
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 22 July 2021
Sec. Children and Health
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.689021
Background: To identify distinct trajectories of body mass index (BMI) in a large sample of Chinese children by urban-rural and sex disparities.
Methods: Data for this study were obtained from the National Surveys on Chinese Students' Constitution and Health among 16,060 children aged 6–11 years. Weight and height data were used to calculate BMI. Group-based trajectory modeling (GBTM) was used to identify distinct BMI trajectories.
Results: Seven distinct trajectories were identified, “sustained healthy weight” (46.01%), “sustained obesity” (17.26%), “sustained underweight” (4.50%), “obesity to overweight” (6.45%), “obesity to healthy weight” (11.75%), “healthy weight to overweight” (8.67%), and “healthy weight to obesity” (5.36%). The proportions of “sustained obesity,” “healthy weight to obesity,” and “healthy weight to overweight” trajectories were much higher among boys compared with girls (P < 0.001). Meanwhile, children living in rural areas were more represented in the “healthy weight to obesity” trajectory (P < 0.001).
Conclusion: In this study, the proportions of BMI development trajectories among 6–11-year-old children varied by sex and urban-rural areas, which may require tailored interventions specifically toward these at-risk trajectories.
To our knowledge, the prevalence of childhood obesity has increased rapidly over time and attracts significant attention from many fields. It is reported that the prevalence of obesity among Chinese children aged 7–18 years increased to 7.5% in 2006–2010 (1) and still rose in 2010–2015 (2). Importantly, almost 28.0% of children will be overweight and obese by 2030. Childhood obesity is known to have immediate and long-term unhealthy consequences (3, 4). Body mass index (BMI) trajectories could reflect the potential obesity dynamic changing patterns during the life course (5) and might provide a valuable dimension for consideration. Such research is necessary because it will enhance our understanding to identify the possible risk factors of obesity onset and development during childhood.
Most of the previous reports have shown differences in the prevalence of obesity among children by sex, age group, and urban-rural regions (6). However, they only focused on one time point and ignored the dynamics of childhood obesity. Although a few studies have explored the risk factors and detrimental outcomes associated with children's BMI trajectories (5, 7–9). There is still a paucity of studies exploring the difference of children's BMI trajectories in terms of urban-rural and sex parameters. In China, rapid economic development and dramatic changes to lifestyles and eating habits have led to a substantial difference in the prevalence of obesity among children in recent years (10). Thus, this study aimed to provide current estimates of sex and urban-rural BMI trajectories and dynamic change of obesity status with age in China.
Data for this study came from the National Surveys on Chinese Students' Constitution and Health 2013–2018 in Zibo city, which is an ongoing nationally representative school-based sample of children followed into adolescents. A sample of 17,175 students (8,910 boys and 8,265 girls) aged 6 years in 2013 participated in this study. After 6 years of follow-up, 16,060 students (8,347 boys and 7,713 girls) completed six measurements of height and weight. Informed consent was provided by a parent or legal guardian for all study participants. The study was approved by the Ethics Committee of the Affiliated Hospital of Qingdao University (project identification code: 20130817). This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and later amendments.
In this research, a stratified multi-stage cluster randomization sampling method was used. In the first stage, Zibo city was divided into 10 municipal districts, each was considered as a stratum. The number of schools in each stratum was determined using the stratified sampling method proportional to size and the number of schools in that stratum. In the second stage, once the sample size in each stratum was determined, the schools within the strata were considered as clusters and the Excel 2016 software was used to cluster two randomly selected elementary schools from each district in order to collect the representative data. In the third stage, all the students aged 6 years in the first grade were invited to participate in this study. The sample size was determined through the use of the following formula and taking into account α = 0.05, π =4% (the rate of the “healthy weight to obesity” trajectory), δ = 0.15π, design effect = 1.5. Considering the possibility of withdrawal at 10%, the final sampling size was 17,175 participants.
The present study included children with available information on sex, age, region (urban/rural), and data of height and weight. The height and weight were measured annually. All measurements were conducted by a team of trained technicians in each of the 10 districts using the same type of apparatus and following the same procedures. Height was measured using a wall-mounted stadiometer to the nearest 0.1 cm and weight was measured with a standardized scale to the nearest 0.1 kg. Both height and weight were measured twice, and the mean value was recorded. Body mass index (BMI) was calculated using the following formula: BMI = weight (kg)/height2 (m2). Subjects were defined as being overweight or obese by referring to the age-specific and sex-specific classification criteria for Screening Overweight and Obesity in Chinese Children and Adolescents.
