- 1Faculty of Health Sciences, Curtin School of Allied Health, Curtin University, Perth, WA, Australia
- 2Australian Centre for Health Services Innovation and Centre for Healthcare Transformation, Faculty of Health, School of Public Health & Social Work, Queensland University of Technology, Brisbane, QLD, Australia
- 3Clinical Informatics Directorate, Metro South Health, Brisbane, QLD, Australia
- 4Healthscope Academic and Research Collaborative in Health, La Trobe University, Bundoora, VIC, Australia
- 5College of Healthcare Sciences, James Cook University, Douglas, QLD, Australia
- 6School of Primary and Allied Health Care, Monash University, Frankston, VIC, Australia
- 7Royal Perth Hospital, Perth, WA, Australia
- 8Western Australian Centre for Health and Ageing, Medical School, University of Western Australia, Perth, WA, Australia
- 9Malcom Randall Veterans Affairs Medical Center, Geriatric Research Education and Clinical Center, Gainesville, FL, United States
- 10College of Medicine, University of Florida, Gainesville, FL, United States
- 11Institute for Health Research, The University of Notre Dame Australia, Fremantle, WA, Australia
- 12Department of Geriatric Rehabilitation, Armadale Health Service, Department of Health, Perth, WA, Australia
Recently hospitalized older people are at risk of falls and face barriers to undertaking fall prevention strategies after they return home from hospital. The authors examined the effects of tailored education delivered by physiotherapists on the knowledge (capability) and the motivation of older people to engage in fall prevention after hospital discharge. Utilizing data gathered from a recent trial, data was analyzed from 390 people who were 60 years and over without impaired cognition (>7/10 abbreviated mental test score) and discharged from three Australian hospitals. Motivation and capability were measured at baseline in the hospital and at 6-months after hospital discharge by blinded assistants using structured surveys. Bivariate analysis using generalized linear modeling explored the impact of education on the capability and motivation. Engagement in fall prevention strategies was entered as an independent variable during analysis to determine associations with capability and motivation. The education significantly improved capability [−0.4, 95% CI (−0.7, −0.2), p < 0.01] and motivation [−0.8, 95% CI (−1.1, −0.5), p < 0.01] compared with social-control at the time of hospital discharge. In contrast, social-control participants gained capability and motivation over the 6-months, and no significant differences were found between groups in capability [0.001, 95% CI (−0.2, 0.2), p = 0.9] and motivation [−0.01, 95% CI (−0.3, 0.3), p = 0.9] at follow-up. Tailored fall prevention education is recommended around hospital discharge. Participants still needed to overcome barriers to falls prevention engagement post hospitalization. Thus, tailored education along with direct clinical services such as physiotherapy and social supports is warranted for older people to avoid falls and regain function following hospitalization.
Introduction
The problem of falls and associated ongoing costs for healthcare are recognized to be serious among older people who have recently been discharged home from hospital (1, 2). Apart from having age-related comorbidities (3), this population is recovering from illness or disability, and can experience ongoing effects from being in hospital (4). Heightened falls risk is reflective of discharge care practices and the diminished function of many older individuals (5–7). Underlying effective discharge care is the concept of patient-centered care (8) that values patients' understanding of their own health risks, while helping them to gain necessary health knowledge to maintain safety and independence (9).
Previous studies have shown older people to have limited knowledge about fall prevention following hospitalization (10). Sometimes they believe that fall prevention activities are more important for other older people than for themselves (11). Reduced knowledge about falls risks and low motivation affect the engagement of older people in fall strategies, such as exercise (12, 13). To address this need, we recently implemented a novel education program that was designed based on the COM-B model (14). It aimed to reduce falls in older people by encouraging uptake of fall prevention strategies once they returned home from hospital. However, we did not find any differences in the uptake of fall prevention strategies after returning home from hospital for those who received the education compared with control. It is important to evaluate the constructs of the model that underpinned the education program which may help to explain the lack of uptake of falls prevention behavior in these people. Importantly, it may assist in the refinement of the education program for future use.
