1111/j.1365-2702.2008.02739.x
78. Ishikawa H, Takeuchi T, Yano E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care. (2008) 31:874–9. doi: 10.2337/dc07-1932
79. Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, et al. Association of numeracy and diabetes control. Ann Intern Med. (2008) 148:737–46. doi: 10.7326/0003-4819-148-10-200805200-00006
80. Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. (2006) 24:7–21. doi: 10.1186/1471-2296-7-21
81. Lee TW, Kang SJ, Lee HJ, Hyun SI. Testing health literacy skills in older Korean adults. Patient Educ Couns. (2009) 75:302–7. doi: 10.1016/j.pec.2009.04.002
82. Sørensen K, Van den Broucke S, Pelikan JM, Fullam J, Doyle G, Slonska Z, et al. Measuring health literacy in populations: illuminating the design and development process of the European health literacy survey questionnaire (HLS-EU-Q). BMC Public Health. (2013) 13:948. doi: 10.1186/1471-2458-13-948
83. Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. (2005) 3:514–22. doi: 10.1370/afm.405
84. Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. (1995) 10:537–41. doi: 10.1007/BF02640361
85. Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. (1999) 38:33–42. doi: 10.1016/S0738-3991(98)00116-5
86. Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, et al. Rapid assessment of literacy levels of adult primary care patients. Fam Med. (1991) 23:433–5.
87. Bass PF 3rd, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. (2003) 18:1036–8. doi: 10.1111/j.1525-1497.2003.10651.x
88. Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health. (2013) 13:658. doi: 10.1186/1471-2458-13-658
89. Huizinga MM, Elasy TA, Wallston KA, Cavanaugh K, Davis D, Gregory RP, et al. Development and validation of the Diabetes Numeracy Test (DNT). BMC Health Serv Res. (2008) 8:96. doi: 10.1186/1472-6963-8-96
90. Lee EH, Kim CJ, Lee J, Moon SH. Self-administered health literacy instruments for people with diabetes: systematic review of measurement properties. J Adv Nurs. (2017) 73:2035–48. doi: 10.1111/jan.13256
91. Wolf MS, Williams MV, Parker RM, Parikh NS, Nowlan AW, Baker DW. Patients' shame and attitudes toward discussing the results of literacy screening. J Health Commun. (2007) 12:721–32. doi: 10.1080/10810730701672173
Keywords: health literacy, medication literacy, measurement tool, assessment, patient, chronic disease, healthcare system
Citation: Levic M, Bogavac-Stanojevic N and Krajnovic D (2021) The Instruments Used to Assess Health Literacy and Pharmacotherapy Literacy of Diabetes Mellitus Type 2 Patients: A Scoping Review. Front. Public Health 9:747807. doi: 10.3389/fpubh.2021.747807
Received: 26 July 2021; Accepted: 31 August 2021;
Published: 27 September 2021.
Edited by:
Georgi Iskrov, Plovdiv Medical University, BulgariaReviewed by:
Maria Stefanova Kamusheva, Medical University of Sofia, BulgariaBeata Gavurova, Tomas Bata University in Zlín, Czechia
Mohammad Rezal Hamzah, Universiti Malaysia Perlis, Malaysia
Copyright © 2021 Levic, Bogavac-Stanojevic and Krajnovic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dusanka Krajnovic, ZHVzaWNhLmtyYWpub3ZpY0BwaGFybWFjeS5iZy5hYy5ycw==
 Marija Levic
Marija Levic Dusanka Krajnovic
Dusanka Krajnovic