The group-based trajectory modeling (GBTM) approach implemented in SAS Proc Traj was used to identify trajectory groups between ages 6 and 12 years that shared similar underlying trajectories of body shape (11). Chi-square tests were conducted to estimate the disparities of BMI trajectories by sex and urban-rural areas. All statistical analyses were conducted using SAS V.9.3 (SAS Institute, Cary, North Carolina, USA). The statistical significance level was set to α = 0.05 for all association analyses.
Using BIC to assess the goodness-of-fit of the competing GBTM models, seven discrete BMI trajectories were identified among the 16,060 participants (Figure 1, Table 1). A total of 4.50, 46.01, and 17.26% followed a trajectory where the average predicted BMI levels remained within underweight (Trajectory 1, “sustained underweight”), healthy weight (Trajectory 3, “sustained healthy weight”), and obesity body shapes (Trajectory 7, “sustained obesity”), respectively. A total of 8.67% of participants maintained a progressive overweight body shape (Trajectory 5, “healthy weight to overweight”), 5.36% followed the trajectory of a progressive obese body shape (Trajectory 6, “healthy weight to obesity”), 6.45% started out as obese then experienced a decrease to an overweight body shape (Trajectory 4, “obesity to overweight”), 11.75% started out as obese then experienced a decrease to a healthy weight body shape (Trajectory 2, “obesity to healthy weight”).
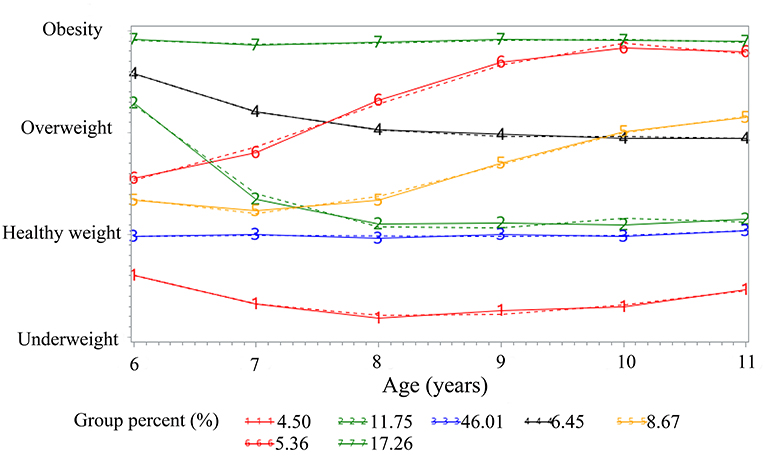
Figure 1. Trajectories of body shape during children from 6 to 11 years. Solid lines represent observed values, and dashed lines represent expected values. Trajectory 1, “sustained underweight” (4.50%); Trajectory 2, “obesity to healthy weight” (11.75%); Trajectory 3, “sustained healthy weight” (46.01%); Trajectory 4, “obesity to overweight” (6.45%); Trajectory 5, “healthy weight to overweight” (8.67%); Trajectory 6, “healthy weight to obesity” (5.36%); Trajectory 7, “sustained obesity” (17.26%).
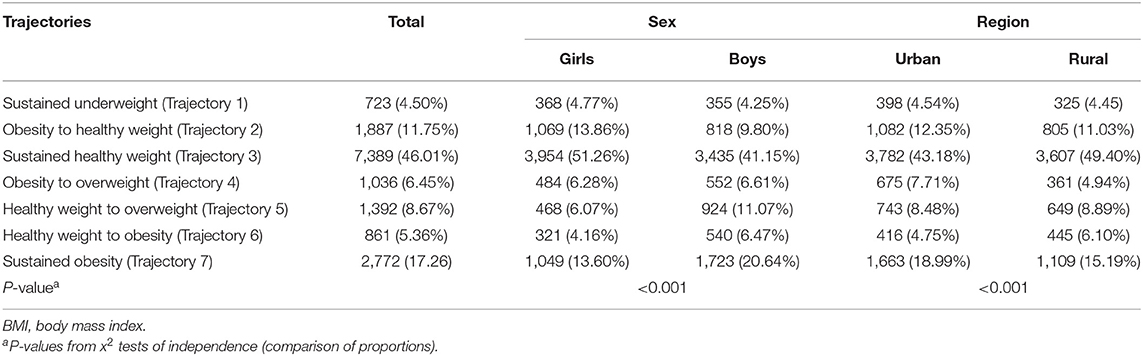
Table 1. Participant disparities by sex and urban-rural region for each of the seven different BMI trajectory groups.
Disparities were indicated in the proportions and the patterns of the BMI trajectories modeled separately by sex and region (P < 0.001) (Table 1). Of note, there were strong associations between children's BMI trajectory assignment and the region and sex of the children. The results showed that boys were more likely to follow the “sustained obesity,” “healthy weight to obesity,” and “healthy weight to overweight” trajectories. Similarly, children living in a rural area were more likely to follow the “healthy weight to obesity” trajectory.