The theory of health behavior change proposes that people require the opportunity to make changes within their daily lives, as well as the knowledge and motivation to change their behavior (14). Previous studies of hospital discharge care reported that older people understood discharge plans, yet were unprepared to carry these out when faced with different demands in their living environment (15, 16). Some older people also report difficulty in overcoming barriers (lacked opportunity) to implement fall prevention action plans once they returned home (17). Nonetheless, opportunity is only one of the constructs in the model. The COM-B health behavior change model explains that people may not take-up opportunities or address barriers to undertake fall prevention activities if they lack the capability or motivation (14). Thus, evaluating the capability and motivation of recipients would provide us with a better understanding of the interplay between these constructs, leading to a behavioral change. This study aimed to measure the impact of tailored education on the level of capability (knowledge) and motivation of older people to engage in fall prevention during 6 months after hospitalization, compared with control conditions.
Methods
Research Design
A secondary analysis of data from a randomized controlled trial (RCT) (n = 390) was published previously (2). This quantitative evaluation used data from three collection points, namely: at baseline in hospital prior to education delivery (T1), following education delivery prior to hospital discharge (T2), and at 6 months after discharge (T3). Ethical approvals were obtained from human research ethics committees of the participating hospitals and universities. All participants provided written informed consent. This study has been reported according to the CONSORT (2010) statement (18).
Participants and Setting
Participants (n = 390) were hospital patients who were aged 60 years and over who were enrolled in a trial and randomized in a trial to receive either a tailored education intervention in addition to the usual care or a social control intervention and followed up after receiving the intervention prior to discharge and at 6-months after discharge from three rehabilitation hospitals in Perth, Western Australia (2). Participants were recovering from a variety of geriatric conditions, including orthopedic, neurological, and general medical conditions. They were included in the trial if they spoke English as a first language, could give written informed consent, and were discharged to the community. Participants were excluded if they were to be discharged to a residential care facility, had hearing or visual problems that excluded them from engaging with the education materials, or had impaired cognition [inclusion criteria >7/10 on abbreviated mental test score (19)]. The protocol for this study has been published (20).
Capability and Motivation: COM-B Theory of Behavior Change
The behavioral change theory utilized during the design of the education intervention suggests that capability, motivation, and opportunity interact to affect behavioral outcomes (COM-B) (14). For this study, capability and motivation outcomes were framed as internal factors that could be modified by the education, such as their general knowledge about falls risks (capability), self-perceived awareness of their own falls risks (motivation), and willingness to participate in fall prevention strategies (motivation). For example, participants were asked to consider social supports to complete their daily activities when they returned home from hospital, for which they required (capability) knowledge and motivation, as well as the opportunity to access social supports. External components (opportunity) were explored during a separate qualitative study (17) and were considered external social and physical enablers (such as access to therapy and social supports) that may have existed within the environment and life-circumstances of the participants after hospital discharge. This evaluation focused on the internal constructs of capability and motivation from the COM-B model.
Outcomes
The outcomes for the study were as follows:
i) Capability: participant perceived knowledge about the risks of falls and falls injuries.
ii) Motivation: self-perceived awareness of the participant about their own fall risks, likelihood of reduced independence following hospitalization, and willingness to engage in fall prevention strategies.
Capability and motivation outcomes were measured for both groups by blinded research assistants using structured surveys face to face in hospital prior to allocation at baseline (T1), following the education intervention, but prior to discharge (T2), and by telephone at six months following hospitalization (T3). The surveys were modified from previous studies that evaluated fall prevention behavioral change interventions (10, 21–23), and contained questions that were closed-item statements requiring responses on a five-point Likert response scale, where 1 (“strongly agree”) indicated a better outcome compared to 2 (“agree”), 3 (“undecided”), 4 (“disagree”), and 5 (“strongly disagree”). Survey questions were worded to stimulate a response that would indicate the presence of capability and motivation to engage in fall prevention strategies based on their level of agreement or disagreement. For example, the wording of a survey item pertaining to capability, regarding participant knowledge of falls risks in older people following hospitalization was, “I think that older people who go home from hospital are at risk of falling over in the first 6 months following hospitalization.” The survey was pilot tested on a representative sample of 10 older people recently discharged home from hospital to confirm face, content, and construct validity (24).
Data Collection and Procedure
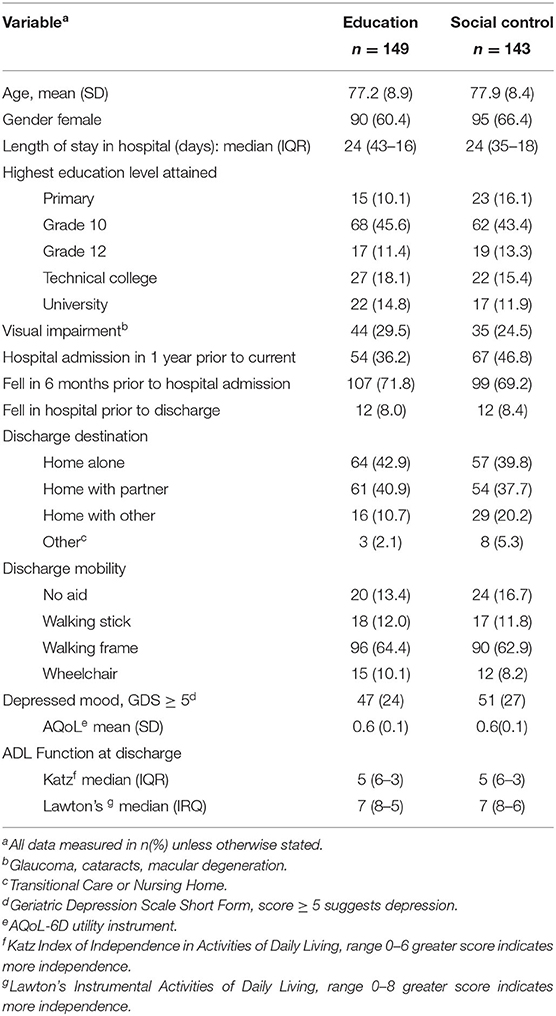
Demographic data were collected at baseline (see Table 1) using a structured questionnaire. Prior to discharge, the education group received the education in addition to usual care. The control group received a social intervention in addition to usual care that discussed positive aging without reference to falls prevention. The education was delivered by physiotherapists using a workbook and video (2). It presented fall-prevention strategies specific to the post discharge period and tailored to participants based on their perceived knowledge of falls risks, willingness to participate in falls prevention strategies, and identified barriers to fall prevention engagement after hospitalization. A goal-directed action plan to initiate after hospital discharge was then provided to help prepare participants for their imminent discharge home and it included fall prevention strategies, such as completion of safe exercise, an occupational therapist home hazard assessment, and seeking assistance with daily activities (ADLs) to enable a gradual return of independence (2). The same educators provided guided feedback once per month via telephone for 3 months after hospital discharge.
Statistical Analysis
This was a post-hoc secondary analysis of the outcomes of capability and motivation with consideration of the covariates of engagement in fall prevention strategies. All analyses were conducted using Stata release 16, (StataCorp, College Station, Texas, 2020), the significance level set at = 0.05, and the sample size previously determined by primary trial effect analysis (2). Intention to treat analysis was undertaken to determine influence of group allocation on outcomes based on the trial randomization. Non-parametric Likert scale outcome data were summarized using median and interquartile range (IQR) for both groups at data collection timepoints (T1, T2, T3). Graphs of the proportion of response ratings between 1 and 5 for each outcome at the three timepoints were completed to present the data. Differences in capability and motivation within and between groups, with and without the interaction of time were compared using mixed-effects generalized linear modeling, with adjustment for identified fall risk factors in this population, including older age, previous falls, presence of visual impairment, depressed mood, and use of a walking aid at the time of discharge, consistent with a pilot study of the intervention (21). Further, analysis to determine the association between the presence of capability and motivation (as binary data) and engagement in falls prevention strategies was completed. Data from a previous evaluation (25) regarding the reported engagement of the participants in fall prevention strategies after hospital discharge at 6 months follow-up (T3) was included as an independent variable during analysis, using mixed effects generalized linear modeling with adjustment for falls risk factors. This was completed to identify any association between engagement as behavior change, and the primary outcomes of capability and motivation. The fall prevention strategies were categorized as discrete data and consisted of participants having received assistance with ADLs (such as showering and dressing); instrumental activities of daily living [IADLs, (such as cleaning and shopping)]; completed home (hazard) modifications; and completed an exercise program during the 6 months post hospitalization.
Results
Participant flow through the study (in Supplementary Figure 1) shows that from the original cohort of 390 participants at baseline, there were 292 who completed measures at 6 months follow-up. There were no significant differences in characteristics between the two groups (Table 1).