This study revealed that seven body shape trajectories were identified in children aged 6–11 years. Similarly, a systematic review indicated conclusively that the number of children's BMI trajectories often ranged from three to seven (12). According to our data, a large number of children followed the trajectory of “sustained obesity” with the exception of a healthy trajectory, which was consistent with several previous studies (6, 13, 14). Therefore, practitioners and researchers should pay more attention to a decrease in the rate of obesity maintenance in the future.
Our study indicated that sex was a key factor of trajectory assignment. Boys had higher odds of following unhealthy weight trajectories, such as “sustained obesity,” “healthy weight to obesity,” and “healthy weight to overweight” trajectories. Sun et al.'s study showed a similar result that strongly supported our findings (15). Dietary and physical activity behaviors posed a possible explanation for this discrepancy. First, family or social environment and personal perception exerted different impacts on the control of diet for girls but not for boys (16). Girls tended to choose more fad dieting or unhealthy eating behaviors to pursue a slim figure especially during adolescence (17). Furthermore, along with a fast-paced life and widespread use of the Internet, a report of risk behavior monitoring indicated higher odds in the intake of soft drinks and time spent playing computer games for boys than girls, which might contribute to the obesity disparity (18). Accordingly, different health-care recommendations and health resources should be taken into consideration for these at-risk groups in follow-up investigation and intervention.
Our results suggested a complex relationship between region and children's BMI trajectories. The data only showed that children living in rural areas were more likely to follow the trajectory of “healthy weight to obesity,” which might largely be accounted for by the urbanization of rural areas in recent years. Although many previous studies have reported that the prevalence rate of being overweight or obese are higher in children living in urban compared to those living in rural areas (19), a meta-analysis indicated that the difference had decreased over time due to urbanization (20). Indeed, the surveys in rural areas of Shandong province documented that the rate of obese and overweight children was rapidly increasing over time (10, 21). There was a minimal urban-rural difference with regard to healthy diet and physical activity (22). The increasing trend of urbanization was consistent with the rate of obese or overweight children. Consequently, future longitudinal studies in various regions with regard to different eating habits and economic situation are warranted to verify our results.
Although this study provided a novel insight and valuable opportunity to target interventions for children who are overweight and obese, some limitations are still apparent. First, we focused our analyses on modeling the temporal dynamics of BMI change with age. We did not examine potential behavioral or psychosocial factors influencing childhood obesity trajectories which might explain the disparities by sex and urban-rural areas. Addressing this question requires additional covariates which were not available in our analysis and is a topic for future research. Second, GBTM is an exploratory data-driven technique and it is possible that chance relationships in our data will influence trajectory group findings. We were conservative in identifying most likely latent class groups and the trajectories we identified were plausible.
This study provided a comprehensive estimation on the disparities of body shape trajectories of 6–12-year-old children in a representative sample for sex and urban-rural areas in eastern China. Boys and children living in rural areas were at increased risk of following unhealthy BMI trajectories. The results will provide valuable evidence for the control of being overweight and obese in children. Health professionals and health-care institutions should take different measures in terms of different sex and regions of children.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of the Affiliated Hospital of Qingdao University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
This study was sponsored by Postdoctoral Science Foundation of China (2019M6601) and Shandong Provincial Natural Science Foundation (ZR2020QG059).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Yu Z, Han S, Chu J, Xu Z, Zhu C, Guo X. Trends in overweight and obesity among children and adolescents in China from 1981 to 2010: a meta-analysis. PLoS ONE. (2012) 12:e51949. doi: 10.1371/journal.pone.0051949
2. Zhang J, Li X, Hawley N, Zheng Z, Zou Z, Tan L, et al. Trends in the prevalence of overweight and obesity among Chinese school-age children and adolescents from 2010 to 2015. Child Obes. (2018) 3:182–8. doi: 10.1089/chi.2017.0309
3. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. J Am Med Assoc. (2018) 16:1723–5. doi: 10.1001/jama.2018.3060
4. Pan L, Blanck HM, Park S, Galuska DA, Freedman DS, Potter A, et al. State-specific prevalence of obesity among children aged 2–4 years enrolled in the special supplemental nutrition program for women, infants, and children - United States, 2010–2016. Morb Mortal Wkly Rep. (2019) 46:1057–61. doi: 10.15585/mmwr.mm6846a3
5. Oluwagbemigun K, Buyken AE, Alexy U, Schmid M, Herder C, Nöthlings U. Developmental trajectories of body mass index from childhood into late adolescence and subsequent late adolescence-young adulthood cardiometabolic risk markers. Cardiovasc Diabetol. (2019) 1:9. doi: 10.1186/s12933-019-0813-5
6. Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. J Am Med Assoc. (2018) 23:2410–8. doi: 10.1001/jama.2018.5158
7. Nedelec R, Miettunen J, Männikkö M, Järvelin MR, Sebert S. Maternal and infant prediction of the child BMI trajectories; studies across two generations of Northern Finland birth cohorts. Int J Obes. (2021) 2:404–14. doi: 10.1038/s41366-020-00695-0
8. Sharman MJ, Jose KA, Tian J, Venn AJ, Canary J, Banks S, et al. Childhood factors related to diverging body mass index trajectories from childhood into mid-adulthood: a mixed methods study. Soc Sci Med. (2021) 2021:113460. doi: 10.1016/j.socscimed.2020.113460
9. Wang X, Dong B, Huang S, Ma Y, Zou Z, Ma J, et al. Body mass index trajectory and incident hypertension: results from a longitudinal cohort of Chinese children and adolescents, 2006–2016. Am J Public Health. (2020) 11:1689–95. doi: 10.2105/AJPH.2020.305873
10. Zhou Y, Wang S, Zhang Q, Zhang Y. Wang T. Prevalence of overweight and obesity among children and adolescents increased rapidly in Chinese rural regions while level off in urban areas. Int J Cardiol. (2016) 223:61–2. doi: 10.1016/j.ijcard.2016.08.169
11. Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Method Res. (2007) 35:542–71. doi: 10.1177/0049124106292364
12. Mattsson M, Maher GM, Boland F, Fitzgerald AP, Murray DM, Biesma R. Group-based trajectory modelling for BMI trajectories in childhood: a systematic review. Obes Rev. (2019) 7:998–1015. doi: 10.1111/obr.12842
13. Kwon S, Janz KF, Letuchy EM, Burns TL, Levy SM. Association between body mass index percentile trajectories in infancy and adiposity in childhood and early adulthood. Obesity. (2017) 1:166–71. doi: 10.1002/oby.21673
14. Montazeri P, Vrijheid M, Martinez D, Basterrechea M, Fernandez-Somoano A, Guxens M, et al. Maternal metabolic health parameters during pregnancy in relation to early childhood BMI trajectories. Obesity. (2018) 3:588–96. doi: 10.1002/oby.22095
15. Sun X, Zhao B, Liu J, Wang Y, Xu F, Wang Y, et al. A 3-year longitudinal study of the association of physical activity and sedentary behaviours with childhood obesity in China: the childhood obesity study in China mega-cities. Pediatr Obes. (2020) 2020:e12753. doi: 10.1111/ijpo.12753
16. Jendrzyca A, Warschburger P. Weight stigma and eating behaviours in elementary school children: a prospective population-based study. Appetite. (2016) 2016:51–9. doi: 10.1016/j.appet.2016.02.005
17. Mak KK, Pang JS, Lai CM, Ho RC. Body esteem in Chinese adolescents: effect of gender, age, and weight. J Health Psychol. (2013) 1:46–54. doi: 10.1177/1359105312437264
18. Ji CYA. Comprehensive Survey of Health-Related Risk Behaviors among Adolescents in China 2005. Beijing: Peking University Medical Press (2007).
19. Liu JH, Jones SJ, Sun H, Probst JC, Merchant AT, Cavicchia P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: an urban and rural comparison. Child Obes. (2012) 5:440–8. doi: 10.1089/chi.2012.0090
20. Guo Y, Yin X, Wu H, Chai X, Yang X. Trends in overweight and obesity among children and adolescents in China from 1991 to 2015: a meta-analysis. Int J Environ Res Public Health. (2019) 23:4656. doi: 10.3390/ijerph16234656
21. Zhang YX, Wang ZX, Zhao JS, Chu ZH. Trends in overweight and obesity among rural children and adolescents from 1985 to 2014 in Shandong, China. Eur J Prev Cardiol. (2016) 12:1314–20. doi: 10.1177/2047487316643830
Keywords: children, body mass index, trajectory, sex, region
Citation: Zhou Y, Yu P, Zhang Y, Wang T and Wang A (2021) Distinct Patterns of Urban-Rural and Sex Disparities in Children's BMI Trajectories From 2013 to 2018. Front. Public Health 9:689021. doi: 10.3389/fpubh.2021.689021
Received: 01 April 2021; Accepted: 24 May 2021;
Published: 22 July 2021.
Edited by:
Joemer Maravilla, University of Queensland, AustraliaReviewed by:
Nihar Ranjan Mishra, Veer Surendra Sai Medical College and Hospital, IndiaCopyright © 2021 Zhou, Yu, Zhang, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunping Zhou, bHd6aG91eXVucGluZ0AxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.