Table 2 presents differences in capability and motivation compared between education and control groups at baseline in hospital (T1), follow-up prior to hospital discharge (T2), and 6 months post hospitalization (T3). Participants who received the education significantly improved their capability (knowledge about fall risks of other people and falls injury risks), and motivation (awareness of their own falls risks and loss of independence) compared with control following education delivery in hospital (T2). Education group participants maintained capability and motivation when surveyed at the 6-month follow-up (T3), whereas, those in control gained capability (knowledge) and motivation during their post hospitalization recovery at home, leading to no significant differences between education and control groups at 6-months (T3).
Figure 1 presents participant levels of capability and motivation in both intervention (education) and control groups at baseline (T1), in hospital prior to discharge (T2), and at 6 months post hospitalization (T3). Supplementary Table 1 presents summarized descriptive statistics (median and interquartile range), and Supplementary Table 2 presents complete data (number and percentage) of the levels of capability and motivation for both groups at baseline (T1), at follow-up prior to discharge (T2), and at 6 months post hospitalization (T3).
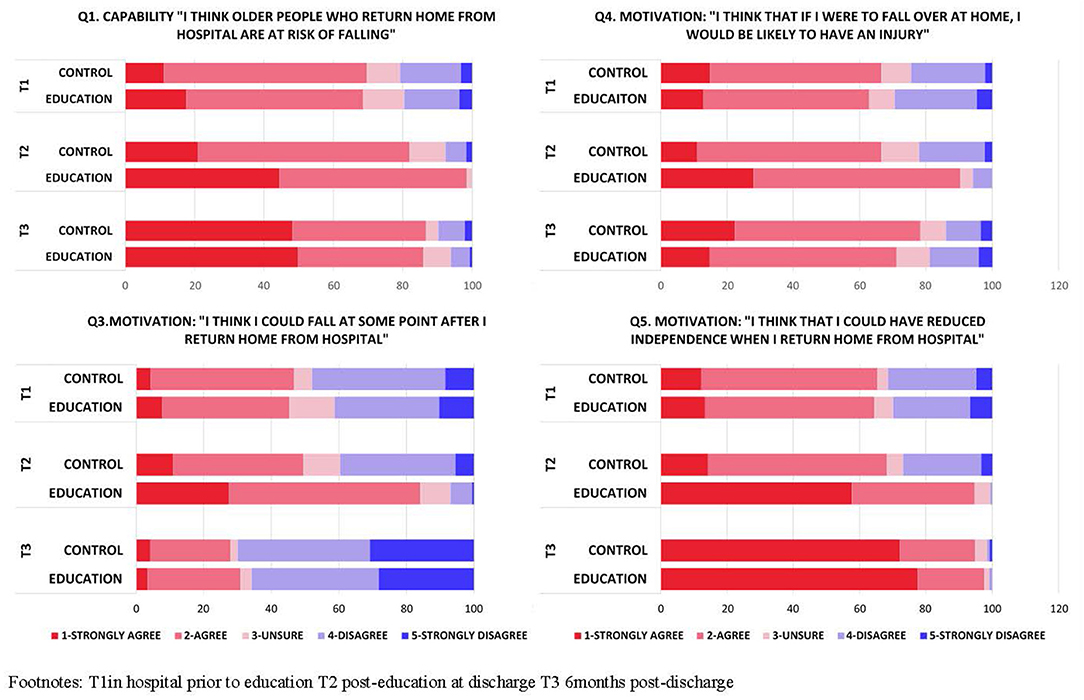
Figure 1. Change in levels of capability and motivation compared between education and control group at three timepoints.
Significant associations were found between the presence of capability and motivation outcomes and engagement in post hospitalization fall–prevention strategies in both groups (Table 3). Those participants who scored positively (strongly agree and agree) for knowledge (capability) of risk of post hospitalization falls of other older people were significantly more likely to complete an occupational therapist home (hazard) assessment [95% CI, 0.9, 3.1, p = 0.05]. Participants in both groups who were more positively aware of their own post hospitalization falls risks (motivation), were significantly more likely to complete home (hazard) modifications [95% CI, 1.0, 2.5, p = 0.03]. While participants in both groups who were more positively aware of their own post hospitalization fall-injury risks (motivation) were significantly more likely to ask for formal ADL assistance [95% CI, 1.1, 2.5, p < 0.01]. Participants in both groups who were more positively aware of their own risk of losing independence (motivation) were significantly more likely to ask for informal ADL assistance [95% CI, 0.4, 0.9, p = 0.02] and to exercise after hospitalization [95% CI, 1.2, 2.6, p < 0.01].
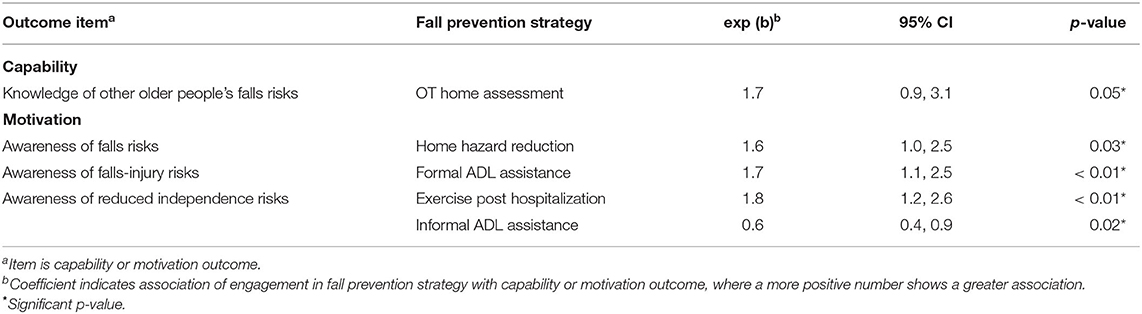
Table 3. Associations between post hospitalization engagement in fall prevention and presence of capability and motivation within groups.
Discussion
The key finding of this study was that tailored education delivered in hospital significantly improved the capability and motivation of older people to engage in fall prevention strategies at the time of hospital discharge. Although there were no significant differences between groups at 6-months follow-up (T3), the intervention group maintained their levels of capability and motivation after 6-months post hospitalization.
Tailored fall prevention education in hospital prepares patients for a gradual and safe transition home (26, 27). It also optimizes the capability and motivation of older patients to engage in fall-prevention strategies once home (2, 10). This positive change did not translate into improved or long-lasting engagement in falls prevention strategies post hospitalization (25). This implementation gap was correlated with the finding that fall incidence was not reduced (2). The results support prior studies, which show reduced participation in fall prevention strategies, such as exercises after hospitalization (12, 28). They also support prior trials showing that some older people can be passive when given a list of recommendations (29). Older people often find it easier to complete fall-prevention action plans in the hospital setting, where more structure and support is available, compared with their immediate home environment (30).
Participants who received tailored fall prevention education showed raised motivation and awareness of their own post hospitalization falls risks and likelihood of falls-injury at the time of hospital discharge. This was encouraging given that some older people do not acknowledge their own heightened fall risk (31, 32). Many are reluctant to engage in fall prevention strategies because they do not believe they are at the risk of fall (11, 12, 33).
Education recipients were not only more aware of their own risks of falls (motivation), but they were also more (capable) knowledgeable about the risk of post-discharge falls and falls injuries for other older people, at the time of hospital discharge. In contrast, participants in control group showed raised knowledge only by 6 months follow-up. Those who did not receive the education were more reliant upon their existing health knowledge and experiential learning during the post hospitalization recovery period (34, 35). This is when they are known to be more vulnerable to adverse events such as falls (2, 36).
Strengths and Limitations
The current study was conducted according to a published protocol and accompanied an RCT (20) that delivered an evidenced-based tailored education intervention with minimal drop-out (2). All outcomes were measured using blinded assessors. Most discharge studies have a limited follow-up period of 30 to 90 days (37, 38), whereas, this study explored the longer-term impact of the education on the capability and motivation for fall-prevention behavior following hospitalization of older people.
Although some external social and environmental demands were considered at the time of education delivery, some were not foreseeable to educators or patients, such as delayed provision of social assistance, and therefore could not be considered during the RCT (2). Educators prepared patients to engage with available supports delivered through hospital and community organizations, however the intervention did not provide direct support in the home and community. Participant experiences of external demands that were faced after hospital discharge, such as the availability and timing of community support, were not explored.
Conclusion
This study revealed complexities to enable behavioral change in older people who have been recently hospitalized. The tailored education delivered around the time of discharge can be helpful as it improved motivation and capability for fall prevention at the time of discharge. Participants still needed to overcome barriers to implement fall prevention activities once they returned home from hospital. These barriers represent gaps in the living environment and life-circumstances of older people after discharge from hospital. Thus, having some support to overcome these gaps in opportunity after hospitalization appear to be essential steps toward enabling older people to safely regain their independence in their home and community.
Data Availability Statement
The raw data supporting the conclusions of this article may be made available by the authors upon request.
Ethics Statement
The studies involving human participants were reviewed and approved by Human Research Ethics Committees of North Metropolitan Health Service and South Metropolitan Health Service with reciprocal approval from the University of Notre Dame Australia and Curtin University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
A-MH, CN, SM, and TH conceptualized the current study design and research protocol with ongoing expertise and support from MM, CE-B, RS, LF, MB, D-CL, JF-C, and NW. A-MH and CN led trial management including data collection and management and site procedure, in consultation with TH, MM, CE-B, LF, and NW. A-MH, CN, and SM led statistical analyses with support from TH and MB. CN led the drafting of all sections of the manuscript in consultation with A-MH, SM, MM, D-CL, CE-B, and JF-C. All authors critically revised the manuscript for important intellectual content and read and approved the final version of the manuscript.
Funding
SM, TH, MM, CE-B, RS, LF, MB, NW, and A-MH have received a grant from the National Health and Medical Research Council (Australia) to conduct a trial which investigated how to reduce falls after hospital discharge (Project App no:1078918). This grant funding has not been received directly to the authors rather to the institutions they represent. The authors have not received financial support for this study. A-MH, LF, and SM receive career funding support from the National Health and Medical Research Council (Australia).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.683723/full#supplementary-material
Supplementary Figure 1. Participant flow through the study.
Supplementary Table 1. Descriptive statistics of capability and motivation for education and control groups.
Supplementary Table 2. Capability and motivation: complete Likert-scale responses for education and control groups at baseline and follow-up.
References
1. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. (2018) 66:693–8. doi: 10.1111/jgs.15304
2. Hill AM, McPhail SM, Haines TP, Morris ME, Etherton-Beer C, Shorr R, et al. Falls after hospital discharge: a randomized clinical trial of individualized multi-modal falls prevention education. J Gerontol A Biol Sci Med Sci. (2019) 974:1511–7. doi: 10.1093/gerona/glz026
3. Hoffman GJ, Liu H, Alexander NB, Tinetti M, Braun TM, Min LC. Posthospital fall injuries and 30-day readmissions in adults 65 years and older. JAMA Netw Open. (2019) 2:e194276. doi: 10.1001/jamanetworkopen.2019.4276
4. Krumholz HM. Post-hospital syndrome — an acquired, transient condition of generalized risk. N Engl J Med. (2013) 368:100–2. doi: 10.1056/NEJMp1212324
5. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I'm not sure”. JAMA. (2011) 306:1782–93. doi: 10.1001/jama.2011.1556
6. Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. JAMA. (2010) 304:1919–28. doi: 10.1001/jama.2010.1568
7. Loyd C, Markland AD, Zhang Y, Fowler M, Harper S, Wright NC, et al. Prevalence of hospital-associated disability in older adults: a meta-analysis. J Am Med Dir Assoc. (2020) 21:455–61.e5. doi: 10.1016/j.jamda.2019.09.015
8. de Wit M, Cooper C, Tugwell P, Bere N, Kirwan J, Conaghan PG, et al. Practical guidance for engaging patients in health research, treatment guidelines and regulatory processes: results of an expert group meeting organized by the World Health Organization and the European Society for clinical and economic aspects of osteoporosis, osteoarthritis and musculoskeletal diseases. Aging Clin Exp Res. (2019) 31:905–15. doi: 10.1007/s40520-019-01193-8
9. Heavey E, Waring J, De Brún A, Dawson P, Scott J. Patients' conceptualizations of responsibility for healthcare: a typology for understanding differing attributions in the context of patient safety. J Health Soc Behav. (2019) 60:188–203. doi: 10.1177/0022146519849027
10. Hill AM, Hoffmann T, McPhail S, Beer C, Hill KD, Oliver D, et al. Evaluation of the sustained effect of inpatient falls prevention education and predictors of falls after hospital discharge–follow-up to a randomized controlled trial. J Gerontol A Biol Sci Med Sci. (2011) 66:1001–12. doi: 10.1093/gerona/glr085
11. Haines TP, Day L, Hill KD, Clemson L, Finch C. “Better for others than for me”: a belief that should shape our efforts to promote participation in falls prevention strategies. Arch Gerontol Geriatr. (2014) 59:136–44. doi: 10.1016/j.archger.2014.03.003
12. Hill AM, Hoffmann T, McPhail S, Beer C, Hill KD, Brauer SG, et al. Factors associated with older patients' engagement in exercise after hospital discharge. Arch Phys Med Rehabil. (2011) 92:1395–403. doi: 10.1016/j.apmr.2011.04.009
13. Resnick B, Palmer MH, Jenkins LS, Spellbring AM. Path analysis of efficacy expectations and exercise behaviour in older adults. J Adv Nurs. (2000) 31:1309–15. doi: 10.1046/j.1365-2648.2000.01463.x
14. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
15. Grimmer K, Moss J, Falco J. Experiences of elderly patients regarding independent community living after discharge from hospital: a longitudinal study. Int J Qual Health Care. (2004) 16:465–72. doi: 10.1093/intqhc/mzh071
16. Greysen SR, Hoi-Cheung D, Garcia V, Kessell E, Sarkar U, Goldman L, et al. “Missing pieces”—functional, social, and environmental barriers to recovery for vulnerable older adults transitioning from hospital to home. J Am Geriatr Soc. (2014) 62:1556–61. doi: 10.1111/jgs.12928
17. Naseri C, McPhail SM, Haines TP, Morris ME, Shorr R, Etherton-Beer C, et al. Perspectives of older adults regarding barriers and enablers to engaging in fall prevention activities after hospital discharge. Health Soc Care Community. (2020) 28:1710–22. doi: 10.1111/hsc.12996
18. Schulz K, Altman D, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. (2010) 18:604–12. doi: 10.1016/j.ijsu.2010.09.006
19. Hodkinson H. Evaluation of a mental test score for assessment of mental impairment in the elderly 1972. Age Ageing. (2012) 41(Suppl. 3):iii35–40. doi: 10.1093/ageing/afs148
20. Naseri C, McPhail SM, Netto J, Haines TP, Morris ME, Etherton-Beer C, et al. Impact of tailored falls prevention education for older adults at hospital discharge on engagement in falls prevention strategies postdischarge: protocol for a process evaluation. BMJ Open. (2018) 8:e020726. doi: 10.1136/bmjopen-2017-020726
21. Hill AM, Etherton-Beer C, Haines TP. Tailored education for older patients to facilitate engagement in falls prevention strategies after hospital discharge–a pilot randomized controlled trial. PLoS ONE. (2013) 8:e63450. doi: 10.1371/journal.pone.0063450
22. Hill AM, McPhail S, Hoffmann T, Hill K, Oliver D, Beer C, et al. A randomized trial comparing digital video disc with written delivery of falls prevention education for older patients in hospital. J Am Geriatr Soc. (2009) 57:1458–63. doi: 10.1111/j.1532-5415.2009.02346.x
23. Hill AM, McPhail SM, Francis-Coad J, Waldron N, Etherton-Beer C, Flicker L, et al. Educators' perspectives about how older hospital patients can engage in a falls prevention education programme: a qualitative process evaluation. BMJ Open. (2015) 5:e009780. doi: 10.1136/bmjopen-2015-009780
24. Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4th ed. Thousand Oaks, CA: SAGE Publications (2014).
25. Naseri C, McPhail SM, Haines TP, Morris ME, Etherton-Beer C, Shorr R, et al. Evaluation of tailored falls education on older adults' behavior following hospitalization. J Am Geriatr Soc. (2019) 00:1–8. doi: 10.1111/jgs.16053
26. Horwitz LI, Moriarty JP, Chen C, Fogerty RL, Brewster UC, et al. M. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. (2013) 173:1715–22. doi: 10.1001/jamainternmed.2013.9318
27. Kang E, Gillespie BM, Tobiano G, Chaboyer W. Discharge education delivered to general surgical patients in their management of recovery post discharge: a systematic mixed studies review. Int J Nurs Stud. (2018) 87:1–13. doi: 10.1016/j.ijnurstu.2018.07.004
28. Sherrington C, Lord SR, Vogler CM, Close JC, Howard K, Dean CM, et al. A post-hospital home exercise program improved mobility but increased falls in older people: a randomised controlled trial. PLoS ONE. (2014) 9:e104412. doi: 10.1371/journal.pone.0104412
29. Tinetti ME, Gordon C, Sogolow E, Lapin P, Bradley EH. Fall-risk evaluation and management: challenges in adopting geriatric care practices. Gerontologist. (2006) 46:717–25. doi: 10.1093/geront/46.6.717
30. Hill AM, McPhail SM, Waldron N, Etherton-Beer C, Ingram K, Flicker L, et al. Fall rates in hospital rehabilitation units after individualised patient and staff education programmes: a pragmatic, stepped-wedge, cluster-randomised controlled trial. Lancet. (2015) 385:2592–9. doi: 10.1016/S0140-6736(14)61945-0
31. Lee D-CA, McDermott F, Hoffmann T, Haines TP. ‘They will tell me if there is a problem': limited discussion between health professionals, older adults and their caregivers on falls prevention during and after hospitalization. Health Educ Res. (2013) 28:1051–66. doi: 10.1093/her/cyt091
32. Mihaljcic T, Haines TP, Ponsford JL, Stolwyk RJ. Investigating the relationship between reduced self-awareness of falls risk, rehabilitation engagement and falls in older adults. Arch Gerontol Geriatr. (2017) 69:38–44. doi: 10.1016/j.archger.2016.11.003
33. Shuman CJ, Montie M, Hoffman GJ, Powers KE, Doettl S, Anderson CA, et al. Older adults' perceptions of their fall risk and prevention strategies after transitioning from hospital to home. J Gerontol Nurs. (2019) 4523–30. doi: 10.3928/00989134-20190102-04
34. Beier ME, Ackerman PL. Age, ability, and the role of prior knowledge on the acquisition of new domain knowledge: promising results in a real-world learning environment. Psychol Aging. (2005) 20:341–55. doi: 10.1037/0882-7974.20.2.341
35. Dharmarajan K, Hsieh AF, Kulkarni VT, Lin Z, Ross JS, Horwitz LI, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. (2015) 350:h411. doi: 10.1136/bmj.h411
36. Hill AM, Hoffmann T, Haines TP. Circumstances of falls and falls-related injuries in a cohort of older patients following hospital discharge. Clin Interv Aging. (2013) 8:765–74. doi: 10.2147/CIA.S45891
37. Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention. J Am Geriatr Soc. (2004) 52:1817–25. doi: 10.1111/j.1532-5415.2004.52504.x
Keywords: fall prevention, hospital discharge, health behavior change, education, post-hospital home falls, older adults, physiotherapy
Citation: Naseri C, McPhail SM, Morris ME, Haines TP, Etherton-Beer C, Shorr R, Flicker L, Bulsara M, Lee D-CA, Francis-Coad J, Waldron N and Hill A-M (2021) Tailored Education Increased Capability and Motivation for Fall Prevention in Older People After Hospitalization. Front. Public Health 9:683723. doi: 10.3389/fpubh.2021.683723
Received: 22 March 2021; Accepted: 28 June 2021;
Published: 03 August 2021.
Edited by:
Isabelle Natalina Fabbricotti, Erasmus University Rotterdam, NetherlandsReviewed by:
Georgeta Vaidean, Fairleigh Dickinson University, United StatesLotte Vestjens, Erasmus University Rotterdam, Netherlands
Copyright © 2021 Naseri, McPhail, Morris, Haines, Etherton-Beer, Shorr, Flicker, Bulsara, Lee, Francis-Coad, Waldron and Hill. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chiara Naseri, Y2hpYXJhLm5hc2VyaUBjdXJ0aW4uZWR1LmF1; b3JjaWQub3JnLzAwMDAtMDAwMS04MDQxLTE4MzU=
 Chiara Naseri
Chiara Naseri Steven M. McPhail2,3
Steven M. McPhail2,3 Meg E. Morris
Meg E. Morris Ronald Shorr
Ronald Shorr Leon Flicker
Leon Flicker Max Bulsara
Max Bulsara Jacqueline Francis-Coad
Jacqueline Francis-Coad Anne-Marie Hill
Anne-Marie Hill